Abstract
Dry socket is one of the postoperative complications of tooth extraction. It is the partial or total loss of the post-extraction blood clot, resulting in severe pain that usually starts one to five days postoperatively, with clinical evidence of exposed alveolar bone, necrotic debris, halitosis, and tenderness on examination. The purpose of our systematic review was to answer the question “Is there a relationship between smoking and dry socket?”. After meeting the inclusion and exclusion criteria, eleven studies were included in this systematic review (according to the PRISMA statement guidelines). Based on a meta-analysis, tobacco smokers had a more than three-fold increase in the odds of dry socket after tooth extraction. Overall, the combined incidence of dry socket in smokers was found to be about 13.2% and in non-smokers about 3.8%. Despite the heterogeneity of the included studies (different types of teeth extracted, different age groups), cigarette smoking was related to an increased risk of dry socket after tooth extraction.
Keywords: dry socket, alveolitis, smoking, cigarettes, tooth extraction, dental surgery
1. Introduction
Tooth extraction is one of the most frequent procedures in surgical dentistry, particularly widespread during the first wave of the COVID-19 pandemic [1,2]. The indications include oral mucositis, periapical inflammation, bone loss, periodontal ligament damage, orthodontic indications, resorption of adjacent teeth [3,4]. Extraction techniques are divided into nonsurgical extractions and surgical extractions. Nonsurgical extractions require simple elevation or separation of the root without reflection of the mucoperiosteal flap. Surgical extractions need the reflection of the mucoperiosteal flap with or without bone removal [5,6]. Tooth extraction is associated with complications both during and after the procedure [7]. The most common complications are prolonged bleeding, purulent alveolitis, postoperative pain, and dry socket [8].
As mentioned above, one of the more common complications is dry socket [9]. Dry socket is the partial or total loss of the post-extraction blood clot. It usually starts with severe pain one to five days postoperatively, what is accompanied by clinical symptoms such as exposed alveolar bone, necrotic debris, and halitosis. Other terms for this condition include alveolar osteitis, fibrinolytic alveolitis, localised osteomyelitis, postoperative alveolitis, and alveolitis sicca [10]. The pathogenesis of dry socket remains still unclear [11]. The most popular theory is the disintegration of the blood clot in the alveolus caused by elevated fibrinolytic activity. The initiation of the fibrinolysis is reported to be associated with several factors such as the following: age, gender, smoking habits, oral contraceptives use, menstrual cycle, surgery duration, surgical trauma, condition of the extracted teeth, type of the extracted teeth, presence of a previous periapical or pericoronal infection, inadequate curettage or irrigation of the socket after extraction, excessive use of local anaesthetic with vasoconstrictor [12].
The adverse effects of cigarette smoking on oral health are well established, extending from cosmetic effects, such as tooth staining, to potentially life-threatening conditions such as oral cancer [13]. Particularly, pathological effects of smoking on periodontal tissues that render smokers more susceptible to periodontal disease have been reviewed in the literature [14,15]. Previous studies present that smokers demonstrate a higher prevalence, severity, and progression of periodontitis compared to former smokers or non-smokers. Moreover, tobacco smoking negatively influences nonsurgical and surgical periodontal therapy, including regenerative and plastic surgeries. Although heavy cigarette smokers suffer from more severe forms of periodontitis and unfavourable treatment prognosis, quitting smoking decreases the progression of periodontal destruction and leads to better clinical outcomes [16]. The systematic review by Ralho et al. [17] suggests that the use of electronic cigarettes is less harmful to oral health. However, the authors observed a greater susceptibility to developing different lesions of the oral mucosa than ex-smokers or non-smokers.
Our systematic review was designed in order to answer the question “Is there a relationship between smoking and dry socket?”, formulated according to PICO (population, intervention, comparison, and outcome).
2. Materials and Methods
2.1. Search Strategy and Data Extraction
A systematic review was conducted up to 10th March 2022, according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement guidelines [18], using the databases PubMed, Scopus, and Web of Science. The search formulas included:
-
-
For PubMed: ((dry socket) OR (dry alveol*) OR (alveolar osteitis) OR (alveolitis osteitis) OR (fibrynolitic alveolitis)) AND ((smoker*) OR (alcoholic*) OR (smoking) OR (alcohol consumption) OR (cigarette) OR (nicotine) OR (tobacco) OR (alcohol) OR (alcohol addiction) OR (cigarette addiction))
-
-
For Scopus: TITLE-ABS-KEY ((“dry socket”) OR (“dry alveol*”) OR (“alveolar osteitis”) OR (“alveolitis osteitis”) OR (“fibrynolitic alveolitis”)) AND ((smoker*) OR (alcoholic*) OR (smoking) OR (“alcohol consumption”) OR (cigarette) OR (nicotine) OR (tobacco) OR (alcohol) OR (“alcohol addiction”) OR (“cigarette addiction”))
-
-
For Web of Science: TS = (dry socket OR dry alveol* OR alveolar osteitis OR alveolitis osteitis OR fibrynolitic alveolitis) AND TS = (smoker* OR alcoholic* OR smoking OR alcohol consumption OR cigarette OR nicotine OR tobacco OR alcohol OR alcohol addiction OR cigarette addiction).
The results were filtered by publication date (after 2000).
Records were screened by the title, abstract, and full text by two independent investigators. Studies included in this review matched all the predefined criteria according to PICOS (population, intervention, comparison, outcome, and study design), as shown in Table 1. A detailed search flowchart is presented in the Results section. The study protocol was registered in the international prospective register of systematic reviews PROSPERO (CRD42022336307).
Table 1.
Inclusion and exclusion criteria according to the PICOS.
| Parameter | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | patients with dry socket—both genders, regardless of age | patients with other complications after tooth extraction |
| Intervention | smoking | |
| Comparison | non-smoking | |
| Outcomes | prevalence of dry socket | prevalence of dry socket with other predisposing factors, such as alcohol, contraceptives, or water pipe |
| Study design | case-control, cohort and cross-sectional studies | literature reviews, case reports, expert opinion, conference reports |
| published after 2000 | not published in English |
The results of the meta-analysis are presented in forest plots using MedCalc Statistical Software version 19.5.3 (MedCalc Software Ltd., Ostend, Belgium) and Statistica 13.3 software (StatSoft, Cracow, Poland).
2.2. Quality Assessment and Critical Appraisal for the Systematic Review of Included Studies
The risk of bias in each individual study was assessed according to the study quality assessment tool issued by the National Heart, Lung, and Blood Institute within the National Institute of Health [19]. These questionnaires were answered by two independent investigators, and any disagreements were resolved by discussion between them.
The summarised quality assessment for every single study is reported in Figure 1. Critical appraisal was summarised by adding up the points for each criterion of potential risk (points: 1—low, 0.5—unspecified, 0—high). Nine studies (81.8%) were classified as having “good” quality (≥80% total score) and two (18.2%) as “intermediate” (≥60% total score).
Figure 1.
Quality assessment, including the main potential risk of bias (risk level: green—low, yellow—unspecified, red—high; quality score: green—good, yellow—intermediate, red—poor) [21,22,23,24,25,26,27,28,29,30,31].
The level of evidence was assessed using the classification of the Oxford Centre for Evidence-Based Medicine levels for diagnosis [20]. All of the included studies have the third or fourth level of evidence (in this 5-graded scale).
3. Results
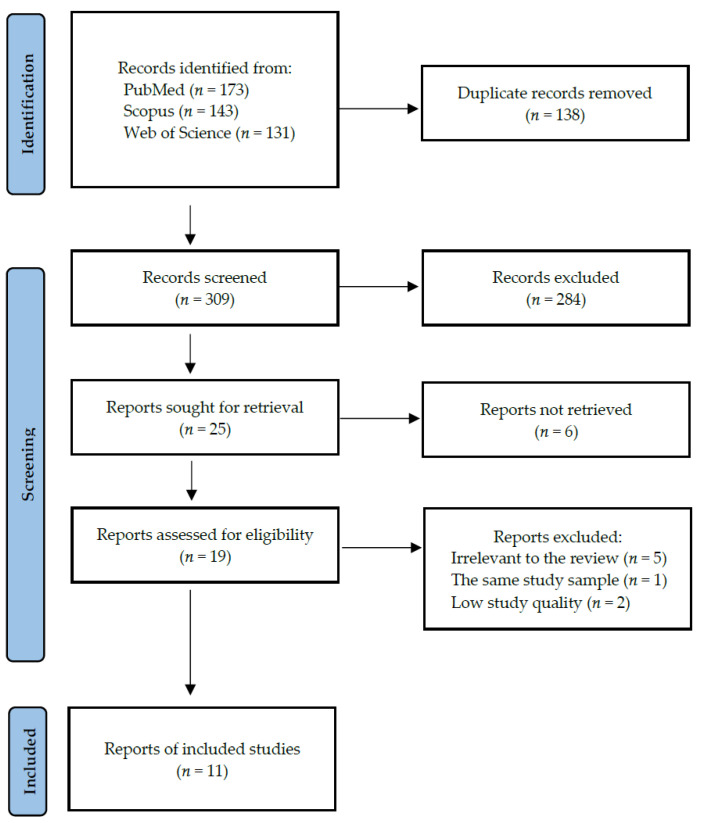
Following the search criteria, our systematic review included eleven studies, demonstrating data collected in ten different countries from a total of 10195 participants (including 3007 smokers and 7188 non-smokers). Figure 2 shows the detailed selection strategy of the articles. The inclusion and exclusion criteria are presented in Table 1 (in the Materials and Methods section).
Figure 2.
PRISMA flow diagram presenting search strategy.
From each eligible study included in the present systematic review, we collected data about its general characteristics, such as year of publication and setting, involved participants (gender and age), smoking status, inclusion and exclusion criteria, medical history, oral hygiene (Table 2). Table 3 presents the detailed characteristics considering prevalence of dry socket, kind of extracted tooth, extraction technique, symptoms recognised as the onset of dry socket, and provided prophylaxis or treatment.
Table 2.
General characteristics of included studies.
| Author, Year, Setting | Participants (F/M) | Age (Years) | Smoking Status (% of Smokers) | Inclusion Criteria | Exclusion Criteria | Comorbidities | Oral Hygiene Status |
|---|---|---|---|---|---|---|---|
| Al-Belasy, 2004, Egypt [21] | 200 (0/100) | mean 27 (range: 20–38) | 50.0 | patients who were treated at the Oral Surgery Department, Faculty of Dentistry, Mansoura University between January 2000 and February 2002, healthy patients required to have unilateral high mesioangular impactions of a mandibular third molar with an exposed occlusal surface | women, former smokers, men who smoked both cigarettes and shisha, patients with recent antibiotic use, and patients with medical need for prophylactic antibiotics | 100% no systemic disease | NR |
| Alsaleh et al., 2018 Kingdom of Saudi Arabia [22] | 201 (79/122) | NR | 26.4 | patients classified as ASA I (healthy patients) and ASA II (patients with mild, controlled systemic disease without functional limitation), patients with a history of nonsurgical extraction of a permanent tooth | patients who required treatment under general anaesthesia, children under 6 years of age who have not yet grown permanent teeth, and all patients with exodontia of primary teeth and retained teeth | 90.1% no systemic disease | NR |
| Bortoluzzi et al., 2012, Brazil [23] | 793 (337/456) | 41.6 ± 16.0 (range: 9–85) | 23.3 | simple and erupted teeth exodontia, procedures conducted by undergraduate students under similar conditions between March 2007 and December 2011 | extractions of third molars that had not fully erupted and/or were classified as difficult for undergraduate students to remove and extractions of deciduous teeth | NR | NR |
| Eshghpour & Nejat, 2013, Iran [24] | 189 (91/98) | 18–48 | 40.7 | extraction of impacted third mandibular molar teeth performed between April 2009 and August 2010 in Dental Clinic of Oral and Maxillofacial Surgery | NR | 86.0% no systemic disease | prior to surgery, all the patients underwent a thorough scaling and oral prophylaxis |
| Halabí et al., 2012, Chile [25] | 1302 (90/1212) | 39.7 ± 16 | 4.4 | patients who underwent dental extraction from March to June 2011 in dental clinic in Valdiva, Chile | extraction in the operating theatre necessary, residents of rural areas who did not present themselves for the follow-up, patients undergoing antimicrobial therapy | 96.8% no systemic disease | 8% poor oral hygiene |
| Heng et al., 2007 USA [26] | 219 (219/0) | mean 37.7 | 61.1 | inmates who had tooth extractions in the 8 months before the smoking ban (January 2004–August 2004) and 8 months after the ban (September 2004–April 2005) | inmates whose tooth extractions were performed at different times | NR | NR |
| López-Carriches et al., 2006, Spain [27] | 64 (46/18) | mean 23.5 (range: 18–53) | 48.4 | patients subjected to lower third molar extraction in the Unit of Oral and Maxillofacial Surgery (Madrid Complutense University, Spain), healthy volunteers over age 18 years and requiring surgical lower third molar extraction, absence of systemic disease, absence of any habitual medication | pregnant or nursing women, allergy to local anaesthetics, antibiotics, or analgesics, patients with cardiovascular disease or any other systemic pathology | 100% no systemic disease | 68.8% of the patients claimed not to have brushed in the zone at the time of suture removal |
| Momeni et al., 2011 Iran [28] | 4779 (2197/2581) | with dry socket 36.61 ± 13.59, without dry socket 42.86 ± 15.49 | 34.7 | patients referred to dental clinics in Yazd for tooth extraction between May 2010 and June 2010 | patients referred to dental clinics in Yazd for tooth extraction in another time period | 63.7% no systemic disease | 64% poor oral hygiene |
| Parthasarathi et al., 2011, Australia [29] | 284 (142/142) | NR | 30.8 | patients having an exodontia procedure at 4 comparable public dental clinics in Victoria between June and September 2008 | patients who underwent an exodontic procedure at 4 comparable public dental clinics in Victoria during a different time period | 47.0% no systemic disease | 85.3% poor oral hygiene |
| Schwartz-Arad et al., 2018, Israel [30] | 463 (257/206) | mean 29 (range: 13–75) | 26.0 | patients having third molar extractions at Schwartz Arad Surgical Center between 2001 and 2011 | patients having extractions of a tooth other than a third molar | NR | NR |
| Vettori et al., 2019, Italy [31] | 1701 (845/876) | 55.3 ± 19.9 | 29.7 | patients who underwent single or multiple tooth extractions between June 2015 and February 2016 at the University of Trieste | patients subjected to periodontal surgery or major oral surgery, patients without specification of which antibiotic was prescribed after extraction | 40.0% no systemic disease | caries was the reason of 57% extractions and periodontitis was of 31% |
Legend: F, females; M, males; NR, not reported; ASA, American Society of Anaesthesiologists; USA, the United States of America.
Table 3.
Detailed characteristics of included studies considering prevalence of dry socket.
| Study | Prevalence of Dry Socket in All Patients [%] | Prevalence of Dry Socket in Smokers [%] | Tooth Extracted | Extraction Technique | Symptoms Recognised as the Onset of Dry Socket | Provided Prophylaxis or Treatment |
|---|---|---|---|---|---|---|
| Al-Belasy, 2004 [21] | 11.5 | 16.0 | 100% impacted mandibular third molars | 100% atraumatic extractions | constant radiating pain not relieved by the analgesic, accompanied by a denuded socket or necrotic clot and a fetid smell | postoperative medications given orally for analgesia were naproxen or diflunisal at a dose of 500 mg twice daily; if dry socket was diagnosed, sockets were irrigated with saline and packed with a eugenol-iodoform dressing |
| Alsaleh et al., 2018 [22] | 7.0 | 9.4 | all teeth except retained third molars | single tooth extractions | severe pain at the extraction site within 3 days, no blood clot at the extraction site, visible bone at the extraction site, bad breath, bad taste in mouth | patients were given post-extraction instructions verbally after the extraction |
| Bortoluzzi et al., 2012 [23] | 1.3 | 2.7 | all kinds of fully erupted teeth | 12% traumatic extractions, 88% simple extractions | NR | NR |
| Eshghpour & Nejat, 2013 [24] | 25.9 | 35.1 | 100% impacted mandibular third molars | 100% traumatic extractions | 1 to 3 days after extraction with severe pain, halitosis, foul taste, and regional lymphadenitis; no blood clot in the socket and the bone is exposed | flap sutured using 3-0 silk suture; regimen of amoxicillin (500 mg) and Gelofen (400 mg cap, TID, for maximum 3 days) was prescribed |
| Halabí et al., 2012 [25] | 6.1 | 57.9 | 93.6% maxillary, 6.4% mandibular | 4.9% traumatic extractions, 95.1% simple extractions | increasing postoperative pain intensity for 4 days within and around the socket and/or total or partial breakdown of the blood clot in the socket with or without bone exposure | reported measures for alleviating alveolar osteitis in high-risk patients include local treatment with tetracycline or preoperative and 7-day postoperative rinsing with 0.12% chlorhexidine |
| Heng et al., 2007 [26] | 5.0 | 6.7 | 83.1% maxillary, 16.9% mandibular | 27.9% traumatic extractions, 72.1% simple extractions | alveolar osteitis, pain, swelling, bleeding | patients received a verbal and written postoperative recommendation, usually ibuprofen as an analgesic; for postoperative complaints, patients had open access to the clinic |
| López-Carriches et al., 2006 [27] | 3.1 | 6.5 | 100% lower third molar | NR | wound appearance and condition were assessed in terms of colour, marginal swelling, ulceration, the presence of plaque | no antibiotic treatment was prescribed postoperatively, and the patients received only metamizole as analgesic treatment, diclofenac was also prescribed as antiinflammatory treatment |
| Momeni et al., 2011 [28] | 0.6 | 0.6 | 36.3% maxillary, 63.7% mandibular | NR | throbbing pain, oral malodour, and unpleasant taste; onset of symptoms 42–72 h after tooth extraction and there is no redness or purulent discharge at the affected sites | palliative intervention with prescribing anti-inflammatory drugs |
| Parthasarathi et al., 2011 [29] | 4.2 | 4.6 | 38.8% maxillary, 61.2% mandibular | 17% traumatic extractions, 83% simple extractions | the patient’s history of pain and the presence of exposed bone, intraorally | NR |
| Schwartz-Arad et al., 2018 [30] | 11.7 | 33.3 | 100% third molar extraction | NR | NR | all patients were prescribed oral antibiotics (amoxicillin 1.5 g for 5 days) or clindamycin (1.2 mg for 4 days), and dexamethasone (4 mg for 2 days); rinsing with 0.25% chlorohexidine continued twice a day for 10 days after extraction; naproxen was provided as a nonsteroidal anti-inflammatory drug twice a day |
| Vettori et al., 2019 [31] | 3.2 | 5.5 | 51% maxillary, 49% mandibular | 15.7% traumatic extractions, 84.3% simple extractions | NR | almost all surgical sites had been sutured, in 10.47% of cases the patient had started an antibiotic therapy before the intervention; after the intervention, the surgeon prescribed antibiotic therapy to 9.23% of patients, steroids to 0.24% of patients, NSAIDs to 3% of patients |
Legend: NR, not reported; TID, three times a day; NSAIDs, non-steroidal anti-inflammatory drugs.
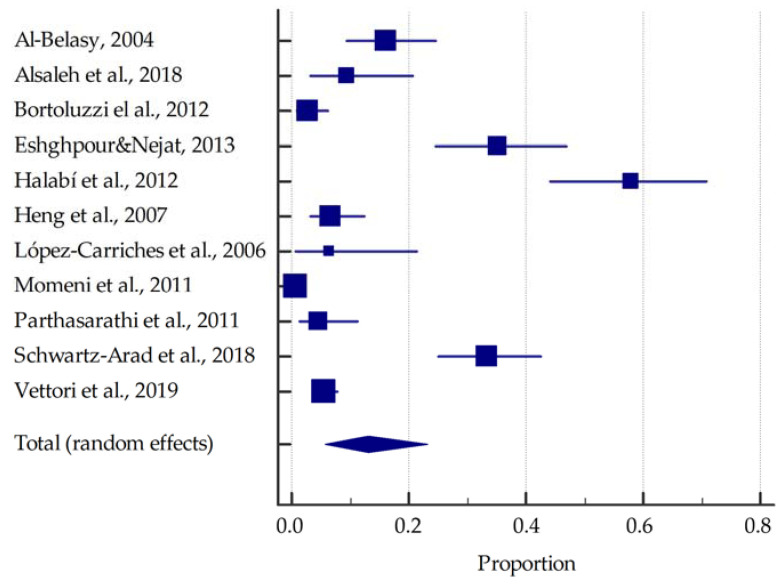
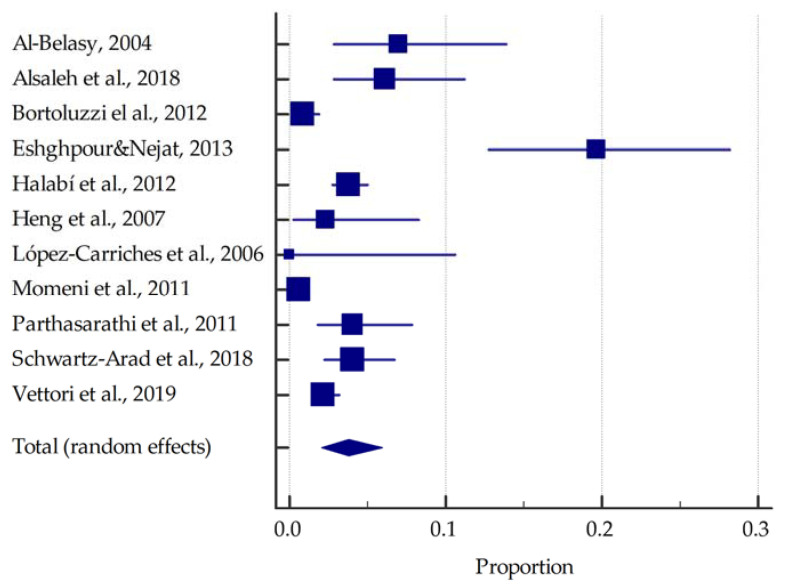
On the basis of the included studies reporting the prevalence of dry socket in smokers, it was determined that the summarised prevalence is approximately 13.2% (95%CI: 5.8–23.1%) (Figure 3). In contrast, in non-smokers the summarised prevalence of dry socket was estimated to be around 3.8% (95%CI: 2.1–6.0%) (Figure 4).
Figure 3.
Forest plot presenting the summarised prevalence of dry socket among smokers [21,22,23,24,25,26,27,28,29,30,31].
Figure 4.
Forest plot presenting the summarised prevalence of dry socket among non-smokers [21,22,23,24,25,26,27,28,29,30,31].
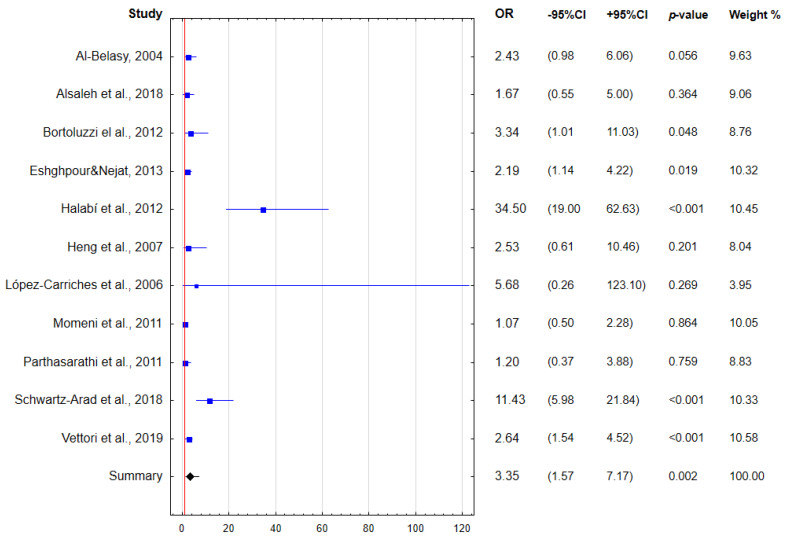
Altogether, regular smoking is associated with a more than three-fold increase in the odds of dry socket after tooth extraction (Figure 5).
Figure 5.
Forest plot presenting the odds for dry socket considering regular smoking (OR—odds ratio; CI—confidence interval) [21,22,23,24,25,26,27,28,29,30,31].
4. Discussion
Our systematic review found an association between the dry socket occurrence and cigarette smoking. Because of the type of extraction (surgical/nonsurgical), type of tooth extracted, and amount of cigarette smoking, it is difficult to relate the summarised results to individual studies. Therefore, the literature discussed sequentially begins with simple extractions of all kinds and ends with the literature about only retained third molars. An additional criterion for the studies discussed was the number of cigarettes smoked.
Halabi et al. [25] presented a logistic regression analysis of risk factors for the alveolitis development. Prior extraction site infection, surgical trauma, and smoking habits were associated with an increased risk of dry socket. They included 1302 participants who underwent tooth extractions in their study. Extractions were performed on all types of teeth. Tobacco use was assessed as smoking (above 5 cigarettes 24 h after extraction) or non-smoking (below 5 cigarettes 24 h after extraction). The incidence of alveolar osteitis was 6.8% in patients overall. However, in smokers, the dry socket incidence was 58%.
In the most recent study, Vettori et al. [31] discussed the factors affecting the occurrence of intraoperative and postoperative complications after tooth extraction: a retrospective study on a group of 1701 patients. They extracted every type of tooth. This study aimed to evaluate the type and frequency of complications after exodontic procedures, their correlation with antibiotic administration and with patient-related systemic factors. Smoking habits and presented coagulopathy were associated with higher risk of postoperative alveolitis. Based on the results presented here, antibiotic intake did not appear to reduce the incidence of postoperative infectious complications.
Bortoluzzi et al. [23] attempted to answer whether smoking increases the incidence of postoperative complications after simple extractions. They conducted a single-centre, prospective study of postoperative complications in the alveolar process. Excluded from the study were extractions of third molars that had not fully erupted or were classified as difficult to remove by students, as well as extractions of deciduous teeth. Logistic regression showed that tooth dissection, smoking, and the number of cigarettes smoked (>20 cigarettes per day) were associated with the occurrence of dry socket.
In contrast, Parthasaranthi et al. [29] obtained different results from the other authors. They discussed several factors that could be associated with the occurrence of dry socket. In their study, they examined tooth extractions of all types. Logistic regression analysis showed that posterior teeth, teeth extracted due to periapical disease, intraoperative crown-root fractures, teeth extracted by specialists or dentists, and psychotropic medication history were significant independent factors for the alveolar osteomyelitis development. However, the most important finding of the study was that smoking habits and extraction techniques (nonoperative or operative) were not found to significantly influence the alveolitis development.
Momeni et al. [28] evaluated distribution and risk factors in patients with dry socket referring to their dental clinics after extractions of all types of teeth. The results showed that alveolitis was more common in women than in men. The ratio of mandible to maxilla was 2.5 to 1, and mandibular third molars were more often involved than other teeth. Smoking habits, poor oral hygiene, and surgical trauma increased the dry socket incidence
Similarly, Alshaleh et al. [22] discussed how patients’ behaviours after tooth extraction affect the development of dry socket. For their study, they did not consider retained third molars. Among other things, 26.4% of the patients were smokers. These participants were instructed not to smoke for the next three days, some of them complied, and some did not. In total, 68% of the smokers smoked on the extraction day, and the rest did not smoke (for the next 72 h). There was no significant association between smokers and patients who developed dry alveolus.
Heng et al. [26] examined the relationship between cigarette smoking and dry socket incidence in the total number of extractions, only for third molar extractions. They found a significant difference in the incidence of overall complications between smokers and non-smokers. There was a significant difference in the incidence of alveolar osteitis between mandibular third molar extractions and other extractions regardless of smoking status. Moreover, surgical trauma contributed significantly to the increase in overall complications and alveolar osteitis, as well as smoking seemed to be a causative factor to the increase in complications among multiple extractions. In this study, smoking habits, mandibular third molars, and surgical trauma were significantly related to higher rates of postoperative complications, including alveolitis.
The first study that focused on the lower third molars was conducted by Lopez-Carriches et al. [27]. Although two cases of alveolitis were documented among smokers, there was no statistically significant difference between these groups in pain complaints, but trismus was higher in smokers. Smoking habits had no effect on wound condition.
Another study focusing on third molars was performed in an Iranian population by Eshghpour and Nejat [24]. They found that some factors such as gender, systemic diseases, age, and use of antibiotics before surgery showed no significant association with the alveolitis incidence. However, the incidence of dry socket was significantly associated with smoking. In addition to smoking, other factors associated with the incidence of dry alveolus were: the difficulty of the surgery, length of the surgery, oral contraceptives use, menstrual cycle, and number of carpules used to achieve anaesthesia.
Al-Belasy [21] also focused on the same type of teeth as the previous article mentioned above. His study found that smokers had a two- to three-fold higher risk of dry socket than non-smokers. Patients who smoked on the day of surgery had a significantly higher incidence of dry socket than ones who smoked on the second day after surgery. Increased frequency of smoking and smoking on the day of surgery significantly elevated the prevalence of dry socket.
Lastly, Schwartz-Arad et al. [30] analysed the incidence of complications after third molar extraction according to risk factors. The most common complication in this study was dry socket. Partially retained teeth had the highest incidence of complications. Cigarette smoking was associated with a higher incidence of dry sockets, and complications were more common on the left side. The authors concluded that complications after mandibular third molar surgical removal increase with smoking habits, age, degree of enucleation, and extraction site.
The practical value of our systematic review should be emphasised, confirming the potential relationship between the negative habit of smoking by patients and the occurrence of complications after surgical procedures, such as dry socket. From a clinical point of view, the obtained results oblige dentists to intensify pro-health education of patients in order to avoid the harmful effects of the cigarettes. The conducted systematic review had limitations related to the heterogeneity of the included studies. The main reasons of potential bias include different age groups of patients, gender, and racial diversity, as well as different tooth extraction techniques and types of extracted teeth. Moreover, the selected research design models and the various sizes of the studied samples were not without significance. Therefore, further prospective studies on larger groups of patients are necessary, taking into account in detail the frequency of smoking, the use of other stimulants or the presence of comorbidities.
5. Conclusions
Cigarette smoking is related to an increased risk of dry socket. Our review found that approximately 13.2% of cigarette smokers developed a dry socket after tooth extraction. However, it is difficult to establish clear associations due to the heterogeneity of the included studies (different types of extracted teeth, different age groups).
Author Contributions
Conceptualisation, K.B., W.K. and K.N.; methodology, K.N.; formal analysis, K.N.; investigation and data curation, K.B., W.K. and K.N.; writing—original draft preparation, K.B., W.K. and K.N.; writing—review and editing, K.N. and A.S.; visualisation, K.N.; supervision, A.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nijakowski K., Cieślik K., Łaganowski K., Gruszczyński D., Surdacka A. The Impact of the COVID-19 Pandemic on the Spectrum of Performed Dental Procedures. Int. J. Environ. Res. Public Health. 2021;18:3421. doi: 10.3390/ijerph18073421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cagetti M.G., Balian A., Camoni N., Campus G. Influence of the COVID-19 Pandemic on Dental Emergency Admissions in an Urgent Dental Care Service in North Italy. Int. J. Environ. Res. Public Health. 2021;18:1812. doi: 10.3390/ijerph18041812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farooq Z., Waqar A., Saeed A. Incidence and Treatment of Complications in Patients Who Had Third Molars or Other Teeth Extracted. Indoam. J. Pharm. Sci. 2018;5:8540–8545. doi: 10.5281/zenodo.1413644. [DOI] [PubMed] [Google Scholar]
- 4.Cahen P.M., Frank R.M., Turlot J.C. A Survey of the Reasons for Dental Extractions in France. J. Dent. Res. 1985;64:1087–1093. doi: 10.1177/00220345850640081401. [DOI] [PubMed] [Google Scholar]
- 5.Nusair Y.M., Younis M.H.A. Prevalence, Clinical Picture, and Risk Factors of Dry Socket in a Jordanian Dental Teaching Center. J. Contemp. Dent. Pract. 2007;8:53–63. doi: 10.5005/jcdp-8-3-53. [DOI] [PubMed] [Google Scholar]
- 6.Abu Younis M.H., Abu Hantash R.O. Dry Socket: Frequency, Clinical Picture, and Risk Factors in a Palestinian Dental Teaching Center. Open Dent. J. 2011;5:7–12. doi: 10.2174/1874210601105010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grossi G.B., Maiorana C., Garramone R.A., Borgonovo A., Creminelli L., Santoro F. Assessing Postoperative Discomfort after Third Molar Surgery: A Prospective Study. J. Oral Maxillofac. Surg. 2007;65:901–917. doi: 10.1016/j.joms.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 8.Bouloux G.F., Steed M.B., Perciaccante V.J. Complications of Third Molar Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2007;19:117–128. doi: 10.1016/j.coms.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 9.Saravanan K., Santhosh Kumar M.P. Assessment of Post Extraction Complications in Indians. Bioinformation. 2021;17:1120–1125. doi: 10.6026/973206300171120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akinbami B.O., Godspower T. Dry Socket: Incidence, Clinical Features, and Predisposing Factors. Int. J. Dent. 2014;2014:796102. doi: 10.1155/2014/796102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghosh A., Aggarwal V.R., Moore R. Aetiology, Prevention and Management of Alveolar Osteitis-A Scoping Review. J. Oral Rehabil. 2022;49:103–113. doi: 10.1111/joor.13268. [DOI] [PubMed] [Google Scholar]
- 12.Bortoluzzi M.C., Manfro R., De Déa B.E., Dutra T.C. Incidence of Dry Socket, Alveolar Infection, and Postoperative Pain Following the Extraction of Erupted Teeth. J. Contemp. Dent. Pract. 2010;11:33–40. doi: 10.5005/jcdp-11-1-33. [DOI] [PubMed] [Google Scholar]
- 13.Giorgetti A.P.O., César Neto J.B., Casati M.Z., Sallum E.A., Nociti Júnior F.H. Cigarette Smoke Inhalation Influences Bone Healing of Post-Extraction Tooth Socket: A Histometric Study in Rats. Braz. Dent. J. 2012;23:228–234. doi: 10.1590/S0103-64402012000300008. [DOI] [PubMed] [Google Scholar]
- 14.Jiang Y., Zhou X., Cheng L., Li M. The Impact of Smoking on Subgingival Microflora: From Periodontal Health to Disease. Front. Microbiol. 2020;11:66. doi: 10.3389/fmicb.2020.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chou H.-H., Lu S.-L., Wang S.-T., Huang T.-H., Chen S.L.-S. The Association between Bone Mineral Density and Periodontal Disease in Middle-Aged Adults. Int. J. Environ. Res. Public Health. 2021;18:3321. doi: 10.3390/ijerph18063321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramôa C.P., Eissenberg T., Sahingur S.E. Increasing Popularity of Waterpipe Tobacco Smoking and Electronic Cigarette Use: Implications for Oral Healthcare. J. Periodontal. Res. 2017;52:813–823. doi: 10.1111/jre.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ralho A., Coelho A., Ribeiro M., Paula A., Amaro I., Sousa J., Marto C., Ferreira M., Carrilho E. Effects of Electronic Cigarettes on Oral Cavity: A Systematic Review. J. Evid.-Based Dent. Pract. 2019;19:101318. doi: 10.1016/j.jebdp.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Heart, Lung, and Blood Institute, National Institutes of Health Study Quality Assessment Tools. [(accessed on 22 August 2020)]; Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 20.Oxford Centre for Evidence-Based Medicine Levels of Evidence. [(accessed on 22 August 2020)]. Available online: https://www.cebm.net/2016/05/ocebm-levels-of-evidence.
- 21.Al-Belasy F.A. The Relationship of “Shisha” (Water Pipe) Smoking to Postextraction Dry Socket. J. Oral Maxillofac. Surg. 2004;62:10–14. doi: 10.1016/j.joms.2002.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Alsaleh M.K., Alajlan S.S., Alateeq N.F., Alamer N.S., Alshammary F., Alhobeira H.A., Khan S., Siddiqui A.A. Alveolar Osteitis: Patient’s Compliance with Post-Extraction Instructions Following Permanent Teeth Extraction. J. Contemp. Dent. Pract. 2018;19:1518–1525. doi: 10.5005/jp-journals-10024-2459. [DOI] [PubMed] [Google Scholar]
- 23.Bortoluzzi M.C., Capella D.L., Barbieri T., Marchetti S., Dresch C.P., Tirello C. Does Smoking Increase the Incidence of Postoperative Complications in Simple Exodontia? Int. Dent. J. 2012;62:106–108. doi: 10.1111/j.1875-595X.2011.00098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eshghpour M., Nejat A.H. Dry Socket Following Surgical Removal of Impacted Third Molar in an Iranian Population: Incidence and Risk Factors. Niger. J. Clin. Pract. 2013;16:496–500. doi: 10.4103/1119-3077.116897. [DOI] [PubMed] [Google Scholar]
- 25.Halabí D., Escobar J., Muñoz C., Uribe S. Logistic Regression Analysis of Risk Factors for the Development of Alveolar Osteitis. J. Oral Maxillofac. Surg. 2012;70:1040–1044. doi: 10.1016/j.joms.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 26.Heng C.K., Badner V.M., Clemens D.L., Mercer L.T., Mercer D.W. The Relationship of Cigarette Smoking to Postoperative Complications from Dental Extractions among Female Inmates. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007;104:757–762. doi: 10.1016/j.tripleo.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 27.López-Carriches C., Gómez-Font R., Martínez-González J.M., Donado-Rodríguez M. Influence of Smoking upon the Postoperative Course of Lower Third Molar Surgery. Med. Oral Patol. Oral Cir. Bucal. 2006;11:56–60. [PubMed] [Google Scholar]
- 28.Momeni H., Shahnaseri S., Hamzeheil Z. Evaluation of Relative Distribution and Risk Factors in Patients with Dry Socket Referring to Yazd Dental Clinics. Dent. Res. J. 2011;8:S84–S87. [PMC free article] [PubMed] [Google Scholar]
- 29.Parthasarathi K., Smith A., Chandu A. Factors Affecting Incidence of Dry Socket: A Prospective Community-Based Study. J. Oral Maxillofac. Surg. 2011;69:1880–1884. doi: 10.1016/j.joms.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz-Arad D., Lipovsky A., Pardo M., Adut O., Dolev E. Interpretations of Complications Following Third Molar Extraction. Quintessence Int. 2018;49:33–39. doi: 10.3290/j.qi.a39334. [DOI] [PubMed] [Google Scholar]
- 31.Vettori E., Costantinides F., Nicolin V., Rizzo R., Perinetti G., Maglione M., Di Lenarda R. Factors Influencing the Onset of Intra- and Post-Operative Complications Following Tooth Exodontia: Retrospective Survey on 1701 Patients. Antibiotics. 2019;8:264. doi: 10.3390/antibiotics8040264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on request from the corresponding author.