Abstract
Objective:
Using data from a cohort of World Trade Center (WTC) rescue and recovery workers with asthma, we assessed whether meeting criteria for post-traumatic stress disorder (PTSD), sub-threshold PTSD, and for specific PTSD symptom dimensions are associated with increased asthma morbidity.
Methods:
Participants underwent a Structured Clinical Interview for Diagnostic and Statistical Manual to assess the presence of PTSD following DSM-IV criteria during in-person interviews between December 2013 and April 2015. We defined sub-threshold PTSD as meeting criteria for two of three symptom dimensions: re-experiencing, avoidance, or hyper-arousal. Asthma control, acute asthma-related healthcare utilization, and asthma-related quality of life data were collected using validated scales. Unadjusted and multiple regression analyses were performed to assess the relationship between sub-threshold PTSD and PTSD symptom domains with asthma morbidity measures.
Results:
Of the 181 WTC workers with asthma recruited into the study, 28% had PTSD and 25% had sub-threshold PTSD. Patients with PTSD showed worse asthma control, higher rates of inpatient healthcare utilization, and poorer asthma quality of life than those with sub-threshold or no PTSD. After adjusting for potential confounders, among patients not meeting the criteria for full PTSD, those presenting symptoms of re-experiencing exhibited poorer quality of life (p = 0.003). Avoidance was associated with increased acute healthcare use (p = 0.05). Sub-threshold PTSD was not associated with asthma morbidity (p > 0.05 for all comparisons).
Conclusions:
There may be benefit in assessing asthma control in patients with sub-threshold PTSD symptoms as well as those with full PTSD to more effectively identify ongoing asthma symptoms and target management strategies.
Keywords: Asthma, asthma management, asthma morbidity, asthma outcomes, PTSD, stress, sub-threshold PTSD, trauma, WTC, 9/11
Introduction
Asthma and post-traumatic stress disorder (PTSD) are among the most common chronic conditions affecting World Trade Center (WTC) rescue and recovery workers [1]. A systematic review of the mental health of WTC rescue and recovery workers [2] reported that first responders were 11 times more likely to suffer from PTSD than the general population. Estimates of the prevalence of PTSD among WTC rescue and recovery workers vary, with some studies reporting rates as high as 32% 9 years after exposure [1]. Similarly, rates of asthma are relatively high in this population, with prevalence estimates ranging from 12% [3] to 28% [1]. Studies also report substantial burden of asthma morbidity among WTC rescue and recovery workers [4]. Thus, PTSD and asthma are a major source of morbidity and have a substantial impact on this population’s quality of life.
Prior studies suggest that PTSD may lead to asthma [5-7], and that rates of comorbidity in WTC workers are high [3]. Likewise, studies showed that WTC rescue and recovery workers with PTSD and other mental health conditions had substantially increased odds of poor or very poorly controlled asthma, as well as acute healthcare utilization, compared to participants without mental health comorbidities [4,8]. However, almost all studies used self-reported measures of PTSD symptoms rather than tools based on structured clinical interviews [3,4,9,10]. Moreover, prior studies have not assessed the dimensional structure of PTSD (i.e., re-experiencing, avoidance/numbing, and arousal) [11-14] in regard to its potential association with asthma morbidity. PTSD symptom dimensions of re-experiencing (i.e., recurrent and intrusive distressing recollections or dreams about the traumatic event), avoidance (i.e., efforts to avoid thoughts, feelings, conversations, activities, places, or people that arouse recollections of the trauma), and hyper-arousal (i.e., irritability or outbursts of anger, difficulty concentrating, or hypervigilance) have been linked to a number of different illnesses and health-related behaviors. Re-experiencing and avoidance have been associated with adherence to hypertension medication [15], treatment and medical recommendations after heart transplantation [16], and highly active antiretroviral treatment [17].
Many WTC rescue and recovery workers who do not meet the criteria for PTSD may develop sub-threshold PTSD, also referred to as partial PTSD, a condition that can lead to distress and impairment in social, occupational, and other important areas of functioning [18]. Moreover, several studies have shown an association between sub-threshold PTSD and alcohol use [19], suicidal ideation [20], and increased healthcare use [21]. However, the potential impact of sub-threshold PTSD or PTSD symptom dimensions on asthma morbidity is unknown. Understanding how sub-threshold PTSD and specific PTSD symptom dimensions may affect asthma control has important clinical and policy implications for the management of WTC rescue and recovery workers, and may provide important knowledge for the development of targeted behavioral interventions for this vulnerable population.
In this study, we used data from a cohort of WTC rescue and recovery workers with asthma to assess whether meeting criteria for sub-threshold PTSD and for specific PTSD symptom dimensions are associated with worse asthma control, increased healthcare utilization, and poorer quality of life.
Methods
Study population
The study consisted of a cohort of WTC rescue and recovery workers with a physician diagnosis of asthma enrolled in the Mount Sinai Hospital or North Shore-Long Island Jewish Health System/Queens College World Trade Center Health Program (WTCHP). In order to be eligible for the WTCHP, WTC responders had to have worked or volunteered for ≥4 hours from September 11–14, 2001; ≥24 hours during September 2001; or ≥80 hours from September to December 2001. Members of the Office of the Chief Medical Examiner who processed human remains were also eligible as were workers from the Port Authority Trans-Hudson Corporation who were engaged in cleaning tunnels for ≥24 hours from September 11, 2001 to July 1, 2002 [22,23]. Details on recruitment into the WTCHP have been published elsewhere [1].
For the present study, rescue and recovery workers from the WTCHP were invited to participate according to the following eligibility criteria: >18 years of age, asthma diagnosis after September 11, 2001 made by a healthcare provider (or prior asthma that worsened after WTC exposure), and the ability to communicate in English or Spanish. Rescue and recovery workers were excluded if they had chronic obstructive lung disease (COPD) or other chronic respiratory illness. Additionally, individuals with a history of heavy smoking (15 lifetime pack-years or more) were excluded because of the possibility of undiagnosed COPD. Current smokers were included in the study if their cumulative smoking history did not exceed this threshold.
Potential participants were contacted by mail and invited to join the study. Those interested in participating completed a standardized in-person interview conducted by trained research coordinators either in English or Spanish based on the participant’s preference. The study was approved by the Institutional Review Boards of the Icahn School of Medicine at Mount Sinai and Queens College. Interviews were carried out at baseline, and at 6 and 12 months. For the purposes of this study, data are reported from the first interview for which a full SCID (Structured Clinical Interview for DSM-IV-TR) was available, and all the data reported were collected during the same session. Interviews were carried out between December 2013 and April 2015.
Study variables
Socio-demographic data included questions on age, sex, race and ethnicity, education, income, marital status, language, alcohol and tobacco use, and other comorbidities, using items adapted from the National Health Interview Survey [24].
Symptoms of PTSD were assessed using the Structured Clinical Interview for DSM Disorders (SCID) I/P (Patient Edition) for the Diagnostic and Statistical Manual, Version Four, Revised (DSM-IV-TR) [25]. The SCID is considered a gold standard for psychiatric interviews, and has great reliability (kappa = 0.80) for most disorders according to several validation studies [26,27]. From the SCID, we administered the sections “Overview”, “Screener questions”, and the modules for PTSD, major depressive disorder (MDD), and panic disorder (PD). Diagnosis of PTSD, MDD, and PD was based on the DSM-IV-TR criteria [28]. Sub-threshold PTSD was determined according to the recommendations made by McLaughlin et al. [29], extrapolated from the DSM-5, arising from the World Health Organization World Mental Health Surveys, which require meeting any two PTSD symptom clusters. While no consensus exists on the optimal classification of sub-threshold PTSD [29,30], the guidelines set forth by McLaughlin et al. [30], arising from the first cross-national comparison of all possible definitions of sub-threshold PTSD done through structured interviews, noted that the classification of sub-threshold PTSD as meeting any two symptom dimensions is associated with more adverse outcomes. The authors also noted that classifications that require the presence of a specific symptom dimension (criteria B) did not arise from the evidence of special importance of any specific symptom dimension over the others.
The history of asthma was ascertained both through review of participants’ electronic medical records and through participant self-report of physician diagnosis. In order to be eligible for the study, patients had to be certified for asthma by the WTCHP, as specified in their electronic medical records. Certification requires a physician diagnosis of asthma as a WTC-related health condition in order to cover treatment costs, as per program protocols. As part of their regular WTCHP monitoring exams, WTC rescue and recovery workers are asked to complete an interview-based standardized questionnaire during each visit. The questionnaire inquires about a physician diagnosis of asthma during the baseline interview: “Have you EVER been told by a doctor or other health professional that you had asthma or RADS (Reactive Airway Dysfunction Syndrome)?” They are also asked to provide the list of current medications. Case ascertainment for asthma includes review of answers to WTCHP monitoring questionnaires and electronic medical treatment records. In addition, evaluation for asthma includes but is not limited to reviewing provocability, symptoms, and spirometry or pulmonary function tests as per the NIH National Heart, Lung and Blood Institute (NHLBI) Guidelines for the Diagnosis and Management of Asthma. Finally, at the research baseline interview, participants were asked, “Have you EVER been told by a doctor or other health professional that you had asthma or RADS (Reactive Airway Dysfunction Syndrome)?.” Asthma history, including age of onset, family history, history of intubation, and asthma medication were obtained by self-report. We used the Asthma Control Questionnaire (ACQ) [31], a validated tool to assess the level of asthma control, which is recommended by the National Asthma Education and Prevention Program (NAEPP) [32]. The ACQ has a good reliability and internal consistency (α = 0.9), responsiveness, and construct validity [33]. The ACQ items are scored on a scale of 0–6 (0 representing good control and 6 representing very poor control); a difference of 0.5 units is considered clinically significant [34].
Acute asthma-related healthcare utilization were classified as outpatient (unscheduled physician visits) or inpatient exacerbations (emergency room visit or hospitalizations) due to worsening asthma in the prior 12 months. Both inpatient and outpatient asthma-related healthcare use was categorized into dichotomous variables of none versus one or more visits in the past 12 months. We also inquired as to comorbidities linked to worse asthma outcomes, by asking whether they had been diagnosed with gastro-esophageal reflux disease (GERD), chronic sinusitis, rhinitis, and allergies.
The 15-item Mini Asthma Quality of Life Questionnaire (Mini-AQLQ) was used to assess functional problems (physical, emotional, social, and occupational) that are most problematic for adults with asthma [31,35]. Items are rated on a Likert-type scale from 1 (all of the time; totally limited) to 7 (none of the time; not at all limited). Higher scores indicate better quality of life and a change in 0.5 units is considered clinically meaningful [36].
Statistical analysis
We conducted univariate tests to examine differences in the baseline characteristics of WTC rescue and recovery workers of three PTSD categories (full PTSD, sub-threshold, and no PTSD) using the chi-square test, Fisher’s exact test, and Kruskal–Wallis test. The unadjusted relationship of the three PTSD categories with asthma control (ACQ scores), healthcare utilization, and quality of life (AQLQ scores) was assessed using the Kruskal–Wallis or chi-square test; adjusted analyses for these relationships were conducted using multiple linear or logistic regressions. The unadjusted association between PTSD dimensions (re-experiencing, avoidance, and hyper-arousal), asthma morbidity, and healthcare utilization were assessed with Wilcoxon sum-rank test or chi-square test, with adjusted analyses conducted via multiple linear or logistic regressions. Further analyses were done to assess if meeting criteria for PTSD dimensions was associated with asthma morbidity measures in patients not meeting the criteria for full PTSD. Dunnett post hoc tests were carried out to evaluate significant differences in the full PTSD versus no PTSD, and full PTSD versus sub-threshold PTSD comparisons. All models were adjusted for age, sex, education, race/ethnicity, and the presence of depression. Models were built manually using a stepwise selection procedures based on the results of univariate analyses and prior knowledge regarding determinants of asthma morbidity. Analyses were performed with SAS 9.3 (SAS, Inc., Cary, NC, USA) statistical software, using two-sided p-values with a significance level of 0.05.
Results
The final sample for the purposes of this analysis was 181. Of the 1270 patients identified from the WTCHP as potential candidates, we were unable to reach 864 (68%), and 446 (35%) were ineligible (COPD (7%), smoking history ≥ 15 pack-years (3%), language (3%), or other reasons (19%)). 274 agreed to participate (22%). Among those who actively declined, 34% were Spanish-speaking, and 20% were female. Study participants had a mean age of 53.3 (sd = 8.4), 24% were female, and 21% spoke Spanish as their primary language. 15% were non-Hispanic black, 40% were non-Hispanic white, 38% were Hispanic, and 7% were categorized as “other.” Out of the 181 participants for whom a full SCID without skip rules was available, 51 (28%) and 46 (25%) patients were categorized as meeting the criteria for full PTSD and sub-threshold PTSD, respectively. With regard to specific PTSD symptom domains, 126 (70%) participants met the dimension criteria for re-experiencing, 76 (42%) for avoidance, and 94 (52%) for hyper-arousal. As shown in Table 1, patients diagnosed with full PTSD, in comparison to patients with sub-threshold or no PTSD, were more likely to have lower levels of education (p = 0.001) and lower incomes (p < 0.001), and speak Spanish (p < 0.0001), as well as less likely to be married (p = 0.05). Patients with full PTSD were also more likely to be depressed (p < 0.0001) and have GERD (p = 0.0005), as well as less likely to have allergies (p = 0.03). There were no significant associations between the three PTSD categories and the distribution of age, race, gender, or the presence of sinusitis or rhinitis (p > 0.05 for all comparisons).
Table 1.
Baseline characteristics of study participants according to post-traumatic stress disorder symptoms.
| Characteristics | All participants | PTSD | Sub-threshold PTSD | No PTSD | p-value |
|---|---|---|---|---|---|
| Total, No. (%) | 181 (100) | 51 (28) | 46 (25) | 84 (46) | |
| Age, years (mean, SD) | 53.3 (8.4) | 55.2 (8.8) | 51.4 (7.5) | 53.1 (8.4) | 0.15 |
| Female, No. (%) | 44 (24) | 15 (29) | 8 (18) | 21 (25) | 0.41 |
| Race, No. (%) | 0.38 | ||||
| Non-hispanic black | 26 (15) | 5 (11) | 7 (16) | 14 (17) | |
| Non-hispanic white | 68 (40) | 14 (31) | 17 (39) | 37 (45) | |
| Hispanic | 65 (38) | 23 (51) | 18 (41) | 24 (29) | |
| Other | 12 (7) | 3 (7) | 2 (4) | 7 (9) | |
| Monthly income, US $, No. (%) | <0.0001 | ||||
| $2000 or less | 41 (23) | 23 (46) | 8 (17) | 10 (12) | |
| $2001 to 2500 | 11 (6) | 4 (8) | 2 (4) | 5 (6) | |
| $2501 or more | 115 (64) | 17 (34) | 30 (65) | 68 (81) | |
| Do not know/Refused | 13 (7) | 6 (12) | 6 (13) | 1 (1) | |
| Education, No. (%) | 0.001 | ||||
| Less than high school | 15 (8) | 10 (20) | 4 (9) | 1 (1) | |
| High school or GED | 25 (14) | 11 (22) | 3 (7) | 11 (13) | |
| Some college | 73 (40) | 18 (35) | 19 (41) | 36 (43) | |
| College or higher degree | 68 (38) | 12 (23) | 20 (43) | 36 (43) | |
| Marital status, No. (%) | 0.05 | ||||
| Married/Living with a partner | 112 (62) | 26 (51) | 27 (59) | 59 (71) | |
| Single | 22 (12) | 5 (10) | 6 (13) | 11 (13) | |
| Other | 46 (26) | 20 (39) | 13 (28) | 13 (16) | |
| Primary language Spanish, No. (%) | 39 (21) | 22 (44) | 10 (23) | 7 (8) | <0.0001 |
| Smoking, pack-years (mean, SD) | 4.8 (7.9) | 5.9 (11.1) | 2.8 (4.2) | 5.2 (7.0) | 0.31 |
| Comorbidities, No. (%) | |||||
| GERD | 111 (62) | 43 (84) | 26 (57) | 42 (51) | 0.0005 |
| Allergies | 101 (57) | 23 (45) | 24 (52) | 54 (68) | 0.03 |
| Chronic sinusitis | 109 (62) | 33 (65) | 31 (70) | 45 (57) | 0.31 |
| Rhinitis | 112 (64) | 31 (65) | 32 (70) | 49 (61) | 0.64 |
| Depression | 29 (16) | 20 (39) | 6 (13) | 3 (3) | <0.0001 |
GED = General educational development; GERD = Gastro-esophageal reflux disease; PTSD = Post-traumatic stress disorder.
Participants had a mean (standard deviation [SD]) asthma control score of 1.5 (1.2) and a mean asthma quality of life score of 4.8 (1.2), suggesting relatively low levels of asthma control and moderate to low asthma quality of life. Overall, 28% had utilized outpatient healthcare, and 17% of patients had utilized inpatient healthcare, due to asthma in the last year. As seen in Table 2, unadjusted analyses among the entire cohort showed that worse asthma control scores were associated with symptoms of re-experiencing (1.7 vs. 1.0, p = 0.0002), avoidance (1.7 vs. 1.3, p = 0.003), and hyper-arousal (1.7 vs. 1.2, p = 0.003). A significant relationship was found between symptoms of re-experiencing and exacerbations requiring outpatient care (33% vs. 18%, p = 0.04), while symptoms of hyper-arousal and avoidance were not associated with exacerbations requiring outpatient care. Exacerbations requiring inpatient care were more frequent among patients with re-experiencing (21% vs. 7%, p = 0.03), avoidance (28% vs. 9%, p = 0.0007), and hyper-arousal (23% vs. 9%, p = 0.01) symptoms. Lower asthma quality of life scores were associated with all three PTSD dimensions: re-experiencing (4.6 vs. 5.4, p < 0.0001), avoidance (4.5 vs. 5.0, p = 0.002), and hyper-arousal (4.5 vs. 5.2, p = 0.0002). Table 2 also shows that among patients who were not diagnosed with PTSD, unadjusted analyses revealed that those with re-experiencing symptoms reported worse asthma control (1.5 vs. 1.0, p = 0.03) and poorer quality of life (4.8 vs. 5.4, p = 0.01). No other significant relationships between specific PTSD dimensions and either healthcare utilization or measures of asthma morbidity were found in unadjusted analyses for patients not diagnosed with PTSD (p > 0.05 for all comparisons).
Table 2.
Unadjusted relationship between specific post-traumatic stress disorder symptom clusters and asthma morbidity.
| All participants, n = 181 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Re-experiencing, n = 126 |
Avoidance, n = 76 |
Hyper-arousal, n = 94 |
|||||||
| Met | Unmet | p-value | Met | Unmet | p-value | Met | Unmet | p-value | |
| Asthma control (ACQ score, SD) | 1.7 (1.2) | 1.0 (0.9) | 0.0002 | 1.7 (1.1) | 1.3 (1.1) | 0.003 | 1.7 (1.1) | 1.2 (1.1) | 0.0033 |
| Quality of life (AQLQ score, SD) | 4.6 (1.2) | 5.4 (1.0) | <0.0001 | 4.5 (1.1) | 5.0 (1.2) | 0.002 | 4.5 (1.2) | 5.2 (1.1) | 0.0002 |
| One or more outpatient visits during last year due to asthma (No, %) | 41 (33) | 10 (18) | 0.04 | 25 (33) | 26 (25) | 0.20 | 31 (33) | 20 (23) | 0.10 |
| One or more inpatient visits during last year due to asthma (No, %) | 26 (21) | 4 (7) | 0.03 | 21 (28) | 9 (9) | 0.0007 | 22 (23) | 8 (9) | 0.01 |
| Participants not diagnosed with PTSD, n = 130 |
|||||||||
| Re-experiencing, n = 75 |
Avoidance, n = 25 |
Hyper-arousal, n = 43 |
|||||||
| Met | Unmet | p-value | Met | Unmet | p-value | Met | Unmet | p-value | |
| Asthma control (ACQ score, SD) | 1.5 (1.2) | 1.0 (0.9) | 0.03 | 1.3 (1.1) | 1.3 (1.1) | 0.94 | 1.4 (1.2) | 1.2 (1.1) | 0.58 |
| Quality of life (AQLQ score, SD) | 4.8 (1.2) | 5.4 (1.0) | 0.01 | 5.0 (1.2) | 5.0 (1.2) | 0.86 | 4.8 (1.3) | 5.2 (1.1) | 0.13 |
| One or more outpatient visits during last year due to asthma (No, %) | 23 (31) | 10 (18) | 0.11 | 7 (28) | 26 (25) | 0.74 | 13 (30) | 20 (23) | 0.37 |
| One or more inpatient visits during last year due to asthma (No, %) | 9 (12) | 4 (7) | 0.56 | 4 (16) | 9 (9) | 0.27 | 5 (12) | 8 (9) | 0.76 |
ACQ = asthma control questionnaire; AQLQ = asthma quality of life questionnaire.
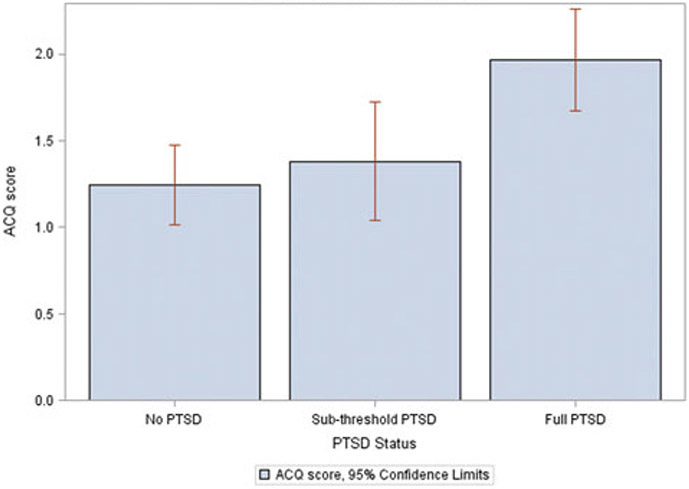
As seen in Table 3, unadjusted analyses showed worse asthma control among patients with full PTSD compared to those with sub-threshold or no PTSD (ACQ scores of 2.0 vs. 1.4 and 1.2, respectively, p < 0.0003). Dunnett post hoc tests revealed significant differences in the full PTSD versus no PTSD (p < 0.05), and full PTSD versus sub-threshold PTSD comparisons (p < 0.05). Patients with full PTSD had higher rates of exacerbations requiring inpatient care than those with sub-threshold or no PTSD (33% vs. 9% and 10%, respectively, p = 0.0007). Similarly (suggestive of worse asthma quality of life), patients with full PTSD were also found to have lower asthma quality of life scores than their peers (4.2 vs. 4.8 and 5.1, p < 0.0001), with Dunnett post-hoc tests finding significant differences in the full PTSD versus both the no PTSD (p < 0.05) and sub-threshold PTSD (p < 0.05) conditions. No other significant relationships were found between PTSD categories and both healthcare utilization and measures of asthma morbidity (p > 0.05 for all comparisons).
Table 3.
Participants meeting the criteria for full or sub-threshold post-traumatic stress disorder and relation to respiratory outcomes—univariate and adjusted analysis.
| Unadjusted analysis | ||||
|---|---|---|---|---|
| Full PTSD, n = 51 | Sub-threshold PTSD, n = 46 | No PTSD, n = 84 | p-value | |
| Asthma control (ACQ score, sd) | 2.0 (1.0) | 1.4 (1.2) | 1.2 (1.1) | 0.0003 |
| Quality of life (AQLQ score, sd) | 4.2 (1.0) | 4.8 (1.1) | 5.1 (1.1) | <0.0001 |
| One or more outpatient visits during last year due to asthma (No, %) | 18 (35) | 15 (33) | 18 (21) | 0.20 |
| One or more inpatient visits during last year due to asthma (No, %) | 17 (33) | 5 (9) | 8 (10) | 0.0007 |
| Adjusted analysis | ||||
| Full PTSD, n = 51 | Sub-threshold PTSD, n = 46 | No PTSD, n = 84 | p-value | |
| Asthma control, mean difference (95% CI) | 0.57 (0.12, 1.02) | 0.06 (−0.35, 0.47) | Reference | 0.04 |
| Quality of life, mean difference (95% CI) | −0.83 (−1.32, −0.34) | −0.38 (−0.83, 0.07) | Reference | 0.002 |
| One or more outpatient visits during last year due to asthma, OR (95% CI) | 2.32 (0.90, 6.00) | 1.85 (0.77, 4.43) | Reference | 0.17 |
| One or more inpatient visits during last year due to asthma, OR (95% CI) | 11.86 (3.51, 40.09) | 1.70 (0.47, 6.08) | Reference | 0.0002 |
Adjusted for age, sex, education, race/ethnicity, and depression; CI = 95% Confidence interval; OR = Odds ratio.
Adjusted analyses, also depicted in Table 3, showed worse asthma control scores among patients with full PTSD compared to those without PTSD (mean difference: 0.57; 95% CI: [0.12, 1.02]; p = 0.01), while no significant difference was observed between patients with sub-threshold PTSD and no PTSD. Patients with full PTSD also showed worse asthma control scores than those with sub-threshold PTSD (mean difference: 0.51; 95% CI: [0.02, 1.00]; p = 0.04), as shown in Figure 1. With regard to outpatient healthcare utilization, no significant association was found. Higher odds of inpatient healthcare utilization were found in patients with full PTSD compared to those without PTSD (OR = 11.86, 95% CI: [3.51, 40.09], p < 0.0001), while a significant difference was also observed between patients with full PTSD and sub-threshold PTSD (OR = 6.99, 95% CI: [1.89, 25.86], p = 0.004). No difference was found with regard to the odds of inpatient visits between the sub-threshold PTSD and no PTSD groups. Worse asthma quality of life scores were also found among patients with full PTSD compared to those without PTSD (mean difference: −0.83; 95%: [−1.32, −0.34]; p = 0.002), whereas no differences were found between patients with sub-threshold PTSD and both their peers without PTSD and their peers with full PTSD.
Figure 1.
Asthma Control by PTSD status.
As seen in Table 4, adjusted analyses found that among the entire cohort, patients meeting the criteria for re-experiencing had worse asthma control (mean difference = 0.52; 95% CI: [0.15, 0.89]; p = 0.007), greater likelihood of outpatient healthcare utilization (OR = 2.33; 95% CI: [0.98, 5.51]; p = 0.05), greater likelihood of inpatient healthcare utilization (OR = 5.53; 95% CI: [1.45, 21.10]; p = 0.01), and worse quality of life (mean difference = −0.79; 95% CI: [−1.18, −0.40]; p = 0.0002). Patients meeting the criteria for avoidance had a greater likelihood of inpatient healthcare utilization (OR = 7.09; 95% CI: [2.55, 19.70]; p = 0.0002). Patients meeting the criteria for hyper-arousal also had a greater likelihood of inpatient healthcare utilization (OR: 4.38; 95% CI: [1.60, 12.03]; p = 0.004), in addition to worse quality of life (mean difference = −0.61; 95% CI: [−1.00, −0.22]; p = 0.002). No other significant relationships between specific PTSD symptom dimensions and both healthcare utilization and asthma morbidity measures were found in adjusted analysis (p > 0.05 for all comparisons).
Table 4.
Participants meeting the criteria for specific post-traumatic stress disorder symptom clusters and relation to respiratory outcomes—adjusted analysis.
| All participants, n = 181 | ||||||
|---|---|---|---|---|---|---|
| Re-experiencing | p-value | Avoidance | p-value | Hyper-arousal | p-value | |
| Asthma control, mean difference, (95% CI) | 0.52 (0.15, 0.89) | 0.007 | 0.23 (−0.14, 0.60) | 0.23 | 0.25 (−0.10, 0.60) | 0.17 |
| Quality of life, mean difference, (95% CI) | −0.79 (−1.18, −0.40) | 0.0002 | −0.39 (−0.80, 0.02) | 0.07 | −0.61 (−1.00, −0.22) | 0.002 |
| One or more outpatient visits during last year due to asthma, OR (95% CI) | 2.33 (0.98, 5.51) | 0.05 | 1.48 (0.68, 3.20) | 0.32 | 1.83 (0.87, 3.86) | 0.11 |
| One or more inpatient visits during last year due to asthma, OR (95% CI) | 5.53 (1.45, 21.10) | 0.01 | 7.09 (2.55, 19.70) | 0.0002 | 4.38 (1.60, 12.03) | 0.004 |
| Participants not diagnosed with PTSD, n = 130 | ||||||
| Re-experiencing | p-value | Avoidance | p-value | Hyper-arousal | p-value | |
| Asthma control, mean difference, (95% CI) | 0.40 (−0.01, 0.81) | 0.06 | −0.25 (−0.78, 0.28) | 0.35 | −0.07 (−0.50, 0.36) | 0.76 |
| Quality of life, mean difference, (95% CI) | −0.69 (−1.12, −0.26) | 0.003 | 0.20 (−0.37, 0.77) | 0.49 | −0.21 (−0.70, 0.28) | 0.40 |
| One or more outpatient visits during last year due to asthma, OR (95% CI) | 2.10 (0.82, 5.41) | 0.15 | 1.07 (0.35, 3.28) | 0.90 | 1.70 (0.70, 4.12) | 0.30 |
| One or more inpatient visits during last year due to asthma, OR (95% CI) | 4.68 (0.93, 23.73) | 0.10 | 4.73 (1.00, 22.43) | 0.05 | 1.64 (0.44, 6.18) | 0.62 |
Adjusted for age, sex, education, race/ethnicity, and depression; CI = 95% Confidence interval; OR = Odds ratio.
We conducted additional adjusted analyses to assess the relationship between PTSD dimensions (re-experiencing, avoidance, and hyper-arousal) and measures of asthma morbidity and healthcare utilization among patients who were not diagnosed with full PTSD, which are also shown in Table 4. Re-experiencing was associated with worse asthma quality of life (mean difference = −0.69; 95% CI: [−1.12, −0.26]; p = 0.003). Avoidance was associated with higher odds of inpatient healthcare utilization (OR = 4.73; 95% CI: [1.00, 22.43]; p = 0.05). No other significant relationships between specific PTSD symptom dimensions and both healthcare utilization and asthma morbidity measures were identified (p > 0.05 for all comparisons).
Discussion
PTSD and asthma are common sources of morbidity among WTC rescue and recovery workers. In this study, we found a strong association between PTSD (though not sub-threshold PTSD) and worse asthma control, increased healthcare utilization, and poorer quality of life. However, specific PTSD symptom domains were associated with some measures of asthma morbidity among patients without full PTSD. These findings highlight the importance of addressing comorbid PTSD in WTC rescue and recovery workers with asthma. Moreover, it suggests that PTSD symptoms may be associated with worse asthma morbidity among patients without full PTSD.
Our results extend prior reports linking PTSD symptoms with worse asthma control, increased hospitalizations, and poor asthma quality of life among WTC rescue and recovery workers [4,8]. We also found that having PTSD was associated with lower income, lower level of education, being a Spanish speaker, and not being married. Previous studies had documented a strong association between asthma and PTSD symptoms [3,6], mental health comorbidities and poor asthma control [4], and PTSD as a predictor of asthma symptom severity and use of urgent healthcare services [8]. Nevertheless, it is important to note that in our study, participants were assessed by trained psychological interviewers with a background in clinical psychology, using the SCID. Previous studies relied on self-report measures [3,4,9,10], which have the potential of overestimating PTSD symptoms [37].
This is the first study examining the role of sub-threshold PTSD and specific PTSD dimensions in predicting asthma outcomes in WTC rescue and recovery workers. While in previous studies sub-threshold PTSD has been associated with comorbidity (i.e., depression, alcohol use, health problems, suicidal ideation, or overall greater impairment) [18,20], which could in turn affect asthma management, our findings indicate that having sub-threshold PTSD was not associated with worse asthma outcomes. The present study also provides new information regarding the relationship between PTSD dimensions (re-experiencing, avoidance, and hyper-arousal) and asthma outcomes, and our results confirmed a unique contribution of each dimension into different aspects of asthma management such as asthma control, asthma quality of life, outpatient visits, and inpatient hospitalizations, even among patients without PTSD.
Biological and psychosocial pathways can explain the associations between PTSD and worse asthma morbidity. Biological pathways include abnormalities of the hypothalamic-pituitary-adrenal (HPA) axis reported among patients with PTSD, which alters the sensitivity of the glucocorticoid receptor and can interfere in the regulation of the sympathetic nervous system [38-41]. This can lead to increased levels of pro-inflammatory cytokines, which in turn causes inflammation and thus worsening of asthma [39,41]. However, behavioral pathways have also been implicated, suggesting that mental health conditions can worsen asthma via greater use of quick relief medication and lack of adherence to other self-management behaviors [8,42,43].
Our study has strengths and limitations. We used a validated tool to identify patients with full and sub-threshold PTSD. However, while the DSM-5 contains new criteria for PTSD based on 4 dimensions instead of the 3-dimension structure outlined in the DSM-IV, it was not possible to assess the DSM-5 categories because an updated version of the SCID was not yet available at the time of the interviews. Likewise, while research has shown potential advantages of considering 4 or 5 symptom dimensions of PTSD [11,12], it was not possible to evaluate these models since no guidelines are available to assess whether a patient has met the criteria or not for these dimensions. The information on inpatient and outpatient episodes was based on self-reported measures, instead of medical records. Nonetheless, we used validated items, and self-report allowed us to capture healthcare use at other facilities. Finally, because the data used in this study is cross-sectional, it is not possible to establish causal relationships between PTSD or PTSD symptoms and asthma morbidity.
These findings have important implications for the management of WTC rescue and recovery workers with asthma. First, it highlights the importance of screening for and addressing symptoms of PTSD in this high-risk population. Second, it suggests that attention to symptoms of re-experiencing and avoidance among patients who do not meet the criteria for full PTSD may be important, particularly among patients with poor asthma control. Additional research is needed to further understand the potential biological and behavioral mechanisms underlying the association between PTSD and worse asthma control, in order to develop interventions to improve the outcomes of these patients.
Funding
This study was funded by the National Institute for Occupational Safety and Health (U01OH010405).
Footnotes
Declaration of interest
Dr. Wisnivesky is a member of the research board of EHE International, and has received consulting honorarium from Quintiles, BMS, and Merck, and research grants from Aventis and Quorum. All other authors have nothing to report.
References
- 1.Wisnivesky JP, Teitelbaum SL, Todd AC, Boffetta P, Crane M, Crowley L, et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: a cohort study. Lancet. 2011;378(9794):888–897. Epub 2011/09/06. doi: 10.1016/s0140-6736(11)61180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bills CB, Levy NA, Sharma V, Charney DS, Herbert R, Moline J, et al. Mental health of workers and volunteers responding to events of 9/11: review of the literature. Mt Sinai J Med. 2008;75(2):115–127. Epub 2008/05/27. doi: 10.1002/msj.20026. [DOI] [PubMed] [Google Scholar]
- 3.Brackbill RM, Hadler JL, DiGrande L, Ekenga CC, Farfel MR, Friedman S, et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA. 2009;302(5):502–516. Epub 2009/08/06. doi: 10.1001/jama.2009.1121. [DOI] [PubMed] [Google Scholar]
- 4.Jordan HT, Stellman SD, Reibman J, Farfel MR, Brackbill RM, Friedman SM, et al. Factors associated with poor control of 9/11-related asthma 10–11 years after the 2001 World Trade Center terrorist attacks. J Asthma. 2015;52(6):630–637. Epub 2014/12/30. doi: 10.3109/02770903.2014.999083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGrady A, Moss D. Psychophysiological Etiology of Illness. Pathways to Illness, Pathways to Health. New York: Springer; 2013. p. 47–62. [Google Scholar]
- 6.Goodwin RD, Fischer ME, Goldberg J. A twin study of post-traumatic stress disorder symptoms and asthma. Am J Respir Critic Care Med. 2007;176(10):983–987. Epub 2007/08/19. doi: 10.1164/rccm.200610-1467OC. [DOI] [PubMed] [Google Scholar]
- 7.de la Hoz RE, Jeon Y, Miller GE, Wisnivesky JP, Celedón JC. Post-traumatic stress disorder, bronchodilator response, and incident asthma in World Trade Center rescue and recovery workers. Am J Respir Crit Care Med 2016;194:1383–1391. Epub 2016/08/23. doi: 10.1164/rccm.201605-1067OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fagan J, Galea S, Ahern J, Bonner S, Vlahov D. Relationship of self-reported asthma severity and urgent health care utilization to psychological sequelae of the September 11, 2001 terrorist attacks on the World Trade Center among New York City area residents. Psychosom Med. 2003;65(6):993–996. Epub 2003/12/04. [DOI] [PubMed] [Google Scholar]
- 9.Liu B, Tarigan LH, Bromet EJ, Kim H. World Trade Center disaster exposure-related probable posttraumatic stress disorder among responders and civilians: a meta-analysis. PLoS One. 2014;9(7):e101491. Epub 2014/07/23. doi: 10.1371/journal.pone.0101491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Niles JK, Webber MP, Gustave J, Cohen HW, Zeig-Owens R, Kelly KJ, et al. Comorbid trends in World Trade Center cough syndrome and probable posttraumatic stress disorder in firefighters. Chest. 2011;140(5):1146–1154. Epub 2011/05/07. doi: 10.1378/chest.10-2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pietrzak RH, Feder A, Schechter CB, Singh R, Cancelmo L, Bromet EJ, et al. Dimensional structure and course of post-traumatic stress symptomatology in World Trade Center responders. Psychol Med. 2013:1–14. doi: 10.1017/S0033291713002924. [DOI] [PubMed] [Google Scholar]
- 12.Ruggero CJ, Kotov R, Callahan JL, Kilmer JN, Luft BJ, Bromet EJ. PTSD symptom dimensions and their relationship to functioning in World Trade Center responders. Psychiatry Res. 2013;210(3):1049–1055. Epub 2013/09/26. doi: 10.1016/j.psychres.2013.08.052. [DOI] [PubMed] [Google Scholar]
- 13.Stellman JM, Smith RP, Katz CL, Sharma V, Charney DS, Herbert R, et al. Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. Environ Health Perspect. 2008;116(9):1248–1253. Epub 2008/09/17. doi: 10.1289/ehp.11164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palmieri PA, Weathers FW, Difede J, King DW. Confirmatory factor analysis of the PTSD checklist and the clinician-administered PTSD scale in disaster workers exposed to the world trade center ground zero. J Abnorm Psychol. 2007;116(2):329–341. Epub 2007/05/23. doi: 10.1037/0021-843x.116.2.329. [DOI] [PubMed] [Google Scholar]
- 15.Shemesh E, Rudnick A, Kaluski E, Milovanov O, Salah A, Alon D, et al. A prospective study of posttraumatic stress symptoms and nonadherence in survivors of a myocardial infarction (MI). Gen Hosp Psychiatry 2001;23(4):215–222. Epub 2001/09/07. [DOI] [PubMed] [Google Scholar]
- 16.Favaro A, Gerosa G, Caforio AL, Volpe B, Rupolo G, Zarneri D, et al. Posttraumatic stress disorder and depression in heart transplantation recipients: the relationship with outcome and adherence to medical treatment. Gen Hosp psychiatry. 2011;33(1):1–7. Epub 2011/03/01. doi: 10.1016/j.genhosppsych.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Delahanty DL, Bogart LM, Figler JL. Posttraumatic stress disorder symptoms, salivary cortisol, medication adherence, and CD4 levels in HIV-positive individuals. AIDS care. 2004;16(2):247–260. Epub 2003/12/17. doi: 10.1080/09540120410001641084. [DOI] [PubMed] [Google Scholar]
- 18.Yarvis JS, Schiess L. Subthreshold posttraumatic stress disorder (PTSD) as a predictor of depression, alcohol use, and health problems in veterans. J Workplace Behav Health. 2008;23(4):395–424. doi: 10.1080/15555240802547801. [DOI] [Google Scholar]
- 19.Boscarino JA, Galea S, Adams RE, Ahern J, Resnick H, Vlahov D. Mental health service and medication use in New York City after the September 11, 2001, terrorist attack. Psychiatr Serv. 2004;55(3):274–283. Epub 2004/03/06. [DOI] [PubMed] [Google Scholar]
- 20.Marshall RD, Olfson M, Hellman F, Blanco C, Guardino M, Struening EL. Comorbidity, impairment, and suicidality in subthreshold PTSD. Am J Psychiatry. 2001;158(9):1467–1473. Epub 2001/09/05. [DOI] [PubMed] [Google Scholar]
- 21.Deykin EY, Keane TM, Kaloupek D, Fincke G, Rothendler J, Siegfried M, et al. Posttraumatic stress disorder and the use of health services. Psychosom Med. 2001;63(5):835–841. Epub 2001/09/27. [DOI] [PubMed] [Google Scholar]
- 22.Moline JM, Herbert R, Levin S, Stein D, Luft BJ, Udasin IG, et al. WTC medical monitoring and treatment program: comprehensive health care response in aftermath of disaster. Mt Sinai J Med. 2008;75(2):67–75. Epub 2008/05/27. doi: 10.1002/msj.20022. [DOI] [PubMed] [Google Scholar]
- 23.Herbert R, Moline J, Skloot G, Metzger K, Baron S, Luft B, et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect. 2006;114(12):1853–1858. Epub 2006/12/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. Vital Health Stat 10. 2010;(249):1–207. Epub 2011/09/13. [PubMed] [Google Scholar]
- 25.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 26.Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the structured clinical interview for DSM-IV axis I disorders (SCID I) and axis II disorders (SCID II). Clin Psychol Psychother. 2011;18(1):75–79. Epub 2010/03/24. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- 27.Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, et al. The collaborative longitudinal personality disorders study: Reliability of axis I and II diagnoses. J Pers Disord. 2000;14(4):291–299. Epub 2001/02/24. [DOI] [PubMed] [Google Scholar]
- 28.APA APA. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. ed. Washington, DC: 2000. [Google Scholar]
- 29.McLaughlin KA, Koenen KC, Friedman MJ, Ruscio AM, Karam EG, Shahly V, et al. Subthreshold posttraumatic stress disorder in the world health organization world mental health surveys. Biol Psychiatry. 2015;77(4):375–384. Epub 2014/05/21. doi: 10.1016/j.biopsych.2014.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schnurr PP. A guide to the literature on partial PTSD. PTSD research quarterly. 2014;25(1):1–8. [Google Scholar]
- 31.Juniper EF, O’Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14(4):902–907. Epub 1999/11/26. [DOI] [PubMed] [Google Scholar]
- 32.NHLBI. NHLBI NAEPP Expert Pa NHLBI NAEPP Expert Panel Report 3: Guidelines for the Diagnosis nel Report 3: Guidelines for the Diagnosis and Management of Asthma (EPR-3). 2007. [DOI] [PubMed]
- 33.Juniper EF, Guyatt GH, Cox FM, Ferrie PJ, King DR. Development and validation of the mini asthma quality of life questionnaire. Eur Respir J. 1999;14(1):32–38. [DOI] [PubMed] [Google Scholar]
- 34.Juniper EF, Svensson K, Mörk A-C, Ståhl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med. 2005;99(5):553–558. doi: 10.1016/j.rmed.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 35.Williams LK, Joseph CL, Peterson EL, Wells K, Wang M, Chowdhry VK, et al. Patients with asthma who do not fill their inhaled corticosteroids: a study of primary nonadherence. J Allergy Clin Immunol. 2007;120(5):1153–1159. Epub 2007/10/16. doi: 10.1016/j.jaci.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 36.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol. 1994;47(1):81–87. [DOI] [PubMed] [Google Scholar]
- 37.Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust NZ J Psychiatry 2010;44(1):4–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McFarlane AC, Atchison M, Yehuda R. The acute stress response following motor vehicle accidents and its relation to PTSD. Ann N Y Acad Sci. 1997;821:437–441. Epub 1997/06/21. [DOI] [PubMed] [Google Scholar]
- 39.Cavalcanti-Ribeiro P, Andrade-Nascimento M, Morais-de-Jesus M, de Medeiros GM, Daltro-Oliveira R, Conceicao JO, et al. Post-traumatic stress disorder as a comorbidity: impact on disease outcomes. Expert Rev Neurother. 2012;12(8):1023–1037. Epub 2012/09/26. doi: 10.1586/ern.12.77. [DOI] [PubMed] [Google Scholar]
- 40.Zohar J, Juven-Wetzler A, Sonnino R, Cwikel-Hamzany S, Balaban E, Cohen H. New insights into secondary prevention in post-traumatic stress disorder. Dialog Clin Neurosci. 2011;13(3):301–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.von Kanel R, Hepp U, Kraemer B, Traber R, Keel M, Mica L, et al. Evidence for low-grade systemic proinflammatory activity in patients with posttraumatic stress disorder. J Psychiatric Res. 2007;41(9):744–752. doi: 10.1016/j.jpsychires.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 42.Cluley S, Cochrane GM. Psychological disorder in asthma is associated with poor control and poor adherence to inhaled steroids. Respir Med. 2001;95(1):37–39. Epub 2001/02/24. doi: 10.1053/rmed.2000.0968. [DOI] [PubMed] [Google Scholar]
- 43.Feldman JM, Siddique MI, Morales E, Kaminski B, Lu SE, Lehrer PM. Psychiatric disorders and asthma outcomes among high-risk inner-city patients. Psychosom Med. 2005;67(6):989–996. Epub 2005/11/30. doi: 67/6/989 [pii] 10.1097/01.psy.0000188556.97979.13 [doi]. [DOI] [PubMed] [Google Scholar]