Abstract
AIM
To examine the prevalence and composition of refractive errors in Hungary.
METHODS
Nationwide cross-sectional data collected between 2014 and 2019 were analysed from the Comprehensive Health Screening Program of Hungary, which provided spectacle dioptric power and autorefractometry data for 68 227 people (35 850 women and 32 377 men). Their age distribution, 18-99y, was similar to the national demographic distributions.
RESULTS
Of the total population, 16.50% of the refractive errors exhibited hyperopia, 40.05% emmetropia, and 43.45% myopia. Myopia was 3 times more frequent (58.7%) in younger ages (18-35y of age) compared to older age groups (19.4% of those 56-70y of age; P<0.001). High myopia showed a low prevalence (0.21%), and an increase parallel with ageing (r=0.716; P=0.009).
CONCLUSION
Myopia is the most frequent refractive error in Hungary. The prevalence of myopia is especially increased, up to 2-3 times, in the younger age groups. Nationwide actions need to be taken to reduce the onset of myopia and its associated consequences.
Keywords: refractive errors, myopia, hyperopia, emmetropia, Hungary
INTRODUCTION
Refractive errors are a significant cause of vision impairments worldwide, due to its associated ocular diseases and incorrect or absent corrections[1]–[4]. Myopia is one of the leading refractive errors worldwide, particularly in Chinese populations, but also among white populations as well[2],[4]–[5]. In a review of 145 studies, Holden et al[2] estimated that globally, there are 1406 million people with myopia (22.9% of the worldwide population) and 163 million people with high myopia (2.7% of the world population), and predicted a 3.4-fold increase in myopia and a 5.8-fold increase in high myopia by 2050. These estimates show the importance of developing and introducing preventive measures and the precise clinical management of myopia[2],[4]–[5].
In Europe, data is available regarding the prevalence of refractive errors in different countries (e.g., France, Denmark, the Netherlands, Norway, Northern Ireland, and the United Kingdom)[6]–[12]; however, only a few studies show the novel increase of the prevalence of myopia in younger age groups[2],[8],[12]–[14]. The estimated prevalence of myopia [-0.5 dioptres (D) or less] throughout Central Europe was 34.6% in 2020, and is expected to increase to 54.1% by 2050[2].
In Hungary, very few studies were published on the prevalence of refractive errors. In 1934, based on the examination of 8860 schoolchildren (aged between 4 and 18y) in Budapest, emmetropia was found in 24.8% and 20.1%, hyperopia in 50.0% and 50.5%, and myopia in 7.0% and 6.5%, of boys and girls, respectively[15]. The prevalence of myopia increased parallel with age: it was 2.0% among 6-10 years old and 2.5% among 10-14 years old. Above these ages, it increased to a larger extent: in 15 year-old it was 6.0%, in 16-year-old 7.9%, in 17-year-old 12.0%, and in 18-year-old 10.6%. The authors stated in the discussion that the prevalence of myopia in Budapest was far lower than the reported data from other large towns in Germany or Austria[15]. In 1960, among 48 020 persons evaluated at a regional eye examination centre in Budapest, 22.10% had hyperopia or presbyopia, and 4.73% had myopia. The data were skewed toward younger age groups, due to the age composition of the sample (0-20y: 37.53%, 21-40y: 19.97%, 41-60y: 28.92%, and 61+ years: 13.58%)[16].
In the present manuscript, we present data on the prevalence of refractive errors in different age groups among the population of Hungary, and on the increase of myopia in younger age groups. The data has been retrieved from the database of the nationwide general health screening campaign[17].
SUBJECTS AND METHODS
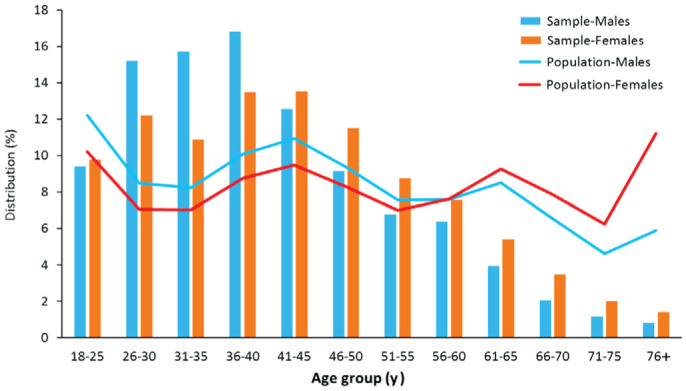
The nationwide Comprehensive Health Screening Program of Hungary, 2010-2020, included eye examinations and provided autorefractometry data for 68 227 people aged 18 and older, who participated in the nationwide screening program between 2014 and 2019[17]. The inclusion of participants was voluntary. Among the participants, there were 35 850 women (52.5%) and 32 377 men (47.5%). To analyse the distribution of refractive errors throughout the different age groups, the entire population was subdivided into 12 age groups (18-25, 26-30, 31-35, 36-40, 41-45, 46-50, 51-55, 56-60, 61-65, 66-70, 71-75, and 76+ years). The distribution of the population in each age group is shown in Figure 1. The distribution of age and sex in the sample population was similar to the national demographic distributions of 18 to 99 years old, but the 26-45 years old age group in both sexes was somewhat overrepresented in the sample, while the 61 and older age group was underrepresented[18].
Figure 1. Distribution of the number of men and women in the different age groups of the sample (bars) and Hungarian (lines) populations.
Refraction measurements were performed without pupillary dilatation, using a PRK-6000 Auto Ref-Keratometer (Potec, Daejeon, Korea), which was calibrated every 4mo. The refractometer performed 3 automated measurements on each eye, and calculated an unweighted arithmetic mean for each parameter. The instrument indexed the measurement accuracy, being set to indicate an error for a scatter greater than 0.25 D and to request a repeat measurement. The mean spherical and cylindrical refraction of both eyes were entered into an electronic data table, based on which spherical equivalents (SE) were calculated (SE=spherical refraction+0.5×cylindrical refraction). Refractive errors were classified into 3 types: hyperopia (SE≥+0.5 D), low myopia (SE≤-0.5 D but >-6.0 D), and high myopia (SE≤-6.0 D). Emmetropia was defined as SE<+0.5 D but >-0.5 D. Visual acuity was not measured during the collection of this data.
The results were presented as the relative prevalence of the various refractive errors, and the statistical difference in the prevalence of myopia by age group was calculated using the Chi-square test, while the increased prevalence of high myopia with increasing age was calculated using the Pearson correlation test.
The National Public Health and Medical Officer Service approved (operating license number: ÁNTSZ 2380-5/2010) the Comprehensive Health Screening Program of Hungary, 2010-2020. The data collected did not include any personal identification information, and the participants volunteered to participate in the screening examinations with implied consent.
RESULTS
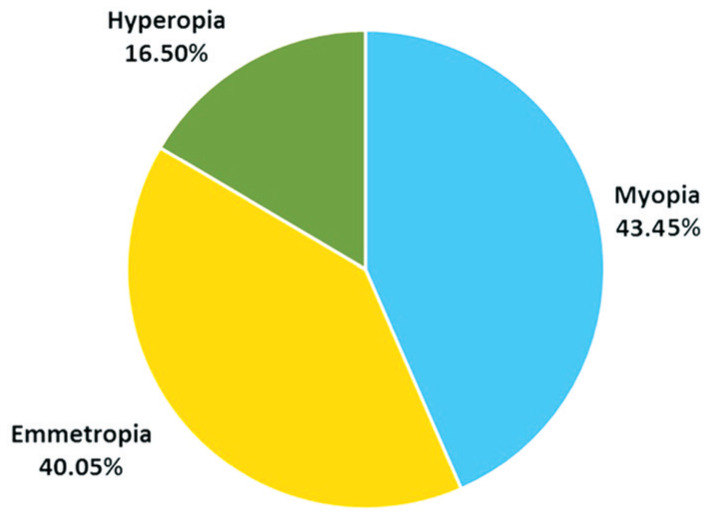
Analysing the results of the refractive measurements obtained from the Comprehensive Health Screening Program of Hungary, 2010-2020, refractive errors were found in the right eye of 60.0% of all participants (62.1% in women and 57.5% in men). Data on the left eyes showed similar results. The distribution of refractive errors, calculated using the spherical equivalents of the right eye of all participants, is shown in Figure 2. The relative distribution of SE refractive errors was as follows: hyperopia, 16.50%; emmetropia, 40.05%; low myopia, 43.24%; and high myopia, 0.21%. The proportion of myopia was the same in women and men (low myopia, 43.1% and 43.4%, and high myopia, 0.2% and 0.2%, respectively). However, hyperopia was more frequent among women than men (18.8% vs 14.0%, respectively), while emmetropia was less frequent among women than men (37.9% vs 42.5%, respectively).
Figure 2. Distribution of spherical equivalents of refractive errors in the right eyes of the total sample.
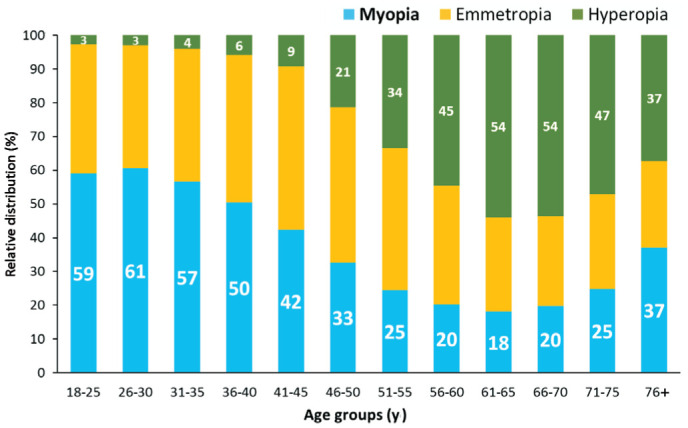
Data regarding the distribution of the refractive errors of individuals in various age groups show that myopia is 3 times more frequent in younger age groups (between 18 and 35y of age, relative prevalence of 58.7%) than in the older ones (56-70y, 19.4%; Chi-square=4364.646, P<0.001), and that hyperopia is more frequent in the older age groups (49.4%) than in the younger ones (3.3%; Chi-square =10 903.98, P<0.001), as seen in Figure 3. The relative prevalence of myopia increased over the age of 71y, while hyperopia decreased. High myopia was least prevalent (0.1%) in the 18-25 year-old group, which increased to 0.3% in the age groups between 46 and 65y, and then again up to 1.0% in those 75y and older (Pearson correlation, r=0.716; P=0.009).
Figure 3. Distribution of refractive errors in various age groups.
DISCUSSION
The results of our survey showed that a high number of individuals in Hungary have refractive errors (60%), of which myopia was the most frequent refractive error in both sexes, affecting 43% of the adult Hungarian population. Myopia was found to be 2.6 times more frequent than hyperopia.
The European Eye Epidemiology Consortium found in their meta-analysis that the most frequent refractive error between 1990 and 2003 in the European population, aged 25-90y, was low myopia (30.6%), closely followed by hyperopia (25.2%), and then high myopia (2.7%)[12]. Our results showed a higher prevalence of low myopia, but a lower prevalence of high myopia and hyperopia. The disparity concerning low myopia might be due to the different definitions of refractive errors (non-cycloplegic SE defined as ≤-0.75 D vs ≤-0.5 D); however, it might be also due to the increase of myopia and associated decrease of hyperopia in the younger age groups, taking into account the approximately 15-year difference in the data sampling between their analysis and ours. The UK Biobank Study[19] exhibited a lower prevalence of myopia (26.6%) based on their resource database of people aged 40-69y, which is, however, similar to the prevalence of myopia found in our study in similar age groups.
Another important finding from the present review was that the prevalence of myopia was 3 times higher (57%-61%) in younger age groups (18-35y of age) than in older ones (18%-20%, 56-70y of age). There may be at least two reasons for this drastic difference: 1) the increasing prevalence of myopia in younger age groups, and 2) the hyperopic shift associated with aging. Our cross-sectional study was not able to estimate the contribution rate of these two factors, although both may be significant. The trend of the higher prevalence of myopia in the younger age groups is supported by the fact that in 1934 the prevalence of myopia among 18-year-old schoolchildren in Hungary was found to be 10.6%, which is almost 6 times lower than the current value[15]. The rise in myopia in younger age groups nowadays could be attributed to children's intensive education training, which both extends near work and reduces outdoor time[5],[9].
In France, the highest prevalence of myopia was also found in the age groups between 10-39y of age, with a similarly high peak for the prevalence of myopia in those aged 20-29y, which was 52.4%[8]. The European Eye Epidemiology Consortium also found higher rates of myopia (SE≤-0.75 D) in younger age groups around 40%), and higher rates of hyperopia (SE≥1.0 D, around 55%) in those older than 50y of age[12]. When comparing our results with previous data[8],[20], we found a similar prevalence of hyperopia in older age groups; however, we found a higher prevalence of myopia in younger age groups, which may be due to the increasing myopia epidemics in younger individuals.
Significant geographical differences, however, have also been reported from Europe[21]–[24]. A study of Norwegian adolescents found a completely different distribution than we found in the present study, which in fact seem to defy worldwide trends. That study found that in 16-19 year-old Norwegian individuals, the prevalence of myopia and hyperopia was 12.7% and 56.7%, respectively[6]. In another study in Norway, the general population exhibited a higher prevalence of myopia (SE≤-0.25 D, 33%)[22]. These lower prevalences of myopia might be due to a potentially delayed onset of myopia compared to other parts of Europe and East-Asia[6],[22]. Among university students, however, an even higher prevalence of myopia (46.9%) and lower prevalence of hyperopia were found (29.5%)[22]. Fledelius[23] found a similarly high (50.0%) prevalence of myopia (SE≤-0.5 D) among medical students (median age, 26y) in Denmark, with no obvious trend of an increasing prevalence of academic myopia, despite an increasing prevalence in the overall population. A study in the UK, which focused on younger white adults, 18-20y of age, found a lower prevalence both of myopia (18.6%) and hyperopia (17.7%), but did note a significant increasing tendency of myopia[13]. A study in Israel found a relatively low prevalence of myopia among 16-19-year-old, but noted a 1.3-fold increase in those over 24y of age, from 20.4 to 26.2%, respectively[24].
We found a higher prevalence of myopia in those 76y and older than in those in the 51-75y range. This difference may be due to the well-known effects of nuclear sclerosis of the lens, and also to the fact that many of those 76y or older in Hungary had already undergone cataract surgery, with a typical outcome target refraction between 0 to -1 D. We know from our previous Rapid Assessment of Avoidable Blindness (RAAB) study that 25.1% of the 75y and older Hungarian population have already undergone cataract surgery with intraocular lens implantation[3],[25]. In this same age group in a French study by Montrachet[26], the crude prevalence of myopia increased with age, and was found to be higher in pseudophakic (40%-50%) than in phakic eyes (23%-32%), while hyperopia was far lower in pseudophakic than phakic eyes (9%-16% vs 49%-59%, respectively)[26].
Altogether, we found that a bimodal pattern represented the prevalence of myopia across various age-groups in Hungary, with a peak seen in younger age groups, those between 18 and 35y of age, and another peek seen in those older than 75y of age. A similar bimodal pattern was found in France, Germany, and a few other countries, as well[8],[20],[27]–[28].
High myopia was found to have a low prevalence in our Hungarian sample, but the 10-fold increase found with ageing and the expected increase in the future spur the need for preventive actions, especially as there is no safe threshold for myopia in regards to its complications, related eye diseases, and associated visual impairment[21]. Pathologic myopic diseases, e.g., macular degeneration, retinal detachment, optic neuropathy, and other severe complications, may be due to the elongation of the eyeball seen in myopia. In this respect, it is important to note that elongation is not necessarily proportional to refraction but only in eyeballs with medium and high myopia[29]. In particular, 20.9% of cases of low myopia are due to a purely corneal origin, with no eyeball elongation; moreover, emmetropic, and even hypermetropic eyes, can be found to have elongated eyeballs, with possibility of myopic complications[29].
How to Decrease the Onset of Myopia and Its Associated Visual Impairments
An increase in the frequency of myopia, and the associated rise in blindness and visual impairments due to myopia, are well documented worldwide[1]–[2],[4]–[5]. The growing number of younger individuals worldwide with low and high myopia spurs the need to develop and implement guidelines and programs to reduce the incidence and progression of myopia, which many countries and organisations have already done worldwide in the last decade[30]. The National Committee for the Prevention of Blindness in China and the International Myopia Institute have recently published their white papers on myopia and the prevention of blindness[5]. In New Zealand, the multidisciplinary Myopia Action Group (NZMAG) was created[31], and currently, the European Society of Ophthalmology has developed a European update and guidance on myopia management[21]. Currently, the need for the prevention of myopia and its progression are more real, as home confinement during the coronavirus 2019 (COVID-19) outbreak might worsen the global burden of myopia[32].
Limitations
The present study does have some limitations. First, the Comprehensive Health Screening Program of Hungary, 2010-2020, covers a large number of cases and individuals, ranging in age from 18 to 99 years old. Participants, however, were not chosen at statistical random, but rather their inclusion was voluntary, which may have influenced the results, as individuals with complaints may be motivated to participate, while people with good vision may not[17]. However, we believe that the risk of sampling bias may be relatively low from an ophthalmic viewpoint for two reasons: first, about half of the program provided screening for large companies and organisations where participation rates are typically above 90%, ensuring that there is no selection bias; second, the other half of the screening program, is based on the participation of individuals from all across the country in their respective villages or towns, which are visited by screening teams. Due to the availability of 40 different types of examinations of body functions in the same place on the same day, which involves a free and immediate evaluation, the primary drive for participation in these public screenings is a person's interest in their general health, and curiosity about what their body and its functions are like. Because ophthalmic examinations are a minor component and have no priority over other examinations, participation may be regarded as random and free of selection bias form an ophthalmic viewpoint.
Another limitation of the present study is that the refractive measurements were performed using non-cycloplegic automated refractometry which may overestimate myopia while underestimating hyperopia and emmetropia[33]. As the possibility of measurement error varies with age, the use of cycloplegia is generally accepted for research of children and adolescents, but it is controversial for studies of young adults, and a targeted investigation found that cycloplegia is not required in population estimates of refractive errors after the age of 20[34]. Many large epidemiological studies, however, have used non-cycloplegic refraction[8],[12], making our findings comparable to similar studies.
In summary, 60% of the overall population has refractive errors in Hungary. Myopia (43%) is the most common refractive error, and its prevalence is increasing significantly among younger age groups (up to 61%). A national myopia program for children must be implemented, including more time spent outdoors and less time spent doing near work, to prevent the onset of myopia. Additionally, a national screening of pre-myopes and the introduction of myopia-controlling interventions (e.g., low dose atropine and orthokeratology) would be beneficial to slow the progression of myopia[21],[31].
Acknowledgments
Authors' contributions: Németh J was responsible for analyzing data, interpreting results, updating reference list and writing the report. Daiki T was responsible for extracting and analyzing data. Dankovics G and Barna I was responsible for designing the survey and conducting the data collection. Limburg H and Nagy ZZS provided feedback on the report and contributed to writing the report.
Conflicts of Interest: Németh J, None; Daiki T, None; Dankovics G, None; Barna I, None; Limburg H, None; Nagy ZZS, None.
REFERENCES
- 1.Fricke TR, Jong M, Naidoo KS, Sankaridurg P, Naduvilath TJ, Ho SM, Wong TY, Resnikoff S. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, Meta-analysis and modelling. Br J Ophthalmol. 2018;102(7):855–862. doi: 10.1136/bjophthalmol-2017-311266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Szabó D, Sándor GL, Tóth G, Pék A, Lukács R, Szalai I, Tóth GZ, Papp A, Nagy ZZ, Limburg H, Németh J. Visual impairment and blindness in Hungary. Acta Ophthalmol. 2018;96(2):168–173. doi: 10.1111/aos.13542. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organisation. World Report on Vision. 2019. [Accessed on 04 Feb. 2021]. https://www.who.int/publications/i/item/world-report-on-vision.
- 5.Resnikoff S, Jonas JB, Friedman D, He M, Jong M, Nichols JJ, Ohno-Matsui K, Wildsoet CF, Taylor HR, Wolffsohn JS, Wong TY. Myopia - A 21st century public health issue. Invest Ophthalmol Vis Sci. 2019;60(3):Mi–Mii. doi: 10.1167/iovs.18-25983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hagen LA, Gjelle JVB, Arnegard S, Pedersen HR, Gilson SJ, Baraas RC. Prevalence and possible factors of myopia in Norwegian adolescents. Sci Rep. 2018;8(1):13479. doi: 10.1038/s41598-018-31790-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lundberg K, Suhr Thykjaer A, Søgaard Hansen R, Vestergaard AH, Jacobsen N, Goldschmidt E, Lima RA, Peto T, Wedderkopp N, Grauslund J. Physical activity and myopia in Danish children-The CHAMPS Eye Study. Acta Ophthalmol. 2018;96(2):134–141. doi: 10.1111/aos.13513. [DOI] [PubMed] [Google Scholar]
- 8.Matamoros E, Ingrand P, Pelen F, Bentaleb Y, Weber M, Korobelnik JF, Souied E, Leveziel N. Prevalence of myopia in France: a cross-sectional analysis. Medicine (Baltimore) 2015;94(45):e1976. doi: 10.1097/MD.0000000000001976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O'Donoghue L, Kapetanankis VV, McClelland JF, Logan NS, Owen CG, Saunders KJ, Rudnicka AR. Risk factors for childhood myopia: findings from the NICER study. Invest Ophthalmol Vis Sci. 2015;56(3):1524–1530. doi: 10.1167/iovs.14-15549. [DOI] [PubMed] [Google Scholar]
- 10.Rudnicka AR, Owen CG, Nightingale CM, Cook DG, Whincup PH. Ethnic differences in the prevalence of myopia and ocular biometry in 10- and 11-year-old children: the Child Heart and Health Study in England (CHASE) Invest Ophthalmol Vis Sci. 2010;51(12):6270–6276. doi: 10.1167/iovs.10-5528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tideman JWL, Polling JR, Vingerling JR, Jaddoe VWV, Williams C, Guggenheim JA, Klaver CCW. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018;96(3):301–309. doi: 10.1111/aos.13603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams KM, Verhoeven VJM, Cumberland P, et al. Prevalence of refractive error in Europe: the European eye epidemiology (E^3) consortium. Eur J Epidemiol. 2015;30(4):305–315. doi: 10.1007/s10654-015-0010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCullough SJ, O'Donoghue L, Saunders KJ. Six year refractive change among white children and young adults: evidence for significant increase in myopia among white UK children. PLoS One. 2016;11(1):e0146332. doi: 10.1371/journal.pone.0146332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pärssinen O, Soh ZD, Tan CS, Lanca C, Kauppinen M, Saw SM. Comparison of myopic progression in Finnish and Singaporean children. Acta Ophthalmol. 2021;99(2):171–180. doi: 10.1111/aos.14545. [DOI] [PubMed] [Google Scholar]
- 15.Cs Mócsy M, Sz Ajtay M. Refraction of ten thousand students. Iskola és Egészségügy. 1934;2:62–68. [Google Scholar]
- 16.Györffy I, Mezey P. On the frequency of refractive errors and eye-diseases. Szemészet. 1963;100:95–99. [PubMed] [Google Scholar]
- 17.Barna I, Kékes E, Halmy E, Balogh Z, Kubányi J, Szőts G, Németh J, Pécsvárady Zs, Majoros A, Daiki T, Erdei O, Dankovics G. Summary data of Hungary's Comprehensive Health Screening Program (MAESZ) 2010-2019. LAM. 2020;30:89–102. [Google Scholar]
- 18.Hungarian Central Statistical Office. Population of Hungary by sex and age, 1 January 2018. https://www.ksh.hu/interaktiv/korfak/orszag.html.
- 19.Cumberland PM, Bao YC, Hysi PG, Foster PJ, Hammond CJ, Rahi JS, UK Biobank Eyes & Vision Consortium Frequency and distribution of refractive error in adult life: methodology and findings of the UK biobank study. PLoS One. 2015;10(10):e0139780. doi: 10.1371/journal.pone.0139780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Foster PJ, Jiang Y. Epidemiology of myopia. Eye (Lond) 2014;28(2):202–208. doi: 10.1038/eye.2013.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Németh J, Tapasztó B, Aclimandos WA, et al. Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur J Ophthalmol. 2021;31(3):853–883. doi: 10.1177/1120672121998960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kinge B, Midelfart A, Jacobsen G. Refractive errors among young adults and university students in Norway. Acta Ophthalmol Scand. 1998;76(6):692–695. doi: 10.1034/j.1600-0420.1998.760612.x. [DOI] [PubMed] [Google Scholar]
- 23.Fledelius HC. Myopia profile in Copenhagen medical students 1996-98. Refractive stability over a century is suggested. Acta Ophthalmol Scand. 2000;78(5):501–505. doi: 10.1034/j.1600-0420.2000.078005501.x. [DOI] [PubMed] [Google Scholar]
- 24.Shapira Y, Mimouni M, Machluf Y, Chaiter Y, Saab H, Mezer E. The increasing burden of myopia in Israel among young adults over a generation: analysis of predisposing factors. Ophthalmology. 2019;126(12):1617–1626. doi: 10.1016/j.ophtha.2019.06.025. [DOI] [PubMed] [Google Scholar]
- 25.Sándor GL, Tóth G, Szabó D, Szalai I, Lukács R, Pék A, Tóth GZ, Papp A, Nagy ZZ, Limburg H, Németh J. Cataract blindness in Hungary. Int J Ophthalmol. 2020;13(3):438–444. doi: 10.18240/ijo.2020.03.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Creuzot-Garcher C, Binquet C, Daniel S, Bretillon L, Acar N, de Lazzer A, Arnould L, Tzourio C, Bron AM, Delcourt C. The Montrachet Study: study design, methodology and analysis of visual acuity and refractive errors in an elderly population. Acta Ophthalmol. 2016;94(2):e90–e97. doi: 10.1111/aos.12842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zocher MT, Rozema JJ, Oertel N, Dawczynski J, Wiedemann P, Rauscher FG, EVICR net Biometry and visual function of a healthy cohort in Leipzig, Germany. BMC Ophthalmol. 2016;16:79. doi: 10.1186/s12886-016-0232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weale RA. Epidemiology of refractive errors and presbyopia. Surv Ophthalmol. 2003;48(5):515–543. doi: 10.1016/s0039-6257(03)00086-9. [DOI] [PubMed] [Google Scholar]
- 29.Barcsay G, Nagy ZZ, Németh J. Distribution of axial, corneal, and combined ametropia in a refractive surgery unit. Eur J Ophthalmol. 2003;13(9-10):739–744. doi: 10.1177/1120672103013009-1001. [DOI] [PubMed] [Google Scholar]
- 30.Németh J, Tóth G, Resnikoff S, de Faber JT. Preventing blindness and visual impairment in Europe: what do we have to do? Eur J Ophthalmol. 2019;29(2):129–132. doi: 10.1177/1120672118819397. [DOI] [PubMed] [Google Scholar]
- 31.Petty AD, Wilson G. Reducing the impact of the impending myopia epidemic in New Zealand. N Z Med J. 2018;131(1487):80–85. [PubMed] [Google Scholar]
- 32.Pellegrini M, Bernabei F, Scorcia V, Giannaccare G. May home confinement during the COVID-19 outbreak worsen the global burden of myopia? Graefes Arch Clin Exp Ophthalmol. 2020;258(9):2069–2070. doi: 10.1007/s00417-020-04728-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sun YY, Wei SF, Li SM, Hu JP, Yang XH, Cao K, Lin CX, Du JL, Guo JY, Li H, Liu LR, Morgan IG, Wang NL. Cycloplegic refraction by 1% cyclopentolate in young adults: is it the gold standard? The Anyang University Students Eye Study (AUSES) Br J Ophthalmol. 2018 doi: 10.1136/bjophthalmol-2018-312199. [DOI] [PubMed] [Google Scholar]
- 34.Sanfilippo PG, Chu BS, Bigault O, Kearns LS, Boon MY, Young TL, Hammond CJ, Hewitt AW, MacKey DA. What is the appropriate age cut-off for cycloplegia in refraction? Acta Ophthalmol. 2014;92(6):e458–e462. doi: 10.1111/aos.12388. [DOI] [PubMed] [Google Scholar]


