Abstract
We investigated whether the coronavirus disease 2019 (COVID-19) pandemic, in conjunction with public health measures, influenced the incidence of gastrointestinal diseases according to age and sex during the pandemic. Changes in the monthly incidence rates (January 2018 to June 2021) of common gastrointestinal diseases were assessed using data from the Korean National Health Insurance Service by comparing the data of two periods: before COVID-19 (January 2018–February 2020) and during COVID-19 (March 2020–June 2021). The Mann–Whitney U test and Levene’s test were used to compare the differences in the incidences before and during the pandemic. In the pandemic period, compared to in the pre-COVID-19 period, the incidence rates of ulcerative colitis, Crohn’s disease, cholelithiasis, and esophageal reflux significantly increased, whereas those of infective enteritis and irritable bowel syndrome decreased, regardless of age or sex. There were no significant changes in the incidence rates of pancreatitis, acute appendicitis, liver cirrhosis, and hemorrhoids. No seasonal variations in gastrointestinal disease occurrence were observed. In conclusion, the COVID-19 pandemic may have had unprecedented and long-term impacts on the epidemiology of gastrointestinal disease. These changes may indicate a substantial future burden on healthcare resources during the recovery phase of the pandemic and thereafter.
Keywords: COVID-19, gastrointestinal disease, epidemiology, incidence rate
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has led to a shift in the patterns of incidences of various diseases, and a paradigm shift in healthcare systems over the past 2 years [1,2]. A wide range of public health interventions, including both non-pharmaceutical (e.g., hand washing, social distancing, face mask use, voluntary quarantine, travel restrictions, limiting nonessential activities, school closures, and shutting down borders) and pharmaceutical (e.g., ventilators and vaccines) measures have been enforced worldwide against the COVID-19 pandemic [3], of which the former may inhibit human-to-human infections by avoiding the transmission of aerosols that are emitted by infected patients [4]. These measures have led to unprecedented changes in behavioral patterns, as well as the occurrence of other infectious diseases [5]. For example, previous studies have shown a significant decline in the incidence of upper and lower respiratory tract infections such as seasonal influenza, and some non-infectious diseases in pediatric populations [5,6,7,8,9,10]. However, there are a lack of national-level data on yearly or seasonal changes in the incidence rates of gastrointestinal (GI) diseases, which are commonly encountered in clinical settings.
The number of endoscopic and surgical procedures for GI diseases declined by 50–90% during the COVID-19 pandemic [1,2,11,12], with an overall operation cancellation rate of 72% for benign GI diseases [12]. As compared with corresponding durations in 2018 and 2019, in 2020–2022, regular follow-up visits for GI diseases were interrupted or delayed by the pandemic [1,2,13]. The spread of COVID-19 has been impeded due to the enforcement of preventive hygiene policies such as mask wearing, hand washing, and social distancing [5]. These lifestyle changes have also drastically reduced the incidence of other infectious diseases [5], such as GI viral infections that are transmitted through the fecal-to-oral route or direct contact between people [14]. Hence, the COVID-19 pandemic may have had a major influence on the occurrence and management of other GI diseases [6]. Since GI symptoms are also observed in patients with COVID-19 and have been associated with severe COVID-19 disease [15], healthcare providers should promptly differentiate between COVID-19 and non-COVID-19 GI diseases, keeping in mind the prevalence of GI diseases. Nevertheless, there is a lack of studies on the incidence trends of non-COVID-19 GI diseases and the influence of age, sex, and seasonal variation on the same during the national pandemic crisis. In anticipation of the recovery phase of the pandemic and the subsequent post-pandemic era, it is important for healthcare providers to develop preventive programs than can address a potentially significant shift in the incidence of GI diseases.
The present study analyzed data from the nationwide Korean National Health Insurance Service database to determine the changes in the incidence rates of GI diseases due to the COVID-19 pandemic, as well as the influence of seasonal variation, age, and sex. We hypothesized that the incidence rates of both infectious and non-infectious GI diseases were impacted by the COVID-19 pandemic. This study highlights the importance of monitoring GI disease incidence during the COVID-19 pandemic and the need for appropriate planning to address the anticipated challenges in prevention and treatment during the post-pandemic period.
2. Materials and Methods
2.1. Ethics
The study protocol was approved by the ethics committee of Hallym University (2021-11-004). The requirement for written informed consent was waived by the institutional review board.
2.2. Participants and Data Collection
South Korea’s population of over 50 million is under the National Health Insurance (NHI) program. The NHI collects medical information from facilities ranging from primary clinics to tertiary hospitals in one unified database. These data are publicly available for national-level research on disease epidemiology. As the first COVID-19 patients in South Korea were identified on 20 January 2020 and disease prevention and infection control measures were started on the national level in March 2020, we compared the following two periods in the present study: January 2018–February 2020 (before COVID-19) and March 2020–June 2021 (during COVID-19).
We evaluated the monthly incidence rates of the top 10 GI diseases that were common at medical institutions from January 2018 through to June 2021. The incidences of those diseases were investigated using the medical histories of patients’ who visited the clinics for each GI disease. The diagnosis of GI diseases was based on the following International Classification of Diseases-10 codes: cholelithiasis (K80); pancreatitis (K85, K860, K861); infective enteritis (A04, A05, A08, A09); Crohn’s disease (K50); ulcerative colitis (K51); acute appendicitis (K35, K36, K37); liver cirrhosis (K74, K702, K703); esophageal reflux (K21); hemorrhoids including perianal venous thrombosis (K64); and irritable bowel syndrome including other functional intestinal disorders (K58, K59). The diagnostic codes are registered by physicians. Since the patients were identified with a unique resident registration number in the NHI that covered both hospitals and primary clinics, none of the disease incidence data were duplicated.
2.3. Statistical Analysis
Differences in the mean incidence rates of the diseases before and during the COVID-19 pandemic were compared using the Mann–Whitney U test for nonparametric values. The differences in the variances of medical visits for the diseases before and during the COVID-19 pandemic were compared using Levene’s test for nonparametric values [16]. Subgroup analyses were performed for age (0–19, 20–59, and 60+ years old) and sex. Two-tailed analyses were conducted, and the level of statistical significance was set at p < 0.05. All statistical analyses were conducted with SPSS version 22.0 (IBM, Armonk, NY, USA).
3. Results
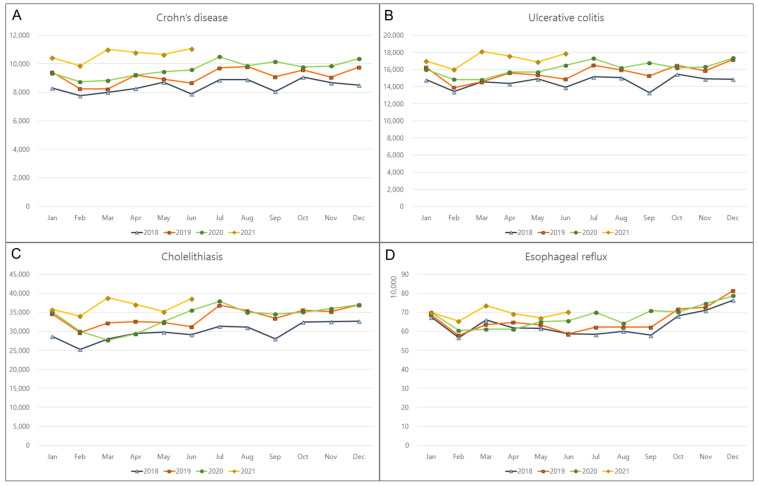
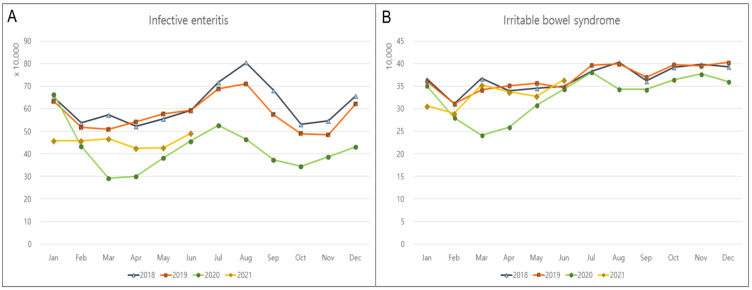
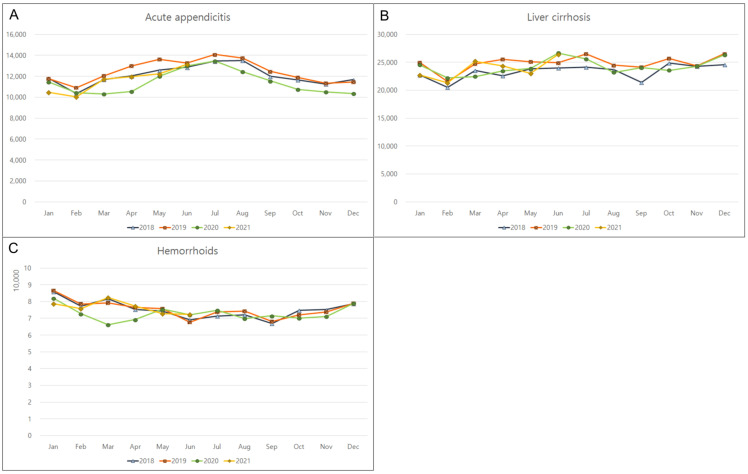
The monthly incidence rates of the top 10 GI diseases that were unrelated to COVID-19 were monitored from January 2018 to June 2021. The incidence rates of Crohn’s disease, ulcerative colitis, cholelithiasis, and esophageal reflux significantly increased by 14.6% (p < 0.001); 10% (p < 0.001), 9.7% (p = 0.003); and 5.8% (p = 0.030), respectively, during the pandemic (Table 1; Figure 1). In contrast, there was a significant decline in the incidence rates of infective enteritis (29.5%, p < 0.001) and irritable bowel syndrome (9%, p = 0.007) (Figure 2). No significant changes were observed in the incidences of pancreatitis, acute appendicitis, liver cirrhosis, or hemorrhoids during the COVID-19 pandemic (Figure 3). Monthly or seasonal variations in the incidence rates of the monitored GI diseases were unremarkable in the overall population, regardless of the COVID-19 pandemic period.
Table 1.
Differences in the means and standard deviations of incidences of diseases before and during COVID-19.
| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance † | |
| Cholelithiasis | 31,908.2 | 2980.4 | 34,999.7 | 3053.7 | 0.003 * | 0.842 |
| Pancreatitis | 9376.2 | 487.7 | 9397.0 | 562.6 | 0.786 | 0.952 |
| Infective enteritis | 592,974.9 | 86,207.8 | 418,206.6 | 66,354.2 | <0.001 * | 0.117 |
| Crohn’s disease | 8799.0 | 595.7 | 10,087.6 | 644.9 | <0.001 * | 0.268 |
| Ulcerative colitis | 15,125.1 | 946.1 | 16,638.8 | 889.8 | <0.001 * | 0.501 |
| Acute appendicitis | 12,173.0 | 1016.7 | 11,537.4 | 1127.0 | 0.100 | 0.506 |
| Liver cirrhosis | 24,059.7 | 1490.0 | 24,171.6 | 1535.7 | 0.816 | 0.559 |
| Esophageal reflux | 647,717.8 | 62,784.3 | 685,385.2 | 47,978.9 | 0.030 * | 0.141 |
| Hemorrhoids | 75,509.2 | 5076.9 | 73,697.4 | 4252.5 | 0.300 | 0.988 |
| Irritable bowel syndrome | 364,276.6 | 31,985.2 | 331,089.3 | 40,512.7 | 0.007 * | 0.499 |
* Mann–Whitney U test, significance at <0.05. † Levene’s test in non-parametric data, significance at <0.05.
Figure 1.
Overall increase in the monthly incidences of gastrointestinal diseases in 2018, 2019, 2020, and 2021. (A) Crohn’s disease, (B) ulcerative colitis, (C) cholelithiasis, and (D) esophageal reflux.
Figure 2.
Overall decrease in the monthly incidences of gastrointestinal diseases in 2018, 2019, 2020, and 2021. (A) Infective enteritis and (B) irritable bowel syndrome.
Figure 3.
Lack of overall changes in the monthly incidences of gastrointestinal diseases in 2018, 2019, 2020, and 2021. (A) Acute appendicitis, (B) liver cirrhosis, and (C) hemorrhoids.
Regarding sex, fluctuations in the incidence rates throughout the COVID-19 pandemic were observed among men. There was an increase in the incidence rates of Crohn’s disease (16%), cholelithiasis (10.2%), ulcerative colitis (10%), and esophageal reflux (5%); in contrast, the incidence rates of infective enteritis and irritable bowel syndrome decreased by 30% and 10%, respectively (all p < 0.05, Table 2). Among women, Crohn’s disease (12%) showed the largest increase in incidence, followed by ulcerative colitis (10%), cholelithiasis (9%), and esophageal reflux (7%) (all p < 0.05); the incidence rates of infective enteritis and irritable bowel syndrome had significantly decreased by 28.8% (p < 0.001) and 8.6% (p = 0.004), respectively.
Table 2.
Sex-based differences in the means and standard deviations of incidences of diseases before and during COVID-19.
| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance † | |
| Men | ||||||
| Cholelithiasis | 15,126.3 | 1399.4 | 16,671.3 | 1336.0 | 0.002 * | 0.901 |
| Pancreatitis | 6460.2 | 326.1 | 6424.1 | 352.6 | 0.698 | 0.990 |
| Infective enteritis | 280,916.2 | 42,954.1 | 195,956.6 | 32,499.2 | <0.001 * | 0.109 |
| Crohn’s disease | 6170.8 | 426.8 | 7138.8 | 468.1 | <0.001 * | 0.187 |
| Ulcerative colitis | 9028.5 | 554.6 | 9952.4 | 508.6 | <0.001 * | 0.282 |
| Acute appendicitis | 6292.9 | 508.5 | 5951.8 | 554.3 | 0.070 | 0.342 |
| Liver cirrhosis | 14,234.9 | 830.9 | 14,091.3 | 858.3 | 0.338 | 0.672 |
| Esophageal reflux | 274,281.2 | 29,925.5 | 287,298.8 | 22,815.4 | 0.049 * | 0.141 |
| Hemorrhoids | 39,706.4 | 2771.5 | 38,089.9 | 2122.7 | 0.055 | 0.674 |
| Irritable bowel syndrome | 170,369.7 | 16,209.7 | 153,845.9 | 19,914.3 | 0.011 * | 0.866 |
| Women | ||||||
| Cholelithiasis | 16,781.9 | 1598.0 | 18,328.4 | 1739.5 | 0.005 * | 0.942 |
| Pancreatitis | 2935.6 | 173.7 | 2972.9 | 216.8 | 0.453 | 0.211 |
| Infective enteritis | 312,058.7 | 43,398.8 | 222,250.1 | 33,911.1 | <0.001 * | 0.103 |
| Crohn’s disease | 2628.3 | 176.0 | 2948.8 | 182.7 | <0.001 * | 0.459 |
| Ulcerative colitis | 6096.6 | 396.8 | 6686.4 | 391.3 | <0.001 * | 0.579 |
| Acute appendicitis | 5880.1 | 518.6 | 5585.6 | 580.9 | 0.178 | 0.499 |
| Liver cirrhosis | 9824.8 | 667.1 | 10,080.3 | 699.2 | 0.468 | 0.550 |
| Esophageal reflux | 373,436.5 | 33,381.3 | 398,086.4 | 25,737.6 | 0.013 * | 0.276 |
| Hemorrhoids | 35,802.8 | 2341.0 | 35,607.6 | 2195.4 | 0.816 | 0.878 |
| Irritable bowel syndrome | 193,907.0 | 16,213.5 | 177,243.3 | 20,934.0 | 0.004 * | 0.451 |
* Mann–Whitney U test, significance at <0.05. † Levene’s test in non-parametric data, significance at <0.05.
A subgroup analysis by age indicated that the incidence rate of Crohn’s disease in the pediatric subgroup (0–19 years old) increased during the pandemic by 16%, compared to the average rate that was reported for the prior 2 years (p < 0.001). In contrast, the incidence rates of infective enteritis, irritable bowel syndrome, acute appendicitis, and hemorrhoids had reduced by 42%, 25%, 21%, and 11%, respectively (all p < 0.05, Table 3). The monthly variation in the incidence of liver cirrhosis was lower during the COVID-19 pandemic than before (SD = 3.6 vs. 6.5, p = 0.010), whereas that of esophageal reflux was higher during the pandemic (SD = 4486.2 vs. 2626.0, p = 0.003), although the mean yearly occurrences of those diseases were relatively constant (p = 0.194 and p = 0.816, respectively).
Table 3.
Age-based differences in the means and standard deviations of incidences of diseases before and during COVID-19.
| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance | |
| Age 0–19 years old | ||||||
| Cholelithiasis | 126.0 | 17.4 | 129.3 | 18.3 | 0.364 | 0.469 |
| Pancreatitis | 154.9 | 24.2 | 150.4 | 24.4 | 0.907 | 0.140 |
| Infective enteritis | 253,267.9 | 43,009.3 | 148,682.7 | 36,095.9 | <0.001 * | 0.076 |
| Crohn’s disease | 1198.3 | 72.2 | 1391.4 | 139.5 | <0.001 * | 0.905 |
| Ulcerative colitis | 510.6 | 40.3 | 506.8 | 34.0 | 0.907 | 0.923 |
| Acute appendicitis | 2668.0 | 334.7 | 2128.2 | 321.7 | <0.001 * | 0.211 |
| Liver cirrhosis | 21.9 | 6.5 | 20.1 | 3.6 | 0.194 | 0.010 † |
| Esophageal reflux | 18,068.5 | 2626.0 | 18,186.0 | 4486.2 | 0.816 | 0.003 † |
| Hemorrhoids | 2165.0 | 283.3 | 1941.1 | 166.7 | 0.004 * | 0.895 |
| Irritable bowel syndrome | 59,571.1 | 9637.7 | 44,838.4 | 9480.1 | <0.001 * | 0.173 |
| Age 20–59 years old | ||||||
| Cholelithiasis | 14,874.7 | 1467.3 | 15,915.9 | 1463.0 | 0.026 * | 0.754 |
| Pancreatitis | 5609.0 | 257.6 | 5393.8 | 278.6 | 0.008 * | 0.680 |
| Infective enteritis | 249,570.0 | 40,599.1 | 189,414.1 | 29,746.8 | <0.001 * | 0.428 |
| Crohn’s disease | 6928.2 | 491.9 | 7876.1 | 456.5 | <0.001 * | 0.272 |
| Ulcerative colitis | 10,469.3 | 628.4 | 11,397.7 | 578.1 | <0.001 * | 0.651 |
| Acute appendicitis | 7431.3 | 626.9 | 7214.0 | 664.0 | 0.319 | 0.183 |
| Liver cirrhosis | 10,709.2 | 537.2 | 9589.1 | 678.8 | <0.001 * | 0.296 |
| Esophageal reflux | 353,522.5 | 41,252.4 | 362,350.3 | 27,233.5 | 0.147 | 0.008 † |
| Hemorrhoids | 54,427.3 | 3560.4 | 51,725.9 | 2417.1 | 0.013 * | 0.510 |
| Irritable bowel syndrome | 163,525.9 | 18,245.6 | 143,566.3 | 20,468.9 | 0.004 * | 0.861 |
| Age 60+ years old | ||||||
| Cholelithiasis | 16,934.4 | 1563.0 | 18,987.3 | 1649.2 | <0.001 * | 0.848 |
| Pancreatitis | 3639.8 | 257.5 | 3861.1 | 289.1 | 0.013 * | 0.365 |
| Infective enteritis | 90,246.6 | 8755.6 | 80,201.4 | 8146.2 | 0.003 * | 0.575 |
| Crohn’s disease | 680.1 | 67.3 | 829.5 | 78.0 | <0.001 * | 0.191 |
| Ulcerative colitis | 4156.8 | 313.8 | 4748.4 | 312.2 | <0.001 * | 0.163 |
| Acute appendicitis | 2086.7 | 149.7 | 2209.4 | 203.7 | 0.076 | 0.312 |
| Liver cirrhosis | 13,350.0 | 1051.1 | 14,581.4 | 1014.7 | 0.001 * | 0.701 |
| Esophageal reflux | 276,550.2 | 24,140.3 | 305,290.8 | 21,752.4 | 0.001 * | 0.405 |
| Hemorrhoids | 19,012.7 | 1777.7 | 20,122.5 | 2018.1 | 0.120 | 0.916 |
| Irritable bowel syndrome | 141,340.6 | 9617.7 | 142,834.1 | 13,519.3 | 0.365 | 0.100 |
* Mann–Whitney U test, significance at <0.05. † Levene’s test in non-parametric data, significance at <0.05.
In the adult subgroup (20–59 years old), the incidence rates of Crohn’s disease, ulcerative colitis, and cholelithiasis had increased by 13.7% (p < 0.001), 8.9% (p < 0.001), and 7% (p = 0.026), respectively, during the pandemic. The incidence rates of infective enteritis, irritable bowel syndrome, liver cirrhosis, hemorrhoids, and pancreatitis decreased by 24.4% (p < 0.001); 12.2% (p = 0.004); 10.4% (p < 0.001); 5% (p = 0.013); and 4% (p = 0.008), respectively. The monthly variation in the incidence of esophageal reflux was lower during the COVID-19 pandemic than before (SD = 27,233.5 vs. 41,252.4, p = 0.008).
In the older subgroup (>60 years), an increase in the incidence rates during the pandemic was observed for the following six GI diseases: Crohn’s disease (22%, p < 0.001); ulcerative colitis (14%, p < 0.001); cholelithiasis (12.1%, p < 0.001); esophageal reflux (10.4%, p = 0.001); liver cirrhosis (9%, p = 0.001); and pancreatitis (6%, p = 0.013). The incidence rate of infective enteritis had reduced by 11% during the pandemic period (p = 0.003).
4. Discussion
There is a lack of research on the differences in the national incidence rates of GI diseases before and during the COVID-19 pandemic, while accounting for the moderating effects of age and sex. Using a Korean nationwide data set, we demonstrated that the current COVID-19 pandemic led to a reconfiguration of the incidence patterns of both infectious and non-infectious GI diseases in patients without COVID-19. Over the past 2 years of the pandemic, the incidence rate of inflammatory bowel diseases (including Crohn’s disease and ulcerative colitis) showed the highest increase among all GI diseases, while that of infective enteritis showed the most significant decline; these trends were consistent, irrespective of age subgroup or sex. Our findings are applicable to non-COVID-19 GI diseases across South Korea and highlight the need for effective preventive and therapeutic public health initiatives at the national level to address anticipated changes in the burden of care, both in the recovery phase from the COVID-19 pandemic and in the post-pandemic period.
The incidence rates of inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis were 14.6% and 10% higher, respectively, during the pandemic than the rates in the pre-COVID-19 period. Both of these inflammatory bowel diseases are chronic and immune-mediated conditions [17]. The finding that the incidence rates of these two inflammatory bowel diseases increased consistently across all age subgroups requires special attention, as older patients with immune-mediated diseases are particularly vulnerable to both COVID-19 and opportunistic infections and have higher morbidity and mortality rates [17]. Thus, appropriate medical care for these inflammatory bowel diseases should be specifically adapted for pediatric, adult, and older patients. With the establishment of the Realignment of the Health Care Institution Use System during the pandemic, 270 hospitals in South Korea were designated as COVID-19 protection hospitals and the remaining health care institutions were required to ensure non-COVID-19 patients’ safety and access to hospitals by separating areas for patients with respiratory illnesses from those for patients with other illnesses since 30 September 2020 [18]. Although telemedicine services were previously considered to be illegal in South Korea, the government allowed physicians to offer over-the-phone medical consultation and prescriptions temporarily, until the end of the COVID-19 outbreak. Moreover, the health care institutions and pharmacies were open as usual as per the Infectious Disease Prevention and Management Act. Therefore, the patients with chronic disease, including inflammatory bowel diseases, could use the hospitals and pharmacies without any inconvenient restrictions, so the inaccessibility of hospitals or pharmacies does not explain the increase in the incidence of inflammatory bowel diseases during the pandemic. The reason for the increase in the number of people affected by inflammatory bowel diseases during the COVID-19 pandemic is currently unclear; stress during this period might have contributed to disease deterioration [19,20]. Previous studies have linked globally stressful disasters to symptom deterioration and increased disease severity among patients with Crohn’s disease and ulcerative colitis [19,20]. The relevance of pandemic-related stress might be supported by the latest national and international demands for heightened attention to mental disorders and psychological distress during this pandemic [21,22].
We found that the incidence rates of cholelithiasis and esophageal reflux significantly increased by 9.7% and 5.8%, respectively, during the COVID-19 pandemic. The elevated incidence rate of cholelithiasis was evident in both the adult and older subgroups, while that of esophageal reflux was only identified in the older subgroup. Although cholelithiasis is a very common disease that can occur in 20% of the population in developed countries, complicated cases may require hospital admission and critical care [23]. Esophageal reflux may lead to an increased risk of both COVID-19 and aspiration pneumonia in all ages [24,25], and it might be one of the manifestations of stress affecting a wide range of gastrointestinal disorders, including inflammatory bowel disease [26]. In particular, the monthly variation in esophageal reflux was found in pediatric and adult groups, although the yearly mean disease occurrences were relatively constant. The monthly variance in esophageal reflux in children may be one of the overweight/obesity-related comorbidities that are caused by a lack of outdoor or school activities, and dietary changes such as increased snacking at home, owing to school closure [27]. Thus, medical services for these diseases may require specific care, according to age group.
Further, a significant decline in the number of cholelithiasis cases was noted in the early phase of the pandemic period; however, a subsequent increase occurred over time. This finding is in line with that of a previous study that was carried out in Germany, which reported a 20% increase in the incidence rate of cholelithiasis/cholecystitis during the COVID-19 pandemic in mid-2020, compared to that the pre-COVID-19 period in 2019 [28]. The authors suggested that postponing emergency care for patients with cholelithiasis in the beginning of the pandemic outbreak could have resulted in an increased need for care upon the subsequent loosening of the infection control measures, such as social distancing [28]. Due to the increase in the number of cholelithiasis cases, a long surgical waiting list is currently a major problem in Spanish medical institutions [29]. These observations emphasize the need for appropriate changes in health care systems to accommodate the anticipated backlog of cases requiring surgical care, as long delays before definitive treatment are likely to result in increased morbidity and mortality.
We observed a 29.5% reduction in infective enteritis cases during the COVID-19 pandemic. This finding may be ascribed to the implementation of infection control policies during the pandemic and may have implications for the incidence of other GI infectious diseases. Indeed, a previous study that was conducted in South Korea reported that viral pathogens that were responsible for GI infections drastically diminished during the pandemic period [14]. The incidence rates of infections with total viruses, norovirus, group A rotavirus, and enteric adenovirus were 32%, 40.2%, 31.8%, and 13.4% lower, respectively, during the pandemic than the rates in the 2-year period before the pandemic [14]. In South Korea, non-pharmaceutical interventions such as social distancing, online schooling, the restriction of gatherings, and personal protective measures were strictly enforced during the COVID-19 pandemic [3]. These interventions not only suppressed the spread of COVID-19, but also appeared to have a large impact on the incidence of other infectious diseases, including GI infections [5,6,7,14].
A 9% reduction in irritable bowel syndrome cases was observed in the pandemic period from that in the pre-COVID-19 period; however, the reason for this change is currently unclear, and the phenomenon is referred to as “COVID-19 irritable bowel syndrome paradox” [30]. Irritable bowel syndrome is a frequent functional GI disorder with a prevalence of 3–5% worldwide [26]. Patients may complain of repetitive abdominal pain that is accompanied with changes in the consistency or frequency of stools, without any gross peculiarity [31]. Several studies have presented strong evidence that irritable bowel syndrome is a stress-sensitive illness; the primary effects of psychosocial stress on gut physiology involve increases in visceral hypersensitivity and mucosal permeability, changes in gut motility and secretions, and negative effects on gut microbiota [26,32]. The sudden arrival of the COVID-19 pandemic likely acted as a major stressor for patients with irritable bowel syndrome [26]. Unexpectedly, our survey showed a paradoxical decline in irritable bowel syndrome cases during the COVID-19 pandemic, instead of symptom deterioration [30]. Lockdowns allowed easy access to toilets at home, and the subsequent adoption of flexible work and school schedules in Singapore, Japan, and France resulted in a decrease in illnesses, as well as improvements in sleep and exercise, reduced burnout, an improved sense of well-being, and a reduction in commute-related stress [30,31,33]. These factors may have contributed to the decrease in symptom severity among patients with irritable bowel syndrome, which might have reduced their need for professional medical care [31].
No significant changes in yearly average incidences of pancreatitis, acute appendicitis, liver cirrhosis, or hemorrhoids were observed in the overall population between the pre-COVID-19 and pandemic periods, suggesting that these diseases might not have been severely affected by the lifestyle changes that were made during the pandemic. Pancreatitis and liver cirrhosis are likely related to existing alcohol-use disorder, because alcohol-related pancreatic or liver disease often occurs after years of regular, heavy alcohol use [15]. Since those diseases are relatively common, sometimes requiring emergency surgery or critical care [15,34,35], the similar rates of medical visits for those diseases between two periods may be related to the stability of medical systems. In addition, there were no monthly or seasonal variations in GI diseases in the overall population when comparing the corresponding months before and during the COVID-19 pandemic, except for some diseases in different age groups. Hence, either changes in disease incidence rates were evenly distributed across all seasons, or there were no seasonal variations in disease incidence rates.
This study has several limitations. First, the results might not be applicable to other countries due to discrepancies in the severity of the COVID-19 pandemic in different countries [36,37]. Second, this study was based on health claims data that categorized diseases using diagnostic codes; therefore, undiagnosed or subclinical diseases could not be accounted for. Third, specific data on the differences in presentations between primary care and hospital visits, which might indicate disease severity, were not collected. In addition, we were unable to reconfirm the accuracy of the diagnoses, as we did not have access to laboratory test results. In order to minimize potential bias due to disease misclassification, we analyzed data of 2 years (2018 and 2019) before the COVID-19 pandemic period. Fourth, possible bias due to multiple comparisons could not be excluded, as we analyzed 10 GI diseases. Nonetheless, the main strength of this study is that it collected data from a centralized nationwide healthcare database that included every citizen that attended a primary care or hospital clinic. Therefore, our results may offer valuable information for understanding the main changes in GI diseases and the possible underlying causes during the pandemic crisis in the South Korean context.
5. Conclusions
The COVID-19 pandemic era has altered the incidence patterns of certain GI diseases, and this may foreshadow an increased burden of those diseases in the aftermath of the pandemic. The unprecedented changes highlight the need for the restructuring of healthcare systems at a national level to address anticipated changes in the burden of care, both in the recovery phase and the post-pandemic period.
Author Contributions
M.J.K., investigation, funding acquisition, writing—original draft, review and editing; H.G.C., funding acquisition, project administration; H.S.K. and H.L., funding acquisition, methodology; J.-H.K. and J.H.K., formal analysis; S.-J.C. and E.S.N., methodology; K.-W.M. and H.Y.P., software; N.Y.K., validation. All authors have agreed to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The present study was approved by the ethics committee of Hallym University (2019-10-023), and the requirement for written informed consent was waived by the Institutional Review Board.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are available from the database of the National Health Insurance Sharing Service (NHISS) https://nhiss.nhis.or.kr/ (accessed on 31 August 2021). The NHISS grants researchers access to its data if they agree to follow the research ethics at a cost. Those seeking access to the data in this article can download the data from the website after agreeing to follow the research ethics.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded in part by the National Research Foundation (NRF) of Korea from the Korean Ministry of Science and ICT, grant No. NRF-2021-R1C1C1004986 to HGC, grant No. NRF-2021R1G1A1093593 to HSK, grant No. NRF-2019R1C1C1004463 to MJK and grant No. NRF-2022R1F1A1065335 to MJK. The APC was funded by NRF-2019R1C1C1004463.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kim K.H., Kim S.B., Kim T.N. Changes in endoscopic patterns before and during COVID-19 outbreak: Experience at a single tertiary center in Korean. World J. Clin. Cases. 2021;9:3576–3585. doi: 10.12998/wjcc.v9.i15.3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiriac S., Stanciu C., Cojocariu C., Sfarti C., Singeap A.M., Girleanu I., Cuciureanu T., Huiban L., David D., Zenovia S., et al. The impact of the COVID-19 pandemic on gastrointestinal endoscopy activity in a tertiary care center from Northeastern Romania. Healthcare. 2021;9:100. doi: 10.3390/healthcare9010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dighe A., Cattarino L., Cuomo-Dannenburg G., Skarp J., Imai N., Bhatia S., Gaythorpe K.A.M., Ainslie K.E.C., Baguelin M., Bhatt S., et al. Response to COVID-19 in South Korea and implications for lifting stringent interventions. BMC Med. 2020;18:321. doi: 10.1186/s12916-020-01791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aiello A.E., Murray G.F., Perez V., Coulborn R.M., Davis B.M., Uddin M., Shay D.K., Waterman S.H., Monto A.S. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: A randomized intervention trial. J. Infect. Dis. 2010;201:491–498. doi: 10.1086/650396. [DOI] [PubMed] [Google Scholar]
- 5.Mun S.K., Yang B.R., Chang M. Changes in respiratory diseases in South Korea during the COVID-19 pandemic: An interrupted time series study. BMJ Glob. Health. 2021;6:e006912. doi: 10.1136/bmjgh-2021-006912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoo I.H., Kang H.M., Jeong D.C. Changes in the incidence of intussusception and infectious diseases after the COVID-19 Pandemic in Korea. J. Korean Med. Sci. 2022;37:e60. doi: 10.3346/jkms.2022.37.e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang Q.S., Wood T., Jelley L., Jennings T., Jefferies S., Daniells K., Nesdale A., Dowell T., Turner N., Campbell-Stokes P., et al. Impact of the COVID-19 nonpharmaceutical interventions on influenza and other respiratory viral infections in New Zealand. Nat. Commun. 2021;12:1001. doi: 10.1038/s41467-021-21157-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu P., Xu M., Cao L., Su L., Lu L., Dong N., Jia R., Zhu X., Xu J. Impact of COVID-19 pandemic on the prevalence of respiratory viruses in children with lower respiratory tract infections in China. Virol. J. 2021;18:159. doi: 10.1186/s12985-021-01627-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tempia S., Walaza S., Bhiman J.N., McMorrow M.L., Moyes J., Mkhencele T., Meiring S., Quan V., Bishop K., McAnerney J.M., et al. Decline of influenza and respiratory syncytial virus detection in facility-based surveillance during the COVID-19 pandemic, South Africa, January to October 2020. Eurosurveillance. 2021;26:2001600. doi: 10.2807/1560-7917.ES.2021.26.29.2001600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee K.H., Yon D.K., Suh D.I. Prevalence of allergic diseases among Korean adolescents during the COVID-19 pandemic: Comparison with pre-COVID-19 11-year trends. Eur. Rev. Med. Pharm. Sci. 2022;26:2556–2568. doi: 10.26355/eurrev_202204_28492. [DOI] [PubMed] [Google Scholar]
- 11.Ielpo B., Prieto M., Ortega I., Balibrea J.M., Rubio-Perez I., Juvany M., Gomez-Bravo M.A., Ramia J.M. National survey on the treatment of cholelitiasis in Spain during the initial period of the COVID-19 pandemic. Cir. Esp. 2021;99:346–353. doi: 10.1016/j.ciresp.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lisi G., Campanelli M., Grande S., Milito G., Grande M. Sclerotherapy with 3% polidocanol foam for third- and fourth-degree hemorrhoids as “bridge treatment” during the COVID-19 pandemic in Italy. Int. J. Colorectal Dis. 2021;36:1321–1322. doi: 10.1007/s00384-021-03848-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seo S., Suda K., Kato H., Abe E., Kosaka S., Fujiwara K., Ochi T., Koga H., Urao M., Okazaki T., et al. Decreased incidence of intussusception during the COVID-19 pandemic. Trends in pediatric surgical emergencies. Pediatr. Surg. Int. 2021;37:1761–1764. doi: 10.1007/s00383-021-04992-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahn S.Y., Park J.Y., Lim I.S., Chae S.A., Yun S.W., Lee N.M., Kim S.Y., Choi B.S., Yi D.Y. Changes in the occurrence of gastrointestinal infections after COVID-19 in Korea. J. Korean Med. Sci. 2021;36:e180. doi: 10.3346/jkms.2021.36.e180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Velez C., Paz M., Silvernale C., Stratton L.W., Kuo B., Staller K., Suffolk County C.-G.S.A. Factors associated with chronic de novo post-coronavirus disease gastrointestinal disorders in a metropolitan US County. Clin. Gastroenterol. Hepatol. 2021;20:e1488–e1492. doi: 10.1016/j.cgh.2021.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nordstokke D.W., Zumbo B.D. A New Nonparametric Levene Test for Equal Variances. Psicológica. 2010;31:401–430. [Google Scholar]
- 17.Monteleone G., Ardizzone S. Are patients with inflammatory bowel disease at increased risk for COVID-19 infection? J. Crohns Colitis. 2020;14:1334–1336. doi: 10.1093/ecco-jcc/jjaa061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeong G.H., Lee H.J., Lee J., Lee J.Y., Lee K.H., Han Y.J., Yoon S., Ryu S., Kim D.K., Park M.B., et al. Effective control of COVID-19 in South Korea: Cross-sectional study of epidemiological data. J. Med. Internet Res. 2020;22:e22103. doi: 10.2196/22103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodday S.M., Travis S., Walsh A., Friend S.H. Stress-related consequences of the coronavirus disease 2019 pandemic on symptoms of Crohn’s disease. Eur. J. Gastroenterol. Hepatol. 2021;33:1511–1516. doi: 10.1097/MEG.0000000000002081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shiga H., Miyazawa T., Kinouchi Y., Takahashi S., Tominaga G., Takahashi H., Takagi S., Obana N., Kikuchi T., Oomori S., et al. Life-event stress induced by the Great East Japan Earthquake was associated with relapse in ulcerative colitis but not Crohn’s disease: A retrospective cohort study. BMJ Open. 2013;3:e002294. doi: 10.1136/bmjopen-2012-002294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaufman K.R., Petkova E., Bhui K.S., Schulze T.G. A global needs assessment in times of a global crisis: World psychiatry response to the COVID-19 pandemic. BJPsych Open. 2020;6:e48. doi: 10.1192/bjo.2020.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee S.Y., Ro Y.S., Jeong J., Shin S.D., Moon S. Impact of the COVID-19 Pandemic on the incidence and characteristics of patients with psychiatric illnesses visiting emergency departments in Korea. J. Clin. Med. 2022;11:488. doi: 10.3390/jcm11030488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Portincasa P., Molina-Molina E., Garruti G., Wang D.Q. Critical care aspects of gallstone disease. J. Crit. Care Med. 2019;5:6–18. doi: 10.2478/jccm-2019-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ong J.S., Gharahkhani P., Vaughan T.L., Whiteman D., Kendall B.J., MacGregor S. Assessing the genetic relationship between gastro-esophageal reflux disease and risk of COVID-19 infection. Hum. Mol. Genet. 2022;31:471–480. doi: 10.1093/hmg/ddab253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sikavi D.R., Cai J.X., Leung R., Carroll T.L., Chan W.W. Impaired proximal esophageal contractility predicts pharyngeal reflux in patients with laryngopharyngeal reflux symptoms. Clin. Transl. Gastroenterol. 2021;12:e00408. doi: 10.14309/ctg.0000000000000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Konturek P.C., Brzozowski T., Konturek S.J. Stress and the gut: Pathophysiology, clinical consequences, diagnostic approach and treatment options. J. Physiol. Pharm. 2011;62:591–599. [PubMed] [Google Scholar]
- 27.Hu P., Samuels S., Maciejewski K.R., Li F., Aloe C., Name M.V., Savoye M., Sharifi M. Changes in weight-related health behaviors and social determinants of health among youth with overweight/obesity during the COVID-19 Pandemic. Child. Obes. 2021. ahead of print . [DOI] [PMC free article] [PubMed]
- 28.Jaehn P., Holmberg C., Uhlenbrock G., Pohl A., Finkenzeller T., Pawlik M.T., Quack I., Ernstberger A., Rockmann F., Schreyer A.G. Differential trends of admissions in accident and emergency departments during the COVID-19 pandemic in Germany. BMC Emerg. Med. 2021;21:42. doi: 10.1186/s12873-021-00436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prieto M., Ortega I., Balibrea J.M., Ielpo B. Management of cholelithiasis in times of COVID-19: A challenge for the system. Cir. Esp. 2021;99:699–700. doi: 10.1016/j.ciresp.2021.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quek S.X.Z., Loo E.X.L., Demutska A., Chua C.E., Kew G.S., Wong S., Lau H.X., Low E.X.S., Loh T.L., Lung O.S., et al. Impact of the coronavirus disease 2019 pandemic on irritable bowel syndrome. J. Gastroenterol. Hepatol. 2021;36:2187–2197. doi: 10.1111/jgh.15466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sabate J.M., Deutsch D., Melchior C., Entremont A., Mion F., Bouchoucha M., Facon S., Raynaud J.J., Zerbib F., Jouet P. COVID-19 pandemic and lockdown stress consequences in people with and without Irritable Bowel Syndrome. Ethics Med. Public Health. 2021;18:100660. doi: 10.1016/j.jemep.2021.100660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Mahony L., McCarthy J., Kelly P., Hurley G., Luo F., Chen K., O’Sullivan G.C., Kiely B., Collins J.K., Shanahan F., et al. Lactobacillus and bifidobacterium in irritable bowel syndrome: Symptom responses and relationship to cytokine profiles. Gastroenterology. 2005;128:541–551. doi: 10.1053/j.gastro.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 33.Oshima T., Siah K.T.H., Yoshimoto T., Miura K., Tomita T., Fukui H., Miwa H. Impacts of the COVID-19 pandemic on functional dyspepsia and irritable bowel syndrome: A population-based survey. J. Gastroenterol. Hepatol. 2021;36:1820–1827. doi: 10.1111/jgh.15346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yawar B., Marzouk A., Ali H., Asim A., Ghorab T., Bahli Z., Abousamra M., Fleville S. Acute pancreatitis during COVID-19 pandemic: An overview of patient demographics, disease severity, management and outcomes in an acute district hospital in Northern Ireland. Cureus. 2021;13:e18520. doi: 10.7759/cureus.18520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baral S., Chhetri R.K., Thapa N. Comparison of acute appendicitis before and within lockdown period in COVID-19 era: A retrospective study from rural Nepal. PLoS ONE. 2021;16:e0245137. doi: 10.1371/journal.pone.0245137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim S.Y., Kim D.W. Does the clinical spectrum of Coronavirus Disease 2019 (COVID-19) show regional differences? Clin. Exp. Otorhinolaryngol. 2020;13:83–84. doi: 10.21053/ceo.2020.00612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Park J.H., Jang W., Kim S.W., Lee J., Lim Y.S., Cho C.G., Park S.W., Kim B.H. The clinical manifestations and chest computed tomography findings of Coronavirus Disease 2019 (COVID-19) patients in China: A proportion meta-analysis. Clin. Exp. Otorhinolaryngol. 2020;13:95–105. doi: 10.21053/ceo.2020.00570. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available from the database of the National Health Insurance Sharing Service (NHISS) https://nhiss.nhis.or.kr/ (accessed on 31 August 2021). The NHISS grants researchers access to its data if they agree to follow the research ethics at a cost. Those seeking access to the data in this article can download the data from the website after agreeing to follow the research ethics.