Abstract
Objective:
A common intervention to prevent alcohol-impaired driving are alcohol ignition interlock devices (IIDs), which prevent drivers with a blood alcohol concentration greater than .025% from starting the car. These devices force drivers to adapt their drinking to accommodate the device. Prior studies indicated a transfer of risk as some drivers with an IID may increase cannabis use as they decrease alcohol use. This study examines whether this increase in cannabis use persists after IID removal when alcohol use reverts to pre-IID levels.
Method:
The data are from the Managing Heavy Drinking (MHD) study of drivers in New York State. The MHD is a comprehensive three-wave study of drivers convicted of driving under the influence from 2015 to 2020. Participants (N = 189) completed all waves, and provided oral fluid/blood and hair samples to measure cannabis and alcohol use, respectively. Mixed between-within analysis of variance was conducted to assess cannabis use at IID installation (Time 1), removal (Time 2), and at 6-month follow-up (Time 3).
Results:
In aggregate, participants increased their cannabis use over the course of the study. Drivers who decreased their alcohol use while the IID was installed on their car significantly increased their cannabis use while the IID was in place and further increased cannabis use after the device's removal.
Conclusions:
IIDs are efficacious in preventing alcohol-impaired driving. However, in some cases, they may have the unintended effect of increasing other substance use. The current study outlines the need for supplemental treatment interventions while on IID to prevent a transfer of risk to other substances, or polysubstance use after the device is removed.
Driving under the influence (dui) of alcohol continues to be a major public health concern (National Highway Traffic Safety Administration, 2019a, 2019b). Installing alcohol ignition interlock devices (IIDs) on the vehicles of drivers recently convicted of an impaired driving offense has been shown to be effective at reducing rate of alcohol-impaired driving (Voas et al., 2016), alcohol-related collisions (Voas, 2020), and alcohol-related re-arrests while the device is installed (Elder et al., 2011; Vanlaar et al., 2017). These reductions have been found in addition to the decrease in alcohol consumption following the initial arrest (Voas et al., 2021). The relative success of alcohol IIDs in reducing adverse alcohol-related outcomes has contributed to their growing adoption as a mandatory intervention for alcohol-impaired driving violations in nearly every state in the United States and many countries throughout the world.
As a result of IID installation, drivers are forced to adjust some of their behaviors to accommodate the alcohol-related restrictions imposed by the device. These accommodations include the use of alternative transportation modes (e.g., increased use of public transportation, bicycles) as well as changing how often and where they consume alcohol (Nochajski et al., 2020; Romosz et al., 2021), even if drivers do not necessarily decrease the amount of alcohol they consume on average (Marques et al., 2010). In part, it is these adjustments made while the IID is installed that may explain the reduction of adverse alcohol-related outcomes. However, following the removal of the device, recidivism rates often return to pre-IID levels (Elder et al., 2011; Voas et al., 2020; Willis et al., 2004).
Of note, in some cases, policies designed to limit the availability of alcohol to users have had the unintended consequence of promoting the use of another substance (Scherer et al., 2020). This phenomenon is attributed to filling a void resulting from abstaining from an addictive behavior and a need to cope with internal or external stressors (Sussman & Black, 2008). The substituting of substances in alcohol treatment settings is hypothesized to produce the desired appetitive effects with the activity or compulsive behaviors that occur from addictions. Additionally, the substitution achieves a pathway to the personal, societal, and or familial benefits that addiction often brings (Sussman, 2017). By a similar mechanism, then, there is the potential that installing an IID on a vehicle unintentionally creates a transfer of risk—from drunk driving to drugged driving—each of which has a significant contribution to crash risk (Hels et al., 2011; Li, 2012). Equally important, however, are drivers who increase their other drug use while the interlock is installed and continue to use these drugs when the device is removed. These drivers who demonstrate an increase in cannabis use may now be at risk for the additive combination of alcohol and cannabis. Research has demonstrated an increased crash risk compared with those who use neither or only one of the two substances (Hels et al., 2011; Wilson et al., 2014). Given that the most commonly co-occurring substance used with alcohol among drivers on interlock is cannabis (Scherer et al., 2018), an exploration of cannabis use with an interlock installed is necessary.
Cannabis use and driving
Indeed, despite the high levels of use of both substances, the rate of weekend nighttime drivers who have positive blood alcohol concentrations (BACs) has steadily dropped from 12.4% in 2007 to 8.3% in 2014 according to the most recent data from a nationwide roadside survey conducted by the National Highway Traffic Safety Administration (Ramirez et al., 2016). However, cannabis use among drivers has steadily increased in recent years. In 2007, 4.5% of daytime drivers and 7.7% of nighttime drivers tested positive for cannabis (Lacey et al., 2009). In 2014, those numbers increased to 7.4% of daytime drivers and 11.3% of nighttime drivers (Kelley-Baker et al., 2017). The rate of drivers using cannabis and driving is compounded by the legalization of cannabis for medicinal and/or recreational use throughout the United States. In Colorado, for example, although traffic fatalities decreased 14.8% from 2007 to 2012, traffic fatalities in which the driver tested positive for cannabis increased from 7% to 16.5% in the same period (Rocky Mountain High Intensity Drug Trafficking Area, 2016).
Given the likelihood of other substance use among problematic alcohol users who are forced to restrict their alcohol consumption (Alter et al., 2006; Reiman, 2009), the high co-occurrence of alcohol and cannabis use, and the general increase in cannabis use in the United States and throughout the world, it is little surprise that research has found an increase in cannabis use by some drivers while the interlock is installed on the vehicle (Scherer et al., 2020). In their study, Scherer and colleagues found that, among those who decreased their alcohol use while on interlock, there was also a significant increase in cannabis use relative to pre-interlock levels of use. The increase in cannabis use while individuals had an IID installed on their vehicles could be attributed to various reasons. One such possibility is the common perception that driving under the influence of cannabis is less risky than driving under the influence of alcohol (Greene, 2018; Wadsworth & Hammond, 2018; Wickens et al., 2019). Further, some individuals may feel they are more conscientious of their surroundings while driving under the influence of cannabis as opposed to driving while completely sober. This means that in their view, using cannabis before driving may actually improve their driving ability (Greene, 2018).
To relate this to drivers with the interlock, it is conceivable that when the IID forces drivers to restrict their alcohol use, they opt to use a substance they believe may improve their performance while driving. What is not clear, however, is whether this increase in cannabis use persists when the IID is removed from their vehicle. Further, if cannabis use remains at the relatively high levels following the device removal, would alcohol use revert to pre-IID levels as some prior IID literature has suggested (Elder et al., 2011; Willis et al., 2004)? If so, this could mean that following the removal of the IID, some drivers are at risk for polysubstance use while driving. Prior studies have found that polysubstance-using drivers have notably adverse driving-related outcomes including impaired driving and crash involvement (Hels et al., 2011; Movig et al., 2004; Scherer et al., 2018). However, the role IIDs may play in this relationship is unclear. The current study is an effort to examine what happens to the alcohol and cannabis use patterns of drivers after the IID is removed from the vehicle.
Method
The current analysis was pulled from a study of alcohol IID installers in Erie County, NY, called the Managing Heavy Drinking (MHD) study, a comprehensive three-wave study of drivers convicted of a DUI from 2015 to 2020. The MHD includes data from interlock providers, self-report, and biomarkers. The parent study recruited participants (N = 277) using fliers distributed at impaired-driving classes, victim impact panels, alcohol ignition interlock installation centers, substance abuse treatment facilities, and health centers. Participants in the MHD identified primarily as male (n = 161, 58.1%) and White, not Hispanic (n = 223, 80.5%). Although this sample was somewhat homogeneous, this demographic make-up is consistent with the demographics for Erie County, NY, from where the sample was drawn (U.S. Census, 2019). Less than half of MHD participants had a history of alcohol or drug treatment (45.1%) and only 20.5% were mandated by the courts to receive alcohol treatment. The MHD protocol called for collection of biological data, which provided objective evaluation of substance use behaviors to augment self-report.
In 2009, the state of New York passed Leandra's Law, which requires that an alcohol IID be installed on all vehicles of a person convicted of a DUI (Leandra's Law, 2009). If a person chooses not to install the device, the alternative is to remove their car from the road or sell it. State monitoring agencies do ongoing checks of the Department of Motor Vehicles’ database to show that the individual convicted of a DUI has not registered a car without an IID throughout their sentence period if they did not install an alcohol IID or claimed that they could not install it because they did not have a car. Effectively, this means that all drivers convicted of a DUI who wished to continue to drive have had an alcohol IID installed.
Recruitment
The current study used a subsample of the total MHD participant pool. To be included, the participant needed to have installed an alcohol IID; provided blood and hair samples for cannabis and alcohol screening, respectively; and provided data for all three time points (N = 189). In the parent MHD study, recruitment fliers were distributed at impaired-driving classes, victim impact panels, alcohol ignition interlock installation centers, substance abuse treatment facilities, and health centers. After responding to the fliers, participants were interviewed by study staff at a research center or in a mobile office where computer surveys and interviews were conducted and blood and hair samples collected (Time 1 [T1]). Participants were tracked by study staff and brought back to complete Time 2 (T2) evaluations around the time the IID was removed from the vehicle (about 4–8 months), and Time 3 (T3) evaluations approximately 6 months after the device was removed. Participants in the MHD were remunerated $125 for completing T1 interviews, $75 for T2 interviews, and $125 for T3 interviews. Participants were also offered an additional $25 at each time point to provide blood samples—for a total of $400 per participant. Overall retention of participants from T1 to T3 was 85.6%.
Measures
Demographic data. The demographic information collected were age, sex, and race/ethnicity. For sex, participants were given the option of male, female, or their own descriptor, but all participants in the current study selected either male or female. Age was coded as a continuous variable. Race comprised White, Black, Asian, Pacific Islander, Middle Eastern, Native Alaskan or American Indian, biracial, and other. Ethnicity included Hispanic and non-Hispanic—however, because of limited variation in race/ethnicity (consistent with the demographic makeup of Erie County, NY) resulting in low individual cell counts, the variable was trichotomized into “non-Hispanic White” and “Black” or “other.”
Prior DUI status. Participants self-reported on any history with having an alcohol IID installed on a vehicle and/or prior alcohol DUI convictions. When possible, study staff confirmed this information with the Department of Motor Vehicles.
Alcohol use. Alcohol use was measured at each of the three time periods using hair Ethyl Glucuronide (hEtG) in participant hair samples. Samples were approximately 3 cm in length at all time points and were shipped to a laboratory in Bad Salzuflen, Germany for preparation, analysis, and measurement of hEtG via tandem mass spectrometry. hEtG is a widely used biomarker used to assess alcohol use proclivity over the prior 1–3 months (Biondi et al., 2019) and has been used previously to examine patterns of alcohol use among drivers convicted of a DUI (Marques et al., 2014; Scherer et al., 2020).
Cannabis use. Blood samples were collected at each of the three time periods to assess for the presence of Δ-9-tetrahydrocannabinol (THC)—the active ingredient in cannabis. Blood was collected by trained phlebotomists and sent to a laboratory (Immunalysis, Pasadena, CA) where screenings were conducted using enzyme-linked immunosorbent assay. Specimens that screened positive were confirmed using either gas chromatography with mass spectral detection or liquid chromatography with tandem mass spectral detection. The minimum detection criteria for cannabis in blood was 10 ng/ml. Participants with no cannabis in their blood, or a cannabis level under the minimum detection criteria, were given a value of 0 ng/L.
Analytic approach
Descriptive statistics and chi-square solutions were calculated for participant demographics. We also applied regression analyses to estimate cannabis use at each of the three time periods. When conducting regression analyses, assumptions of multicollinearity were assessed using variance inflation factors, which revealed no values exceeding 1.5. Mahalanobis’ Distance Test identified no outliers to be removed from the current data set. Variables measuring blood THC and hEtG levels demonstrated significantly skewed distributions (skewness ranged from 3.514 to 9.133 and kurtosis ranged from 3.821 to 16.512). As such, these variables were normalized using log-adjustment.
A mixed between-within subjects analysis of variance was used to assess temporal fluctuations in cannabis use across three levels of alcohol use behaviors. Consistent with prior research (Scherer et al., 2020), alcohol conditions were trichotomized based on deviations (or lack thereof) of alcohol use behaviors from T1 to T2. Specifically, those that decreased their alcohol use (i.e., hEtG levels at T2 less than 90% of their T1 hEtG levels) were classified as the “alcohol decrease” (AD) group; those that maintained their alcohol use behaviors (i.e., hEtG levels ±10% of their T1 hEtG levels) were classified as the “alcohol maintenance” (AM) group; and those that increased their alcohol use (i.e., hEtG levels were greater than 110% of their T1 hEtG levels) were classified as the “alcohol increase” (AI) group. Multivariate linear regression analyses were used to determine the impact of demographic factors, prior DUI status, and alcohol change group membership on total lockout ratios and high BAC lockout ratios. Data were analyzed using IBM SPSS Statistics for Windows, Version 21 (IBM Corp., Armonk, NY).
Results
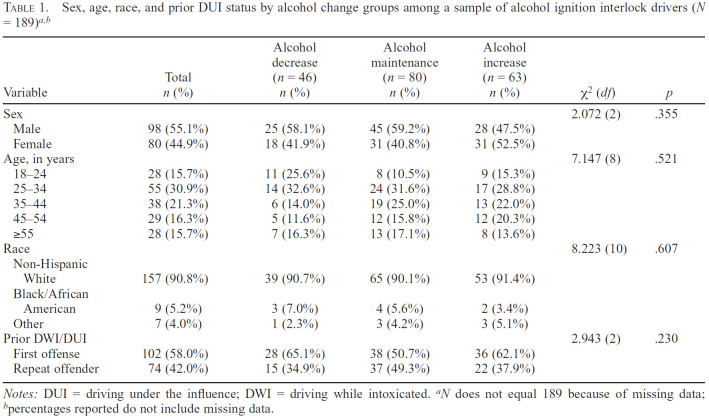
Participants in the current study primarily identified as male (55.1%). Participants overwhelmingly identified as non-Hispanic White (90.8%), whereas 5.2% identified as Black and 4.0% other. Participant ages varied from 18.8 years to 72.62 years, with an average age of 38.08 (SD = 12.79). More than half of the sample denied having had a prior DUI offense (58%), with the remainder reporting at least one prior DUI offense (42%). Participants were divided into one of three alcohol change groups based on changes in alcohol consumption from T1 to T2. The majority of participants fell into the alcohol maintenance group (42.3%), whereas about a third increased their alcohol use (33.3%), and about a quarter decreased their alcohol use from T1 to T2 (24.3%). No significant differences were found in demographic distributions between the three alcohol change groups (Table 1). The demographics of participants in the current study were comparable to the demographics in the MHD.
Table 1.
Sex, age, race, and prior DUI status by alcohol change groups among a sample of alcohol ignition interlock drivers (N = 189)a,b
| Variable | Total n (%) | Alcohol decrease (n = 46) n (%) | Alcohol maintenance (n = 80) n (%) | Alcohol increase (n = 63) n (%) | χ2(df) | P |
|---|---|---|---|---|---|---|
| Sex | 2.072 (2) | .355 | ||||
| Male | 98 (55.1%) | 25 (58.1%) | 45 (59.2%) | 28 (47.5%) | ||
| Female | 80 (44.9%) | 18 (41.9%) | 31 (40.8%) | 31 (52.5%) | ||
| Age, in years | 7.147 (8) | .521 | ||||
| 18-24 | 28 (15.7%) | 11 (25.6%) | 8 (10.5%) | 9 (15.3%) | ||
| 25-34 | 55 (30.9%) | 14 (32.6%) | 24 (31.6%) | 17 (28.8%) | ||
| 35-44 | 38 (21.3%) | 6 (14.0%) | 19 (25.0%) | 13 (22.0%) | ||
| 45-54 | 29 (16.3%) | 5 (11.6%) | 12 (15.8%) | 12 (20.3%) | ||
| ≥55 | 28 (15.7%) | 7 (16.3%) | 13 (17.1%) | 8 (13.6%) | ||
| Race | 8.223 (10) | .607 | ||||
| Non-Hispanic White | 157 (90.8%) | 39 (90.7%) | 65 (90.1%) | 53 (91.4%) | ||
| Black/African American | 9 (5.2%) | 3 (7.0%) | 4 (5.6%) | 2 (3.4%) | ||
| Other | 7 (4.0%) | 1 (2.3%) | 3 (4.2%) | 3 (5.1%) | ||
| Prior DWI/DUI | 2.943 (2) | .230 | ||||
| First offense | 102 (58.0%) | 28 (65.1%) | 38 (50.7%) | 36 (62.1%) | ||
| Repeat offender | 74 (42.0%) | 15 (34.9%) | 37 (49.3%) | 22 (37.9%) |
Notes: DUI = driving under the influence; DWI = driving while intoxicated.
N does not equal 189 because of missing data;
percentages reported do not include missing data.
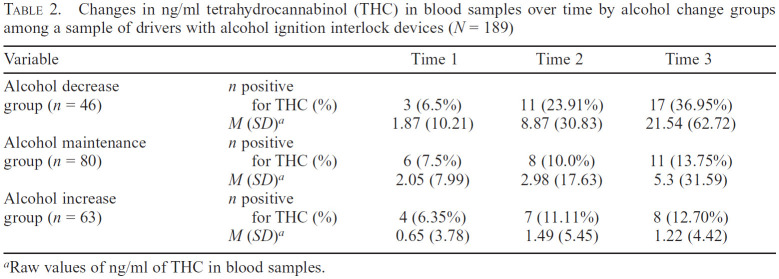
The purpose of the current study was to follow up on prior research conducted by Scherer et al. (2020) and examine change in THC levels in drivers both over the duration of the alcohol IID (T1 to T2) and after its removal (T3). To do this, we first looked at overall trends of cannabis use in the sample. As can be seen in Figure 1, there was a general increase in cannabis use over time through the entire sample. However, when cannabis use was parceled out by alcohol change condition, participants in the AD condition increased their mean cannabis use more than those in either the AM or AI conditions. Similarly, the number of participants in the AD condition who tested positive for THC in their blood increased over the course of the study at greater rates than those in the AM or AI conditions (Table 2).
Figure 1.
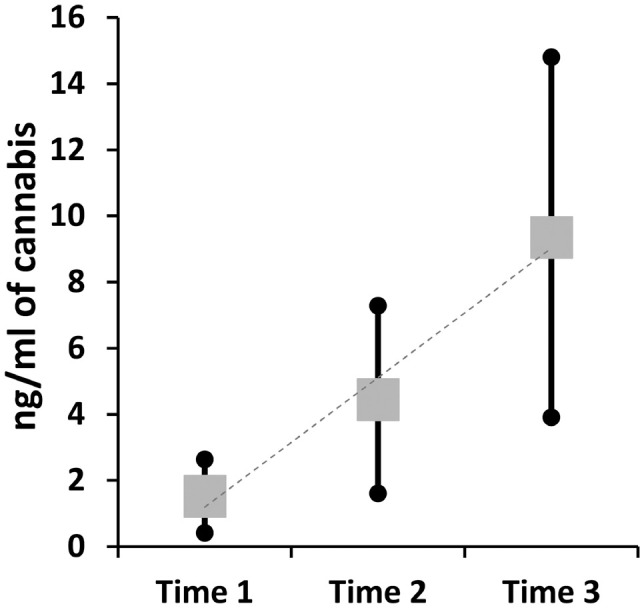
Main effects of estimates of log-adjusted ng/ml of THC in blood by time period among a sample of interlock drivers (N =189)
Table 2.
Changes in ng/ml tetrahydrocannabinol (THC) in blood samples over time by alcohol change groups among a sample of drivers with alcohol ignition interlock devices (N = 189)
| Variable | Time 1 | Time 2 | Time 3 | |
|---|---|---|---|---|
| Alcohol decrease group (n = 46) | n positive for THC (%) | 3 (6.5%) | 11 (23.91%) | 17 (36.95%) |
| M (SD)a | 1.87 (10.21) | 8.87 (30.83) | 21.54 (62.72) | |
| Alcohol maintenance | n positive | |||
| group (n = 80) | for THC (%) | 6 (7.5%) | 8 (10.0%) | 11 (13.75%) |
| M (SD)a | 2.05 (7.99) | 2.98 (17.63) | 5.3 (31.59) | |
| Alcohol increase | n positive | |||
| group (n = 63) | for THC (%) | 4 (6.35%) | 7 (11.11%) | 8 (12.70%) |
| M (SD)a | 0.65 (3.78) | 1.49 (5.45) | 1.22 (4.42) |
Raw values of ng/ml of THC in blood samples.
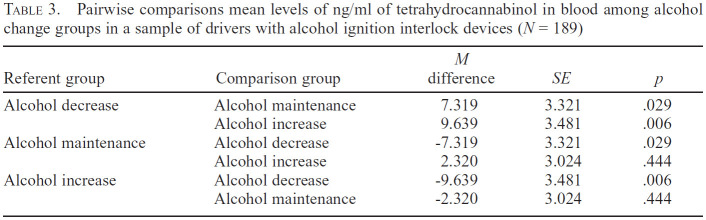
Unsurprisingly, these results yielded a significant main effect for time, F(2, 185) = 5.577, p = .004, partial η2 = .057. However, more relevant to the purpose of the study was the interaction effect between time and alcohol change group, which was also statistically significant, F(4, 370) = 2.650, p = .033, partial η2 = .028. This indicates that cannabis use over time was contingent on alcohol change group membership (Figure 2). Importantly, although there was some increase in cannabis use in the AM and AI conditions, those in the AD condition significantly increased their cannabis use over the duration of the alcohol IID and further increased it after the removal of the device. Further, pairwise comparisons of alcohol change groups showed that the AD condition demonstrated significant mean differences from both the AM group (p = .029) and the AI group (p = .006) (Table 3).
Figure 2.
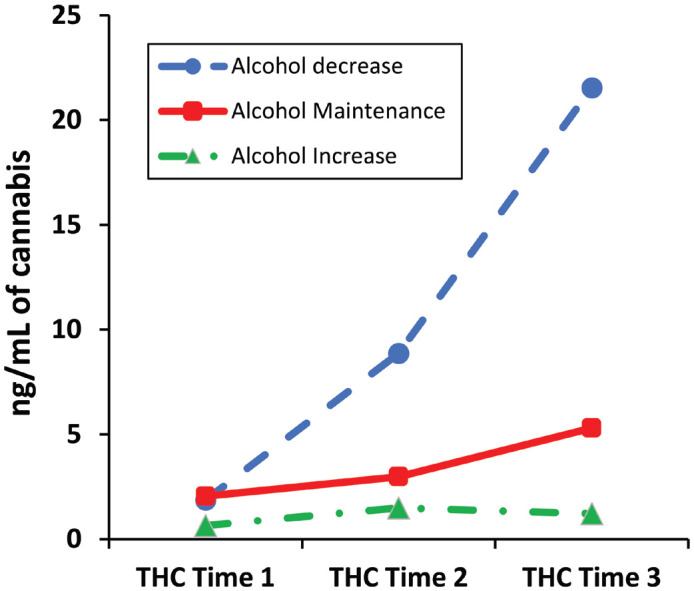
Log-adjusted blood tetrahydrocannabinol (THC) levels over time by alcohol use group in a sample of drivers with alcohol ignition interlock devices on their vehicles (N = 189)
Table 3.
Pairwise comparisons mean levels of ng/ml of tetrahydrocannabinol in blood among alcohol change groups in a sample of drivers with alcohol ignition interlock devices (N = 189)
| Referent group | Comparison group | M difference | SE | p |
|---|---|---|---|---|
| Alcohol decrease | Alcohol maintenance | 7.319 | 3.321 | .029 |
| Alcohol increase | 9.639 | 3.481 | .006 | |
| Alcohol maintenance | Alcohol decrease | −7.319 | 3.321 | .029 |
| Alcohol increase | 2.320 | 3.024 | .444 | |
| Alcohol increase | Alcohol decrease | −9.639 | 3.481 | .006 |
| Alcohol maintenance | −2.320 | 3.024 | .444 |
Discussion
The current study seeks to understand how adaptation to the alcohol IID may affect cannabis use both following installation of the alcohol IID on a driver's vehicle and after the device was removed. This study has several findings of importance to understanding the role of driver adaptation to alcohol IIDs. First, of note, the data suggest that the majority of participants maintained levels of alcohol use throughout the course of the study (i.e., AM group). Although the AM drivers did increase their use of cannabis over time, the increase was not statistically significant. This suggests that the majority of drivers adapted to the alcohol IID through other means. Such behavioral changes during alcohol IID may indicate that drivers adapted by changing when they drank or when they drove to prevent the two from overlapping. This is also consistent with prior studies which found that, in aggregate, drivers do not change drinking behaviors as a result of installing the alcohol IID (Marques et al., 1999, 2010; Vanlaar et al., 2017). Because the purpose of the alcohol IID is to prevent alcohol-impaired driving—and not to prevent alcohol use—those that adapt their behaviors while the IID is installed to prevent driving after drinking could be said to be successfully adapting to the device.
Cannabis use during and after IID installation
However, perhaps the central finding of the current study is that for a select subgroup of drivers—namely, those who decreased their alcohol use after installing the alcohol IID—there was a significant increase in cannabis use. In addition, this significant increase in cannabis use was not only retained after removal of the device but, in fact, increased. This is particularly concerning, as prior work with this study sample demonstrated that alcohol levels after device removal reverted to pre-IID levels (Voas et al., 2021). This may create a transfer of risk from alcohol-impaired driving behaviors before the IID installation, to cannabis-impaired driving behaviors while the device is installed, and then potentially to polysubstance-impaired driving following its removal.
The current study cannot establish whether the IID was responsible for the substitution of cannabis for alcohol, as additional information would be needed. However, an increase in the use of cannabis while individuals participated in required alcohol treatment settings is consistent with prior research on substance substitution (Alter et al., 2006; Reiman, 2009). This phenomenon has been found to be either a temporary or long-term replacement throughout the duration of treatment. In some cases, policies designed to limit the availability of alcohol to users have had the unintended consequence of substance substitution. Further, those who substituted cannabis for alcohol during treatment increased the hazard of alcohol relapse and decreased the likelihood of stable abstinence posttreatment (Aharonovich et al. 2005). This demonstrates the need to examine the role of cannabis substitution for alcohol in places where cannabis is recreationally available and in situations where alcohol use is restricted or otherwise prohibited—as may be the case when a driver is convicted of a DUI. Future research should target the potential for substance substitution in IID populations.
These findings should not be interpreted to undermine the utility of alcohol IIDs. Prior research has consistently found that alcohol is a greater contributor to fatal and nonfatal crashes than drugs (Hels et al., 2011; Romano & Voas, 2011; Romano et al., 2014), and alcohol IIDs have consistently been found to prevent drinking-and-driving–related behaviors while they are installed on the vehicle (e.g., Elder, 2011; Voas et al., 2021; Willis et al., 2004). Preventing drinking and driving clearly has significant public health implications. However, what this study does show is that interventions designed to reduce or eliminate episodes of impaired driving are not as straightforward as they might appear. Indeed, it appears alcohol IIDs may contribute to an unintended side effect similar to what can be seen in other alcohol treatment modalities—namely the transfer of risk from alcohol to cannabis use (or perhaps even other substance use). Further, this risk may be compounded after the removal of the device as alcohol levels revert to pre-IID levels of use, but the rate of cannabis use continues to increase. This may indicate an increase in rates of polysubstance use post-IID relative to pre-IID.
This may outline a need to expand on the alcohol IID programmatic requirements. Specifically, the current study indicates there is a need to enhance treatments to include psychoeducational or clinical components targeting the propensity to substitute another substance simply to avoid detection. Many states currently use impaired driving task forces that consider the potential for intervention with drivers on IID. Such committees could identify drivers at risk for substance substitution during the IID and mandate additional treatment to curtail its adverse effects on future driving-related outcomes. Findings from the study also outline the need for future research to develop comprehensive criteria on which drivers are likely to substitute substances while on the IID, and outline potential intervention strategies to use with them. Indeed, prior research has found that interventions coupled with IIDs have demonstrated reduced rates of recidivism after device removal relative to those without interventions (Voas et al., 2016; Zador et al., 2011); however, such work has not yet included the potential for substance substitution. Identification of drivers in the different alcohol–cannabis use paths (early in the IID process) should allow early interventions to prevent drivers from developing risky trajectories, perhaps even allowing them to sustain the IID benefits after the device removal.
The current study has some limitations that must be considered for proper interpretation of the findings. First, similar to the Scherer et al. (2020) study, the difference in construct measurement of the blood and alcohol instruments is not ideal. Specifically, the duration in which cannabis was identified in the blood samples was relatively brief, whereas the hair EtG used to assess alcohol use reflects up to 3 months. Ideally, these two measures would be commensurate. However, as the detectable range in blood is so limited, we might expect this to work against the hypothesis in the current study by making cannabis use difficult to assess. Despite this mismatch, the current study still found significant relationships. Further, although the findings of the current study are consistent with what we would expect to see if participants were indeed substituting cannabis for alcohol use, additional research is needed before a definitive statement to this effect can be made. Finally, we examined only cannabis use and alcohol use; although prior research has indicated worse driving-related outcomes for other substances, the occurrence of those substances in the current sample was too low to permit meaningful assessment. Future research should seek to identify similar relationships with other substances—particularly opioids and benzodiazepines, which have been identified as contributing to crash risk (Scherer et al., 2018).
Summary
The current study builds on previous work by Scherer et al. (2020), which outlined the potential for cannabis use in a smaller sample of drivers from the MHD study but was limited in its ability to follow drivers after removal of the device. The current study supports that cannabis use both during and after IID removal could be an unintended adverse outcome for a relatively specific subsample of drivers. Although alcohol IIDs are still powerful tools in preventing adverse alcohol-related outcomes, they should be coupled with comprehensive interventions designed to identify and curtail unintended adverse outcomes associated with their installation.
Conflict-of-Interest Statement
The authors have no conflicts of interest.
Footnotes
The research and preparation of this article were conducted under National Institute on Alcohol Abuse and Alcohol Grant R01 AA022312. Points of view or opinions in this document are those of the authors and do not necessarily represent the official position or policies of the National Institutes of Health.
References
- Aharonovich E., Liu X., Samet S., Nunes E., Waxman R., Hasin D. Postdischarge cannabis use and its relationship to cocaine, alcohol, and heroin use: A prospective study. American Journal of Psychiatry. 2005;162:1507–1514. doi: 10.1176/appi.ajp.162.8.1507. doi:10.1176/appi.ajp.162.8.1507. [DOI] [PubMed] [Google Scholar]
- Alter R. J., Lohrmann D. K., Greene R. Substitution of marijuana for alcohol: The role of perceived access and harm. Journal of Drug Education. 2006;36:335–355. doi: 10.2190/2780-G96W-J17N-R3H1. doi:10.2190/2780-G96W-J17N-R3H1. [DOI] [PubMed] [Google Scholar]
- Biondi A., Freni F., Carelli C., Moretti M., Morini L. Ethyl glucuronide hair testing: A review. Forensic Science International. 2019;300:106–119. doi: 10.1016/j.forsciint.2019.05.004. doi10.1016/j.forsciint.2019.05.004. [DOI] [PubMed] [Google Scholar]
- Elder R. W., Voas R., Beirness D., Shults R. A., Sleet D. A., Nichols J. L., Compton R. Effectiveness of ignition interlocks for preventing alcohol-impaired driving and alcohol-related crashes: A Community Guide systematic review. American Journal of Preventive Medicine. 2011;40:362–376. doi: 10.1016/j.amepre.2010.11.012. doi:10.1016/j.amepre.2010.11.012. [DOI] [PubMed] [Google Scholar]
- Greene K. M. Perceptions of driving after marijuana use compared to alcohol use among rural American young adults. Drug and Alcohol Review. 2018;37:637–644. doi: 10.1111/dar.12686. doi:10.1111/dar.12686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hels T., Bernhoft I. M., Lyckegaard A., Houwing S., Hagenzieker M., Legrand S.-A., Verstraete A. Risk of injury by driving with alcohol and other drugs (Project No TREN-05-FP6TR-S07.61320-518404-DRUID. 2011. http://orbit.dtu.dk/ws/files/6341143/prod11323338408067.Deliverable_2_3_5.pdf Retrieved from.
- Kelley-Baker T., Berning A., Ramirez A., Lacey J. H., Carr K., Waehrer G., Compton R. Washington, DC: National Highway Traffic Safety Administration; 2017. 2013-2014 National Roadside Study of alcohol and drug use by drivers: Drug results (DOT HS 812 411) [Google Scholar]
- Lacey J. H., Kelley-Baker T., Furr-Holden C. D. M., Voas R. B., Romano E., Ramirez A., Berning A. Washington, DC: Department U.S. of Transportation, National Highway Traffic Safety Administration; 2009. 2007 National Roadside Survey of Alcohol and Drug Use by Drivers: Drug results (DOT HS 811 249)https://www.nhtsa.gov/sites/nhtsa.gov/files/documents/811249.pdf Retrieved from. [Google Scholar]
- Leandra's Law. New York Vehicle Traffic Law Section 1192 2-a(b. 2009 https://www.nysenate.gov/legislation/laws/VAT/1192 . [Google Scholar]
- Li G. Relative and attributable risks of fatal crashes associated with drug use. Injury Prevention. 2012;18(Supplement 1):A39. doi:10.1136/injuryprev-2012-040580d.4. [Google Scholar]
- Marques P. R., Tippetts A. S., Yegles M. Ethylglucuronide in hair is a top predictor of impaired driving recidivism, alcohol dependence, and a key marker of the highest BAC interlock tests. Traffic Injury Prevention. 2014;15:361–369. doi: 10.1080/15389588.2013.824569. doi:10.1080/15389588.2013.824569. [DOI] [PubMed] [Google Scholar]
- Marques P., Tippetts S., Allen J., Javors M., Alling C., Yegles M., Wurst F. Estimating driver risk using alcohol biomarkers, inter-lock blood alcohol concentration tests and psychometric assessments: Initial descriptives. Addiction. 2010;105:226–239. doi: 10.1111/j.1360-0443.2009.02738.x. doi:10.1111/j.1360-0443.2009.02738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques P. R., Voas R. B., Tippetts A. S., Beirness D. J. Behavioral monitoring of DUI offenders with the Alcohol Ignition Interlock Recorder. Addiction. 1999;94:1861–1870. doi: 10.1046/j.1360-0443.1999.9412186111.x. doi:10.1046/j.1360-0443.1999.9412186111.x. [DOI] [PubMed] [Google Scholar]
- Movig K. L., Mathijssen M. P. M., Nagel P. H. A., van Egmond T., De Gier J. J., Leufkens H. G. M., Egberts A. C. Psychoactive substance use and the risk of motor vehicle accidents. Accident Analysis and Prevention. 2004;36:631–636. doi: 10.1016/S0001-4575(03)00084-8. doi:10.1016/S0001-4575(03)00084-8. [DOI] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration. Washington, DC: Author; 2019a. Alcohol impaired driving: 2018 data. (Traffic Safety Facts Report No. DOT HS 812 864. [Google Scholar]
- National Highway Traffic Safety Administration. Washington, DC: Author; 2019b. State alcohol impaired-driving estimates: 2017 data (Traffic Safety Facts Report No. DOT HS 812 724. [Google Scholar]
- Nochajski T. H., Manning A. R., Voas R., Taylor E. P., Scherer M., Romano E. The impact of interlock installation on driving behavior and drinking behavior related to driving. Traffic Injury Prevention. 2020;21:419–424. doi: 10.1080/15389588.2020.1802020. doi:10.1080/15389588.2020.1802020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez A., Berning A., Kelley-Baker T., Lacey J. H., Yao J., Tippetts A. S., Compton R. Washington, DC: National Highway Traffic Safety Administration; 2016. 2013–2014 National Roadside Survey of alcohol and drug use by drivers: Alcohol results. (DOT HS 812 362.https://rosap.ntl.bts.gov/view/dot/2084/dot_2084_DS1.pdf? Retrieved from. [Google Scholar]
- Reiman A. Cannabis as a substitute for alcohol and other drugs. Harm Reduction Journal. 2009;6:35–40. doi: 10.1186/1477-7517-6-35. doi:10.1186/1477-7517-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocky Mountain High Intensity Drug Trafficking Area. Denver, CO: Author; 2016. Sep, The legalization of cannabis in Colorado: The impact. [Google Scholar]
- Romano E., Torres-Saavedra P., Voas R. B., Lacey J. H. Drugs and alcohol: Their relative crash risk. Journal of Studies on Alcohol and Drugs. 2014;75:56–64. doi: 10.15288/jsad.2014.75.56. doi:10.15288/jsad.2014.75.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano E., Voas R. B. Drug and alcohol involvement in four types of fatal crashes. Journal of Studies on Alcohol and Drugs. 2011;72:567–576. doi: 10.15288/jsad.2011.72.567. doi:10.15288/jsad.2011.72.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romosz A. M., Scherer M., Voas R. B., Romano E., Nochajski T. H., Taylor E. P., Manning A. R. Understanding non-installers of the ignition interlock device: A qualitative analysis. Drug and Alcohol Review. 2021;40:1083–1091. doi: 10.1111/dar.13275. doi:10.1111/dar.13275. [DOI] [PubMed] [Google Scholar]
- Scherer M., Canham S., Voas R. B., Furr-Holden C. D. Inter-correlation of alcohol and other drug use disorders among a national sample of drivers. Journal of Psychoactive Drugs. 2018;50:143–150. doi: 10.1080/02791072.2017.1366605. doi:10.1080/02791072.2017.1366605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer M., Marques P., Manning A. R., Nochajski T. H., Romano E., Taylor E., King S. Potential for cannabis adaptation among participants in a drunk driving intervention. Journal of Substance Use. 2020;25:605–609. doi: 10.1080/14659891.2020.1749950. doi:10.1080/14659891.2020.1749950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer M., Romano E., Voas R., Taylor E. Latent classes of polydrug users as a predictor of crash involvement and alcohol consumption. Journal of Studies on Alcohol and Drugs. 2018;79:481–489. doi: 10.15288/jsad.2018.79.481. doi:10.15288/jsad.2018.79.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S. New York, NY: Cambridge University Press; 2017. Substance and behavioral addictions: Concepts, causes, and cures. [Google Scholar]
- Sussman S., Black D. S. Substitute addiction: A concern for researchers and practitioners. Journal of Drug Education. 2008;38:167–180. doi: 10.2190/DE.38.2.e. doi:10.2190/DE.38.2.e. [DOI] [PubMed] [Google Scholar]
- U.S. Census. New York: 2019. Quick facts of Erie County.https://www.census.gov/quickfacts/eriecountynewyork Retrieved from. [Google Scholar]
- Vanlaar W. G., Mainegra Hing M., Robertson R. D. An evaluation of Nova Scotia's alcohol ignition interlock program. Accident Analysis and Prevention. 2017;100:44–52. doi: 10.1016/j.aap.2016.12.017. doi:10.1016/j.aap.2016.12.017. [DOI] [PubMed] [Google Scholar]
- Voas R. B. Vehicle safety features aimed at preventing alcohol-related crashes. Forensic Science Review. 2020;32:55–81. doi:10.4324/9781003030799-21. [PubMed] [Google Scholar]
- Voas R. B., Tippetts A. S., Bergen G., Grosz M., Marques P. Mandating treatment based on interlock performance: Evidence for effectiveness. Alcoholism: Clinical and Experimental Research. 2016;40:1953–1960. doi: 10.1111/acer.13149. doi:10.1111/acer.13149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voas R. B., Tippetts A. S., Romano E., Nochajski T. H., Manning A. R., Taylor E., Scherer M. Changes in alcohol use and drinking and driving outcomes from before arrest for driving under the influence to after interlock removal. Alcoholism: Clinical and Experimental Research. 2021;45:743–751. doi: 10.1111/acer.14558. doi:10.1111/acer.14558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadsworth E., Hammond D. International differences in patterns of cannabis use among youth: Prevalence, perceptions of harm, and driving under the influence in Canada. England & United States. Addictive Behaviors. 2019;90:171–175. doi: 10.1016/j.addbeh.2018.10.050. doi:10.1016/j.addbeh.2018.10.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickens C. M., Watson T. M., Mann R. E., Brands B. Exploring perceptions among people who drive after cannabis use: Collision risk, comparative optimism and normative influence. Drug and Alcohol Review. 2019;38:443–451. doi: 10.1111/dar.12923. doi:10.1111/dar.12923. [DOI] [PubMed] [Google Scholar]
- Willis C., Lybrand S., Bellamy N. Alcohol ignition interlock programmes for reducing drink driving recidivism. Cochrane Database of Systematic Reviews. 2004;18(4):CD004168. doi: 10.1002/14651858.CD004168.pub2. doi:10.1002/14651858.CD004168.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson F. A., Stimpson J. P., Pagán J. A. Fatal crashes from drivers testing positive for drugs in the U.S., 1993-2010. Public Health Reports. 2014;129:342–350. doi: 10.1177/003335491412900409. doi:10.1177/003335491412900409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zador P. L., Howard J. M., Rauch W. J., Ahlin E. M., Duncan G. D. Latency periods between alcohol-related traffic violations: Implications for recidivism. Traffic Injury Prevention. 2011;12:297–305. doi: 10.1080/15389588.2011.568554. doi:10.1080/15389588.2011.568554. [DOI] [PubMed] [Google Scholar]