Abstract
Aspects of poor body acceptance (BA), such as internalized weight bias and dissatisfaction with one’s shape and size, are the strongest predictors of disordered eating and are associated with reduced engagement in healthy behaviors. Perceiving oneself as having a family history of overweight (PFH) could boost BA by increasing attributions for inherited, biological causes of weight. A community sample of 289 women who were overweight from the Washington, DC metropolitan area who were dissatisfied with their current weight (68% Black; 32% White) enrolled in in this study in 2012. PFH of overweight was associated with decreased internalized weight bias among white women and marginally increased body shape satisfaction generally. The relationship between PFH and BA was not explained by biological attributions for weight. Perceptions that overweight runs in one’s family can be protective with respect to BA. This is suggestive of the potential benefit of integrating family-based approaches into weight management interventions.
Keywords: Body Acceptance, Weight Bias Internalization, Race, Family History of Overweight, Biological Attributions for Weight
Introduction
Overweight and obesity are considered major public health issues in the United States. Despite the fact that over 60% of the population is overweight (Flegal, et al. 2012), stigma toward persons who are obese has not lessened. Rather, recent research shows that it has become worse over the past decade, especially toward women (Andreyeva, et al. 2008). Many women who are overweight are actively trying to lose or control their weight through healthy diet and exercise (Bish, et al. 2005; Nissen and Holm 2015; Nicklas, et al. 2012). However, doing so in a dominant U.S. culture that devalues overweight people exacerbates body dissatisfaction and can inhibit attempts at successful weight loss or maintenance (Puhl, et al. 2007; Schvey, et al. 2011). Internalization of these negative views toward people who are overweight leads to reduced engagement in healthy behaviors (Puhl, et al. 2007; Hilbert, et al. 2013; Schvey, et al. 2011). Internalized weight bias, body shape dissatisfaction and body size dissatisfaction, all aspects of poor body acceptance, not only inhibit healthy weight control behaviors but are also some of the leading causes of eating disorders among women (Puhl, et al. 2007; Bacon and Aphramor 2011; Durso, et al. 2012; Hartmann, et al. 2015; Sonneville, et al. 2012). Thus, it is important to identify personal characteristics that may be associated with internalized weight bias and body shape and size dissatisfaction potentially to buffer against this negative societal context, and create a more conducive environment for improving health (Bacon and Aphramor 2011; Sonneville, et al. 2012).
The current study examined whether perceiving that overweight runs in one’s family was associated with women’s internalized weight bias, body size dissatisfaction, and body shape dissatisfaction and whether these associations varied by race. Given both the high rates of overweight in the United States and the fact that obesity is highly heritable (Wardle, et al. 2008; Farooqi and O’Rahilly 2007), the majority of women who are overweight have a family history of overweight (Semmler, et al. 2009). Recognition of this could potentially improve body acceptance by reducing self-blame or by creating more realistic expectations regarding weight loss. A primary route through which perceived family history (PFH) could improve body acceptance is through its association with the extent to which one makes biological attributions for one’s weight.
Perceived Family History and Biological Attributions for Weight
Perceiving that one has a family history of overweight (i.e., that overweight “runs in” one’s family) has important implications for the beliefs one holds about what causes or influences body weight. Indeed, when surveyed, most women who were overweight or obese recognized not only the influence of behaviors like diet and exercise on weight but also held beliefs implicating a genetic or inherited biological propensity (Gonçalves, et al. 2012; Sonntag, et al. 2010)
Attribution theory (Weiner 1985) may explain why the genetic and biological causal attributions that can accompany PFH can be protective. Attribution theory addresses whether people blame the person versus the situation for a negative outcome. Specifically, it offers that: locus of causality (internal or external), controllability (controllable or uncontrollable), and stability (stable or unstable) each influence whether one makes personal or situational attributions. In general, when people deem an event controllable, internal, and stable, they tend to attribute blame to the person. Applied to obesity stigma, researchers have focused on the role of perceived controllability on prejudice (Ebneter, et al. 2011; Ogden and Flanagan 2008). While much literature has demonstrated that controllability beliefs motivate obesity stigma (Hilbert, et al. 2008), researchers have had only limited success trying to reduce stigma by changing people’s controllability beliefs about obese others (Daníelsdóttir, et al. 2010).
Research results have suggested that ability to control weight may influence the attitudes that persons who are overweight and obese hold toward themselves. Believing that genetic, familial predisposition causes one’s overweight may help reduce self-blame and lead to more body and self-acceptance. In experiments in which individuals have received information describing genetic or biological underpinnings of overweight, reduced self-blame and more realistic weight loss expectations resulted (Conradt, et al. 2008; Meisel, et al. 2012). Rief et, al. showed that genetic consultations with patients were most successful at reducing internalized blame when the patient reported a family history of overweight (Rief, et al. 2007). Although this work examines the effect of receiving genetic information with internalized blame in a research context, it gave us reason to believe that one’s pre-existing beliefs about familial influence on weight may also play an important role in shaping body acceptance. Indeed, pre-existing beliefs could be even more influential since one’s life experience and knowledge shape them over an extended period of time.
Race and Body Acceptance
Attitudes toward overweight and body acceptance tend to vary by race in the United States, with a greater acceptance of overweight in primarily Black communities (Grabe and Hyde 2006; Webb, et al. 2013; Hebl, et al. 2009; Hebl and Turchin 2005) than primarily White ones. One explanation is that because Black women are, on average, larger than White women (Ogden, et al. 2014), they may disengage with the “thin ideal” more than White women to protect their own self-esteem (Hebl, et al. 2009). Alternatively, the mere presence of heavy social comparison targets in Black women’s neighborhoods can also buffer the negative influence of mainstream pressures to be thin (Granberg, et al. 2009). Thus, one’s racial identity may modify the extent to which one’s PFH is influential in shaping self and body acceptance. For example, if the internalization of body acceptance norms associated with Black communities has already heightened one’s body acceptance, perceiving a family history of overweight may not be as beneficial. Therefore, it is important to consider the racial/ethnic background of individuals when exploring the relationship between factors like PFH and body acceptance.
Aims of the current study
The association between PFH of overweight and aspects of body acceptance is an unexplored area. To test this, we had three specific aims. The first was to test the association of PFH with three components of body acceptance: internalized weight bias, body shape dissatisfaction, and body size dissatisfaction among women who were overweight. The second aim was to determine whether race moderated the association of PFH with any of the components of body acceptance. The third aim was to explore whether these women’s biological attributions for their own weight explained the association of PFH with body acceptance.
Methods
Participants and Procedure
A convenience sample of participants from the Washington, DC metro area who were part of a parent experimental trial (Persky and Street 2015) and a pilot test (data not published), both assessing the influence of physician communication of genomic information on weight counseling outcomes participated in this study in 2012. Prospective participants were recruited through flyers, internet postings, and word-of-mouth and then were telephone-screened to ensure that they qualified for the study. For this study, 422 women were screened for eligibility, and 347 were found eligible (eligibility rate = 75.8%). Participants were told that they were participating in a study on weight management counseling in the health care system using electronic research tools. Participants reported both their race and education during the telephone screenings. Those deemed eligible completed an online pre-test questionnaire (the data from which are used in this analysis, n = 298). Inclusion criteria for the larger study that were relevant to this analysis included being a woman 20–50 years old, having a body mass index (BMI) greater than 25 kg/m2, self-identifying as overweight, and being at least somewhat dissatisfied with one’s weight (options ranged from 1=very dissatisfied to 6=very satisfied; participants who scored, “4” or higher (somewhat satisfied) were excluded). Next, participants deemed eligible for the study visited a secure website where they indicated their consent and then completed the pre-test questionnaire (the source of the data reported here). This occurred before coming to the lab for the experimental session that was the focus of the parent study. This research protocol was approved by the relevant institutional review board.
To create clear distinctions between groups for this study, we only included women who identified as Black or White and who indicated either having or not having a family history of overweight in the current analysis. Therefore, the final sample consisted of 229 women (35% White; 65% Black/African American).
Measures
Perceived family history (PFH) of overweight. Participants answered a single item: Does overweight or obesity run in your family? Answer choices were, “yes”, “no”, and “I don’t know.” Analyses included only those answering “yes” or “no”.
Race.
Participants answered the question, “How would you describe your racial background.” Researchers coded the answers as: American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, White, or other. Analyses included only those in the “White” or “Black or African American” categories, and did not include women who indicated multiple races.
Weight bias internalization (Durso and Latner 2008).
Participants answered the 11-item Weight Bias Internalization Scale. Possible answer choices ranged from 1 (strongly disagree) to 7 (strongly agree). An example item is, “I don’t feel that I deserve to have a really fulfilling social life, as long as I’m overweight.” These items had high internal consistency (Cronbach’s α=0.88).
Body size dissatisfaction and body shape dissatisfaction (Gavin, et al. 2010).
Participants answered two questions on a scale from 1(strongly disagree) to 7(strongly agree) regarding how dissatisfied they felt with the size of their bodies and the shape of their bodies. These items had a correlation of r = 0.58, suggesting a strong relationship but also capturing distinct aspects of body acceptance; therefore, we conceptualized them as separate outcome variables.
Biological attributions for weight (Ogden and Flanagan 2008).
Participants responded on a scale ranging from 1(strongly disagree) to 5(strongly agree) regarding the extent to which they agreed or disagreed that their metabolism, hormones, and genetics caused their own body weight. Each of these three items (i.e., slow metabolism, hormones, and genetics; Cronbach’s α=0.63) were from the biological subscale of the beliefs about the causes of obesity scale, and we averaged them to create this score.
Education.
Participants answered a single item, “What is the highest grade or year of school you completed?” We dichotomized scores to distinguish those who graduated college from those who had not.
BMI.
Participants self-reported both height and weight and we calculated Body Mass Index (BMI) using the formula kg/m2.
Age.
Each participant self-reported her age.
Data Analysis
We used a multivariate analysis of covariance to estimate the association of family history and race with internalized weight bias, body shape satisfaction, and body size satisfaction. We statistically controlled for BMI, age, and education because BMI and age were associated theoretically with the independent and outcome variables, particularly for White women, and education was theoretically associated with race, the moderator, and the outcome variables. We used the overall F-score for each outcome variable to assess model fit. We conducted mediation analyses (Preacher and Hayes 2008; PROCESS, Models 4 and 7) to test whether biological attributions explained the association between PFH and internalized weight bias and PFH and body shape satisfaction. Because race moderated the association of PFH on internalized weight bias, we used a model of moderated mediation for that analysis only. The study had greater than 80% power to detect meaningful associations at the two-sided α=.05 significance level (increase in r2 by at least 0.03 in multiple regressions) between family history and internalized weight bias and body shape satisfaction while accounting for race and all other control variables, given the sample size of 229 participants. We conducted all power analyses using PASS, version 11 (http://www.ncss.com/).
Results
Of the 229 participants included in this analysis, the majority reported a family history of overweight (68.1%). Black women with a PFH of overweight comprised the largest group in the sample (45.2%); 22.8% of participants were Black women without a PFH; 26% were White women with a PFH, and 10.5% of the sample was White women without a PFH. Distribution of PFH did not vary by race (x2(1) =0.55, p>0.05). While about half of the sample (54.6%) reported having graduated college, significantly more White women had graduated college than Black women. Participants had a mean age of about 35 years and a mean BMI of about 35.0 kg/m2, meaning that the average participant would be categorized as moderately obese. While White women had significantly lower BMIs than Black women, they had significantly more internalized weight bias (Table 1). Results from the MANOVA showed that the model was a good fit for each of the outcome variables (all p-values <0.04)
Table 1.
Sample Characteristics by Participants’ Race.
| Total Sample | White Women | Black Women | |
|---|---|---|---|
| N = 229 | N = 80 | N = 149 | |
| Mean ± sd | Mean ± sd | Mean ± sd | |
|
| |||
| BMI (kg/m2)*** | 34.99 ± 7.72 | 31.76 ± 5.60 | 36.72±8.16 |
| Age (years) | 35.37± 9.53 | 35.48±10.66 | 35.32±8.91 |
| Body Shape Dissatisfaction | 4.97±1.84 | 5.24±1.68 | 4.82±1.92 |
| Body Size Dissatisfaction | 5.83±1.24 | 5.90±1.09 | 5.80±1.32 |
| Internalized Weight Bias*** | 3.71±1.29 | 4.29±1.22 | 3.39±1.22 |
| Percent | Percent | Percent | |
| College Graduate*** | 54.6% | 81.3% | 40.3% |
| Currently Employed | 73.4% | 80.0% | 69.8% |
Results from correlation analyses showed that for White Women, but not Black women, having a PFH of overweight was negatively associated with internalized weight bias. A PFH of overweight also trended toward association with higher biological attributions for weight, although this did not reach significance (Table 2).
Table 2.
Correlations of family history with biological attributions, age, BMI, and body acceptance variables.
| Mean (SD) Or % within race group | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
|
White Participants Only (N = 83)
|
||||||||
| 1. Perceived FH | 71.3% | ____ | ||||||
| 2. Biological Attribution | 3.38 (1.09) | 0.22 Ϯ | ____ | |||||
| 3. Body Shape Dissatisfaction | 2.78 (1.67) | −0.16 | −0.04 | ____ | ||||
| 4. Body Size Dissatisfaction | 2.15 (1.11) | −0.06 | −0.17 | 0.56*** | ____ | |||
| 5. Internalized Weight Bias | 4.24 (1.23) | −0.23* | −0.07 | 0.38*** | 0.56*** | ____ | ||
| 6. BMI | 31.61 (5.56) | 0.26* | −0.06 | 0.18 | 0.25* | 0.30** | ____ | |
| 7. Age | 35.08 (10.67) | 0.06 | −0.07 | 0.32** | 0.20 Ϯ | 0.21 Ϯ | 0.34** | ____ |
| 8. Education | 0.09 | 0.01 | −0.01 | 0.12 | 0.07 | −0.02 | 0.05 | |
| Black Participants Only (N = 165) | ||||||||
| 1. Perceived FH | 66.4% | ____ | ||||||
| 2. Biological Attributions | 3.38 (.88) | 0.12 | ____ | |||||
| 3. Body Shape Dissatisfaction | 3.16 (1.93) | −0.08 | −0.04 | ____ | ||||
| 4. Body Size Dissatisfaction | 2.19 (1.31) | −0.001 | −0.08 | 0.57*** | ____ | |||
| 5. Internalized Weight Bias | 3.46 (1.25) | 0.09 | −0.07 | 0.38*** | 0.29*** | ____ | ||
| 6. BMI | 36.36 (7.96) | 0.13 | −0.08 | 0.09 | 0.18* | 0.07 | ___ | |
| 7. Age | 34.97 (8.98) | −0.12 | 0.11 | 0.16* | 0.14 Ϯ | −0.08 | 0.06 | ____ |
| 8. Education | −0.03 | −0.06 | 0.15 | 0.04 | 0.03 | 0.31*** | 0.12 | |
Note: Perceived FH answers were coded as 0=no, 1=yes
p<0.10
p<0.05
p<0.01
p<0.001
The Association between PFH of overweight and Internalized Weight Bias, Body Shape Satisfaction, and Body Size Satisfaction
No significant main association was observed for PFH with internalized weight bias [F(1,222)=2.03, p>0.05, ηp2=0.009; Table 3], but significantly [F(1,222)=34.90, p<0.001, ηp2=0.136] more White women reported internalized bias than Black women. We also found a significant interaction of race with PFH such that the inverse association of PFH of overweight with internalized weight bias was significant only for White women [F(1, 222)=5.87, p=0.02, ηp2=0.026; Figure 1].
Table 3.
Estimated Marginal Means for Internalized Weight Bias, Body Shape Satisfaction, and Body Size satisfaction
| Family History M (SE), n = 189 |
No Family History M (SE), n = 86 |
Total | |
|---|---|---|---|
|
| |||
| Age (years) | |||
| White | 35.88 (1.51) a | 34.48 (1.80) a | 35.08 (10.67) |
| Black | 34.58 (.89) a | 36.78 (8.98) a | 34.97 (8.98) |
| Total | 34.56 (9.81) | 35.72 (1.27) | |
| BMI (kg/m2) | |||
| White | 32.69 (0.81)ab | 29.45 (0.62) a | 31.61 (5.56) |
| Black | 37.48 (0.87) c | 35.23 (0.98)bc | 36.36 (7.93) |
| Total | 35.19 (7.88) | 33.25 (6.96) | |
| Biological Attributions for Overweight | |||
| White | 3.43 (0.12) a | 3.28 (0.18) a | 3.43 (0.92) a |
| Black | 3.36 (0.10) ab | 2.89 (0.15) ab | 3.36 (0.96) ab |
| Total | 3.45 (0.93) | 3.45 (0.93) | 3.45 (0.93) |
| Internalized Weight Bias: * | |||
| White | 4.16 (0.17) a | 4.86 (0.26) b | 4.51 (0.16) |
| Black | 3.41 (0.12) c | 3.23(0.17) c | 3.32 (0.11) |
| Total | 3.78 (0.10) | 4.05 (0.16) | |
| Body Shape Dissatisfaction: * | |||
| White | 5.21 (0.25) ab | 5.95 (0.39) a | 5.58 (0.24) |
| Black | 4.65 (0.18) b | 4.93 (0.25) b | 4.79 (0.16) |
| Total | 4.93 (0.15) | 5.44 (0.16) | |
| Body Size Dissatisfaction: * | |||
| White | 5.94 (0.17) a | 6.21 (0.27) a | 6.07 (0.17) |
| Black | 5.73 (0.13) a | 5.76 (0.17) a | 5.75 (0.11) |
| Total | 5.83 (0.10) | 5.99 (0.16) | |
Note. Means estimates within each outcome that share subscripts do not differ significantly
indicates estimated marginal means and standard errors while controlling for age, BMI, and college education
Figure 1.
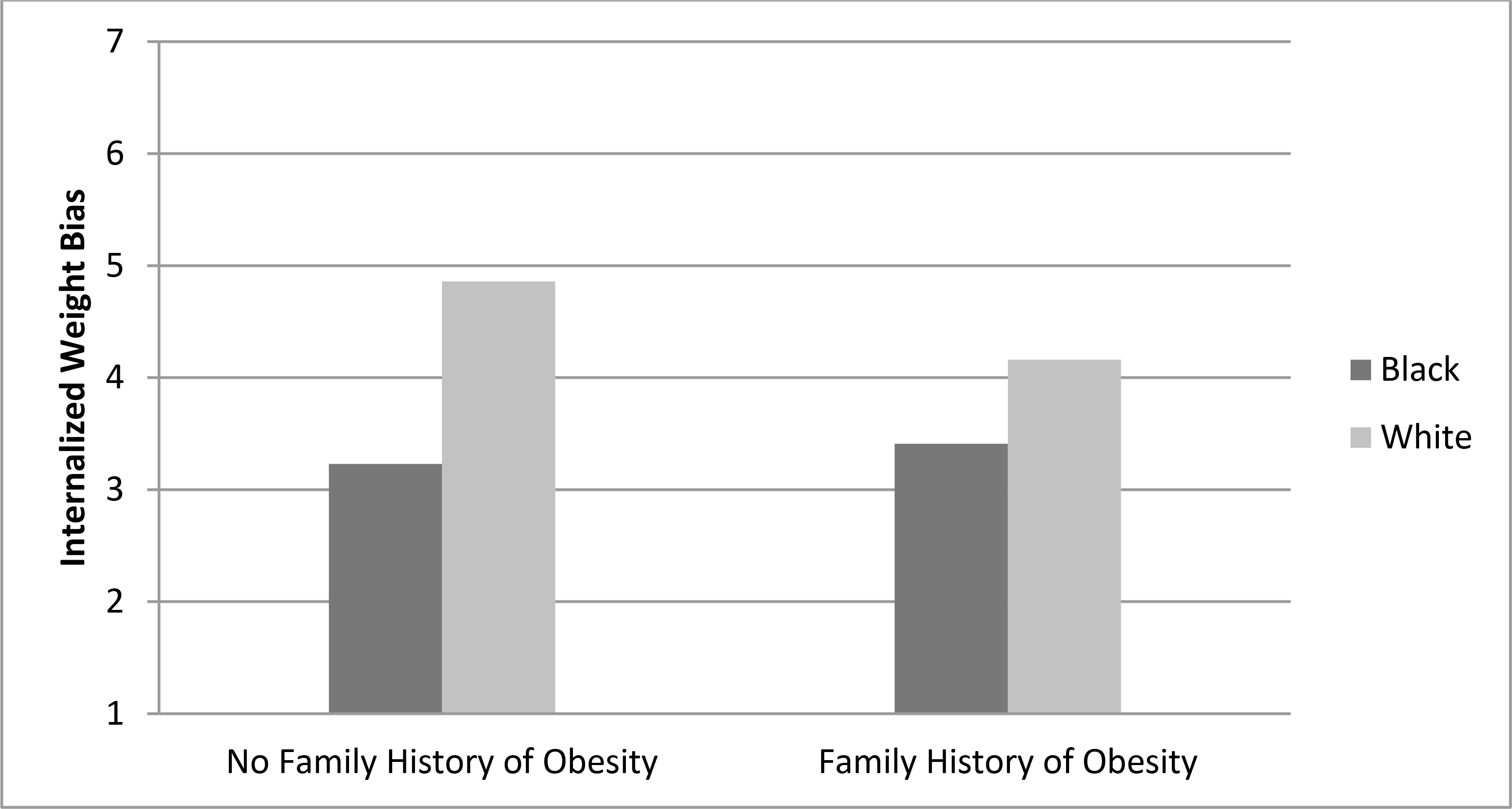
PFH of Overweight Attenuated the Internalization of Weight Bias, but Only for White Women.
Note: Higher numbers represent more weight bias internalization.
The main effect of perceived family history of overweight on body shape dissatisfaction approached, but did not reach, statistical significance such that those reporting a PFH of overweight were more satisfied with their shape than women without a PFH of overweight [F(1,222)=3.50, p=0.06, ηp2=0.016; Table 3]. A significant association was observed with race, such that White women were more dissatisfied than Black women with their body shape [F(1,222)=7.03, p=0.01, ηp2=0.031]. We found no significant interaction for PFH-by-race [F(1,222)=0.73, p>0.05]. Neither PFH, race, nor a PFH-by-race interaction were significantly associated with body size dissatisfaction (p-values>0.05).
Biological Attributions and the Association of PFH on Internalized Weight Bias
Bootstrapping results revealed no significant conditional indirect association of PFH with internalized weight bias via biological attributions for White women (Estimate of indirect effect=−0.03, 95% CI=−0.16, 0.05) or Black women (Estimate of indirect effect=−0.02, 95% CI=−0.11, 0.03). The indirect association of PFH with internalized weight through biological attributions was not different for White versus Black women (Index=0.01, 95% CI=−0.03, 13).
No significant indirect association was observed of PFH with body shape dissatisfaction due to biological attributions (Estimate of indirect effect=0.03, 95% CI=−0.04, 0.18). Because no significant relationship between PFH and body size dissatisfaction was observed, we did not test for mediation.
Discussion
The current sample consisted of women who were overweight and obese and at least somewhat dissatisfied with their bodies. This sample is reflective of many women who are overweight in the United States who are already motivated and trying to enact healthy weight control behaviors. This is a particularly important segment of the population on which to focus with respect to reducing internalized weight bias and body dissatisfaction, as these aspects of poor BA can undermine these healthy efforts (Schvey, et al. 2011; Vartanian and Smyth 2013; Puhl, et al. 2007) or cause eating disorders (e.g., Phelps, et al. 1999; Polivy and Herman 2002; Sonneville, et al. 2012).
Our results showed that, overall, the association of perceiving a family history of overweight with body acceptance was quite variable, depending upon the specific indicator under consideration. For internalized weight bias, this relationship differed by race. PFH did not make a significant difference for Black women, but was protective for White women. This may be because Black women already had lower levels of internalized weight bias and may have less room for improvement due to the influence of PFH. This is consistent with work by (Granberg, et al. 2009) showing that Black women who are overweight tend already to have relatively positive feelings about their bodies and may already have positive overweight role models. White women, on the other hand, may not have these resources.
Women reporting a PFH of overweight also reported less body shape dissatisfaction, although this association did not reach statistical significance. This occurred regardless of race, though similar to internalized weight bias, the mean differences appeared larger for White women than Black women. We found no difference in body size dissatisfaction based on women’s PFH. Because only women at least somewhat dissatisfied with their weight were eligible for the study, this was likely a more conservative estimate of the relationship between PFH and body dissatisfaction than one would find in the general population. This may also have contributed to the non-significant association between PFH and body shape satisfaction. Future studies should test this association among a sample that includes women who are satisfied and dissatisfied with their size and shape.
We found a strong main effect for race such that Black women had less internalized weight bias and less body shape dissatisfaction, despite having higher BMIs on average than the White women in the study. Research has shown this association previously (Kronenfeld, et al. 2010). However, no significant main effect of race was observed for body size dissatisfaction. A few possible explanations exist for this finding. As mentioned previously, we had a truncated range in body size dissatisfaction scores because women had to be at least somewhat dissatisfied to join the study. Another possible explanation is based on a meta-analysis showing that Black-White differences in body image have diminished over time among women on weight-related measures of body image but increased over time on global measures of body image (Roberts, et al. 2006). Internalized weight bias and even body shape dissatisfaction, but not body size dissatisfaction, incorporate other evaluative aspects of the body and the self besides just weight. Thus, this may explain why the current study results showed significant racial differences in internalized weight bias and body shape dissatisfaction but not in body size dissatisfaction. In future studies, it could be useful to explore whether these results generalize to other racial and ethnic groups. For example, some evidence has indicated that Latina women are just as much, if not more, accepting of larger frames than Black women, though findings are mixed (Grabe and Hyde 2006).
We had anticipated that the association of PFH with body acceptance would be explained primarily by the accompanying genetic and biological attributions that women would make for their weight; however, the findings did not support this hypothesis. Given that the association of PFH with body acceptance did not appear to occur due to differences in biological attributions for weight, it stands to reason that the strongest route of influence may be through social mechanisms. PFH as a concept captures not only a shared, inherited biological predisposition, but also the shared family environment. Presumably, someone who reports having a family history of overweight does so based on having other heavy family members, many of whom have likely surrounded the individual as an integral part of her social context. Thus, the family may be important not just because of shared biology, but because of familial social and environmental influences – such as providing social comparison targets, social support, or norms with respect to larger body shapes and sizes.
Strengths and limitations
The current study is the first of which we are aware to test the association of women’s pre-existing PFH with body acceptance. We focused on previously held beliefs, which are likely based on a lifetime of experiences, making them particularly likely to be influential on real-world attitudes and behaviors. We did not have the data to parse out, post-hoc, whether and which aspects of familial, social influence might explain the association of PFH with body acceptance. This limited our ability to draw firm conclusions as to the mechanisms through which PFH operates. The cross-sectional design of this study limited the ability to assess temporal and thus potentially causal relationships.
The sample also included only women who were overweight and who reported dissatisfaction with their weight. Thus, this is a biased sample and generalizability of these results is limited. For example, not all women who are overweight are dissatisfied with their bodies. Given the benefits of BA on physical and psychological health regardless of weight (Robison 2005; Bacon and Aphramor 2011), future research should examine other protective factors to body image. Further, not all women with body dissatisfaction are overweight. It would be interesting to examine the role of PFH and race on BA in women who are not overweight.
Furthermore, the two body satisfaction measures were each single items, which limited our ability to capture the construct of body image fully. However, by using body shape satisfaction, body size satisfaction, and weight bias internalization, we conceptualized body acceptance in multiple ways and were able to show that each of these conceptualizations performed differently from the others.
Another limitation was the unequal distributions in terms of racial and family history groups in our sample. Our unequal cell means may explain the marginal main effect and non-significant interaction effect for body shape satisfaction (e.g., only 23 white women did not have a family history). However, given that overweight typically runs in families, this distribution is representative of the population and our large sample of Black women allowed us to test a moderating role of race.
Conclusions
The current study was exploratory in nature, but results suggested a relationship between PFH and internalized weight bias and signs of a potential relationship with body shape dissatisfaction as well. Results also showed that this association was not due to differences in women’s biological attributions for weight, but rather was likely to relate to differences in the familial social environment. This suggests the intriguing possibility of a benefit to family-focused interventions for improving body acceptance among overweight females. Family-based interventions are often used in the area of childhood obesity (Sung-Chan, et al. 2013), but researchers have not considered them in the context of body image and self-acceptance. Focusing on improving body image, rather than just BMI, is an important outcome rarely addressed in the obesity literature. Poor body image and internalized weight bias not only fail to motivate healthy weight control behaviors, but they are related to larger weight gain over time (Neumark-Sztainer 2012) and disordered eating (e.g., Phelps, et al. 1999). In addition, the integration of other interventions to bolster body acceptance into weight management programs may be particularly needed for White women without a PFH of overweight, as these women are less likely to have social or familial structures in place that help them cope with negative societal attitudes about overweight.
Contributor Information
Miriam H. Eisenberg, Health Behaviors Branch, Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Rockville, Maryland, USA.
Richard L. Street, Jr, Department of Communication, Texas A&M University, College Station, Texas, USA.; Section of Health Services Research, Department of Medicine, Houston Center for Quality of Care and Utilization Studies, Baylor College of Medicine, Houston, Texas, USA.
Susan Persky, Social and Behavioral Research Branch, National Human Genome Research Institute, National Institutes of Health, Bethesda, Maryland, USA..
References:
- Andreyeva T, Puhl RM, and Brownell KD. 2008. Changes in Perceived Weight Discrimination among Americans, 1995–1996 through 2004–2006. Obesity 16: 1129–34. [DOI] [PubMed] [Google Scholar]
- Bacon L, and Aphramor L. 2011. Weight Science: Evaluating the Evidence for a Paradigm Shift. Nutrition Journal 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bish CL, Blanck HM, Serdula MK, Marcus M, Kohl Iii HW, and Khan LK. 2005. Diet and Physical Activity Behaviors among Americans Trying to Lose Weight: 2000 Behavioral Risk Factor Surveillance System. Obesity Research 13: 596–607. [DOI] [PubMed] [Google Scholar]
- Conradt M, Dierk JM, Schlumberger P, Rauh E, Hebebrand J, and Rief W. 2008. Who Copes Well? Obesity-Related Coping and Its Associations with Shame, Guilt, and Weight Loss. Journal of Clinical Psychology 64: 1129–44. [DOI] [PubMed] [Google Scholar]
- Daníelsdóttir S, O’Brien KS, and Ciao A. 2010. Anti-Fat Prejudice Reduction: A Review of Published Studies. Obesity Facts 3: 47–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durso LE, and Latner JD. 2008. Understanding Self-Directed Stigma: Development of the Weight Bias Internalization Scale. Obesity 16: S80–S86. [DOI] [PubMed] [Google Scholar]
- Durso LE, Latner JD, White MA, Masheb RM, Blomquist KK, Morgan PT, and Grilo CM. 2012. Internalized Weight Bias in Obese Patients with Binge Eating Disorder: Associations with Eating Disturbances and Psychological Functioning. International Journal of Eating Disorders 45: 423–27. 10.1002/eat.20933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebneter DS, Latner JD, and O’Brien KS. 2011. Just World Beliefs, Causal Beliefs, and Acquaintance: Associations with Stigma toward Eating Disorders and Obesity. Personality and Individual Differences 51: 618–22. [Google Scholar]
- Farooqi IS, and O’Rahilly S. 2007. Genetic Factors in Human Obesity. Obesity Reviews 8: 37–40. 10.1111/j.1467-789X.2007.00315.x [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll D, Kit BK, and Ogden CL. 2012. Prevalence of Obesity and Trends in the Distribution of Body Mass Index among Us Adults, 1999–2010. JAMA - Journal of the American Medical Association 307: 491–97. [DOI] [PubMed] [Google Scholar]
- Gavin AR, Simon GE, and Ludman EJ. 2010. The Association between Obesity, Depression, and Educational Attainment in Women: The Mediating Role of Body Image Dissatisfaction. Journal of Psychosomatic Research 69: 573–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonçalves H, González DA, Araújo CP, Muniz L, Tavares P, Assunção MC, Menezes AMB, and Hallal PC. 2012. Adolescents’ Perception of Causes of Obesity: Unhealthy Lifestyles or Heritage? Journal of Adolescent Health 51: S46–S52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabe S, and Hyde JS. 2006. Ethnicity and Body Dissatisfaction among Women in the United States: A Meta-Analysis. Psychological Bulletin 132: 622–40. [DOI] [PubMed] [Google Scholar]
- Granberg EM, Simons LG, and Simons RL. 2009. Body Size and Social Self-Image among Adolescent African American Girls: The Moderating Influence of Family Racial Socialization. Youth and Society 41: 256–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann AS, Thomas JJ, Greenberg JL, Rosenfield EH, and Wilhelm S. 2015. Accept, Distract, or Reframe? An Exploratory Experimental Comparison of Strategies for Coping with Intrusive Body Image Thoughts in Anorexia Nervosa and Body Dysmorphic Disorder. Psychiatry Res 225: 643–50. 10.1016/j.psychres.2014.11.031 [DOI] [PubMed] [Google Scholar]
- Hebl MR, King EB, and Perkins A. 2009. Ethnic Differences in the Stigma of Obesity: Identification and Engagement with a Thin Ideal. Journal of Experimental Social Psychology 45: 1165–72. 10.1016/j.jesp.2009.04.017 [DOI] [Google Scholar]
- Hebl MR, and Turchin JM. 2005. The Stigma of Obesity: What About Men? Basic and Applied Social Psychology 27: 267–75. 10.1207/s15324834basp2703_8 [DOI] [Google Scholar]
- Hilbert A, Braehler E, Haeuser W, and Zenger M. 2013. Weight Bias Internalization, Core Self-Evaluation, and Health in Overweight and Obese Persons. Obesity (Silver Spring). 10.1002/oby.20561 [DOI] [PubMed] [Google Scholar]
- Hilbert A, Rief W, and Braehler E. 2008. Stigmatizing Attitudes toward Obesity in a Representative Population-Based Sample. Obesity 16: 1529–34. [DOI] [PubMed] [Google Scholar]
- Kronenfeld LW, Reba-Harrelson L, Von Holle A, Reyes ML, and Bulik CM. 2010. Ethnic and Racial Differences in Body Size Perception and Satisfaction. Body Image 7: 131–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisel SF, Walker C, and Wardle J. 2012. Psychological Responses to Genetic Testing for Weight Gain: A Vignette Study. Obesity 20: 540–46. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D 2012. Integrating Messages from the Eating Disorders Field into Obesity Prevention. Adolescent Medicine: State of the Art Reviews 23: 529–43. [PubMed] [Google Scholar]
- Nicklas JM, Huskey KW, Davis RB, and Wee CC. 2012. Successful Weight Loss among Obese U.S. Adults. Am J Prev Med 42: 481–5. 10.1016/j.amepre.2012.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nissen NK, and Holm L. 2015. Literature Review: Perceptions and Management of Body Size among Normal Weight and Moderately Overweight People. Obes Rev 16: 150–60. 10.1111/obr.12231 [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, and Flegal KM. 2014. Prevalence of Childhood and Adult Obesity in the United States, 2011–2012. JAMA 311: 806–14. 10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden J, and Flanagan Z. 2008. Beliefs About the Causes and Solutions to Obesity: A Comparison of Gps and Lay People. Patient Education and Counseling 71: 72–78. [DOI] [PubMed] [Google Scholar]
- Persky S, and Street R Jr. 2015. Evaluating Approaches for Communication About Genomic Influences on Body Weight. Annals of Behavioral Medicine 1–10. 10.1007/s12160-015-9701-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelps L, Johnston LS, and Augustyniak K. 1999. Prevention of Eating Disorders: Identification of Predictor Variables. Eating Disorders 7: 99–108. 10.1080/10640269908251189 [DOI] [Google Scholar]
- Polivy J, and Herman CP. 2002. Causes of Eating Disorders. Annual Review of Psychology 53: 187–213. doi: 10.1146/annurev.psych.53.100901.135103 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, and Hayes AF. “Contemporary Approaches to Assessing Mediation in Communication Research.” In The Sage Sourcebook of Advanced Data Analysis Methods for Communication Research, edited by Hayes AF, Slater MD and Snyder LB, 13–54. Thousan Oaks, CA: Sage Publications, 2008. [Google Scholar]
- Puhl RM, Moss-Racusin CA, and Schwartz MB. 2007. Internalization of Weight Bias: Implications for Binge Eating and Emotional Well-Being. Obesity 15: 19–23. [DOI] [PubMed] [Google Scholar]
- Rief W, Conradt M, Dierk JM, Rauh E, Schlumberger P, Hinney A, and Hebebrand J. 2007. Is Information on Genetic Determinants of Obesity Helpful or Harmful for Obese People? - a Randomized Clinical Trial. Journal of General Internal Medicine 22: 1553–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts A, Cash TF, Feingold A, and Johnson BT. 2006. Are Black-White Differences in Females’ Body Dissatisfaction Decreasing? A Meta-Analytic Review. Journal of Consulting and Clinical Psychology 74: 1121–31. [DOI] [PubMed] [Google Scholar]
- Robison J 2005. Health at Every Size: Toward a New Paradigm of Weight and Health. Medscape General Medicine 7: 13–13. [PMC free article] [PubMed] [Google Scholar]
- Schvey NA, Puhl RM, and Brownell KD. 2011. The Impact of Weight Stigma on Caloric Consumption. Obesity 19: 1957–62. [DOI] [PubMed] [Google Scholar]
- Semmler C, Ashcroft J, Van Jaarsveld CHM, Carnell S, and Wardle J. 2009. Development of Overweight in Children in Relation to Parental Weight and Socioeconomic Status. Obesity 17: 814–20. [DOI] [PubMed] [Google Scholar]
- Sonneville KR, Calzo JP, Horton NJ, Haines J, Austin SB, and Field AE. 2012. Body Satisfaction, Weight Gain and Binge Eating among Overweight Adolescent Girls. International Journal of Obesity 36: 944–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonntag U, Esch T, von Hagen L, Renneberg B, Braun V, and Heintze C. 2010. Locus of Control, Self-Efficacy and Attribution Tendencies in Obese Patients - Implications for Primary Care Consultations. Medical Science Monitor 16: 330–35. [PubMed] [Google Scholar]
- Sung-Chan P, Sung YW, Zhao X, and Brownson RC. 2013. Family-Based Models for Childhood-Obesity Intervention: A Systematic Review of Randomized Controlled Trials. Obesity Reviews 14: 265–78. [DOI] [PubMed] [Google Scholar]
- Vartanian LR, and Smyth JM. 2013. Primum Non Nocere: Obesity Stigma and Public Health. Journal of Bioethical Inquiry 10: 49–57. [DOI] [PubMed] [Google Scholar]
- Wardle J, Carnell S, Haworth CMA, and Plomin R. 2008. Evidence for a Strong Genetic Influence on Childhood Adiposity Despite the Force of the Obesogenic Environment. American Journal of Clinical Nutrition 87: 398–404. [DOI] [PubMed] [Google Scholar]
- Webb JB, Warren-Findlow J, Chou YY, and Adams L. 2013. Do You See What I See?: An Exploration of Inter-Ethnic Ideal Body Size Comparisons among College Women. Body Image 10: 369–79. [DOI] [PubMed] [Google Scholar]
- Weiner B 1985. An Attributional Theory of Achievement Motivation and Emotion. Psychological Review 92: 548–73. [PubMed] [Google Scholar]


