Abstract
Listeria monocytogenes (Lm) is a ubiquitous foodborne pathogen comprising of 14 serotypes, of which serovar 4h isolates belonging to hybrid sub-lineage Ⅱ exhibit hypervirulent features. LMxysn_1693 of serovar 4h Lm XYSN, a member of genomic island-7 (GI-7), is predicted to a membrane protein with unknown function, which is conserved in serovar 4h Listeria monocytogenes. Under bile salts stress, Lm XYSN strain lacking LMxysn_1693 (XYSN∆1693) exhibited a stationary phase growth defect as well as a reduction in biofilm formation and strikingly down-regulated bile-salts-resistant genes and virulent genes. Particularly, LMxysn_1693 protein plays a crucial role in Lm XYSN adhesion and invasion to intestinal epithelial cells, as well as colonization in the ileum of mice. Taken together, these findings indicate that the LMxysn_1693 gene encodes a component of the putative ABC transporter system, synthetically interacts with genes involved in bile resistance, biofilm formation and virulence, and thus contributes to Listeria monocytogenes survival within and outside the host.
Keywords: Listeria monocytogenes, bile salt, virulence, biofilm, ABC transporter, genomic island
1. Introduction
Listeria monocytogenes (Lm) is ubiquitously distributed in diverse environments, which can survive in extreme conditions at a low temperature −0.4 °C–45 °C [1], wide pH range (4.5–9.0) and high concentration of 10% NaCl [2]. Lm is a facultative intracellular pathogen that is responsible for gastroenteritis, meningitis and maternofetal infections [3], and the mortality rate reaches up to 20% to 30% [4]. It is presently assumed that foodborne outbreaks are increasingly caused by hypervirulent complex clones (CCs) such as CC1, CC2, CC4, and CC6 with high clinical frequency [5]. CC33, consisting of hybrid sub-lineage Ⅱ (HSL-Ⅱ) hypervirulent isolates, is an emerging complex clone with 200–400 folds higher virulence than Lm EGD-e via oral infection [6], which is highly susceptible to wild-type mice. While early work suggested that 108–1010 CFU were normally needed to establish intestinal infection in mice, it was shown that the oral infectious dose of CC33 isolates was 105 CFU, which suggested that their unique virulence genes were involved in breaking through the intestinal barrier and responsible for making mice a susceptible host.
Multiple Listeria genes associated with resisting heat (dnaK, groES, clpC, clpP and clpE), cold (cspA, cspB and cspD) and acid (sigB) contribute to its survival in harsh environmental conditions [7]. Once Lm enters the gastrointestinal tract, bacteria cells face several threats, such as trypsin, stomach acid, bile salts and inflammatory responses. Moreover, some genes are related to the resistance of acidic environment in Lm, including the glutamate decarboxylase system (GAD) [8], the F0F1-ATPase system [9] and Sigma B (SigB) [10]. Additionally, the bsh gene, regulated by prfA and sigB, encodes the bile salt hydrolase (BSH), which is essential for bacteria to break through the gastrointestinal barrier. BSH can hydrolyze bile salts into amino acids and bile acids to protect bacteria [11]. Furthermore, BilE and bile regulatory transcription factor A (BrtA) could also enhance bile salts tolerance and colonization in the liver and gallbladder [12]. However, how hypervirulent strains resist the stress and survive in the gastrointestinal tract remains unknown.
Bacteria could obtain new phenotypic characteristics through genomic islands, which are of great significance for pathogenicity and antibiotic resistance, and even form new bacterial pathogenic subspecies. Genome islands are often closely related to horizontal gene transfer and are the basis and source for discovering and identifying novel functional islands such as new pathogenicity islands, resistance islands, metabolic islands and symbiotic islands. Kovačević et al., found that a 50 kb genomic island LGI1 carrying resistance gene to cefoxitin and nalidixic acid in three strains of 1/2a Listeria [13]. Lee et al., identified that a 4b clonal complex could resist arsenic and cadmium with a 35 kb genomic island. Moreover, metabolic islands have also been detected in other pathogenic bacteria [14]. For example, Salmonella Senftenberg could survive under glucose as the sole carbon source, mainly due to the metabolic island CTnscr94 with related genes, which is crucial for enhancing environmental adaptability [15]. Undoubtedly, CC33 isolate Lm XYSN harbor eight genomic islands essentially involved in the adaption of saprophytic and parasitic life [6]. Understanding functions of genes in the genomic islands contribute to deciphering the pathogenic mechanism from virulence to hypervirulence.
LMxysn_1693 is a member of genomic island-7 (GI-7) carrying 20 ORFs (LMxysn_1677-LMxysn_1696), and most genes of GI-7 are hypothetical proteins with unknown function. In this study, we found that LMxysn_1693 was involved in up-regulating bile resistant and virulence genes, thereby facilitating resistance to bile salts and enhancing colonization in mice. Our work paves the way to understand the role of genomic island and the hypervirulence of CC33 isolates.
2. Materials and Methods
2.1. Bacterial Strains, Cell Lines and Animals
High-virulent Lm XYSN was isolated from a case of ovine listeriosis [6]. Shuttle vector pAULA was kindly donated by Prof. Chakraborty (Justurs Liebig University, Giessen, Germany). All Lm strains were cultured in brain heart infusion (BHI; Becton Dickinson, Sparks, MD, USA). The Caco-2 BBe cell line was propagated in the Dulbecco’s modified Eagle medium (DMEM; Gibco, Waltham, MA, USA) supplemented with 10% fetal bovine serum (FBS; Gibco, Waltham, MA, USA). Six-week-old female C57BL/6 mice were purchased from Vital River Laboratory Animal Technology Co., Ltd. (Beijing, China). Animal experiments were conducted by following guidelines laid down for the welfare and ethics of experimental animals. All animals were kept at the animal biosafety facilities according to procedures approved by the Institutional Animal Ethics Committee of Yangzhou University (reference number 202205007).
2.2. Bioinformatics Analysis
IslandViewer4 (creator Brinkman lab, Burnaby, BC, Canada) was used to predictive analysis for genomic islands (https://www.pathogenomics.sfu.ca/islandviewer/resources/ (accessed on 13 November 2021)). Nucleobase sequence and amino acids of LMxysn_1693 were compared with database to search for homology gene and proteins via Blast (creator National Institutes of Health, Bethesda, MD, USA) (https://blast.ncbi.nlm.nih.gov/Blast.cgi (accessed on 15 November 2021)). The domains of proteins of GI-7 were predicted through SMART (version 9, Heidelberg, Germany) (http://smart.embl-heidelberg.de, accessed on 20 November 2021) and InterPro (version 87.0, creator European Bioinformatics Institute, Cambridge, Britain) (https://www.ebi.ac.uk/interpro/ (accessed on 20 November 2021)). Signal peptide and transmembrane structure of all proteins were analyzed using SingnalP-6.0 (https://services.healthtech.dtu.dk/service.php?SignalP-6.0 (version 6.0, creator Technical University of Denmark, Lyngby, Denmark) (accessed on 20 November 2021)) and TMHMM-2.0 (https://services.healthtech.dtu.dk/service.php?TMHMM-2.0 (version 2.0, creator Technical University of Denmark, Lyngby, Denmark) (accessed on 20 November 2021)), respectively. Amino acid sequence of LMxysn_1693 protein was submitted to the SWISS-MODEL (creator SIB Swiss Institute of Bioinformatics and the Biozentrum of the University, Basel, Switzerland) to obtain the hypothetical 3D structure (http://swissmodel.expasy.org (accessed on 22 November 2021)).
2.3. Mutant and Complemented Strains Construction
Construction of mutant and complemented strains was performed as previously described [16]. Briefly, LMxysn_1693 gene flanking regions for achieving homologous recombination were amplified and ligated with digested pAULA by clone express Ⅱ one-step cloning kit (Vazyme, Nanjing, China). The recombinant plasmid pAULA-1693-SX was identified and transferred into competent strain Lm XYSN by electroporation to generate the mutant strain XYSNΔ1693. The complemented strain XYSNΔ1693::1693 was obtained on the basis of the deletion strain according to the same method within plasmid pAULA-1693H-SX, of which synonymous mutations at two amino acids following the termination codon of the LMxysn_1693 gene. All the primers used for constructing mutant and complemented strains in this study are listed in Supplementary Table S1.
2.4. Evaluation of Biological Characteristics
Lm XYSN, XYSNΔ1693 and XYSNΔ1693::1693 were cultured on BHI plate for 24 h. The next day, the bacteria cells were scraped from the plate using an inoculating loop and transferred into 5 mL of 0.45% normal saline. The bacterial turbidity was controlled at ∼0.5 with a nephelometer and biochemical characteristics were identified using a VITEK®2 GN ID card (Biomerieux, Marcy-l’Étoile, France).
2.5. Growth Curve Analysis
Bacterial of exponentially growing cultures of Lm XYSN, XYSNΔ1693 and XYSNΔ1693::1693 were harvested and adjusted to an initial OD600 value of 0.05 in BHI culture and 0.2% bile salt (Merck Sigma, Darmstadt, Germany) in BHI media, respectively. Three parallel replicates were set for each strain and each treatment with 20 mL media for 12 h. The OD600 value of each flask was measured at an hour interval for BHI culture and 0.2% bile salt in BHI culture treatment.
2.6. Determination of Biofilm Formation
The ability of bacterial biofilm formation was conducted by crystal violet assay. The overnight cultures of XYSN, XYSNΔ1693 and XYSNΔ1693::1693 were washed twice, then the OD600 was adjusted to 1.0 and diluted 10 times with BHI medium or bile salt medium. Following this, 200 μL bacteria culture was added to the wells of a 96-well plate and incubated at 4 °C, 37 °C or 42 °C for 48 h, respectively. The medium was discarded and stained with 0.1% crystal violet for 15 min, then crystal violet was removed and washed three times with ultrapure water. After drying at 56 °C, 100 μL 96% ethanol was added to each well for 15 min for elution. The biofilm formation was measured at 595 nm by BioTek synergy 2 enzyme-labeled instrument (BioTek, Winooski, VT, USA).
2.7. Analysis of Gene Expression at Transcriptional Level
Total RNA from exponentially growing cultures was extracted with RNAprep pure Cell/Bacteria Kit (Tiangen, Beijing, China). Then, 1 μg RNA was reverse transcribed into cDNA through the PrimeScript RT reagent kit (Takara, Beijing, China). The quantitative real-time PCR (qRT-PCR) operation program followed the recommended thermal cycling conditions of 7500 Real Time PCR System (Applied Biosystems, Waltham, MA, USA) under the following cycling conditions: 95 °C for 10 min, 40 cycles (95 °C for 15 s, 60 °C for 1 min) with AceQ Universal SYBR qPCR Master Mix (Vazyme, Nanjing, China). The house-keeping gene gyrB was selected as the internal reference gene to reflect the differences in gene expression objectively. The 2ΔΔCt (ΔCt = Ctobjective gene − Ctreference gene) method was used to calculate the relative changes. All the primers used for qRT-PCR in this study are listed in Supplementary Table S2.
2.8. Adhesion, Invasion and Replication Capacity of Lm
Human intestinal epithelial cells Caco-2 BBe with stabilized growth conditions were seeded into 24-well cell culture plates. Freshly cultured cells of Lm XYSN, XYSNΔ1693 and XYSNΔ1693::1693 were added at a bacterium/cell ratio (multiplicity of infection, MOI) of 20. After incubating for 1 h at 37 °C with 5% CO2, the medium was removed, and the cells were lysed in 0.2% Triton X-100 buffer for 9 min to release the bacteria. The number of bacteria was assessed after serial dilutions of the lysates onto agar plates to calculate the adhesion ability. Additionally, the cells were incubated for another 15 min and 2 h, respectively, with DMEM medium (containing 50 μg/mL gentamicin sulfate) to determine the invasion and proliferation.
2.9. Infection to Mice
Six-week-old C57BL/6 female mice (n = 5/group) were starved for 12–16 h before treatment (water allowed) and orogastrically inoculated with Lm XYSN, XYSNΔ1693 and XYSNΔ1693::1693. Briefly, the mice were starved for 12 h before treatment (water was allowed) and challenged with approximately 3 × 106 CFU of bacteria at a volume of 500 μL (containing 30 mg/mL CaCO3) per mouse. Bacterial loads in the spleen, liver, colon and ileum were evaluated at 72 h post-infection (p.i.). Intestine samples were treated as follows: about 2-cm-length intestine was taken and washed by a syringe with 5 mL of phosphate-buffered saline (PBS) to remove the luminal contents. The organs were homogenized and plated serial dilutions on the BHI plate, the intestine samples were spread onto modified Oxford medium (Becton Dickinson, Sparks, MD, USA) chromogenic plate, then the bacterial loads were counted after 20 h post spreading.
2.10. Date Analysis
Statistical analyses were performed with GraphPad Prism 8 (GraphPad Software, version 8.0.1, San Diego, CA, USA). The results were expressed as the means ± SD for the results of all qRT-PCR. The results of detecting adhesion, invasion and replication capacity of Lm were expressed as such as well. Values were means ± SEM for the results of growth curves and in vivo experiments. Data were analyzed by Student’s t-test or Tukey’s multiple comparisons test. Differences were considered significant at ns (no significance), * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001 and **** p < 0.0001.
3. Results
3.1. Association with the Transporter System
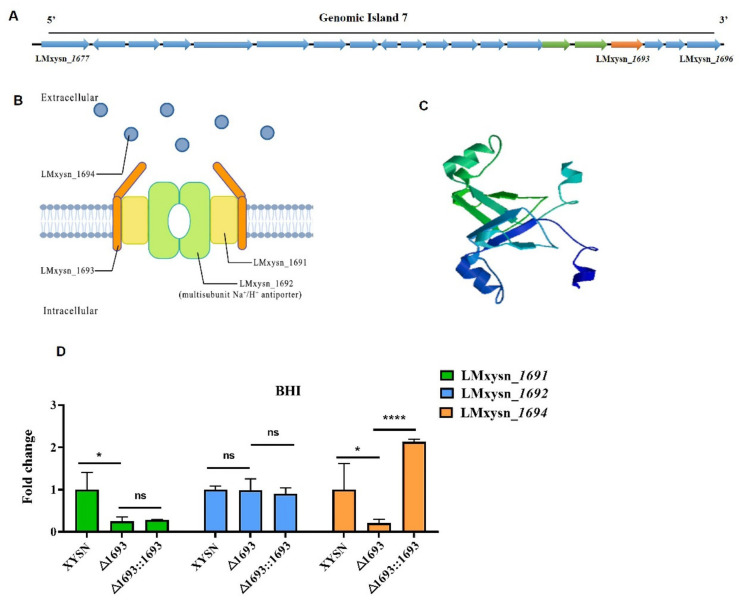
LMxysn_1693, a previously uncharacterized 534 bp-length gene located on GI-7 harboring 20 genes (Figure 1A) was a conservative and unique gene in CC33 (HSL-II) Listeria strains. The bioinformatics analysis predicted that LMxysn_1693 encoded a transmembrane protein (Supplementary Figure S1) could form a unique shape dimer (Figure 1C). Interestingly, the adjacent genes LMxysn_1691 and LMxysn_1692 were predicted to encode multiple spanning transmembrane barrel proteins to form hydrophobic channels (Table 1). Moreover, LMxysn_1691 was predicted to be a membrane electron transporter, and LMxysn_1692 encoded a multisubunit Na+/H+ antiporter (Table 1). Additionally, LMxsyn_1695 encoded a N-acetylmuramoyl-L-alanine amidase. These data supported that LMxysn_1691, LMxysn_1692 and LMxysn_1693 were possible to form an ABC transporter system, GI-7 possibly composed of two ABC transporters, which were involved in transporting extracellular and cell surface proteins (Figure 1B and Figure S2).
Figure 1.
Bioinformatics analysis of XYSN GI-7. All genes located in GI-7 are shown in (A). The cellular localization and function of the proteins encoded by LMxysn_1691, LMxysn_1692 and LMxysn_1693 were predicated via Biorender (Toronto, Canada) (https://biorender.com/ (accessed on 5 May 2022)) (B). Three-dimensional structure was predicted of the protein encoded by LMxysn_1693 gene (C). The expression levels of Lmxysn_1691, Lmxysn_1692 and Lmxysn_1694 genes were detected with LMxysn_1693 deletion strain by qRT-PCR (D). Error bars represent SD, n = 3 independent experiments. Statistical analysis was performed using Student’s t-test: ns, no significance; * p < 0.05, **** p < 0.0001.
Table 1.
Predictions the function of genes in GI-7.
| Gene | Domain | Location | Functional Prediction |
|---|---|---|---|
| LMxysn_1677 | None | Outside | exonuclease SbcD |
| LMxysn_1678 | PlsC Domain | Outside | 1-acyl-sn-glycerol-3-phosphate acyltransferase |
| LMxysn_1679 | Transmembrane Region | TM helix | Lipoprotein |
| LMxysn_1680 | Transmembrane Region | TM helix | Hypothetical Protein |
| LMxysn_1681 | AAA Domain | TM helix | ABC transporter ATP-binding protein/permease |
| LMxysn_1682 | AAA Domain | TM helix | ABC transporter ATP-binding protein/permease |
| LMxysn_1683 | Transmembrane Region | TM helix | Cellsurface protein |
| LMxysn_1684 | None | Outside | Proteolysis |
| LMxysn_1685 | None | Inside | Hypothetical Protein |
| LMxysn_1686 | Transmembrane Region | TM helix | Hypothetical Protein |
| LMxysn_1687 | None | Inside | Hypothetical Protein |
| LMxysn_1688 | Low complexity | Outside | DUF3221 Domain-containing Protein |
| LMxysn_1689 | None | Inside | Hypothetical Protein |
| LMxysn_1690 | Low complexity | Outside | Hypothetical Protein |
| LMxysn_1691 | Transmembrane Region | TM helix | Hypothetical Protein |
| LMxysn_1692 | Transmembrane Region | TM helix | Multisubunit Na+/H+ antiporter |
| LMxysn_1693 | Transmembrane Region | TM helix | Hypothetical Protein |
| LMxysn_1694 | None | Outside | Hypothetical Protein |
| LMxysn_1695 | SH3B Domain | Inside | N-acetylmuramoyl-L-alanine amidase |
| LMxysn_1696 | Phage_integrase | Outside | Belongs to the ‘phage’ integrase family |
The corresponding bioinformatic predictions of the genes contained in GI-7 are shown in Table 1, including the domains contained in the protein, cellular localization and functional predictions.
To evaluate the function of LMxysn_1693, we constructed XYSNΔ1693 and XYSNΔ1693::1693 (Supplementary Figure S3) and detected the transcriptional expression level of the genes in GI-7. Interestingly, LMxysn_1693 could up-regulate the expression of almost all the genes, such as LMxysn_1691, LMxysn_1694 and LMxysn_1695 (Figure 1D and Figure S2). Our results suggested that LMxysn_1693 could regulate multiple genes in the cluster, thus playing a crucial role in the function of GI-7.
To evaluate the role of LMxysn_1693 protein in cell homeostasis, the structures of XYSN, XYSNΔ1693 and XYSNΔ1693::1693 were observed by transmission electron microscopy. We found that there was no obvious ultrastructural change in the cell wall surface among the three strains (Supplementary Figure S4). Additionally, the mutant exhibited similar sensitivity to penicillin, chloramphenicol, polymyxin B and kanamycin (Supplementary Table S3). In summary, these data suggested that LMxysn_1693 was possibly not involved in Listeria cell remodel. The 43 biochemical characteristics of Lm conducted by the automatic microbial identification instrument verified that LMxysn_1693 might not be involved in metabolism of XYSN (Supplementary Table S4).
3.2. Involvement in Resisting Bile Salt
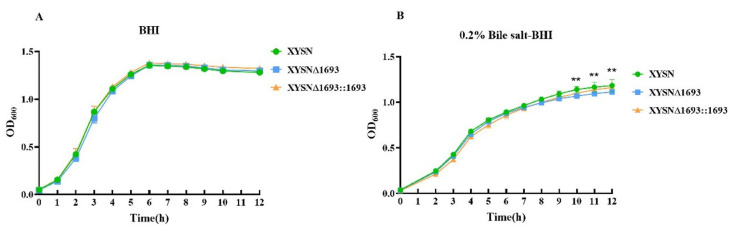
The growth curves of XYSN, XYSNΔ1693 and XYSNΔ1693::1693 (Figure 2A) were generally similar when culturing in BHI at 37 °C. While the growth of the mutant was significantly inhibited in the stationary phase cultured in the BHI supplemented with 0.2% bile salt (Figure 2B). The treatment of bile salts affected the growth of the mutant in the stationary phase, which indicated that LMxysn_1693 contributed to resisting the stress response.
Figure 2.
LMxysn_1693 gene participates in bile salt resistance of Lm. The fresh culture of wild type, LMxysn_1693 mutant and complemented strains were adjusted to OD600 = 0.05, they were inoculated to BHI medium and 0.2% bile salt–BHI medium under 37 °C, respectively. The growing curve was measured in BHI medium (A). Values are means ± SEM, n = 3 independent experiments. There is no difference among the three strains. The growing curve was measured in 0.2% bile salt-BHI medium (B). Values are means ± SEM, n = 3 independent experiments. Statistically significant differences among the deletion strain and parental or reverse mutation strains, and they were determined by Tukey’s multiple comparisons test: ns, no significance; ** p < 0.01.
3.3. Contribution to Biofilm Formation
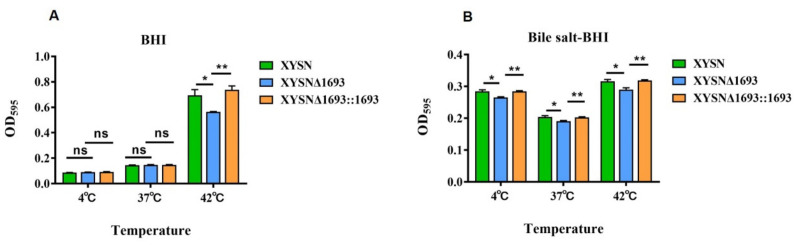
Biofilms are composed of polysaccharides, lipoproteins, fibrin and other component secreted from the cell, which assist bacteria attach to the surface to resist various adverse factors in the environment, such as high temperature, acid and poor nutrition. Here, we assumed that LMxysn_1693 was associated with biofilm formation at 4 °C, 37 °C and 42 °C in BHI medium and bile salt medium. We found that the biofilm strength of the XYSN mutant was reduced dramatically compared with the WT and complete strains at 42°C (p < 0.05), but there was no difference at 4 °C or 37 °C (Figure 3A). Unexpectedly, in the bile salt medium, the biofilm formation of XYSNΔ1693 decreased distinctly under the above three culturing temperatures (Figure 3B). These results indicated that deletion of LMxysn_1693 formed less biofilm in bile salt conditions, therefore decreasing resistance to bile salts stress.
Figure 3.
LMxysn_1693 gene contributes to biofilm formation. A quantity of overnight bacterial cultures was added into a sterile 96-well for 72 h at 37 °C. The level (OD) of the crystal violet present in destaining solution was measured at 595 nm in BHI medium at 4 °C, 37 °C and 42 °C (A), bile salt-BHI medium at three temperatures (B). Each strain was tested in triplicate. They were determined by Student’s t-test: ns, no significance; * p < 0.05, ** p < 0.01.
3.4. Interaction with Virulence and Bile-Salt-Resistant Genes
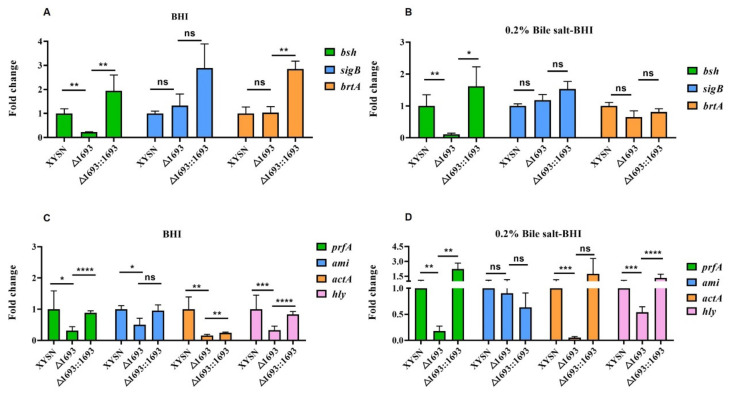
Generally, bsh encoded bile salt hydrolase, while brtA and sigB were involved in regulating coupled genes related to bile salt resistance. All the three genes were used to evaluate the interaction between LMxysn_1693 and bile salt resistance genes. We compared the transcriptional levels of these three genes within mutant, wild-type and reversion when they were cultured in BHI or BHI supplemented with 0.2% bile salt. Interestingly, bsh was remarkably down-regulated in the mutant under two culturing conditions (p < 0.01) (Figure 4A,B), whereas brtA and sigB had no significant changes between the mutant and the parental strain. The qRT-PCR results indicated that LMxysn_1693 could up-regulate the expression of bsh, thus enhancing the survival ability in the bile salt environment.
Figure 4.
The expression of bile salt resistance genes and virulence genes by qRT-PCR. The transcriptional expressions of bile salt resistance genes were determined in BHI medium and 0.2% bile salt-BHI medium (A,B). The transcriptional expressions of virulence genes were determined in BHI medium and 0.2% bile salt–BHI medium (C,D). Error bars represented SD, n = 3 independent experiments. Statistical analysis was carried out by Student’s t-test: ns, no significance; * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001.
Furthermore, we detected the potential interaction between LMxysn_1693 and virulent genes prfA, actA, ami and hly. prfA, as the encoding virulent regulator, could not only play key roles in Listeria infection and pathogenicity but also contribute to survival in bile and bile salt conditions. Notably, the expression of prfA in the mutant has been down-regulated in both media, even significantly inhibited in the 0.2% bile salt-BHI (Figure 4C). Furthermore, ami, actA and hly were obviously down-regulated in both culturing conditions (Figure 4D). These results suggested that LMxysn_1693 could regulate both bile salt resisting genes and virulence genes.
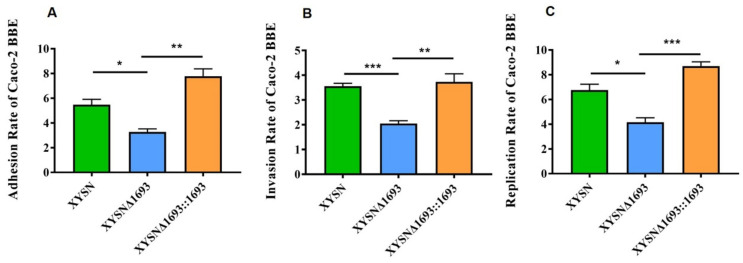
3.5. Enhancement Adhesion and Invasion Capacity
The foodborne pathogen Lm is able to cause systemic infections by crossing the intestinal barrier colonize intestinal tracts and subsequently crosses the intestinal barrier. The Caco-2 BBE cell is derived from human colon cancer epithelial cells, and its structure and function are similar to those of human small intestinal, so it has been recognized as a model for studying bacterial infection in vitro. In this study, the Caco-2 BBE cell was selected to evaluate the infection ability of Listeria strains. The mutant significantly reduced the adhesion, invasion and proliferation abilities compared with XYSN, XYSNΔ1693 and XYSNΔ1693::1693 (p < 0.05, p < 0.001, p < 0.05) (Figure 5A–C). These results strongly supported that the LMxysn_1693 played crucial role in XYSN infection epithelial cells.
Figure 5.
Adhesion, invasion and proliferation capacities of Lm. Caco-2 BBe cell was infected (MOI = 20) with Lm XYSN, XYSNΔ1693 and XYSNΔ1693::1693, respectively. The percentage of intracellular bacteria was calculated after 15 min of bacteria invasion or two hours of bacteria proliferation. The results are the adhesion (A), invasion (B) and replication (C), respectively. Among them, Lm XYSN is represented by the green bar, the mutant strain is represented by the blue bar and the complemented strain is represented by the orange bar. Error bars represented SD, n = 3 independent experiments. Statistical analysis was carried out by Student’s t-test: * p < 0.05, ** p < 0.01, *** p < 0.001.
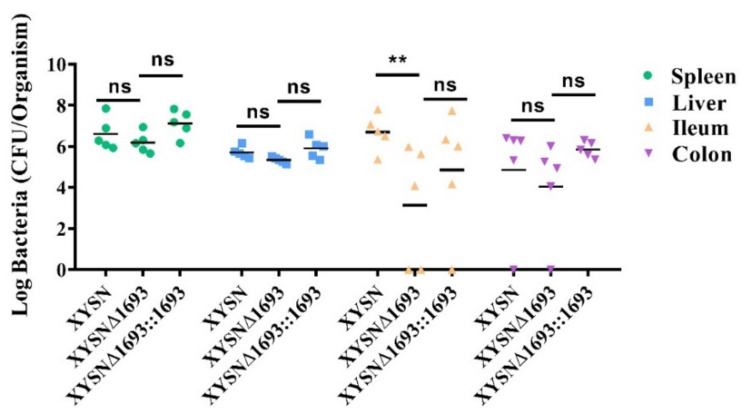
3.6. Promotion of Listeria Colonization
Mice are not naturally susceptible to Lm, whereas a low dose of hypervirulent XYSN can cause listeriosis via oral infection. We selected C57BL/6 mice for oral infection to assess the role of gene colonization in vivo. After 72 h p.i., the spleen, liver, colon and ileum of the mice were homogenized, and CFUs were counted, for which the results were analyzed through the Tukey’s multiple comparisons test. Just as expected, the bacterial load of the LMxysn_1693-deficient strain in the ileum was 100-fold lower than that of the wild-type strain (Figure 6), indicating that the loss of the gene impaired Listerial invasion and colonization ability to small intestine.
Figure 6.
Bacteria loads in organs after Lm infection mice. Lm XYSN, XYSNΔ1693 and XYSNΔ1693::1693 (3 × 106 CFU) were intragastrically inoculated to mice (n = 5). Animals were euthanized 72 h after infection, and organs were recovered, homogenized and plated. The numbers of bacteria able to colonize the ileum, colon, liver and spleen are shown. Among them, spleen is represented by the green circle, liver is represented by the blue square, ileum is represented by the orange triangle and colon is represented by the purple reverse triangle. Values are mean ± SEM; n = 3 independent experiments. Statistical analysis was performed using Tukey’s multiple comparisons test: ns, no significance; ** p < 0.01.
4. Discussion
The gastrointestinal tract contains a variety of stress factors, including proteolytic enzymes, gastric acid, high osmotic pressure, cytokines and bile salts, etc. [17]. Lm is a foodborne pathogen that has evolved a variety of strategies to survive in the gastrointestinal environment. The secretion of extracellular polysaccharides to form a biofilm is one of the ways to resist the stress factors in the gut environment [18]. Previous studies have demonstrated that transcription activators PrfA, SigB, DegU, the quorum sensing (QS) system and the accessory gene regulatory system (Agr) operon could up-regulate biofilm formation, and down-regulate by ABC transfusion permease and LuxS [19]. Notably, in this study, we find that LMxysn_1693 can up-regulate the transcriptional expression of PrfA, which indicates that the interaction between LMxysn_1693 and PrfA contributes to an increase in the biofilm formation ability. Interestingly, under bile salt stress, the biofilm formation ability of Lm is strikingly increased, and LMxysn_1693 further enhances the producing ability, which suggests that biofilm formation is associated with effector genes responding to environmental changes [20]. In brief, our study demonstrates that the LMxysn_1693 gene is involved in biofilm formation, thus contributing to Lm resistance in the intestinal environment.
Lm can enter and replicate in the lumen of the gallbladder of infected animals, whereas relatively little is known about the mechanisms of survive and growth in this location [21]. Bile salts are the major components in bile to degrade lipid-containing membranes, which have been synthesized by cholesterol in the liver and secreted from the gallbladder into the upper small intestine [11,22]. Thereby, confronting the bile-rich environments is critical for Lm persistence and survival in the gastrointestinal tract. Until now, multiple reported genes (bsh, cadC, mdrM, mdrT, brtA, etc.) have been elucidated to play crucial roles in enhancing bile salt tolerance and the colonization of Lm [11,23,24,25]. Among these, the bile exclusion locus bilE, coordinately regulated by SigB and principal virulence regulator PrfA, plays an essential role in intestinal colonization and virulence [26]. Bile sensor BrtA controls the expression of the cholic acid efflux pump MdrT [27], and CadC represses BSH expression to avoid the over expression of the cholic acid efflux pump MdrT [12]. Meanwhile, the mechanism to resist bile or bile salts for Lm is not fully understood. In this study, we find that LMxysn_1693 is involved in resistance to bile salt stress through up-regulation with prfA and bsh. We deduce that LMxysn_1693 possibly promotes the degradation or efflux pumping of bile salts in Listeria cells through activating a regulator of PrfA and unknown proteins, thereby impairing bile toxicity toward bacteria.
PrfA and SigB are global regulators in Lm, which are associated with biofilm formation and bile salt resistance, as well as coordinating with a variety of virulence factors, i.e., genes involved in adhesion, invasion, replication and cell-to-cell translocation [28,29,30]. The present study reveals that LMxysn_1693 can participate in regulating the expression of prfA, key virulence factor hly and autolysin-adhesin ami, thus ultimately affecting the expression of various virulence factors. Our work verifies that LMxysn_1693, as a unique gene distribution in all CC33 Listeria strains, not only participates in biofilm formation and bile salt resistance, but also involves adherence and invasion in to intestinal epithelial cells, therefore crossing the intestine barrier and colonizing the small intestines of mice. Based on these data, we propose that LMxysn_1693 plays an important role for CC33 strains to break through the intestinal barrier, ultimately improving the ability of survival and colonization in the gastrointestinal tract [11,20,24,25,26].
ABC transporters play multiple functions in bacterial metal utilization [31], biofilm formation [32,33,34], resistance to various stress [35,36,37,38,39], virulence and infection [40,41]. Diverse ABC transport systems have been reported in Lm, which are composed of four core members: ATP-binding proteins containing NBDs domains work as dimers, and two transmembrane TMD domain-containing proteins with a short cytoplasmic helix can transport substrate across the cell membrane, among which, NBDs and TMDs can be formed by either homodimers or heterodimers [42]. The energy for the ABC transporters is from hydrolyzing ATP, electron translocation or osmotic pressure. Moreover, extracellular substrate binding protein (SBP) is also required for capturing and delivering substrates to ABC transporters. Interestingly, LMxysn_1691 protein and LMxysn_1692 protein own TMDs with alpha helices, in which the LMxysn_1692 protein features a short cytoplasmic helix. Moreover, LMxysn_1693 is a transmembrane protein forming a uniquely shaped dimer. In our study, based on structural and function predication, we deduce that LMxysn_1693 is a member of the potential ABC transporter involved in delivering the substrates to anchoring on the cell surface or outside of the cells, such as biofilm formation components, virulent proteins (ActA) and bile salt hydrolase (BSH). Notably, we find that LMxysn_1693 interacts with multiple genes within and outside of GI-7, plays an important role in biofilm formation, bile salt resistance and virulence, enhancing the survival and colonization capacity of Lm in a gastrointestinal environment.
Taken together, our study suggests that membrane protein LMxysn_1693 is possibly the member of one transporter complex, which may be involved in delivering extracellular proteins. LMxysn_1693 not only interacts with most genes in GI-7 but also up-regulates the expression of bile-resistance genes and virulence genes, which plays important roles in biofilm formation, bile salt resistance and virulence, therefore contributing to Lm invasion and colonization in the intestine of mice. In a word, LMxysn_1693 plays a critical role in hypervirulent CC33 isolates survival in the gut, infection and pathogenicity. Further research will be necessary to decipher the coordination mechanism and role of LMxysn_1693 in enhancement Lm survival within and outside the host.
Acknowledgments
We also thank Chakraborty for kindly donating the shuttle vector pAULA to us.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/microorganisms10071263/s1, Supplementary Figure S1: Bioinformatics prediction of LMxysn_1693, Supplementary Figure S2: Bioinformatics prediction and detecting expression levels of GI-7, Supplementary Figure S3: The construction of LMxysn_1693 deletion and recovery strains, Supplementary Figure S4: Transmission electron microscopic images depicting intact cell wall structures of XYSN, XYSNΔ1693 and XYSNΔ1693::1693; Supplementary Table S1: Primers for construction of mutant and complement strains used in this study, Supplementary Table S2: Primers for quantitative real-time PCR detection used in this study, Supplementary Table S3: Determination the minimum inhibitory concentration of Lm, Supplementary Table S4: Physiological and biochemical characteristics of Lm.
Author Contributions
Y.Y. and X.J. designed the experiments. F.J. and Y.F. were involved in the experiments and analyzed the results. F.J. inference of overall genome island-7 function via bioinformatics analysis. F.M. and H.Y. participated in animal infection experiments. Q.Z. and C.C. partook in determination of biofilms and growth curves. F.J. and Y.Y. wrote the manuscript. R.Z. and Y.Y. contributed various comments for manuscript. X.C. and X.J. provided a lot of guidance in the design and writing process. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Animal experiments were conducted by following per under guidelines laid down for the welfare and ethics of experimental animals. All animals were kept at the animal biosafety facilities according to procedures approved by the Institutional Animal Ethics Committee of Yangzhou University.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Statement
This work was supported by the National Natural Science Foundation of China (No. 32161133025), Jiangsu agricultural science and technology independent innovation funds (CX(21)1004), the Key Research and Development Program (Modern Agriculture) Project of Jiangsu Province (No. BE2017341), Jiangsu Agricultural Science and Technology Independent Innovation Funds [No. CX(21)1049], and the Priority Academic Development Program of Jiangsu Higher Education Institutions (PAPD).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chen S., Meng F., Sun X., Yao H., Wang Y., Pan Z., Yin Y., Jiao X. Epidemiology of human Listeriosis in China during 2008–2017. Foodborne Pathog. Dis. 2020;17:119–125. doi: 10.1089/fpd.2019.2683. [DOI] [PubMed] [Google Scholar]
- 2.Chawla C.S., Chen H., Donnelly C.W. Mathematically modeling the repair of heat-injured Listeria monocytogenes as affected by temperature, pH, and salt concentration. Int. J. Food Microbiol. 1996;30:231–242. doi: 10.1016/0168-1605(96)00945-2. [DOI] [PubMed] [Google Scholar]
- 3.Buchanan R.L., Gorris L.G.M., Hayman M.M., Jackson T.C., Whiting R.C. A review of Listeria monocytogenes: An update on outbreaks, virulence, dose-response, ecology, and risk assessments. Food Control. 2017;75:1–13. doi: 10.1016/j.foodcont.2016.12.016. [DOI] [Google Scholar]
- 4.Núñez-Montero K., Leclercq A., Moura A., Vales G., Peraza J., Pizarro-Cerdá J., Lecuit M. Listeria costaricensis sp. nov. Int. J. Syst. Evol. Microbiol. 2018;68:844–850. doi: 10.1099/ijsem.0.002596. [DOI] [PubMed] [Google Scholar]
- 5.Lee S., Chen Y., Gorski L., Ward T.J., Osborne J., Kathariou S. Listeria monocytogenes source distribution analysis indicates regional heterogeneity and ecological niche preference among serotype 4b clones. MBio. 2018;9:e00396-18. doi: 10.1128/mBio.00396-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yin Y., Yao H., Doijad S., Kong S., Shen Y., Cai X., Tan W., Wang Y., Feng Y., Ling Z., et al. A hybrid sub-lineage of Listeria monocytogenes comprising hypervirulent isolates. Nat. Commun. 2019;10:4283. doi: 10.1038/s41467-019-12072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheet S., Yesupatham S., Ghosh K., Choi M.S., Shim K.S., Lee Y.S. Modulatory effect of low-shear modeled microgravity on stress resistance, membrane lipid composition, virulence, and relevant gene expression in the food-borne pathogen Listeria monocytogenes. Enzyme Microb. Technol. 2020;133:109440. doi: 10.1016/j.enzmictec.2019.109440. [DOI] [PubMed] [Google Scholar]
- 8.Cotter P.D., Gahan C.G., Hill C. A glutamate decarboxylase system protects Listeria monocytogenes in gastric fluid. Mol. Microbiol. 2001;40:465–475. doi: 10.1046/j.1365-2958.2001.02398.x. [DOI] [PubMed] [Google Scholar]
- 9.Sebald W., Friedl P., Schairer H.U., Hoppe J. Structure and genetics of the H+-conducting F0 portion of the ATP synthase. Ann. N. Y. Acad. Sci. 1982;402:28–44. doi: 10.1111/j.1749-6632.1982.tb25730.x. [DOI] [PubMed] [Google Scholar]
- 10.Chaturongakul S., Raengpradub S., Palmer M.E., Bergholz T.M., Orsi R.H., Hu Y., Ollinger J., Wiedmann M., Boor K.J. Transcriptomic and phenotypic analyses identify coregulated, overlapping regulons among PrfA, CtsR, HrcA, and the alternative sigma factors sigmaB, sigmaC, sigmaH, and sigmaL in Listeria monocytogenes. Appl. Environ. Microbiol. 2011;77:187–200. doi: 10.1128/AEM.00952-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Begley M., Sleator R.D., Gahan C.G., Hill C. Contribution of three bile-associated loci, bsh, pva, and btlB, to gastrointestinal persistence and bile tolerance of Listeria monocytogenes. Infect. Immun. 2005;73:894–904. doi: 10.1128/IAI.73.2.894-904.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pombinho R., Vieira A., Camejo A., Archambaud C., Cossart P., Sousa S., Cabanes D. Virulence gene repression promotes Listeria monocytogenes systemic infection. Gut Microbes. 2020;11:868–881. doi: 10.1080/19490976.2020.1712983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kovačević J., Mesak L.R., Allen K.J. Occurrence and characterization of Listeria spp. in ready-to-eat retail foods from Vancouver, British Columbia. Food Microbiol. 2012;30:372–378. doi: 10.1016/j.fm.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 14.Lee S., Parsons C., Chen Y., Hanafy Z., Brown E., Kathariou S. Identification and characterization of a novel genomic island harboring cadmium and arsenic resistance genes in Listeria welshimeri. Biomolecules. 2021;11:560. doi: 10.3390/biom11040560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hochhut B., Jahreis K., Lengeler J.W., Schmid K. CTnscr94, a conjugative transposon found in enterobacteria. J. Bacteriol. 1997;179:2097–2102. doi: 10.1128/jb.179.7.2097-2102.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park S.F., Stewart G.S. High-efficiency transformation of Listeria monocytogenes by electroporation of penicillin-treated cells. Gene. 1990;94:129–132. doi: 10.1016/0378-1119(90)90479-B. [DOI] [PubMed] [Google Scholar]
- 17.NicAogáin K., O’Byrne C.P. The role of stress and stress adaptations in determining the fate of the bacterial pathogen Listeria monocytogenes in the food chain. Front. Microbiol. 2016;7:1865. doi: 10.3389/fmicb.2016.01865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi X., Zhu X. Biofilm formation and food safety in food industries. Trends Food Sci. Technol. 2009;20:407–413. doi: 10.1016/j.tifs.2009.01.054. [DOI] [Google Scholar]
- 19.Liu Y., Wu L., Han J., Dong P., Luo X., Zhang Y., Zhu L. Inhibition of biofilm formation and related gene expression of Listeria monocytogenes in response to four natural antimicrobial compounds and sodium hypochlorite. Front. Microbiol. 2021;11:617473. doi: 10.3389/fmicb.2020.617473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiler C., Ifland A., Naumann A., Kleta S., Noll M. Incorporation of Listeria monocytogenes strains in raw milk biofilms. Int. J. Food Microbiol. 2013;161:61–68. doi: 10.1016/j.ijfoodmicro.2012.11.027. [DOI] [PubMed] [Google Scholar]
- 21.Dowd G.C., Joyce S.A., Hill C., Gahan C.G. Investigation of the mechanisms by which Listeria monocytogenes grows in porcine gallbladder bile. Infect. Immun. 2011;79:369–379. doi: 10.1128/IAI.00330-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chand D., Avinash V.S., Yadav Y., Pundle A.V., Suresh C.G., Ramasamy S. Molecular features of bile salt hydrolases and relevance in human health. Biochim. Biophys. Acta. Gen. Subj. 2017;1861:2981–2991. doi: 10.1016/j.bbagen.2016.09.024. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz K.T., Carleton J.D., Quillin S.J., Rollins S.D., Portnoy D.A., Leber J.H. Hyperinduction of host beta interferon by a Listeria monocytogenes strain naturally overexpressing the multidrug efflux pump MdrT. Infect. Immun. 2012;80:1537–1545. doi: 10.1128/IAI.06286-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang Q., Feng Y., Deng L., Feng F., Wang L., Zhou Q., Luo Q. SigB plays a major role in Listeria monocytogenes tolerance to bile stress. Int. J. Food Microbiol. 2011;145:238–243. doi: 10.1016/j.ijfoodmicro.2010.12.028. [DOI] [PubMed] [Google Scholar]
- 25.Dussurget O., Cabanes D., Dehoux P., Lecuit M., Buchrieser C., Glaser P., Cossart P., European Listeria Genome Consortium Listeria monocytogenes bile salt hydrolase is a PrfA-regulated virulence factor involved in the intestinal and hepatic phases of listeriosis. Mol. Microbiol. 2002;45:1095–1106. doi: 10.1046/j.1365-2958.2002.03080.x. [DOI] [PubMed] [Google Scholar]
- 26.Sleator R.D., Wemekamp-Kamphuis H.H., Gahan C.G., Abee T., Hill C. A PrfA-regulated bile exclusion system (BilE) is a novel virulence factor in Listeria monocytogenes. Mol. Microbiol. 2005;55:1183–1195. doi: 10.1111/j.1365-2958.2004.04454.x. [DOI] [PubMed] [Google Scholar]
- 27.Quillin S.J., Schwartz K.T., Leber J.H. The novel Listeria monocytogenes bile sensor BrtA controls expression of the cholic acid efflux pump MdrT. Mol. Microbiol. 2011;81:129–142. doi: 10.1111/j.1365-2958.2011.07683.x. [DOI] [PubMed] [Google Scholar]
- 28.Vazquez-Armenta F.J., Hernandez-Oñate M.A., Martinez-Tellez M.A., Lopez-Zavala A.A., Gonzalez-Aguilar G.A., Gutierrez-Pacheco M.M., Ayala-Zavala J.F. Quercetin repressed the stress response factor (sigB) and virulence genes (prfA, actA, inlA, and inlC), lower the adhesion, and biofilm development of L. monocytogenes. Food Microbiol. 2020;87:103377. doi: 10.1016/j.fm.2019.103377. [DOI] [PubMed] [Google Scholar]
- 29.Lemon K.P., Freitag N.E., Kolter R. The virulence regulator PrfA promotes biofilm formation by Listeria monocytogenes. J. Bacteriol. 2010;192:3969–3976. doi: 10.1128/JB.00179-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Toledo-Arana A., Dussurget O., Nikitas G., Sesto N., Guet-Revillet H., Balestrino D., Loh E., Gripenland J., Tiensuu T., Vaitkevicius K., et al. The Listeria transcriptional landscape from saprophytism to virulence. Nature. 2009;459:950–956. doi: 10.1038/nature08080. [DOI] [PubMed] [Google Scholar]
- 31.Feng Z., Liu D., Wang L., Wang Y., Zang Z., Liu Z., Song B., Gu L., Fan Z., Yang S., et al. A putative efflux transporter of the ABC family, YbhFSR, in Escherichia coli functions in tetracycline efflux and Na+(Li+)/H+ transport. Front. Microbiol. 2020;11:556. doi: 10.3389/fmicb.2020.00556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benda M., Schulz L.M., Stülke J., Rismondo J. Influence of the ABC transporter YtrBCDEF of Bacillus subtilis on competence, biofilm formation and cell wall thickness. Front. Microbiol. 2021;12:587035. doi: 10.3389/fmicb.2021.587035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poudyal B., Sauer K. The ABC of biofilm drug tolerance: The MerR-like regulator BrlR is an activator of ABC transport systems, with PA1874-77 contributing to the tolerance of Pseudomonas aeruginosa biofilms to tobramycin. Antimicrob. Agents. Chemother. 2018;62:e01981-17. doi: 10.1128/AAC.01981-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pinweha P., Pumirat P., Cuccui J., Jitprasutwit N., Muangsombut V., Srinon V., Boonyuen U., Thiennimitr P., Vattanaviboon P., Cia F., et al. Inactivation of bpsl1039-1040 ATP-binding cassette transporter reduces intracellular survival in macrophages, biofilm formation and virulence in the murine model of Burkholderia pseudomallei infection. PLoS ONE. 2018;13:e0196202. doi: 10.1371/journal.pone.0196202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jiang X., Geng Y., Ren S., Yu T., Li Y., Liu G., Wang H., Meng H., Shi L. The VirAB-VirSR-AnrAB multicomponent system is involved in resistance of Listeria monocytogenes EGD-e to cephalosporins, bacitracin, nisin, benzalkonium chloride, and ethidium bromide. Appl. Environ. Microbiol. 2019;85:e01470-19. doi: 10.1128/AEM.01470-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grubaugh D., Regeimbal J.M., Ghosh P., Zhou Y., Lauer P., Dubensky T.W., Jr., Higgins D.E. The VirAB ABC transporter is required for VirR regulation of Listeria monocytogenes virulence and resistance to nisin. Infect. Immun. 2018;86:e00901-17. doi: 10.1128/IAI.00901-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Collins B., Curtis N., Cotter P.D., Hill C., Ross R.P. The ABC transporter AnrAB contributes to the innate resistance of Listeria monocytogenes to nisin, bacitracin, and various beta-lactam antibiotics. Antimicrob. Agents Chemother. 2010;54:4416–4423. doi: 10.1128/AAC.00503-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kang J., Wiedmann M., Boor K.J., Bergholz T.M. VirR-mediated resistance of Listeria monocytogenes against food antimicrobials and cross-protection induced by exposure to organic acid salts. Appl. Environ. Microbiol. 2015;81:4553–4562. doi: 10.1128/AEM.00648-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rismondo J., Schulz L.M. Not just transporters: Alternative functions of ABC transporters in Bacillus subtilis and Listeria monocytogenes. Microorganisms. 2021;9:163. doi: 10.3390/microorganisms9010163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matthysse A.G., Yarnall H.A., Young N. Requirement for genes with homology to ABC transport systems for attachment and virulence of Agrobacterium tumefaciens. J. Bacteriol. 1996;178:5302–5308. doi: 10.1128/jb.178.17.5302-5308.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Soni D.K., Dubey S.K., Bhatnagar R. ATP-binding cassette (ABC) import systems of Mycobacterium tuberculosis: Target for drug and vaccine development. Emerg. Microbes. Infect. 2020;9:207–220. doi: 10.1080/22221751.2020.1714488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Locher K.P. Mechanistic diversity in ATP-binding cassette (ABC) transporters. Nat. Struct. Mol. Biol. 2016;23:487–493. doi: 10.1038/nsmb.3216. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.