Abstract
Highly Pathogenic Avian Influenza Viruses (HPAIVs) arise from low pathogenic precursors following spillover from wild waterfowl into poultry populations. The main virulence determinant of HPAIVs is the presence of a multi-basic cleavage site (MBCS) in the hemagglutinin (HA) glycoprotein. The MBCS allows for HA cleavage and, consequently, activation by ubiquitous proteases, which results in systemic dissemination in terrestrial poultry. Since 1959, 51 independent MBCS acquisition events have been documented, virtually all in HA from the H5 and H7 subtypes. In the present article, data from natural LPAIV to HPAIV conversions and experimental in vitro and in vivo studies were reviewed in order to compile recent advances in understanding HA cleavage efficiency, protease usage, and MBCS acquisition mechanisms. Finally, recent hypotheses that might explain the unique predisposition of the H5 and H7 HA sequences to obtain an MBCS in nature are discussed.
Keywords: Highly Pathogenic Avian Influenza Viruses, Low-Pathogenic Avian Influenza Viruses, multibasic cleavage site, virulence, pathogen evolution, proteolytic cleavage, RNA-dependent RNA polymerase
1. Introduction
Avian influenza A viruses (AIVs) circulate in wild waterfowl, predominantly in the orders of the Anseriformes (e.g., ducks and geese) and Charadriiformes (e.g., gulls) [1]. AIVs are categorized based on the antigenic properties of their surface glycoproteins, the hemagglutinin (HA) and the neuraminidase (NA). Sixteen subtypes of HA (H1–H16) and nine subtypes of NA (N1–N9) have been distinguished in wild waterfowl [2]. In wild waterfowl, AIV infections are generally asymptomatic and do not cause histological lesions [3,4]. The replication of AIVs primarily takes place in the gastro intestinal tract (GIT), which results in fecal shedding with limited oropharyngeal shedding [5,6,7]. Therefore, fecal–oral transmission is considered to be the main route of transmission among wild birds.
Incursions of AIVs from wild waterfowl into terrestrial poultry species, e.g., chickens and turkeys, occur frequently via (in)direct contact [8,9]. In these species, AIV replication is restricted to the GIT and respiratory tract (RT), resulting in mild clinical manifestations. Such AIVs are called Low Pathogenic Avian Influenza Viruses (LPAIVs) [10]. Upon transmission to terrestrial poultry, LPAIVs of the H5 and H7 subtypes can mutate into Highly Pathogenic Avian Influenza Viruses (HPAIVs). HPAIVs cause severe hemorrhagic disease with mortality rates reaching 100% and therefore pose a significant threat to animal welfare and to the poultry industry [10]. The LPAIV to HPAIV transition is characterized by the acquisition of nucleotides coding for basic amino acids at the proteolytic cleavage site of HA. Such nucleotides can be acquired through nucleotide substitutions, sequence duplications, and/or non-homologous recombination (NHR) between HA RNA and RNA from viral or host origin. The presence of multiple basic amino acids at the cleavage site of HA, the multibasic cleavage site (MBCS), is the main determinant of the high virulence of HPAIVs in terrestrial poultry [10]. Official guidelines for the classification of AIVs as LPAIV or HPAIV have been established by The Organization of Animal Health (OIE) [11]. Classification as HPAIV is determined by the pathogenicity upon intravenous inoculation of chickens, and/or the amino acid sequence at the cleavage site of HA. Pathogenicity is defined by the Intravenous Pathogenicity Index (IVPI), which has to be experimentally determined by following disease progression in 10 4- to 8-week-old chickens at 24-h intervals for 10 days and scoring each bird as follows: 0 if normal, 1 if sick, 2 if severely sick, or 3 if dead. The IVPI is the mean score per bird per observation over the 10-day period. AIVs that have an IVPI between 1.2 and 3 are classified as HPAIV. AIVs that contain an MBCS with an identical amino acid sequence as that of previously identified HPAIVs are considered highly pathogenic irrespective of experimentally confirmed pathogenicity. The IVPI has to be determined for AIVs with novel MBCS motifs to allow for HPAIV classification.
There have been 51 independent documented events of MBCS acquisition in natural settings since 1959. In this review, all historical emergences of AIVs with an MBCS since 1959 are listed, and the current understanding of MBCS amino acid composition and acquisition is discussed. Furthermore, we shine light on the remaining questions regarding HPAIV genesis, primarily on the molecular mechanisms of nucleotide insertions leading to MBCS acquisition and why those are restricted to LPAIVs of the H5 and H7 subtypes.
2. Historical Emergences of HPAIVs
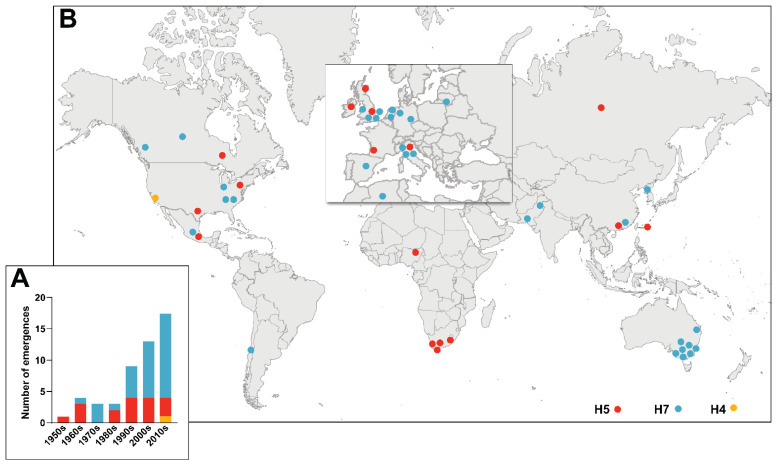
The first recorded AIV outbreak occurred in 1878, when a chicken flock in Italy contracted a contagious disease with high mortality rates [12]. Over the following decades, outbreaks with similar clinical manifestations occurred in poultry flocks and the causative pathogen was termed Fowl Plague Virus. These outbreaks were later determined to be caused by HPAIVs of the H7 subtype [13]. The first H5 HPAIV was isolated in 1959 in Scotland [14], after which the causative agents of the many HPAIV outbreaks that followed were determined and subtyped. All reported AIVs with MBCS since 1959 are listed in Table 1 (also reviewed in [15,16]). Their epidemiology varied as some caused outbreaks and others were single detections. Interestingly, not all MBCS-containing AIVs had a highly pathogenic phenotype, therefore Table 1 includes AIVs of high, low, and unknown pathogenicity. The only non-H5/H7 AIV with an MBCS is an H4N2 LPAIV from 2012 [17]. The number of MBCS acquisitions in AIVs per year has increased over time (Figure 1A), which correlates with improved surveillance efforts and the increasing demand for poultry in an expanding human population. The highest number of reported MBCS acquisitions in AIVs occurred in Europe and North America (Figure 1B). Phylogenetic analysis of newly emerged MBCS-containing AIVs showed that they belong to unique lineages [15,18], indicating that they arose from independent LPAIV to HPAIV conversions.
Table 1.
Historical emergence of MBCS-containing AIVs 1959–2021: epidemiological data, cleavage site sequence, IVPI, phenotypical classification, and progenitor (LPAIV) detection.
| Year | Country | Subtype | Cleavage Site Sequence | HA Accession Number | IVPI (Phenotype a) |
Progenitor Detection b | HA Accession Number Progenitor | Number of Affected Premises (Species) | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| 1959 | Scotland | H5N1 | PQRKKR*G c | GU052518 | N.D. d (HP) | No e | N.A. f | 2 (unknown) | [14] |
| 1961 | South Africa | H5N3 | PQRETRRQKR*G | GU052822 | N.D. (HP) | No | N.A. | N.A. g (common terns) | [34,35,36] |
| 1963 | England | H7N3 | PKRRRR*G | AF202238 | N.D. (HP) | No | N.A. | 3 (turkeys) | [37,38] |
| 1966 | Canada | H5N9 | PQRRKKR*G | CY107859 | N.D. (HP) | Yes | CY087808 | 1 (turkeys) | [39,40] |
| 1967 | USSR | H5N1 | unknown | N.A. | N.D. (HP) | No | N.A. | 1 (chickens) | [41] |
| 1976 | Australia | H7N7 | PEIPKKKEKR*G | CY024786 | N.D. (HP) | No h | N.A. | 1 (chickens) | [42,43] |
| 1979 | England | H7N7 | PEIPKKRKR*G PEIPKRRRR*G PEIPKKREKR*G |
N.A. | N.D. (HP) | No | N.A. | 3 (turkeys) | [44] |
| 1979 | Germany | H7N7 | PEIPKKKKR*G PEIPKRKKR*G PEIPKKKKKKR*G PEIPKKRKKR*G PETPKKKKKKR*G |
U20459 L43913 CY107844 L43915 L43914 |
N.D. (HP) | No i | N.A. | 2 (chickens, geese) | [45] |
| 1983–1984 | USA | H5N2 | PQKKKR*G | GU052771 | 2.37 (HP) | Yes | J04325 | 356 (chickens, turkeys, guinea fowl, chuckar) | [46,47,48] |
| 1983 | Ireland | H5N8 | PQRKRKKR*G | M18451 | 2.76 (HP) | No | N.A. | 4 (turkeys, ducks, chickens) | [49] |
| 1985 | Australia | H7N7 | PEIPKKREKR*G | M17735 | N.D. (HP) | No | N.A. | 1 (chickens) | [50,51] |
| 1991 | England | H5N1 | PQRKRKTR*G | GU052510 | 3 (HP) | No | N.A. | 1 (turkeys) | [52] |
| 1992 | Australia | H7N3 | PEIPKKKKR*G | AF202227 | 2.71 (HP) | No | N.A. | 1 (chickens, ducks) | [53,54] |
| 1994–1995 | Australia | H7N3 | PEIPRKRKR*G | CY022685 | N.D. (HP) | No | N.A. | 1 (chickens) | [54] |
| 1994–1995 | Mexico | H5N2 | PQRKRKTR*G PQRKRKRKTR*G |
AB558473 U85390 |
N.D. (HP) | Yes | GU186573 | 360 (chickens) | [55,56,57] |
| 1994–1995 | Pakistan | H7N3 | PETPKRKRKR*G PETPKRRKR*G |
AF202226 AF202230 |
N.D. (HP) | No | N.A. | Many (chickens) | [58,59] |
|
1996– now |
China | H5N1 + H5Nx j | PQRERRRKKR*G ( + many variations) |
AF144305 | 2.1 (HP) | No | N.A. | Many (many) | [60] |
| 1997 | Australia | H7N4 | PEIPRKRKR*G PEIPRKRKR*G |
AY943924 CY022701 |
2.52 k (HP) | No | N.A. | 3 (chickens, emu) | [61] |
| 1997–1998 | Italy | H5N2 | PQRRRKKR*G | CY017403 | 2.98–3 (HP) | No | N.A. | 8 outbreaks (chickens, ducks, geese, turkeys, guinea fowl, pigeons) | [62] |
| 1999–2000 | Italy | H7N1 | PKGSRVRR*G | CY021405 | 3 (HP) | Yes | GU052999 | 413 outbreaks (chickens, turkeys, guinea fowl, ducks, pheasants, quails, ostriches) | [63,64] |
| 2002 | Chile | H7N3 | PEKPKTCSPLSRCRETR*G PEKPKTCSPLSRCRKTR*G |
AY303631 AY303632 |
2.24–3 (HP) | Yes | AY303630 | 4 (chickens, turkeys) | [65,66,67] |
| 2003 | Netherlands | H7N7 | PEIPKRRRR*G | AY338458 | 2.93 (HP) | No l | N.A. | 255 (chickens) | [68,69] |
| 2003 | Netherlands | H7N3 | PEIPKGSRVRR*G | EPI1595425 | 2.4 (HP) | Yes | EPI1595417 | N.A. m (turkeys) | [70,71] |
| 2003 | Pakistan | H7N3 | PETPKRRKR*G | HM346493 | 2.8 (HP) | No | N.A. | 522 (chickens) | [59,72] |
| 2004 | USA | H5N2 | PQRKKR*G | AY849793 | 0 (LP) | No | N.A. | 6 (chickens) | [73] |
| 2004 | Canada | H7N3 | PENPKQAYRKRMTR*G (+ many variations) |
AY648287 | 2.87 (HP) | Yes | AY650270 | 42 (chickens) | [74] |
| 2004 | South Africa | H5N2 | PQREKRRKKR*G | FJ519983 | 0.63 n (HP) | No | N.A. | 38 (ostriches) | [75] |
| 2005 | North Korea | H7N7 | PEIPKGRHRRPKR*G | N.A. | N.D. (HP) | No | N.A. | 3 (chickens | [76] |
| 2006 | South Africa | H5N2 | PQRRKKR*G | EF591749 | N.D. (HP) | Yes | EF591757 | 24 (ostriches) | [77] |
| 2007 | Canada | H7N3 | PENPKTTKPRPRR*G | EU500860 | 3 (HP) | No | N.A. | 1 (chickens) | [78] |
| 2007 | Nigeria | H5N2 | KEKRRKKR*G REKRRKKR*G |
N.A. | N.D. (LPo) | No | N.A. | N.A. o (duck, geese) | [79] |
| 2008 | England | H7N7 | PEIPKRKKR*G PEIPKKKKR*G PEIPKKKKKKR*G |
FJ476173 | 2.95–3 (HP) | No | N.A. | 1 (chickens) | [80] |
| 2009 | Spain | H7N7 | PKGTKPRPRR*G | GU121458 | N.D. (HP) | No | N.A. | 1 (chickens) | [81] |
| 2011–2013 | South Africa | H5N2 | PQRRKKR*G PQRRRKKR*G PQRKRKKR*G PQRRRKR*G |
JX069081 | 0.8–1.37 p (HP) | No | N.A. | 50 (ostriches) | [82] |
| 2012 | Australia | H7N7 | PEIPRKRKR*G | N.A. | N.D. (HP) | No | N.A. | 1 (chickens) | [83] |
| 2012–2013 | Taiwan | H5N2 | PQRKKR*G PQRRKR*G |
KJ162620 KF193394 |
2.91 (HP) | No q | N.A. | 5 (chickens) | [84] |
| 2012–now | Mexico | H7N3 | PENPKDRKSRHRRTR*G | JX908509 | N.D. (HP) | No | N.A. | Many (chickens) | [85,86] |
| 2012 | USA | H4N2 | PEKRRTR*G | KF986862 | 0 (LP) | No | N.A. | 1 (quail) | [17] |
| 2013 | Italy | H7N7 | PKRKRR*G PKRKRR*G PKRRERR*G PKRKRR*G |
KF569186 | N.D. (HP) | No | N.A. | 6 (chickens, turkeys) | [87,88] |
| 2013 | Australia | H7N2 | PEIPRKRKR*G | N.A. | N.D. (HP) | No | N.A. | 2 (chickens) | [89] |
| 2015 | England | H7N7 | PEIPRHRKGR*G PEIPRHRKRR*G |
EPI623939 | 2.52 (HP) | No | N.A. | 1 (chickens) | [90] |
| 2015 | Germany | H7N7 | PEIPKRKRR*G | EPI634885 | N.D. (HP) | Yes | EPI624526 | 1 (chickens) | [91] |
| 2015–2016 | France | H5(N1, N2,N9) |
HQRRKR*G | H5N1:KU310447 H5N2:KX014878 H5N9:KX014886 |
H5N1: 2.9 (HP) | No | N.A. | 81 (chickens, ducks, geese, guinea fowl) | [92,93] |
| 2016 | Algeria | H7N1 | unknown | N.A. | N.D. (HP) | No | N.A. | N.A. r (many wild bird species) | [94] |
| 2016 | USA | H7N8 | PKKRKTR*G | KU558906 | N.D. (HP) | Yes | EPI709576 | 1 (turkeys) | [95,96] |
| 2016 | Italy | H7N7 | PELPKGRKRR*G PELPKRRERR*G |
EPI756028 | N.D. (HP) | No | N.A. | 2 (chickens, turkeys) | [97] |
| 2016–now | China | H7N9 | PEVPKGKRTAR*G PEVPKRKRTAR*G PEVPKGKRIAR*G |
EPI919533 EPI917102 |
2.92 (HP) | No s | N.A. | Many (primarily chickens) | [29,30] |
| 2017 | USA | H7N9 | PENPKTDRKSRHRRIR*G | MF357740 | N.D. (HP) | Yes | MF357732 | 2 (chickens) | [98] |
| 2020 | USA | H7N3 | PENPKTDRKSRHRRIR*G | EPI1775733 | 2.46 (HP) | Yes | MT444363 | 13 (turkeys) | [99] |
| 2020 | Australia | H7N7 | unknown | N.A. | N.D. (HP) | No | N.A. | 3 (chickens) | [100] |
| 2021 | Lithuania | H7N7 | unknown | N.A. | N.D. (HP) | No | N.A. | N.A.t (mute swan) | [101] |
a Phenotype of viral strain is based on whether the birds were showing severe (HP) or no (LP) symptoms during the time of detection and/or IVPI. b Direct progenitor is defined as the LPAIV that was detected in the same or neighboring poultry farm prior to HPAIV detection. If a virus with a closely related HA gene was reported in either poultry or wild birds, information regarding this virus will be disclosed in the footnotes. c *: site of cleavage between HA1 and HA2. d N.D.: not determined. e No: no reported progenitor. f N.A.: not applicable. g Mass mortality of common terns along the coast of The Cape of South Africa. h Direct progenitor is unknown, but domestic duck LPAIV A/duck/Victoria/76 (with tribasic cleavage site sequence PEIPKKR*G) has been hypothesized to be the progenitor of this HPAIV. i Direct progenitor is unknown, but closely related wild bird LPAIVs have been identified (A/tern/Potsdam/342-6/79 and A/swan/Potsdam/63-6/81). j Reassortant HPAIVs with the subtypes H5N1, H5N2, H5N3, H5N4, H5N5, H5N6, and H5N8 have been detected. k IVPI of HPAIV isolated from chickens (A/chicken/NSW/1/97). IVPI of emu isolate (A/emu/NSW/97) was 1.3. l Direct progenitor is unknown, but closely related wild bird LPAIV was detected (A/mallard/Netherlands/12/00). m HPAIV was retrospectively detected at low frequencies during an LPAIV outbreak in turkeys. n HPAIV was ostrich-adapted. IVPI increased to 1.2 after one passage in embryonated eggs and to 2.73 after one passage in chickens. o MBCS-containing AIVs were detected in one healthy whistling duck and multiple spur-winged geese. p Low IVPI is probably due to ostrich adaptation. q LPAIV with cleavage site motif PQRKKR*G was detected in 2008 (A/chicken/Taiwan/A703-1/08). r A total of 1300 dead migratory birds were found in a wetland. s Direct progenitor is unknown, but HA of LPAIV A/Guizhou/03240/2015 is highest in similarity to that of the early HPAIVs. t HPAIV was detected in one mute swan that was found dead.
Figure 1.
Chronological and geographical depiction of the historical emergence of AIVs with MBCS 1959–2021. (A) Number of detections of novel AIVs with MBCS of the H5 (red), H7 (blue), and H4 (orange) HA subtypes per decade. (B) Geographical origin of MBCS-containing AIVs. Dots have been slightly displaced in areas with high emergence density in order to improve visibility.
Generally, HPAIV outbreaks occurred in terrestrial poultry holdings, e.g., chicken, turkey, and ostrich farms, and were short-term epizootics with limited regional spread. Most outbreaks were halted by stringent culling measures and/or vaccination. However, despite intervention attempts, multiple HPAIVs have circulated for longer periods of time following their initial emergence. HPAIVs from the H5 lineage whose HA originates from the H5N1 HPAIV A/goose/Guangdong/1/96 (Gs/Gd) strain are currently enzootic in poultry and wild birds in various parts of the world. Gs/Gd-H5 HPAIVs caused outbreaks in poultry in Hong Kong in 1997, alongside human infections [19,20]. The outbreaks were stamped out by a massive poultry eradication scheme. However, the Gs/Gd-H5 HPAIVs resurfaced in terrestrial and aquatic poultry and wild birds in Hong Kong and mainland China in 2001/2002 and caused two human infections in Hong Kong in 2003 [21]. From late 2003 onwards, Gs/Gd-H5 HPAIVs spread to many countries on four continents, likely through poultry trade and bird migration, causing outbreaks in poultry and wild birds and sporadic human infections [22,23,24]. As of the 4th of March 2022, a total of 953 confirmed human cases of Gs/Gd-H5 HPAIV infection have been documented, of which 491 were fatal, emphasizing the threat that HPAIVs pose to human health [25]. In 2012, H7N3 HPAIVs arose in Mexico and became enzootic in poultry populations despite vaccination efforts [26]. Only two human cases of conjunctivitis due to the Mexican H7N3 HPAIVs have been reported in almost a decade of circulation [27]. From 2013 to 2018, H7N9 AIVs caused annual waves of human infection in China. Sporadic human-to-human transmission was reported, increasing the concern for a potential pandemic [28]. Initially, the H7N9 AIVs were LPAIVs. In 2016, H7N9 HPAIVs were detected following an LPAIV to HPAIV conversion in chickens [29,30,31]. Poultry vaccination programs were put in place, which greatly reduced H7N9 AIV detections but did not eliminate circulation entirely [32,33]. As of the 4th of March 2022, the total number of reported zoonotic H7N9 infections was 1568, including 616 deaths [25].
The emergence of HPAIVs is thought to occur in terrestrial poultry following the transmission of H5 or H7 LPAIVs from the wild bird reservoir. The link between HPAIV genesis and terrestrial poultry is evident when an LPAIV progenitor is detected in the same or neighboring poultry farm prior to HPAIV detection. These sparse occasions (12 in total) have been indicated in Table 1. For another four cases, LPAIVs carrying a closely related HA were identified and are mentioned in the footnotes of Table 1. In most cases, a progenitor was not identified and the species in which the LPAIV to HPAIV conversion occurred could not be unambiguously determined. Nevertheless, HPAIV genesis has historically not been associated with wild birds as, prior to the emergence of the Gs/Gd-H5 lineage, HPAIVs had only been sporadically detected in a handful of wild birds near infected poultry populations [102,103] and during one South African outbreak of H5N3 HPAIV in common terns in 1961 [35]. In 1996, the Gs/Gd-H5 HPAIVs were first detected in domestic geese rather than in terrestrial poultry [60]. After becoming enzootic in China and Southeast Asia in 2003 and 2004, they have disseminated to Africa, Europe, and North America, probably by long-distance bird migration [2,104,105,106]. Recently, a few other AIVs with MBCS that could not be linked to outbreaks in poultry holdings have been detected in wild birds. In 2007, H5N2 AIVs with the MBCS motifs KEKRRKKR and REKRRKKR were detected in healthy geese during wild bird surveillance in Nigeria [79], however, the inability to culture the AIVs from original material prevented further investigation into their pathogenicity. In 2016, an H7N1 HPAIV outbreak occurred in a nature reserve in Algeria, leading to a high number of bird deaths [94], and an H7N7 HPAIV was detected in a dead mute swan in Lithuania in 2021 [101]. Taken together, the majority of HPAIV emergences (45 out of 51) could be linked to outbreaks in terrestrial poultry species. However, surveillance gaps and differences in pathogenicity between hosts might lead to the underdetection of the emergence of MBCS-containing AIVs.
3. HA Cleavage and Virulence
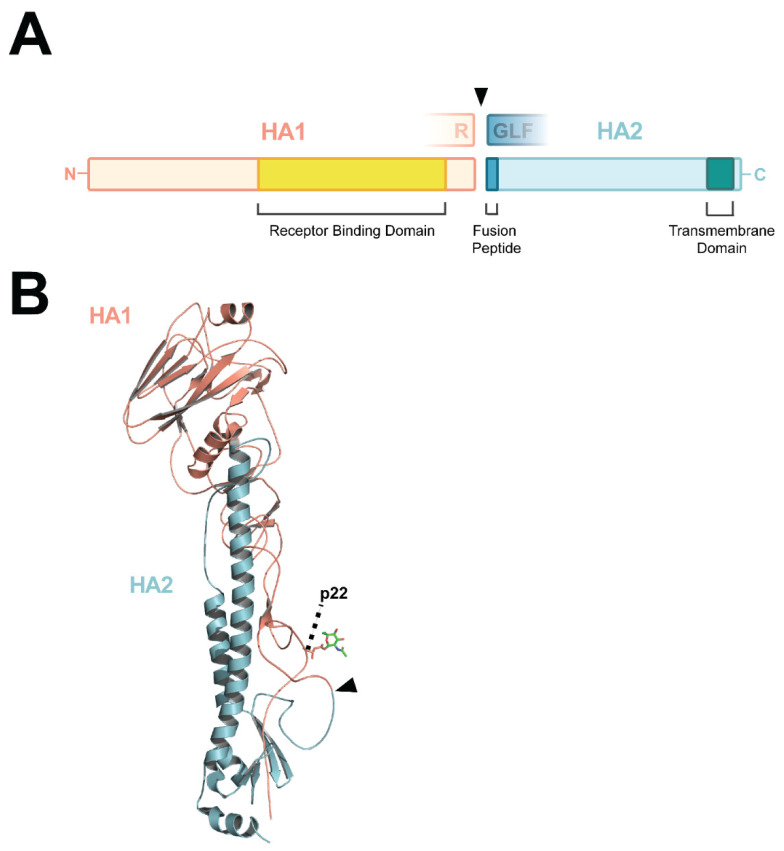
The HA glycoprotein mediates two essential events during viral entry, i.e., binding to sialic acid moieties on target cells and fusion between the viral and endosomal membranes. HA is produced as precursor HA0, anchored in the membrane of the endoplasmic reticulum [107]. HA0 monomers consist of two disulfide-linked subunits, whose boundaries are marked by a proteolytic cleavage site: subunit HA1 harbors the globular head domain with the receptor-binding pocket, and subunit HA2 harbors a large part of the HA stalk region (Figure 2A,B). Upon translation, HA0 monomers non-covalently assemble as homotrimers. The cleavage site is situated in a membrane-proximal loop (Figure 2B) [108]. The cleavage of HA0 into the HA1 and HA2 subunits activates the fusogenic properties of HA by exposing the first 11 residues of the HA2 N-terminus, which form the hydrophobic fusion peptide (Figure 2A) [109]. The fusion peptide relocates to the interior of the trimer interface upon HA0 cleavage [108]. This conformational change is the prerequisite for membrane fusion, which is triggered in an acidic environment such as the late endosomal compartment upon endocytosis [110,111].
Figure 2.
Schematic representation and structure of the HA protein. (A) Schematic representation of HA following the cleavage of HA0 into the HA1 and HA2 subunits. The amino acids flanking the cleavage site (arrow head), fusion peptide, and the receptor binding and transmembrane domains are depicted. (B) Structure of H3 HA0 monomer (PDB entry 1HA0; non-cleaved R329Q mutant [108]), made in the PyMOL Molecular Graphics System version 2.5.2 Schrödinger LLC, showing the membrane-proximal cleavage loop and site (arrow head), and glycosylation site on position 22.
The cleavage of HA0 is performed by host proteases as AIV genomes do not encode proteases. The cleavage site of LPAIVs contains one basic amino acid, an arginine (R) or in some cases a lysine (K). This monobasic cleavage site is recognized by trypsin-like serine proteases that are expressed in a tissue-specific manner. In chickens, trypsin-like proteases are expressed in the RT and GIT, limiting the tropism of LPAIVs to these organ systems. In contrast, the MBCS, here referred to as cleavage site motifs that contain a minimum of four basic amino acids or at least one inserted basic amino acid, from HPAIVs is cleaved by proteases from the subtilisin-like proprotein convertase family, including furin [112,113]. In chickens, the ubiquitous expression of this family of proteases allows for systemic viral dissemination, leading to the severe disease that is associated with HPAIV infections. The removal of the MBCS from HPAIV HAs by reverse genetics confirmed that the MBCS is the main virulence determinant of HPAIVs in terrestrial poultry [114].
The virulence of HPAIVs is a polygenic trait that is, apart from the presence of an MBCS, mediated by other properties of HA as well as other viral proteins. This is exemplified by the fact that the virulence in chickens of an LPAIV H5 with artificially inserted MBCS does not necessarily equal that of a Gs/Gd-H5 HPAIV [115]. Many amino acid changes exist between HPAIVs and their direct LPAIV progenitors, mostly in HA and the polymerase proteins, but no genetic markers common to HPAIVs apart from the MBCS have been identified [116,117]. A large phylogenetic and statistical screening was performed in which HPAIV and LPAIV sequences from different monophyletic lineages were compared, leading to the identification of a subset of parallel substitutions in HA and in the polymerase genes, which are positively associated with the evolution of HPAIV [118]. It is not yet elucidated whether substitutions accompanying HPAIV emergence are neutral, permissive, compensatory, or the result of adaptation to replication in terrestrial poultry. Indeed, AIVs show a high degree of species adaptation, and consequently, adaptations to terrestrial poultry are present in HPAIVs, such as deletions in NA [119,120,121,122,123,124] and NS1 [125,126]. Furthermore, poultry AIVs often have additional glycosylation sites (GSs) in HA that influence replication [120,124,127]. Many other factors that influence AIV virulence have been described, such as the pH stability of HA [128,129,130].
4. Proteases That Activate HA
The cleavage of HA0 can occur at multiple stages during the viral replication cycle. HA0 can be cleaved upon translation in infected cells by proteases in the secretory pathway, in the extracellular space by soluble proteases, or on the plasma membrane of target cells following budding or prior to endocytosis [131]. The nature of the particular protease that cleaves HA0 is dependent on its tissue-specific expression and substrate specificity. Furthermore, substrate cleavage efficiencies by various proteases differ between the HA subtypes [132], which might be due to differences in cleavage site sequence composition. Many proteases have been identified as likely candidates to cleave monobasic HA0 (reviewed in [131]). The Type II Transmembrane Serine Protease (TMPRSS2) has been shown to activate most, but not all, human and avian HAs in mice [133,134,135,136,137], human respiratory cell culture models [138,139], and overexpression systems [132]. Human Airway Trypsin (HAT) is expressed in respiratory ciliated cells and can cleave LPAIV HA0, albeit to a lesser extent than TMPRSS2 [132]. This might be due to the fact that HAT is active only at the plasma membrane, whereas TMPRSS2 exerts its activity both at the plasma membrane and in the secretory pathway [140], or due to the substrate specificity differences between TMPRSS2 and HAT [141]. Other proteases that can cleave monobasic HA0 are matriptase [142,143,144] and TMPRSS4 [145]. In rats, the presence of excreted HA0-cleaving proteases has been reported, such as tryptase Clara [146] and mini-plasmin [147]. Little is known regarding the avian counterparts of the mammalian LPAIV-activating proteases. Gotoh et al. found that a blood clotting factor Xa-like protease from embryonated chicken eggs activates LPAIV HA [148]. Recently, it has been shown that mallard duck TMPRSS2 can cleave H1–12, H15, and H16, but not the H14 prototype that was used in the study [139]. The NA of a few specific viral strains can also mediate the non-canonical cleavage of HA0. The NA of the mouse-adapted H1N1 A/WSN/33 strain sequesters plasminogen near HA, which, upon activation by NA, can cleave HA0 [149,150]. Similarly, the NA of LPAIV H7N6 A/mallard/Korea/6L/07 activates prothrombin into thrombin, which cleaves the consensus sequence GR*G (* represents the site of cleavage), which is present in Eurasian H7 isolates [151]. Both NA-mediated HA cleavage mechanisms allow for viral replication outside of the RT and GIT, because plasminogen and prothrombin are present systemically.
Furin was the first protease to be appointed as the activator of HPAIV HA0. Furin belongs to the proprotein convertase (PC) family, consisting of nine proteases that activate protein precursors during post-translational processing. PCs are membrane-attached or soluble and each have specific subcellular residencies (reviewed in [152]). Furin and furin-like PCs (i.e., PC5/6, PACE4, and PC7) are often implicated in the glycoprotein processing of many different viruses due to their ubiquitous/broad expression patterns [152,153]. Apart from furin, PC5/6 has been shown to cleave MBCS motifs, whereas PACE4 and PC7 did not or did so to a lesser extent [154,155]. The membrane-anchored furin and PC5 isoform PC5B accumulate in the Trans-Golgi Network (TGN), but both are present along the secretory pathway [152]. HPAIV HA trimers are therefore cleaved during post-translational processing, mainly in the TGN, which results in the release of infectious virions from the cell [156]. The minimal consensus motif for furin is RXXR, but the motif RXR/KR is considered the minimal furin-cleavage consensus for the cleavage of HA, with X representing any amino acid [152,157]. The MBCS motif KKKR is poorly cleaved by furin but is efficiently cleaved by the ubiquitously expressed Mosaic Serine Protease Large-form (MSPL) and its splice variant TMPRSS13 [158]. Most studies on the role of furin-like proteases in HA cleavage have been performed in mammalian systems. The only data available so far on avian furin-like proteases in relation to HA cleavage is that chicken furin can also cleave HPAIV HA [159], and more work is necessary to increase our knowledge of avian counterparts.
5. MBCS Amino Acid Composition
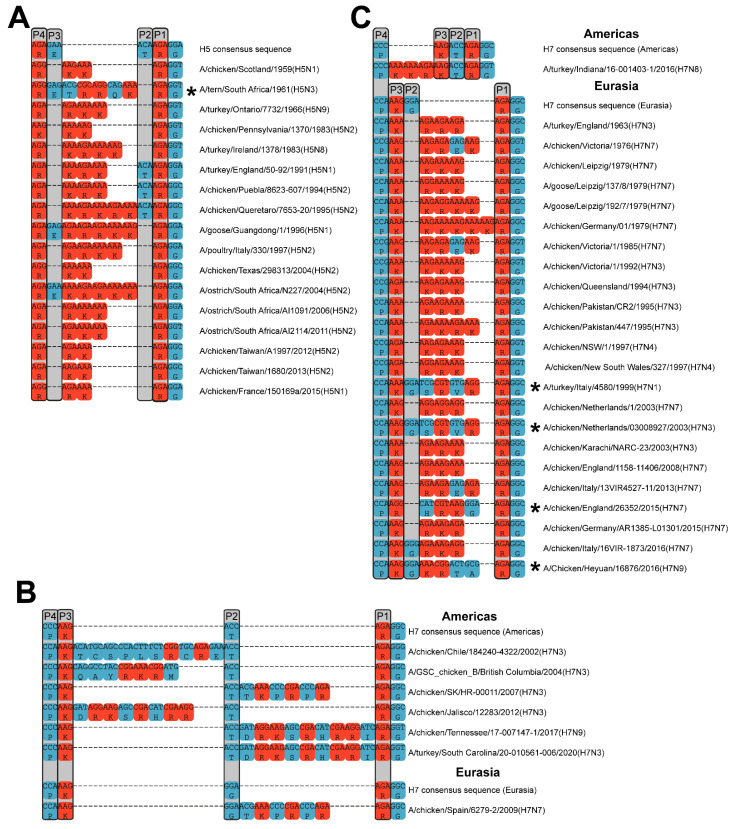
The MBCS amino acid composition, surrounding sequence, three-dimensional loop structure, and accessibility of the cleavage site strongly influence HPAIV H0 cleavage by host proteases. The cleavage site motifs of documented newly emerged HPAIV strains vary extensively in length and in amino acid composition (Table 1; Figure 3). Moreover, MBCS sequences can vary following the initial conversion event, exemplified by the diversity of the MBCS motifs in the Gs/Gd-H5 lineage (reviewed in [160]). Once an MBCS has been acquired in HA, variation at the nucleotide and amino acid level due to subsequent substitutions and/or insertions/deletions, which might be favored by the presence of purine-rich sequences in HPAIV MBCS motifs, might be tolerated as long as the resulting cleavage site can be cleaved by furin-like proteases. Although the basic amino acid arginine can be coded for by six codons, MBCS motifs almost exclusively contain purine-rich arginine codons (AGA and AGG) (Figure 3). The minimal consensus sequence of AIV-cleaving furin-like proteases is RXR/KR, but the amino acid sequence up to position six relative to the C-terminus of HA1 (P6) is thought to influence furin cleavage [161,162]. Mutational studies on the P1 to P4 positions in HPAIV HAs determined that altering either the P1 or P4 arginines resulted in reduced cleavability, whereas the P2 and P3 positions allowed for more flexibility [157,163]. Most H5 and all H7 MBCS motifs contain amino acid insertions of basic and/or non-basic amino acids in the cleavage site region (Figure 3). Two-amino-acid insertions are most frequently observed amongst natural MBCS motifs and the longest reported insertion is of 20 amino acids in a laboratory H7N7 strain [164]. It is hypothesized that amino acid insertions enlarge the cleavage loop so that it protrudes into the solvent, making it more accessible to proteases. Some H5 HPAIVs harbor a minimal furin cleavage site (Figure 3A; Table 2), but the presence of insertions leads to more optimal furin cleavage [163], and upon the passage of viruses containing cleavage site motifs RKTR and RKKR in chickens, HPAIVs with insertions at the HA cleavage site had a selective advantage [165]. In contrast, insertions were shown to be essential for the trypsin independence of an H7N2 AIV, as just substitutions of non-basic by basic amino acids in the LPAIV variant were insufficient, even when the resulting cleavage site motif was PEKRKKR [166]. In some HPAIVs, the cleavage site sequence deviates from the RXR/KR consensus motif, such as the MSPL-cleaved H5 HAs as well as H7 HAs originating from NHR (Figure 3B). Following NHR, MBCS motifs often contain RXnbXnbR, where Xnb is any non-basic amino acid. Such a motif can still be cleaved by furin, as was demonstrated for a laboratory H7N3 AIV with a large insertion, resulting in the MBCS motif SLSPLYPGRTTVLHVRTAR [167]. H7 MBCS motifs that arose through NHR also contain more histidines than MBCS motifs that arose through other mechanisms, although not in the positions essential for furin cleavage. The presence of basic histidine residues in the MBCS has been shown to contribute to furin cleavage, i.e., for the MBCS motif NSTHKQLTHHMRKKR in an equine H7N7 strain [168].
Figure 3.
Alignment of cleavage site regions of all available newly emerged natural H5 and H7 MBCS-containing AIV sequences. Nucleotide and amino acid alignments of H5 MBCS-containing AIVs (A) and alignments of H7 MBCS-containing AIVs that did (B) or presumably did not (C) arise through NHR. The asterisks indicate strains that might have emerged through NHR based on codon usage and sequence alignment. The grey boxes delineate conserved amino acids from the LPAI consensus sequence with P1 to P4 indicated on top. Arginines and lysines are depicted in red and all other amino acids are depicted in blue. All sequences are available in fasta format as Supplementary Material.
Table 2.
Natural occurrences of H5 AIVs containing a tetrabasic MBCS: molecular and in vivo characteristics.
| Viral Strain | Cleavage Site Sequence | Trypsin-Independent HA Cleavage | Putative GS p22 a | IVPI b (Phenotype c) |
Ref. |
|---|---|---|---|---|---|
| A/chicken/Scotland/1959 (H5N1) | PQRKKR*G d | + | - | N.D. e (HP) | [171] |
| A/chicken/Pennsylvania/1/1983 (H5N2) | PQKKKR*G | - | + | 0 (LP) | [171,172] |
| A/chicken/Pennsylvania/1370/1983 (H5N2) | PQKKKR*G | + | - | 2.37 (HP) | [171,172] |
| A/chicken/Texas/298313/2004 (H5N2) | PQRKKR*G | - | + | 0 (LP) | [73] |
| A/chicken/Taiwan/A703-1/2008 (H5N2) | PQRKKR*G | + | + | 0.89 (LP) | [174,175] |
| H5N2 HPAIV from Taiwan 2012 f | PQRRKR*G | N.D. | + | 2.91 (HP) | [176] |
| A/chicken/France/150169a/2015 (H5N1) | HQRRKR*G | N.D. | + | 2.9 (HP) | [93] |
a Presence of putative glycosylation site (GS) p22 (H3 numbering), based on amino acid sequence only. b IVPI: intravenous pathogenicity index. c Phenotype of viral strain is based on whether the birds were showing severe (HP) or no (LP) symptoms during the time of detection and/or IVPI. d *: site of cleavage between HA1 and HA2. e N.D.: not determined. f It is unclear which exact strain was used for IVPI determination.
The presence of an MBCS in AIVs does not automatically confer trypsin-independency or high virulence in vivo [169]. As indicated in Table 2, multiple MBCS-containing AIVs with a tetrabasic MBCS have been classified as LPAIV due to an IVPI below 1.2. A well-documented example is that of the H5 AIV that caused an outbreak in Pennsylvania in the USA in 1983. AIV isolates from the early stages of the outbreak harbored the KKKR cleavage site motif, but had low virulence in poultry (IVPI: 0). AIV isolates from later stages of the outbreak gained virulence (IVPI: 2.37), but no changes in the MBCS motif were observed [47]. Kawaoka et al. attributed the change in virulence to the loss of an N-linked glycosylation site at position 22 in HA (H3 numbering) [170]. This carbohydrate neighbors the cleavage loop, therefore causing steric hindrance and blocking protease access to the cleavage site (Figure 2B). An artificial increase in the number of basic amino acids can overcome the hindering presence of the carbohydrate chain [73,171,172]. The loss of this putative glycosylation site at p22 has been reported as a mechanism for virulence gain in AIVs of the H5 and H9 subtypes [171,173] and its impact is HA-dependent. Nevertheless, the presence of the putative glycosylation site p22 does not always hinder the cleavage of tetrabasic MBCS motifs as multiple H5 HPAIVs containing that combination have been described (Table 2). Conversely, a trypsin-dependent H5 AIV from Texas (IVPI: 0), harboring an RKKR MBCS and glycosylation p22, did not become trypsin-independent upon removal of the glycosylation site p22 [73].
6. Subtype Restriction of MBCS Acquisition: Compatibility of an MBCS at the Protein Level
All naturally evolved AIVs with an MBCS, defined as a tetrabasic motif or with inserted basic amino acids, are of the H5 and H7 subtypes, except for the previously mentioned trypsin-dependent H4N2 isolate with cleavage site motif PEKRRTR (IVPI: 0) [17,177]. However, non-H5/H7 LPAIVs with a tribasic cleavage site due to substitutions (within P1 to P4) have been described, e.g., canine H3N2 virus (PERRTR) [178] and many H9N2 LPAIVs (PAKSKR, PARSRR, and PARSKR) [179,180,181]. Why the acquisition of an MBCS is restricted to the AIVs from the H5 and H7 subtypes has not yet been elucidated, but multifactorial hypotheses have been proposed.
Firstly, it was hypothesized that the putative glycosylation site p22, which can reduce HA cleavage efficiency by furin-like proteases, might be less present in H5 and H7 AIVs [182]. However, it is conserved in AIVs from all 16 avian HA subtypes, including H5 and H7 [182] and the highest frequencies of LPAIVs without putative glycosylation site p22 have been detected in non-H5/H7 subtypes (in 3.2% (242/7657) of H9 sequences) [182]. Yet, this absence can potentiate trypsin-independent HA cleavage in certain H9N2 LPAIVs [179]. Secondly, the subtype specificity of HPAIV emergence is not due to the fact that H5 and H7 LPAIVs circulate to higher extents in poultry populations, in which virtually all MBCS acquisitions have been detected, than the other LPAIVs. H6, H9, and H10 LPAIVs are also frequently detected in poultry [183,184].
Thirdly, it has been hypothesized that the subtype restriction of MBCS acquisition might be the result of incompatibility at the protein level of an MBCS in HAs from subtypes other than H5 and H7. Nevertheless, reverse genetics studies have shown that HAs from non-H5/H7 subtypes can accommodate an artificial MBCS, which can be cleaved by ubiquitous proteases [185,186,187,188,189,190,191]. However, trypsin-independent MBCS-containing non-H5/H7 AIVs are not necessarily highly pathogenic in chickens, as both the HA and the internal gene cassette contribute to the highly pathogenic phenotype [115,177,185,186]. An H3N8-MBCS AIV did not result in severe disease upon the oculonasal inoculation of chickens [190], whereas an H6N1-MBCS AIV did show systemic replication upon the intranasal inoculation of chickens (IVPI: 1.4) [187]. Veits et al. characterized AIVs that contained H1, H2, H3, H4, H6, H8, H10, H11, H14, or H15 HAs with an engineered MBCS and the remaining seven segments of an H9N2 LPAIV or H5N1 HPAIV [185]. All reassortants had HPAIV characteristics in vitro, but only the H2, H4, H8, and H14 HAs in an HPAIV H5N1 genetic background resulted in high virulence in vivo. Interestingly, Gischke et al. reported the in vivo attenuation of an H4N2 AIV with a PEKRRTR cleavage site when the T was mutated to R or K, despite a modest increase in trypsin-independent activation by endogenous proteases [177]. Furthermore, the H4 virus with PEKRRKR cleavage site motif only supported an HPAIV phenotype when combined with the internal genes of an H5 HPAIV [177]. The virulence of MBCS-containing LPAIVs can increase upon consecutive passaging in chickens, as was exemplified by a trypsin-dependent H9N2-MBCS AIV (PARKKR) that acquired trypsin independence (following the removal of GS p22), associated with increased morbidity and mortality upon intravenous inoculation, over the course of ten passages [173]. To conclude, AIVs from non-H5/H7 subtypes with artificial MBCS show an HPAIV phenotype in vitro, which indicates that there are no major structural constraints in the HA protein, explaining the absence of MBCS motifs in non-H5/H7 AIVs. The restriction of HPAIV to H5 and H7 subtypes is, therefore, most likely due to differences and/or constraints at the RNA level, which will be discussed later in this review. However, the in vivo pathogenicity of MBCS-containing non-H5/H7 AIVs can remain low due to virulence determinants beyond the MBCS or suboptimal HA cleavage, which might hamper natural selection. Furthermore, the lack of LPAIV adaptation to poultry might partially explain why some MBCS-containing AIVs do not display a full HPAIV phenotype in vivo, especially because many of the LPAIVs in the above-mentioned studies were isolated from wild birds.
7. Mechanisms of MBCS Acquisition
Although the exact mechanisms by which H5 and H7 LPAIVs acquire an MBCS have not been elucidated, multiple non-exclusive hypotheses have been proposed [192,193,194,195]. The hypotheses are based on sequence analyses of MBCS motifs from naturally occurring HPAIVs and consist of (A) the substitution of single nucleotides resulting in codons coding for R or K, (B) stuttering or backtracking on homopolymer-rich and/or realignment-prone sequences resulting in duplications, and (C) NHR between HA RNA and RNA from viral or host origin. Both H5 and H7 HPAIVs are thought to have been generated through nucleotide substitutions and/or backtracking (Figure 3A,C), whereas NHR has been so far restricted to H7 HPAIVs (Figure 3B). These MBCS acquisition mechanisms could occur in a stepwise manner [196,197]. The following paragraphs will discuss each of the hypothesized mechanisms and the related factors that set H5/H7 HA apart from HA from other subtypes.
7.1. Nucleotide Substitutions
The influenza A virus RNA-dependent RNA polymerase (RdRp) is inherently error-prone. Single nucleotide substitutions occur at an approximate rate of 2.5 × 10−5 substitutions per nucleotide per replication cycle [198]. The consensus sequence of the HA cleavage site of H5 LPAIVs is RETR, with glutamic acid and threonine encoded by GAA and ACA codons, respectively [183]. Both codons can be converted into a basic amino acid-encoding codon upon only one nucleotide substitution, e.g., into AAA (K) or AGA (R). Such substitutions resulted in the genesis of H5 HPAIVs containing tetrabasic MBCS motifs, such as A/chicken/Scotland/1959 (RKKR) and A/chicken/France/150169a/2015 (RRKR) (Table 2). Low frequencies of amino acid substitutions within H5 and H7 LPAIV cleavage sites, resulting in tribasic motifs, have been detected [160,199].
7.2. Influenza Virus RdRp Stuttering and Backtracking
MBCS insertions are often duplications of neighboring sequences, as can be appreciated by comparing HPAIV and LPAIV cleavage site sequences (Figure 3A,C). Such duplications are thought to arise through the backtracking and realignment of the RdRp. This probably occurred in an HPAIV from the Mexican H5N2 outbreak in 1994/1995, during which an LPAIV is thought to have acquired an MBCS by one substitution followed by the duplication of six nucleotides (Figure 3A) [200]. The duplication seems to have occurred twice, eventually resulting in an RKRKRKTR cleavage site. The stuttering of the RdRp, i.e., repeatedly replicating the same nucleotide in a homopolymer stretch, could explain the presence of long adenine (A; in cRNA orientation) stretches often observed in MBCS sequences (Figure 3A,C). Stuttering on uracil residues has been well-described for poly-A-tail formation in mRNA by the viral RdRp, but this is dependent on physical constraints due to the 5′ vRNA hook remaining bound to the RdRp [201], which is not applicable to the MBCS region.
7.2.1. Influence of the Nucleotide Sequence on Influenza Virus RdRp Stuttering and Backtracking
Templates with adenine/uracil stretches have been shown to be more prone to influenza virus RdRp slippage than those with cytosine and guanine stretches, probably due to weak interactions between the base pairs [202]. Interestingly, A-rich codons often code for basic amino acids R (AGA amongst others) and K (AAA and AAG). Therefore, duplication or stuttering on A-rich templates often result in the insertion of basic amino acids at the protein level. It has been hypothesized that H5 AIVs are prone to RdRp slippage due to high numbers of adenines, and purines in general, at the cleavage site [200]. Nao et al. compared the average number of purines at the cleavage site region between a subset of HA subtypes and found that H5 and H7 HA sequences isolated in ducks contained more purine-rich sequences than H4, H6, H9, and H16 [203]. We have performed a comprehensive analysis investigating the average number of adenines and purines at the cleavage site region in all publicly available avian LPAIV HA sequences from all subtypes [183]. Large differences between HA subtypes regarding adenine usage in cRNA were detected. H5 cRNA sequences stood out as particularly A-rich, with 85% of sequences having eight or more As in P1 to P4, not necessarily consecutive. Other A-rich sequences were observed in the H3 and H14 subtypes, with 27% and 70% of sequences having eight or more As, although the latter might be unreliable due to the low number (33) of available sequences. In contrast, H7 LPAIVs contained a number of As close to average. The number of consecutive As within A-stretches per HA subtype was also analyzed, but in this regard, H5 and H7 HAs did not stand out from the other subtypes [183]. On the other hand, when considering purine or pyrimidine nucleotides, both H5 and Afro-Eurasia-Oceania (AEO) H7 sequences stand out from other subtypes, with the highest number of purines or the longest purine stretch length in the P1 to P4 region, respectively. These results mark H5 and AEO H7 LPAIVs as possibly more prone to RdRp stuttering and backtracking than other subtypes due to a higher adenine/purine content in the cleavage site.
These hypotheses are corroborated by results from experiments on the genetic stability of different sequences at the HA cleavage site. The serial passaging of LPAIVs with mono-, di-, or tribasic cleavage sites in cell culture without trypsin, embryonated eggs, or chickens to generate and/or select for HPAIVs has been attempted (Supplementary Table S1) [164,165,172,173,175,196,204,205,206,207,208,209,210,211,212,213,214,215,216]. Many of these experiments were performed using field isolates rather than clonal recombinant viruses, preventing the differentiation between MBCS genesis and the selection of already present minor HPAIV populations. Furthermore, multiple studies have applied next-generation sequencing to assess the presence of MBCS motifs at low frequencies [197,203,210,212]. However, the results of these studies should be interpreted with care, as homopolymer stretches are intrinsically error-prone for the replication enzymes used during the sequencing procedure. Nevertheless, it is apparent from passaging experiments that MBCS acquisition and HPAIV emergence are difficult to reproduce in experimental settings and require stringent selection pressure. Strains harboring the H5 LPAIV consensus RETR motif show high genetic stability during passaging [165,210]. For example, Ito et al. passaged an H5N3-RETR isolate 24 times in chicken air sacs, during which T was substituted for K, and five times in the brain, during which E was substituted for R and an R was inserted, resulting in the motif RRKKR [196]. In contrast, upon the inoculation of chickens or embryonated eggs with LPAIVs containing a dibasic cleavage site, and consequently containing longer stretches of adenines (cRNA), additional basic residues were readily introduced [165,211]. The genetic instability of di- and tribasic cleavage sites has also been shown previously using non-clonal isolates as starting material [205,206]. Increased nucleotide insertion rates were observed in in vitro reporter assays when the template contained long stretches of uracils [180,203,212] and insertions were acquired rapidly when clonal AIV stocks that already contained an MBCS were passaged once in chickens [165,173,212]. However, not all MBCS motifs are genetically unstable, e.g., H5N2-RKKR [175] and H9N2-RKKR [173], whose cleavage sites contain homopolymer stretches of seven and six adenines, respectively, and yet remained stable upon passaging (respectively eight and ten times) in chickens.
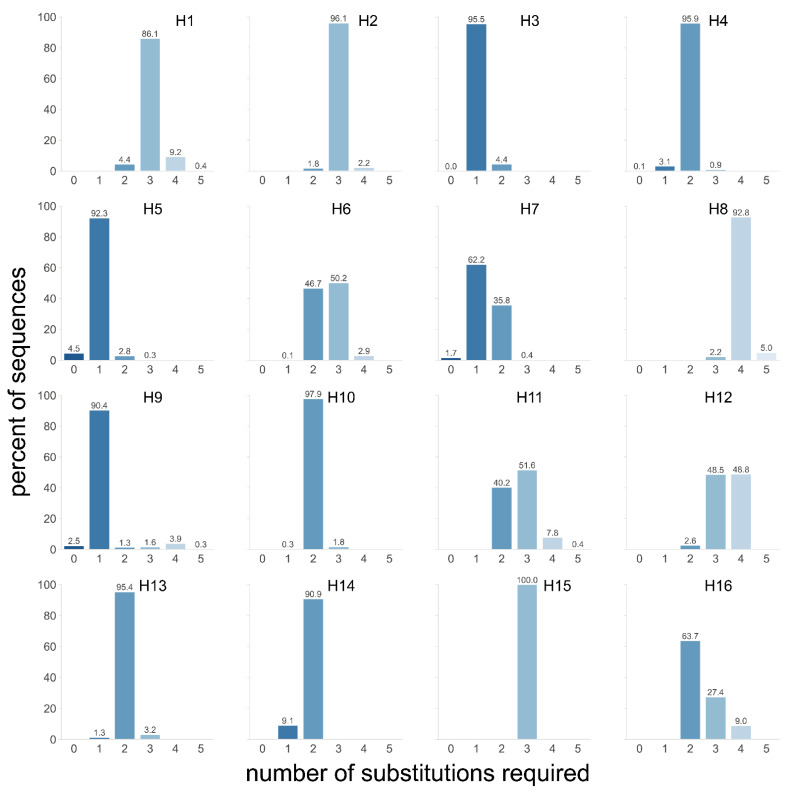
The results from the abovementioned passaging experiments and in vitro reporter systems [180,203,212] suggest that the initial acquisition of additional adenine (cRNA) nucleotides by substitutions might be the bottleneck for MBCS acquisition, as the resulting homopolymer-rich cleavage site sequence is more prone to subsequent insertions. We therefore hypothesize that H5 and H7 HAs are more prone to acquire an insertion-prone minimal MBCS than those from other subtypes. This could be due to a combination of nucleotide usage in H5 and H7 LPAIVs HAs and/or the positive selection of variants with a minimal MBCS that would be better cleaved by proteases and therefore have a fitness advantage. We investigated whether H5 and H7 LPAIV Has are more prone to acquire an MBCS due to the specifics of their cleavage site sequences, i.e., sequence differences and codon usage [183]. To that end, we assessed how many nucleotide substitutions are required in LPAIV cleavage site sequences in order to form a cleavage site motif that acts as a stepping stone for further mutational events. Such a motif was defined as containing at least three basic amino acids in P1 to P4 and an arginine in P1, excluding histidine and pyrimidine-containing arginine codons based on codon usage in HPAIVs [183]. Strikingly, an average of two to three substitutions were required in HAs from most subtypes to obtain a tribasic cleavage site (Figure 4). In contrast, the H3, H5, H7, and H9 subtypes contained a high percentage of HA sequences for which only one substitution was required to form a potentially insertion-prone tribasic cleavage site. However, the P3 serine in H9 was the remaining non-basic amino acid in such a tribasic cleavage site, coded for by TCA or TCT, interrupting the stretch of adenines which might disfavor insertions [180]. There was also an unfavorable ACC threonine codon present in the resulting H3 tribasic cleavage sites. In addition, RNA stem-loop structures, which have been suggested to potentiate stuttering and backtracking, as will be discussed in Section 7.2.2, are not conserved in the majority of avian H3 lineages [194], potentially explaining why H3 HAs have so far not acquired an MBCS in nature. Interestingly, fewer substitutions, on average, were required in AEO H7 LPAIVs to form a non-consecutive tribasic cleavage site than in those from the Americas—one and two, respectively [183]. It is tempting to speculate that this difference contributes to the observation that American H7 MBCS acquisition primarily involves NHR, whereas insertions via backtracking/stuttering are common in AEO H7 HPAIVs (Figure 3). Furthermore, when the number of required substitutions to mutate to a tribasic cleavage site were subdivided over three species categories (i.e., Anseriformes and Charadriiformes, terrestrial poultry, and others), it was apparent that fewer substitutions were required in H5 HAs from viruses detected in terrestrial poultry than in those from viruses from the other species [183]. This might indicate that there is more selection pressure on cleavage site sequences containing multiple basic amino acids in terrestrial poultry than in other birds, such as wild waterfowl. The abovementioned analysis does not take codon usage at P1 to P4 into account, thus a second analysis was performed that only allowed for codons that were naturally detected on each position per HA subtype, but the number of required substitutions to reach a stretch of a predetermined number of As was determined [183]. H5 and H7 HAs required the fewest mutations to reach long A-stretches, followed by H6 HAs. Taken together, this analysis indicates that LPAIVs from the H5 and H7 subtypes might have a genetic predisposition for acquiring an MBCS because of their cleavage site nucleotide sequence, which requires fewer random substitutions than HAs from other subtypes to obtain a cleavage site sequence that is prone to insertions.
Figure 4.
Number of nucleotide substitutions necessary to acquire a tribasic cleavage site in HAs from LPAIVs. The number of single nucleotide substitutions required to obtain a tribasic cleavage site, defined as containing at least three basic amino acids in P1 to P4 and an arginine in P1, excluding histidine and pyrimidine-containing arginine codons based on codon usage in HPAIVs, in all reported LPAIV sequences from H1–H16 HA subtypes. The exact percent of sequences is indicated on top of each bar and a darker blue color indicates fewer substitutions required (Adapted from [183], reproduced with permission from Mathis Funk, Viruses; published by MDPI, 2022).
7.2.2. Influence of RNA Structure on Influenza Virus RdRp Stuttering and Backtracking
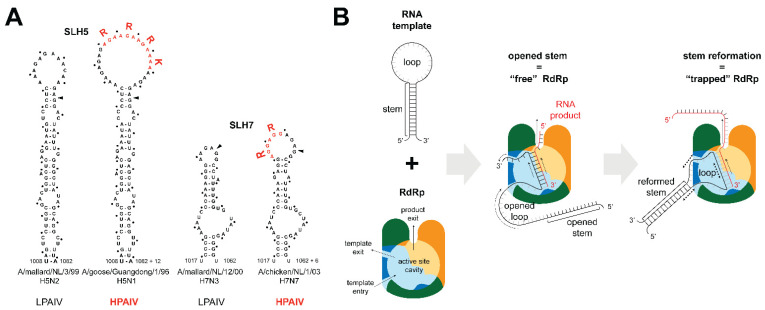
RNA folding in the region coding for the HA cleavage site has been suggested to influence RdRp backtracking/stuttering [55,70,91,180,194,197,200,203]. Although viral RNA is bound by NP molecules, local RNA structures are still formed due to the non-uniformity of NP binding [217,218]. Subtype-specific conserved stem-loop structures in the region coding for the cleavage site have been predicted by RNA folding algorithms and covariation analyses (Figure 5A) [194,219]. In H5 and H7 HA, additional basic amino acid-coding codons are inserted in the predicted loop, increasing its size [91,194,203]. Nevertheless, the presence of conserved secondary structures at the cleavage site is not unique to H5/H7 HAs, as similar stem-loop structures have been identified in non-H5/H7 HAs, albeit not in all subtypes [194,220]. Therefore, the conserved RNA secondary structures at the HA cleavage site might have a role beyond MBCS acquisition, such as the stalling of ribosomes during translation to allow the correct folding of the HA1/HA2 connecting peptide. An extensive phylogenetic and structural study, comparing LPAIV lineages that never gave rise to an HPAIV and lineages from which an HPAIV emerged, hinted at the presence of specific RNA structures in American H7 LPAIVs associated with MBCS acquisition via NHR [220]. The thermodynamic stability of these RNA secondary structures did not correlate with the capacity to become HPAIV [194,219,220]. We have previously hypothesized that the RdRp can get trapped while replicating RNA that contains strongly paired stem structures, promoting stuttering and backtracking [194]. The RdRp template entrance and exit channel are in close proximity [221], suggesting that parts of the template entering and exiting the RdRp could interact during replication. This would allow the local refolding of the HA stem, stalling the RdRp in the loop that is threaded through the polymerase, forcing it to stutter/backtrack and insert non-templated nucleotides in adenine/uracil-rich loop sequences (Figure 5B). Detailed functional studies using structured templates of HAs from different subtypes will hopefully determine whether cryptic differences between RNA stem-loop structures, such as local RNA folding during cRNA or vRNA replication, could explain subtype-specific MBCS acquisition. The first studies applying such a template-based approach in in vitro reporter systems hint toward the importance of the presence of the structure and size of the loop for MBCS acquisition and note that H5 LPAIVs contain larger loops than LPAIVs from other subtypes [180,203,212].
Figure 5.
RNA secondary structures in the cleavage site region and their hypothesized influence on RdRp replication. (A) Examples of predicted cRNA structures encompassing the cleavage site region in H5 and H7 LPAIV and HPAIV. The predicted stem-loop (SL) structures are conserved in the H5 and H7 lineages. The nucleotides coding for (part of) the MBCS are inserted in the loop and depicted in red. The boundary between HA1 and HA2 is depicted with an arrowhead. Codons are distinguished from each other by dots (Adapted with permission from [219], available under the Creative Commons Attribution 4.0 International License). (B) Proposed model for increased stuttering and backtracking rates in the stem-loop region of HA due to RNA structure. The RdRp (PB1 in blue; PB2 in orange; PA in green) replicates the viral genome into product RNA (in red). Due to the close proximity of the template entry and exit channels in PB1, local structures based on complementary sequences in the template can form around the RdRp. The RdRp is trapped in the loop region, resulting in increased rates of stuttering and backtracking, leading to duplications in the RNA product.
7.3. Non-Homologous Recombination
The insertion of exogenous RNA into the cleavage site sequence following NHR has been shown in seven out of 33 natural H7 HPAIV emergences and is probable in four additional H7 emergences based on codon usage and sequence alignment, as the stretch of inserted nucleotides did not consist of duplications of the surrounding sequence (Figure 3B,C; Supplementary Figure S1A) [195,222]. NHR has also occurred on at least two separate occasions upon the passaging of H7 viruses in experimental settings [164,214]. NHR cases are considered to be confirmed when the origin or the inserted RNA can be reliably established by blast. Most of the NHR cases belong to the American H7 lineage (Figure 3B), whereas insertions via backtracking/stuttering are thought to have occurred primarily in Eurasian H7 HPAIVs (Figure 3C). Inserted RNA either originated from host 28S ribosomal RNA (rRNA) [85,98,195,214], or viral RNA such as the nucleoprotein (NP) gene [65,164] or matrix (M) gene [74]. Some of the shorter inserted RNA sequences have been suggested to be derived from transfer RNA [195]. An equine H7N7 virus contained a stretch of 10 inserted amino acids in the cleavage site, but subsequent substitutions in this sequence prevented the determination of the original source RNA [168]. Surprisingly, recombination in H5 HA has been detected by the next-generation sequencing of samples from the H5N2 virus serially passaged in ovo [210]. Moreover, the MBCS from the 1961 H5N3 outbreak in South Africa might have arisen through NHR, as the cleavage site contains codons that are unlikely to have arisen through the duplication of neighboring sequences (Supplementary Figure S1B). Little is known of the mechanism that underlies the recombination of HA RNA with exogenous RNA. The presence of (partially) palindromic sequences flanking some cleavage sites has been suggested to play a role in some cases, but the significance of this is unclear [85,214]. We recently showed that virtually all sequences of exogenous RNA inserted in H7 correspond to small nucleolar (sno) RNA binding sites. SnoRNAs are cellular RNAs, whose main function is to guide RNA modifying proteins (e.g., methyltransferase) through complementary binding sites in the rRNA [223]. Interestingly, we found that two snoRNA binding sites out of more than 100 in 28S rRNA were involved in five independent recombination events with rRNA. Additionally, we identified chicken snoRNA binding sites corresponding to the known sites of the recombination of H7 with NP and M segments. Based on these observations, we hypothesized that snoRNAs facilitate the recombination of H7 HA with exogenous RNA [195], but further studies are warranted to prove or disprove this hypothesis.
8. Concluding Remarks
There have been a total of 51 independent emergences of MBCS-containing AIVs in the past 60 years, and their frequency has increased over the past decades. The importance of an MBCS as a virulence determinant was already established decades ago. More recently, knowledge has been acquired about factors beyond the MBCS that determine the pathogenicity of AIVs in avian hosts. Interesting discoveries were made recently regarding HA-activating proteases, such as the systemic dissemination of LPAIVs due to alternative HA cleavage mechanisms, and work is underway to characterize proteases in avian species. The biggest remaining questions concern the emergence of HPAIVs at the molecular level and the restriction of the HPAIV phenotype to the H5 and H7 subtypes in nature. Here, we shed light on the different aspects that might explain the subtype restriction of HPAIV emergence. Viruses with HAs of the H5 and H7 subtypes do not stand out from those of other subtypes with regards to circulation in terrestrial poultry, the glycosylation of p22, the presence of RNA structures at the cleavage site region, or the intrinsic ability to accommodate an MBCS at the protein level. The presence of yet-undetermined factors within H5 and H7 HA might influence the genesis of HPAIVs. Our recent analysis confirmed the previously published notion that H5 LPAIVs harbor exceptionally high numbers of adenine and purine residues at the cleavage site, which might promote errors by the RdRp. Furthermore, we showed that the minimum number of substitutions necessary for an LPAIV to obtain an insertion-prone cleavage site sequence is significantly lower in H5 and H7 subtypes. We postulated that the chance of H5 and H7 HAs acquiring an MBCS in this multi-step process is therefore higher. Recent advances have been made by using reporter assays and deep sequencing methods to elucidate the mechanisms of MBCS acquisition, highlighting that the RNA template sequence seems to be crucial for RdRp stuttering and backtracking. The role of local RNA structures remains to be investigated. Future studies utilizing in vitro replication systems and ultra-sensitive deep sequencing methods will provide the reproducibility, flexibility, throughput, and sensitivity that are necessary to elucidate the specific details of stuttering, backtracking, and recombination by the influenza RdRp.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/v14071566/s1, Supplementary Table S1: Overview of AIV passaging experiments that focus on MBCS acquisition and virulence gain. Supplementary Figure S1: Alternative alignments of MBCS-containing H5 and H7 AIVs that propose NHR as the mechanism of MBCS acquisition. Supplementary Fasta Files: Supplement H5-HPAIs and Supplement H7-HPAIs.
Author Contributions
Conceptualization, A.C.M.d.B. and M.R.; writing—original draft preparation, A.C.M.d.B. and M.R.; writing—review and editing, A.C.M.d.B., M.R., M.I.S., M.F., A.P.G. and R.A.M.F.; funding acquisition, M.R., R.A.M.F. and M.F. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The authors of this work have received funding from the European Union’s Horizon 2020 research and innovation program under DELTA-FLU, grant agreement No. 727922, from NIAID/NIH contract number 75N93021C00014, and from ZonMW Off Road project number 04510012010056.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stallknecht D.E., Shane S.M. Host range of avian influenza virus in free-living birds. Vet. Res. Commun. 1988;12:125–141. doi: 10.1007/BF00362792. [DOI] [PubMed] [Google Scholar]
- 2.Olsen B., Munster V.J., Wallensten A., Waldenström J., Osterhaus A.D.M.E., Fouchier R.A.M. Global patterns of influenza A virus in wild birds. Science. 2006;312:384–388. doi: 10.1126/science.1122438. [DOI] [PubMed] [Google Scholar]
- 3.Daoust P.Y., Kibenge F.S.B., Fouchier R.A.M., van de Bildt M.W.G., Van Riel D., Kuiken T. Replication of low pathogenic avian influenza virus in naturally infected mallard ducks (Anas platyrhynchos) causes no morphologic lesions. J. Wildl. Dis. 2011;47:401–409. doi: 10.7589/0090-3558-47.2.401. [DOI] [PubMed] [Google Scholar]
- 4.Kuiken T. Is low pathogenic avian influenza virus virulent for wild waterbirds? Proc. R. Soc. B Biol. Sci. 2013;280:20130990. doi: 10.1098/rspb.2013.0990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webster R.G., Yakhno M., Hinshaw V.S., Bean W.J., Copal Murti K. Intestinal influenza: Replication and characterization of influenza viruses in ducks. Virology. 1978;84:268–278. doi: 10.1016/0042-6822(78)90247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slemons R.D., Easterday B.C. Virus replication in the digestive tract of ducks exposed by aerosol to type-A influenza. Avian Dis. 1978;22:367–377. doi: 10.2307/1589291. [DOI] [PubMed] [Google Scholar]
- 7.Munster V.J., Baas C., Lexmond P., Bestebroer T.M., Guldemeester J., Beyer W.E.P., De Wit E., Schutten M., Rimmelzwaan G.F., Osterhaus A.D.M.E., et al. Practical considerations for high-throughput influenza A virus surveillance studies of wild birds by use of molecular diagnostic tests. J. Clin. Microbiol. 2009;47:666–673. doi: 10.1128/JCM.01625-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pepin K.M., Spackman E., Brown J.D., Pabilonia K.L., Garber L.P., Weaver J.T., Kennedy D.A., Patyk K.A., Huyvaert K.P., Miller R.S., et al. Using quantitative disease dynamics as a tool for guiding response to avian influenza in poultry in the United States of America. Prev. Vet. Med. 2014;113:376–397. doi: 10.1016/j.prevetmed.2013.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergervoet S.A., Pritz-Verschuren S.B.E., Gonzales J.L., Bossers A., Poen M.J., Dutta J., Khan Z., Kriti D., van Bakel H., Bouwstra R., et al. Circulation of low pathogenic avian influenza (LPAI) viruses in wild birds and poultry in the Netherlands, 2006–2016. Sci. Rep. 2019;9:13681. doi: 10.1038/s41598-019-50170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.França M.S., Brown J.D. Influenza pathobiology and pathogenesis in avian species. Curr. Top. Microbiol. Immunol. 2014;385:221–242. doi: 10.1007/82_2014_385. [DOI] [PubMed] [Google Scholar]
- 11.Office International des Épizooties . Avian Influenza (Including Infection with High Pathogenicity Avian Influenza Viruses) OIE; Paris, France: 2021. [(accessed on 5 August 2021)]. Chapter 3.3.4. Available online: https://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.03.04_AI.pdf. [Google Scholar]
- 12.Perroncito E. Epizoozia tifoide nei gallinacei. Ann. Accad. Agric. 1878;21:87–126. [Google Scholar]
- 13.Kaleta E.F., Rülke C.P.A. Avian Influenza. John Wiley & Sons, Inc.; Hoboken, NJ, USA: 2009. The Beginning and Spread of Fowl Plague (H7 High Pathogenicity Avian Influenza) across Europe and Asia (1878–1955) pp. 145–189. [Google Scholar]
- 14.Pereira H.G., Tůmová B., Law V.G. Avian influenza A viruses. Bull. World Health Organ. 1965;32:855–860. [PMC free article] [PubMed] [Google Scholar]
- 15.Lee D.H., Criado M.F., Swayne D.E. Pathobiological origins and evolutionary history of highly pathogenic avian influenza viruses. Cold Spring Harb. Perspect. Med. 2021;11:1–22. doi: 10.1101/cshperspect.a038679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dhingra M.S., Artois J., Dellicour S., Lemey P., Dauphin G., Von Dobschuetz S., Van Boeckel T., Castellan D.M., Morzaria S., Gilbert M. Geographical and Historical Patterns in the Emergences of Novel Highly Pathogenic Avian Influenza (HPAI) H5 and H7 Viruses in Poultry. Front. Vet. Sci. 2018;5:84. doi: 10.3389/fvets.2018.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong S.S., Yoon S.W., Zanin M., Song M.S., Oshansky C., Zaraket H., Sonnberg S., Rubrum A., Seiler P., Ferguson A., et al. Characterization of an H4N2 influenza virus from Quails with a multibasic motif in the hemagglutinin cleavage site. Virology. 2014;468–470:72–80. doi: 10.1016/j.virol.2014.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Röhm C., Horimoto T., Kawaoka Y., Süss J., Webster R.G. Do Hemagglutinin Genes of Highly Pathogenic Avian influenza Viruses Constitute Unique Phylogenetic Lineages? Virology. 1995;209:664–670. doi: 10.1006/viro.1995.1301. [DOI] [PubMed] [Google Scholar]
- 19.Chan P.K.S. Outbreak of avian influenza A(H5N1) virus infection in Hong Kong in 1997. Clin. Infect. Dis. 2002;34:58–64. doi: 10.1086/338820. [DOI] [PubMed] [Google Scholar]
- 20.De Jong J.C., Claas E.C.J., Osterhaus A.D.M.E., Webster R.G., Lim W.L. A pandemic warning? Nature. 1997;389:554. doi: 10.1038/39218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li K.S., Guan Y., Wang J., Smith G.J.D., Xu K.M., Duan L., Rahardjo A.P., Puthavathana P., Buranathai C., Nguyen T.D., et al. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature. 2004;430:209–213. doi: 10.1038/nature02746. [DOI] [PubMed] [Google Scholar]
- 22.Kilpatrick A.M., Chmura A.A., Gibbons D.W., Fleischer R.C., Marra P.P., Daszak P. Predicting the global spread of H5N1 avian influenza. Proc. Natl. Acad. Sci. USA. 2006;103:19368–19373. doi: 10.1073/pnas.0609227103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lycett S.J., Bodewes R., Pohlmann A., Banks J., Bányai K., Boni M.F., Bouwstra R., Breed A.C., Brown I.H., Chen H., et al. Role for migratory wild birds in the global spread of avian influenza H5N8. Science. 2016;354:213. doi: 10.1126/SCIENCE.AAF8852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ducatez M.F., Olinger C.M., Owoade A.A., De Landtsheer S., Ammerlaan W., Niesters H.G.M., Osterhaus A.D.M.E., Fouchier R.A.M., Muller C.P. Avian flu: Multiple introductions of H5N1 in Nigeria. Nature. 2006;442:37. doi: 10.1038/442037a. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization Avian Influenza Weekly Update Number 832. [(accessed on 4 March 2022)]. Available online: https://www.who.int/docs/default-source/wpro---documents/emergency/surveillance/avian-influenza/ai_20220218.pdf?sfvrsn=5f006f99_87.
- 26.Youk S., Lee D.H., Ferreira H.L., Afonso C.L., Absalon A.E., Swayne D.E., Suarez D.L., Pantin-Jackwood M.J. Rapid evolution of Mexican H7N3 highly pathogenic avian influenza viruses in poultry. PLoS ONE. 2019;14:0222457. doi: 10.1371/journal.pone.0222457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lopez-Martinez I., Balish A., Barrera-Badillo G., Jones J., Nuñez-García T.E., Jang Y., Aparicio-Antonio R., Azziz-Baumgartner E., Belser J.A., Ramirez-Gonzalez J.E., et al. Highly pathogenic avian influenza A(H7N3) virus in poultry workers, Mexico, 2012. Emerg. Infect. Dis. 2013;19:1531–1534. doi: 10.3201/eid1909.130087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang X., Jiang H., Wu P., Uyeki T.M., Feng L., Lai S., Wang L., Huo X., Xu K., Chen E., et al. Epidemiology of avian influenza A H7N9 virus in human beings across five epidemics in mainland China, 2013–2017: An epidemiological study of laboratory-confirmed case series. Lancet. Infect. Dis. 2017;17:822–832. doi: 10.1016/S1473-3099(17)30323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang L., Zhu W., Li X., Chen M., Wu J., Yu P., Qi S., Huang Y., Shi W., Dong J., et al. Genesis and Spread of Newly Emerged Highly Pathogenic H7N9 Avian Viruses in Mainland China. J. Virol. 2017;91:e01277-17. doi: 10.1128/JVI.01277-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qi W., Jia W., Liu D., Li J., Bi Y., Xie S., Li B., Hu T., Du Y., Xing L., et al. Emergence and Adaptation of a Novel Highly Pathogenic H7N9 Influenza Virus in Birds and Humans from a 2013 Human-Infecting Low-Pathogenic Ancestor. J. Virol. 2018;92:e00921-17. doi: 10.1128/JVI.00921-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shi J., Deng G., Kong H., Gu C., Ma S., Yin X., Zeng X., Cui P., Chen Y., Chen H., et al. H7N9 virulent mutants detected in chickens in China pose an increased threat to humans. Cell Res. 2017;27:1409–1421. doi: 10.1038/cr.2017.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeng X., Tian G., Shi J., Deng G., Li C., Chen H. Vaccination of poultry successfully eliminated human infection with H7N9 virus in China. Science China. Life Sci. 2018;61:1465–1473. doi: 10.1007/s11427-018-9420-1. [DOI] [PubMed] [Google Scholar]
- 33.Chen J., Liu Z., Li K., Li X., Xu L., Zhang M., Wu Y., Liu T., Wang X., Xie S., et al. Emergence of novel avian origin H7N9 viruses after introduction of H7-Re3 and rLN79 vaccine strains to China. Transbound. Emerg. Dis. 2021 doi: 10.1111/tbed.14401. online ahead of print . [DOI] [PubMed] [Google Scholar]
- 34.Becker W.B. The isolation and classification of Tern virus: Influenza Virus A/Tern/South Africa/1961. J. Hyg. 1966;64:309–320. doi: 10.1017/S0022172400040596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rowan M.K. Mass mortality among European Common Terns in South Africa in April-May 1961. Br. Birds. 1961;55:103–114. [Google Scholar]
- 36.Uys C.J., Becker W.B. Experimental infection of chickens with influenza A/Tern/South Africa/1961 and Chicken/Scotland/1959 viruses: II. Pathology. J. Comp. Pathol. 1967;77:167–173. doi: 10.1016/0021-9975(67)90007-2. [DOI] [PubMed] [Google Scholar]
- 37.Wells R.J.H. An outbreak of fowl plague in turkeys. Vet. Rec. 1963;75:783–786. [Google Scholar]
- 38.Alexander D.J., Allan W.H., Parsons G. Characterisation of influenza viruses isolated from turkeys in Great Britain during 1963–1977. Res Vet Sci. 1979;26:17–20. doi: 10.1016/S0034-5288(20)30934-6. [DOI] [PubMed] [Google Scholar]
- 39.Ping J., Selman M., Tyler S., Forbes N., Keleta L., Brown E.G. Low-pathogenic avian influenza virus A/turkey/Ontario/6213/1966 (H5N1) is the progenitor of highly pathogenic A/turkey/Ontario/7732/1966 (H5N9) J. Gen. Virol. 2012;93:1649–1657. doi: 10.1099/vir.0.042895-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lang G., Narayan O., Rouse B.T., Ferguson A.E., Connell M.C. A new influenza A virus infection in turkeys II. A highly pathogenic variant, a/turkey/ontario 772/66. Can. Vet. J. 1968;9:151–160. [PMC free article] [PubMed] [Google Scholar]
- 41.Lvov D.K., Shchelkanov M.Y., Alkhovsky S.V., Deryabin P.G. Zoonotic Viruses in Northern Eurasia. Academic Press; Cambridge, MA, USA: 2015. Single-Stranded RNA Viruses; pp. 135–392. [Google Scholar]
- 42.Turner A.J. The isolation of fowl plague virus in Victoria. Aust. Vet. J. 1976;52:384. doi: 10.1111/j.1751-0813.1976.tb09503.x. [DOI] [PubMed] [Google Scholar]
- 43.Westbury H.A., Turner A.J., Kovesdy L. The pathogenicity of three Australian fowl plague viruses for chickens, turkeys and ducks. Vet. Microbiol. 1979;4:223–234. doi: 10.1016/0378-1135(79)90058-0. [DOI] [Google Scholar]
- 44.Alexander D.J., Spackman D. Characterisation of influenza A viruses isolated from turkeys in England during March-May 1979. Avian Pathol. 1981;10:281–293. doi: 10.1080/03079458108418477. [DOI] [PubMed] [Google Scholar]
- 45.Röhm C., Süss J., Pohle V., Webster R.G. Different hemagglutinin cleavage site variants of H7N7 in an influenza outbreak in chickens in Leipzig, Germany. Virology. 1996;218:253–257. doi: 10.1006/viro.1996.0187. [DOI] [PubMed] [Google Scholar]
- 46.Kawaoka Y., Webster R.G. Evolution of the A/Chicken/Pennsylvania/83 (H5N2) Influenza Virus. Virology. 1985;146:130–137. doi: 10.1016/0042-6822(85)90059-5. [DOI] [PubMed] [Google Scholar]
- 47.Bean W.J., Kawaoka Y., Wood J.M., Pearson J.E., Webster R.G. Characterization of virulent and avirulent A/chicken/Pennsylvania/83 influenza A viruses: Potential role of defective interfering RNAs in nature. J. Virol. 1985;54:151–160. doi: 10.1128/jvi.54.1.151-160.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Webster R.G., Kawaoka Y., Bean W.J. Molecular changes in A/Chicken/Pennsylvania/83 (H5N2) influenza virus associated with acquisition of virulence. Virology. 1986;149:165–173. doi: 10.1016/0042-6822(86)90118-2. [DOI] [PubMed] [Google Scholar]
- 49.McNulty M.S., McParland P.J., Allan G.M., McCracken R.M. Isolation of a highly pathogenic influenza virus from turkeys. Avian Pathol. 1985;14:173–176. doi: 10.1080/03079458508436216. [DOI] [PubMed] [Google Scholar]
- 50.Barr D.A., Kelly A.P., Badman R.T., Campey A.R., O’Rourke M.D., Grix D.C., Reece R.L. Avian influenza on a multi-age chicken farm. Aust. Vet. J. 1986;63:195–196. doi: 10.1111/j.1751-0813.1986.tb02976.x. [DOI] [PubMed] [Google Scholar]
- 51.Nestorowicz A., Kawaoka Y., Bean W.J., Webster R.G. Molecular analysis of the hemagglutinin genes of Australian H7N7 influenza viruses: Role of passerine birds in maintenance or transmission? Virology. 1987;160:411–418. doi: 10.1016/0042-6822(87)90012-2. [DOI] [PubMed] [Google Scholar]
- 52.Alexander D.J., Lister S.A., Johnson M.J., Randall C.J., Thomas P.J. An outbreak of highly pathogenic avian influenza in turkeys in Great Britain in 1991. Vet. Rec. 1993;132:535–536. doi: 10.1136/vr.132.21.535. [DOI] [PubMed] [Google Scholar]
- 53.Selleck P.W., Gleeson L.J., Hooper P.T., Westbury H.A., Hansson E. Identification and characterisation of an H7N3 influenza A virus from an outbreak of virulent avian influenza in Victoria. Aust. Vet. J. 1997;75:289–292. doi: 10.1111/j.1751-0813.1997.tb10099.x. [DOI] [PubMed] [Google Scholar]
- 54.Westbury H.A. History of Highly Pathogenic Avian Influenza in Australia. Avian Dis. 2003;47:23–30. doi: 10.1637/0005-2086-47.s3.806. [DOI] [PubMed] [Google Scholar]
- 55.García M., Crawford J.M., Latimer J.W., Rivera-Cruz E., Perdue M.L. Heterogeneity in the haemagglutinin gene and emergence of the highly pathogenic phenotype among recent H5N2 avian influenza viruses from Mexico. J. Gen. Virol. 1996;77:1493–1504. doi: 10.1099/0022-1317-77-7-1493. [DOI] [PubMed] [Google Scholar]
- 56.Horimoto T., Rivera E., Pearson J., Senne D., Krauss S., Kawaoka Y., Webster R.G. Origin and molecular changes associated with emergence of a highly pathogenic H5N2 influenza virus in Mexico. Virology. 1995;213:223–230. doi: 10.1006/viro.1995.1562. [DOI] [PubMed] [Google Scholar]
- 57.Swayne D.E. Pathobiology of H5N2 Mexican avian influenza virus infections of chickens. Vet. Pathol. 1997;34:557–567. doi: 10.1177/030098589703400603. [DOI] [PubMed] [Google Scholar]
- 58.Naeem K., Hussain M. An outbreak of avian influenza in poultry in Pakistan. Vet. Rec. 1995;137:439. doi: 10.1136/vr.137.17.439. [DOI] [PubMed] [Google Scholar]
- 59.Abbas M.A., Spackman E., Swayne D.E., Ahmed Z., Sarmento L., Siddique N., Naeem K., Hameed A., Rehmani S. Sequence and phylogenetic analysis of H7N3 avian influenza viruses isolated from poultry in Pakistan 1995-2004. Virol. J. 2010;7:137. doi: 10.1186/1743-422X-7-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xu X., Subbarao K., Cox N.J., Guo Y. Genetic characterization of the pathogenic influenza A/Goose/Guangdong/1/96 (H5N1) virus: Similarity of its hemagglutinin gene to those of H5N1 viruses from the 1997 outbreaks in Hong Kong. Virology. 1999;261:15–19. doi: 10.1006/viro.1999.9820. [DOI] [PubMed] [Google Scholar]
- 61.Selleck P.W., Arzey G., Kirkland P.D., Reece R.L., Gould A.R., Daniels P.W., Westbury H.A. An outbreak of highly pathogenic avian influenza in Australia in 1997 caused by an H7N4 virus. Avian Dis. 2003;47:806–811. doi: 10.1637/0005-2086-47.s3.806. [DOI] [PubMed] [Google Scholar]
- 62.Capua I., Marangon S., Selli L., Alexander D.J., Swayne D.E., Dalla Pozza M., Parenti E., Cancellotti F.M. Outbreaks of highly pathogenic avian influenza (H5N2) in Italy during October 1997 to January 1998. Avian Pathol. 1999;28:455–460. doi: 10.1080/03079459994470. [DOI] [PubMed] [Google Scholar]
- 63.Capua I., Mutinelli F., Pozza M.D., Donatelli I., Puzelli S., Cancellotti F.M. The 1999–2000 avian influenza (H7N1) epidemic in Italy: Veterinary and human health implications. Acta Trop. 2002;83:7–11. doi: 10.1016/S0001-706X(02)00057-8. [DOI] [PubMed] [Google Scholar]
- 64.Monne I., Fusaro A., Nelson M.I., Bonfanti L., Mulatti P., Hughes J., Murcia P.R., Schivo A., Valastro V., Moreno A., et al. Emergence of a highly pathogenic avian influenza virus from a low-pathogenic progenitor. J. Virol. 2014;88:4375–4388. doi: 10.1128/JVI.03181-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Suarez D.L., Senne D.A., Banks J., Brown I.H., Essen S.C., Lee C.W., Manvell R.J., Mathieu-Benson C., Moreno V., Pedersen J.C., et al. Recombination Resulting in Virulence Shift in Avian Influenza Outbreak, Chile. Emerg. Infect. Dis. 2004;10:693–699. doi: 10.3201/eid1004.030396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rojas H., Moreira R., Avalos P., Capua I., Marangon S. Avian influenza in poultry in Chile. Vet. Rec. 2002;151:188. [PubMed] [Google Scholar]
- 67.Jones Y.L., Swayne D.E. Comparative pathobiology of low and high pathogenicity H7N3 Chilean avian influenza viruses in chickens. Avian Dis. 2004;48:119–128. doi: 10.1637/7080. [DOI] [PubMed] [Google Scholar]
- 68.Elbers A.R.W., Fabri T.H.F., De Vries T.S., De Wit J.J., Pijpers A., Koch G. The highly pathogenic avian influenza A (H7N7) virus epidemic in The Netherlands in 2003—Lessons learned from the first five outbreaks. Avian Dis. 2004;48:691–705. doi: 10.1637/7149. [DOI] [PubMed] [Google Scholar]
- 69.Stegeman A., Bouma A., Elbers A.R.W., De Jong M.C.M., Nodelijk G., De Klerk F., Koch G., Van Boven M. Avian influenza A virus (H7N7) epidemic in The Netherlands in 2003: Course of the epidemic and effectiveness of control measures. J. Infect. Dis. 2004;190:2088–2095. doi: 10.1086/425583. [DOI] [PubMed] [Google Scholar]
- 70.Beerens N., Heutink R., Harders F., Bossers A., Koch G., Peeters B. Emergence and Selection of a Highly Pathogenic Avian Influenza H7N3 Virus. J. Virol. 2020;94:e01818-19. doi: 10.1128/JVI.01818-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Velkers F.C., Bouma A., Matthijs M.G.R., Koch G., Westendorp S.T., Stegeman J.A. Outbreak of avian influenza H7N3 on a turkey farm in the Netherlands. Vet. Rec. 2006;159:403–405. doi: 10.1136/vr.159.13.403. [DOI] [PubMed] [Google Scholar]
- 72.Naeem K., Siddique N., Ayaz M., Jalalee M.A. Avian influenza in Pakistan: Outbreaks of low- and high-pathogenicity avian influenza in Pakistan during 2003–2006. Avian Dis. 2007;51:189–193. doi: 10.1637/7617-042506R.1. [DOI] [PubMed] [Google Scholar]
- 73.Lee C.-W., Swayne D.E., Linares J.A., Senne D.A., Suarez D.L. H5N2 Avian Influenza Outbreak in Texas in 2004: The First Highly Pathogenic Strain in the United States in 20 Years? J. Virol. 2005;79:11412–11421. doi: 10.1128/JVI.79.17.11412-11421.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hirst M., Astell C.R., Griffith M., Coughlin S.M., Moksa M., Zeng T., Smailus D.E., Holt R.A., Jones S., Marra M.A., et al. Novel avian influenza H7N3 strain outbreak, British Columbia. Emerg. Infect. Dis. 2004;10:2192–2195. doi: 10.3201/eid1012.040743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Abolnik C., Londt B.Z., Manvell R.J., Shell W., Banks J., Gerdes G.H., Akol G., Brown I.H. Characterisation of a highly pathogenic influenza A virus of subtype H5N2 isolated from ostriches in South Africa in 2004. Influenza Other Respi. Viruses. 2009;3:63–68. doi: 10.1111/j.1750-2659.2009.00074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Alexander D.J., Brown I.H. History of highly pathogenic avian influenza. Rev. Sci. Tech. 2009;28:19–38. doi: 10.20506/rst.28.1.1856. [DOI] [PubMed] [Google Scholar]
- 77.Abolnik C. Molecular characterization of H5N2 avian influenza viruses isolated from South African ostriches in 2006. Avian Dis. 2007;51:873–879. doi: 10.1637/7953-022107-REGR.1. [DOI] [PubMed] [Google Scholar]
- 78.Berhane Y., Hisanaga T., Kehler H., Neufeld J., Manning L., Argue C., Handel K., Hooper-McGrevy K., Jonas M., Robinson J., et al. Highly pathogenic avian influenza virus A (H7N3) in domestic poultry, Saskatchewan, Canada, 2007. Emerg. Infect. Dis. 2009;15:1492–1495. doi: 10.3201/eid1509.080231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gaidet N., Cattoli G., Hammoumi S., Newman S.H., Hagemeijer W., Takekawa J.Y., Cappelle J., Dodman T., Joannis T., Gil P., et al. Evidence of infection by H5N2 highly pathogenic avian influenza viruses in healthy wild waterfowl. PLoS Pathog. 2008;4:e1000127. doi: 10.1371/journal.ppat.1000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Seekings A.H., Slomka M.J., Russell C., Howard W.A., Choudhury B., Nuñéz A., Löndt B.Z., Cox W., Ceeraz V., Thorén P., et al. Direct evidence of H7N7 avian influenza virus mutation from low to high virulence on a single poultry premises during an outbreak in free range chickens in the UK, 2008. Infect. Genet. Evol. 2018;64:13–31. doi: 10.1016/j.meegid.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 81.Iglesias I., Martínez M., Muñoz M.J., De La Torre A., Sánchez-Vizcaíno J.M. First case of highly pathogenic avian influenza in poultry in Spain. Transbound. Emerg. Dis. 2010;57:282–285. doi: 10.1111/j.1865-1682.2010.01145.x. [DOI] [PubMed] [Google Scholar]
- 82.Abolnik C., Olivier A.J., Grewar J., Gers S., Romito M. Molecular analysis of the 2011 HPAI H5N2 outbreak in ostriches, South Africa. Avian Dis. 2012;56:865–879. doi: 10.1637/10171-041012-Reg.1. [DOI] [PubMed] [Google Scholar]
- 83.Office International des Épizooties Report Id. FUR-12739, Australia. 2012. [(accessed on 27 March 2022)]. Available online: https://wahis.oie.int/#/report-info?reportId=4656.
- 84.Lee C.D., Zhu H., Huang P., Peng L., Chang Y., Yip C., Li Y., Cheung C., Compans R., Yang C., et al. Emergence and Evolution of Avian H5N2 Influenza Viruses in Chickens in Taiwan. J. Virol. 2014;88:5677. doi: 10.1128/JVI.00139-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Maurer-Stroh S., Lee R.T., Gunalan V., Eisenhaber F. The highly pathogenic H7N3 avian influenza strain from July 2012 in Mexico acquired an extended cleavage site through recombination with host 28S rRNA. Virol. J. 2013;10:139. doi: 10.1186/1743-422X-10-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kapczynski D.R., Pantin-Jackwood M., Guzman S.G., Ricardez Y., Spackman E., Bertran K., Suarez D.L., Swayne D.E. Characterization of the 2012 Highly Pathogenic Avian Influenza H7N3 Virus Isolated from Poultry in an Outbreak in Mexico: Pathobiology and Vaccine Protection. J. Virol. 2013;87:9086–9096. doi: 10.1128/JVI.00666-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bonfanti L., Monne I., Tamba M., Santucci U., Massi P., Patregnani T., Loli Piccolomini L., Natalini S., Ferri G., Cattoli G., et al. Highly pathogenic H7N7 avian influenza in Italy. Vet. Rec. 2014;174:382. doi: 10.1136/vr.102202. [DOI] [PubMed] [Google Scholar]
- 88.Fusaro A., Tassoni L., Milani A., Hughes J., Salviato A., Murcia P.R., Massi P., Zamperin G., Bonfanti L., Marangon S., et al. Unexpected Interfarm Transmission Dynamics during a Highly Pathogenic Avian Influenza Epidemic. J. Virol. 2016;90:6401–6411. doi: 10.1128/JVI.00538-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Office International des Épizooties Rerport Id. FUR_14811, Australia. 2013. [(accessed on 27 March 2022)]. Available online: https://wahis.oie.int/#/report-info?reportId=5343.
- 90.Byrne A.M.P., Reid S.M., Seekings A.H., Núñez A., Prieto A.B.O., Ridout S., Warren C.J., Puranik A., Ceeraz V., Essen S., et al. H7N7 avian influenza virus mutation from low to high pathogenicity on a layer chicken farm in the uk. Viruses. 2021;13:259. doi: 10.3390/v13020259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dietze K., Graaf A., Homeier-Bachmann T., Grund C., Forth L., Pohlmann A., Jeske C., Wintermann M., Beer M., Conraths F.J., et al. From low to high pathogenicity—Characterization of H7N7 avian influenza viruses in two epidemiologically linked outbreaks. Transbound. Emerg. Dis. 2018;65:1576–1587. doi: 10.1111/tbed.12906. [DOI] [PubMed] [Google Scholar]
- 92.Briand F.X., Niqueux E., Schmitz A., Hirchaud E., Quenault H., Allée C., Le Prioux A., Guillou-Cloarec C., Ogor K., Le Bras M.O., et al. Emergence and multiple reassortments of French 2015-2016 highly pathogenic H5 avian influenza viruses. Infect. Genet. Evol. 2018;61:208–214. doi: 10.1016/j.meegid.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 93.Briand F.X., Schmitz A., Ogor K., Le Prioux A., Guillou-Cloarec C., Guillemoto C., Allée C., Le Bras M., Hirchaud E., Quenault H., et al. Emerging highly pathogenic H5 avian influenza viruses in France during winter 2015/16: Phylogenetic analyses and markers for zoonotic potential. Euro Surveill. 2017;22:30473. doi: 10.2807/1560-7917.ES.2017.22.9.30473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Office International des Épizooties Report Id. FUR_22420, Algeria. 2016. [(accessed on 27 March 2022)]. Available online: https://wahis.oie.int/#/report-info?reportId=8691.
- 95.Pantin-Jackwood M.J., Stephens C.B., Bertran K., Swayne D.E., Spackman E. The pathogenesis of H7N8 low and highly pathogenic avian influenza viruses from the United States 2016 outbreak in chickens, turkeys and mallards. PLoS ONE. 2017;12:e0177265. doi: 10.1371/journal.pone.0177265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Killian M.L., Kim-Torchetti M., Hines N., Yingst S., DeLiberto T., Lee D.H. Outbreak of H7N8 Low Pathogenic Avian Influenza in Commercial Turkeys with Spontaneous Mutation to Highly Pathogenic Avian Influenza. Genome Announc. 2016;4:e00457-16. doi: 10.1128/genomeA.00457-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mulatti P., Zecchin B., Monne I., Vieira J.T., Dorotea T., Terregino C., Lorenzetto M., Piccolomini L.L., Santi A., Massi P., et al. H7N7 Highly Pathogenic Avian Influenza in Poultry Farms in Italy in 2016. Avian Dis. 2017;61:261–266. doi: 10.1637/11540-112516-Case.1. [DOI] [PubMed] [Google Scholar]
- 98.Lee D.H., Torchetti M.K., Killian M.L., Berhane Y., Swayne D.E. Highly pathogenic avian influenza A(H7N9) virus, Tennessee, USA, March 2017. Emerg. Infect. Dis. 2017;23:1860–1863. doi: 10.3201/eid2311.171013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Youk S., Lee D.H., Killian M.L., Pantin-Jackwood M.J., Swayne D.E., Torchetti M.K. Highly Pathogenic Avian Influenza A(H7N3) Virus in Poultry, United States, 2020. Emerg. Infect. Dis. 2020;26:2966–2969. doi: 10.3201/eid2612.202790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Office International des Épizooties Report Id. FUR_37191, Australia. 2020. [(accessed on 27 March 2022)]. Available online: https://wahis.oie.int/#/report-info?reportId=16548.
- 101.Office International des Épizooties Report Id. FUR_150999, Lithuania. 2021. [(accessed on 27 March 2022)]. Available online: https://wahis.oie.int/#/report-info?reportId=37130.
- 102.Morgan I.R., Kelly A.P. Epidemiology of an avian influenza outbreak in Victoria in 1985. Aust. Vet. J. 1990;67:125–128. doi: 10.1111/j.1751-0813.1990.tb07727.x. [DOI] [PubMed] [Google Scholar]
- 103.Philippa J.D.W., Munster V.J., Bolhuis H.V., Bestebroer T.M., Schaftenaar W., Beyer W.E.P., Fouchier R.A.M., Kuiken T., Osterhaus A.D.M.E. Highly pathogenic avian influenza (H7N7): Vaccination of zoo birds and transmission to non-poultry species. Vaccine. 2005;23:5743–5750. doi: 10.1016/j.vaccine.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 104.Verhagen J.H., Fouchier R.A.M., Lewis N. Highly pathogenic avian influenza viruses at the wild–domestic bird interface in europe: Future directions for research and surveillance. Viruses. 2021;13:212. doi: 10.3390/v13020212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chen H., Smith G.J.D., Zhang S.Y., Qin K., Wang J., Li K.S., Webster R.G., Peiris J.S.M., Guan Y. H5N1 virus outbreak in migratory waterfowl. Nature. 2005;436:191–192. doi: 10.1038/nature03974. [DOI] [PubMed] [Google Scholar]
- 106.Office International des Épizooties Report Id. CAN-2021-HPAI-001, Canada. 2021. [(accessed on 21 May 2022)]. Available online: https://wahis.oie.int/#/report-info?reportId=45054.
- 107.Wiley D.C., Skehel J.J. The structure and function of the hemagglutinin membrane glycoprotein of influenza virus. Annu. Rev. Biochem. 1987;56:365–394. doi: 10.1146/annurev.bi.56.070187.002053. [DOI] [PubMed] [Google Scholar]
- 108.Chen J., Lee K.H., Steinhauer D.A., Stevens D.J., Skehel J.J., Wiley D.C. Structure of the hemagglutinin precursor cleavage site, a determinant of influenza pathogenicity and the origin of the labile conformation. Cell. 1998;95:409–417. doi: 10.1016/S0092-8674(00)81771-7. [DOI] [PubMed] [Google Scholar]
- 109.Klenk H.-D., Rott R., Orlich M., Blödorn J. Activation of influenza A viruses by trypsin treatment. Virology. 1975;68:426–439. doi: 10.1016/0042-6822(75)90284-6. [DOI] [PubMed] [Google Scholar]
- 110.Maeda T., Ohnishi S. Activation of influenza virus by acidic media causes hemolysis and fusion of erythrocytes. FEBS Lett. 1980;122:283–287. doi: 10.1016/0014-5793(80)80457-1. [DOI] [PubMed] [Google Scholar]
- 111.Skehel J.J., Bayley P.M., Brown E.B., Martin S.R., Waterfield M.D., White J.M., Wilson I.A., Wiley D.C. Changes in the conformation of influenza virus hemagglutinin at the pH optimum of virus-mediated membrane fusion. Proc. Natl. Acad. Sci. USA. 1982;79:968–972. doi: 10.1073/pnas.79.4.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Stieneke-Gröber A., Vey M., Angliker H., Shaw E., Thomas G., Roberts C., Klenk H.D., Garten W. Influenza virus hemagglutinin with multibasic cleavage site is activated by furin, a subtilisin-like endoprotease. EMBO J. 1992;11:2407–2414. doi: 10.1002/j.1460-2075.1992.tb05305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bosch F.X., Garten W., Klenk H.D., Rott R. Proteolytic cleavage of influenza virus hemagglutinins: Primary structure of the connecting peptide between HA1 and HA2 determines proteolytic cleavability and pathogenicity of Avian influenza viruses. Virology. 1981;113:725–735. doi: 10.1016/0042-6822(81)90201-4. [DOI] [PubMed] [Google Scholar]
- 114.Horimoto T., Kawaoka Y. Reverse genetics provides direct evidence for a correlation of hemagglutinin cleavability and virulence of an avian influenza A virus. J. Virol. 1994;68:3120–3128. doi: 10.1128/jvi.68.5.3120-3128.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bogs J., Veits J., Gohrbandt S., Hundt J., Stech O., Breithaupt A., Teifke J.P., Mettenleiter T.C., Stech J. Highly pathogenic H5N1 influenza viruses carry virulence determinants beyond the polybasic hemagglutinin cleavage site. PLoS ONE. 2010;5:11826. doi: 10.1371/journal.pone.0011826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Abdelwhab E.S.M., Veits J., Mettenleiter T.C. Genetic changes that accompanied shifts of low pathogenic avian influenza viruses toward higher pathogenicity in poultry. Virulence. 2013;4:441–452. doi: 10.4161/viru.25710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Richard M., Fouchier R., Monne I., Kuiken T. Mechanisms and risk factors for mutation from low to highly pathogenic avian influenza virus. EFSA Support. Publ. 2017;14:1287E. doi: 10.2903/SP.EFSA.2017.EN-1287. [DOI] [Google Scholar]
- 118.Escalera-Zamudio M., Golden M., Gutiérrez B., Thézé J., Keown J.R., Carrique L., Bowden T.A., Pybus O.G. Parallel evolution in the emergence of highly pathogenic avian influenza A viruses. Nat. Commun. 2020;11:5511. doi: 10.1038/s41467-020-19364-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Li J., Cardona C.J. Adaptation and Transmission of a Wild Duck Avian Influenza Isolate in Chickens. Avian Dis. 2010;54:586–590. doi: 10.1637/8806-040109-ResNote.1. [DOI] [PubMed] [Google Scholar]
- 120.Matrosovich M., Zhou N., Kawaoka Y., Webster R. The Surface Glycoproteins of H5 Influenza Viruses Isolated from Humans, Chickens, and Wild Aquatic Birds Have Distinguishable Properties. J. Virol. 1999;73:1146. doi: 10.1128/JVI.73.2.1146-1155.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hoffmann T.W., Munier S., Larcher T., Soubieux D., Ledevin M., Esnault E., Tourdes A., Croville G., Guérin J.-L., Quéré P., et al. Length Variations in the NA Stalk of an H7N1 Influenza Virus Have Opposite Effects on Viral Excretion in Chickens and Ducks. J. Virol. 2012;86:584–588. doi: 10.1128/JVI.05474-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sorrell E.M., Song H., Pena L., Perez D.R. A 27-Amino-Acid Deletion in the Neuraminidase Stalk Supports Replication of an Avian H2N2 Influenza A Virus in the Respiratory Tract of Chickens. J. Virol. 2010;84:11831–11840. doi: 10.1128/JVI.01460-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhou H., Yu Z., Hu Y., Tu J., Zou W., Peng Y., Zhu J., Li Y., Zhang A., Yu Z., et al. The special neuraminidase stalk-motif responsible for increased virulence and pathogenesis of H5N1 influenza A virus. PLoS ONE. 2009;4:e6277. doi: 10.1371/journal.pone.0006277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Li J., Dohna H.Z., Cardona C.J., Miller J., Carpenter T.E. Emergence and Genetic Variation of Neuraminidase Stalk Deletions in Avian Influenza Viruses. PLoS ONE. 2011;6:e14722. doi: 10.1371/journal.pone.0014722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dundon W.G., Milani A., Cattoli G., Capua I. Progressive truncation of the Non-Structural 1 gene of H7N1 avian influenza viruses following extensive circulation in poultry. Virus Res. 2006;119:171–176. doi: 10.1016/j.virusres.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 126.Abdelwhab E.S.M., Veits J., Breithaupt A., Gohrbandt S., Ziller M., Teifke J.P., Stech J., Mettenleiter T.C. Prevalence of the C-terminal truncations of NS1 in avian influenza A viruses and effect on virulence and replication of a highly pathogenic H7N1 virus in chickens. Virulence. 2016;7:546–557. doi: 10.1080/21505594.2016.1159367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Abdelwhab E.S.M., Veits J., Tauscher K., Ziller M., Grund C., Hassan M.K., Shaheen M., Harder T.C., Teifke J., Stech J., et al. Progressive glycosylation of the haemagglutinin of avian influenza H5N1 modulates virus replication, virulence and chicken-to-chicken transmission without significant impact on antigenic drift. J. Gen. Virol. 2016;97:3193–3204. doi: 10.1099/jgv.0.000648. [DOI] [PubMed] [Google Scholar]
- 128.Sealy J.E., Howard W.A., Molesti E., Iqbal M., Temperton N.J., Banks J., Slomka M.J., Barclay W.S., Long J.S. Amino acid substitutions in the H5N1 avian influenza haemagglutinin alter pH of fusion and receptor binding to promote a highly pathogenic phenotype in chickens. J. Gen. Virol. 2021;102:001672. doi: 10.1099/jgv.0.001672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.DuBois R.M., Zaraket H., Reddivari M., Heath R.J., White S.W., Russell C.J. Acid Stability of the Hemagglutinin Protein Regulates H5N1 Influenza Virus Pathogenicity. PLOS Pathog. 2011;7:e1002398. doi: 10.1371/journal.ppat.1002398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Reed M.L., Bridges O.A., Seiler P., Kim J.-K., Yen H.-L., Salomon R., Govorkova E.A., Webster R.G., Russell C.J. The pH of Activation of the Hemagglutinin Protein Regulates H5N1 Influenza Virus Pathogenicity and Transmissibility in Ducks. J. Virol. 2010;84:1527–1535. doi: 10.1128/JVI.02069-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Garten W., Braden C., Arendt A., Peitsch C., Baron J., Lu Y., Pawletko K., Hardes K., Steinmetzer T., Böttcher-Friebertshäuser E. Influenza virus activating host proteases: Identification, localization and inhibitors as potential therapeutics. Eur. J. Cell Biol. 2015;94:375–383. doi: 10.1016/j.ejcb.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 132.Galloway S.E., Reed M.L., Russell C.J., Steinhauer D.A. Influenza HA Subtypes Demonstrate Divergent Phenotypes for Cleavage Activation and pH of Fusion: Implications for Host Range and Adaptation. PLoS Pathog. 2013;9:e1003151. doi: 10.1371/journal.ppat.1003151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hatesuer B., Bertram S., Mehnert N., Bahgat M.M., Nelson P.S., Pöhlman S., Schughart K. Tmprss2 Is Essential for Influenza H1N1 Virus Pathogenesis in Mice. PLoS Pathog. 2013;9:e1003774. doi: 10.1371/journal.ppat.1003774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tarnow C., Engels G., Arendt A., Schwalm F., Sediri H., Preuss A., Nelson P.S., Garten W., Klenk H.D., Gabriel G., et al. TMPRSS2 Is a Host Factor That Is Essential for Pneumotropism and Pathogenicity of H7N9 Influenza A Virus in Mice. J. Virol. 2014;88:4744–4751. doi: 10.1128/JVI.03799-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sakai K., Ami Y., Tahara M., Kubota T., Anraku M., Abe M., Nakajima N., Sekizuka T., Shirato K., Suzaki Y., et al. The Host Protease TMPRSS2 Plays a Major Role in In Vivo Replication of Emerging H7N9 and Seasonal Influenza Viruses. J. Virol. 2014;88:5608–5616. doi: 10.1128/JVI.03677-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lambertz R.L.O., Gerhauser I., Nehlmeier I., Leist S.R., Kollmus H., Pöhlmann S., Schughart K. Tmprss2 knock-out mice are resistant to H10 influenza a virus pathogenesis. J. Gen. Virol. 2019;100:1073–1078. doi: 10.1099/jgv.0.001274. [DOI] [PubMed] [Google Scholar]
- 137.Lambertz R.L.O., Gerhauser I., Nehlmeier I., Gärtner S., Winkler M., Leist S.R., Kollmus H., Pöhlmann S., Schughart K. H2 influenza A virus is not pathogenic in Tmprss2 knock-out mice. Virol. J. 2020;17:56. doi: 10.1186/s12985-020-01323-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Limburg H., Harbig A., Bestle D., Stein D.A., Moulton H.M., Jaeger J., Janga H., Hardes K., Koepke J., Schulte L., et al. TMPRSS2 Is the Major Activating Protease of Influenza A Virus in Primary Human Airway Cells and Influenza B Virus in Human Type II Pneumocytes. J. Virol. 2019;93:e00649-19. doi: 10.1128/JVI.00649-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bestle D., Limburg H., Kruhl D., Harbig A., Stein D.A., Moulton H., Matrosovich M., Abdelwhab E.M., Stech J., Böttcher-Friebertshäuser E. Hemagglutinins of Avian Influenza Viruses Are Proteolytically Activated by TMPRSS2 in Human and Murine Airway Cells. J. Virol. 2021;95:e0090621. doi: 10.1128/JVI.00906-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Böttcher-Friebertshäuser E., Freuer C., Sielaff F., Schmidt S., Eickmann M., Uhlendorff J., Steinmetzer T., Klenk H.-D., Garten W. Cleavage of Influenza Virus Hemagglutinin by Airway Proteases TMPRSS2 and HAT Differs in Subcellular Localization and Susceptibility to Protease Inhibitors. J. Virol. 2010;84:5605–5614. doi: 10.1128/JVI.00140-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wysocka M., Spichalska B., Lesner A., Jaros M., Brzozowski K., Łgowska A., Rolka K. Substrate specificity and inhibitory study of human airway trypsin-like protease. Bioorg. Med. Chem. 2010;18:5504–5509. doi: 10.1016/j.bmc.2010.06.059. [DOI] [PubMed] [Google Scholar]
- 142.Baron J., Tarnow C., Mayoli-Nüssle D., Schilling E., Meyer D., Hammami M., Schwalm F., Steinmetzer T., Guan Y., Garten W., et al. Matriptase, HAT, and TMPRSS2 Activate the Hemagglutinin of H9N2 Influenza A Viruses. J. Virol. 2013;87:1811–1820. doi: 10.1128/JVI.02320-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Beaulieu A., Gravel É., Cloutier A., Marois I., Colombo É., Désilets A., Verreault C., Leduc R., Marsault É., Richter M.V. Matriptase Proteolytically Activates Influenza Virus and Promotes Multicycle Replication in the Human Airway Epithelium. J. Virol. 2013;87:4237–4251. doi: 10.1128/JVI.03005-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Hamilton B.S., Gludish D.W.J., Whittaker G.R. Cleavage Activation of the Human-Adapted Influenza Virus Subtypes by Matriptase Reveals both Subtype and Strain Specificities. J. Virol. 2012;86:10579–10586. doi: 10.1128/JVI.00306-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bertram S., Glowacka I., Blazejewska P., Soilleux E., Allen P., Danisch S., Steffen I., Choi S.-Y., Park Y., Schneider H., et al. TMPRSS2 and TMPRSS4 Facilitate Trypsin-Independent Spread of Influenza Virus in Caco-2 Cells. J. Virol. 2010;84:10016–10025. doi: 10.1128/JVI.00239-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kido H., Yokogoshi Y., Sakai K., Tashiro M., Kishino Y., Fukutomi A., Katunuma N. Isolation and characterization of a novel trypsin-like protease found in rat bronchiolar epithelial Clara cells. A possible activator of the viral fusion glycoprotein. J. Biol. Chem. 1992;267:13573–13579. doi: 10.1016/S0021-9258(18)42250-8. [DOI] [PubMed] [Google Scholar]
- 147.Murakami M., Towatari T., Ohuchi M., Shiota M., Akao M., Okumura Y., Parry M.A.A., Kido H. Mini-plasmin found in the epithelial cells of bronchioles triggers infection by broad-spectrum influenza A viruses and Sendai virus. Eur. J. Biochem. 2001;268:2847–2855. doi: 10.1046/j.1432-1327.2001.02166.x. [DOI] [PubMed] [Google Scholar]
- 148.Gotoh B., Ogasawara T., Toyoda T., Inocencio N.M., Hamaguchi M., Nagai Y. An endoprotease homologous to the blood clotting factor X as a determinant of viral tropism in chick embryo. EMBO J. 1990;9:4189–4195. doi: 10.1002/j.1460-2075.1990.tb07643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lazarowitz S.G., Goldberg A.R., Choppin P.W. Proteolytic cleavage by plasmin of the HA polypeptide of influenza virus: Host cell activation of serum plasminogen. Virology. 1973;56:172–180. doi: 10.1016/0042-6822(73)90296-1. [DOI] [PubMed] [Google Scholar]
- 150.Goto H., Kawaoka Y. A novel mechanism for the acquisition of virulence by a human influenza A virus. Proc. Natl. Acad. Sci. USA. 1998;95:10224–10228. doi: 10.1073/pnas.95.17.10224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kwon H.I., Kim Y.I., Park S.J., Kim E.H., Kim S., Si Y.J., Song M.S., Pascua P.N.Q., Govorkova E.A., Webster R.G., et al. A novel neuraminidase-dependent hemagglutinin cleavage mechanism enables the systemic spread of an H7N6 avian influenza virus. MBio. 2019;10:e02369-19. doi: 10.1128/mBio.02369-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Garten W. Characterization of Proprotein Convertases and Their Involvement in Virus Propagation. In: Böttcher-Friebertshäuser E., Garten W., Klenk H., editors. Activation of Viruses by Host Proteases. Springer; Cham, Switzerland: 2018. pp. 205–248. [Google Scholar]
- 153.Shang J., Wan Y., Luo C., Ye G., Geng Q., Auerbach A., Li F. Cell entry mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. USA. 2020;117:11727–11734. doi: 10.1073/pnas.2003138117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Horimoto T., Nakayama K., Smeekens S.P., Kawaoka Y. Proprotein-processing endoproteases PC6 and furin both activate hemagglutinin of virulent avian influenza viruses. J. Virol. 1994;68:6074–6078. doi: 10.1128/jvi.68.9.6074-6078.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Basak A., Zhong M., Munzer J.S., Chrétien M., Seidah N.G. Implication of the proprotein convertases furin, PC5 and PC7 in the cleavage of surface glycoproteins of Hong Kong, Ebola and respiratory syncytial viruses: A comparative analysis with fluorogenic peptides. Biochem. J. 2001;353:537–545. doi: 10.1042/bj3530537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Klenk H.D., Wöllert W., Rott R., Scholtissek C. Association of influenza virus proteins with cytoplasmic fractions. Virology. 1974;57:28–41. doi: 10.1016/0042-6822(74)90105-6. [DOI] [PubMed] [Google Scholar]
- 157.Vey M., Orlich M., Adler S., Klenk H.D., Rott R., Garten W. Hemagglutinin activation of pathogenic avian influenza viruses of serotype H7 requires the protease recognition motif R-X-K/R-R. Virology. 1992;188:408–413. doi: 10.1016/0042-6822(92)90775-K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Okumura Y., Takahashi E., Yano M., Ohuchi M., Daidoji T., Nakaya T., Böttcher E., Garten W., Klenk H.-D., Kido H. Novel Type II Transmembrane Serine Proteases, MSPL and TMPRSS13, Proteolytically Activate Membrane Fusion Activity of the Hemagglutinin of Highly Pathogenic Avian Influenza Viruses and Induce Their Multicycle Replication. J. Virol. 2010;84:5089–5096. doi: 10.1128/JVI.02605-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Feldmann A., Schäfer M.K.-H., Garten W., Klenk H.-D. Targeted Infection of Endothelial Cells by Avian Influenza Virus A/FPV/Rostock/34 (H7N1) in Chicken Embryos. J. Virol. 2000;74:8018–8027. doi: 10.1128/JVI.74.17.8018-8027.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Luczo J.M., Stambas J., Durr P.A., Michalski W.P., Bingham J. Molecular pathogenesis of H5 highly pathogenic avian influenza: The role of the haemagglutinin cleavage site motif. Rev. Med. Virol. 2015;25:406–430. doi: 10.1002/rmv.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Duckert P., Brunak S., Blom N. Prediction of proprotein convertase cleavage sites. Protein Eng. Des. Sel. 2004;17:107–112. doi: 10.1093/protein/gzh013. [DOI] [PubMed] [Google Scholar]
- 162.Tian S. A 20 Residues Motif Delineates the Furin Cleavage Site and its Physical Properties May Influence Viral Fusion. Biochem. Insights. 2009;2:9–20. doi: 10.4137/BCI.S2049. [DOI] [Google Scholar]
- 163.Kawaoka Y., Webster R.G. Sequence requirements for cleavage activation of influenza virus hemagglutinin expressed in mammalian cells. Proc. Natl. Acad. Sci. USA. 1988;85:324–328. doi: 10.1073/pnas.85.2.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Orlich M., Gottwald H., Rott R. Nonhomologous recombination between the hemagglutinin gene and the nucleoprotein gene of an influenza virus. Virology. 1994;204:462–465. doi: 10.1006/viro.1994.1555. [DOI] [PubMed] [Google Scholar]
- 165.Luczo J.M., Tachedjian M., Harper J.A., Payne J.S., Butler J.M., Sapats S.I., Lowther S.L., Michalski W.P., Stambas J., Bingham J. Evolution of high pathogenicity of H5 avian influenza virus: Haemagglutinin cleavage site selection of reverse-genetics mutants during passage in chickens. Sci. Rep. 2018;8:11518. doi: 10.1038/s41598-018-29944-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Lee C.W., Lee Y.J., Senne D.A., Suarez D.L. Pathogenic potential of North American H7N2 avian influenza virus: A mutagenesis study using reverse genetics. Virology. 2006;353:388–395. doi: 10.1016/j.virol.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 167.Morsy J., Garten W., Rott R. Activation of an influenza virus A/turkey/Oregon/71 HA insertion variant by the subtilisin-like endoprotease furin. Virology. 1994;202:988–991. doi: 10.1006/viro.1994.1424. [DOI] [PubMed] [Google Scholar]
- 168.Hamilton B.S., Sun X., Chung C., Whittaker G.R. Acquisition of a novel eleven amino acid insertion directly N-terminal to a tetrabasic cleavage site confers intracellular cleavage of an H7N7 influenza virus hemagglutinin. Virology. 2012;434:88–95. doi: 10.1016/j.virol.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Londt B.Z., Banks J., Alexander D.J. Highly pathogenic avian influenza viruses with low virulence for chickens in in vivo tests. Avian Pathol. 2007;36:347–350. doi: 10.1080/03079450701589134. [DOI] [PubMed] [Google Scholar]
- 170.Kawaoka Y., Naeve C.W., Webster R.G. Is virulence of H5N2 influenza viruses in chickens associated with loss of carbohydrate from the hemagglutinin? Virology. 1984;139:303–316. doi: 10.1016/0042-6822(84)90376-3. [DOI] [PubMed] [Google Scholar]
- 171.Kawaoka Y., Webster R.G. Interplay between carbohydrate in the stalk and the length of the connecting peptide determines the cleavability of influenza virus hemagglutinin. J. Virol. 1989;63:3296–3300. doi: 10.1128/jvi.63.8.3296-3300.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ohuchi M., Orlich M., Ohuchi R., Simpson B.E.J., Garten W., Klenk H.D., Rott R. Mutations at the cleavage site of the hemagglutinin alter the pathogenicity of influenza virus a/chick/penn/83 (H5N2) Virology. 1989;168:274–280. doi: 10.1016/0042-6822(89)90267-5. [DOI] [PubMed] [Google Scholar]
- 173.Soda K., Asakura S., Okamatsu M., Sakoda Y., Kida H. H9N2 influenza virus acquires intravenous pathogenicity on the introduction of a pair of di-basic amino acid residues at the cleavage site of the hemagglutinin and consecutive passages in chickens. Virol. J. 2011;8:64. doi: 10.1186/1743-422X-8-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Cheng M.-C., Soda K., Lee M.-S., Lee S.-H., Sakoda Y., Kida H., Wang C.-H. Isolation and Characterization of Potentially Pathogenic H5N2 Influenza Virus from a Chicken in Taiwan in 2008. Source Avian Dis. 2010;54:885–893. doi: 10.1637/9208-120609-Reg.1. [DOI] [PubMed] [Google Scholar]
- 175.Soda K., Cheng M.C., Yoshida H., Endo M., Lee S.H., Okamatsu M., Sakoda Y., Wang C.H., Kida H. A low pathogenic H5N2 influenza virus isolated in Taiwan acquired high Pathogenicity by consecutive passages in chickens. J. Vet. Med. Sci. 2011;73:767–772. doi: 10.1292/jvms.10-0532. [DOI] [PubMed] [Google Scholar]
- 176.Brown I., Abolnik C., Garcia-Garcia J., McCullough S., Swayne D.E., Cattoli G. High-pathogenicity avian influenza outbreaks since 2008, excluding multi-continental panzootic of H5 Goose/Guangdong-lineage viruses. In: Swayne D.E., editor. Animal Influenza. John Wiley & Sons, Inc.; Hoboken, NJ, USA: 2016. pp. 248–270. [Google Scholar]
- 177.Gischke M., Ulrich R., Fatola O.I., Scheibner D., Salaheldin A.H., Crossley B., Böttcher-Friebertshäuser E., Veits J., Mettenleiter T.C., Abdelwhab E.M. Insertion of basic amino acids in the hemagglutinin cleavage site of H4N2 avian influenza virus (AIV)—reduced virus fitness in chickens is restored by reassortment with highly pathogenic H5N1 AIV. Int. J. Mol. Sci. 2020;21:2353. doi: 10.3390/ijms21072353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Sun Y., Sun S., Ma J., Tan Y., Du L., Shen Y., Mu Q., Pu J., Lin D., Liu J. Identification and characterization of avian-origin H3N2 canine influenza viruses in northern China during 2009–2010. Virology. 2013;435:301–307. doi: 10.1016/j.virol.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 179.Tse L.V., Hamilton A.M., Friling T., Whittaker G.R. A Novel Activation Mechanism of Avian Influenza Virus H9N2 by Furin. J. Virol. 2014;88:1673–1683. doi: 10.1128/JVI.02648-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Zhang J., Ma K., Li B., Chen Y., Qiu Z., Xing J., Huang J., Hu C., Huang Y., Li H., et al. A risk marker of tribasic hemagglutinin cleavage site in influenza A (H9N2) virus. Commun. Biol. 2021;4:71. doi: 10.1038/s42003-020-01589-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Parvin R., Schinkoethe J., Grund C., Ulrich R., Bönte F., Behr K.P., Voss M., Samad M.A., Hassan K.E., Luttermann C., et al. Comparison of pathogenicity of subtype H9 avian influenza wild-type viruses from a wide geographic origin expressing mono-, di-, or tri-basic hemagglutinin cleavage sites. Vet. Res. 2020;51:48. doi: 10.1186/s13567-020-00771-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Gischke M., Bagato O., Breithaupt A., Scheibner D., Blaurock C., Vallbracht M., Karger A., Crossley B., Veits J., Böttcher-Friebertshäuser E., et al. The role of glycosylation in the N-terminus of the hemagglutinin of a unique H4N2 with a natural polybasic cleavage site in virus fitness in vitro and in vivo. Virulence. 2021;12:666–678. doi: 10.1080/21505594.2021.1881344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Funk M., de Bruin A.C.M., Spronken M.I., Gultyaev A.P., Richard M. In silico analyses of the role of codon usage in H5 and H7 hemagglutinins in highly pathogenic avian influenza genesis. Viruses. 2022;14:1352. doi: 10.3390/v14071352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Gu M., Xu L., Wang X., Liu X. Current situation of H9N2 subtype avian influenza in China. Vet. Res. 2017;48:1–10. doi: 10.1186/s13567-017-0453-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Veits J., Weber S., Stech O., Breithaupt A., Gräber M., Gohrbandt S., Bogs J., Hundt J., Teifke J.P., Mettenleiter T.C., et al. Avian influenza virus hemagglutinins H2, H4, H8, and H14 support a highly pathogenic phenotype. Proc. Natl. Acad. Sci. USA. 2012;109:2579–2584. doi: 10.1073/pnas.1109397109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Gohrbandt S., Veits J., Breithaupt A., Hundt J., Teifke J.P., Stech O., Mettenleiter T.C., Stech J. H9 avian influenza reassortant with engineered polybasic cleavage site displays a highly pathogenic phenotype in chicken. J. Gen. Virol. 2011;92:1843–1853. doi: 10.1099/vir.0.031591-0. [DOI] [PubMed] [Google Scholar]
- 187.Munster V.J., Schrauwen E.J.A., de Wit E., van den Brand J.M.A., Bestebroer T.M., Herfst S., Rimmelzwaan G.F., Osterhaus A.D.M.E., Fouchier R.A.M. Insertion of a Multibasic Cleavage Motif into the Hemagglutinin of a Low-Pathogenic Avian Influenza H6N1 Virus Induces a Highly Pathogenic Phenotype. J. Virol. 2010;84:7953–7960. doi: 10.1128/JVI.00449-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Ohuchi R., Ohuchi M., Garten W., Klenk H.D. Human influenza virus hemagglutinin with high sensitivity to proteolytic activation. J. Virol. 1991;65:3530–3537. doi: 10.1128/jvi.65.7.3530-3537.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kawaoka Y. Structural features influencing hemagglutinin cleavability in a human influenza A virus. J. Virol. 1991;65:1195–1201. doi: 10.1128/jvi.65.3.1195-1201.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Stech O., Veits J., Weber S., Deckers D., Schröer D., Vahlenkamp T.W., Breithaupt A., Teifke J., Mettenleiter T.C., Stech J. Acquisition of a Polybasic Hemagglutinin Cleavage Site by a Low-Pathogenic Avian Influenza Virus Is Not Sufficient for Immediate Transformation into a Highly Pathogenic Strain. J. Virol. 2009;83:5864–5868. doi: 10.1128/JVI.02649-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Schrauwen E.J.A., Bestebroer T.M., Munster V.J., de Wit E., Herfst S., Rimmelzwaan G.F., Osterhaus A.D.M.E., Fouchier R.A.M. Insertion of a multibasic cleavage site in the haemagglutinin of human influenza H3N2 virus does not increase pathogenicity in ferrets. J. Gen. Virol. 2011;92:1410–1415. doi: 10.1099/vir.0.030379-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Suarez D.L. Influenza A virus. In: Swayne D.E., editor. Animal Influenza. John Wiley and Sons, Inc.; Hoboken, NJ, USA: 2017. p. 17. [Google Scholar]
- 193.Perdue M., Crawford J., Garcia M., Latimer J., Swayne D. Occurrence and Possible Mechanisms of Cleavage-Site Insertions in the Avian Influenza Hemagglutinin Gene. Avian Dis. 2003;47:182–193. [Google Scholar]
- 194.Gultyaev A.P., Richard M., Spronken M.I., Olsthoorn R.C.L., Fouchier R.A.M. Conserved structural RNA domains in regions coding for cleavage site motifs in hemagglutinin genes of influenza viruses. Virus Evol. 2019;5:vez034. doi: 10.1093/ve/vez034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Gultyaev A.P., Spronken M.I., Funk M., Fouchier R.A.M., Richard M. Insertions of codons encoding basic amino acids in H7 hemagglutinins of influenza A viruses occur by recombination with RNA at hotspots near snoRNA binding sites. RNA. 2021;27:123–132. doi: 10.1261/rna.077495.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Ito T., Goto H., Yamamoto E., Tanaka H., Takeuchi M., Kuwayama M., Kawaoka Y., Otsuki K. Generation of a Highly Pathogenic Avian Influenza A Virus from an Avirulent Field Isolate by Passaging in Chickens. J. Virol. 2001;75:4439. doi: 10.1128/JVI.75.9.4439-4443.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Abolnik C. Evolution of H5 highly pathogenic avian influenza: Sequence data indicate stepwise changes in the cleavage site. Arch. Virol. 2017;162:2219–2230. doi: 10.1007/s00705-017-3337-x. [DOI] [PubMed] [Google Scholar]
- 198.Sanjuán R., Domingo-Calap P. Mechanisms of viral mutation. Cell. Mol. Life Sci. 2016;73:4433–4448. doi: 10.1007/s00018-016-2299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Metreveli G., Zohari S., Ejdersund A., Berg M. Phylogenetic Analysis of the Hemagglutinin Gene of Low Pathogenic Avian Influenza Virus H7N7 Strains in Mallards in Northern Europe. Avian Dis. 2010;54:453–456. doi: 10.1637/8691-031309-ResNote.1. [DOI] [PubMed] [Google Scholar]
- 200.Perdue M.L., García M., Senne D., Fraire M. Virulence-associated sequence duplication at the hemagglutinin cleavage site of avian influenza viruses. Virus Res. 1997;49:173–186. doi: 10.1016/S0168-1702(97)01468-8. [DOI] [PubMed] [Google Scholar]
- 201.Wandzik J.M., Kouba T., Karuppasamy M., Pflug A., Drncova P., Provaznik J., Azevedo N., Cusack S. A Structure-Based Model for the Complete Transcription Cycle of Influenza Polymerase. Cell. 2020;181:877–893.e21. doi: 10.1016/j.cell.2020.03.061. [DOI] [PubMed] [Google Scholar]
- 202.Poon L.L.M., Pritlove D.C., Fodor E., Brownlee G.G. Direct evidence that the poly(A) tail of influenza A virus mRNA is synthesized by reiterative copying of a U track in the virion RNA template. J. Virol. 1999;73:3473–3476. doi: 10.1128/JVI.73.4.3473-3476.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Nao N., Yamagishi J., Miyamoto H., Igarashi M., Manzoor R., Ohnuma A., Tsuda Y., Furuyama W., Shigeno A., Kajihara M., et al. Genetic predisposition to acquire a polybasic cleavage site for highly pathogenic avian influenza virus hemagglutinin. MBio. 2017;8:e02298-16. doi: 10.1128/mBio.02298-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Brugh M., Perdue M.L. Emergence of Highly Pathogenic Virus during Selective Chicken Passage of the Prototype Mildly Pathogenic Chicken/Pennsylvania/83 (H5N2) Influenza Virus. Avian Dis. 1991;35:824–833. doi: 10.2307/1591616. [DOI] [PubMed] [Google Scholar]
- 205.Horimoto T., Kawaoka Y. Molecular Changes in virulent mutants arising from avirulent avian influenza viruses during Replication in 14-day-old embryonated eggs. Virology. 1995;206:755–759. doi: 10.1016/S0042-6822(95)80004-2. [DOI] [PubMed] [Google Scholar]
- 206.Perdue M.L., Garcia M., Beck J., Brugh M., Swayne D.E. An arg-lys insertion at the hemagglutinin cleavage site of an H5N2 avian influenza isolate. Virus Genes. 1996;12:77–84. doi: 10.1007/BF00370003. [DOI] [PubMed] [Google Scholar]
- 207.Silvano F.D., Yoshikawa M., Shimada A., Otsuki K., Umemura T. Enhanced Neuropathogenicity of Avian Influenza A Virus by Passages through Air Sac and Brain of Chicks. J. Vet. Med. Sci. 1997;59:143–148. doi: 10.1292/jvms.59.143. [DOI] [PubMed] [Google Scholar]
- 208.Shinya K., Awakura T., Shimada A., Silvano F.D., Umemura T., Otsuki K. Pathogenesis of pancreatic atrophy by avian influenza a virus infection. Avian Pathol. 1995;24:623–632. doi: 10.1080/03079459508419102. [DOI] [PubMed] [Google Scholar]
- 209.Brugh M., Beck J.R. Recovery of Minority Subpopulations of Highly Pathogenic Avian Influenza Virus. Avian Dis. 2003;47:166–174. [Google Scholar]
- 210.Laleye A.T., Abolnik C. Emergence of highly pathogenic H5N2 and H7N1 influenza A viruses from low pathogenic precursors by serial passage in ovo. PLoS ONE. 2020;15:e0240290. doi: 10.1371/journal.pone.0240290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Seekings A.H., Howard W.A., Nuñéz A., Slomka M.J., Banyard A.C., Hicks D., Ellis R.J., Nuñéz-García J., Hartgroves L.C., Barclay W.S., et al. The emergence of H7N7 highly pathogenic avian influenza virus from low pathogenicity avian influenza virus using an in ovo embryo culture model. Viruses. 2020;12:920. doi: 10.3390/v12090920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Kida Y., Okuya K., Saito T., Yamagishi J., Ohnuma A., Hattori T., Miyamoto H., Manzoor R., Yoshida R., Nao N., et al. Structural Requirements in the Hemagglutinin Cleavage Site-Coding RNA Region for the Generation of Highly Pathogenic Avian Influenza Virus. Pathogens. 2021;10:1597. doi: 10.3390/pathogens10121597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Brugh M. Highly pathogenic virus recovered from chickens infected with mildly pathogenic 1986 isolates of H5N2 avian influenza virus. Avian Dis. 1988;32:695–703. doi: 10.2307/1590987. [DOI] [PubMed] [Google Scholar]
- 214.Khatchikian D., Orlich M., Rott R. Increased viral pathogenicity after insertion of a 28S ribosomal RNA sequence into the haemagglutinin gene of an influenza virus. Nature. 1989;340:156–157. doi: 10.1038/340156a0. [DOI] [PubMed] [Google Scholar]
- 215.Orlich M., Khatchikian D., Teigler A., Rott R. Structural variation occurring in the hemagglutinin of influenza virus A/turkey/Oregon/71 during adaptation to different cell types. Virology. 1990;176:531–538. doi: 10.1016/0042-6822(90)90023-K. [DOI] [PubMed] [Google Scholar]
- 216.Li S.Q., Orlich M., Rott R. Generation of seal influenza virus variants pathogenic for chickens, because of hemagglutinin cleavage site changes. J. Virol. 1990;64:3297–3303. doi: 10.1128/jvi.64.7.3297-3303.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Williams G.D., Townsend D., Wylie K.M., Kim P.J., Amarasinghe G.K., Kutluay S.B., Boon A.C.M. Nucleotide resolution mapping of influenza A virus nucleoprotein-RNA interactions reveals RNA features required for replication. Nat. Commun. 2018;9:465. doi: 10.1038/s41467-018-02886-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Le Sage V., Nanni A.V., Bhagwat A.R., Snyder D.J., Cooper V.S., Lakdawala S.S., Lee N. Non-uniform and non-random binding of nucleoprotein to influenza A and B viral RNA. Viruses. 2018;10:522. doi: 10.3390/v10100522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Gultyaev A.P., Spronken M.I., Richard M., Schrauwen E.J.A., Olsthoorn R.C.L., Fouchier R.A.M. Subtype-specific structural constraints in the evolution of influenza A virus hemagglutinin genes. Sci. Rep. 2016;6:38892. doi: 10.1038/srep38892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Dupré G., Hoede C., Figueroa T., Bessière P., Bertagnoli S., Ducatez M., Gaspin C., Volmer R. Phylodynamic study of the conserved RNA structure encompassing the hemagglutinin cleavage site encoding region of H5 and H7 low pathogenic avian influenza viruses. Virus Evol. 2021;7:veab093. doi: 10.1093/ve/veab093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Kouba T., Drncová P., Cusack S. Structural snapshots of actively transcribing influenza polymerase. Nat. Struct. Mol. Biol. 2019;26:460–470. doi: 10.1038/s41594-019-0232-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Banks J., Speidel E.S., Moore E., Plowright L., Piccirillo A., Capua I., Cordioli P., Fioretti A., Alexander D.J. Changes in the haemagglutinin and the neuraminidase genes prior to the emergence of highly pathogenic H7N1 avian influenza viruses in Italy. Arch Virol. 2001;146:963–973. doi: 10.1007/s007050170128. [DOI] [PubMed] [Google Scholar]
- 223.Bratkovič T., Bozič J., Rogelj B. Functional diversity of small nucleolar RNAs. Nucleic Acids Res. 2020;48:1627–1651. doi: 10.1093/nar/gkz1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.