Abstract
The purpose of this case report was to describe chiropractic management of acute lumbar disc herniation in a patient with a large abdominal aortic aneurysm. A 72-year-old male patient presented with low back pain and right lower leg numbness for 12 months. A review of full-spine X-ray and lumbar MRI revealed moderate spondylosis at L2-5, moderate lumbar scoliosis, and a 7.15 cm abdominal aortic aneurysm (AAA). Given the minimum 2-weeks of referral waiting time to receive treatment for AAA, the patient received chiropractic treatment with a hybrid rehabilitation to address the disc herniation causing severe physical disability. Through the treatments, the patient's pain was significantly alleviated with careful consideration of potential risk factors associated with AAA. In addition, the acute disc herniation was successfully managed by a series of chiropractic treatments before and after the operation for AAA. This case supports that low back pain in patients with AAA can be managed by manual therapy, in contrast to a widespread belief that manual therapy is contraindicated in AAA. More case reports of AAA patients with low back pain are warranted to assess the effectiveness and safety of manual therapy along with surgical treatment for AAA.
Keywords: AAA, chiropractic therapy, abdominal aortic aneurysms, patient-centric
ABBREVIATIONS: AAA – Abdominal aortic aneurysm, MRI – Magnetic resonance image, NSAIDs – Nonsteroidal anti-inflammatory drugs, CT – Computed tomography
INTRODUCTION
Abdominal aortic aneurysms (AAA) affect over 200,000 people annually only in the United States. Ultrasound screening studies revealed that 4–8% of the male geriatric population have an occult abdominal aortic aneurysm [1]. Frequently, it is identified coincidentally with other diagnostic techniques [2]. Ruptured aneurysms have a fatality rate of 50% to 95%, accounting for the 10th leading cause of death in men older than 55 [3]. AAAs can be detected during a routine abdominal physical examination in which the physician palpates the abdomen for an enlarged pulsating mass more than 3 cm in diameter [2, 4]. However, the palpation examination suffers from a low sensitivity of less than 65% [3], and approximately 30% of ruptured AAAs are misdiagnosed [3]. The geriatric population in the United States was about 16.9%, and 5% of them see chiropractors annually [5]. Thus, it is estimated that a substantial portion of geriatric patients who presented to chiropractors may also have AAA.
Spinal manipulation performed by chiropractic professionals has traditionally been regarded as a red flag in patients with AAA despite the absence of published reports showing its correlation with aortic dissection [6–8]. It has been considered that increased intraabdominal or intrathoracic pressure during spinal manipulation may increase the likelihood of dissection or rupture of the aorta. This view is challenged by the paucity of chiropractic reports on patients with AAA since the last case in 2010 [9]. As such, this report aims to detail the chiropractic care provided to a patient with large AAA and acute lumbar disc herniation without a notable secondary complication.
CASE REPORT
A 72-year-old Asian male experienced mild right wrist pain, moderate low back pain, and right lower leg numbness for 12 months. The symptoms first started as ache and constant low back pain for 2 years that slowly radiated as episodic right leg numbness for 12 months. As the symptoms had suddenly worsened over the past 2 months, the patient could walk only with a cane. He had difficulties walking for over 15 minutes and more frequent awakening at night due to back pain. The patient had a past medical history of angioplasty and gout 10 years ago, with no known trauma history. The severity of back pain was rated 9/10, which negatively impacted his quality of life and mental health. He was initially diagnosed by the family physician with sciatic pain and received treatment including NSAIDs and celecoxib (Celebrex®), which provided only temporary relief. The patient then sought chiropractic care for conservative management.
Investigation: Tophus formations were identified in bilateral hands, and lumbar scoliosis was observed with paraspinal muscle spasm. His pain was provoked by trunk extension, right bending, and right ankle inversion and eversion. The lower quarter neurological screening revealed a diminished light touch of the right ankle and feet. The spinal intervertebral restriction was identified at L4/5 and the right sacroiliac joint. His range of motion in the lumbar region was restricted by muscle spasms. The straight leg test was positive for disc herniation at 30°. He was sent to radiography in a weight-bearing position to evaluate his orthopedic conditions. To alleviate his symptoms, spinal manipulation with NYMG Scoliosis® protocol was applied to his lumbar spine, and acupuncture was administered to the paraspinal muscles. The patient had immediate relief from his symptoms.
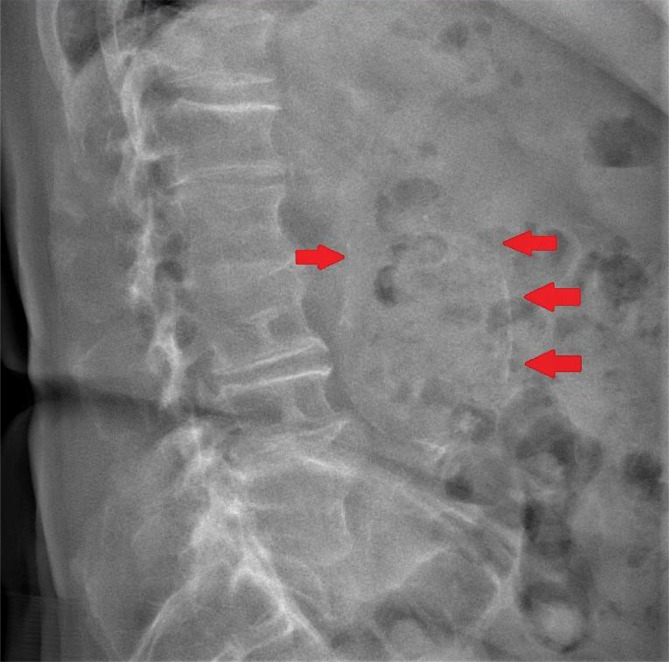
The patient described the symptoms as reduced by 20% on the 2nd visit, and his sleeping quality improved. The radiograph showed moderate spondylosis at L2-5, moderate lumbar scoliosis, and a presence of a significant calcified aorta from the L2-L5 region (Figure 1). An apparent increase in soft tissue opacity was observed over the volar aspect of the right wrist, consistently with gouty tophi deposition. With the differential diagnosis of gout, AAA, and lumbar disc herniation, the patient was arranged for a lumbar MRI and abdominal CT aortogram with the radiology department. Careful pretreatment planning was organized with the rehabilitation, radiology, and orthopedic departments. Hybrid conservative techniques, including acupuncture, chiropractic instrument adjustment technique, gua sha soft tissue treatment, joint mobilization, and preoperative physical therapy, were considered reasonable strategies for disc herniation. Any types of high-velocity spinal manipulation techniques were avoided.
Figure 1.
Lateral view identified the presence of a significant calcified aorta from the L2-L5 region.
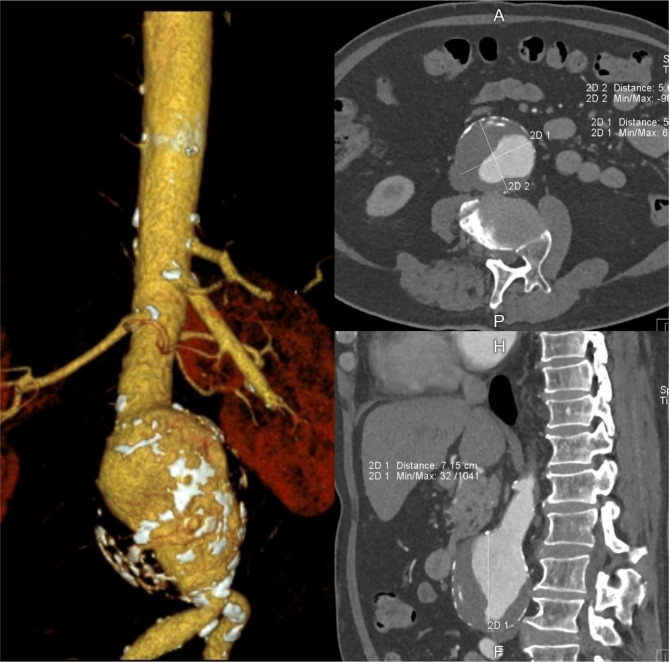
The patient received conservative intervention daily for 5 consecutive days for the management of lumbar disc herniation. On the 6th day of the clinic visit, his lumbar MRI identified disc bulging compressing on the spinal cord and cauda equina at L3/4 and L4/5 levels and impingement of right nerve roots. In addition, a 7 cm AAA was identified at L2-4 (Figure 2). The CT abdominal aortogram (Figure 3) also confirmed the measurement of 7.15 cm × 5.67 cm × 5.46 cm diameter in the diagnosis of AAA. He was immediately referred to the cardiologist.
Figure 2.
Magnetic resonance (MR) image revealed dilatation of abdominal aorta (red arrows) and marginal osteophyte formation of the lumbar vertebrae and posterior protrusion at the L3/L4 and L4/L5 levels pinching the spinal nerve extending from the spinal cord and cauda equina (red arrow).
Figure 3.
Computed tomography abdominal aortogram measured a 7.15 cm × 5.67 cm × 5.46 cm diameter abdominal aortic aneurysm.
Diagnosis: On the 7th day, he was reviewed by a cardiologist with the confirmation of lumbar disc herniation with an abdominal aortic aneurysm.
Treatment: He transferred to a vascular-surgical consultation on the 9th day and received endovascular repair at the AAA and angioplasty of two of the coronary arteries on the 14th day. At one week post-surgery, the patient started a post-operative physical therapy program with a cardiovascular fitness exercise prescription for 45 minutes at a target intensity of 60% heart rate reserve. Treatment for disc herniation and lumbar scoliosis was also administered three weeks after the surgery. The first phase of treatment aimed at regaining muscle strength and reducing back pain conservatively. Laser acupuncture and diversified chiropractic adjustment were applied 5 times a week for 2 weeks. A spinal decompression treatment by intermittent robotic traction (MID Series, WIZ Medical, Korea) was further added to the subsequent treatments to restore nerve dysfunction. The frequency of treatments was reduced to 3 times a week for 3 months.
Outcome: Under conservative management, the patient reported 50% relief of musculoskeletal symptoms before the operation. After the operation, the back pain and motor strength started to recover following the second week of post-surgical rehabilitation. The patient continued his treatment once a week, which focused on restoring lumbar disc herniation for an additional 3 months. His sensorimotor dysfunction was mostly resolved after treatment. He was symptom-free and was able to return to normal daily activity. The Oswestry Disability Index was reduced from 68% to 2%. At 12th month follow-up, the patient remained healthy and returned to his weekly hiking hobby. No adverse event was reported.
DISCUSSION
According to the literature study on PubMed, the last chiropractic case report of patients with AAAs was dated 11 years ago, and the published reports are mostly focused on the physical examinations without manual therapy when patients need surgical treatment for AAA [6, 8, 10–12]. As AAA is associated with 91% of low back pain [12], it is important to understand the procedures of co-management of back pain and AAA through multidisciplinary approaches. This is the first case report describing the clinical management of low back pain with co-management procedures for AAA from a patient-centric perspective. Most clinicians ignored the patient's original chief complaints when the AAA was identified. Most reports failed to describe the differentiated diagnosis with advanced imaging systems, collaborating treatment options with the surgical team, and following up on postoperative rehabilitation as the primary care physicians. Consistently with the outcome in our case, pre-operative physical therapy reported positive effects in reducing post-AAA surgery complication risks [13]. Thus, conservative treatments may need to be considered prior to surgical treatment.
Post-surgery care is important for patients with AAA and low back pain. For example, cardiovascular exercise has positive effects in reducing cardiovascular risk and suppression of AAA diameter progression [14]. Given the biomechanical impacts in various aspects, chiropractic manipulation manages complicated lumbar disc herniation even after the AAA treatment [15–17]. In addition, a combination with acupuncture therapy may provide an improved outcome [18], consistently with the present case. This case also suggests that conservative treatments for low back pain can be performed for patients with AAA without causing any complications, consistently with the lack of literature showing any adverse effect of chiropractic spinal manipulation on AAA [19]. Although it contrasts with the traditional belief that AAA is a contraindication to spinal manipulation [7, 8], the current evidence supports that conservative management is sometimes effective in managing patients with surgical advice [20].
CONCLUSION
This case supports that low back pain in patients with AAA can be managed by conservative treatment options without any complications. More case reports of AAA patients with low back pain are warranted to assess the effectiveness and safety of manual therapy along with surgical treatment for AAA.
ACKNOWLEDGEMENTS
Conflict of interest
The author declares that there is no conflict of interest.
Consent to participate
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Data availability
Further data is available from the corresponding author on reasonable request.
Author contribution statement
EC contributed the case information, drafted the manuscript, and prepared the figures. The author has read and approved the final manuscript.
References
- 1.Singh K, Bønaa KH, Jacobsen BK, Bjørk L, Solberg S. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study : The Tromsø Study. Am J Epidemiol. 2001 Aug 1;154(3):236–44. doi: 10.1093/aje/154.3.236. [DOI] [PubMed] [Google Scholar]
- 2.Porter RS, Kaplan JL. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2011. The Merck manual of diagnosis and therapy. [Google Scholar]
- 3.Gibbons RC, Singh G, Donuru A, Young M. StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. Abdominal Aortic Aneurysm Imaging 2021 Aug,13. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470237/ [PubMed] [Google Scholar]
- 4.Aggarwal S, Qamar A, Sharma V, Sharma A. Abdominal aortic aneurysm: A comprehensive review. Exp Clin Cardiol. 2011 Spring;16(1):11–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Dougherty PE, Hawk C, Weiner DK, Gleberzon B, et al. The role of chiropractic care in older adults. Chiropr Man Therap. 2012 Feb 21;20(1):3. doi: 10.1186/2045-709X-20-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hadida C, Rajwani M. Abdominal aortic aneurysms: case report. J Can Chiropr Assoc. 1998;42(4):216–221. [Google Scholar]
- 7.Harger BL. Abdominal aortic aneurysm: a case report. ACA J Chiropr. 1993;1993(Dec):69–71. [Google Scholar]
- 8.Weston JP. Chiropractic management of abdominal aortic aneurysm: a case report. J Can Chiropr Assoc. 1995;39(2):75–79. [Google Scholar]
- 9.Tuling JR, Crowther ET, McCord P. Clinical considerations in the chiropractic management of the patient with Marfan syndrome. J Manipulative Physiol Ther. 2000 Sep;23(7):498–502. doi: 10.1067/mmt.2000.108815. [DOI] [PubMed] [Google Scholar]
- 10.Patel SN, Kettner NW. Abdominal aortic aneurysm presenting as back pain to a chiropractic clinic: a case report. J Manipulative Physiol Ther. 2006 Jun;29(5):409.e1-7. doi: 10.1016/j.jmpt.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 11.González Gay M, Alonso Pérez M, Adeba Vallina E. Rev Esp Cir Ortop Traumatol. 6. Vol. 56. Spanish: 2012. Nov-Dec, Erosión vertebral en aneurismas de aorta abdominal como causa de dolor lumbar crónico Serie de 5 casos [Vertebral erosions in abdominal aortic aneurysms as a cause of chronic low back pain. A series of 5 cases] pp. 478–81. [DOI] [PubMed] [Google Scholar]
- 12.García-Macero RA, Balbuena Domínguez JC, Fernández-Castañón Martínez E, Herbello Rodríguez A. Rehabilitacion (Madr) Vol. 6. Spanish: 2021. Sep, Dolor lumbar y aneurisma de aorta abdominal: red flags [Low back pain and abdominal aortic aneurysm: Red flags] pp. S0048–7120(21)00076-1. [DOI] [PubMed] [Google Scholar]
- 13.Hillegass EA. 3rd ed. Vol. 72. St. Louis, MO: Elsevier/Saunders; 2011. Essentials of Cardiopulmonary Physical Therapy; pp. 397–398. [Google Scholar]
- 14.Myers J, McElrath M, Jaffe A, Smith K, et al. A randomized trial of exercise training in abdominal aortic aneurysm disease. Med Sci Sports Exerc. 2014 Jan;46(1):2–9. doi: 10.1249/MSS.0b013e3182a088b8. [DOI] [PubMed] [Google Scholar]
- 15.Chu ECP, Chan AKC, Lin AFC. Pitting oedema in a polio survivor with lumbar radiculopathy complicated disc herniation. J Family Med Prim Care. 2019 May;8(5):1765–1768. doi: 10.4103/jfmpc.jfmpc_254_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chu ECP. Taming of the Testicular Pain Complicating Lumbar Disc Herniation With Spinal Manipulation. Am J Mens Health. 2020 Jul-Aug;14(4):1557988320949358. doi: 10.1177/1557988320949358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pu Chu EC, Chakkaravarthy DM, Huang KHK, Ho VWK, et al. Changes in radiographic parameters following chiropractic treatment in 10 patients with adolescent idiopathic scoliosis: A retrospective chart review. Clin Pract. 2020 Sep 4;10(3):1258. doi: 10.4081/cp.2020.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang P, Chen C, Zhang QH, Sun GD, et al. Retraction of lumbar disc herniation achieved by noninvasive techniques: A case report. World J Clin Cases. 2021;9(27):8082–8089. doi: 10.12998/wjcc.v9.i27.8082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neff SM, Okamoto CS. Chiropractic Management of a Patient With Thoracic Pain and a Stable Thoracic Aortic Aneurysm: A Case Report. J Chiropr Med. 2017;16(1):78–82. doi: 10.1016/j.jcm.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chu EC. Improvement of quality of life by conservative management of thoracic scoliosis at 172°: a case report. J Med Life. 2022 Jan;15(1):144–148. doi: 10.25122/jml-2021-0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Further data is available from the corresponding author on reasonable request.