Abstract
Objective:
The aim of this study was to retrospectively determine the prevalence of severe external root resorption in maxillary incisors during fixed orthodontic treatment and to evaluate the possible predisposing factors.
Methods:
The treatment records of 7000 patients who had been treated between 1990 and 2019 at the Department of Orthodontics Faculty of Dentistry Marmara University were examined, and a total of 120 patients with severe root resorption in at least one of their upper incisors were identified. The following data were retrieved from the patients' records and radiographs: gender, root morphology, overjet, overbite, treatment modality (extraction, non-extraction), treatment duration, buccal and palatal alveolar bone thickness for the maxillary incisors, and amount of movement of the incisal root apices and incisal edges. These data from a group of 90 patients with severe root resorption were compared with the data from a control group of 90 patients with minimal root resorption. The Chi-square test, the Mann–Whitney U-test, and the independent t-test were used for statistical analysis.
Results:
The prevalence of severe external root resorption was 3.23%, and the results demonstrated significant difference between the groups for the variables of treatment modality (extractions), treatment duration, thickness of the alveolar bone, and amount of incisor movement at the end of the treatment.
Conclusion:
It can be concluded that extractions, increased treatment duration, thin alveolar bone, and excessive incisor movement represent risk factors for severe root resorption in maxillary incisors following orthodontic treatment.
Keywords: Orthodontics, external root resorption, maxillary incisors, root morphology, bone thickness
Main Points
Severe EARR is multifactorial in origin.
Treatment duration, treatment type, alveolar bone thickness, and amount of orthodontic movement play a major role in the development of severe EARR.
These factors should be taken into consideration when planning orthodontic treatment.
Introduction
External apical root resorption (EARR) is an unwanted side effect following orthodontic treatment, as a result of induced tooth movement.1,2 However, EARR can be avoided, and its severity and the number of affected teeth can be reduced.3 The diagnosis of EARR is generally done by using periapical and panoramic radiographs,4 and it is usually asymptomatic. The function and retention of the affected teeth are at risk only if severe resorption causes significant root loss.5,6
Malmgren et al.7 proposed a scoring system to classify the teeth, to assess EARR severity. It is a visual qualitative approach that is relatively subjective.
The root resorption classification scores, according to Malmgren et al.,7 are as follows: score 0, absence of root resorption; score 1, irregularity in the apical root contour; score 2, resorption of up to 2 mm; score 3, resorption from 2 mm up to 1/3 of the root; and score 4, loss greater than 1/3 of the root length.
The etiology and mechanisms of action of EARR with an orthodontic origin are not fully understood; many studies have reported a multifactorial etiology involving both individual factors (age, individual susceptibility, systemic disease, genetic factors, root morphology, etc.) and other factors associated with orthodontic treatment (duration, type of appliance, extractions, magnitude of applied force, range of movement, etc.).8,9 Studies have revealed that maxillary anterior teeth are more likely to develop severe EARR than other teeth.10
The aim of this retrospective study was to determine the prevalence and the predisposing factors of severe EARR in the maxillary incisors in patients treated at Marmara University, Faculty of Dentistry, Department of Orthodontics. The findings of this study will be useful for a self-assessment of the outcomes of treatments provided in our department and for the orthodontic community, and to show the extent to which we were able to maintain biological integrity of the dentition when striving for optimal orthodontic outcomes. By helping practitioners to determine potential risk factors, we will be able to plan the orthodontic treatment by taking into consideration the predisposing factors related to the development of EARR.
Methods
Ethical Approval
The Ethical Committee of the Institute of Health Sciences, Marmara University approved of this retrospective study, which assessed the records of 7000 patients from the archives of Marmara University, Faculty of Dentistry, Department of Orthodontics (Protocol number: 2019-326).
Patient Selection
The treatment files of 7000 patients who had been treated in Marmara University between 1990 and 2019 were examined, considering the following:
Inclusion criteria:
Completed fixed orthodontic treatment with 0.018”-slot edgewise multibracket system
Presence of pretreatment and post-treatment radiographic films (panoramic and cephalometric radiographs)
Completed root development of the maxillary incisors before fixed orthodontic treatment
No visible EARR in the maxillary incisors before the treatment
Root resorption scored 4 according to Malmgren et al.7 in one or more of the maxillary incisors following fixed orthodontic treatment
The exclusion criteria were:
Radiographs with low quality
Teeth that had been endodontically treated
Incompletely developed root apex
Mild or moderate EARR of the incisors
Patients with missing radiographic records
Patients with history of trauma to the incisors before the start of the treatment
Patients treated with removable appliances
Patients treated with a surgical approach
Patients presented with cleft lip/palate
Patients presented with systemic conditions like asthma, and patients with chronic use of medications affecting orthodontic tooth movement, such as bisphosphonate
Patients presented with history of parafunctional habits
After scanning of all patients' archives, the total number of subjects with severe EARR anteriorly was found to be 120, while mild/moderate EARR was found in 3595 of the patients. Of the original sample size, 3285 subjects were excluded for the following reasons: 2316 patients with missing files, 244 patients who had been treated with removable appliances and did not go through fixed orthodontic treatment, 375 patients who had been treated by orthognathic surgical approach, and 350 patients who had presented with cleft lip/palate.
Of the patients in the study group who presented with severe EARR, a second scanning was performed for 120 patients, and 30 patients were excluded due to incomplete records, of whom 2 were patients with missing pre-orthodontic cephalometric radiographs, and 28 were patients with missing post-orthodontic cephalometric radiographs.
Once all subjects with severe EARR (score 4) were identified, a group of 90 control subjects were randomly selected among the patients identified with minimal EARR (score 1) for statistical comparisons.
Inclusion criteria for the control group:
Completed fixed orthodontic treatment with 0.018”-slot edgewise multibracket system
Presence of pretreatment and post-treatment radiographs (panoramic and cephalometric radiographs)
Completed root development of the maxillary incisors before fixed orthodontic treatment
No visible EARR in the maxillary incisors before the treatment
Root resorption scored 1 according to Malmgren et al.7 in the maxillary incisors following fixed orthodontic treatment
Exclusion criteria for the control group:
Radiographs with inferior quality
Teeth that had been endodontically treated
Incompletely developed root apex
Severe EARR of the incisors
Patients with missing radiographic records
Patients with a history of trauma to the incisors before the start of the treatment
Patients treated with removable appliances
Patients treated with surgical approach
Patients presented with cleft lip/palate
Patients presented with systemic conditions like asthma, and patients presented with chronic use of medications affecting orthodontic tooth movement, such as bisphosphonate
Patients presented with history of parafunctional habits
The final sample consisted of a study group of 90 patients and a control group of 90 patients. The gender distribution was 44 males and 46 females in the study group and 40 males and 50 females in the control group. The mean age at the beginning of orthodontic treatment in the study and control groups was 16.69 years and 15.35 years, respectively.
Treatment Protocol
Patients who presented to the clinic in Marmara University, Faculty of Dentistry, Department of Orthodontics were diagnosed, examined, and treated under supervision of the specialists and professors. Treatment started with fixed appliances of 18”-slot brackets. The initial phase, alignment of the dentition, was initiated by round NiTi wires, followed by rectangular wires. The working phase followed later, ending with stainless steel wires, and elastics were used as needed.
Data Collection
The initial archival scanning was performed by checking and evaluating the pre-operative and post-operative panoramic radiographs of the whole sample (Figure 1), and subjects who presented with severe (score 4) EARR at the end of treatment were selected.
Figure 1.

Pre-operative (above) and post-operative (below) panoramic radiographs
To determine potential predisposing factors of EARR, the following data were retrieved from the patients' files:
Gender
Root morphology
Overjet
Overbite
Treatment modality (extraction, non-extraction)
Treatment duration
Labial and palatal alveolar bone thickness in the maxillary incisor region
Amount of movement of the incisal root apices and incisal edges in both horizontal and vertical directions
Data Assessment
Root morphology was assessed on post-operative panoramic radiographs according to the classification proposed by Quintanilha et al.,11 as follows: rhomboid, triangular, dilacerated, and pipette (Figure 2).
Figure 2. A-D.
Root morphologies A, B, C, D. Triangular (A), rhomboid (B), pipette (C), and dilacerated (D) (11)
Overjet, overbite, buccal and palatal maxillary alveolar bone thickness, and amount of movement of the incisal root apices and incisal edges were assessed on cephalometric radiographs using cephalometric tracing software (Nemotec version 10.4.2, Software Nemotec S.L., Spain).
Cephalometric Analysis
Cephalometric radiographs were used to record the changes in overjet, overbite, labial and palatal maxillary alveolar bone thickness, and amount of movement of the maxillary incisors’ apices and incisal edges between pre-orthodontic treatment and post-orthodontic treatment records, between the 2 groups––the anterior EARR group and the control group. Cephalometric tracing software was used to trace all cephalometric radiographs, and the radiographs were all traced by the same examiner. The cephalometric points and planes used are shown in Figure 3, and described in Table 1.
Figure 3.
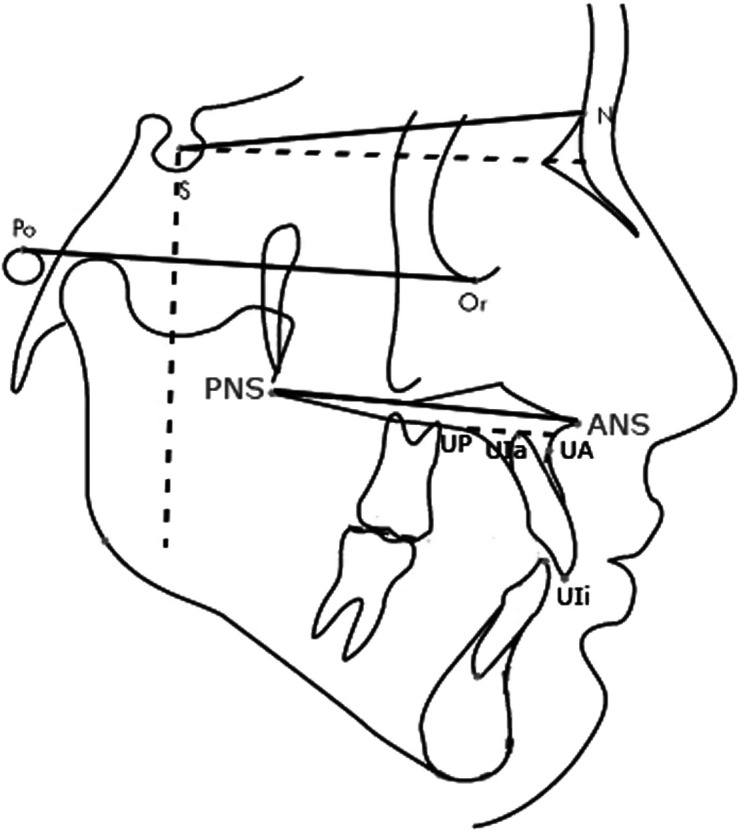
Cephalometric points and planes used
Table 1.
Cephalometric planes
| Plane | Description |
|---|---|
| SN Lines | Line crossing between sella turcica and Nasion points. |
| Palatal Plane (PP) | Plane connecting anterior nasal spine with posterior nasal spine. |
| Frankfort Horizontal Plane (FH) | Plane crossing from the Porion to the Orbitale. |
| Bone Plane | A constructed line parallel to the palatal plane passing through the apex of the root, with marking the anterior and posterior limits passing through the bone. |
| Horizontal Line | A constructed line intersecting the S point with angle of 7 degrees to SN line. |
| Vertical Line | A constructed vertical line dropped perpendicular to the horizontal line and intersecting the S point. |
Method of Measurement
Evaluations on panoramic radiographs were carried out according to Malmgren’s proposed method, which, despite being relatively subjective, has the advantage of not depending on the standardization of the radiograph.12 Calibration of both pre- and post-operative cephalometric radiographs was performed as an initial step prior to recording any measurement. Cephalometric radiographs were calibrated using the length of the middle cranial base for every patient; the growth of middle cranial base is completed in early periods and at the age of 7 years, maintaining its stability in all developmental phases.13 Two cephalometric landmarks found in the middle cranial base show high stability over the years.13,14 These points are: the lower contours of the anterior clinoid processes intersecting the contour of the anterior wall of the sella, called as Walker's point (T, W); and the intersection point of the middle cranial fossa by the greater wing of the sphenoid bone, also called as the Wing point (w) (Figure 4).13,15
Figure 4.

Middle cranial base points. T, Tuberculum sella, Walker's point; W, the intersection point of the middle cranial fossa by the greater wing of the sphenoid bone
Alveolar Bone Thickness
Alveolar bone thickness (width) is the sum of the width of labial (anterior), abbreviated as UA, and posterior (palatal) alveolar bone, abbreviated as UP.16 The upper anterior bone (UA) is measured using a line drawn through the maxillary central incisor’s root apex to the limit of labial cortex, and parallel to the palatal plane (ANS-PNS). The upper posterior bone (UP) is measured using a line drawn through the maxillary central incisor’s root apex to the limit of palatal cortex, and parallel to the palatal plane (ANS-PNS) (Figure 3).16 The alveolar bone thickness was measured in pre-operative cephalometric radiographs.
Amount of Incisor Movement
The pre- and post-operative cephalometric radiographs were assessed in order to measure the amount of movement of the incisors. For both incisal edge and root apex, movement in vertical and horizontal directions was measured. Measurements were performed using a vertical and horizontal reference for all subjects in pre- and post-operative radiographs. The angle formed by the Frankfort Horizontal (FH) plane and the sella-nasion line was reported in literature to be 7 degrees, and for an individual, this does not vary significantly over time.17 This angle was the base we built on to create horizontal and vertical references for linear measurements. The horizontal reference was a line parallel to the Frankfort Horizontal plane (FH). For the vertical reference, a line constructed perpendicular to the horizontal reference intersecting the sella (S) point was used. The perpendicular distances from root apex and incisal edge to horizontal and vertical references were recorded, in both pre- and post-operative radiographs (Figure 5).
Figure 5.

Vertical and horizontal references and distances to root apex and incisal edge
EARR causes shortening in total root and tooth length, leaving the root apex blunt and poorly visible in cephalometric radiographs. This limitation was overcome by measuring the initial tooth length in pre-operative cephalometric radiographs, and later transferring exactly the same length to the post-operative radiograph as a reference to measure from.
Statistical Analysis
Statistical analysis was performed using the IBM SPSS Statistics software for Windows, version 26.0. A post hoc power analysis was performed, the results of which can be seen in Table 2. The Shapiro–Wilk test results for bone thickness for both control and resorption groups, in addition to vertical movement for root apex in the resorption group, indicated that P values were greater than .05. In other words, normality assumptions were met.
Table 2.
Post-hoc power analysis, effect size and N needed for 0.80 power for initial age, treatment time, overjet, overbite, bone thickness, tooth movement gender, treatment type, and root morphology
| Variable |
Observed Power
|
Effect Size | N Needed (Each Group) for 80% Power |
|---|---|---|---|
| Treatment time | 0.999 | 1.080 | 15 |
| Overjet | 0.087 | 0.084 | 2207 |
| Overbite | 0.100 | 0.098 | 1637 |
| Bone Thickness | 1.000 | 1.223 | 12 |
| Horizontal movement | |||
| Incisal Edge | 0.999 | 0.769 | 28 |
| Root Apex | 0.810 | 0.425 | 88 |
| Vertical movement | |||
| Incisal Edge | 0.490 | 0.290 | 188 |
| Root Apex | 0.999 | 0.741 | 30 |
| Gender | 0.086 | 0.045 | 1976 |
| Treatment type | 0.977 | 0.288 | 46 |
| Root morphology | 0.191 | 0.105 | 495 |
Calculations based on assuming alpha = 0.05.
The relationship between EARR and the predisposing factors was assessed using the following statistical tests: the Chi-square test for intergroup comparison of gender, root morphology, and treatment modality; the independent samples t-test for alveolar bone thickness; and the Mann–Whitney U-test for comparison of treatment duration, overjet, overbite, and amount of tooth movement between the 2 groups.
Intra-operator reliability of the method was evaluated by repeating the EARR assessments on randomly selected 20 panoramic films after a 2-week interval. The agreement between the scores of EARR at 2 different time points was evaluated by the Kappa test, and the level of agreement was found to be substantial; the kappa coefficient was 0.643 and scoring of EARR was reliable between 2 measurements. The reliability of the measurements of overbite, overjet, buccal and palatal alveolar bone thickness in the maxillary incisor region, and amount of movement of the incisal root apices were evaluated by repeating these measurements after a 2-week interval on randomly selected 20 cephalometric films using Dahlberg’s18 formula to estimate the random error, which showed that the highest linear error was for the bone thickness (UA+UP) variable, at 0.23 mm.
Results
To calculate the prevalence of severe EARR in our study, the initial sample of 120 patients who presented with severe EARR was used. The results showed that 3.23% of total patients developed severe EARR, while 96.77% showed clinically acceptable root resorption (mild and moderate). The intergroup comparison of treatment duration showed that difference in treatment duration was statistically significant between both groups (Table 3). Intergroup comparisons of the resorption and the control groups in terms of gender, type of treatment, and root morphology showed that only the treatment type presented with premolar extractions showed statistically significant difference (Table 4). Among cephalometric measurements including overjet, overbite, and bone thickness, statistically significant difference was seen only in bone thickness between the resorption and the control groups (Table 5). For the amount and direction of tooth movement, statistically significant differences were seen in both horizontal and vertical directions at both incisal edge and root apex levels (Table 5). Moreover, the difference in the distribution of the vertical displacements among subjects showed statistical significance between the resorption and control groups (Table 6).
Table 6.
Distribution of subjects in terms of posterior (backward), anterior (forward), intrusion (upward) and extrusion movements (downward) in the horizontal and vertical directions
| Horizontal Displacement | Control | Resorption | P-value | ||
|---|---|---|---|---|---|
| Posterior | Anterior | Posterior | Anterior | ||
| Incisal Edge | 37 | 53 | 36 | 54 | .879 |
| Root Apex | 58 | 32 | 69 | 21 | .072 |
| Vertical Displacement | |||||
| Incisal Edge | 44 | 46 | 27 | 63 | .009 |
| Root Apex | 36 | 54 | 20 | 70 | <.001 |
Table 5.
Intergroup comparison of overjet, overbite, bone thickness, and amount of tooth movement in horizontal and vertical directions in millimeters with Independent samples T-test (*) and Mann-Whitney U test (†)
| Variable | Control Group (n = 90) | Resorption Group (n = 90) | P-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Overjet | 4.39 | 2.24 | 4.61 | 2.93 | .458† |
| Overbite | 2.19 | 2.01 | 1.93 | 3.17 | .350† |
| Bone Thickness | 15.06 | 1.99 | 12.54 | 2.13 | <.001* |
| Tooth Movement | |||||
| Horizontal Displacement | |||||
| Incisal Edge | 1.41 | 1.34 | 2.82 | 2.22 | <.001† |
| Root apex | 1.17 | 1.08 | 1.69 | 1.35 | .011† |
| Vertical Displacement | |||||
| Incisal Edge | 1.14 | 1.15 | 1.45 | 0.96 | <.001† |
| Root apex | 1.02 | 1.01 | 1.81 | 1.12 | <.001† |
Discussion
The main goal of this study was to retrospectively determine the prevalence of severe EARR (score 4 according to Malmgren et al.7), in maxillary incisors throughout fixed orthodontic treatment and to evaluate the possible predisposing factors for EARR.
EARR is known as one of the most common complications following orthodontic treatment, and being irreversible, it is considered as a true limitation to obtaining an optimal orthodontic outcome.
Since the most affected teeth are known to be the maxillary incisors (Levander and Malmgren, 198832), the present study aimed to focus on these teeth. The presence of at least one severely resorbed maxillary incisor was considered sufficient to categorize a patient into the resorption group. Division of the incisors into centrals and laterals for comparisons according to tooth type was not deemed necessary as there is already substantial evidence in the literature that the central incisors are more frequently affected.19The root morphology of the anterior teeth was a determining factor that classified the study group into 4 different subgroups according to the root shape; triangular, rhomboid, dilacerated, and pipette. The triangular root shape was the most common in the study group, while rhomboid roots were the most common in the control group. Evaluation of root morphology was done using panoramic radiographs. The main limitation in this evaluation was the poor quality of radiographic films for some patients, which made the evaluation process more challenging.
The rest of the variables studied––overjet, overbite, bone thickness, and tooth movement––were measured using cephalometric radiographs. Another difficulty faced in the present study was the calibration and standardization of cephalometric radiograph dimensions and measurements. As our sample consisted of growing patients, a stable and non-changing reference was necessary to be followed. The middle cranial base was found to maintain its stability in all pubertal growth periods,15,20 which allowed us to use it as a calibration tool. As alveolar bone width was measured on cephalometric radiographs, the limitation of unclear and poor-quality radiographic films was faced again. In a few instances, the precise location of the root apex was difficult to find.
For the assessment of tooth movement, post-treatment values were subtracted from pretreatment ones, and absolute values were used for statistical comparisons. Later on, the displacement values were classified into positive and negative values; positive results indicated backward/upward movement, while negative values indicated forward/downward movement.
In agreement with the findings of previous research, this study discovered a low prevalence of maxillary incisors that developed severe EARR (3.23%) with the loss of more than 1/3 of root length, while 96.77% showed clinically acceptable EARR classified as mild and moderate, as part of the biological tissue reaction to orthodontic treatment. Several authors have reported that a prevalence of 1-5% of severe EARR can be seen following an orthodontic treatment.1,21,22
The control group presented shorter treatment duration, with a mean of 2.48 years, when compared to resorption group, with a mean of 3.7 years (Table 3). Patients who underwent longer orthodontic treatment were at higher risk of developing severe EARR. Prolonged treatment time results in longer periods of stimulation of the root and development of EARR.21 The correlation between the duration of orthodontic treatment and the incidence and severity of EARR is debatable. Some studies concluded that there is positive correlation between EARR and treatment duration,12,26 while other studies found no significant relationship between EARR and treatment time.24,25
Similar to findings in numerous studies, there was no significant relationship between severe EARR and gender of the patient (Table 4).6,12
Table 4.
Intergroup comparison of gender, treatment modality and root morphology with Chi-Square Test
| Variable | Distribution | Control Group (n=90) | Resorption Group (n=90) | P-value |
|---|---|---|---|---|
| Gender |
Male
(n=84) |
40 (47.62%) |
44 (52.38%) |
.550 |
|
Female
(n=96) |
50 (52.08%) |
46 (47.92%) |
||
| Treatment Modality |
Without extraction
(n=124) |
74 (59.68%) |
50 (40.32%) |
<.001 |
|
With extraction
(n=56) |
16 (28.57%) |
40 (71.43%) |
||
| Root Morphology |
Triangular
(n=79) |
35 (44.3%) |
44 (55.7%) |
.575 |
|
Rhomboid
(n=69) |
38 (55%) |
31 (45%) |
||
|
Pipette
(n=16) |
9 (56.25%) |
7 (43.75%) |
||
|
Dilacerated
(n=16) |
8 (50%) |
8 (50%) |
Treatment type may also affect the treatment duration, as they are both linked and affected simultaneously. The results showed a significant relationship between treatment type and severe EARR (Table 4). The resorption group presented 40 patients that were treated with the extraction protocol, involving mainly the upper first premolars, while just 16 patients were treated with the same treatment modality in control group. As extractions result in prolonged treatment time needed to close extraction spaces, relieve crowding, and retract anterior teeth, many authors agree with this finding, reporting that treatment type should be chosen wisely in patients accompanied by higher risk factors that could develop EARR.6,12,21,24
The root morphology was found to have no significant relationship with severe EARR (Table 4). This finding seems to contradict previous reports, which reported that teeth with pipette or dilacerated (irregular) root shape have a higher risk of EARR.11,24 This finding is likely to be the result of having a high percentage of rhomboid roots in the sample, which are associated with a reduced risk of EARR.4,6,11
Increased overjet is usually considered to be a risk factor for root resorption because the correction may require that maxillary anterior teeth move a long distance in order to reduce the maxillary anterior protrusion.4,26 On the other hand, there are also reports which state that there is no correlation between increased overjet and overbite and EARR.6,27 In the present study, the mean overjet and overbite values at the beginning of orthodontic treatment did not show a statistically significant difference between the 2 groups (Table 5). It was noted that a high percentage of patients with increased overjet and overbite in the control group had treatment plans that included fewer extractions when compared to the resorption group (fixed functional appliances, intermaxillary elastics). It is also worth mentioning that some authors claim that increased overjet of more than 5 mm can be a risk factor, which is in agreement with our results, as the mean overjet was less than this value.21
With relatively thin alveolar bone seen in the resorption group (12.5 mm), in comparison with thicker bone in the control group (15 mm) (Table 5), the hypothesis that thin alveolar bone is a risk factor for severe EARR because teeth are being pushed against the thin cortical bone is confirmed.6,16
Results of the present study showed a significant relationship between the amount of tooth movement––net displacement of the root apex and incisal edge during the treatment––and severe EARR (Table 5). This finding is confirmed by many authors; the increase in the amount of tooth movement is a risk factor for EARR.25,28 In horizontal displacement, no difference was seen between the 2 groups with respect to the number of patients with either proclination (anterior) and retraction (posterior) movements (Table 6). For the vertical displacement, statistically significant differences were seen in the distribution of subjects with extrusion (downward) and intrusion (upward) displacements in both groups. In the EARR group, greater downward movement of the incisal edge and root apex was seen compared to the control group (Table 6). This finding may seem controversial as there are many authors who have reported that intrusion is most likely to be a risk factor for EARR when compared to extrusion; intrusion of teeth causes about 4 times more EARR than extrusion.29 Since the resorption group included a greater number of patients with extraction treatment, this finding can be justified because the extractions of premolars and retraction of the incisors during space closure result in controlled and uncontrolled tipping of the incisors, which may cause relative extrusion of these teeth.28-31
When interpreting the findings of the present study, we should keep in mind that it is a retrospective study which has certain limitations with regard to grouping and standardization of the subjects. Moreover, the post hoc power analysis showed that the study was underpowered for a few variables (Table 2). Also, the direction and amount of tooth movement were measured as the displacement of the incisal edges and root apices in anteroposterior and superior-inferior directions during treatment period, not as absolute tooth movement. Finally, the effect of the interactions of the parameters with each other on EARR was ignored. For this reason, the aforementioned statistical analyses were made and the data were interpreted in this regard.
Conclusion
The results of the present investigation conducted on the available records of fixed orthodontic patients treated in Marmara University Faculty of Dentistry Department of Orthodontics between 1990 and 2019 showed that the prevalence of severe EARR of the upper incisors was 3.23%. Prolonged treatment duration, treatment with premolar extractions, presence of a thin alveolar bone, and excessive amounts of horizontal and vertical displacement of the teeth were identified to be risk factors for the occurrence of severe EARR. These factors should be taken into consideration when making treatment plans for future patients in order to minimize the risk of severe EARR and to optimize the treatment results. A further clinical study designed to elucidate the prognosis and longevity of these severely resorbed teeth in the long term may provide interesting and useful findings which could provide a better understanding of the outcome of this undesirable clinical phenomenon.
Table 3.
Intergroup comparison of treatment duration with Mann-Whitney U test
| Control Group (n = 90) | Resorption Group (n = 90) | P-value | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Treatment time (years) | 2.48 | 0.93 | 3.7 | 1.3 | <.001 |
Footnotes
Ethics Committee Approval: Ethics committee approval was received from the Ethical Committee of Marmara University, Faculty of Dentistry, İstanbul, Turkey (approval date and number: 28.03.2019, 2019-317; protocol number: 2019-326).
Informed Consent: Written informed consent was obtained from all patients before starting orthodontic treatment.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.A.; Design - A.A.,B.S.; Supervision - A.A.; Data Collection and/or Processing - B.S.; Analysis and/or Interpretation - A.A.,B.S.; Literature Review - B.S.; Writing - B.S.; Critical Review - A.A.
Declaration of Interests: The authors have no conflict of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. Årtun J, Van ’t Hullenaar R, Doppel D, Kuijpers-Jagtman AM. Identification of orthodontic patients at risk of severe apical root resorption. Am J Orthod Dentofacial Orthop. 2009. Cited 2019 Dec 29;135(4):448 455. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19361730. 10.1016/j.ajodo.2007.06.012) [DOI] [PubMed] [Google Scholar]
- 2. Bartley N, Türk T, Colak C.et al. Physical properties of root cementum: Part 17. Root Resorption After Appl Of 2.5° and 15° of buccal root torque for 4 weeks: A microcomputed tomography study . Am J Orthod Dentofac Orthop [Internet]. 2011. Cited 2019 Dec 29;139(4):e353 e360. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21457842. [DOI] [PubMed] [Google Scholar]
- 3. Consolaro A. Force distribution is more important than its intensity! Dent Press J Orthod. 2014;19(1):5 7. 10.1590/2176-9451.19.1.005-007.oin) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sameshima GT, Sinclair PM. Predicting and preventing root resorption: Part I. Diagnostic factors [internet]. Am J Orthod Dentofacial Orthop. Mosby Inc. 2001. Cited 2019 Dec 30;119(5):505 510. Available at: https://linkinghub.elsevier.com/retrieve/pii/S0889540601916622. 10.1067/mod.2001.113409) [DOI] [PubMed] [Google Scholar]
- 5. Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135(4):434 437. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19361727. 10.1016/j.ajodo.2008.10.014) [DOI] [PubMed] [Google Scholar]
- 6. Picanço GV, Freitas de KMS, Cançado RH.et al. Predisposing factors to severe external root resorption associated to orthodontic treatment. Dent Press J Orthod. 2013;18(1):110 120. 10.1590/s2176-94512013000100022) [DOI] [PubMed] [Google Scholar]
- 7. MalmgrenOlle GL, Hill C, Orwin A.et al. Root resorption after orthodontic treatment of traumatized teeth. 1982;82(6):487 491. [DOI] [PubMed] [Google Scholar]
- 8. Owman-Moll P, Kurol J. The early reparative process of orthodontically induced root resorption in adolescents - Location and type of tissue. Eur J Orthod. 1998;20(6):727 732. 10.1093/ejo/20.6.727) [DOI] [PubMed] [Google Scholar]
- 9. Owman-Moll P, Kurol J, Lundgren D. The effects of a four-fold increased orthodontic force magnitude on tooth movement and root resorptions. An intra-individual study in adolescents. Eur J Orthod. 1996;18(3):287 294. 10.1093/ejo/18.3.287) [DOI] [PubMed] [Google Scholar]
- 10. Liou EJW, Chang PMH. Apical root resorption in orthodontic patients with en-masse maxillary anterior retraction and intrusion with miniscrews. Am J Orthod Dentofacial Orthop. 2010;137(2):207 212. 10.1016/j.ajodo.2008.02.027) [DOI] [PubMed] [Google Scholar]
- 11. Quintanilha L, Fernandes P, Couto Figueiredo N.et al. Predisposing factors for external apical root resorption associated with orthodontic treatment. 2019. Available at: 10.4041/kjod.2019.49.5.310. Accessed 2020 May 20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pastro JDV, Nogueira ACA, Salvatore de Freitas KM.et al., de Oliveira RCGRCG. Factors associated to apical root resorption after orthodontic treatment. Open Dent J. 2018;12(1):331 339. 10.2174/1874210601812010331) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Björk A, Skieller V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983;5(1):1 46. 10.1093/ejo/5.1.1) [DOI] [PubMed] [Google Scholar]
- 14. Hatewar SK, Reddy GH, Singh JR.et al. A new dimension to cephalometry: DW plane. J Indian Orthod Soc. 2015;49(4):206 212. Available at: http://journals.sagepub.com/doi/10.4103/0301-5742.171317. [Google Scholar]
- 15. Arat ZM, Türkkahraman H, English JD, Gallerano RL, Boley JC. Longitudinal growth changes of the cranial base from puberty to adulthood. A comparison of different superimposition methods. Angle Orthod. 2010;80(4):537 544. 10.2319/080709-447.1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Handelman CS. The anterior alveolus : its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996;66(2):95 109; discussion 109. [DOI] [PubMed] [Google Scholar]
- 17. Huh YJ, Huh KH, Kim HK, et al. Constancy of the angle between the Frankfort horizontal plane and the sella-nasion line: A nine-year longitudinal study. Angle Orthod. 2014;84(2):286 291. 10.2319/062013-464.1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dahlberg G. Statistical methods for medical and biological students. Stat Methods Biol Stud. 1940. [Google Scholar]
- 19. Samandara A, Papageorgiou SN, Ioannidou-Marathiotou I, Kavvadia-Tsatala S, Papadopoulos MA. Evaluation of orthodontically-induced external root resorption following orthodontic treatment using cone beam computed tomography (CBCT): a systematic review and meta-analysis. Eur J Orthod. 2019;41(1):67 79. 10.1093/ejo/cjy027) [DOI] [PubMed] [Google Scholar]
- 20. Torlakovic L, Færøvig E. Age-related changes of the soft tissue profile from the second to the fourth decades of life. Angle Orthod. 2011;81(1):52 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mauès CPR, do Nascimento RR, Vilella Ode V. Severe root resorption resulting from orthodontic treatment: prevalence and risk factors. Dent Press J Orthod. 2015;20(1):52 58. 10.1590/2176-9451.20.1.052-058.oar) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mirabella AD, Artun J. Prevalence and severity of apical root resorption of maxillary anterior teeth in adult orthodontic patients. Eur J Orthod. 1995;17(2):93 99. 10.1093/ejo/17.2.93) [DOI] [PubMed] [Google Scholar]
- 23. Tian YL, Wang K, Wang J, Liu F, Piao ML. Root resorption after orthodontic treatment: a study of age factor and prevalence in anterior teeth. Shanghai Kou Qiang Yi Xue. 2013;22(2):224 227. [PubMed] [Google Scholar]
- 24. Elhaddaoui R, Benyahia H, Azeroual MF.et al. Resorption of maxillary incisors after orthodontic treatment – clinical study of risk factors. Int Orthod. 2016;14(1):48 64. 10.1016/j.ortho.2015.12.015) [DOI] [PubMed] [Google Scholar]
- 25. Kim KW, Kim SJ, Lee JY.et al. Apical root displacement is a critical risk factor for apical root resorption after orthodontic treatment. Angle Orthod. 2018;88(6):740 747. 10.2319/111417-777.1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nanekrungsan K, Patanaporn V, Janhom A, Korwanich N. External apical root resorption in maxillary incisors in orthodontic patients: associated factors and radiographic evaluation. Imaging Sci Dent. 2012;42(3):147 154. 10.5624/isd.2012.42.3.147) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jung YH, Cho BH. External root resorption after orthodontic treatment: A study of contributing factors. Imaging Sci Dent. 2011;41(1):17 21. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21977469. 10.5624/isd.2011.41.1.17) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Motokawa M, Sasamoto T, Kaku M.et al. Association between root resorption incident to orthodontic treatment and treatment factors. Eur J Orthod. 2012;34(3):350 356. 10.1093/ejo/cjr018) [DOI] [PubMed] [Google Scholar]
- 29. Han G, Huang S, Von Den Hoff JW, Zeng X, Kuijpers-Jagtman AM. Root resorption after orthodontic intrusion and extrusion: an intraindividual study. Angle Orthod. 2005;75(6):912 918. 10.1043/0003-3219(2005)75[912:RRAOIA]2.0.CO;2) [DOI] [PubMed] [Google Scholar]
- 30. Jayaratne YSN, Uribe F, Janakiraman N. Maxillary incisors changes during space closure with conventional and skeletal anchorage methods: a systematic review. J Istanb Univ Fac Dent. 2017;51(3)(suppl 1):S90 S101. Avaialble at: https://europepmc.org/articles/PMC5750832. 10.17096/jiufd.52884) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Luiz G, Ribeiro U, Jacob HB. Understanding the basis of space closure in Orthodontics for a more efficient orthodontic treatment. Dent Press J Orthod. 2016;21(2):115 125. 10.1590/2177-6709.21.2.115-125.sar) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Levander E, Malmgren O . (1988). Evaluation of the risk of root resorption during orthodontic treatment: A study of upper incisors. European Journal of Orthodontics. 10(1):30 38. [DOI] [PubMed] [Google Scholar]



