Abstract
Autophagy, a cellular self-digestion process, involves the degradation of targeted cell components such as damaged organelles, unfolded proteins, and intracellular pathogens by lysosomes. It is a major quality control system of the cell and plays an important role in cell differentiation, survival, development, and homeostasis. Alterations in the cell autophagic machinery have been implicated in several disease conditions, including neurodegeneration, autoimmunity, cancer, infection, inflammatory diseases, and aging. In non-alcoholic fatty liver disease, including its inflammatory form, non-alcoholic steatohepatitis (NASH), a decrease in cell autophagic activity, has been implicated in the initial development and progression of steatosis to NASH and hepatocellular carcinoma (HCC). We present an overview of autophagy as it occurs in mammalian cells with an insight into the emerging understanding of the role of autophagy in NASH and NASH-related HCC.
Keywords: cell autophagy, NASH, NASH-related HCC
1. Introduction
Non-alcoholic fatty liver disease (NAFLD) is a spectrum of disease that ranges from steatosis to its inflammatory form, non-alcoholic steatohepatitis (NASH), which can progress with or without advanced fibrosis (cirrhosis) to hepatocellular carcinoma (HCC) [1,2]. It is one of the leading causes of liver-related morbidity and mortality in the Western countries, mainly due to a prevalence of sedentary lifestyle and increased consumption of high fat diets [1,2]. The forecasted prevalence of NAFLD in 2030 is conservatively 100.9 million cases worldwide, with NASH’s prevalence increasing up to 27 million cases [3]. NASH and its sequelae HCC have been rising as a global health challenge since it is more common in obese patients, and it has been estimated that 1.2 billion people will be overweight or obese by 2030. NAFLD is a condition in which an excess of fat from the diet accumulates in the liver in an absence of excessive alcohol consumption. In its inflammatory form, NASH is considered the initial phase of liver inflammation, damage, and fibrosis. Clinically, NASH is considered when serum aminotransferases are elevated in an obese subject with metabolic syndrome (hypertension and insulin resistance), or with incidental findings on abdominal imaging [4]. Histologically, it mimics alcoholic liver disease, showing inflammatory infiltrates, focal necrosis, and fibrosis [5]. It is well documented that NASH can progress to HCC, the most common type of primary liver cancer [6,7].
Growing evidence shows that the molecular mechanism underlying the progression of NAFLD to NASH is multifactorial, including metabolomic, immunologic, genetic, and endocrine pathways in concert with changes in gut microbiota communities [8]. Metabolically, NASH comorbidities include hyperlipidemia, insulin resistant status, obesity, and hypertension [9,10,11]. The presence of increased CD68+ cells, such as macrophages and regulatory T cells in affected livers with NASH [12], infers an important role of the host immunity in the regulation of inflammatory pathways. In addition, the loss of liver macrophages and Kupffer cells at the early stage of NASH development with subsequent infiltrations of Ly-6C+ monocyte-derived macrophages [13] reinforces the role of an immune response in the development of NASH. Genetically, there seems to be a difference in susceptibility to NASH progression among ethnic groups. NASH-related cirrhosis is more prevalent in European American descents compared to African American descents [14,15], even though there is a disproportionately large number of underdiagnosed African Americans with NASH [15]. The role of microbiota community changes in NASH is still controversial. Nevertheless, significant changes observed in gut micro-communities are consistent, albeit the specific bacterial species vary among authors [16].
The “two hit” hypothesis is one of the most widely accepted theories for the progression of NASH, proposing steatosis and insulin resistance as the initiating factors that set the stage from metabolic oxidative stress [17]. In addition, we would like to propose autophagy as another cellular process that enhances NASH progression. Autophagy, also referred to as “self-eating”, is a process found across many species in the eukaryotes. It involves the delivery and degradation of cytoplasmic materials by lysosomes and plays a prominent role in cell survival, differentiation, development, and homeostasis by controlling cytoplasmic physiology through energy balance and the removal of misfolded proteins, damaged organelles, and lipid droplets [18,19,20]. In mammalian cells, autophagy can be divided into three main types depending on the method in which the cytoplasmic cargo is delivered to the lysosomes, namely macro-autophagy, micro-autophagy, and chaperone-mediated autophagy [18,20,21].
2. Macro-Autophagy (MA)
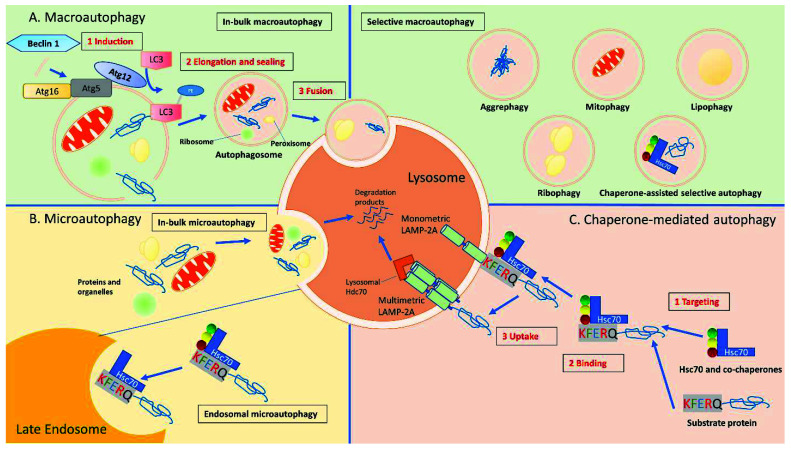
MA, the most studied and major catabolic process used by eukaryotic cells to renew unfunctional proteins or unneeded organelles, operates physiologically at a lower rate, but its function is enhanced under stressful conditions, such as nutrient or energy deprivation [21,22]. It increases substrates that are needed for biosynthesis or energy production for cell survival through the degradation of cytosolic materials [21,23]. The MA process starts with the formation of a double membrane-bound vacuole known as autophagosome, which delivers targeted cytoplasmic materials for degradation to the lysosomes [19,24]. The autophagosome is formed via a non-selective or selective bulk sequestration of cytoplasmic “cargo” (portions of organelles, protein aggregates, or lipid droplets) that is to be delivered for degradation [19,24]. Selective MA targets a particular organelle or substrate cargo for sequestration and degradation by the autophagosome, i.e., mitophagy when mitochondria are the targeted cargo, ER-phagy—the endoplasmic reticulum, pexophagy—the peroxisomes, lipophagy for lipids removal, and aggrephagy for aggregate proteins, while ribophagy targets the ribosomes, and xenophagy—the removal of microorganisms invading the cytoplasm [19,25]. In selective MA, specific cargo is targeted to the autophagosomal membrane for sequestering via a ubiquitin-dependent or ubiquitin-independent pathway that involves autophagy adaptors such as sequestosome 1 (SQSTM1/p62), non-race-specific disease resistance 1 (NDR1), calcium-binding and coiled-coil domain-containing protein 2 (NDP52/CALCOCO2), and optineurin [19,24,26]. On the contrary, non-selective MA involves the degradation of materials by the lysosome in a non-specific manner [27]. The process of MA cargo delivery to the lysosomes for degradation is achieved via the movement of the autophagosome along microtubules, the acquisition of acidic and degradative properties through its fusion with endosomal compartments in the cells, and subsequent fusion with the lysosomal membrane [19,28]. Furthermore, MA is mediated by the activity of proteins encoded by autophagy-related genes (ATGs) and class III phosphatidylinositol 3-kinase (hVps34) in a complex with Beclin 1 and autophagy-related 14 (ATG14L) to produce phosphatidylinositol 3-phosphate (PI3P) that is required for autophagosome formation. Nevertheless, the maturation of the autophagosome into an autolysosome depends on certain autophagy-related (ATG) proteins including ATG14L, as well as on the activity of Ras-associated binding (Rab) GTPases, tethering factors (homotypic fusion and protein sorting (HOPS) complex), adaptors such as pleckstrin homology domain-containing family M member 1 (PLEKHM1), and soluble N-ethylmaleimide sensitive factor attachment protein receptors (SNAREs) for the final execution of the membrane-fusion process [19,20,24]. A summary of the three main types of autophagic processes in mammalian cells culminating in the final degradation of cargos by the lysosomes is shown in Figure 1.
Figure 1.
Autophagic pathways in mammalian cells. There are three major autophagic processes identified in most mammalian cells. (A) Macro-autophagy: in MA, cytosolic substrates determined to be transported are first packaged into autophagosomes, which are double-membrane vesicles formed through conjugation of autophagy-related proteins (i.e., Atg5, Atg12, Atg16) and autophagy-related protein LC3 with lipid PE. The formation of these autophagosomes is initiated by the phosphorylation of lipids in the membrane of organelles such as the endoplasmic reticulum, mitochondria, and Golgi apparatus, triggered by a kinase complex regulated by Beclin-1. Autophagosomes are targeted to lysosomes, and, after fusion of both vesicles, the cargo is delivered to the lysosomes for complete degradation. (B) Micro-autophagy: the in-bulk mA pathway allows cytosolic proteins and organelles to be degraded in bulk through invaginations at the lysosomal membrane. Through endosomal mA, cytosolic proteins can be selectively identified by Hsc70 to be transported to late endosomes using the KFERQ-like motif on the target proteins, leading to their internalization and degradation in the lysosomes. (C) Chaperone mediated autophagy: proteins in the cytosol with a KFERQ-like motif in their sequence can be identified by a molecular chaperone, Hsc70, and brought to the lysosomal membrane for translocation across the LAMP-2A multimeric complex. Lysosomal Hsc70 assist the translocation of the substrate protein, which is then degraded once inside the lysosomes (Adapted and modified from Scrivo et al. 2018) [20].
2.1. Macro-Autophagy (MA) Process
The mechanism of MA involves primarily three processes, namely, (i) autophagosome formation, (ii) fusion of the outer membrane of the autophagosome with the lysosomal membrane to form an autolysosome, and (iii) degradation of the autolysosome contents by lysosomal enzymes. The formation of autophagosome is the first step in the MA process comprising initiation and nucleation, elongation, and, finally, the closure and maturation of the autophagosome. An autophagosome is a double membrane vesicle that is formed via the nucleation of a unique membrane structure known as a phagophore. Upon phagophore formation, cytoplasmic constituents are sequestered into it and, subsequently, the phagophore elongates, bends its membrane, and closes to give rise to the spherical-oriented autophagosome [18,21]. While in the yeast, phagophore formation starts at a single perivacuolar location called the phagophore assembly site (PAS); in mammals, phagophore formation could be initiated at several cytoplasmic locations, such as the endoplasmic reticulum (ER)-associated structures, known as omegasomes [21,29,30,31,32]. The origin of the phagophore membrane is still unclear, but it is hypothesized to come from the plasma membrane, Golgi complex, and/or mitochondria [21,24]. Once the autophagosome closes and matures, it moves along microtubules and fuses with the lysosomal membrane, resulting in the delivery of the sequestered cargo into the lysosome and the formation of a hydrolytic structure known as an autolysosome [21,22,24,33]. As part of the fusion process, there is a degradation of the inner membrane of the autophagosome due to its exposure to the acidic lumen of the lysosomes as well as its hydrolytic enzymes [18,21]. Upon a successful formation of the autolysosome, the autophagic enclosed materials are degraded by lysosomal hydrolases. The resultant components, including amino acids, lipids, and carbohydrate moieties that are derived from the autophagic degradation, are exported back to the cytoplasm through transporters and permeases for recycling or energy production [23,24,33]. In addition, in mammalian cells, the convergence of the MA pathway to the endocytic pathway often occurs, with the autophagosomes fusing with early or late endosomes to form structures referred to as amphisomes. Subsequently, the amphisomes fuse with the lysosomes to give rise to autolysosomes, leading to the final degradation of the autophagic cargo [21,34,35].
2.2. Regulation of Autophagosome Formation
The formation of the autophagosome includes the processes of initiation, nucleation, and elongation/maturation.
2.2.1. Initiation
In the yeast, a protein complex comprising Atg1, Atg13, Atg17, Atg31, and Atg29 kinases controls its initiation and formation. Its mammalian counterpart is made up of either Unc-51-like autophagy-activating kinase 1/2 (ULK1 or ULK2, which is an Atg1 homolog from the Unc-51-like kinase family), ATG13 (the mammalian homolog of Atg13), and RB1-inducible coiled-coil 1/focal adhesion kinase family-interacting protein of 200 kDa (RB1CC1/FIP200), which appears to be the ortholog of Atg17 of yeast [18,21,36,37]. Associated with this complex in mammals is C12orf44/ATG101, which binding to ATG13 is necessary for the MA mechanism [21,38]. The ULK1/2-ATG13-RB1CC1 complex is a very stable complex and forms irrespective of the cell nutritional status. This complex integrates the incoming autophagy signals to initiate the biogenesis of the autophagosome [18,21,39].
2.2.2. Nucleation
The nucleation and assembly of the initial phagophore membrane involves the recruitment of another complex, namely, the class III phosphatidylinositol 3-kinase (PtdIns3K) complex, to the location of autophagosome formation [18,21,37]. This complex is formed by the interaction of Beclin 1 (which is the mammalian ortholog of yeast Atg6), with class III phosphatidylinositol 3-kinase and other key subunits including the PtdIns3K regulatory protein kinase p150 (hVps15), Atg14L, or Beclin1-associated autophagy-related key regulator (Barkor) and UV irradiation resistance-associated gene (UVRAG) [18,21,37,40,41,42]. In mammals and yeast, the PtdIns3K complex generates Phosphatidylinositol 3-phosphate (PtdIns3P), which is critical for the MA process [21,37,43].
2.2.3. Elongation and Maturation
The elongation/maturation of the phagophore is mediated by two ubiquitin-like modification systems, the Atg12-Atg5-Atg16L (Atg16-like protein) complex, and LC3 (microtubule-associated protein 1 light chain 3) conjugation system [18,37,44,45,46]. In the Atg12-Atg5-Atg16L conjugation complex, the ubiquitin-like protein Atg12 is covalently tagged to Atg5. This process is mediated by the E1-like ubiquitin activating enzyme Atg7 and E2-like ubiquitin conjugating enzyme Atg10. Thereafter, the Atg12-Atg5 conjugate interacts non-covalently with ATG16L to form the Atg12-Atg5-Atg16L tetramers, which act as a E3-like ubiquitin ligase, playing a role in the autophagosome membrane elongation by heightening LC3 lipidation [18,21,47,48,49,50,51]. In mammals, the ATG12-ATG5-ATG16L1 complex associates with the pre-autophagosomal membrane, but it dissociates following the complete formation of autophagosome [21,37]. The second ubiquitin-like conjugation reaction involves the conjugation of LC3 to PE (phosphatidylethanolamine) with the help of E1-like Atg7 and E2-like Atg3 to give rise to LC3-II [18,21,37,52]. LC3-II is then specifically targeted to the elongating membrane to drive the closure of the autophagosomal membrane, forming a matured autophagosome [18,53].
One of the principal upstream signals that control the MA process, including the initiation step, is the mechanistic target of rapamycin complex 1 (mTORC1) [18,21,37]. In the cell, the association of the mTORC1 with the autophagy induction complex (ULK1/2-ATG13-RB1CC1) is nutrient-dependent. The availability of energy-producing compounds promotes the association of mTORC1 with the complex, leading to the phosphorylation and subsequent inactivation of ULK1/2 and ATG13 kinases, which drives the inhibition of autophagy. On the contrary, during starvation or when cells are treated with rapamycin, mTORC1 dissociates from the induction complex, driving the dephosphorylation of the proteins that make up the induction complex, resulting in the induction of MA [18,21,37,54,55].
3. Micro-Autophagy (mA)
mA is the lysosomal degradation process involving the direct engulfment of cytoplasmic cargos, without the involvement of autophagosomes as its transport intermediates. In mA, the lysosomal/endosomal membrane invaginates and forms a bud, which sequesters cytoplasmic material. This invaginated bud pinches off as a micro-autophagic body into the lumen of the organelle to be degraded and recycled [56,57,58,59]. Compared to other forms of autophagy, its mechanisms are poorly known, partly due to the significant overlap of its core components with other forms of autophagy, as well as the difficulty in isolating its functions for targeted studies [56,57,58,59].
3.1. mA Process
This involves five major steps. First is the constitutive invagination of the membrane of the lysosome/endosome, leading to the creation of an autophagic tube, a process that is upregulated under cellular starvation [60]. The formation of autophagic tubes is an active process, requiring the use of adenosine triphosphate (ATP) by vacuolar ATPases, and it is mediated by dynamin related GTPase Vps1p [61,62]. Starvation-induced mA is regulated via Atg7-dependednt ubiquitin-like conjugation (Ublc) systems that mediate membrane tethering [63,64]. In yeast, the vacuolar transporter chaperone (VTC) complex plays a role in the autophagic tube formation by modulating the membrane protein distribution, as well as serving as a site for calmodulin activation, which orchestrates acting binding proteins for autophagic tube formation [65]. Vesicle formation involves the sorting of membrane constituents with high-lipid and low-protein composition at the top of the autophagic tube [60]. Then, the vesicle binds with enzymes, implicating a reverse of the endocytosis process, and expanding the cytoplasmic leaflet [62]. Such vesicles have tendency to pinch themselves off into the lysosomal/endosomal lumen from the autophagic tube, and this vesicle scission does not require the various machinery required for MA [66]. After scission from the autophagic tubes, the released vesicles are broken down by Atg15 and hydrolyses and their contents are recycled via the actions of Atg22 [67].
3.2. Regulation of mA Activity
mA is active under cellular stress by starvation or nitrogen deprivation, maintaining organellar size and adjusting the membrane lipid composition by the allocation and degradation of excess cellular components through recycling [68,69,70]. mA works in association with MA and chaperone-mediated autophagy [71], but whether its function is limited to a compensatory mechanism from other forms of autophagy remains to be determined. mA is active in cells, with augmentation of the rate of invagination possibly from its interaction with MA-related pathways [72]. As the invagination and budding takes away portions of lysosomal membrane and lipid components, it contributes to the regulation of lysosomal size [69], in addition to controlling lipid metabolism [73]. Thus, mA serves an important role in cellular housekeeping [73].
3.3. Types of mA
There are various classifications of mA due to the diversity in its processes [74]. General mA in both yeast and mammals does not require the core autophagy machinery, but instead uses the endosomal sorting complex required for transport (ESCRT) [74,75,76]. General mA can be selective (micro-ER-phagy, micro-nucleophagy) or non-selective [74]. The functional classifications are based on the site of mA (lysosome or endosome) or sequestration process of cellular components (membrane invagination or extension) [74,77]. Another point of view proposed differentiating mA into fission and fusion types. The fission type occurs with the invagination and fission of endosomal/lysosomal membranes, requiring ESCRTs and conferring selectivity through the binding of ubiquitylated cargo to ESCRTs [74,78]. The fusion type occurs with invagination and extensions that become sealed by vertex fusion using core autophagy machinery with selectivity conferred with specific receptors [74]. Both mechanisms of mA are involved in the maintenance of cellular homeostasis and have been linked to neurodegenerative diseases such as Alzheimer’s disease and Huntington’s disease [79,80], as well as lysosomal glycogen storage diseases, such as Pompe disease [81].
4. Chaperone-Mediated Autophagy (CMA)
CMA is a selective, receptor-mediated form of autophagy that contributes to lysosomal proteolysis pathways that regulate the turnover of soluble cytosolic proteins [82]. The timely degradation of certain cytosolic proteins is essential in various cellular functions, such as the cellular response to stress, the metabolism of glucose and lipids, and DNA repairs. Thus, CMA plays an important role in cellular quality control and the supplementation of energy to cells under prolonged cellular stress [83]. The CMA process is a selective process, where target substrates are recognized and guided by their degradation tag (chaperone proteins), making the translocation across the lysosomal membrane a regulated process [84]. Since they require a targeting motif in their amino acid sequence that binds to HSC70 (heat shock protein-70 kDa), not all cytosolic proteins can be a candidate for lysosomal degradation through this process [85]. CMA does not require the formation of vesicles for the translocation of the target proteins into lysosomes, and thus, the direct lysosomal translocation of cargos occurs in CMA [86].
4.1. CMA Process
The selectivity in CMA is maintained by a sequence of the substrate protein, the pentapeptide KFERQ motif that enables its targeting for lysosome degradation. This motif is present in about 30% of the cytosolic proteins [87,88]. As with most intracellular targeting motifs, the KFERQ sequence exists in its inactive form and its specificity depends on the charges on the sequence component, rather than its amino acid combination [89]. The CMA-targeting motif contains, on one side, a glutamine (Q), one negatively charged acidic residue (D or E), one positively charged basic residue (K or R), a hydrophobic residue (F, I, L or V), and, lastly, a fifth residue, which can be positively/negatively charged. In some proteins, the motif can be hidden inside a protein folding before unfolding with post-translational modification, and in others it can be present in the pre-post-translational state to be eliminated if the targeted protein is present in excess amounts [89]. Crucial to the mechanism of CMA is HSC70s, the cytosolic chaperone that recognizes the KFERQ motif and assists with the protein complex translocation across the lysosomal membranes [85]. HSC70 is also responsible for clathrin disassembly from coated vesicles, and the folding of unfolded cytosolic proteins. HSC70 typically binds to the hydrophobic region of a protein to help the folding of unfolded or misfolded proteins, but upon binding to the KFERQ motif, it promotes protein degradation through CMA [85]. Other chaperones that interact with HSC70, such as heat-shock protein-40 kDa (HSC40) increase the effectiveness of HSC70 by forming a complex, but HSC70 seems to be the only known chaperone that directly binds to the KFERQ-like motif [90]. Other co-chaperones that interact with HSC70 may either help with the targeting of a certain substrate or unfolding of the substrate before the translocation across lysosomal membranes [90]. HSC70 exists as lysosomal or luminal HSC70. At the membrane, luminal HSC70 plays a role in the unfolding of substrate proteins [91], as well as the recycling of receptor proteins from CMA translocation complex by facilitating their dissociation after the substrate is internalized into lysosome [92]. Lysosomal HSC70 is needed for the completion of the translocation of substrate into lysosomes, in which the substrate undergoes enzymatic degradation. Once the complex of the bound substrate and chaperone is transported to the lysosomal surface, it binds to the lysosomal membrane and begins its unfolding and subsequent translocation into the lysosomal lumen; this process is saturable [93]. This saturability comes from the required binding of lysosome-associated membrane protein-type 2A (LAMP2A) to the CMA substrates. LAMP2A is one of the three splice variants of the gene lamp2: LAMP2A, LAMP2B, and LAMP2C. They have the same luminal region with different transmembrane and cytosolic regions, but LAMP2A is the only one required for CMA [94,95]. While cytosolic HSC70 is abundant in the cytosol, the LAMP2A level on the lysosomal membrane is restricted, limiting the CMA process rate, and its blockage leads to highly specific CMA inhibition. LAMP2A synthesis is shown to be increased during cellular stress, such as mild oxidative stress and hypoxia [96,97,98,99]. Heat-shock protein 90 kDa (HSP90), also a known chaperone, also binds to the luminal side of the lysosomal membrane and helps to stabilize the integrity of the LAMP2A complex during the translocation process [92].
4.2. CMA Activity
CMA activity is regulated by several pathways, but mainly by the mechanistic target of the rapamycin complex 2-protein kinase B-PH domain leucine-rich repeat protein phosphatase (mTORC2-Akt-PHLPP1) axis. The regulation of the CMA translocation complex was shown to be dependent upon the phosphorylation of the lysosomal glial fibrillary acidic protein (GFAP) [100]; in its unphosphorylated form, GFAP binds to the cytosolic binding motif of LAMP2A to form part of the CMA translocation complex. While GFAP activity is upregulated by Akt and the lysosomal kinase target of rapamycin complex 2 (mTORC2), GPAP is downregulated at the lysosomal membrane by the PH-domain leucine-rich repeat protein phosphatase (PHLPP1). At the basal state, mTORC2 activates Akt [101], which then phosphorylates GFAP, resulting in the basal inhibition of CMA [102]. When CMA is activated, PHLPP1 is recruited to the lysosomal membrane to inhibit Akt from phosphorylating lysosomal GFAP, which then promotes LAMP2A complex formation to drive CMA [102]. Additionally, the regulation of CMA through Akt is also associated with the insulin-phosphoinositide-3-kinase-3-phosphoinositide-dependent protein kinase 1 (INS-PI3K-PDPK1) pathway that regulates Akt activity [103].
4.3. CMA Activity in Health and Disease
Chaperone-mediated autophagy activity is required in many cell processes to maintain normal homeostasis, and its decreased activity has been associated with the development of some pathological conditions.
(a) Nutritional starvation stress. CMA is known to be triggered via nutritional starvation. The degradation of many enzymes involved in metabolism by CMA is significantly increased in the liver during fasting [104,105]. CMA induced by starvation provides cells with the retrieved amino acids to be used for protein synthesis and energy source generation. This controlled and selective retrieval of cellular fuels and maintenance of protein biosynthesis during such cellular stress reaches its maximal turnover rate in around 12 h, following the initiation of MA processes that precede it, and continues to be active until the starvation is resolved [104,105,106]. In metabolically demanding organs like the liver, MA lasts for close to 8 h following starvation, starting with proteolysis and then switching over to the more preferential lipids degradation. If the starvation lasts longer, CMA becomes the main pathway to replenish the amino acids [104,105,106]. Those newly provided amino acids contribute to both protein synthesis and gluconeogenesis. Interestingly, even though their functions overlap, MA and CMA processes have non-redundant functions in cellular regulation. In CMA-impaired livers, MA can compensate for the lack of CMA in clearing damaged proteins, but cannot fully mitigate the cellular damage caused by the inability to adequately address the genetic damage and change in metabolic flux [104]. Highlighting the importance of CMA in energy supplementation during starvation, both in vitro and in vivo models with impaired CMA exhibited reduced levels of ATP in nutrient-deprived states [104,107].
(b) Metabolic pathway regulation. CMA is also involved in hepatic glycolysis regulation by degrading the glycolytic enzymes that stop hepatic glycolysis, and the inhibition of CMA leads to energy deficiency in peripheral organs [104]. Previous studies on a CMA-defective mouse model showed that many of the enzymes involved in the tricarboxylic acid (TCA) cycle are degraded by CMA during a period of starvation [104]. Moreover, CMA is involved in lipolysis as lipid carriers and coating proteins such as perilipins 2 and 3 (PLIN2 and PLIN3), and lipogenesis enzymes have been shown to be substrates targeted by CMA [104]. It is worth noting that lipid droplet coat protein removal during starvation is triggered via the 5′-AMP-activated protein kinase (AMPK)-dependent phosphorylation of PLIN2 [108].
(c) Regulation of transcription. CMA also play a role in the control of transcription, mainly through its action on factor-κB (NF-κB), by degrading its inhibitor NF-κ-B inhibitor-α (IκBα) [109] and selective degradation of myocyte-specific enhancer factor 2A (MEF2A) and myocyte-specific enhancer factor 2D (MEF2D) in neurons [110].
(d) Immune response regulation. CMA is associated with immune response regulation, through the degradation of stimulator of interferon genes protein (STING), which is involved in innate immunity [111]. I additionally plays a role in the degradation of Itch (ubiquitin ligase), and as a regulator of calcineurin 1 (Rcan1, a factor that has been implicated in the pathophysiology of Alzheimer’s disease) [96].
(e) Cell cycle control. CMA initiates cell-cycle progression following DNA repair through the targeted degradation of hypoxia-inducible factor 1-alpha (HIF1α), a cell-cycle progression regulator [98], and serine/threonine-specific protein kinase 1, which is a cell-cycle checkpoint kinase that is integral in DNA repair [90].
(f) Cell senescence. There is an age-dependent decrease in activity of CMA in most cells and tissues in both rodents and humans, as the binding and translocation of substrate proteins by lysosomes are reduced with age in direct proportion to a decrease of LAMP2A [88,96,111,112]. The decrease in LAMP2A is not transcriptional or post-translational (from gene expression), but rather due to decreased CMA receptor stability [113]. Earlier studies have shown that the overexpression of liver LAMP2A in the transgenic aging mouse model improved the maintenance of cellular homeostasis [114], implicating CMA as a potential player in NASH progression and HCC development.
CMA has been associated with several neurodegenerative and lysosomal storage disorders [115]. In neurodegenerative diseases, such as Parkinson’s disease many of the associated proteins in their unmodified state can serve as CMA substrates; nevertheless, their pathogenic variants are unable to be targeted and transported to lysosomes to be degraded, and their accumulation not only produces cellular damage, but further slows CMA efficiency [116,117,118]. Lysosomal storage disorders, such as galactosialidosis and Tay–Sachs disease, are genetic diseases that have dysfunctional lysosomal enzymes, aggravating the protein degradation process that leads to substrate accumulation and cellular toxicity [115,116,117,118]. CMA activities in cancer cell lines have upregulated LAMP2A levels [107,119], enhancing cell survival against cellular stressors such as hypoxia and oxidative stress [119,120,121]. CMA may aid cancer proliferation by the degradation of the inhibitors of cell proliferation, such as Rho-related GTP binding protein RhoE (RND3] [122], and pro-apoptotic protein Bcl-2-binding component 3 (BBC3) [123]. CMA has also been implicated as a tumor suppressor [124,125] by maintaining genomic stability through improving DNA repair [90].
5. Autophagy in Liver Physiology
Prolonged starvation induces liver cell autophagy, implicating the activation of metabolic pathways to replenish needed nutrients through the degradation of substrates during liver malnutrition and/or parenchymal damage [126,127]. During periods of nutrient deprivation, autophagy acts as one of the drivers of gluconeogenesis, ketogenesis, and ß-oxidation in the liver. Previous studies have shown that autophagy is involved in the degradation of glycogen and the formation of autophagic vacuoles dependent on cell energy status [126,128], which correlated with stress and hepatocyte amino acid deprivation [126,129,130]. In neonates, autophagy mediates the restoration of plasma glucose levels during fasting by gluconeogenesis from amino acids [127,131]. A non-selective autophagy drives the process of proteolysis, making available amino acids for use in the process of gluconeogenesis [127,132]. In addition, the selective autophagy of triglycerides stored in lipid droplets (lipophagy) fuels the ß-oxidation cycle [127,133]. Lipophagy also regulates the rate of very-low-density lipoprotein (VLDL) assembly by the release of fatty acids and degradation of apolipoprotein B [127].
Autophagy may play a key role in preventing cell death in the liver. Following the induction of hepatocellular necrosis by dimethylnitrosamine (DMNA), an increase in the number and size of autophagic vacuoles was observed [126,134]. Induced liver cell autophagy by carbamazepine (CBZ) decreased the hepatic load of mutant alpha1-antitrypsin Z (ATZ), and the severity of the deficiency in a mouse model of AT-deficiency-associated liver disease [127,135]. Additionally, the preservation of liver autophagic activity resulted in the lower intracellular accumulation of damaged proteins, an improved ability to handle protein damage, and an overall improvement in hepatic function [114]. Liver autophagy activity balances diverse metabolic pathways, but also removes damaged organelles (e.g., mitochondria, endoplasmic reticulum, peroxisomes), protecting and repairing liver cells from injury, thereby playing a key role in hepatocyte homeostasis [126].
6. Autophagy in NASH and NASH-Related HCC
Cell autophagy activity is impaired in NAFLD, NASH, and NASH-related HCC. Obesity and a prolonged high-fat diet affect the cell autophagy machinery at various stages, including the blockade of autophagosome formation, the inhibition of autophagosome–lysosome fusion, and the disruption of lysosome physiology [136,137]. Sustained high-fat diets affect lipid cell autophagy activity with increased accumulation of lipids in the liver, downregulating lipid β-oxidation and ATP production [136,137]. In addition, lipid accumulation causes alterations in the autophagosome membrane, leading to a non-efficient fusion process between autophagosomes and lysosomes [106,136]. The knocking down of autophagy-related genes, or their pharmacological inhibition, leads to the accumulation of triglycerides as lipid droplets [106,137], lower free fatty-acid oxidation, and decreased VLDL vesicle secretion from the liver cells [137]. Emerging data show that autophagy is impaired in the NAFLD cell line, in animal models of NAFLD, and in liver specimens from NAFLD patients [137,138]. Inducing hepatic autophagy through the increased expression of liver specific Atg7 in ob/ob mice ameliorated metabolic stress and attenuated hepatic steatosis [137,139]. Furthermore, the upregulation of pro-autophagic transcription factors such as FoxO1 and transcription factor EB (TFEB) prevented steatosis [137,140,141]. Previous studies have also revealed that enhancing autophagy prevented cell death in hepatocytes that had been exposed to prolonged treatment with palmitic acid [137,138]. In addition, treatment with carbamazepine and rapamycin, which are autophagy-inducing drugs, leads to a reduction in liver steatosis and triglyceride levels in both the liver and blood [137,142]. Nevertheless, the specific role of autophagy in the progression of steatosis to NASH and NASH-HCC remains elusive [143].
The loss of beclin-1 (an autophagy gene) leads to HCC development [143,144,145]. The knocking out of beclin-1 in mice results in spontaneous HCC [143,144,145], and in human HCC, the loss of beclin-1 is a common feature that correlates with poor prognosis [143,146]. Rubicon (a suppressor of the late stage of autophagy) is increased in NAFLD and plays a key role in driving hepatocellular fat accumulation and apoptosis [147,148]. Furthermore, cell autophagy activity is suppressed in hepatocyte-specific TGF β-activated kinase 1 (TAK1) knockout mice [137,149]. TAK1 serves as a positive regulator of AMPK, and its deletion in these mice led to increased mTOR activity and the suppression of autophagy, followed by severe hepato-steatosis [137,149]. Interestingly, these animals (with a hepatocyte-specific knockout of Tak1 developed spontaneous hepatocarcinogenesis, with high levels of p62/SQSTM in the hepatocytes. Restored autophagy activity by rapamycin was associated with both the downregulation of mTOR and the attenuation of liver cancer development and growth [137,149]. The deletion of protein tyrosine phosphatase receptor type O (PTPRO) in mice (a tumor suppressor), resulted in severe autophagy impairment [137,150]. Additionally, immunohistochemical staining from human samples revealed that hepatic PTPRO was reduced in livers from subjects with NAFLD compared to subjects with normal livers, while p62/SQSTM1 was increased [137,150].
Impaired cell autophagy activity may induce inflammation due to its role in clearing damaged mitochondria. The release of reactive oxygen intermediates and mitochondrial DNA leads to the inhibition of inflammasomes and Toll-like receptor 9 [137,151,152]. In addition, cell autophagy is implied in the degradation of p62/SQSTM1, an activator of nuclear factor kappa B (NF-κB), enhancing the transcription of pro-inflammatory cytokines [137]. The inhibition of cell autophagy activity in NASH leads to the accumulation of p62/SQSTM1, an autophagic substrate hypothesized to be involved in the formation of the Mallory–Denk bodies (MDB). MDB are present in ballooned hepatocytes and are key markers for NASH diagnosis. The upregulation of cell autophagy by rapamycin results in MDB resolution in mice [136]. Furthermore, the impairment of autophagy in tumor cells following metabolic stress also results in the accumulation of p62/SQSTM1, leading to increased retainment of damaged mitochondria, heightening oxidative stress and DNA damage [148,153]. The ubiquitin-binding protein p62 is a multifunctional protein involved in the activation the NF-κB-signaling pathway, as well as in the transcription of genes encoding for antioxidant proteins and detoxification enzymes through the activation of the nuclear factor erythroid 2–related factor 2 (Nrf2) transcription factor [127,154,155]. Defective autophagy decreases cell energy, resulting in a low cell redox state by decreasing recycling damaged organelles, DNA, aggregated proteins, and pathogens to maintain energy balance, promoting an anaerobic inefficient metabolism [136,156]. Concomitantly, previous studies have shown a progressive upregulation of p62 in obese patients with steatosis and NASH in comparison to subjects with a normal liver, thereby suggesting a downregulation of autophagy in obese patients with hepatic steatosis and NASH [136,138].
A complete pathway of how cell autophagy activity influences NASH progression to ESLD and HCC remains to be determined [157]. Nevertheless, it appears that impaired cell autophagy activity affects early liver fat accumulation and mitochondrial function, leading to a progressive widening of metabolic disturbances that enhance cell senescence and cell apoptosis. Further metabolic disturbances enhance epigenetic changes and NASH progression, promoting an apoptotic switch with subsequent liver malignant genesis [158].
Abbreviations
AKT1: protein kinase B; AMPK: adenosine 5′ monophosphate-activated protein kinase; AT: alpha1-antitrypsin; ATG: Autophagy-related; ATP: adenosine triphosphate; ATZ: alpha1-antitrypsin Z; Barkor: beclin1-associated autophagy-related key regulator; BBC3: Bcl-2-binding component 3; CALCOCO2: calcium binding and coiled-coil domain 2; CBZ: carbamazepine; CMA: chaperone-mediated autophagy; CTSA: cathepsin A; DMNA: dimethylnitrosamine; DNA: deoxyribonucleic acid; ESCRT: endosomal sorting complex required for transport; FoxO1: forkhead box protein O1; GFAP: glial fibrillary acidic protein; HCC: hepatocellular carcinoma; HOPS: homotypic fusion and protein sorting; HSC70: heat-shock protein-70 kDa; INS-PI3K-PDPK1: insulin-phosphoinositide-3-kinase-3-phosphoinositide-dependent protein kinase 1; LAMP2A: lysosome-associated membrane protein type 2A; LC3: microtubule-associated protein 1 light chain 3; MA: macroautophagy; MDB: Mallory–Denk bodies; MEF2A: myocyte-specific enhancer factor 2A; MEF2D: myocyte-specific enhancer factor 2D; mTORC1: mechanistic target of rapamycin complex 1; mTORC2: mechanistic target of rapamycin complex 2; MVB: multivesicular body; NAFLD: non-alcoholic fatty liver disease; NASH: non-alcoholic steatohepatitis; NDR1: non-race-specific disease resistance1; NF-κB: nuclear factor kappa B; Nrf2: nuclear factor erythroid 2-related factor 2; PAS: phagophore assembly site, PD: Parkinson’s disease; PE: phosphatidylethanolamine; PHLPP1: PH domain leucine-rich repeat protein phosphatase PLEKHM1: pleckstrin homology domain-containing family M member 1; PI3P: phosphatidylinositol 3-phosphate; PPCA: protective protein/cathepsin A; PTPRO: protein tyrosine phosphatase receptor type O; PtdIns3K: class III phosphatidylinositol 3-kinase; PtdIns3P: phosphatidylinositol 3-phosphate; (Rab) GTPases: Ras-associated binding GTPases; RND3/RhoE: Rho-related GTP binding protein; SNARE: soluble N-ethylmaleimide sensitive factor attachment protein receptor; SQSTM1: sequestosome 1; STING: stimulator of interferon genes protein; TFEB: transcription factor EB; TAK1: transforming growth factor β-activated kinase 1; Ublc: ubiquitin-like conjugation; VLDL: very-low-density lipoprotein; UVRAG: UV irradiation resistance-associated gene; VPS34: class III phosphatidylinositol 3; VTC: vacuolar transporter chaperone.
Author Contributions
U.-A.S.U., P.K.R., Y.N., R.F. and J.R.S. wrote and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
No applicable.
Informed Consent Statement
No applicable.
Data Availability Statement
No applicable.
Conflicts of Interest
The authors have no conflict of interest to declare with respect to authorship and publication of this article.
Funding Statement
This review was funded by a Grant to Dr. J Sanabria from the Edwards Comprehensive Cancer Center.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chalasani N., Younossi Z., Lavine J.E., Charlton M., Cusi K., Rinella M., Harrison S.A., Brunt E.M., Sanyal A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 2.Kleiner D.E., Brunt E.M., Wilson L.A., Behling C., Guy C., Contos M., Cummings O., Yeh M., Gill R., Chalasani N., et al. Association of Histologic Disease Activity with Progression of Nonalcoholic Fatty Liver Disease. JAMA Netw. Open. 2019;2:e1912565. doi: 10.1001/jamanetworkopen.2019.12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Estes C., Razavi H., Loomba R., Younossi Z., Sanyal A.J. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67:123–133. doi: 10.1002/hep.29466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellentani S., Scaglioni F., Marino M., Bedogni G. Epidemiology of non-alcoholic fatty liver disease. Dig. Dis. 2010;28:155–161. doi: 10.1159/000282080. [DOI] [PubMed] [Google Scholar]
- 5.Ludwig J., Viggiano T.R., McGill D.B., Oh B.J. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin. Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 6.Ascha M.S., Hanouneh I.A., Lopez R., Tamimi T.A., Feldstein A.F., Zein N.N. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51:1972–1978. doi: 10.1002/hep.23527. [DOI] [PubMed] [Google Scholar]
- 7.Said A., Ghufran A. Epidemic of non-alcoholic fatty liver disease and hepatocellular carcinoma. World J. Clin. Oncol. 2017;8:429–436. doi: 10.5306/wjco.v8.i6.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kutlu O., Kaleli H.N., Ozer E. Molecular Pathogenesis of Nonalcoholic Steatohepatitis- (NASH-) Related Hepatocellular Carcinoma. Can. J. Gastroenterol. Hepatol. 2018;2018:8543763. doi: 10.1155/2018/8543763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polyzos S.A., Kountouras J., Mantzoros C.S. Obesity and nonalcoholic fatty liver disease: From pathophysiology to therapeutics. Metabolism. 2019;92:82–97. doi: 10.1016/j.metabol.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 10.Finck B.N. Targeting Metabolism, Insulin Resistance, and Diabetes to Treat Nonalcoholic Steatohepatitis. Diabetes. 2018;67:2485–2493. doi: 10.2337/dbi18-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams L.A., Lymp J.F., St Sauver J., Sanderson S.O., Lindor K.D., Feldstein A., Angulo P. The natural history of nonalcoholic fatty liver disease: A population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Soderberg C., Marmur J., Eckes K., Glaumann H., Sallberg M., Frelin L., Rosenberg P., Stal P., Hultcrantz R. Microvesicular fat, inter cellular adhesion molecule-1 and regulatory T-lymphocytes are of importance for the inflammatory process in livers with non-alcoholic steatohepatitis. APMIS. 2011;119:412–420. doi: 10.1111/j.1600-0463.2011.02746.x. [DOI] [PubMed] [Google Scholar]
- 13.Reid D.T., Reyes J.L., McDonald B.A., Vo T., Reimer R.A., Eksteen B. Kupffer Cells Undergo Fundamental Changes during the Development of Experimental NASH and Are Critical in Initiating Liver Damage and Inflammation. PLoS ONE. 2016;11:e0159524. doi: 10.1371/journal.pone.0159524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Browning J.D., Kumar K.S., Saboorian M.H., Thiele D.L. Ethnic differences in the prevalence of cryptogenic cirrhosis. Am. J. Gastroenterol. 2004;99:292–298. doi: 10.1111/j.1572-0241.2004.04059.x. [DOI] [PubMed] [Google Scholar]
- 15.Caldwell S.H., Harris D.M., Patrie J.T., Hespenheide E.E. Is NASH underdiagnosed among African Americans? Am. J. Gastroenterol. 2002;97:1496–1500. doi: 10.1111/j.1572-0241.2002.05795.x. [DOI] [PubMed] [Google Scholar]
- 16.Schade M., Sanabria J.A., Mallick A., Aguilar R., Andryka M., Schlatzer D., Li X., Hazlett F.E., Kachman M., Raskind A., et al. Normalization of the α1-Na/K-ATPase/Src Signalosome Restored Microbiota Communities and Rescinded NASH Progression in the Mouse. [(accessed on 15 June 2022)]. Available online: https://www.preprints.org/manuscript/202109.0023.
- 17.Day C.P., James O.F. Steatohepatitis: A tale of two “hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/S0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 18.Wu H., Chen S., Ammar A.B., Xu J., Wu Q., Pan K., Zhang J., Hong Y. Crosstalk between Macroautophagy and Chaperone-Mediated Autophagy: Implications for the Treatment of Neurological Diseases. Mol. Neurobiol. 2015;52:1284–1296. doi: 10.1007/s12035-014-8933-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allaire M., Rautou P.E., Codogno P., Lotersztajn S. Autophagy in liver diseases: Time for translation? J. Hepatol. 2019;70:985–998. doi: 10.1016/j.jhep.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 20.Scrivo A., Bourdenx M., Pampliega O., Cuervo A.M. Selective autophagy as a potential therapeutic target for neurodegenerative disorders. Lancet Neurol. 2018;17:802–815. doi: 10.1016/S1474-4422(18)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parzych K.R., Klionsky D.J. An overview of autophagy: Morphology, mechanism, and regulation. Antioxid. Redox Signal. 2014;20:460–473. doi: 10.1089/ars.2013.5371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rautou P.E., Mansouri A., Lebrec D., Durand F., Valla D., Moreau R. Autophagy in liver diseases. J. Hepatol. 2010;53:1123–1134. doi: 10.1016/j.jhep.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 23.Yorimitsu T., Klionsky D.J. Autophagy: Molecular machinery for self-eating. Cell Death Differ. 2005;12((Suppl. 2)):1542–1552. doi: 10.1038/sj.cdd.4401765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Madrigal-Matute J., Cuervo A.M. Regulation of Liver Metabolism by Autophagy. Gastroenterology. 2016;150:328–339. doi: 10.1053/j.gastro.2015.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu W., Ocak U., Gao L., Tu S., Lenahan C.J., Zhang J., Shao A. Selective autophagy as a therapeutic target for neurological diseases. Cell. Mol. Life Sci. 2021;78:1369–1392. doi: 10.1007/s00018-020-03667-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khaminets A., Behl C., Dikic I. Ubiquitin-Dependent and Independent Signals in Selective Autophagy. Trends Cell Biol. 2016;26:6–16. doi: 10.1016/j.tcb.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Khandia R., Dadar M., Munjal A., Dhama K., Karthik K., Tiwari R., Yatoo M.I., Iqbal H.M.N., Singh K.P., Joshi S.K., et al. A Comprehensive Review of Autophagy and Its Various Roles in Infectious, Non-Infectious, and Lifestyle Diseases: Current Knowledge and Prospects for Disease Prevention, Novel Drug Design, and Therapy. Cells. 2019;8:674. doi: 10.3390/cells8070674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reggiori F., Ungermann C. Autophagosome Maturation and Fusion. J. Mol. Biol. 2017;429:486–496. doi: 10.1016/j.jmb.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 29.Hemelaar J., Lelyveld V.S., Kessler B.M., Ploegh H.L. A single protease, Apg4B, is specific for the autophagy-related ubiquitin-like proteins GATE-16, MAP1-LC3, GABARAP, and Apg8L. J. Biol. Chem. 2003;278:51841–51850. doi: 10.1074/jbc.M308762200. [DOI] [PubMed] [Google Scholar]
- 30.Chen Y., Klionsky D.J. The regulation of autophagy—Unanswered questions. J. Cell Sci. 2011;124:161–170. doi: 10.1242/jcs.064576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Itakura E., Mizushima N. Characterization of autophagosome formation site by a hierarchical analysis of mammalian Atg proteins. Autophagy. 2010;6:764–776. doi: 10.4161/auto.6.6.12709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yla-Anttila P., Vihinen H., Jokitalo E., Eskelinen E.L. 3D tomography reveals connections between the phagophore and endoplasmic reticulum. Autophagy. 2009;5:1180–1185. doi: 10.4161/auto.5.8.10274. [DOI] [PubMed] [Google Scholar]
- 33.Shen H.M., Mizushima N. At the end of the autophagic road: An emerging understanding of lysosomal functions in autophagy. Trends Biochem. Sci. 2014;39:61–71. doi: 10.1016/j.tibs.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Tooze J., Hollinshead M., Ludwig T., Howell K., Hoflack B., Kern H. In exocrine pancreas, the basolateral endocytic pathway converges with the autophagic pathway immediately after the early endosome. J. Cell Biol. 1990;111:329–345. doi: 10.1083/jcb.111.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berg T.O., Fengsrud M., Stromhaug P.E., Berg T., Seglen P.O. Isolation and characterization of rat liver amphisomes. Evidence for fusion of autophagosomes with both early and late endosomes. J. Biol. Chem. 1998;273:21883–21892. doi: 10.1074/jbc.273.34.21883. [DOI] [PubMed] [Google Scholar]
- 36.He C., Klionsky D.J. Regulation mechanisms and signaling pathways of autophagy. Annu. Rev. Genet. 2009;43:67–93. doi: 10.1146/annurev-genet-102808-114910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mehrpour M., Esclatine A., Beau I., Codogno P. Overview of macroautophagy regulation in mammalian cells. Cell Res. 2010;20:748–762. doi: 10.1038/cr.2010.82. [DOI] [PubMed] [Google Scholar]
- 38.Hosokawa N., Sasaki T., Iemura S., Natsume T., Hara T., Mizushima N. Atg101, a novel mammalian autophagy protein interacting with Atg13. Autophagy. 2009;5:973–979. doi: 10.4161/auto.5.7.9296. [DOI] [PubMed] [Google Scholar]
- 39.Jung C.H., Jun C.B., Ro S.H., Kim Y.M., Otto N.M., Cao J., Kundu M., Kim D.H. ULK-Atg13-FIP200 complexes mediate mTOR signaling to the autophagy machinery. Mol. Biol. Cell. 2009;20:1992–2003. doi: 10.1091/mbc.e08-12-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Furuya N., Yu J., Byfield M., Pattingre S., Levine B. The evolutionarily conserved domain of Beclin 1 is required for Vps34 binding, autophagy and tumor suppressor function. Autophagy. 2005;1:46–52. doi: 10.4161/auto.1.1.1542. [DOI] [PubMed] [Google Scholar]
- 41.Itakura E., Kishi C., Inoue K., Mizushima N. Beclin 1 forms two distinct phosphatidylinositol 3-kinase complexes with mammalian Atg14 and UVRAG. Mol. Biol. Cell. 2008;19:5360–5372. doi: 10.1091/mbc.e08-01-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matsunaga K., Morita E., Saitoh T., Akira S., Ktistakis N.T., Izumi T., Noda T., Yoshimori T. Autophagy requires endoplasmic reticulum targeting of the PI3-kinase complex via Atg14L. J. Cell Biol. 2010;190:511–521. doi: 10.1083/jcb.200911141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burman C., Ktistakis N.T. Regulation of autophagy by phosphatidylinositol 3-phosphate. FEBS Lett. 2010;584:1302–1312. doi: 10.1016/j.febslet.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 44.Romanov J., Walczak M., Ibiricu I., Schuchner S., Ogris E., Kraft C., Martens S. Mechanism and functions of membrane binding by the Atg5-Atg12/Atg16 complex during autophagosome formation. EMBO J. 2012;31:4304–4317. doi: 10.1038/emboj.2012.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matsushita M., Suzuki N.N., Obara K., Fujioka Y., Ohsumi Y., Inagaki F. Structure of Atg5·Atg16, a complex essential for autophagy. J. Biol. Chem. 2007;282:6763–6772. doi: 10.1074/jbc.M609876200. [DOI] [PubMed] [Google Scholar]
- 46.Weidberg H., Shvets E., Elazar Z. Biogenesis and cargo selectivity of autophagosomes. Annu. Rev. Biochem. 2011;80:125–156. doi: 10.1146/annurev-biochem-052709-094552. [DOI] [PubMed] [Google Scholar]
- 47.Ohsumi Y. Molecular dissection of autophagy: Two ubiquitin-like systems. Nat. Rev. Mol. Cell Biol. 2001;2:211–216. doi: 10.1038/35056522. [DOI] [PubMed] [Google Scholar]
- 48.Shintani T., Mizushima N., Ogawa Y., Matsuura A., Noda T., Ohsumi Y. Apg10p, a novel protein-conjugating enzyme essential for autophagy in yeast. EMBO J. 1999;18:5234–5241. doi: 10.1093/emboj/18.19.5234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Geng J., Klionsky D.J. The Atg8 and Atg12 ubiquitin-like conjugation systems in macroautophagy. ‘Protein modifications: Beyond the usual suspects’ review series. EMBO Rep. 2008;9:859–864. doi: 10.1038/embor.2008.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hanada T., Noda N.N., Satomi Y., Ichimura Y., Fujioka Y., Takao T., Inagaki F., Ohsumi Y. The Atg12-Atg5 conjugate has a novel E3-like activity for protein lipidation in autophagy. J. Biol. Chem. 2007;282:37298–37302. doi: 10.1074/jbc.C700195200. [DOI] [PubMed] [Google Scholar]
- 51.Kuma A., Mizushima N., Ishihara N., Ohsumi Y. Formation of the approximately 350-kDa Apg12-Apg5·Apg16 multimeric complex, mediated by Apg16 oligomerization, is essential for autophagy in yeast. J. Biol. Chem. 2002;277:18619–18625. doi: 10.1074/jbc.M111889200. [DOI] [PubMed] [Google Scholar]
- 52.Fujita N., Itoh T., Omori H., Fukuda M., Noda T., Yoshimori T. The Atg16L complex specifies the site of LC3 lipidation for membrane biogenesis in autophagy. Mol. Biol. Cell. 2008;19:2092–2100. doi: 10.1091/mbc.e07-12-1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Harris H., Rubinsztein D.C. Control of autophagy as a therapy for neurodegenerative disease. Nat. Rev. Neurol. 2011;8:108–117. doi: 10.1038/nrneurol.2011.200. [DOI] [PubMed] [Google Scholar]
- 54.Hosokawa N., Hara T., Kaizuka T., Kishi C., Takamura A., Miura Y., Iemura S., Natsume T., Takehana K., Yamada N., et al. Nutrient-dependent mTORC1 association with the ULK1-Atg13-FIP200 complex required for autophagy. Mol. Biol. Cell. 2009;20:1981–1991. doi: 10.1091/mbc.e08-12-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Park J.M., Jung C.H., Seo M., Otto N.M., Grunwald D., Kim K.H., Moriarity B., Kim Y.M., Starker C., Nho R.S., et al. The ULK1 complex mediates MTORC1 signaling to the autophagy initiation machinery via binding and phosphorylating ATG14. Autophagy. 2016;12:547–564. doi: 10.1080/15548627.2016.1140293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.de Duve C.W., Wattiaux R. Functions of Lysosomes. Annu. Rev. Physiol. 1966;28:435–492. doi: 10.1146/annurev.ph.28.030166.002251. [DOI] [PubMed] [Google Scholar]
- 57.Moeller C.H., Thompson W.W. An ultrastructural study of the yeast tonoplast during the shift from exponential to stationary phase. J. Ultrastruct. Res. 1979;68:28–37. doi: 10.1016/S0022-5320(79)90139-4. [DOI] [PubMed] [Google Scholar]
- 58.Campbell C.L., Thorsness P.E. Escape of mitochondrial DNA to the nucleus in yme1 yeast is mediated by vacuolar-dependent turnover of abnormal mitochondrial compartments. Pt 16J. Cell Sci. 1998;111:2455–2464. doi: 10.1242/jcs.111.16.2455. [DOI] [PubMed] [Google Scholar]
- 59.Tuttle D.L., Lewin A.S., Dunn W.A., Jr. Selective autophagy of peroxisomes in methylotrophic yeasts. Eur. J. Cell Biol. 1993;60:283–290. [PubMed] [Google Scholar]
- 60.Muller O., Sattler T., Flotenmeyer M., Schwarz H., Plattner H., Mayer A. Autophagic tubes: Vacuolar invaginations involved in lateral membrane sorting and inverse vesicle budding. J. Cell Biol. 2000;151:519–528. doi: 10.1083/jcb.151.3.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Uttenweiler A., Schwarz H., Neumann H., Mayer A. The vacuolar transporter chaperone (VTC) complex is required for microautophagy. Mol. Biol. Cell. 2007;18:166–175. doi: 10.1091/mbc.e06-08-0664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sattler T., Mayer A. Cell-free reconstitution of microautophagic vacuole invagination and vesicle formation. J. Cell Biol. 2000;151:529–538. doi: 10.1083/jcb.151.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sou Y.S., Waguri S., Iwata J., Ueno T., Fujimura T., Hara T., Sawada N., Yamada A., Mizushima N., Uchiyama Y., et al. The Atg8 conjugation system is indispensable for proper development of autophagic isolation membranes in mice. Mol. Biol. Cell. 2008;19:4762–4775. doi: 10.1091/mbc.e08-03-0309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ichimura Y., Kirisako T., Takao T., Satomi Y., Shimonishi Y., Ishihara N., Mizushima N., Tanida I., Kominami E., Ohsumi M., et al. A ubiquitin-like system mediates protein lipidation. Nature. 2000;408:488–492. doi: 10.1038/35044114. [DOI] [PubMed] [Google Scholar]
- 65.Uttenweiler A., Schwarz H., Mayer A. Microautophagic vacuole invagination requires calmodulin in a Ca2+-independent function. J. Biol. Chem. 2005;280:33289–33297. doi: 10.1074/jbc.M506086200. [DOI] [PubMed] [Google Scholar]
- 66.Tian Y., Li Z., Hu W., Ren H., Tian E., Zhao Y., Lu Q., Huang X., Yang P., Li X., et al. C. elegans screen identifies autophagy genes specific to multicellular organisms. Cell. 2010;141:1042–1055. doi: 10.1016/j.cell.2010.04.034. [DOI] [PubMed] [Google Scholar]
- 67.Yang Z., Klionsky D.J. Permeases recycle amino acids resulting from autophagy. Autophagy. 2007;3:149–150. doi: 10.4161/auto.3631. [DOI] [PubMed] [Google Scholar]
- 68.Roberts P., Moshitch-Moshkovitz S., Kvam E., O’Toole E., Winey M., Goldfarb D.S. Piecemeal microautophagy of nucleus in Saccharomyces cerevisiae. Mol. Biol. Cell. 2003;14:129–141. doi: 10.1091/mbc.e02-08-0483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Todde V., Veenhuis M., van der Klei I.J. Autophagy: Principles and significance in health and disease. Biochim. Biophys. Acta. 2009;1792:3–13. doi: 10.1016/j.bbadis.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 70.Dalby K.N., Tekedereli I., Lopez-Berestein G., Ozpolat B. Targeting the prodeath and prosurvival functions of autophagy as novel therapeutic strategies in cancer. Autophagy. 2010;6:322–329. doi: 10.4161/auto.6.3.11625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cuervo A.M. Autophagy: Many paths to the same end. Mol. Cell Biochem. 2004;263:55–72. doi: 10.1023/B:MCBI.0000041848.57020.57. [DOI] [PubMed] [Google Scholar]
- 72.Dubouloz F., Deloche O., Wanke V., Cameroni E., De Virgilio C. The TOR and EGO protein complexes orchestrate microautophagy in yeast. Mol. Cell. 2005;19:15–26. doi: 10.1016/j.molcel.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 73.Iwata A., Christianson J.C., Bucci M., Ellerby L.M., Nukina N., Forno L.S., Kopito R.R. Increased susceptibility of cytoplasmic over nuclear polyglutamine aggregates to autophagic degradation. Proc. Natl. Acad. Sci. USA. 2005;102:13135–13140. doi: 10.1073/pnas.0505801102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schuck S. Microautophagy—Distinct molecular mechanisms handle cargoes of many sizes. J. Cell Sci. 2020;133:jcs246322. doi: 10.1242/jcs.246322. [DOI] [PubMed] [Google Scholar]
- 75.Oku M., Maeda Y., Kagohashi Y., Kondo T., Yamada M., Fujimoto T., Sakai Y. Evidence for ESCRT- and clathrin-dependent microautophagy. J. Cell Biol. 2017;216:3263–3274. doi: 10.1083/jcb.201611029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sahu R., Kaushik S., Clement C.C., Cannizzo E.S., Scharf B., Follenzi A., Potolicchio I., Nieves E., Cuervo A.M., Santambrogio L. Microautophagy of cytosolic proteins by late endosomes. Dev. Cell. 2011;20:131–139. doi: 10.1016/j.devcel.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Oku M., Sakai Y. Three Distinct Types of Microautophagy Based on Membrane Dynamics and Molecular Machineries. Bioessays. 2018;40:e1800008. doi: 10.1002/bies.201800008. [DOI] [PubMed] [Google Scholar]
- 78.Schafer J.A., Schessner J.P., Bircham P.W., Tsuji T., Funaya C., Pajonk O., Schaeff K., Ruffini G., Papagiannidis D., Knop M., et al. ESCRT machinery mediates selective microautophagy of endoplasmic reticulum in yeast. EMBO J. 2020;39:e102586. doi: 10.15252/embj.2019102586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nixon R.A. Autophagy, amyloidogenesis and Alzheimer disease. J. Cell Sci. 2007;120:4081–4091. doi: 10.1242/jcs.019265. [DOI] [PubMed] [Google Scholar]
- 80.Martin-Aparicio E., Yamamoto A., Hernandez F., Hen R., Avila J., Lucas J.J. Proteasomal-dependent aggregate reversal and absence of cell death in a conditional mouse model of Huntington’s disease. J. Neurosci. 2001;21:8772–8781. doi: 10.1523/JNEUROSCI.21-22-08772.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Takikita S., Myerowitz R., Zaal K., Raben N., Plotz P.H. Murine muscle cell models for Pompe disease and their use in studying therapeutic approaches. Mol. Genet. Metab. 2009;96:208–217. doi: 10.1016/j.ymgme.2008.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bejarano E., Cuervo A.M. Chaperone-mediated autophagy. Proc. Am. Thorac. Soc. 2010;7:29–39. doi: 10.1513/pats.200909-102JS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kaushik S., Cuervo A.M. The coming of age of chaperone-mediated autophagy. Nat. Rev. Mol. Cell Biol. 2018;19:365–381. doi: 10.1038/s41580-018-0001-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cuervo A.M. Chaperone-mediated autophagy: Selectivity pays off. Trends Endocrinol. Metab. 2010;21:142–150. doi: 10.1016/j.tem.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chiang H.L., Terlecky S.R., Plant C.P., Dice J.F. A role for a 70-kilodalton heat shock protein in lysosomal degradation of intracellular proteins. Science. 1989;246:382–385. doi: 10.1126/science.2799391. [DOI] [PubMed] [Google Scholar]
- 86.Salvador N., Aguado C., Horst M., Knecht E. Import of a cytosolic protein into lysosomes by chaperone-mediated autophagy depends on its folding state. J. Biol. Chem. 2000;275:27447–27456. doi: 10.1016/S0021-9258(19)61529-2. [DOI] [PubMed] [Google Scholar]
- 87.Chiang H.L., Dice J.F. Peptide sequences that target proteins for enhanced degradation during serum withdrawal. J. Biol. Chem. 1988;263:6797–6805. doi: 10.1016/S0021-9258(18)68713-7. [DOI] [PubMed] [Google Scholar]
- 88.Dice J.F. Altered degradation of proteins microinjected into senescent human fibroblasts. J. Biol. Chem. 1982;257:14624–14627. doi: 10.1016/S0021-9258(18)33324-6. [DOI] [PubMed] [Google Scholar]
- 89.Dice J.F. Peptide sequences that target cytosolic proteins for lysosomal proteolysis. Trends Biochem. Sci. 1990;15:305–309. doi: 10.1016/0968-0004(90)90019-8. [DOI] [PubMed] [Google Scholar]
- 90.Park C., Suh Y., Cuervo A.M. Regulated degradation of Chk1 by chaperone-mediated autophagy in response to DNA damage. Nat. Commun. 2015;6:6823. doi: 10.1038/ncomms7823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Agarraberes F.A., Dice J.F. A molecular chaperone complex at the lysosomal membrane is required for protein translocation. J. Cell Sci. 2001;114:2491–2499. doi: 10.1242/jcs.114.13.2491. [DOI] [PubMed] [Google Scholar]
- 92.Bandyopadhyay U., Kaushik S., Varticovski L., Cuervo A.M. The chaperone-mediated autophagy receptor organizes in dynamic protein complexes at the lysosomal membrane. Mol. Cell Biol. 2008;28:5747–5763. doi: 10.1128/MCB.02070-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cuervo A.M., Terlecky S.R., Dice J.F., Knecht E. Selective binding and uptake of ribonuclease A and glyceraldehyde-3-phosphate dehydrogenase by isolated rat liver lysosomes. J. Biol. Chem. 1994;269:26374–26380. doi: 10.1016/S0021-9258(18)47204-3. [DOI] [PubMed] [Google Scholar]
- 94.Cuervo A.M., Dice J.F. A receptor for the selective uptake and degradation of proteins by lysosomes. Science. 1996;273:501–503. doi: 10.1126/science.273.5274.501. [DOI] [PubMed] [Google Scholar]
- 95.Cuervo A.M., Dice J.F. Unique properties of lamp2a compared to other lamp2 isoforms. Pt 24J. Cell Sci. 2000;113:4441–4450. doi: 10.1242/jcs.113.24.4441. [DOI] [PubMed] [Google Scholar]
- 96.Valdor R., Mocholi E., Botbol Y., Guerrero-Ros I., Chandra D., Koga H., Gravekamp C., Cuervo A.M., Macian F. Chaperone-mediated autophagy regulates T cell responses through targeted degradation of negative regulators of T cell activation. Nat. Immunol. 2014;15:1046–1054. doi: 10.1038/ni.3003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kiffin R., Christian C., Knecht E., Cuervo A.M. Activation of chaperone-mediated autophagy during oxidative stress. Mol. Biol. Cell. 2004;15:4829–4840. doi: 10.1091/mbc.e04-06-0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ferreira J.V., Fofo H., Bejarano E., Bento C.F., Ramalho J.S., Girao H., Pereira P. STUB1/CHIP is required for HIF1A degradation by chaperone-mediated autophagy. Autophagy. 2013;9:1349–1366. doi: 10.4161/auto.25190. [DOI] [PubMed] [Google Scholar]
- 99.Hubbi M.E., Gilkes D.M., Hu H., Kshitiz A.I., Semenza G.L. Cyclin-dependent kinases regulate lysosomal degradation of hypoxia-inducible factor 1alpha to promote cell-cycle progression. Proc. Natl. Acad. Sci. USA. 2014;111:E3325–E3334. doi: 10.1073/pnas.1412840111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bandyopadhyay U., Sridhar S., Kaushik S., Kiffin R., Cuervo A.M. Identification of regulators of chaperone-mediated autophagy. Mol. Cell. 2010;39:535–547. doi: 10.1016/j.molcel.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yang G., Murashige D.S., Humphrey S.J., James D.E. A Positive Feedback Loop between Akt and mTORC2 via SIN1 Phosphorylation. Cell Rep. 2015;12:937–943. doi: 10.1016/j.celrep.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 102.Arias E., Koga H., Diaz A., Mocholi E., Patel B., Cuervo A.M. Lysosomal mTORC2/PHLPP1/Akt Regulate Chaperone-Mediated Autophagy. Mol. Cell. 2015;59:270–284. doi: 10.1016/j.molcel.2015.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Endicott S.J., Ziemba Z.J., Beckmann L.J., Boynton D.N., Miller R.A. Inhibition of class I PI3K enhances chaperone-mediated autophagy. J. Cell Biol. 2020;219:e202001031. doi: 10.1083/jcb.202001031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Schneider J.L., Suh Y., Cuervo A.M. Deficient chaperone-mediated autophagy in liver leads to metabolic dysregulation. Cell Metab. 2014;20:417–432. doi: 10.1016/j.cmet.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cuervo A.M., Knecht E., Terlecky S.R., Dice J.F. Activation of a selective pathway of lysosomal proteolysis in rat liver by prolonged starvation. Pt 1Am. J. Physiol. 1995;269:C1200–C1208. doi: 10.1152/ajpcell.1995.269.5.C1200. [DOI] [PubMed] [Google Scholar]
- 106.Singh R., Kaushik S., Wang Y., Xiang Y., Novak I., Komatsu M., Tanaka K., Cuervo A.M., Czaja M.J. Autophagy regulates lipid metabolism. Nature. 2009;458:1131–1135. doi: 10.1038/nature07976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kon M., Kiffin R., Koga H., Chapochnick J., Macian F., Varticovski L., Cuervo A.M. Chaperone-mediated autophagy is required for tumor growth. Sci. Transl. Med. 2011;3:109ra117. doi: 10.1126/scitranslmed.3003182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kaushik S., Cuervo A.M. AMPK-dependent phosphorylation of lipid droplet protein PLIN2 triggers its degradation by CMA. Autophagy. 2016;12:432–438. doi: 10.1080/15548627.2015.1124226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cuervo A.M., Hu W., Lim B., Dice J.F. IkappaB is a substrate for a selective pathway of lysosomal proteolysis. Mol. Biol. Cell. 1998;9:1995–2010. doi: 10.1091/mbc.9.8.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang L., Sun Y., Fei M., Tan C., Wu J., Zheng J., Tang J., Sun W., Lv Z., Bao J., et al. Disruption of chaperone-mediated autophagy-dependent degradation of MEF2A by oxidative stress-induced lysosome destabilization. Autophagy. 2014;10:1015–1035. doi: 10.4161/auto.28477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hu M.M., Yang Q., Xie X.Q., Liao C.Y., Lin H., Liu T.T., Yin L., Shu H.B. Sumoylation Promotes the Stability of the DNA Sensor cGAS and the Adaptor STING to Regulate the Kinetics of Response to DNA Virus. Immunity. 2016;45:555–569. doi: 10.1016/j.immuni.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 112.Cuervo A.M., Dice J.F. Age-related decline in chaperone-mediated autophagy. J. Biol. Chem. 2000;275:31505–31513. doi: 10.1074/jbc.M002102200. [DOI] [PubMed] [Google Scholar]
- 113.Kiffin R., Kaushik S., Zeng M., Bandyopadhyay U., Zhang C., Massey A.C., Martinez-Vicente M., Cuervo A.M. Altered dynamics of the lysosomal receptor for chaperone-mediated autophagy with age. J. Cell Sci. 2007;120:782–791. doi: 10.1242/jcs.001073. [DOI] [PubMed] [Google Scholar]
- 114.Zhang C., Cuervo A.M. Restoration of chaperone-mediated autophagy in aging liver improves cellular maintenance and hepatic function. Nat. Med. 2008;14:959–965. doi: 10.1038/nm.1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Venugopal B., Mesires N.T., Kennedy J.C., Curcio-Morelli C., Laplante J.M., Dice J.F., Slaugenhaupt S.A. Chaperone-mediated autophagy is defective in mucolipidosis type IV. J. Cell Physiol. 2009;219:344–353. doi: 10.1002/jcp.21676. [DOI] [PubMed] [Google Scholar]
- 116.Huang C.C., Bose J.K., Majumder P., Lee K.H., Huang J.T., Huang J.K., Shen C.K. Metabolism and mis-metabolism of the neuropathological signature protein TDP-43. Pt 14J. Cell Sci. 2014;127:3024–3038. doi: 10.1242/jcs.136150. [DOI] [PubMed] [Google Scholar]
- 117.Xilouri M., Brekk O.R., Polissidis A., Chrysanthou-Piterou M., Kloukina I., Stefanis L. Impairment of chaperone-mediated autophagy induces dopaminergic neurodegeneration in rats. Autophagy. 2016;12:2230–2247. doi: 10.1080/15548627.2016.1214777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cuervo A.M., Stefanis L., Fredenburg R., Lansbury P.T., Sulzer D. Impaired degradation of mutant alpha-synuclein by chaperone-mediated autophagy. Science. 2004;305:1292–1295. doi: 10.1126/science.1101738. [DOI] [PubMed] [Google Scholar]
- 119.Saha T. LAMP2A overexpression in breast tumors promotes cancer cell survival via chaperone-mediated autophagy. Autophagy. 2012;8:1643–1656. doi: 10.4161/auto.21654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ali A.B., Nin D.S., Tam J., Khan M. Role of chaperone mediated autophagy (CMA) in the degradation of misfolded N-CoR protein in non-small cell lung cancer (NSCLC) cells. PLoS ONE. 2011;6:e25268. doi: 10.1371/journal.pone.0025268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chava S., Lee C., Aydin Y., Chandra P.K., Dash A., Chedid M., Thung S.N., Moroz K., Wu T., Nayak N.C., et al. Chaperone-mediated autophagy compensates for impaired macroautophagy in the cirrhotic liver to promote hepatocellular carcinoma. Oncotarget. 2017;8:40019–40036. doi: 10.18632/oncotarget.16685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhou J., Yang J., Fan X., Hu S., Zhou F., Dong J., Zhang S., Shang Y., Jiang X., Guo H., et al. Chaperone-mediated autophagy regulates proliferation by targeting RND3 in gastric cancer. Autophagy. 2016;12:515–528. doi: 10.1080/15548627.2015.1136770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Xie W., Zhang L., Jiao H., Guan L., Zha J., Li X., Wu M., Wang Z., Han J., You H. Chaperone-mediated autophagy prevents apoptosis by degrading BBC3/PUMA. Autophagy. 2015;11:1623–1635. doi: 10.1080/15548627.2015.1075688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lu T.L., Huang G.J., Wang H.J., Chen J.L., Hsu H.P., Lu T.J. Hispolon promotes MDM2 downregulation through chaperone-mediated autophagy. Biochem. Biophys. Res. Commun. 2010;398:26–31. doi: 10.1016/j.bbrc.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 125.Gomes L.R., Menck C.F.M., Cuervo A.M. Chaperone-mediated autophagy prevents cellular transformation by regulating MYC proteasomal degradation. Autophagy. 2017;13:928–940. doi: 10.1080/15548627.2017.1293767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ke P.Y. Diverse Functions of Autophagy in Liver Physiology and Liver Diseases. Int. J. Mol. Sci. 2019;20:300. doi: 10.3390/ijms20020300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Codogno P., Meijer A.J. Autophagy in the liver. J. Hepatol. 2013;59:389–391. doi: 10.1016/j.jhep.2013.02.031. [DOI] [PubMed] [Google Scholar]
- 128.Pfeifer U. Cellular autophagy: Glycogen segregation in early stages of a partial liver atrophy. Virchows Arch. B Cell Pathol. 1970;5:242–253. doi: 10.1007/BF02893566. [DOI] [PubMed] [Google Scholar]
- 129.Schworer C.M., Mortimore G.E. Glucagon-induced autophagy and proteolysis in rat liver: Mediation by selective deprivation of intracellular amino acids. Proc. Natl. Acad. Sci. USA. 1979;76:3169–3173. doi: 10.1073/pnas.76.7.3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Schworer C.M., Shiffer K.A., Mortimore G.E. Quantitative relationship between autophagy and proteolysis during graded amino acid deprivation in perfused rat liver. J. Biol. Chem. 1981;256:7652–7658. doi: 10.1016/S0021-9258(19)69010-1. [DOI] [PubMed] [Google Scholar]
- 131.Efeyan A., Zoncu R., Chang S., Gumper I., Snitkin H., Wolfson R.L., Kirak O., Sabatini D.D., Sabatini D.M. Regulation of mTORC1 by the Rag GTPases is necessary for neonatal autophagy and survival. Nature. 2013;493:679–683. doi: 10.1038/nature11745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Meijer A.J., Codogno P. Autophagy: Regulation and role in disease. Crit. Rev. Clin. Lab. Sci. 2009;46:210–240. doi: 10.1080/10408360903044068. [DOI] [PubMed] [Google Scholar]
- 133.Czaja M.J. Functions of autophagy in hepatic and pancreatic physiology and disease. Gastroenterology. 2011;140:1895–1908. doi: 10.1053/j.gastro.2011.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hendy R., Grasso P. Autophagy in acute liver damage produced in the rat by dimethylnitrosamine. Chem. Biol. Interact. 1972;5:401–413. doi: 10.1016/0009-2797(72)90077-4. [DOI] [PubMed] [Google Scholar]
- 135.Hidvegi T., Ewing M., Hale P., Dippold C., Beckett C., Kemp C., Maurice N., Mukherjee A., Goldbach C., Watkins S., et al. An autophagy-enhancing drug promotes degradation of mutant alpha1-antitrypsin Z and reduces hepatic fibrosis. Science. 2010;329:229–232. doi: 10.1126/science.1190354. [DOI] [PubMed] [Google Scholar]
- 136.Lavallard V.J., Gual P. Autophagy and non-alcoholic fatty liver disease. Biomed. Res. Int. 2014;2014:120179. doi: 10.1155/2014/120179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wu W.K.K., Zhang L., Chan M.T.V. Autophagy, NAFLD and NAFLD-Related HCC. Adv. Exp. Med. Biol. 2018;1061:127–138. doi: 10.1007/978-981-10-8684-7_10. [DOI] [PubMed] [Google Scholar]
- 138.Gonzalez-Rodriguez A., Mayoral R., Agra N., Valdecantos M.P., Pardo V., Miquilena-Colina M.E., Vargas-Castrillon J., Lo Iacono O., Corazzari M., Fimia G.M., et al. Impaired autophagic flux is associated with increased endoplasmic reticulum stress during the development of NAFLD. Cell Death Dis. 2014;5:e1179. doi: 10.1038/cddis.2014.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yang L., Li P., Fu S., Calay E.S., Hotamisligil G.S. Defective hepatic autophagy in obesity promotes ER stress and causes insulin resistance. Cell Metab. 2010;11:467–478. doi: 10.1016/j.cmet.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Liu H.Y., Han J., Cao S.Y., Hong T., Zhuo D., Shi J., Liu Z., Cao W. Hepatic autophagy is suppressed in the presence of insulin resistance and hyperinsulinemia: Inhibition of FoxO1-dependent expression of key autophagy genes by insulin. J. Biol. Chem. 2009;284:31484–31492. doi: 10.1074/jbc.M109.033936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Settembre C., De Cegli R., Mansueto G., Saha P.K., Vetrini F., Visvikis O., Huynh T., Carissimo A., Palmer D., Klisch T.J., et al. TFEB controls cellular lipid metabolism through a starvation-induced autoregulatory loop. Nat. Cell Biol. 2013;15:647–658. doi: 10.1038/ncb2718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lin C.W., Zhang H., Li M., Xiong X., Chen X., Chen X., Dong X.C., Yin X.M. Pharmacological promotion of autophagy alleviates steatosis and injury in alcoholic and non-alcoholic fatty liver conditions in mice. J. Hepatol. 2013;58:993–999. doi: 10.1016/j.jhep.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Amir M., Czaja M.J. Autophagy in nonalcoholic steatohepatitis. Expert Rev. Gastroenterol. Hepatol. 2011;5:159–166. doi: 10.1586/egh.11.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Qu X., Yu J., Bhagat G., Furuya N., Hibshoosh H., Troxel A., Rosen J., Eskelinen E.L., Mizushima N., Ohsumi Y., et al. Promotion of tumorigenesis by heterozygous disruption of the beclin 1 autophagy gene. J. Clin. Investig. 2003;112:1809–1820. doi: 10.1172/JCI20039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yue Z., Jin S., Yang C., Levine A.J., Heintz N. Beclin 1, an autophagy gene essential for early embryonic development, is a haploinsufficient tumor suppressor. Proc. Natl. Acad. Sci. USA. 2003;100:15077–15082. doi: 10.1073/pnas.2436255100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ding Z.B., Shi Y.H., Zhou J., Qiu S.J., Xu Y., Dai Z., Shi G.M., Wang X.Y., Ke A.W., Wu B., et al. Association of autophagy defect with a malignant phenotype and poor prognosis of hepatocellular carcinoma. Cancer Res. 2008;68:9167–9175. doi: 10.1158/0008-5472.CAN-08-1573. [DOI] [PubMed] [Google Scholar]
- 147.Tanaka S., Hikita H., Tatsumi T., Sakamori R., Nozaki Y., Sakane S., Shiode Y., Nakabori T., Saito Y., Hiramatsu N., et al. Rubicon inhibits autophagy and accelerates hepatocyte apoptosis and lipid accumulation in nonalcoholic fatty liver disease in mice. Hepatology. 2016;64:1994–2014. doi: 10.1002/hep.28820. [DOI] [PubMed] [Google Scholar]
- 148.Takakura K., Oikawa T., Nakano M., Saeki C., Torisu Y., Kajihara M., Saruta M. Recent Insights into the Multiple Pathways Driving Non-alcoholic Steatohepatitis-Derived Hepatocellular Carcinoma. Front. Oncol. 2019;9:762. doi: 10.3389/fonc.2019.00762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Inokuchi-Shimizu S., Park E.J., Roh Y.S., Yang L., Zhang B., Song J., Liang S., Pimienta M., Taniguchi K., Wu X., et al. TAK1-mediated autophagy and fatty acid oxidation prevent hepatosteatosis and tumorigenesis. J. Clin. Investig. 2014;124:3566–3578. doi: 10.1172/JCI74068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhang W., Hou J., Wang X., Jiang R., Yin Y., Ji J., Deng L., Huang X., Wang K., Sun B. PTPRO-mediated autophagy prevents hepatosteatosis and tumorigenesis. Oncotarget. 2015;6:9420–9433. doi: 10.18632/oncotarget.3353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Oka T., Hikoso S., Yamaguchi O., Taneike M., Takeda T., Tamai T., Oyabu J., Murakawa T., Nakayama H., Nishida K., et al. Mitochondrial DNA that escapes from autophagy causes inflammation and heart failure. Nature. 2012;485:251–255. doi: 10.1038/nature10992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Nakahira K., Haspel J.A., Rathinam V.A., Lee S.J., Dolinay T., Lam H.C., Englert J.A., Rabinovitch M., Cernadas M., Kim H.P., et al. Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nat. Immunol. 2011;12:222–230. doi: 10.1038/ni.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mathew R., Karp C.M., Beaudoin B., Vuong N., Chen G., Chen H.Y., Bray K., Reddy A., Bhanot G., Gelinas C., et al. Autophagy suppresses tumorigenesis through elimination of p62. Cell. 2009;137:1062–1075. doi: 10.1016/j.cell.2009.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Liu W.J., Ye L., Huang W.F., Guo L.J., Xu Z.G., Wu H.L., Yang C., Liu H.F. p62 links the autophagy pathway and the ubiqutin-proteasome system upon ubiquitinated protein degradation. Cell Mol. Biol. Lett. 2016;21:29. doi: 10.1186/s11658-016-0031-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Komatsu M. Liver autophagy: Physiology and pathology. J. Biochem. 2012;152:5–15. doi: 10.1093/jb/mvs059. [DOI] [PubMed] [Google Scholar]
- 156.Wang Z., Han W., Sui X., Fang Y., Pan H. Autophagy: A novel therapeutic target for hepatocarcinoma (Review) Oncol. Lett. 2014;7:1345–1351. doi: 10.3892/ol.2014.1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Czaja M.J. Function of Autophagy in Nonalcoholic Fatty Liver Disease. Dig. Dis. Sci. 2016;61:1304–1313. doi: 10.1007/s10620-015-4025-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Udoh U.S., Banerjee M., Rajan P.K., Sanabria J.D., Smith G., Schade M., Sanabria J.A., Nakafuku Y., Sodhi K., Pierre S.V., et al. Tumor-Suppressor Role of the alpha1-Na/K-ATPase Signalosome in NASH Related Hepatocellular Carcinoma. Int. J. Mol. Sci. 2022;23:7359. doi: 10.3390/ijms23137359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No applicable.