Abstract
Background
There are disparities in surgical outcomes for patients of low socioeconomic status globally, including in countries with universal healthcare systems. There is limited data on the impact of low socioeconomic status on surgical outcomes in Australia. This study examines surgical outcomes by both self‐reported unemployment and neighbourhood level socioeconomic status in Australia.
Methods
A retrospective administrative data review was conducted at a tertiary care centre over a 10‐year period (2008–2018) including all adult surgical patients. Multivariable logistic regression adjusting for year, age, sex and Charlson Comorbidity Index was performed.
Results
106 197 patients underwent a surgical procedure in the decade examined. The overall adverse event rates were mortality (1.13%), total postoperative complications (10.9%), failure to rescue (0.75%) and return to theatre (4.31%). Following multivariable testing, unemployed and low socioeconomic patients had a higher risk of postoperative mortality (OR 2.06 (1.50–2.82), OR 1.37 (1.15–1.64)), all complications (OR 1.43 (1.31–1.56), OR 1.21 (1.14–1.28)), failure to rescue (OR 2.03 (1.39–2.95), OR 1.38 (1.11–1.72)) and return to theatre (OR 1.42 (1.27–1.59), OR 1.24 (1.14–1.36)) (P < 0.005 for all).
Conclusions
Despite universal healthcare, there are disparities in surgical adverse events for patients of low socioeconomic status in Australia. Disparities in surgical outcomes can stem from three facets: a patient's access to healthcare (the severity of disease at the time of presentation), variation in perioperative care delivery, and social determinants of health. Further work is required to pinpoint why these disparities are present and to evaluate the impact of strategies that aim to reduce disparities.
Keywords: disparities, socioeconomic status, surgery, surgical outcomes, unemployed
Association between unemployment/socioeconomic disadvantage and surgical adverse events
Introduction
There is a well‐established link between low socioeconomic status and increased morbidity and mortality. 1 , 2 , 3 In the United States (US), patients with a low socioeconomic status have higher rates of postoperative complications, mortality, failure to rescue and readmissions. 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 Some studies suggest that these disparities may be attributable to inequalities in the US healthcare system, rather than differential treatment of patients within individual care settings. 9 , 15 Hospitals disproportionately treating patients with lower socioeconomic status have worse outcomes when compared to other hospitals. 9
One might expect that countries with universal healthcare settings may not encounter socioeconomic disparities in surgical outcomes. However, studies conducted in several countries with universal healthcare systems, including the United Kingdom, 16 , 17 , 18 Finland, 19 the Netherlands, 20 Italy 21 and New Zealand, 22 have found disparities in surgical outcomes for patients of low socioeconomic status.
There are limited studies examining surgical outcomes by socioeconomic status in Australia. This study aimed to examine surgical outcomes by both self‐reported unemployment and a neighbourhood level socioeconomic index at a regional tertiary care centre in Australia.
Methods
Study design
A retrospective study was conducted at a regional tertiary care centre in Queensland, Australia. Data were examined over a 10‐year period between January 2008 and August 2018. All adult (ages >18 years) patients who underwent a surgical procedure at this centre were included. The Townsville Hospital and Health Service Human Research Ethics Committee in Australia granted ethics approval (HREC/QTHS/57820). This approval included a patient consent waiver due to the retrospective study design.
Data source
Two hospital‐based databases were utilized. The Operating Room Management Information System (ORMIS) was used to extract operative details for all surgical procedures performed. Patient identification numbers were then matched to the Hospital Based Corporate Information System (HBCIS) to extract further administrative hospital data.
Socioeconomic status variables
HBCIS includes a free text self‐reported occupation variable. This variable was used to identify responses indicating unemployment. Various synonyms for unemployment, spellings of unemployment and names of unemployment social security benefits (Job Seeker, working for the Dole and Newstart) were included. Only those in the labour force were coded as unemployed; those indicating that they were not in the labour force (e.g., disability support/pensions, stay at home parents, students, retirees or pensioners) were not coded as unemployed.
To attain a neighbourhood marker of socioeconomic status, a patient's residential address was linked to 2016 Census tract Index of Economic Resources (IER) data. 23 This index focuses on financial aspects of socioeconomic advantage and disadvantage. For this study, the bottom three national IER deciles (those with the greatest relative lack of access to economic resources) were compared to the top three national deciles.
Outcomes
Operative mortality was defined as the rate of death occurring in the hospital or within 30 days of surgery. Complications included one or more occurrences of postoperative acute renal failure, acute myocardial infarction, bleeding requiring transfusion of four or more units of red cells within the first 72 h of surgery, cardiac arrest requiring cardiopulmonary resuscitation, coma of 24 h duration or more, deep vein thrombosis, fever, unplanned intubation or ventilation use for more than 48 h, pneumonia, pulmonary embolism, respiratory failure, major wound disruption, surgical site infection, sepsis or the systemic inflammatory response syndrome, septic shock, or return to the operating theatre. The occurrence of one or more of the above listed complications was counted as the total complication rate for each procedure. Failure to rescue is the inability to rescue a patient from death after a postoperative complication. 7 Failure to rescue was coded as those with both a postoperative complications and postoperative mortality. Rates of unplanned readmission within 28 days after discharge were also examined.
Covariates
The Charlson Comorbidity Index (CCI) was used to adjust for pre‐existing comorbidities. The index includes myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, mild liver disease, diabetes with/without chronic complications, hemiplegia or paraplegia, renal disease, any malignancy including lymphoma and leukaemia (except malignant neoplasm of the skin), moderate or severe liver disease, metastatic solid tumour and AIDS/HIV. These variables were derived using ICD 10‐AM (Australian modification) diagnosis codes assigned during the episode of care. 24 A weighted score was then assigned to each comorbidity. A score of zero indicates that no comorbidities were found, the higher the score, the more comorbidities were identified.
Statistical analysis
For group comparisons, Pearson's chi‐squared tests were used for categorical variables, while continuous variables were analysed with analysis of variance (ANOVA) tests. Multivariable logistic regression models based on a conceptual model were used. The first analysis included the independent variables procedure year, patient age, sex and CCI. The second analysis also included adjustment for emergency surgery status. These regressions were performed once for each outcome examined (e.g., mortality, all complications, FTR etc.). Area under the curve (AUC) with 95% confidence intervals were calculated for all regression models.
All analyses were performed using Stata 14/MP statistical software package (StataCorp, College Station, TX). All tests were done two‐sided. The level of significance was set to 0.05.
Results
A total of 106 197 patients underwent a surgical procedure between 2008 and 2018. The overall mortality rate was 1.13% (1198), postoperative complication rate was 10.9% (11 606), failure to rescue rate was 0.75% (792) and the readmission rate was 5.45% (5790). The six individual complications with the highest rates were examined individually; return to theatre rate (4.31%), bleeding (5.76%), intubation (1.57%), acute renal failure (0.96%), fever (0.94%), pneumonia (0.6%) and surgical site infection (0.46%) (Table 1).
Table 1.
Demographics of study population
| Characteristic | Overall | Occupation | Index of economic resources | ||||
|---|---|---|---|---|---|---|---|
| Other | Unemployed | P‐value | Advantaged | Disadvantaged | P‐value | ||
| n = 106 197 | n = 100 554 (94.7%) | n = 5643 (5.31%) | n = 24 948 (23.5%) | n = 28 189 (26.6%) | |||
| Age | |||||||
| Median, n (IQR) | 51 (34–67) | 52 (35–68) | 37 (27–49) | <0.001 | 54 (37–68) | 46 (31–63) | <0.001 |
| Mean, n (SD) | 51 (19) | 52 (19) | 38 (13) | 53 (19) | 48 (19) | ||
| Sex, n (%) | |||||||
| Male | 48 064 (45.3) | 44 380 (44.1) | 3684 (65.3) | <0.001 | 10 385 (41.6) | 13 698 (48.6) | <0.001 |
| Charlson Comorbidity Index, n (SD) | |||||||
| Mean | 0.37 (1.04) | 0.38 (1.05) | 0.31 (0.92) | <0.001 | 0.32 (0.97) | 0.42 (1.10) | <0.001 |
| Admission status, n (%) | |||||||
| Emergency | 27 329 (25.7) | 25 041 (24.9) | 2315 (41.0) | <0.001 | 6151 (24.7) | 7855 (27.9) | <0.001 |
| Outcomes, n (%) | |||||||
| Mortality | 1198 (1.13) | 1152 (1.15) | 46 (0.82) | 0.022 | 201 (0.81) | 393 (1.39) | <0.001 |
| All complications | 11 606 (10.9) | 10 894 (10.8) | 712 (12.62) | <0.001 | 2362 (9.47) | 3528 (12.5) | <0.001 |
| Failure to rescue | 792 (0.75) | 760 (0.76) | 32 (0.57) | 0.109 | 129 (0.52) | 255 (0.90) | <0.001 |
| Return to theatre | 4582 (4.31) | 4205 (4.18) | 377 (6.68) | <0.001 | 919 (3.68) | 1391 (4.93) | <0.001 |
| Bleeding | 6116 (5.76) | 5818 (5.79) | 298 (5.28) | 0.113 | 1249 (5.01) | 1879 (6.67) | <0.001 |
| Intubation | 1662 (1.57) | 1501 (1.49) | 161 (2.85) | <0.001 | 329 (1.32) | 578 (2.05) | <0.001 |
| Acute renal failure | 1019 (0.96) | 980 (0.97) | 39 (0.69) | 0.034 | 207 (0.83) | 309 (1.10) | 0.002 |
| Fever | 999 (0.94) | 940 (0.93) | 59 (1.05) | 0.402 | 201 (0.81) | 294 (1.04) | 0.004 |
| Pneumonia | 636 (0.60) | 600 (0.60) | 36 (0.64) | 0.696 | 136 (0.55) | 207 (0.73) | 0.007 |
| Surgical site infection | 493 (0.46) | 462 (0.46) | 31 (0.55) | 0.334 | 89 (0.36) | 165 (0.59) | <0.001 |
| Readmission | 5790 (5.45) | 5434 (5.4) | 356 (6.31) | 0.004 | 1453 (5.82) | 1547 (5.49) | 0.094 |
Statistically significant figures are bolded
Those who were unemployed were younger (mean age 37 vs. 52, P < 0.001), more likely to be male (65.3% vs. 44.1%, P < 0.001), had a lower mean CCI (0.31 vs. 0.38, P < 0.001) and were more likely to be admitted on an emergency basis (41.0% vs. 24.9%, P < 0.001). Patients who were unemployed had higher rates of all complications (12.6% vs. 10.8%, P < 0.001), return to theatre (6.68% vs. 4.18%, P < 0.001), intubation (2.85% vs. 1.49%, P < 0.001) and readmission (6.31% vs. 5.4%, P = 0.004). Patients who were unemployed had a lower rate of mortality (0.82% vs. 1.15%, P = 0.022) and acute renal failure (0.69% vs. 0.97%, P = 0.034).
Those who resided in an area of disadvantaged IER were younger (mean age 48 vs. 53, P < 0.001), more likely to be male (48.6% vs. 41.6%, P < 0.001), had a higher mean CCI (0.42 vs. 0.32, P < 0.001) and were more likely to be admitted on an emergency basis (27.9% vs. 24.7%, P < 0.001). Patients residing in a disadvantaged IER area had significantly (P < 0.05) higher rates of mortality (1.39% vs. 0.81%), all complications (12.5% vs. 9.47%), failure to rescue (0.90% vs. 0.52%), return to theatre (4.93% vs. 3.63%), bleeding (6.67% vs. 5.01%), intubation (2.05% vs. 1.32%), acute renal failure (1.1% vs. 0.83%), fever (1.04% vs. 0.81%) and surgical site infection (0.59% vs. 0.36%).
The association between unemployment and outcomes
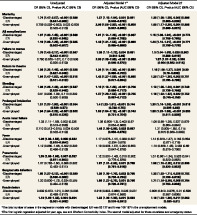
Following multivariate testing, unemployed patients had a higher risk of postoperative mortality (OR 2.06 (1.5–2.82), P < 0.001), all complications (OR 1.43 (1.31–1.56), P < 0.001), failure to rescue (OR 2.03 (1.39–2.95), P < 0.001) and 30‐day readmission (OR 1.22 (1.09–1.36), P = 0.001). When specific postoperative outcomes were examined individually, unemployed patients had higher rates of return to theatre (OR 1.42 (1.27–1.59), P < 0.001), bleeding (OR 1.37 (1.2–1.55), P < 0.001), intubation (OR 1.83 (1.54–2.18), P < 0.001), acute renal failure (OR 1.48 (1.06–2.08), P = 0.023), pneumonia (OR 1.87 (1.31–2.66), P < 0.001) and surgical site infection (OR 1.86 (1.27–2.73), P = 0.001). The only outcome examined where there was no significant variation for unemployed patients was postoperative fever. Most findings remained significant after adjusting for emergency surgery status, a marker for surgical access – the one exception was acute renal failure, this disparity was no longer significant after adjustment for emergency status.
The association between disadvantaged IER and outcomes
Patients residing in disadvantaged IER areas had a higher risk of postoperative mortality (OR 1.37 (1.15–1.64), P = 0.001), complications (OR 1.21 (1.14–1.28), P < 0.001) and failure to rescue (OR 1.38 (1.11–1.72), P = 0.004). When specific postoperative outcomes were examined individually, patients residing in disadvantaged IER areas had higher rates of return to theatre (OR 1.24 (1.14–1.36), P < 0.001), bleeding (OR 1.19 (1.1–1.28), P < 0.001), intubation (OR 1.4 (1.22–1.61), P < 0.001) and surgical site infection (OR 1.36 (1.05–1.76), P = 0.022). There were no significant variations in acute renal failure, fever, or pneumonia. Those residing in disadvantaged IER areas had lower rates of readmission (OR 0.918 (0.852–0.989), p = 0.025). All findings remained significant after adjusting for emergency surgery status.
Area under the curve
The AUC was overall low in univariate regressions and much higher in the multivariate regression (Table 2).
Table 2.
Association between unemployment/socioeconomic disadvantage and surgical adverse events
| Unadjusted | Adjusted Model 1* | Adjusted Model 2† | |
|---|---|---|---|
| OR (95% CI), P‐value (AUC (95% CI)) | OR (95% CI), P‐value (AUC (95% CI)) | OR (95% CI), P‐value (AUC (95% CI)) | |
| Mortality | |||
| ‐Disadvantaged IER | 1.74 (1.47–2.07), <0.001 (0.566 (0.547–0.586)] | 1.37 (1.15–1.64), 0.001 (0.861 (0.846–0.876)) | 1.30 (1.08–1.56), 0.005 (0.896 (0.883–0.909)) |
| ‐Unemployed | 0.709 (0.528–0.953), 0.023 (0.508 (0.502–0.513)) | 2.06 (1.50–2.82), <0.001 (0.858 (0.847–0.869)) | 1.60 (1.17–2.20), 0.004 (0.898 (0.889–0.907)) |
| All complications | |||
| ‐Disadvantaged IER | 1.37 (1.30–1.45), <0.001 (0.539 (0.532–0.545)) | 1.21 (1.14–1.28), <0.001 (0.697 (0.689–0.705)) | 1.15 (1.08–1.22), <0.001 (0.774 (0.766–0.780)) |
| ‐Unemployed | 1.19 (1.09–1.29), <0.001 (0.505 (0.502–0.507)) | 1.43 (1.31–1.56), <0.001 (0.690 (0.685–0.696)) | 1.20 (1.10–1.31), <0.001 (0.771 (0.766–0.776)) |
| Failure to rescue | |||
| ‐Disadvantaged IER | 1.76 (1.42–2.17), <0.001 (0.567 (0.543–0.591)) | 1.38 (1.11–1.72), 0.004 (0.861 (0.841–0.88) | 1.3 (1.04–1.63), 0.020 (0.903 (0.888–0.919)) |
| ‐Unemployed | 0.750 (0.525–1.07), 0.110 (0.506 (0.500–0.513)) | 2.03 (1.39–2.95), <0.001 (0.859 (0.845–0.872)) |
1.57 (1.07–2.28), 0.020 (0.904 (0.893–0.914)) |
| Return to theatre | |||
| ‐Disadvantaged IER | 1.36 (1.25–1.48), <0.001 (0.538 (0.527–0.548)) | 1.24 (1.14–1.36), <0.001 (0.691 (0.680–0.703)) | 1.16 (1.06–1.27), 0.001 (0.80 (0.79–0.809)) |
| ‐Unemployed | 1.64 (1.47–1.83), <0.001 (0.515 (0.511–0.519)) | 1.42 (1.27–1.59), <0.001 (0.685 (0.677–0.694)) | 1.20 (1.07–1.35), 0.002 (0.791 (0.785–0.798)) |
| Bleeding | |||
| ‐Disadvantaged IER | 1.36 (1.26–1.46), <0.001 (0.537 (0.528–0.546)) | 1.19 (1.10–1.28), <0.001 (0.706 (0.696–0.717)) | 1.13 (1.05–1.23), 0.001 (0.749 (0.739–0.758)) |
| ‐Unemployed | 0.91 (0.805–1.02), 0.113 (0.502 (0.500–0.505)) | 1.37 (1.20–1.55), <0.001 (0.705 (0.697–0.712)) | 1.16 (1.02–1.32), 0.022 (0.752 (0.745–0.759) |
| Prolonged intubation | |||
| ‐Disadvantaged IER | 1.57 (1.37–1.80), <0.001 (0.554 (0.539–0.57)) | 1.4 (1.22–1.61), <0.001 (0.744 (0.728–0.76)) | 1.33 (1.16–1.53), <0.001 (0.818 (0.805–0.83)) |
| ‐Unemployed | 1.94 (1.64–2.29), <0.001 (0.522 (0.515–0.529)) | 1.83 (1.54–2.18), <0.001 (0.743 (0.731–0.754)) | 1.58 (1.32–1.88), <0.001 (0.820 (0.811–0.829)) |
| Acute renal failure | |||
| ‐Disadvantaged IER | 1.33 (1.11–1.58), 0.002 (0.535 (0.513–0.556)) | 1.08 (0.900–1.3), 0.403 (0.87 (0.854–0.886)) | 1.06 (0.88–1.28), 0.527 (0.879 (0.864–0.894)) |
| ‐Unemployed | 0.710 (0.513–0.975), 0.034 (0.508 (0.502–0.513)) | 1.48 (1.06–2.08), 0.023 (0.867 (0.856–0.878)) |
1.31 (0.935–1.85), 0.115 (0.879 (0.868–0.889)) |
| Fever | |||
| ‐Disadvantaged IER | 1.29 (1.08–1.55), 0.005 (0.532 (0.510–0.554)) | 1.17 (0.976–1.41), 0.089 (0.657 (0.634–0.679) | 1.14 (0.949–1.37), 0.163 (0.693 (0.671–0.715) |
| ‐Unemployed | 1.12 (0.860–1.46), 0.402 (0.503 (0.496–0.510)) | 1.19 (0.908–1.57), 0.204 (0.663 (0.647–0.678)) | 1.10 (0.839–1.45), 0.483 (0.69 (0.675–0.706)) |
| Pneumonia | |||
| ‐Disadvantaged IER | 1.35 (1.08–1.68), 0.007 (0.537 (0.511–0.563)) | 1.12 (0.897–1.40), 0.318 (0.802 (0.779–0.826)) | 1.07 (0.861–1.34), 0.526 (0.841 (0.820–0.862)) |
| ‐Unemployed | 1.07 (0.763–1.50), 0.696 (0.502 (0.493–0.511)) | 1.87 (1.31–2.66), 0.001 (0.799 (0.781–0.816)) | 1.58 (1.10–2.25), 0.012 (0.836 (0.820–0.852)) |
| Surgical site infection | |||
| ‐Disadvantaged IER | 1.65 (1.27–2.13), <0.001 (0.560 (0.530–0.589)) | 1.36 (1.05–1.76), 0.022 (0.765 (0.736–0.794)) | 1.32 (1.02–1.71), 0.038 (0.792 (0.766–0.819)) |
| ‐Unemployed | 1.20 (0.830–1.72), 0.334 (0.505 (0.494–0.516)) | 1.86 (1.27–2.73), 0.001 (0.760 (0.739–0.781)) | 1.71 (1.16–2.50), 0.006 (0.784 (0.763–0.803)) |
| Readmission | |||
| ‐Disadvantaged IER | 0.939 (0.872–1.01), 0.094 (0.508 (0.499–0.517)) | 0.918 (0.852–0.989), 0.025 (0.531 (0.574–0.596)) | 0.906 (0.840–0.976), 0.01 (0.598 (0.587–0.609)) |
| ‐Unemployed | 1.18 (1.06–1.32), 0.004 (0.504 (0.501–0.508)) | 1.22 (1.09–1.36), 0.001 (0.583 (0.576–0.591)) | 1.16 (1.03–1.30), 0.011 (0.602 (0.595–0.61) |
The total number of cases in the regression models with disadvantaged IER was 53 137 and it was 106 197 in the unemployment models.
The first logistic regression adjusted for year, age, sex and Charlson Comorbidity Index. The second model adjusted for these covariates and emergency status.
Statistically significant figures are bolded.
Discussion
There are widespread disparities in surgical adverse events for patients of low socioeconomic status or unemployed patients in Australia. These disparities can stem from three facets: a patient's access to healthcare and the severity of the disease at the time of presentation, variation in perioperative and follow up care delivery and social determinants of health or lifestyle factors that may have an effect prior to admission, during admission and after discharge. 17
Socioeconomic status may impact healthcare access and health seeking behaviour, both in an acute illness and across a patient's lifespan. There are disparities in access to surgical care for low socioeconomic patients. 25 , 26 Delayed presentations, such as more advanced stage of cancer or more severe peripheral arterial disease, may necessitate higher risk procedures. 25 This analysis adjusted for rates of emergency surgery (a proxy for delayed surgical access). 25 , 27 , 28 Adjusting for rates of emergency surgery decreased the odds of adverse events in low socioeconomic patients for all outcomes examined; however the only outcome where the disparity was no longer statistically significant after adjustment was acute renal failure in unemployed patients. The impacts of a relative lack of access to healthcare across a lifespan cannot be adjusted away using one proxy for delayed surgical access.
Variation in care may stem from within a hospital or from hospital level structural differences. This study involved only one hospital and found significant disparities in surgical outcomes for patients of low socioeconomic status. This eliminates the potential variation in care from hospital level structural differences and suggests potential variation in care within a hospital.
In the United States, studies have identified several racial disparities in surgical process measures including the administration of best‐practise venous thromboembolism prophylaxis 29 and prescription of beta blockers at discharge following cardiac surgery. 30 In contrast to this, a study in the United Kingdom examining disparities in 30‐day laparotomy for low socioeconomic status patients did not find variations in patient level performance in standards of care (e.g., reviewed by a consultant surgeon within 14 h of admission, appropriate time from to arrival to theatre). 17 Further research is required to determine if potential disparities in processes of care may contribute to the disparities in surgical outcomes for patients of low socioeconomic status in Australia.
Unconscious provider bias may contribute to healthcare disparities. International studies have shown that unconscious preferences for white race and upper social class are prevalent among registered nurses, medical students, trauma and acute care surgeons. 31 , 32 , 33 , 34 Unconscious preferences have not been shown to correlate with clinical decision‐making. 31 , 32 , 33 , 34 However, clinician implicit bias is associated with markers of poor visit communication, poor patient ratings of care and patients' perceptions of recommended treatments. 35 , 36 These factors may have downstream effects on clinical care.
Socioeconomic status is associated with health behaviours (smoking, obesity) and associated comorbidities (hypertension, diabetes) which may affect the risks of surgery. This study adjusted for the CCI but did not have data on individual health behaviours like smoking status, which may impact surgical outcomes. Future studies should examine the impact of individual health behaviours, such as smoking, on disparities in surgical outcomes for low socioeconomic patients.
In this study prior to risk adjustment unemployed patients had lower rates of mortality and acute renal failure. However, unemployed patients were significantly younger and had significantly fewer comorbidities when compared to other patients. After adjustment for these variables unemployed patients had significantly higher rates of postoperative mortality and acute renal failure. This example highlights the importance of adjusting for relevant confounding factors.
There are three proposed phases of health disparities research; detecting, understanding and reducing. 37 In the first phase, vulnerable populations are defined, the outcomes being examined are defined and these outcomes are measured for the vulnerable populations to detect potential disparities. The second phase is understanding why the disparities are present; determinants can be identified at several levels: the patient, clinical encounter, healthcare system or broader public policy. In the final phase, strategies that aim to reduce disparities are implemented and their impact is monitored utilizing the disparity sensitive metrics defined in the first phase. 37 This paper focuses on the first phase, detecting disparities. Further work is required to better understand the aetiology of these disparities and evaluate the impact of strategies that aim to reduce the disparities.
Although the AUC was low in univariate regressions it was much higher in multivariate regressions indicating that our multivariate models managed to incorporate most of the important variables related to the outcomes.
This study used residential postcodes to link to census tract data on residential socioeconomic status. There are more granular residential areas (statistical local areas) that can be linked to census tract data. Residential measures of socioeconomic status perform more consistently when more granular areas are used rather than postcodes. 38 , 39 The IER may have been a more reliable indicator of socioeconomic status if residential statistical local areas were linked to the IER data.
Aboriginal and/or Torres Strait Islander patients may experience higher rates of postoperative adverse events. 40 , 41 , 42 , 43 , 44 Aboriginal and/or Torres Strait Islander patients have higher rates of unemployment and are more likely to reside in areas of socioeconomic disadvantage. 45 Socioeconomic disadvantage alone may be responsible for between one‐third to one‐half of the life expectancy gap for Aboriginal and/or Torres Strait Islander Australians. 46 The burden of disease rates for Aboriginal and/or Torres Strait Islander people are the highest in areas where the population is the most socioeconomically disadvantaged and falls with decreasing level of disadvantage. 47 Examining surgical outcomes for Aboriginal and/or Torres Strait Islander people, and exploring the confounding effects of socioeconomic status, is prudent. The data to examine surgical outcomes for Aboriginal and/or Torres Strait Islander people is readily available in hospital administrative databases. Despite acquiring the full Human Research Ethics Committee approval to include a variable on Aboriginal and/or Torres Strait Islander status in this project's dataset and examine for disparities in surgical outcomes for this group, the Queensland Government did not allow the acquisition of the Aboriginal and/or Torres Strait Islander status variable.
Conclusion
Despite Australia's universal healthcare system, there are disparities in surgical adverse events for unemployed patients and patients of low socioeconomic status. Disparities in surgical outcomes can stem from three facets: a patient's access to healthcare (the severity of disease at the time of presentation), variation in perioperative care delivery and social determinants of health or lifestyle factors. Further work is required to pinpoint the aetiology of these disparities, develop strategies to reduce the disparities and evaluate the impact of these strategies utilizing disparity sensitive surgical outcome metrics.
Acknowledgment
Open access publishing facilitated by James Cook University, as part of the Wiley ‐ James Cook University agreement via the Council of Australian University Librarians.
Conflict of interest
None declared.
Disclosures
Elzerie de Jager is a Doctor of Philosophy candidate at an Australian University; this research degree is supported by an Australian Government Research Training Program (RTP) Scholarship. This work is also supported by the Avant Doctor in Training Research Scholarship.
Author contributions
Elzerie de Jager: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; validation; visualization; writing – original draft; writing – review and editing. Ronny Gunnarsson: Supervision; writing – review and editing. Yik‐Hong Ho: Supervision; writing – review and editing.
E. de Jager MBBS(Hons); R. Gunnarsson MD PhD; Y.‐H. Ho MD, FRACS.
References
- 1. Bambra C, Eikemo TA. Welfare state regimes, unemployment and health: a comparative study of the relationship between unemployment and self‐reported health in 23 European countries. J. Epidemiol. Community Health 2009; 63: 92–8. [DOI] [PubMed] [Google Scholar]
- 2. Marmot M, Wilkinson RG (eds). Social Determinants of Health. Oxford University Press, 2005. [Cited 28 Sep 2021.] Available from URL:; 2nd ed. https://books.google.com/books/about/Social_Determinants_of_Health.html?id=AmwiS8HZeRIC. Published to Oxford Scholarship Online: September 2009. [Google Scholar]
- 3. Bartley M. Unemployment and ill health: understanding the relationship. J. Epidemiol. Community Health 1994; 48: 333–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mehaffey JH, Hawkins RB, Charles EJ et al. Distressed communities are associated with worse outcomes after coronary artery bypass surgery. J. Thorac. Cardiovasc. Surg. 2020; 160: 425–432.e9. [DOI] [PubMed] [Google Scholar]
- 5. Mehaffey J, Hawkins R, Charles E et al. Community level socioeconomic status association with surgical outcomes and resource utilisation in a regional cohort: a prospective registry analysis. BMJ Qual. Saf. 2020; 29: 232–7. [DOI] [PubMed] [Google Scholar]
- 6. Hawkins RB, Charles EJ, Mehaffey JH et al. Socioeconomic distressed communities index associated with worse limb‐related outcomes after infrainguinal bypass. J. Vasc. Surg. 2019; 70: 786–794.e2. [DOI] [PubMed] [Google Scholar]
- 7. Reames BN, Birkmeyer NJO, Dimick JB, Ghaferi AA. Socioeconomic disparities in mortality after cancer surgery: failure to rescue. JAMA Surg. 2014; 149: 475–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bennett KM, Scarborough JE, Pappas TN, Kepler TB. Patient socioeconomic status is an independent predictor of operative mortality. Ann. Surg. 2010; 252: 552–7. [DOI] [PubMed] [Google Scholar]
- 9. Birkmeyer NJO, Gu N, Baser O, Morris AM, Birkmeyer JD. Socioeconomic status and surgical mortality in the elderly. Med. Care 2008; 46: 893–9. [DOI] [PubMed] [Google Scholar]
- 10. Bakshi SC, Fobare A, Benarroch‐Gampel J, Teodorescu V, Rajani RR. Lower socioeconomic status is associated with groin wound complications after revascularization for peripheral artery disease. Ann. Vasc. Surg. 2020; 62: 76–82. [DOI] [PubMed] [Google Scholar]
- 11. Qi AC, Peacock K, Luke AA, Barker A, Olsen MA, Joynt Maddox KE. Associations between social risk factors and surgical site infections after colectomy and abdominal hysterectomy. JAMA Netw. Open 2019; 2: e1912339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Coyan GN, Okoye A, Shah A et al. Effect of neighborhood socioeconomic factors on readmissions and mortality after coronary artery bypass grafting. Ann. Thorac. Surg. 2021; 111: 561–7. [DOI] [PubMed] [Google Scholar]
- 13. Vogel TR, Kruse RL, Kim RJ, Dombrovskiy VY. Racial and socioeconomic disparities after carotid procedures. Vasc. Endovasc. Surg. 2018; 52: 330–4. [DOI] [PubMed] [Google Scholar]
- 14. Medbery RL, Gillespie TW, Liu Y et al. Socioeconomic factors are associated with readmission after lobectomy for early stage lung cancer. Ann. Thorac. Surg. 2016; 102: 1660–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. de Jager E, Chaudhary MA, Rahim F et al. The impact of income on emergency general surgery outcomes in urban and rural areas. J. Surg. Res. 2020; 245: 629–35. [DOI] [PubMed] [Google Scholar]
- 16. Leslie SJ, Rysdale J, Lee AJ et al. Unemployment and deprivation are associated with a poorer outcome following percutaneous coronary angioplasty. Int. J. Cardiol. 2007; 122: 168–9. [DOI] [PubMed] [Google Scholar]
- 17. Poulton TE, Moonesinghe R, Raine R, Martin P. Socioeconomic deprivation and mortality after emergency laparotomy: an observational epidemiological study. Br. J. Anaesth. 2020; 124: 73–83. [DOI] [PubMed] [Google Scholar]
- 18. Taylor FC, Ascione R, Rees K, Narayan P, Angelini GD. Socioeconomic deprivation is a predictor of poor postoperative cardiovascular outcomes in patients undergoing coronary artery bypass grafting. Heart 2003; 89: 1062–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Daugbjerg SB, Cesaroni G, Ottesen B, Diderichsen F, Osler M. Effect of socioeconomic position on patient outcome after hysterectomy. Acta Obstet. Gynecol. Scand. 2014; 93: 926–34. [DOI] [PubMed] [Google Scholar]
- 20. Ultee KHJ, Tjeertes EKM, Gonçalves FB et al. The relation between household income and surgical outcome in the Dutch setting of equal access to and provision of healthcare. PLoS One 2018; 13: e0191464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ancona C, Agabiti N, Forastiere F et al. Coronary artery bypass graft surgery: socioeconomic inequalities in access and in 30 day mortality. A population‐based study in Rome, Italy. J. Epidemiol. Community Health 2000; 54: 930–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beliaev AM, Bergin CJ. Impact of socioeconomic deprivation on incidence and outcomes of acute type a aortic dissection repair in New Zealand. J. Card. Surg. 2021; 36: 2035–43. [DOI] [PubMed] [Google Scholar]
- 23. Census of Population and Housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2016. [Cited 27 Sep 2021.] Available from URL: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2016~Main%20Features~IER~21
- 24. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD‐10 version of the Charlson comorbidity index predicted in‐hospital mortality. J. Clin. Epidemiol. 2004; 57: 1288–94. [DOI] [PubMed] [Google Scholar]
- 25. de Jager E, Levine AA, Udyavar NR et al. Disparities in surgical access: a systematic literature review, conceptual model, and evidence map. J. Am. Coll. Surg. 2019; 228: 276–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Levine AA, de Jager E, Britt LD. Perspective: identifying and addressing disparities in surgical access: a health systems call to action. Ann. Surg. 2020; 271: 427–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Prin M, Guglielminotti J, Mtalimanja O, Li G, Charles A. Emergency‐to‐elective surgery ratio: a global indicator of access to surgical care. World J. Surg. 2018; 42: 1971–80. [DOI] [PubMed] [Google Scholar]
- 28. Samuel JC, Tyson AF, Mabedi C et al. Development of a ratio of emergent to total hernia repairs as a surgical capacity metric. Int. J. Surg. 2014; 12: 906–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lau BD, Haider AH, Streiff MB et al. Eliminating health care disparities with mandatory clinical decision support the venous thromboembolism (VTE) example. Med. Care 2015; 53: 18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. O'Neal WT, Efird JT, Davies SW et al. Discharge β‐blocker use and race after coronary artery bypass grafting. Front. Public Health 2014; 2: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Haider AH, Schneider EB, Sriram N et al. Unconscious race and class biases among registered nurses: vignette‐based study using implicit association testing. J. Am. Coll. Surg. 2015; 220: 1077–1086.e3. [DOI] [PubMed] [Google Scholar]
- 32. Haider AH, Schneider EB, Sriram N et al. Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. JAMA Surg. 2015; 150: 457. [DOI] [PubMed] [Google Scholar]
- 33. Haider AH, Sexton J, Sriram N et al. Association of unconscious race and social class bias with vignette‐based clinical assessments by medical students. JAMA 2011; 306: 942–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Haider AH, Schneider EB, Sriram N et al. Unconscious race and class bias. J. Trauma Acute Care Surg. 2014; 77: 409–16. [DOI] [PubMed] [Google Scholar]
- 35. Cooper LA, Roter DL, Carson KA et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am. J. Public Health 2012; 102: 979–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Penner LA, Dovidio JF, Gonzalez R et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J. Clin. Oncol. 2016; 34: 2874–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kilbourne AM, Switzer G, Hyman K, Crowley‐Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am. J. Public Health 2006; 96: 2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Krieger N, Chen JT, Waterman PD, Soobader M‐J, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area‐based measure and geographic level matter?: the public health disparities geocoding project. Am. J. Epidemiol. 2002; 156: 471–82. [DOI] [PubMed] [Google Scholar]
- 39. Hyndman JCG, Holman CDJ, Hockey RL, Donovan RJ, Corti B, Rivera J. Misclassification of social disadvantage based on geographical areas: comparison of postcode and Collector's district analyses. Int. J. Epidemiol. 1995; 24: 165–76. [DOI] [PubMed] [Google Scholar]
- 40. de Jager E, Gunnarsson R, Ho YH. Measuring the quality of surgical care provision to aboriginal and Torres Strait islander patients. ANZ J. Surg. 2019; 89: 1537–8. [DOI] [PubMed] [Google Scholar]
- 41. Alizzi AM, Knight JL, Tully PJ. Surgical challenges in rheumatic heart disease in the Australian indigenous population. Heart Lung Circ. 2010; 19: 295–8. [DOI] [PubMed] [Google Scholar]
- 42. Wiemers P, Marney L, Muller R et al. Cardiac surgery in indigenous Australians–how wide is “the gap”? Heart Lung Circ. 2014; 23: 265–72. [DOI] [PubMed] [Google Scholar]
- 43. Prabhu A, Tully PJ, Bennetts JS, Tuble SC, Baker RA. The morbidity and mortality outcomes of indigenous Australian peoples after isolated coronary artery bypass graft surgery: the influence of geographic remoteness. Heart Lung Circ. 2013; 22: 599–605. [DOI] [PubMed] [Google Scholar]
- 44. Singh TP, Moxon J V, Healy GN, Cadet‐James Y, Golledge J. Presentation and outcomes of indigenous Australians with peripheral artery disease. 2018; [DOI] [PMC free article] [PubMed]
- 45. Australian Bureau of Statistics . Census of Population and Housing: Reflecting Australia ‐ Stories from the Census, 2016. 2018. [Cited 2 June 2021.] Available from URL: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2071.0~2016~Main%20Features~In%20this%20Issue~1
- 46. Zhao Y, Wright J, Begg S, Guthridge S. Decomposing indigenous life expectancy gap by risk factors: a life table analysis. Popul. Health Metrics 2013; 11: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Al‐Yaman F. The Australian burden of disease study: impact and causes of illness and death in aboriginal and Torres Strait islander people, 2011. Public Health Res. Pract 2017; 27: 2741732. [DOI] [PubMed] [Google Scholar]


