Abstract
Mental health nurses aim to provide high‐quality care that is safe and person‐centred. Service users require individualized care, responsive to their preferences, needs, and values. The views of service users, mental health nurses, nurse academics, psychiatrists, and nurse managers about the core competencies of mental health nurses have not been explored. Our study aimed to describe and contrast the views of multiple stakeholder groups on the core competencies of mental health nurses. Concept mapping is a six‐step mixed‐methods study design that combines qualitative data with principal component analysis to produce a two‐dimensional concept map. Forty‐eight people participated in the study from five stakeholder groups that included service users and clinicians. The final concept map had eight clusters: assessment and management of risk; understanding recovery principles; person‐ and family‐centred care; good communication skills; knowledge about mental disorders and treatment; evaluating research and promoting physical health; a sense of humour; and physical and psychological interventions. There were important differences in how service users and health professionals ranked the relative importance of the clusters. Service users reported the understanding recovery principles cluster as the most important, whilst health professionals ranked the assessment and management of risk group the most important. There may be a disconnect between what service users and other stakeholders perceive to be the core competencies of mental health nurses. There is a need for more research to examine the differing perspectives of service users and health professionals on the core competencies of mental health nurses.
Keywords: core competencies, concept mapping, mental health nurse, service user, knowledge
INTRODUCTION
Defined as a combination of knowledge, professional skills, and attitudes, competencies ensure that a nurse can safely and effectively complete a task or activity within the context of a specific job (Hayes, 2020). Competencies enable an organization's workforce to understand the behaviours that must be demonstrated and the levels of performance that are expected to achieve organizational goals. They inform the nurse about the actions and behaviours that will be valued, recognized, and rewarded (Hayes, 2020).
The scope of practice of nurses working in mental health requires a broad set of clinical competencies to address the care needs of service users. Authors have described a broad range of competencies that include communication, management of risk, medication knowledge, and administration (Comiskey et al. 2019; Santangelo et al. 2018; Ward & Gwinner, 2015). The Australian College of Mental Health Nurses (2013) has described mental health nurses' scope of practice as comprising a variety of nursing roles, duties, obligations, accountabilities, activities, creativity, modalities, and innovations and is based on ethical decision‐making.
The impact of mental health nursing care on clinical outcomes for service users
There is no evidence from clinical trials or high‐quality observational studies that shows mental health nursing care as an exposure improves service user clinical outcomes compared to no specialist psychiatric nursing care. For example, Moyo, et al. (2020) reported a systematic review that examined the association between mental nursing skill mix and patient outcomes in adult mental health inpatient units and identified no studies that met inclusion criteria.
Person‐centred care
Person‐centred care is defined as reintroducing the service user into care, reinforcing the ever‐present ethical need to protect dignity, provide autonomy, choose, control, respect decision‐making, and do good (Edvardsson, 2015). Whilst we note that there is no strong evidence from systematic reviews that person‐centred care improves clinical outcomes (Barnett et al. 2019; Bee et al. 2015; Gondek et al. 2017), there is a strong policy emphasis for mental health services in Australia to adopt this approach (Australian Commission on Safety & Quality in Health Care, 2019; Australian Department of Health Victoria, 2021). As a consequence, we have located this study within a person‐centred practice framework.
Mental health nursing in an Australian context
In Victoria, the Nurses Act of 1993 removed the requirement for mental health nurses to be registered separately for new nurses, instead requiring future nursing graduates to be included on a single registry (Division 1) (Happell, 2009; Victorian Government, 1993). The implementation of a new Nurses Act in Victoria in 1993 resulted in the abrupt cessation of direct‐entry mental nursing training programmes (Happell, 2009). The Nurse Act 1993 allowed a registered nurse with no specialist training in mental health to perform the duties previously could only be undertaken by a mental health nurse (Victorian Government, 1993). In 2012, the Nursing and Midwifery Board of Australia changed the registration status of nurses with a sole qualification in mental health to general registration with the condition that they could only practice in psychiatric settings (Nursing & Midwifery Board of Australia, 2012). The ACMHN defines a mental health nurse – in an Australian context – as a registered nurse with a formal specialist qualification in mental health (Australian College of Mental Health Nurses, 2010). The college does not recognize nurses working in mental health settings who do not possess speciality postgraduate qualifications in the discipline as mental health nurses. Mental health nurses can be credentialled by the ACMHN, but it has no regulatory standing (Australian College of Mental Health Nurses, 2010).
We note that other countries offer different pathways to mental health nursing. For example, in the United Kingdom, there is a direct pathway to mental health nursing without the need to complete a comprehensive nursing program (Nursing & Midwifery Council United Kingdom, 2018).
In 2007, the ACMHN conducted a mixed‐method study to review and update the 1995 Australian mental health nurses' standards of practice (Australian College of Mental Health Nurses, 2010). A total of 229 mental health nurses and key stakeholders were involved in the study. Based on this work, the ACMHN published the revised Australian mental health nurses' standards of practice (Australian College of Mental Health Nurses, 2010). Given that there has been important development in mental health services over the past decade, it is, perhaps, worthy to investigate if these competencies are still relevant to contemporary practice.
Stakeholder perspectives on mental health nursing competencies
We searched five databases and identified 80 papers published between July 2006 and 31 December 2021 that explored the perspectives of service users and nurses on the competencies of mental health nurses. Out of 80 studies, we identified six (Askey et al. 2009; Biringer et al. 2021; Jones et al. 2007; McAllister et al. 2021; Santangelo et al. 2018; Sinclair et al. 2006) where service users, nurses, and other health‐care professionals’ views of the competencies of mental health nurses were compared and contrasted. One of these six studies examined the competencies of a nurse prescriber (Jones et al. 2007). Arguably, more research contrasting stakeholder perspectives is warranted. The aim of this study is to use concept mapping to understand and contrast the core competencies of mental health nurses from multiple stakeholder perspectives.
METHODS
Protocol and registrations
Our reporting followed the Good Reporting of A Mixed Methods Study (GRAMMS) (O’Cathain et al. 2008) reporting guidelines. The protocol for this study was submitted for publication prior to commencing data collection but was published after the fieldwork had started (Moyo, et al. 2020).
Study design
We considered two mixed methods for this research: concept mapping and the Delphi technique. These are two discrete and different methods used to examine the perceptions of a group of people about a phenomenon. The Delphi method requires experts to answer complex research questions (Grisham, 2009). Although the Delphi technique is intended to elicit expert opinions, it ultimately results in consensus among respondents and is not helpful in contrasting differences between groups (Lund, 2020). Concept mapping affords the advantage of enabling the views of different stakeholder groups to be compared and contrasted and was consequently considered to be a preferable methodology to achieving the aim of this study.
Theoretical position of concept mapping
Concept mapping is situated between post‐positivist and constructivist paradigms (Ponterotto, 2005). The quantitative (multivariate statistical analysis) part of concept mapping fits with the positivist paradigm, whilst the qualitative part aligns with constructivism. Concept mapping uses standardized procedures to collect data, and the participants entirely determine the content of the map (post‐positivist; Ponterotto, 2005). Constructivism conforms to a relativist viewpoint that implies many tangible and equally valid realities (Schwandt, 1994), consistent with our goal of comparing and contrasting the participants' perceptions.
Concept mapping
We used a concept mapping method originally developed by Trochim (1989). Concept mapping is a mixed‐method participatory research design that combines qualitative approaches with quantitative analytical tools to produce visual displays of the relationships between concepts (Burke et al. 2005). The final output is a concept map which is a geographical representation of stakeholder views of a particular concept. Our study followed the six stages of concept mapping. We have published a protocol (Moyo, et al. 2020) for this study previously.
Recruitment of participants
We sought expertise in addressing this question from the perspective of multiple stakeholders:
Service users aged 18 years or over who had experienced mental illness;
Mental health nurses, nurse managers, and psychiatrists, who were licensed to practice in Australia and were currently working in mental health settings;
Nurse academics working in an Australian University who indicated that they contributed to providing mental health education.
All participants needed to indicate that they had basic computer skills and were able to speak and read English.
Mental health nurses self‐identified, we did not verify their accreditation status with ACMHN as we considered this might negatively impact participation in the study.
We selected the stakeholder groups as we considered that each has a different baring on the work of mental health nurses (Bee et al. 2008; Cowman et al. 2001). For example, nurse academics design the mental health curriculums and educate nurses, and psychiatrists work closely with mental health nurses as part of the multidisciplinary team.
We used newsletters of advocacy organizations and snowballing methods to recruit service users. Professional groups were recruited through social media, newsletters, and snowballing techniques that are described in detail in the study protocol (Moyo, et al. 2020).
Phase 1: Preparation
Stage one involved deciding on the focus question for the study, ‘what are the core competencies (knowledge, clinical skills, and attitudes) of a mental health nurse?’
Phase 2: Generation of statements (Brainstorming)
Participants were interviewed individually by a researcher (who was a mental health nurse). Interviews were conducted using a video conferencing platform. Participants were invited to respond to the question, ‘what are the core competencies (knowledge, clinical skills, and attitudes) of a mental health nurse?’ The interviewer asked participants to elaborate on vague statements and asked follow‐up questions. Interviews were audio‐recorded. We generated more than enough statements for the Adriane software, and we reduced the number of statements by combining repetitive and overlapping concepts into single statements. Following that, the statements were entered into Ariadne.
Phase 3: Structuring of statements
The structuring of statements was conducted online using the Ariadne software package (Ariadne, 2015) and involves two tasks: prioritization and clustering. First, participants were asked to prioritize (rate) competencies in order of importance on a scale of one to five (one being the most important and five the least important). Participants were to ensure that there were an equal number of statements on each of the five points on the scale. Next participants were asked to group statements that seemed to belong together into clusters. Both tasks were completed online by ‘dragging and dropping’ virtual cards on the screen.
Phase 4: Representation
Data from the prioritization and clustering tasks were analysed using the Ariadne software package (Ariadne, 2015). Ariadne produced a matrix of zeros and ones representing the likeness between the statements for each participant. All the individual matrices were changed into one matrix representing all the individuals. The matrix was used as the input for a principal component analysis (PCA). PCA is a method for translating the distances (or the correlation) between statements or other entities into coordinates in a multidimensional space (Ariadne, 2015). The first two dimensions of the PCA solution were presented in the Concept Map. Ariadne then categorized the statements further by completing a cluster analysis with the coordinates of the statements (Ariadne, 2015). Ariadne also calculated the correlation between the priority of each statement and its position on the Concept Map for the individual and groups of participants (Ariadne, 2015).
Determining the best cluster solution
Concept mapping produces multiple (up to 17) cluster solutions. The research team reviewed each cluster to determine which cluster solution best represented the data.
Phase 5: Interpretation of concept maps
We organized a focus group that comprised at least one participant from each stakeholder group to review and interpret the final concept map. First, we calculated the mean rating of the total statements in each cluster to determine the average rating of each cluster. Then, the clusters were presented in a table in order of their relative importance. We used this table to interpret the concept map. Furthermore, the distance between clusters and the location of the clusters were used to interpret the clusters.
Phase 6: Utilization of concept maps
During this stage, the authors had a meeting to discuss how the concept map study results will be used.
Changes to the protocol
Initially, we did not intend to reimburse service users for taking part in the study. In response to feedback from service user advocacy groups, we amended the protocol so that participants were reimbursed $50 for their time. An amendment was submitted and approved by the University human research ethics committee.
Participants were not involved in determining the best cluster solution as proposed in the protocol because we did not want to burden them. We omitted to include a statement about service users and public involvement in our protocol.
Ethical considerations
Ethical approval was granted by the La Trobe University human research ethics committee before commencing the study (Approval No. HEC20257). Written informed consent was obtained from people who had expressed an interest in participating. Participants were informed that they could withdraw from the study at any phase of the concept mapping process. At each stage of the concept mapping, participants were asked if they were still interested in completing the task. We provided a list of addresses and online psychosocial support and counselling services to participants for help and advice in the event of emotional distress during the interview process because of previous experiences of distress and trauma.
Patient and public involvement in the research project
Participants were not involved in developing the focus question or the design of the study. Instead, service users and mental health professionals helped in recruiting other people through the snowball technique. One service user and six mental health professionals, together with the authors, interpreted the final concept map.
RESULTS
The flow of participants through the study is shown in Fig. 1. A total of 48 people participated in the brainstorming and 43 in prioritizing and clustering tasks. There were broadly equal numbers of participants across the five stakeholder groups.
Fig. 1.
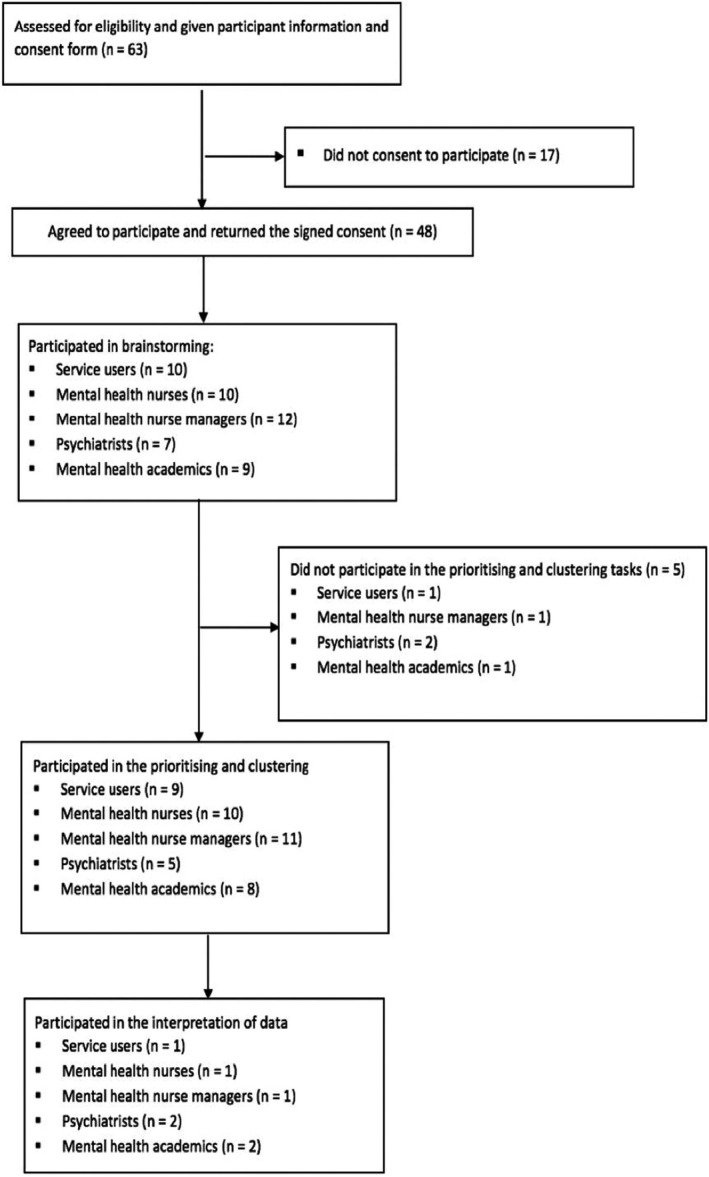
A diagram showing the flow of participants.
Demographic characteristics of participants
The demographic characteristics of the stakeholder groups and the duration of the interviews are shown in Table 1. Most participants identified as female and were in their mid‐40s. The majority of service users reported that they had a diagnosis of depression and/or anxiety. Across the four professional groups most held a postgraduate qualification, had around 20 years of mental health experience, and had trained in Australia. Seven (78%) of the nine nurse academics worked as casual or part‐time mental health nurses in the clinical setting.
Table 1.
Participant characteristics
| Characteristics | Participant groups | |||||
|---|---|---|---|---|---|---|
| All participants (n = 48) | Service users (n = 10) | Mental health nurses (n = 10) | Nurse managers (n = 12) | Psychiatrists (n = 7) | Nurse academics (n = 9) | |
| Gender (identified as female) | 25 (52%) | 8 (80%) | 5 (50%) | 6 (50%) | 1 (14%) | 5 (56%) |
| Age in years M (SD) | 45.63 (9.63) | 45.60 (13.43) | 44.40 (5.91) | 47.75 (7.83) | 41.57 (10.51) | 47.33 (10.45) |
| Educational level | ||||||
| No degree | 8 (17%) | 7 (70%) | 1 (10%) | — | — | — |
| Undergraduate degree | 14 (29%) | 2 (20%) | 4 (40%) | 6 (50%) | 2 (29%) | — |
| Postgraduate qualification | 26 (54%) | 1 (10%) | 5 (50%) | 6 (50%) | 5 (71%) | 9 (100%) |
| Country clinical qualification was obtained | ||||||
| Australia | 27 (71%) | — | 6 (60%) | 8 (67%) | 5 (71%) | 8 (89%) |
| Overseas | 11 (29%) | — | 4 (40%) | 4 (33%) | 2 (29%) | 1 (11%) |
| Work experience in years M (SD) | 19.53 (11.36) | — | 14.60 (5.06) | 21.75 (10.66) | 15.43 (10.39) | 25.22 (15.54) |
| Self‐defined psychiatric diagnosis | ||||||
| Mood and/or anxietydisorder | 8 (80%) | 8 (80%) | — | — | — | — |
| Schizophrenia | 2 (20%) | 2 (20%) | — | — | — | — |
| Interview duration M (SD) in minutes | 20.90 (4.41) | 20.67 (4.95) | 20.22 (4.52) | 22.50 (3.34) | 20.71 (5.44) | 20.33 (4.36) |
| Statements generated | 409 (100%) | 77 (19%) | 85 (21%) | 93 (23%) | 73 (18%) | 81 (20%) |
Generation of statements (brainstorming)
All participants took part in the brainstorming phase of concept mapping. The mean duration of interviews was 21 minutes (SD = 4.41). There were no important differences in the duration of interviews between stakeholder groups. A total of 409 individual statements were identified.
Statement reduction
The researcher retrieved information from the interview by listening back to it and entering it on an Excel spreadsheet. The number of statements exceeded the maximum (98) that can be entered into the concept mapping software package. Therefore, we followed the procedures set out in the study protocol (Moyo, et al. 2020) to reduce statements. Statement reduction was undertaken by NM and RG. We combined repetitive or overlapping statements into single concepts. The final list included 60 understandable, singular, and specific statements (Kikkert et al. 2006). A complete list of statement is shown in Table 2.
Table 2.
Comparing mean importance of statements generated by stakeholder groups
| Statements | All participants (n = 43) | Service users (n = 9) | Nurses (n = 10) | Nurse Managers (n = 11) | Psychiatrists (n = 5) | Nurse Academics (n = 8) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M (SD) | 95% CI | M (SD) | 95% CI | M (SD) | 95% CI | M (SD) | 95% CI | M (SD) | 95% CI | M (SD) | 95% CI | |
| Skilled in engaging people when they are distressed d | 1.42 (0.73) | 1.20, 1.64 | 1.22 (0.44) | 0.93, 1.51 | 1.20 (0.42) | 0.94, 1.46 | 1.82 (1.08) | 1.18, 2.46 | 1.60 (0.89) | 0.82, 2.38 | 1.25 (0.46) | 0.93, 1.57 |
| Can undertake a risk assessment (harm to self) a | 1.72 (1.03) | 1.41, 2.03 | 2.89 (1.36) | 2.00, 3.78 | 1.20 (0.63) | 0.81, 1.59 | 1.73 (0.65) | 1.35, 2.11 | 1.40 (0.55) | 0.92, 1.88 | 1.25 (0.71) | 0.76, 1.74 |
| Conduct a mental state examination a | 1.74 (1.20) | 1.39, 2.10 | 3.00 (1.32) | 2.14, 3.86 | 1.10 (0.32) | 0.90, 1.30 | 1.55 (1.21) | 0.83, 2.27 | 1.80 (1.30) | 0.66, 2.94 | 1.38 (0.74) | 0.87, 1.89 |
| Are able to engage with consumers c | 1.74 (1.03) | 1.44, 2.05 | 1.78 (0.83) | 1.24, 2.32 | 1.50 (0.53) | 1.17, 1.83 | 2.18 (1.08) | 1.54, 2.82 | 2.40 (1.95) | 0.69, 4.11 | 1.00 (0.00) | —* |
| Do not stigmatize patients c | 1.75 (1.10) | 1.42, 2.08 | 1.44 (0.73) | 0.96, 1.92 | 1.40 (0.70) | 0.97, 1.83 | 2.45 (1.37) | 1.64, 3.26 | 2.00 (1.26) | 0.90, 3.10 | 1.38 (1.06) | 0.65, 2.11 |
| Good communication skills d | 1.77 (1.19) | 1.41, 2.12 | 1.67 (0.87) | 1.10, 2.24 | 1.60 (1.07) | 0.94, 2.26 | 1.73 (1.27) | 0.98, 2.48 | 2.80 (1.79) | 1.23, 4.37 | 1.50 (1.07) | 0.76, 2.24 |
| Works in a patient centred way c | 1.77 (1.02) | 1.46, 2.07 | 1.67 (0.87) | 1.10, 2.24 | 1.70 (0.95) | 1.11, 2.29 | 2.45 (1.13) | 1.78, 3.12 | 1.60 (1.34) | 0.43, 2.77 | 1.13 (0.35) | 0.89, 1.37 |
| Knowledge about mental health law e | 1.84 (0.84) | 1.59, 2.09 | 2.22 (0.67) | 1.78, 2.66 | 1.50 (0.71) | 1.06, 1.94 | 1.73 (1.01) | 1.13, 2.33 | 2.20 (0.84) | 1.46, 2.94 | 1.75 (0.89) | 1.13, 2.37 |
| Are able to effectively manage crisis situations d | 1.84 (1.07) | 1.52, 2.16 | 2.00 (1.12) | 1.27, 2.73 | 1.10 (0.32) | 0.90, 1.30 | 1.82 (1.25) | 1.08, 2.56 | 2.60 (1.52) | 1.27, 3.93 | 2.13 (0.64) | 1.69, 2.57 |
| Have good observation skills d | 1.84 (1.25) | 1.46, 2.21 | 2.44 (1.24) | 1.63, 3.25 | 1.30 (0.67) | 0.88, 1.72 | 1.64 (1.29) | 0.88, 2.40 | 2.60 (1.52) | 1.27, 3.93 | 1.63 (1.41) | 0.65, 2.61 |
| Are able to express empathy c | 1.86 (1.04) | 1.55, 2.17 | 1.89 (1.05) | 1.20, 2.58 | 1.60 (0.97) | 1.00, 2.20 | 2.45 (1.13) | 1.78, 3.12 | 2.00 (1.22) | 0.93, 3.07 | 1.25 (0.46) | 0.93, 1.57 |
| Are knowledgeable about risk factors for mental illness e | 1.88 (1.00) | 1.58, 2.18 | 2.22 (0.67) | 1.78, 2.66 | 1.30 (0.48) | 1.00, 1.60 | 1.82 (1.08) | 1.18, 2.46 | 2.60 (1.52) | 1.27, 3.93 | 1.88 (1.13) | 1.10, 2.66 |
| Skilled at talking to patients, families and friends c | 1.93 (1.16) | 1.58, 2.28 | 2.00 (1.50) | 1.02, 2.98 | 1.50 (0.53) | 1.17, 1.83 | 2.18 (0.87) | 1.67, 2.69 | 2.20 (1.64) | 0.76, 3.64 | 1.88 (1.46) | 0.87, 2.89 |
| Skilled at working as part of a team d | 1.95 (1.07) | 1.63, 2.27 | 2.33 (1.00) | 1.68, 2.98 | 1.60 (0.84) | 1.08, 2.12 | 1.82 (0.98) | 1.24, 2.40 | 2.40 (1.67) | 0.94, 3.86 | 1.88 (1.13) | 1.10, 2.66 |
| Do not make judgements about consumers behaviour c | 1.98 (1.02) | 1.67, 2.28 | 1.88 (0.99) | 1.23, 2.53 | 2.40 (1.07) | 1.74, 3.06 | 2.36 (1.12) | 1.70, 3.02 | 1.40 (0.89) | 0.62, 2.18 | 1.38 (0.52) | 1.02, 1.74 |
| Knowledge about the principles of recovery b | 1.98 (1.06) | 1.66, 2.29 | 2.00 (1.12) | 1.27, 2.73 | 1.80 (0.63) | 1.41, 2.19 | 1.82 (0.98) | 1.24, 2.40 | 2.40 (1.14) | 1.40, 3.40 | 2.13 (1.55) | 1.06, 3.20 |
| Are able to handover patients accurately a | 1.98 (1.14) | 1.63, 2.32 | 2.33 (1.22) | 1.53, 3.13 | 1.10 (0.32) | 0.90, 1.30 | 2.27 (1.62) | 1.31, 3.23 | 2.40 (1.55) | 1.04, 3.76 | 2.00 (0.76) | 1.47, 2.53 |
| Skilled in the management of verbal aggression a | 2.00 (1.15) | 1.65, 2.35 | 2.22 (0.97) | 1.59, 2.85 | 1.60 (1.07) | 0.94, 2.26 | 1.82 (1.08) | 1.18, 2.46 | 2.60 (1.52) | 1.27, 3.93 | 2.13 (1.36) | 1.19, 3.07 |
| Are focused on empowering consumers c | 2.02 (1.24) | 1.65, 2.40 | 1.78 (1.09) | 1.07, 2.49 | 2.10 (1.29) | 1.30, 2.90 | 2.45 (1.29) | 1.69, 3.21 | 2.60 (1.82) | 1.00, 4.20 | 1.25 (0.46) | 0.93, 1.57 |
| Skilled in reflecting on their own practice d | 2.05 (0.97) | 1.76, 2.34 | 2.11 (0.93) | 1.50, 2.72 | 2.00 (1.05) | 1.35, 2.65 | 2.09 (1.22) | 1.37, 2.81 | 2.40 (0.55) | 1.92, 2.88 | 1.75 (0.89) | 1.13, 2.37 |
| Do not assume consumers are dangerous (potentially violent) c | 2.07 (0.91) | 1.80, 2.34 | 2.00 (0.71) | 1.54, 2.46 | 1.90 (0.88) | 1.35, 2.45 | 2.27 (0.90) | 1.74, 2.80 | 2.80 (1.30) | 1.66, 3.94 | 1.63 (0.74) | 1.12, 2.14 |
| Can undertake a risk assessment (violence) a | 2.07 (1.14) | 1.73, 2.41 | 3.22 (1.30) | 2.37, 4.07 | 1.70 (0.48) | 1.40, 2.00 | 1.64 (0.81) | 1.16, 2.12 | 2.00 (0.71) | 1.38, 2.62 | 1.88 (1.46) | 0.87, 2.89 |
| Is an advocate for consumers c | 2.07 (1.18) | 1.72, 2.42 | 2.11 (1.05) | 1.42, 2.80 | 2.00 (0.94) | 1.42, 2.58 | 2.45 (1.37) | 1.64, 3.26 | 1.80 (1.30) | 0.66, 2.94 | 1.75 (1.39) | 0.79, 2.71 |
| Skilled in the management of physical aggression a | 2.09 (1.17) | 1.74, 2.44 | 2.89 (1.45) | 1.94, 3.84 | 1.80 (1.23) | 1.04, 2.56 | 1.82 (1.08) | 1.18, 2.46 | 1.60 (0.55) | 1.12, 2.08 | 2.25 (0.89) | 1.63, 2.87 |
| Work in a trauma informed way c | 2.09 (1.17) | 1.74, 2.44 | 1.67 (1.12) | 0.94, 2.40 | 2.60 (0.84) | 2.08, 3.12 | 2.00 (1.10) | 1.35, 2.65 | 2.80 (1.30) | 1.66, 3.94 | 1.63 (1.41) | 0.65, 2.61 |
| Spend time with consumers c | 2.10 (1.10) | 1.77, 2.42 | 2.33 (0.87) | 1.76, 2.90 | 1.89 (0.93) | 1.31, 2.47 | 2.36 (1.21) | 1.64, 3.08 | 1.60 (1.34) | 0.43, 2.77 | 2.00 (1.31) | 1.09, 2.91 |
| Is not condescending c | 2.12 (1.20) | 1.76, 2.47 | 1.78 (1.09) | 1.07, 2.49 | 2.40 (1.43) | 1.51, 3.29 | 2.45 (1.29) | 1.69, 3.21 | 1.80 (1.10) | 0.84, 2.76 | 1.88 (0.99) | 1.19, 2.57 |
| Knowledge about the dual diagnosis (mental disorder and an alcohol or drug problem) e | 2.12 (0.79) | 1.88, 2.35 | 2.22 (0.67) | 1.78, 2.66 | 1.60 (0.52) | 1.28, 1.92 | 2.36 (0.92) | 1.82, 2.90 | 2.40 (0.89) | 1.62, 3.18 | 2.13 (0.83) | 1.55, 2.71 |
| Engender a sense of hope c | 2.14 (1.32) | 1.75, 2.53 | 2.11 (1.17) | 1.35, 2.87 | 1.90 (1.29) | 1.10, 2.70 | 2.82 (1.40) | 1.99, 3.65 | 2.60 (1.82) | 1.00, 4.20 | 1.25 (0.46) | 0.93, 1.57 |
| Works in a culturally competent way c | 2.16 (1.09) | 1.84, 2.49 | 2.00 (1.32) | 1.14, 2.86 | 1.90 (0.99) | 1.29, 2.51 | 2.36 (1.03) | 1.75, 2.97 | 2.60 (1.34) | 1.43, 3.77 | 2.13 (0.99) | 1.44, 2.82 |
| Knowledgeable about the use of Pro re nata (PRN) medication e | 2.19 (1.26) | 1.81, 2.56 | 3.56 (1.13) | 2.82, 4.30 | 1.50 (0.71) | 1.06, 1.94 | 2.09 (1.51) | 1.20, 2.98 | 1.60 (0.55) | 1.12, 2.08 | 2.00 (0.76) | 1.47, 2.53 |
| Is kind c | 2.21 (1.26) | 1.83, 2.59 | 2.00 (1.32) | 1.14, 2.86 | 2.00 (0.82) | 1.49, 2.51 | 2.82 (1.25) | 2.08, 3.56 | 2.60 (2.19) | 0.68, 4.52 | 1.63 (0.74) | 1.12, 2.14 |
| Are able to work autonomously d | 2.23 (0.97) | 1.94, 2.52 | 2.76 (0.97) | 2.13, 3.39 | 1.70 (0.67) | 1.28, 2.12 | 2.36 (1.03) | 1.75, 2.97 | 2.60 (0.89) | 1.82, 3.38 | 1.88 (0.99) | 1.19, 2.57 |
| Knowledge of different mental disorders (DSM/ICD) e | 2.29 (1.15) | 1.95, 2.64 | 2.56 (1.24) | 1.75, 3.37 | 2.20 (1.03) | 1.56, 2.84 | 2.20 (1.40) | 1.37, 3.03 | 2.50 (1.00) | 1.62, 3.38 | 2.13 (1.13) | 1.35, 2.91 |
| Clinical documentation is respectful d | 2.30 (1.08) | 1.98, 2.63 | 2.78 (1.09) | 2.07, 3.49 | 2.00 (0.94) | 1.42, 2.58 | 2.18 (1.08) | 1.54, 2.82 | 3.20 (1.30) | 2.06, 4.34 | 1.75 (0.71) | 1.26, 2.24 |
| Knowledge about co‐occurring physical health problems e | 2.33 (0.94) | 2.04, 2.61 | 2.44 (0.53) | 2.09, 2.79 | 1.80 (0.42) | 1.54, 2.06 | 2.45 (1.21) | 1.73, 3.17 | 3.40 (1.14) | 2.40, 4.40 | 2.00 (0.76) | 1.47, 2.53 |
| Knowledge about psychopharmacology e | 2.35 (1.19) | 1.99, 2.71 | 3.11 (1.69) | 2.01, 4.21 | 2.10 (1.10) | 1.42, 2.78 | 2.09 (0.94) | 1.53, 2.65 | 2.40 (0.89) | 1.62, 3.18 | 2.13 (0.99) | 1.44, 2.82 |
| Skilled at working with family and friends c | 2.37 (1.16) | 2.03, 2.72 | 3.22 (1.39) | 2.31, 4.13 | 2.10 (0.99) | 1.49, 2.71 | 2.18 (0.87) | 1.67, 2.69 | 2.20 (1.10) | 1.24, 3.16 | 2.13 (1.25) | 1.26, 3.00 |
| Are critical thinkers d | 2.38 (1.10) | 2.05, 2.71 | 2.56 (1.24) | 1.75, 3.37 | 2.30 (0.48) | 2.00, 2.60 | 2.36 (1.29) | 1.60, 3.12 | 3.25 (0.50) | 2.81, 3.69 | 1.88 (1.36) | 0.94, 2.82 |
| Can undertake a physical health assessment h | 2.44 (0.98) | 2.15, 2.74 | 3.11 (1.05) | 2.42, 3.80 | 2.10 (0.88) | 1.55, 2.65 | 2.18 (0.87) | 1.67, 2.69 | 2.60 (1.14) | 1.60, 3.60 | 2.38 (0.92) | 1.74, 3.02 |
| Knowledgeable about different psychotherapeutic techniques e | 2.51 (1.05) | 2.20, 2.83 | 3.00 (1.58) | 1.97, 4.03 | 2.20 (0.79) | 1.71, 2.69 | 2.36 (0.92) | 1.82, 2.90 | 3.00 (1.00) | 2.12, 3.88 | 2.25 (0.70) | 1.76, 2.74 |
| Competent in delivering different psychotherapeutic techniques h | 2.53 (1.08) | 2.21, 2.86 | 3.11 (1.36) | 2.22, 4.00 | 2.00 (0.82) | 1.49, 2.51 | 2.82 (0.98) | 2.24, 3.40 | 3.20 (0.84) | 2.46, 3.94 | 1.75 (0.46) | 1.43, 2.07 |
| Are well organized d | 2.53 (1.14) | 2.19, 2.88 | 2.78 (1.20) | 2.00, 3.56 | 2.00 (0.82) | 1.49, 2.51 | 2.82 (1.25) | 2.08, 3.56 | 2.60 (0.89) | 1.82, 3.38 | 2.50 (1.41) | 1.52, 3.48 |
| Attend regular clinical supervision d | 2.53 (1.14) | 2.19, 2.88 | 2.78 (1.09) | 2.07, 3.49 | 2.30 (1.16) | 1.58, 3.02 | 2.36 (1.12) | 1.70, 3.02 | 3.40 (1.40) | 2.17, 4.63 | 2.25 (1.16) | 1.45, 3.05 |
| Spend time with consumers family and friends c | 2.53 (1.18) | 2.18, 2.89 | 2.89 (1.17) | 2.13, 3.65 | 2.50 (1.35) | 1.66, 3.34 | 2.73 (1.01) | 2.13, 3.33 | 1.60 (0.55) | 1.12, 2.08 | 2.50 (1.41) | 1.52, 3.48 |
| Are skilled in promoting physical health f | 2.56 (1.16) | 2.21, 2.91 | 3.11 (1.17) | 2.35, 3.87 | 2.30 (0.82) | 1.79, 2.81 | 2.73 (1.42) | 1.89, 3.57 | 3.20 (0.84) | 2.46, 3.94 | 1.63 (0.74) | 1.12, 2.14 |
| Clinical documentation is reflective d | 2.63 (1.22) | 2.26, 2.99 | 2.89 (1.27) | 2.06, 3.72 | 2.40 (1.43) | 1.51, 3.29 | 2.36 (1.12) | 1.70, 3.02 | 3.00 (1.22) | 1.93, 4.07 | 2.75 (1.16) | 1.95, 3.55 |
| Knowledge about Safewards interventions e | 2.70 (1.19) | 2.34, 3.05 | 3.44 (1.33) | 2.57, 4.31 | 2.20 (1.03) | 1.56, 2.84 | 2.36 (1.29) | 1.60, 3.12 | 3.00 (1.00) | 2.12, 3.88 | 2.75 (0.89) | 2.13, 3.37 |
| Knowledge about the social determinants of health e | 2.72 (1.14) | 2.38, 3.06 | 2.89 (1.17) | 2.13, 3.65 | 2.20 (1.14) | 1.49, 2.91 | 3.18 (1.33) | 2.39, 3.97 | 3.00 (0.71) | 2.38, 3.62 | 2.38 (0.92) | 1.74, 3.02 |
| Are able to administer long acting (depot) injections h | 2.74 (1.33) | 2.34, 3.13 | 3.89 (1.45) | 2.94, 4.84 | 2.20 (1.14) | 1.49, 2.91 | 2.45 (1.37) | 1.64, 3.26 | 2.25 (0.50) | 1.81, 2.69 | 2.75 (1.04) | 2.03, 3.47 |
| Are able to administer intramuscular injection h | 2.74 (1.38) | 2.33, 3.16 | 4.11 (1.17) | 3.35, 4.87 | 1.70 (0.67) | 1.28, 2.12 | 2.82 (1.60) | 1.87, 3.77 | 2.60 (1.14) | 1.60, 3.60 | 2.50 (0.93) | 1.86, 3.14 |
| Can generate a nursing diagnosis h | 2.74 (1.35) | 2.34, 3.15 | 3.67 (1.12) | 2.94, 4.40 | 2.20 (1.40) | 1.33, 3.07 | 2.55 (1.21) | 1.83, 3.27 | 2.80 (1.30) | 1.66, 3.94 | 2.63 (1.51) | 1.58, 3.68 |
| Are able to work flexibly d | 2.79 (1.12) | 2.45, 3.13 | 3.33 (0.87) | 2.76, 3.90 | 2.30 (0.95) | 1.71, 2.89 | 2.64 (1.03) | 2.03, 3.25 | 3.80 (1.10) | 2.84, 4.76 | 2.38 (1.30) | 1.48, 3.28 |
| Skilled in being able to critically evaluate new research f | 2.84 (1.19) | 2.48, 3.19 | 2.78 (1.39) | 1.87, 3.69 | 2.50 (0.71) | 2.06, 2.94 | 2.91 (1.04) | 2.30, 3.52 | 4.20 (1.30) | 3.06, 5.34 | 2.38 (1.19) | 1.56, 3.20 |
| Knowledgeable about the history of psychiatric care and treatment e | 2.91 (1.31) | 2.52, 3.30 | 3.00 (1.50) | 2.02, 3.98 | 2.40 (1.07) | 1.74, 3.06 | 2.82 (1.47) | 1.95, 3.69 | 3.40 (1.52) | 2.07, 4.73 | 3.25 (1.04) | 2.53, 3.97 |
| Have a good sense of humour g | 2.95 (1.15) | 2.61, 3.30 | 3.22 (1.30) | 2.37, 4.07 | 2.60 (0.97) | 2.00, 3.20 | 3.27 (1.10) | 2.62, 3.92 | 2.20 (1.30) | 1.06, 3.34 | 3.13 (1.13) | 2.35, 3.91 |
| Knowledgeable about new research e | 3.12 (1.22) | 2.75, 3.48 | 3.00 (0.71) | 2.54, 3.46 | 2.20 (0.79) | 1.71, 2.69 | 3.45 (1.21) | 2.73, 4.17 | 4.60 (0.55) | 4.12, 5.08 | 3.00 (1.51) | 1.95, 4.05 |
| Are able to administer an ECG h | 3.60 (1.16) | 3.26, 3.95 | 3.67 (1.22) | 2.87, 4.47 | 3.50 (1.18) | 2.77, 4.23 | 3.64 (0.92) | 3.10, 4.18 | 3.20 (1.64) | 1.76, 4.64 | 3.88(1.25) | 3.01, 4.75 |
| Competent in taking blood h | 3.86 (1.23) | 3.49, 4.23 | 4.00 (1.41) | 3.08, 4.92 | 3.80 (1.32) | 2.98, 4.62 | 3.91 (1.22) | 3.19, 4.63 | 3.00 (1.00) | 2.12, 3.88 | 4.25 (1.04) | 3.53, 4.97 |
| Are able to interpret an ECG h | 3.95 (1.00) | 3.65, 4.25 | 4.22 (1.09) | 3.51, 4.93 | 3.70 (1.06) | 3.04, 4.36 | 3.91 (0.54) | 3.59, 4.23 | 3.60 (1.52) | 2.27, 4.93 | 4.25 (1.04) | 3.53, 4.97 |
Each statement was rated regarding its perceived importance as a competence of a mental health nurse using a scale from 1 to 5, with one being the most important. Statements are arranged according to their importance, that is, statements on top were highly rated. The letters (a–h) on each statement represents the eight clusters.
Statement in cluster one, assessment and management of risk.
Statement in cluster two, understanding recovery principles.
Statement in cluster three, family‐ and patient‐centred care.
Statement in cluster four, good communication skills.
Statement in cluster five, knowledge about mental disorders and treatment.
Statement in cluster six, evaluating Research and promoting physical health.
Statement in cluster seven, a sense of humour.
Statement in cluster eight, physical and psychological interventions.
No confidence interval since SD is 0.00.
Phase 3: Structuring of statements
The final list of statements ranked from most through least important for all participants and by stakeholder group is reported in Table 2. Ariadne combined the ratings of all statements by all individuals and calculated the mean score of each statement. 'Skilled in engaging people when they are distressed' was ranked as most important statement overall.
Phase 4: Representation
The Ariadne software package produced a point map that shows the position of each statement (see Fig. 2). Ariadne also generated 17 candidate concept maps. Candidate concept maps had between two and 18 clusters (all candidate concept maps are available in File S1). Two members of the research team (NM, RG) reviewed each concept map to determine which best conceptually represented the views of participants. Initially, we eliminated concept maps with two through six clusters as the clusters were large and contained statements that clearly did not relate to each other. Next, we eliminated nine maps with small clusters because they only contained single statements and statements that seemed to relate to each other were not placed within the same cluster. From a final shortlist of three: seven cluster, eight cluster, and nine cluster solutions, we considered that the eight‐cluster solution best represented the data (Fig. 3 and Table 3).
Fig. 2.
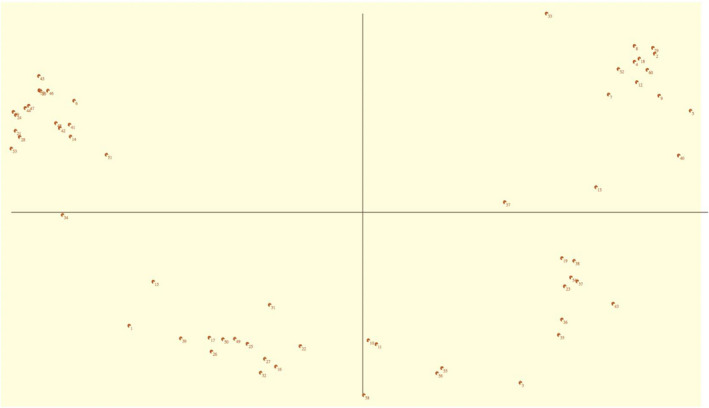
A point map showing the position of each statement.
Fig. 3.
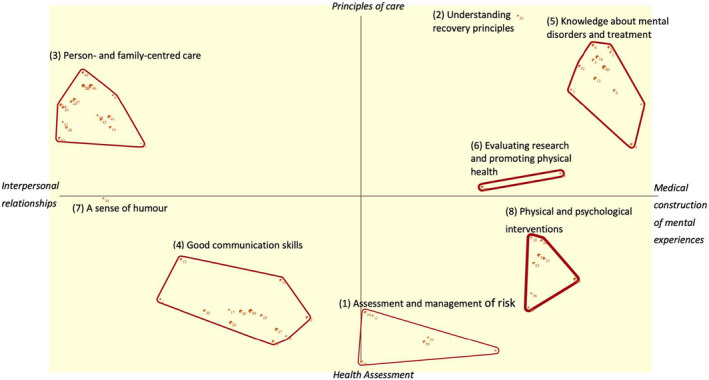
The final eight‐cluster concept map solution showing stakeholder perceptions of the core competencies of a mental health nurse.
Table 3.
Comparing mean importance of eight‐cluster solution of the five stakeholder groups
| Cluster | All participants (n = 43) | Service users (n = 9) | Nurses (n = 10) | Psychiatrist (n = 5) | Nurse managers (n = 11) | Nurse academics (n = 8) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rank | M (SD) | 95% CI | Rank | M (SD) | 95%CI | Rank | M (SD) | 95%CI | Rank | M (SD) | 95%CI | Rank | M (SD) | 95%CI | Rank | M (SD) | 95%CI | |
| Assessment and management of risk | 1 | 1.93 (1.14) | 1.59, 2.27 | 4 | 2.76 (1.27) | 1.93, 3.59 | 1 | 1.42 (0.68) | 1.00, 1.84 | 1 | 1.97 (1.03) | 1.07, 2.87 | 1 | 1.81 (1.08) | 1.17, 2.45 | 2 | 1.82 (0.99) | 1.13, 2.51 |
| Understanding recovery principles | 2 | 1.98 (1.06) | 1.66, 2.30 | 1 | 2.00 (1.12) | 1.27, 2.73 | 2 | 1.80 (0.63) | 1.41, 2.19 | 4 | 2.40 (1.14) | 1.40, 3.40 | 2 | 1.82 (0.98) | 1.24, 2.40 | 5 | 2.13 (1.55) | 1.06, 3.20 |
| Person‐ and family‐centred care | 3 | 2.05 (1.13) | 1.71, 2.39 | 2 | 2.10 (1.07) | 1.40, 2.80 | 5 | 1.96 (0.97) | 1.36, 2.56 | 2 | 2.15 (1.38) | 0.94, 3.36 | 5 | 2.41 (1.14) | 1.74, 3.08 | 1 | 1.64 (0.88) | 1.03, 2.25 |
| Good communication skills | 4 | 2.17 (1.08) | 1.85, 2.49 | 3 | 2.43 (1.03) | 1.76, 3.10 | 3 | 1.83 (0.83) | 1.32, 2.34 | 5 | 2.79 (1.17) | 1.76, 3.82 | 3 | 2.15 (1.15) | 1.47, 2.83 | 3 | 1.96 (1.05) | 1.23, 2.69 |
| Knowledge about mental disorders and treatment | 5 | 2.41 (1.09) | 2.08, 2.74 | 5 | 2.81 (1.07) | 2.11, 3.51 | 4 | 1.93 (0.82) | 1.42, 2.44 | 6 | 2.84 (0.97) | 1.99, 3.69 | 4 | 2.41 (1.19) | 1.71, 3.11 | 6 | 2.30 (0.96) | 1.63, 2.97 |
| Evaluating research and promoting physical health | 6 | 2.70 (1.18) | 2.35, 3.05 | 6 | 2.95 (1.28) | 2.11, 3.79 | 6 | 2.40 (0.77) | 1.92, 2.88 | 8 | 3.70 (1.07) | 2.76, 4.64 | 6 | 2.82 (1.23) | 2.09, 3.55 | 4 | 2.01 (0.97) | 1.34, 2.68 |
| A sense of humour | 7 | 2.95 (1.15) | 2.61, 3.29 | 7 | 3.22 (1.30) | 2.37, 4.07 | 7 | 2.60 (0.97) | 2.00, 3.20 | 3 | 2.20 (1.30) | 1.06, 3.34 | 8 | 3.27 (1.10) | 2.62, 3.92 | 8 | 3.13 (1.13) | 2.35, 3.91 |
| Physical and psychological interventions | 8 | 3.08 (1.19) | 2.72, 3.44 | 8 | 3.72 (1.24) | 2.91, 4.53 | 8 | 2.65 (1.06) | 1.99, 3.31 | 7 | 2.91 (1.09) | 1.95, 3.87 | 7 | 3.04 (1.09) | 2.40, 3.68 | 7 | 3.05 (1.02) | 2.34, 3.75 |
Clusters were ranked on a 1–5 scale, with one being the most important. The Lower the mean score, the more important the cluster.
The concept map is divided into four large areas (north, south, east, and west). The statements located in the same area are related and those in different regions are contrasting, for example, statements in the west contrast those in the east.
Ariadne produces three cluster formats: (a) rectangle with a single line border, (b) rectangle with a border made of multiple lines, (c) a shape that traces the position of the statements that form the boundary of the cluster. We initially selected the rectangle format because they are more straightforward to interpret. However, after reviewing map formats, we concluded that the cluster format that traces the position of statement was a more informative visual representation of the cluster.
Phase 5: Interpretation of concept map
Seven participants (Fig. 1) – at least one from each stakeholder group – and three members of the research team (NM, RG, MJ) agreed to take part in a focus group meeting to review and interpret the final concept map. The focus group was held via video conferencing and lasted 70 min. At the start of the focus group, RG showed participants the concept map, a list of statements in each cluster and asked them to generate labels for each grouping. Possible labels were discussed by the group and were either eliminated or retained. For clusters one, two, three, five, to eight, the consensus was straightforward. However, there was disagreement in the group around the label for cluster four (good communication skills). The debate centred on the inclusion of ‘good’ as an unnecessary adjective to describe communication skills. The majority view was that communication skills can be bad as well as good and it was important to emphasize that the statements in this cluster represented skills that participants valued.
Labelling the x‐ and y‐axes of the concept map
The x‐ and y‐axes on the map are viewed as themes that participants used to sort the statements (Brown, 2018; Rudawska, 2020). The axes can be interpreted based on these themes and labelled to improve the data's visual representation (Brown, 2018). NM proposed candidate names for the x‐axis and y‐axis by examining the statements (competencies) in the four quadrants of the map. The statements on the 'west' end of the x‐axis were related to patient care and communication skills. Therefore, the west end was labelled ‘interpersonal relationships’. The competencies in the extreme 'east' were about knowledge of mental disorders and treatment, and hence, the far east of the x‐axis was labelled ‘medical construction of mental experiences’.
The 'northern' end of the y‐axis was named ‘principles of care’ because the statements on the north of the y‐axis were linked to recovery principles and person‐centred care. The competencies towards the extreme 'southern' of the y‐axis were related to health assessments and communication skills and the 'southern' end was labelled ‘health assessment’.
There was general agreement among the participants about the axis labels. The labelled clusters and axis are shown in Fig. 3.
In the final part of the interpretation phase, participants considered the location and distance between the clusters to interpret the concept map. Participants were also asked to consider the thickness of the line surrounding each cluster as a visual cue to indicate the relative importance of the cluster; the thinner the line, the more important the cluster.
Description of eight clusters
Clusters were ranked according to their relative importance from one (most important) to eight (least important). Figure 3 is the final concept map showing the eight clusters. Table 3 shows the importance ranking of the eight clusters, by stakeholder group.
Cluster one, assessment and management of risk
There are six statements in cluster one, ‘assessment and management of risk’. Statements include ‘can undertake a risk assessment (harm to self)’, ‘conduct a mental state examination’, and ‘are able to handover patients accurately’. Cluster one is in the southeast quadrant of the concept map. The cluster's position on the x‐ and y‐axes indicates that it is related to health assessment (south of the y‐axis) and knowledge of mental disorders (east of the x‐axis). Cluster one is also located on the border of the y‐axis between cluster four, ‘good communication skills’ and cluster eight, ‘physical and psychological intervention’. Clusters four and eight are in different quadrants, suggesting that cluster one is related to these two concepts.
Cluster two, understanding recovery principles
Cluster two, ‘understanding recovery principles’, has one statement, ‘knowledge about the principles of recovery’, and is located on the far northeast of the map. The location suggests that the cluster is related to principles of care (north of the y‐axis). In addition, the positioning close to cluster five, ‘knowledge of mental health disorders and treatment’, also suggests that the two clusters are linked.
Cluster three, person‐ and family‐centred care
The statements in cluster three, ‘person‐ and family‐centred care’, are closely grouped together; consequently, the cluster is relatively small, suggesting an important relationship between statements. Cluster three also has the largest number (n = 17) of statements of all the clusters. Statements in the ‘person‐ and family‐centred care’ cluster include ‘are able to engage with consumers’, ‘works in a patient centred way’, and ‘skilled at talking to patients, families, and friends’. Cluster three is the only cluster positioned in the northwest quadrant of the map, suggesting that the concept is discreet.
Cluster four, good communication skills
‘Skilled in engaging people when they are distressed’, ‘skilled at working as part of a team’, and ‘clinical documentation is respectful’ are examples of the six statements that are included in cluster four, ‘good communication skills’. Cluster four is in the southwest of the map, in the same quadrant as clusters seven and one, suggesting they are related.
Cluster five, knowledge about mental disorders and treatment
Twelve statements are included in the ‘knowledge of different mental disorders and treatment’ cluster and include ‘knowledgeable about the use of Pro Re Nata (PRN) medication’, ‘are knowledgeable about risk factors for mental illness’, and ‘knowledgeable about different psychotherapeutic techniques’. Cluster five is situated between clusters two and six, ‘evaluating research and promoting physical health’ and in the same quadrant, suggesting that these three clusters may be related.
Cluster six, evaluating research and promoting physical health
Cluster six, ‘evaluating research and promoting physical health’, is located just above the x‐axis line towards the east of the map. The cluster has two statements: ‘Skilled in being able to critically evaluate new research’ and ‘are skilled in promoting physical health’. The two statements in cluster six are diagonally opposite, suggesting that they may not be closely related.
Cluster seven, a sense of humour
Located just below the x‐axis and to the west of the map is cluster seven, ‘a sense of humour’. The cluster has a single statement, ‘have a good sense of humour’. Cluster seven is positioned close to cluster three but is in a different quadrant, suggesting they are not related.
Cluster eight, physical and psychological interventions
Cluster eight, ‘physical and psychological interventions’, is made up of eight statements that include ‘can undertake a physical health assessment’, ‘competent in taking blood’, and ‘competent in delivering different psychotherapeutic techniques’. The cluster is located in the southeast quadrant of the map.
Comparisons between stakeholder groups
Table 3 shows the mean, standard deviation, and 95% confidence intervals for each cluster by stakeholder groups and for all participants.
There were notable discrepancies in how different stakeholder groups perceived the relative importance of clusters. For example, service users rated cluster one, ‘assessment and management of risk’, as less important, whilst the other four groups ranked it as the most important. The ‘understanding recovery principles’ cluster was highly ranked by service users, mental health nurses, and managers. Conversely, psychiatrists and academics put this cluster towards the middling of the ranking. There was a marked difference in the rating of cluster three, ‘person‐ and family‐centred care’. It was highly ranked by service users, nurse academics, and psychiatrists, and lowly by mental health nurses and managers. Clusters four and five were ranked similarly by the stakeholder groups. ‘Evaluating research and promoting physical health’ cluster was ranked fourth by nurse academics and low by other groups. All participating groups gave the ‘sense of humour’ cluster a low ranking except for psychiatrists, who ranked the cluster as third most important. Physical and psychological interventions cluster was rated less important by all participant groups.
DISCUSSION
We report a concept mapping study to describe and contrast the core competencies of mental health nurses from the perspective of five stakeholder groups. Our final concept map had eight clusters: Assessment and management of risk, understanding recovery principles, person‐ and family‐centred care, good communication skills, knowledge about mental disorders and treatment, evaluating research and promoting physical health, a sense of humour, physical and psychological interventions.
Broadly, the eight clusters are consistent with those reported in previous systematic reviews (Bee et al. 2008; Delaney & Johnson, 2014) and primary studies (King et al. 2019; Moll et al. 2018; Stewart et al. 2015). For example, assessment and management of risk, person‐centred care, and good communication skills are consistently identified as important competencies of mental health nurses (Gunasekara et al. 2014; Testerink et al. 2019; Ward & Gwinner, 2015).
Our study extends knowledge by enabling us to consider differences between stakeholder groups. The most notable differences we observed were between service users and other groups. For example, professionals rated the 'assessment and management of risk' cluster as the most important whilst service users ranked this cluster as less important. Service users, mental health nurses and managers rated understanding recovery principles as most important, whilst psychiatrists and nurse academics indicated these were less important. The discrepancy between groups has not been previously reported and provides some limited evidence of a disconnect between service users and professionals view about the core work of mental health nurses.
Despite the importance of physical health in mental health, all stakeholder groups ranked the ‘physical and psychological interventions’ cluster as less important. Competencies in physical health interventions benefit service users physically and aid in the development of therapeutic relationships between the service user and the nurse (Hawamdeh & Fakhry, 2014). However, some mental health nurses perceive they are less competent to provide physical care than expected of them (Celik Ince et al. 2018), whilst others believe it falls beyond their scope of practice (Gray & Brown, 2017).
The competencies identified by participants in our study tended to be brief and highly specific (e.g. ‘spending time with consumers’, ‘able to express empathy’) and are seemingly discrepant to how competencies are described in health policy documents that tend to involve multiple elements. For example, in the Australian College of Mental Health Nursing, standard 3 of practice policy states that ‘mental health nurse develops a therapeutic relationship that is respectful of the individual’s choices, experiences and circumstances, this involves building on strengths, holding hope, and enhancing resilience to promote recovery’. Our observation may suggest that stakeholders do not conceptualize – in clinical practice – competencies in the way they are described in policy documents. Rather, stakeholders tend to fracture complex ideas into component concepts that they can interpret and process. The concise descriptions of competency statements in other studies are consistent with our findings. For example, 52 nurses working in mental health intensive care units identified empathy, active listening, and appropriate body language as core nursing competencies (Ward & Gwinner, 2015).
We also observed that some of the competencies identified in our study are not reported in the Standards of Practice for Australian Mental Health Nurses 2010, for example, ‘knowledge about Safewards interventions’ and ‘work in a trauma‐informed way’. Competencies in trauma‐informed care were also noted as important in the Royal Commission into Victoria’s Mental Health System (2021). The Royal Commission into Victoria’s Mental Health System (2021) examined the views of service users, families, carers and supporters, nurses, and other mental health professionals about the competencies of mental health professionals. The Royal Commission identified that mental health professionals (including nurses) lacked competency in promoting personal recovery and helping service users who have been traumatized (Royal Commission into Victoria’s Mental Health System, 2021). Wilson et al. (2017) included 11 studies in the literature review to examine the challenges mental health nurses face in integrating trauma‐informed care into acute inpatient settings in Australia. The authors report that trauma‐informed care can promote a positive organizational culture and improve the care provided to service users (Wilson et al. 2017).
In our study, participants reflected on interventions they had exposure to through their clinical experience. There is a need to consider how the scope of practice of mental health nurses evolves as new evidence emerges. For example, participants noted ‘trauma‐informed care’ as a candidate way of working for the revised scope of mental health nursing practice. The ACMHN needs to consider the quality of evidence that underpins emerging interventions and whether they should be included as a core competency for mental health nurses.
Person‐ and family‐centred care is a method of health‐care planning, delivery, and assessment based on mutually beneficial collaborations between health‐care professionals, service users, and families (Johnson & Abraham, 2012). It is sometimes challenging to collaborate with service users and their families, particularly when they have conflicting agendas (Goodwin & Happell, 2006). Many mental health services claim that person‐centred care is a core value of the service. We observed that the positioning of the person‐ and‐family‐centred care cluster on the concept map was distant from other clusters (the only cluster in the top left‐hand quadrant of the map). This observation perhaps suggests that the concept of person‐centred care has not been meaningfully integrated into practice in a meaningful way.
The ‘understanding recovery principles’ cluster was also a discrete concept – with a single statement – that, although located on the map close to the ‘knowledge about mental disorders and treatment’ and ‘evaluating research and promoting physical health’ clusters was not part of a broader cluster that integrated the multidimensional construct of recovery‐focused working. A single statement has been classified as a cluster in previous studies (see, e.g. Brown et al. 2019; Cardwell et al. 2021).
A ‘sense of humour’ was a discrete cluster, and its location on the map made it distinct from other groups. On the map, it is closely related to ‘good communication skills’. Psychiatrists viewed ‘sense of humour’ as an important competence, but other groups did not. A sense of humour has been identified previously as an important part of mental health nursing practice in previous systematic reviews of qualitative studies (e.g. Cleary et al. 2012).
Limitations
There are several important limitations that need to be considered when interpreting the findings of our study. We used social media and snowballing techniques to recruit participants, this may have introduced selection bias. It is likely that people who actively use social media are systematically different to those who do not. A computer software package was used to undertake prioritization and clustering tasks, this may have discouraged people who did not have good computer skills from participating. Our study did not involve carers, or other professional groups working in mental health settings. These groups may have provided different views and they should be considered in future studies. Nurses working in mental health are not required to have a postgraduate qualification; this may impact the insights that they are able to share about the competencies of mental health nurses. It may be that we should only have included nurses who had evidence that they had completed postgraduate training in mental health, and this is an acknowledged limitation of our study.
On reflection, participants seemly reported an inclusive definition of what a mental health nurse is, which contrasts with the explicit definition used by the ACMHN. In our study, stakeholders were situated within a specific time and place and socio‐political context. Inevitably this will have impacted the competencies that were generated and the relative importance that participants ascribed to them.
The study used convenience sampling, and therefore, the results cannot be generalized beyond the views of the participants. There is no agreed‐upon number of people needed for the concept mapping (Ariadne, 2015; Rosas & Kane, 2012; Trochim, 1989). The sample size in our study is consistent with previous studies that have used a concept mapping methodology (Iris et al. 2010; Johnson et al. 2014; Kabukye et al. 2020; Niemeijer et al. 2011; Robinson & Trochim, 2007). Our aim was not to have a representative sample but rather to inform our understanding of complex phenomena. A final limitation of our study was the decision to have researchers and not stakeholder make the decision about which cluster map solution to use. The researchers may have unknowingly chosen the cluster map solution that had clusters with clinically related statements but not conceptually representing the views of participants.
CONCLUSION
Service users and mental health professionals have conflicting perspectives about the relative importance, particularly the ‘assessment and management of risk’. Further research is needed to test these ideas in representative samples of service users and mental health workers.
RELEVANCE TO CLINICAL PRACTICE
We observed a potential disconnect between service users and professional stakeholder groups about the core work of mental health nurses. A further study examining the differing perspectives of service users and health professionals on the core competencies of mental health nurses is required. The ACMHN should consider reviewing the existing competencies of mental health nurses, particularly in light of emerging evidence about the effectiveness of different interventions.
Supporting information
File S1 Seventeen candidate concept maps produced by Ariadne concept mapping software.
ACKNOWLEDGEMENT
We would like to express our appreciation to the participants who took part in this study. Open access funding provided by La Trobe University.
Authorship statement: All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors. All authors contributed to the conception and design of the study. NM collected, and analysed the data. All authors interpreted the study results. NM wrote the initial draft. NM, MJ and RG reviewed and edited the manuscript. All authors read and approved the final manuscript.
Declaration of conflict of interest: The authors declare no conflicts of interest.
Open Science Framework Registration: https://doi.org/10.17605/OSF.IO/9XJNH.
REFERENCES
- Ariadne . (2015). Manual Ariadne 3.0. Amsterdam, The Netherlands: Ariadne. http://www.minds21.org/images_public/manual%20%20ARIADNE%203.0%20%20april%202015.pdf [Google Scholar]
- Askey, R. , Holmshaw, J. , Gamble, C. & Gray, R. (2009). What do carers of people with psychosis need from mental health services? Exploring the views of carers, service users and professionals. Journal of Family Therapy, 31 (3), 310–331. [Google Scholar]
- Australian College of Mental Health Nurses . (2010). Standards of Practice for Australian Mental Health Nurses: 2010. Canberra, Australia: Australian College of Mental Health Nurses; 16 Jan 2022. https://acmhn.org/wp‐content/uploads/2021/10/standards_2010_web.pdf [Google Scholar]
- Australian College of Mental Health Nurses . (2013). Scope of practice of Mental Health Nurses in Australia 2013. Canberra, Australia: Australian College of Mental Health Nurses, https://acmhn.org/wp‐content/uploads/2021/10/StandardsScopeWebVersion.pdf. [Google Scholar]
- Australian Commission on Safety and Quality in Health Care . (2019). Person‐Centred Care. Sydney, Australia: Australian Commission on Safety and Quality in Health Care. https://www.safetyandquality.gov.au/our‐work/partnering‐consumers/person‐centred‐care [Google Scholar]
- Australian Department of Health Victoria . (2021). Person‐Centred Practice. Melbourne, Australia: Australian Department of Health Victoria. https://www.health.vic.gov.au/patient‐care/person‐centred‐practice [Google Scholar]
- Barnett, E. R. , Concepcion‐Zayas, M. T. , Zisman‐Ilani, Y. & Bellonci, C. (2019). Patient‐centered psychiatric care for youth in foster care: A systematic and critical review. Journal of Public Child Welfare, 13 (4), 462–489. [Google Scholar]
- Bee, P. , Playle, J. , Lovell, K. , Barnes, P. , Gray, R. & Keeley, P. (2008). Service user views and expectations of UK‐registered mental health nurses: A systematic review of empirical research. International Journal of Nursing Studies, 45 (3), 442–457. [DOI] [PubMed] [Google Scholar]
- Bee, P. , Price, O. , Baker, J. & Lovell, K. (2015). Systematic synthesis of barriers and facilitators to service user‐led care planning. British Journal of Psychiatry, 207 (2), 104–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biringer, E. , Hove, O. , Johnsen, Ø. & Lier, H. Ø. (2021). “People just don’t understand their role in it”. Collaboration and coordination of care for service users with complex and severe mental health problems. Perspectives in Psychiatric Care, 57 (2), 900–910. 10.1111/ppc.12633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, E. (2018). What Are the Barriers to Accessing Psychological Therapy in Qatar: A Concept Mapping Study. Ann Arbor, MI: ProQuest Dissertations Publishing. [Google Scholar]
- Brown, E. , Topping, A. & Cheston, R. (2019). What are the barriers to accessing psychological therapy in Qatar: A concept mapping study. Counselling and Psychotherapy Research, 19 (4), 441–454. [Google Scholar]
- Burke, J. G. , O’Campo, P. , Peak, G. L. , Gielen, A. C. , McDonnell, K. A. & Trochim, W. M. K. (2005). An introduction to concept mapping as a participatory public health research method. Qualitative Health Research, 15 (10), 1392–1410. [DOI] [PubMed] [Google Scholar]
- Cardwell, R. , McKenna, L. , Davis, J. & Gray, R. (2021). How is clinical credibility defined in nursing? A concept mapping study. Journal of Clinical Nursing, 30 (17–18), 2441–2452. [DOI] [PubMed] [Google Scholar]
- Çelik, I. S. , Partlak, G. N. & Serçe, Ö. (2018). The opinions of Turkish mental health nurses on physical health care for individuals with mental illness: A qualitative study. Journal of Psychiatric and Mental Health Nursing, 25 (4), 245–257. [DOI] [PubMed] [Google Scholar]
- Cleary, M. , Hunt, G. E. , Horsfall, J. & Deacon, M. (2012). Nurse‐patient interaction in acute adult inpatient mental health units: A review and synthesis of qualitative studies. Issues in Mental Health Nursing, 33 (2), 66–79. [DOI] [PubMed] [Google Scholar]
- Comiskey, C. , Galligan, K. , Flanagan, J. , Deegan, J. , Farnann, J. & Hall, A. (2019). Clients’ views on the importance of a nurse‐led approach and nurse prescribing in the development of the healthy addiction treatment recovery model. Journal of Addictions Nursing, 30 (3), 169–176. [DOI] [PubMed] [Google Scholar]
- Cowman, S. , Farrelly, M. & Gilheany, P. (2001). An examination of the role and function of psychiatric nurses in clinical practice in Ireland. Journal of Advanced Nursing, 34 (6), 745–753. [DOI] [PubMed] [Google Scholar]
- Delaney, K. R. & Johnson, M. E. (2014). Metasynthesis of research on the role of psychiatric inpatient nurses: What is important to staff? Journal of the American Psychiatric Nurses Association, 20 (2), 125–137. [DOI] [PubMed] [Google Scholar]
- Edvardsson, D. (2015). Notes on person‐centred care: What it is and what it is not. Vård I Norden, 35 (2), 65–66. [Google Scholar]
- Gondek, D. , Edbrooke‐Childs, J. , Velikonja, T. et al. (2017). Facilitators and barriers to person‐centred care in child and young people mental health services: A systematic review. Clinical Psychology and Psychotherapy, 24 (4), 870–886. [DOI] [PubMed] [Google Scholar]
- Goodwin, V. & Happell, B. (2006). Conflicting agendas between consumers and carers: The perspectives of carers and nurses. International Journal of Mental Health Nursing, 15 (2), 135–143. [DOI] [PubMed] [Google Scholar]
- Gray, R. & Brown, E. (2017). What does mental health nursing contribute to improving the physical health of service users with severe mental illness? A thematic analysis. International Journal of Mental Health Nursing, 26 (1), 32–40. [DOI] [PubMed] [Google Scholar]
- Grisham, T. (2009). The Delphi technique: A method for testing complex and multifaceted topics. International Journal of Managing Projects in Business, 2 (1), 112–130. [Google Scholar]
- Gunasekara, I. , Pentland, T. , Rodgers, T. & Patterson, S. (2014). What makes an excellent mental health nurse? A pragmatic inquiry initiated and conducted by people with lived experience of service use. International Journal of Mental Health Nursing, 23 (2), 101–109. [DOI] [PubMed] [Google Scholar]
- Happell, B. (2009). Appreciating history: The Australian experience of direct‐entry mental health nursing education in universities. International Journal of Mental Health Nursing, 18 (1), 35–41. [DOI] [PubMed] [Google Scholar]
- Hawamdeh, S. & Fakhry, R. (2014). Therapeutic relationships from the psychiatric nurses’ perspectives: An interpretative phenomenological study. Perspectives in Psychiatric Care, 50 (3), 178–185. [DOI] [PubMed] [Google Scholar]
- Hayes, P. (2020). Why Quality is Important and How It Applies in Diverse Business and Social Environments (Vol. 11). New York, NY: Business Expert Press. [Google Scholar]
- Iris, M. , Ridings, J. W. & Conrad, K. J. (2010). The development of a conceptual model for understanding elder self‐neglect. The Gerontologist, 50 (3), 303–315. [DOI] [PubMed] [Google Scholar]
- Johnson B. H. & Abraham M. R. (2012). Partnering with patients, residents, and families: A resource for leaders of hospitals, ambulatory care settings, and long‐term care communities. Bethesda, MD: Institute for Patient‐ and Family‐Centered Care. [Google Scholar]
- Johnson, D. B. , Quinn, E. , Sitaker, M. et al. (2014). Developing an agenda for research about policies to improve access to healthy foods in rural communities: A concept mapping study. BMC Public Health, 14 (1), 592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, M. , Bennett, J. , Lucas, B. , Miller, D. & Gray, R. (2007). Mental health nurse supplementary prescribing: Experiences of mental health nurses, psychiatrists and patients. Journal of Advanced Nursing, 59 (5), 488–496. [DOI] [PubMed] [Google Scholar]
- Kabukye, J. K. , de Keizer, N. & Cornet, R. (2020). Elicitation and prioritization of requirements for electronic health records for oncology in low resource settings: A concept mapping study. International Journal of Medical Informatics (Shannon, Ireland), 135, 104055. [DOI] [PubMed] [Google Scholar]
- Kikkert, M. J. , Schene, A. H. , Koeter, M. W. J. et al. (2006). Medication adherence in schizophrenia: Exploring patients’, carers’ and professionals’ views. Schizophrenia Bulletin, 32 (4), 786–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, B. M. , Linette, D. , Donohue‐Smith, M. & Wolf, Z. R. (2019). Relationship between perceived nurse caring and patient satisfaction in patients in a psychiatric acute care setting. Journal of Psychosocial Nursing and Mental Health Services, 57 (7), 29–38. [DOI] [PubMed] [Google Scholar]
- Lund, B. D. (2020). Review of the Delphi method in library and information science research. Journal of Documentation, 76 (4), 929–960. [Google Scholar]
- McAllister, S. , Simpson, A. , Tsianakas, V. & Robert, G. (2021). “What matters to me”: A multi‐method qualitative study exploring service users’, carers’ and clinicians’ needs and experiences of therapeutic engagement on acute mental health wards. International Journal of Mental Health Nursing, 30 (3), 703–714. [DOI] [PubMed] [Google Scholar]
- Moll, M. F. , Pires, F. C. , Ventura, C. A. A. , Boff, N. N. & da Silva, N. F. (2018). Psychiatric nursing care in a general hospital: Perceptions and expectations of the family/caregiver. Journal of Psychosocial Nursing and Mental Health Services, 56 (8), 1–36. [DOI] [PubMed] [Google Scholar]
- Moyo, N. , Jones, M. , Cardwell, R. & Gray, R. (2020). What are the core competencies of a mental health nurse? Protocol for a concept mapping study. Nursing Reports (Pavia, Italy), 10 (18), 146–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyo, N. , Jones, M. , Kushemererwa, D. et al. (2020). The Association between the mental health nurse‐to‐registered nurse ratio and patient outcomes in psychiatric inpatient wards: A systematic review. International Journal of Environmental Research and Public Health, 17 (18), 6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemeijer, A. R. , Frederiks, B. J. M. , Depla, M. F. I. A. , Legemaate, J. , Eefsting, J. A. & Hertogh, C. M. P. M. (2011). The ideal application of surveillance technology in residential care for people with dementia. Journal of Medical Ethics, 37 (5), 303–310. [DOI] [PubMed] [Google Scholar]
- Nursing and Midwifery Board of Australia . (2012). Nurses with a sole qualification in mental health nursing. Melbourne, Australia: Nursing and Midwifery Board of Australia. https://www.nursingmidwiferyboard.gov.au/News/Newsletters/March‐2012.aspx#nurseswithasole. [Google Scholar]
- Nursing and Midwifery Council United Kingdom . (2018). Realising Professionalism: Standards for Education and Training. Part 3: STANDARDS for Pre‐registration Nursing Programmes. London, UK: Nursing and Midwifery Council United Kingdom. https://www.nmc.org.uk/globalassets/sitedocuments/standards‐of‐proficiency/standards‐for‐pre‐registration‐nursing‐programmes/programme‐standards‐nursing.pdf [Google Scholar]
- O’Cathain, A. , Murphy, E. & Nicholl, J. (2008). The quality of mixed methods studies in health services research. Journal of Health Services Research & Policy, 13 (2), 92–98. [DOI] [PubMed] [Google Scholar]
- Ponterotto, J. G. (2005). Qualitative research in counseling psychology: A primer on research paradigms and philosophy of science. Journal of Counseling Psychology, 52 (2), 126–136. [Google Scholar]
- Robinson, J. M. & Trochim, W. M. K. (2007). An examination of community members’, researchers’ and health professionals’ perceptions of barriers to minority participation in medical research: an application of concept mapping. Ethnicity & Health, 12 (5), 521–539. [DOI] [PubMed] [Google Scholar]
- Rosas, S. R. & Kane, M. (2012). Quality and rigor of the concept mapping methodology: A pooled study analysis. Evaluation and Program Planning, 35 (2), 236–245. [DOI] [PubMed] [Google Scholar]
- Royal Commission into Victoria’s Mental Health System . (2021). Final Report, Volume 1: A new approach to mental health and wellbeing in Victoria, Parl Paper No. 202, Session 2018–21 (document 2 of 6). Melbourne, Australia: State of Victoria, Royal Commission into Victoria’s Mental Health System. https://finalreport.rcvmhs.vic.gov.au/wp‐content/uploads/2021/02/RCVMHS_FinalReport_Vol1_Accessible.pdf [Google Scholar]
- Rudawska, I. (2020). Concept Mapping in developing an indicator framework for coordinated health care. Procedia Computer Science, 176, 1669–1676. [Google Scholar]
- Santangelo, P. , Procter, N. & Fassett, D. (2018). Seeking and defining the ‘special’ in specialist mental health nursing: A theoretical construct. International Journal of Mental Health Nursing, 27 (1), 267–275. [DOI] [PubMed] [Google Scholar]
- Schwandt, T. A. (1994). Constructivist, interpretivist approaches to human inquiry. Handbook of qualitative research. (pp. 118–137). Thousand Oaks, CA: SAGE. [Google Scholar]
- Sinclair, L. , Hunter, R. , Hagen, S. , Nelson, D. & Hunt, J. (2006). How effective are mental health nurses in A&E departments? Emergency Medicine Journal, 23 (9), 687–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart, D. , Burrow, H. , Duckworth, A. et al. (2015). Thematic analysis of psychiatric patients’ perceptions of nursing staff. International Journal of Mental Health Nursing, 24 (1), 82–90. [DOI] [PubMed] [Google Scholar]
- Testerink, A. E. , Lankeren, J. E. , Daggenvoorde, T. H. , Poslawsky, I. E. & Goossens, P. J. J. (2019). Caregivers experiences of nursing care for relatives hospitalized during manic episode: A phenomenological study. Perspectives in Psychiatric Care, 55 (1), 23–29. [DOI] [PubMed] [Google Scholar]
- Trochim, W. M. (1989). An introduction to concept mapping for planning and evaluation. Evaluation and Program Planning, 12 (1), 1–16. [Google Scholar]
- Victorian Government . (1993). Nurses Act 1993. Melbourne, Australia: Victorian Government. http://classic.austlii.edu.au/au/legis/vic/hist_act/na1993111.pdf [Google Scholar]
- Ward, L. & Gwinner, K. (2015). Have you got what it takes? Nursing in a Psychiatric Intensive Care Unit. The Journal of Mental Health Training, Education, and Practice, 10 (2), 101–116. [Google Scholar]
- Wilson, A. , Hutchinson, M. & Hurley, J. (2017). Literature review of trauma‐informed care: Implications for mental health nurses working in acute inpatient settings in Australia. International Journal of Mental Health Nursing, 26 (4), 326–343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File S1 Seventeen candidate concept maps produced by Ariadne concept mapping software.


