Abstract
Background: Prediabetes is a reversible condition, but lifestyle-changing measures, such as increasing physical activity, should be taken. This article explores the use of Fitbit activity trackers to assess physical activity and its impact on prediabetic patient health. Methods: Intervention study. In total, 30 volunteers (9 males and 21 females), aged 32–65 years, with impaired glucose levels and without diabetes or moving disorders, received Fitbit Inspire activity trackers and physical activity recommendations. A routine blood check was taken during the first and second visits, and body composition was analyzed. Physical activity variability in time was assessed using a Poincare plot. Results: The count of steps per day and variability differed between patients and during the research period, but the change in total physical activity was not statistically significant. Significant positive correlations between changes in lipid values, body mass composition, and variability of steps count, distance, and minutes of very active physical activity were observed. Conclusions: When assessing physical activity, data doctors should evaluate not just the totals or the medians of the steps count, but also physical activity variability in time. The study shows that most changes were better linked to the physical activity variability than the total count of physical activity.
Keywords: prediabetes, activity trackers, variability
1. Introduction
Prediabetes is a term used increasingly to describe people with impaired glucose tolerance (IGT) and/or impaired fasting glucose (IFG) [1]. Impaired glucose tolerance (IGT) and impaired fasting glucose (IFG) are conditions of raised blood glucose levels above the normal range and below the diabetes diagnostic threshold. The importance of IGT and IFG is three-fold: first, they signify a higher risk of the future development of type 2 diabetes mellitus (T2D); second, IGT and IFG indicate an already heightened risk of cardiovascular disease; and third, their detection opens the door to interventions that can lead to the prevention of type 2 diabetes [2,3,4,5,6]. In 2021, 541 million adults, or 10.6% of adults worldwide, were estimated to have IGT. By 2045, this figure is projected to increase to 730 million adults, or 11.4% of all adults. In 2021, there were an estimated 319 million adults, or 6.2% of the global adult population with IFG. An estimated 441 million adults, or 6.9% of the global adult population, are projected to have IFG in 2045 [1]. This makes prediabetes one of the most rapidly growing health problems. The most common causes of this pathology are overweight and obesity and the main reasons for this are malnutrition and low physical activity [7]. Modification in lifestyle plays an important role in avoiding the prognosis of type 2 diabetes (T2D) and its complications in the future. One such lifestyle change that has been positively correlated with stopping the progression of T2D in those with prediabetes is increasing physical activity (PA) [8].
Just 150 min/week of moderate-intensity physical activity, such as brisk walking, showed beneficial effects in those with prediabetes [9]. Several major randomized controlled trials, including the Diabetes Prevention Program (DPP) [9], the Finnish Diabetes Prevention Study (DPS) [10], and the Da Qing Diabetes Prevention Study (Da Qing study) [11], demonstrate that lifestyle/behavioral therapy with an individualized reduced-calorie meal plan is highly effective in preventing or delaying type 2 diabetes and improving other cardiometabolic markers (such as blood pressure, lipids, and inflammation) [12]. The most substantial evidence for diabetes prevention in the U.S. comes from the DPP trial [9]. The DPP demonstrated that intensive lifestyle intervention could reduce the risk of incident type 2 diabetes by 58% over three years.
One of first steps in improving healthy lifestyle behavior is physical activity evaluation. Tools used to assess physical activity (PA) are questionnaires or physical activity diaries and objective data collection. Objective data collections can be divided into four groups. These are the measurement of energy consumption, the measurement of physiological parameters, the measurement of movements, and positioning [13]. Currently, the most popular method for PA estimation is direct motion measurement. Pedometers and accelerometers are used for this purpose. In recent years, we went through enormous mobile devices breakthroughs, and now we can count our steps using smartphones, smartwatches, and activity trackers. Smart bracelets measure the daily number of steps with sufficient accuracy and are suitable for long-term physical activity assessment [14,15,16,17].
At present, diabetes and cardiovascular diseases in Lithuania are among the leading causes of illness and death [18]. The country does not have a unified obesity and diabetes prevention program at the state level, but the greatest prevention is done by family doctors’ practice. The increasing popularity of physical activity trackers gives us the opportunity to evaluate physical activity more objectively and use it in practice. Studies reveal that the use of modern technologies helps not only to evaluate PA but also to improve it [19]. That leads to a reduction of body fat, cholesterol, and glycated hemoglobin levels [20,21].
Our aims were to evaluate the use of Fitbit activity trackers in the assessment of physical activity and its variability in time, and to evaluate physical activity’s impact on body fat, glycated hemoglobin, and cholesterol levels in patients with prediabetes. We used Fitbit activity trackers as the most common tools to reach this goal and evaluate their benefits and limitations [22].
2. Materials and Methods
2.1. Recruitment
This intervention study evaluated Fitbit data clinical use opportunities in primary care and diabetes prevention. Eligible participants, aged from 18 to 65 years old, had increased fasting glucose levels (5.6 to 6.9 mmol/L), had no health issues with the skeletal or muscular system, and other conditions that could compromise their ability to move [23]. Inclusion criteria consisted of voluntary participation in the study and had to have a smartphone with the latest operating system (Apple iOS 13, Android OS 8.0 or later), email address, and being able to use it.
The thirty volunteers were visiting family doctors at Vilnius University Hospital Santaros Klinikos (VUHSK) Family medicine center. Participants received a Fitbit Inspire activity tracker (AT), and they allowed researchers to collect data from their accounts after six months of wearing it.
There were two visits to the Family medicine center. During the first visit, we performed body mass composition analysis with the medical bioimpedance device X-contact 356 and made a routine blood test. Total cholesterol, triglycerides, low-density lipoproteins, high-density lipoproteins, and glycated hemoglobin were performed. After all the tests, the patients were consulted by their family doctor, and recommendations on a healthy diet and physical activity (based on World Health Organisation recommendations) were given.
The second visit was after six months. We repeated the same procedures as in the first visit, and after all, we asked participants to log in to their accounts at accounts.fitbit.com/login and exported data from the research period.
The study was approved by the Vilnius Regional Biomedical Research Ethics Committee (approval no. 2019/6-1143-634). Fitbit was not involved in the design, implementation, data analysis, or manuscript preparation of the study.
2.2. Intervention Tools
Every participant was given a Fitbit Inspire activity tracker. Fitbit is a consumer product to monitor physical activity such as steps, distance, physical activity levels, and sedentary time. These are commonly small devices worn on the wrist and can be used individually by the screen on the device or connected by a smartphone and mobile application. The Fitbit activity tracker uses a microelectronic triaxial accelerometer to capture body motion in 3 dimensions, and then these motions are analyzed by the alghorytmes and converted to physical activity data. These consumer devices showed respective data accuracy and are more commonly used in clinical trials [24]. Every participant was taught how to use these tools and was given full technical support during the study.
2.3. Data Analysis
The data obtained from the smart bracelets were: physical activity recording data, steps per day, distance, minutes sedentary, minutes weakly active, active, minutes fairly active, and minutes very active [25,26].
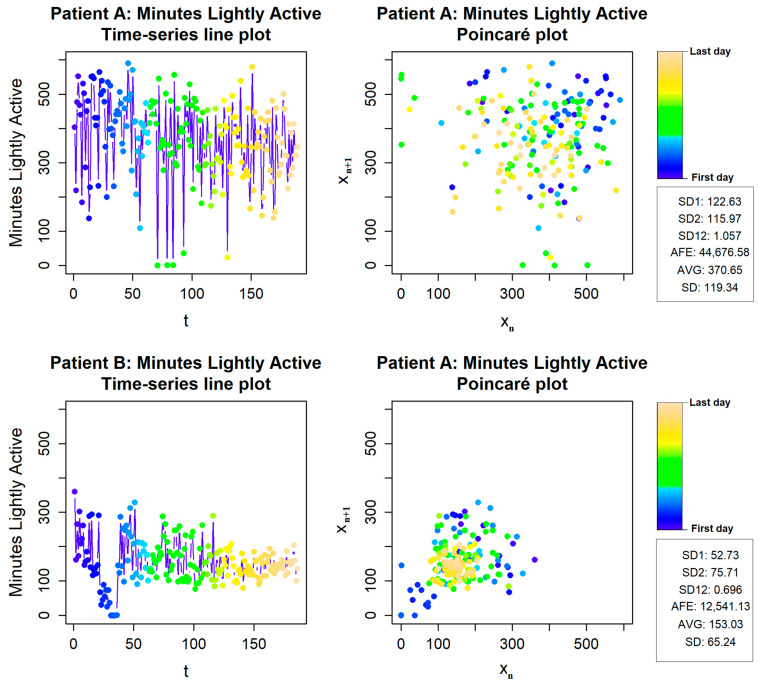
We adapted the Poincaré plot mathematical model to evaluate physical activity variability. This method is widely used to study physiological signals [27,28]. To analyze physical activity variability, the Poincaré plot method with a time delay of one day (i = 1) was applied and additional measures for selected physical activity time series accessed from patients’ Fitbit data were calculated. An average value (AVG), standard deviation (SD), and some standard Poincaré plot parameters representing short-term variability (SD1), long-term variability (SD2), the ratio of SD1 and SD2 (SD12), and area of fitting ellipse (AFE) were selected to analyze the variability.
2.4. Statistical Analysis
The Shapiro–Wilk test was used for normality testing. Paired t-test or Wilcoxon’s matched-pairs signed-rank test were used for baseline and follow-up data comparison. Pearson’s or Spearman’s correlation was performed to assess the association between changes in selected variables and physical activity variability parameters. Analyses were conducted using jamovi 1.6 and R 4.1.0 (RStudio, Boston, CA, USA), and R packages RHRV [29,30,31,32].
3. Results
3.1. Participants
In our study, twenty-one females and nine males participated and their mean age was 53.8 ± 9.1 years.
3.2. Body Mass Composition
The median weight was 87.6 ± 16.9 kg and BMI 32.0 [26.4–34.6]. We found a significant decrease in weight (p = 0.022) and a mass of body fat (p < 0.001). Furthermore, visceral fat level, visceral area, waist to hip ratio, and abdominal circumference decreased (p < 0.001). We obtained the same result in the mass of body fat measurement in the left (p = 0.008) and right arms (p = 0.005), and in the legs (p < 0.001) (Table 1).
Table 1.
Body mass composition.
| Baseline (n = 30) | Follow-Up—Baseline (n = 30) | p Value | Effect Size | SRM | |
|---|---|---|---|---|---|
| Weight [kg] # | 87.6 ± 16.9 | −1.46 ± 3.31 | 0.022 * | −0.4406 | −0.4411 |
| MBF [kg] # | 32.0 ± 9.72 | −1.8 ± 2.36 | <0.001 * | −0.7617 | −0.7627 |
| PBF [%] # | 36.1 ± 6.86 | −1.43 ± 1.59 | <0.001 * | −0.8971 | −0.8994 |
| VFL [Units] $ | 16.0 [13.0–18.0] | −0.867 [0–1.75] | <0.001 * | −0.87619 | −0.8337 |
| VFA [cm2] # | 169 ± 79.1 | −21.9 ± 23.9 | <0.001 * | −0.9162 | −0.9163 |
| WHR # | 0.948 ± 0.0912 | −0.022 ± 0.0282 | <0.001 * | −0.7798 | −0.7801 |
| AC [cm] # | 98.1 ± 13.0 | −2.16 ± 2.84 | <0.001 * | −0.7618 | −0.7606 |
| MBF Lt.ARM [kg] # | 1.93 ± 0.612 | −0.0777 ± 0.149 | 0.008 * | −0.5227 | −0.5215 |
| MBF Rt.ARM [kg] # | 1.91 ± 0.625 | −0.088 ± 0.159 | 0.005 * | −0.5518 | −0.5535 |
| MBF Lt.LEG [kg] # | 5.84 ± 1.75 | −0.345 ± 0.442 | <0.001 * | −0.7810 | −0.7805 |
| MBF Rt.LEG [kg] # | 5.83 ± 1.76 | −0.362 ± 0.444 | <0.001 * | −0.8146 | −0.8153 |
| MBF Trunk [kg] # | 16.5 ± 4.98 | −0.924 ± 1.2 | <0.001 * | −0.7666 | −0.7700 |
Values are presented as mean ± SD or median [Q1–Q3]. * Two-sided p value < 0.05. # Paired t-test, Cohen’s d (effect size). $ Wilcoxon’s matched pairs signed rank test, Rank biserial correlation (effect size). SRM—standardised response mean.
We did not find significant changes in other body mass composition parameters such as lean body mass, soft lean mass, skeletal muscle mass, body minerals and proteins, total body fat, and mass of soft lean mass in limbs.
3.3. Blood Tests
During the study, a statistically significant change in glycated hemoglobin levels, cholesterol, and triglycerides levels was not observed (Table 2).
Table 2.
Blood tests results.
| Baseline (n = 30) | Follow-Up—Baseline (n = 30) | p Value | Effect Size | SRM | |
|---|---|---|---|---|---|
| HgbA1c [%] # | 5.61 ± 0.352 | 0.0467 ± 0.2788 | 0.367 | 0.1674 | 0.1675 |
| HgbA1c [mmol/L] # | 37.7 ± 3.74 | 0.5333 ± 2.9564 | 0.331 | 0.1804 | 0.1804 |
| TC [mmol/L] # | 5.70 ± 1.14 | 0.199 ± 1.1188 | 0.338 | 0.1779 | 0.1779 |
| TG [mmol/L] $ | 1.81 [1.19–2.50] | −0.182 [−0.77–0.303] | 0.271 | −0.2344 | −0.1844 |
| HDL [mmol/L] $ | 1.29 [1.12–1.52] | 0.0287 [−0.1–0.13] | 0.593 | 0.1140 | 0.1643 |
| LDL [mmol/L] # | 3.44 ± 1.04 | 0.228 ± 1.0574 | 0.247 | 0.2156 | 0.2156 |
Values are presented as mean ± SD or median [Q1–Q3]. # Paired t-test, Cohen’s d (effect size). $ Wilcoxon’s matched pairs signed rank test, Rank biserial correlation (effect size). SRM—standardised response mean.
3.4. Physical Activity Evaluation Using Fitbit Inspire Physical Activity Tracker Data
Comparing the means of steps during the first and the last months of the trials, the mean of steps decreased by 1870 per day (p < 0.001), and the distance decreased by 1.29 km/day. Additionally, we have seen a statistically significant decrease in light activity by 47 min/day (p < 0.001), but we did not find any significant change in activity minutes for fairly active and very active physical activity. Sedentary time increased 67.3 min/day, but the change was not statistically significant. The main data is presented in Table 3.
Table 3.
Data from Fitbit Inspire physical activity tracker.
| Steps per Day | |||
| Month | Mean of count | Std. Deviation | Coefficient of variance |
| 1st | 9908 | 3625 | 0.43 |
| 2nd | 9816 | 3834 | 0.41 |
| 3rd | 8881 | 3969 | 0.46 |
| 4th | 8217 | 4117 | 0.53 |
| 5th | 7971 | 3597 | 0.52 |
| 6th | 8038 | 3897 | 0.54 |
| Activity: Sedentary | |||
| Month | Mean of minutes | Std. Deviation | Coefficient of variance |
| 1st | 804 | 274 | 0.24 |
| 2nd | 805 | 287 | 0.19 |
| 3rd | 816 | 275 | 0.18 |
| 4th | 898 | 322 | 0.18 |
| 5th | 927 | 290 | 0.17 |
| 6th | 871 | 266 | 0.25 |
| Activity: Lightly active | |||
| Month | Mean of minutes | Std. Deviation | Coefficient of variance |
| 1st | 281 | 117 | 0.4 |
| 2nd | 270 | 116 | 0.29 |
| 3rd | 263 | 121 | 0.36 |
| 4th | 216 | 132 | 0.54 |
| 5th | 211 | 105 | 0.55 |
| 6th | 233 | 99 | 0.45 |
| Activity: Fairly active | |||
| Month | Mean of minutes | Std. Deviation | Coefficient of variance |
| 1st | 17 | 15 | 1.05 |
| 2nd | 16 | 14 | 1.17 |
| 3rd | 14 | 11 | 1.06 |
| 4th | 10 | 10 | 1.25 |
| 5th | 11 | 10 | 1.49 |
| 6th | 14 | 13 | 1.34 |
| Activity: Very active | |||
| Month | Mean of minutes | Std. Deviation | Coefficient of variance |
| 1st | 8 | 8 | 1.28 |
| 2nd | 10 | 10 | 1.33 |
| 3rd | 9 | 10 | 1.25 |
| 4th | 10 | 15 | 1.43 |
| 5th | 9 | 13 | 1.74 |
| 6th | 11 | 14 | 1.52 |
As the raw physical activity data shows, how long the participants were physically active and the impact of physical activity variability on health results were evaluated.
3.5. Physical Activity Variability Evaluation Using Fitbit Inspire Data
For physical activity variability evaluation, we used the Poincaré plot method. As shown in Figure 1, we have data from two different subjects. In the upper charts, we have the first subject, whose SD1 and SD2 (SD12) ratio is close to 1, which means physical activity variability is always high. The second, lower example shows a much lower SD12 ratio, and the short-term variability is much lower than the long-term.
Figure 1.
Physical activity variability of patients A and B.
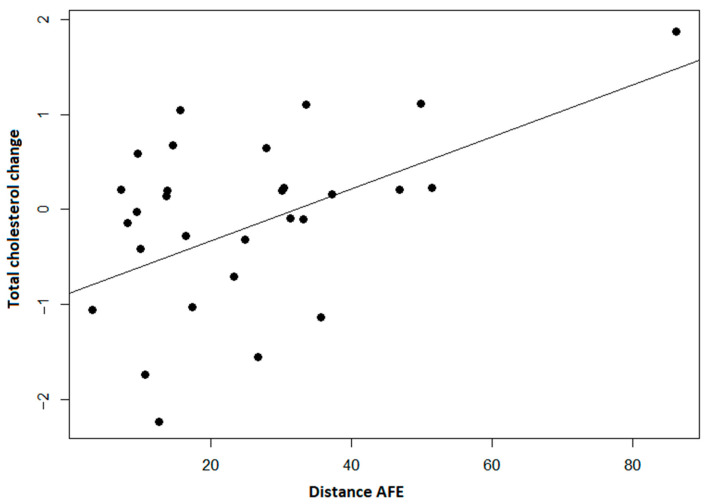
We observed significant positive correlations between changes in lipid values and variability of steps count, distance, and minutes of very active physical activity. It shows a decrease in lipid levels with lower long-term variability and area of an ellipse, but not short-term variability (Figure 2).
Figure 2.
Distance per day area of the fitting ellipse (AFE) and change in total cholesterol shows us that when the fitting ellipse increases, the level of total cholesterol increases (p < 0.001).
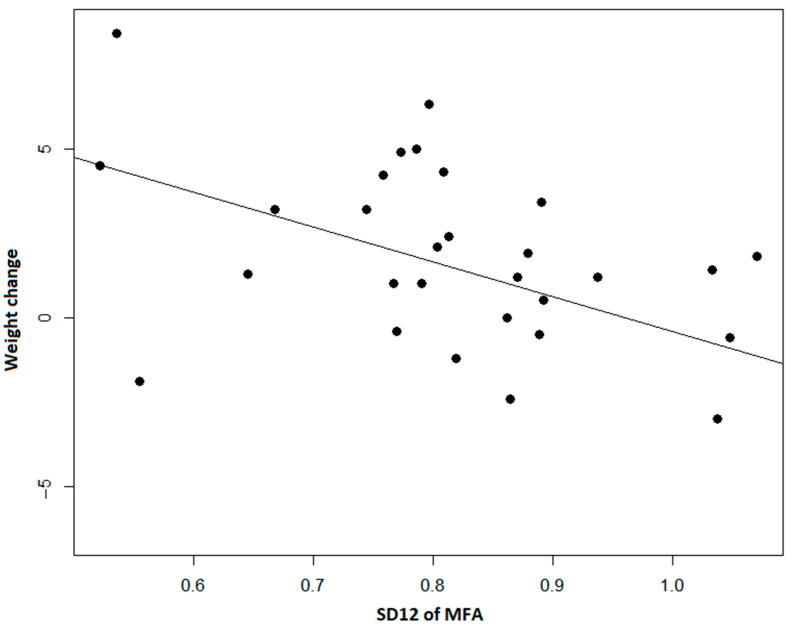
The SD1/SD2 ratio showed an opposite relationship with body fat measures indicating that possibly higher short-term variability could be associated with positive changes (Figure 3).
Figure 3.
The ratio of SD1 and SD2 of Minutes Fairly Active (MFA) shows us a correlation between lower short-term and long-term variability ratios and weight. The smaller the short-term and long-term variability ratio, the smaller the decrease in weight observed (p < 0.001).
4. Discussion
4.1. Principal Result
Studies show that the use of consumer-level physical activity trackers could be the alternative to more conservative methods. It has its strengths such as activity trackers that can track PA all the time, activity is leveled in different intensities, it does not require time to fill the forms, and we should not be afraid of retrospective inaccuracy as physical activity can be tracked for an unlimited time. As we found in our study, Mickael Ringeval et al. also found that Fitbit devices in interventions can promote healthy lifestyles in terms of physical activity and weight [33].
The evaluation of physical activity distribution in time is an important factor in assessing a patient’s lifestyle. Constantly higher physical activity has a higher impact on the metabolic effect and body mass composition. Silva BGC et al. research shows that adipose was lower among those who were constantly active or became active [34]. In addition, the study of Carnero EA et al. conducted research with non-diabetic patients for whom bariatric surgery was performed. Physical activity intervention helped patients in the highest quartile of step/day change lose more fat mass, abdominal adipose tissue, and gain skeletal muscle mass [35]. However, we need further research to establish publicly accessible tools, to evaluate physical activity variability, and keep in touch with a patient. Therefore, our research looks for consumer tools and mathematical models to make it adaptable in clinical practice and everyday life.
Our results show significant monthly steps and physical activity decline during the period of the study. This could be referred to the time of the year, and the epidemiologic situation. The study took place from the end of the summer (August) to the middle of wintertime (February), and, usually, people are less physically active at this time of the year. Second, the study started before the second wave of COVID-19 pandemic and ended during the national lockdown. When comparing these two periods of time, before and after lockdown, the steps per day mean decreased by 1852 steps, and on the other hand, the sedentary time increased by 75 min per day (p < 0.001).
The change in physical activity in time is one of the most important factors that is hard to assess by questionnaires, but now we can track it with smart bracelets, activity trackers, and cell phones. There was little research on physical activity variability, but there are methods to assess biological signals in other fields such as heart rate, muscle strength, and others. The Poincaré model lets us evaluate and visualize physical activity variability. We discovered a significant correlation between activity intensity variability and weight, but further research with bigger samples and different time intervals should be done. Furthermore, there are other models to evaluate variability, such as a change of coefficient of variant, attractors, two-stage modeling, and data processing with ensemble clustering binning, but the best way is still to conduct future research.
To use these methods further, we need to test, adapt, and improve every possible data processing method and make it accessible to health specialists for practical purposes and further clinical research.
4.2. Limitations
Our study has limitations. First, it was conducted with a small sample of patients with no control group, and therefore, these approaches should be tested in other settings. Second, it was run over six months, and more extended studies are needed to determine if these shorter-term changes in body weight lead to longer-term changes in preventing diabetes.
Because of the new strict general data protection regulations in Lithuania, we could not remotely collect patient data for our study. We also could not collect data in between the first and the last visits, because of the strict patient movement restrictions due to the spread of the COVID-19 infection. Therefore, it was not possible to collect data on the actual wear time.
5. Conclusions
Data from Fitbit activity trackers create an excellent opportunity to evaluate physical activity for patients at an increased risk of T2D. When assessing physical activity data, doctors should evaluate not just the totals or the medians of the steps count but also physical activity variability in time. The study shows that body fat composition, weight, and total cholesterol may be better linked to the physical activity variability than the total count of physical activity during the research period.
Abbreviations
| AFE | Area of fitting ellipse |
| AVG | Average value |
| AT | Activity tracker |
| BMI | Body mass index |
| DPP | Diabetes prevention program |
| IFG | Impaired fasting glucose |
| IGT | Impaired glucose tolerance |
| PBF | Percent body fat |
| VFL | Visceral fat level |
| VFA | Visceral fat area |
| WHR | Waist to hip ratio |
| AC | Abdominal circumference |
| MBF | Mass of body fat |
| PA | Physical activity |
| SD | Standard deviation |
| SD1 | Short-term variability |
| SD2 | Long-term variability |
| SD12 | The ratio of SD1 and SD2 |
| T2D | Type 2 diabetes |
Author Contributions
Conceptualization, A.B., V.K. and K.S.; methodology A.B., V.K., R.P. and K.S.; validation, A.B., V.K. and K.S.; formal analysis, A.B. and R.P.; investigation, A.B.; resources, A.B.; data curation, A.B. and R.P.; writing—original draft preparation, A.B. and K.S.; writing—review and editing, V.K.; visualization, A.B. and R.P.; supervision, V.K.; project administration, A.B.; funding acquisition, A.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was approved by the Vilnius Regional Biomedical Research Ethics Committee (approval no. 2019/6-1143-634).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
None declared. Fitbit was not involved in the design, implementation, data analysis, or manuscript preparation of the study.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sun H., Saeedi P., Karuranga S., Pinkepank M., Ogurtsova K., Duncan B.B., Stein C., Basit A., Chan J.C.N., Mbanya J.C., et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. [(accessed on 13 February 2022)];Diabetes Res. Clin. Pract. 2022 183:109119. doi: 10.1016/j.diabres.2021.109119. Available online: https://www.research.ed.ac.uk/en/publications/idf-diabetes-atlas-global-regional-and-country-level-diabetes-pre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heianza Y., Hara S., Arase Y., Saito K., Fujiwara K., Tsuji H., Kodama S., Hsieh S.D., Mori Y., Shimano H., et al. HbA1c 5.7–6.4% and impaired fasting plasma glucose for diagnosis of prediabetes and risk of progression to diabetes in Japan (TOPICS 3): A longitudinal cohort study. [(accessed on 13 February 2022)];Lancet. 2011 378:147–155. doi: 10.1016/S0140-6736(11)60472-8. Available online: https://pubmed.ncbi.nlm.nih.gov/21705064/ [DOI] [PubMed] [Google Scholar]
- 3.Richter B., Hemmingsen B., Metzendorf M.I., Takwoingi Y. Development of type 2 diabetes mellitus in people with intermediate hyperglycaemia. [(accessed on 13 February 2022)];Cochrane Database Syst. Rev. 2018 10:CD012661. doi: 10.1002/14651858.CD012661.pub2. Available online: https://pubmed.ncbi.nlm.nih.gov/30371961/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tabák A.G., Herder C., Rathmann W., Brunner E.J., Kivimäki M. Prediabetes: A high-risk state for diabetes development. [(accessed on 13 February 2022)];Lancet. 2012 379:2279–2290. doi: 10.1016/S0140-6736(12)60283-9. Available online: https://pubmed.ncbi.nlm.nih.gov/22683128/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang Y., Cai X., Mai W., Li M., Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: Systematic review and meta-analysis. [(accessed on 13 February 2022)];BMJ. 2016 355:i5953. doi: 10.1136/bmj.i5953. Available online: https://pubmed.ncbi.nlm.nih.gov/27881363/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeboah J., Bertoni A.G., Herrington D.M., Post W.S., Burke G.L. Impaired Fasting Glucose and the Risk of Incident Diabetes Mellitus and Cardiovascular Events in an Adult Population: The Multi-Ethnic Study of Atherosclerosis. [(accessed on 13 February 2022)];J. Am. Coll. Cardiol. 2011 58:140–146. doi: 10.1016/j.jacc.2011.03.025. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3146297/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Risk C., Ford E.S., Zhao G., Li C. Quarterly Focus Issue: Prevention/Outcomes Pre-Diabetes and the Risk for Cardiovascular Disease A Systematic Review of the Evidence. J. Am. Coll. Cardiol. 2010;55:1310–1317. doi: 10.1016/j.jacc.2009.10.060. [DOI] [PubMed] [Google Scholar]
- 8.Diabetes Prevention Program Research Group. Knowler W.C., Fowler S.E., Hamman R.F., Christophi C.A., Hoffman H.J., Brenneman A.T., Brown-Friday J.O., Goldberg R., Venditti E., et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. [(accessed on 13 February 2022)];Lancet. 2009 374:1677–1686. doi: 10.1016/S0140-6736(09)61457-4. Available online: https://pubmed.ncbi.nlm.nih.gov/19878986/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iabetes D., Revention P., Rogram P., Esearch R., Roup G. Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. [(accessed on 13 February 2022)];N. Engl. J. Med. 2002 346:393–403. doi: 10.1056/NEJMoa012512. Available online: https://www.nejm.org/doi/full/10.1056/nejmoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindström J., Ilanne-Parikka P., Peltonen M., Aunola S., Eriksson J.G., Hemiö K., Hämäläinen H., Härkönen P., Keinänen-Kiukaanniemi S., Laakso M., et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: Follow-up of the Finnish Diabetes Prevention Study. [(accessed on 13 February 2022)];Lancet. 2006 368:1673–1679. doi: 10.1016/S0140-6736(06)69701-8. Available online: https://pubmed.ncbi.nlm.nih.gov/17098085/ [DOI] [PubMed] [Google Scholar]
- 11.Li G., Zhang P., Wang J., An Y., Gong Q., Gregg E.W., Yang W., Zhang B., Shuai Y., Hong J., et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: A 23-year follow-up study. [(accessed on 13 February 2022)];Lancet Diabetes Endocrinol. 2014 2:474–480. doi: 10.1016/S2213-8587(14)70057-9. Available online: https://pubmed.ncbi.nlm.nih.gov/24731674/ [DOI] [PubMed] [Google Scholar]
- 12.Nathan D.M., Bennett P.H., Crandall J.P., Edelstein S.L., Goldberg R.B., Kahn S.E., Knowler W.C., Mather K.J., Mudaliar S., Orchard T.J., et al. Does diabetes prevention translate into reduced long-term vascular complications of diabetes? [(accessed on 13 February 2022)];Diabetologia. 2019 62:1319–1328. doi: 10.1007/s00125-019-4928-8. Available online: https://pubmed.ncbi.nlm.nih.gov/31270584/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strath S.J., Kaminsky L.A., Ainsworth B.E., Ekelund U., Freedson P.S., Gary R.A., Richardson C.R., Smith D.T., Swartz A.M., American Heart Association Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health and Cardiovascular, Exercise, Cardiac Rehabilitation and Prevention Committee of the Council on Clinical Cardiology, and Council Guide to the assessment of physical activity: Clinical and research applications: A scientific statement from the American Heart association. [(accessed on 2 February 2022)];Circulation. 2013 128:2259–2279. doi: 10.1161/01.cir.0000435708.67487.da. Available online: https://www.ahajournals.org/doi/abs/10.1161/01.cir.0000435708.67487.da. [DOI] [PubMed] [Google Scholar]
- 14.Bassett D.R., Toth L.P., LaMunion S.R., Crouter S.E. Step Counting: A Review of Measurement Considerations and Health-Related Applications. [(accessed on 2 February 2022)];Sports Med. 2017 47:1303–1315. doi: 10.1007/s40279-016-0663-1. Available online: https://link.springer.com/article/10.1007/s40279-016-0663-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brickwood K.J., Watson G., O’brien J., Williams A.D. Consumer-Based Wearable Activity Trackers Increase Physical Activity Participation: Systematic Review and Meta-Analysis. [(accessed on 2 February 2022)];JMIR Mhealth Uhealth. 2019 7:e11819. doi: 10.2196/11819. Available online: https://mhealth.jmir.org/2019/4/e11819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Straiton N., Alharbi M., Bauman A., Neubeck L., Gullick J., Bhindi R., Gallagher R. The validity and reliability of consumer-grade activity trackers in older, community-dwelling adults: A systematic review. Maturitas. 2018;112:85–93. doi: 10.1016/j.maturitas.2018.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Evenson K.R., Goto M.M., Furberg R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. [(accessed on 2 February 2022)];Int. J. Behav. Nutr. Phys. Act. 2015 12:159. doi: 10.1186/s12966-015-0314-1. Available online: https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-015-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sergamumas. [(accessed on 2 February 2022)]. Available online: https://hi.lt/php/serg14.php?dat_file=serg14.txt.
- 19.Tang M.S.S., Moore K., McGavigan A., Clark R.A., Ganesan A.N. Effectiveness of Wearable Trackers on Physical Activity in Healthy Adults: Systematic Review and Meta-Analysis of Randomized Controlled Trials. [(accessed on 30 March 2022)];JMIR Mhealth Uhealth. 2020 8:e15576. doi: 10.2196/15576. Available online: https://mhealth.jmir.org/2020/7/e15576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yun I., Joo H.J., Park Y.S., Park E.C. Association between Physical Exercise and Glycated Hemoglobin Levels in Korean Patients Diagnosed with Diabetes. [(accessed on 30 March 2022)];Int. J. Environ. Res. Public Health. 2022 19:3280. doi: 10.3390/ijerph19063280. Available online: https://www.mdpi.com/1660-4601/19/6/3280/htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Franssen W.M.A., Franssen G.H.L.M., Spaas J., Solmi F., Eijnde B.O. Can consumer wearable activity tracker-based interventions improve physical activity and cardiometabolic health in patients with chronic diseases? A systematic review and meta-analysis of randomised controlled trials. [(accessed on 30 March 2022)];Int. J. Behav. Nutr. Phys. Act. 2020 17:57. doi: 10.1186/s12966-020-00955-2. Available online: https://link.springer.com/articles/10.1186/s12966-020-00955-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan A., Chan D., Lee H., Ng C.C., Yeo A.H.L. Reporting adherence, validity and physical activity measures of wearable activity trackers in medical research: A systematic review. Int. J. Med. Inform. 2022;160:104696. doi: 10.1016/j.ijmedinf.2022.104696. [DOI] [PubMed] [Google Scholar]
- 23.American Diabetes Association 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. [(accessed on 22 March 2022)];Diabetes Care. 2021 44((Suppl. S1)):S15–S33. doi: 10.2337/dc21-S002. Available online: https://diabetesjournals.org/care/article/44/Supplement_1/S15/30859/2-Classification-and-Diagnosis-of-Diabetes. [DOI] [PubMed] [Google Scholar]
- 24.Feehan L.M., Geldman J., Sayre E.C., Park C., Ezzat A.M., Yoo J.Y., Hamilton C.B., Li L.C. Accuracy of Fitbit Devices: Systematic Review and Narrative Syntheses of Quantitative Data. [(accessed on 20 June 2022)];JMIR Mhealth Uhealth. 2018 6:e10527. doi: 10.2196/10527. Available online: https://mhealth.jmir.org/2018/8/e10527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El Fatouhi D., Delrieu L., Goetzinger C., Malisoux L., Affret A., Campo D., Fagherazzi G. Associations of Physical Activity Level and Variability with 6-Month Weight Change Among 26,935 Users of Connected Devices: Observational Real-Life Study. [(accessed on 2 February 2022)];JMIR Mhealth Uhealth. 2021 9:e25385. doi: 10.2196/25385. Available online: https://mhealth.jmir.org/2021/4/e25385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tudor-Locke C., Craig C.L., Brown W.J., Clemes S.A., de Cocker K., Giles-Corti B., Hatano Y., Inoue S., Matsudo S.M., Mutrie N., et al. How many steps/day are enough? For adults. [(accessed on 1 February 2022)];Int. J. Behav. Nutr. Phys. Act. 2011 8:79. doi: 10.1186/1479-5868-8-79. Available online: https://pubmed.ncbi.nlm.nih.gov/21798015/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Golińska A.K. Poincaré plots in analysis of selected biomedical signals. Stud. Log. Gramm. Rhetor. 2013;35:117–127. doi: 10.2478/slgr-2013-0031. [DOI] [Google Scholar]
- 28.Satti R., Abid N.U.H., Bottaro M., de Rui M., Garrido M., Rauofy M.R., Montagnese S., Mani A.R. The application of the extended Poincaré plot in the analysis of physiological variabilities. Front. Physiol. 2019;10:116. doi: 10.3389/fphys.2019.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jamovi-Stats. Open. Now. [(accessed on 2 February 2022)]. Available online: https://www.jamovi.org/
- 30.R: The R Project for Statistical Computing. [(accessed on 2 February 2022)]. Available online: https://www.r-project.org/
- 31.CRAN-Package RHRV. [(accessed on 2 February 2022)]. Available online: https://cran.r-project.org/web/packages/RHRV/index.html.
- 32.García Martínez C.A., Otero Quintana A., Vila X.A., Lado Touriño M.J., Rodríguez-Liñares L., Rodríguez Presedo J.M., Méndez PenÍn A.J. Heart Rate Variability Analysis of ECG Data [R package RHRV Version 4.2.6] [(accessed on 2 February 2022)]. Available online: https://CRAN.R-project.org/package=RHRV.
- 33.Ringeval M., Wagner G., Denford J., Paré G., Kitsiou S. Fitbit-Based Interventions for Healthy Lifestyle Outcomes: Systematic Review and Meta-Analysis. [(accessed on 13 February 2022)];J. Med. Internet Res. 2020 22:e23954. doi: 10.2196/23954. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7589007/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.da Silva B.G.C., da Silva I.C.M., Ekelund U., Brage S., Ong K.K., de Lucia Rolfe E., Lima N.P., da Silva S.G., de França G.V.A., Horta B.L. Associations of physical activity and sedentary time with body composition in Brazilian young adults. [(accessed on 21 June 2022)];Sci. Rep. 2019 9:5444. doi: 10.1038/s41598-019-41935-2. Available online: https://www.nature.com/articles/s41598-019-41935-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carnero E.A., Dubis G.S., Hames K.C., Jakicic J.M., Houmard J.A., Coen P.M., Goodpaster B.H. Randomized Trial Reveals that Physical Activity and Energy Expenditure are associated with Weight and Body Composition after RYGB. [(accessed on 21 June 2022)];Obesity. 2017 25:1206. doi: 10.1002/oby.21864. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513190/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.