These findings identify circumstances in the occupational settings of healthcare workers most associated with increased odds of adverse mental health outcomes. These may provide specific targets for potential modifications in these settings to reduce the risks to the mental health of these providers during a pandemic.
Keywords: health care workers, COVID-19: mental health, occupational exposure, presenteeism
Abstract
Objective
The aim of this study was to assess occupational circumstances associated with adverse mental health among health care workers during the COVID-19 pandemic.
Methods
A cross-sectional study examined responses to an on-line survey conducted among 2076 licensed health care workers during the first pandemic peak. Mental health (depression, anxiety, stress, and anger) was examined as a multivariate outcome for association with COVID-related occupational experiences.
Results
Odds of negative mental health were increased among those who worked directly with patients while sick themselves (adjusted odds ratio, 2.29; 95% confidence interval, 1.71–3.08) and were independently associated with working more hours than usual in the past 2 weeks, having family/friends who died due to COVID-19, having COVID-19 symptoms, and facing insufficiencies in personal protective equipment/other shortages.
Conclusions
Occupational circumstances were associated with adverse mental health outcomes among health care workers during the COVID-19 pandemic, and some are potentially modifiable.
In Spring 2020, an early epicenter of the 2019 coronavirus disease (COVID-19) pandemic in and around New York City (NYC) created an unprecedented strain on health care resources. After the first laboratory-confirmed case on February 29, case counts in NYC increased exponentially during the month of March, with a case fatality rate of 32% among hospitalized patients, and over 18,000 deaths occurring before June,1 by which point almost 6000 additional deaths had accrued in the rest of the state.2 Frontline health care workers faced shortages of personal protective equipment (PPE), ventilators, personnel, and even beds.3,4 Work conditions for the selected health care providers within this context included redeployment to understaffed facilities or departments other than those they typically served, and extra hours or shifts.4 Conversely, other health care practitioners saw their hours reduced or practices closed, as social distancing and stay-at-home orders led to a drastic reduction in the utilization of routine health care.5
The risks posed by this situation to the mental well-being of health care professionals were brought to the forefront by the April 2020 death by suicide of a prominent NYC emergency department physician.6 During the same month, a study of internal medicine residents from a single NYC hospital found that nearly one fourth had contemplated suicide or self-harm since the beginning of the pandemic.7 More broadly, a meta-analysis of 65 studies of health care workers in 21 countries indicated that depression and anxiety were widespread.8
Occupational circumstances are a potentially modifiable means through which to address the mental health of workers during a pandemic. Previous studies during epidemics or pandemics, for example, SARS, MERS, H1N1, have identified occupational factors associated with increased psychological distress among health care workers, including being in direct contact with, or treating, infected patients; being quarantined due to potential infection; having colleagues who were infected or died due to infection; long hours; and lack of appropriate training, inadequate PPE, or lack of support.9,10 A survey from a single NYC medical center reported that respondents endorsed facing distress due to a range of experiences, including redeployment, involvement in triage decisions, working with COVID-19 patients, patient deaths, working while symptomatic, clinical hours, the health of family/friends, and a lack of PPE.11 However, they did not test which of these exposures were associated with adverse mental health outcomes, after adjusting for participant characteristics, and did not include providers from across the state. Such information may be critical for identifying key modifiable circumstances to address to protect health care providers’ mental health. Therefore, in a sample drawn from all licensed physicians, physician assistants, and nurse practitioners in New York State (NYS), we examined the association of work-related experiences with mental health outcomes early during the COVID-19 pandemic. While we examined multiple, specific measures of mental health, our overarching concern was to understand the conditions that may negatively impact mental health in several domains as opposed to specifically identifying risk factors for individual disorders.
METHODS
Study Population
The COVID-19 Healthcare Personnel Study is an on-line survey conducted to assess the adverse health impacts of the COVID-19 pandemic on NYS health professionals and has been previously described.12 Briefly, all 139,109 physicians, nurse practitioners, and physician assistants licensed to practice in NYS were invited to participate in the survey by an e-mail from the NYS Commissioner of Health. The survey was open to responses between April 28 and June 30, 2020, in the immediate weeks after the pandemic crested in NYS. The survey was administered through REDCap, a secure Web application. Analyses describe the responses of n = 2076 participants (1.5% response rate). Relative to the sampling base, participants were more likely to be female (48% vs 34%), were more likely to be aged 60 years or older (32% vs 23%), and showed some minor geographical differences.13 The study was approved by the institutional review boards of the participating institutions, and a waiver of documentation of informed consent was obtained. Informed consent was obtained electronically from all participants before gaining access to the on-line survey.
Measures
Mental Health
Mental health was assessed using four dichotomous outcomes: probable depression, probable anxiety (henceforth, “depression” and “anxiety”), stress, and anger. Depression was assessed with the two depression items (Patient Health Questionnaire 2: feeling down, depressed, or hopeless; and having had little interest or pleasure in doing things that you usually enjoy) in the Patient Health Questionnaire 9, scored by participants on a 0–3 scale (not at all, several days, more than half the days, nearly every day). Participants were considered positive for depression if the sum of their responses to these two items was greater than or equal to 3.14,15 Anxiety was assessed with the two anxiety screening items (Generalized Anxiety Disorder 2: feeling nervous, anxious, or on edge; and not being able to stop or control worrying thoughts) from the Generalized Anxiety Disorder 7, scored on the same 0–3 scale. Participants were considered positive for anxiety if the sum of their responses to these two items was greater than or equal to 3.16 Stress and anger were each assessed on a 1 to 10 scale (1 = not at all, 10 = extremely often) based on the questions of how frequently they experience these emotions because of COVID-19. The scales were dichotomized for analysis with scores of 8, 9, or 10 coded as present.
COVID-Related Occupational Experiences
COVID-related occupational experiences were assessed based on participant responses and categorized as shown in Table 1. Participants reported whether they had redeployed to a different location or changed their functions within the same practice location since March 1, 2020, the number of hours that they had worked in the past 2 weeks (absolute work duration), and whether this was the same, less, or more than the they usually worked (relative work duration). Given the correlation between measures, relative work duration was used in the primary analyses. They additionally reported whether they had been involved in a life-or-death triage/prioritizing decision related to a COVID-19 patient; any family member or friend had died from COVID-19; whether, since March 1, 2020, any COVID-19 patients died in the facility in which they worked; they had worked in close physical contact with COVID-19 patients; and if they had experienced symptoms consistent with COVID-19 infection (fever, persistent cough, persistent sore throat, headache).
TABLE 1.
Characteristics and COVID-19 Pandemic-Related Occupational Experiences of New York State Health Care Workers Between April 28 and June 30, 2020
| MD/DOa | NP/CNMWa | PAa | Totala,b | |||||
|---|---|---|---|---|---|---|---|---|
| % | (SE) | % | (SE) | % | (SE) | % | (SE) | |
| Profession | ||||||||
| MD/DO | — | — | — | — | — | — | 74.2 | (1.1) |
| NP/CNMW | — | — | — | — | — | — | 15.3 | (0.8) |
| PA | — | — | — | — | — | — | 10.4 | (0.9) |
| Female | 34.9 | (1.3) | 92.8 | (1.4) | 68.4 | (4.4) | 47.3 | (1.2) |
| Age | ||||||||
| <40 | 19.5 | (1.1) | 25.8 | (2.3) | 20.6 | (2.6) | 20.5 | (1.0) |
| 40–59 | 55.7 | (1.5) | 48.4 | (2.7) | 72.5 | (3.2) | 56.4 | (1.2) |
| ≥60 | 24.9 | (1.2) | 25.9 | (2.5) | 6.9 | (1.8) | 23.1 | (1.0) |
| NYC metro usualc | 72.3 | (1.2) | 57.4 | (2.5) | 60.4 | (4.2) | 68.8 | (1.1) |
| Specialty | ||||||||
| Primary care | 29.1 | (1.3) | 38 | (2.5) | 26.4 | (3.8) | 30.2 | (1.1) |
| Pediatrics | 16.4 | (1.1) | 12 | (1.7) | 6 | (2.3) | 14.7 | (0.9) |
| Emergency | 9 | (0.9) | 3.1 | (0.9) | 16 | (3.3) | 8.8 | (0.7) |
| Critical care | 7.8 | (0.8) | 3.7 | (1.0) | 3.1 | (1.8) | 6.7 | (0.7) |
| Non-surgical specialties | 19 | (1.2) | 25.6 | (2.3) | 17.9 | (3.4) | 19.9 | (1.0) |
| Surgery | 12.2 | (1.0) | 7.9 | (1.4) | 26 | (4.1) | 13 | (0.9) |
| Behavioral | 6 | (0.7) | 8.9 | (1.6) | 3 | (1.5) | 6.1 | (0.6) |
| Other | 0.5 | (0.2) | 0.6 | (0.4) | 1.6 | (1.5) | 0.7 | (0.2) |
| Has children younger than 18 yrs | 44.4 | (1.5) | 39.8 | (2.5) | 52.8 | (4.5) | 44.6 | (1.3) |
| Answered survey anonymously | 33.7 | (1.4) | 27.2 | (2.3) | 22 | (3.4) | 31.5 | (1.2) |
| Redeployment/function change | ||||||||
| None | 60.1 | (1.5) | 56.3 | (2.6) | 65.7 | (4.2) | 60.1 | (1.2) |
| Same location, changed function | 23.5 | (1.3) | 24.5 | (2.3) | 19.8 | (3.6) | 23.3 | (1.1) |
| Redeployed | 16.4 | (1.1) | 19.3 | (2.0) | 14.5 | (3.0) | 16.6 | (0.9) |
| Hours worked in past 2 wks, change | ||||||||
| Less | 34.8 | (1.4) | 52.3 | (2.6) | 54.2 | (4.5) | 39.5 | (1.2) |
| Same as usual | 43.7 | (1.5) | 29.4 | (2.4) | 29.4 | (4.1) | 40 | (1.2) |
| More | 21.6 | (1.2) | 18.4 | (2.1) | 16.4 | (3.4) | 20.5 | (1.0) |
| Work hours, past 2 wks | ||||||||
| None | 4.6 | (0.6) | 5.4 | (1.2) | 7.7 | (2.6) | 5.1 | (0.5) |
| 1–40 | 21.5 | (1.2) | 15.4 | (2.0) | 10.2 | (2.5) | 19.4 | (1.0) |
| 41–80 | 42.6 | (1.5) | 59 | (2.6) | 55.1 | (4.5) | 46.4 | (1.3) |
| 81–100 | 16.5 | (1.1) | 15.1 | (1.9) | 21.1 | (3.8) | 16.7 | (1.0) |
| 101–280 | 14.8 | (1.1) | 5 | (1.2) | 6 | (2.5) | 12.4 | (0.9) |
| Worked with COVID-19 patients | 52 | (1.5) | 43.5 | (2.6) | 59.6 | (4.4) | 51.5 | (1.3) |
| Has family/friends who died | 20.9 | (1.2) | 22.5 | (2.3) | 19.3 | (3.6) | 21 | (1.0) |
| COVID-19 symptoms | 27.6 | (1.3) | 37.9 | (2.5) | 37.8 | (4.5) | 30.3 | (1.2) |
| Patients died | 61.2 | (1.4) | 48.3 | (2.6) | 54 | (4.5) | 58.4 | (1.2) |
| Involved in triage decisions | 13.7 | (1.1) | 8.3 | (1.5) | 6.8 | (2.2) | 12.1 | (0.9) |
| PPE shortages | 55.1 | (1.5) | 57.2 | (2.6) | 65.4 | (4.2) | 56.5 | (1.2) |
| Other shortages | 37 | (1.4) | 31.6 | (2.4) | 37.3 | (4.4) | 36.2 | (1.2) |
aWeighted percentages.
bInformation was missing for variables for the following numbers of observations: sex, n = 19; age, n = 113; NYC metro area, n = 36; specialty, n = 9; children <18, n = 3; redeployment or change in function, n = 52; change in hours worked, n = 6; number of hours worked, n = 43; worked with COVID-19 patients, n = 7; family/friends died, n = 5; COVID-19 symptoms, n = 31; patients died, n = 20; involved in triage decisions, n = 15.
cUsual practice location in New York City, Long Island, Westchester, or Rockland Counties.
Participants were classified as experiencing PPE shortages if they responded affirmatively to questions about whether in the last week they experienced a shortage of N95 masks, had to personally use makeshift PPE, or had to reuse disposable PPE in a manner which seemed unsafe. They were classified as experiencing other shortages if they responded affirmatively to having had, in the last week, shortages of test kits, ventilators, beds, or personnel.
Participant Characteristics
Sex, age, usual practice location, profession, specialty, and whether or not they had children younger than 18 years were reported by the participants and categorized as shown in Table 1. Participants were classified as answering the survey anonymously if they chose not to provide contact information for follow-up.
Statistical Analysis
All analyses incorporated previously defined survey weights12 to make the results more representative of the target population of physicians, nurse practitioners, and medical assistants in NYS. Frequencies of participant characteristics and their COVID-related occupational experiences were tabulated, and the prevalence of each mental health outcome was examined by these characteristics and experiences.
To examine the association of characteristics and experiences with adverse mental health, we treated the four dichotomous mental health variables as a multivariate outcome with four observations (one for each outcome) per participant. Generalized estimating equations with a logit link and robust variance estimates accounted for the correlation between outcomes within individuals, and the predictors included an indicator for the specific type of mental health outcome. Thus, the exponentiated coefficients from the models can be interpreted as odds ratios for adverse mental health generally, accounting for the correlation between specific mental health outcomes within participants. We fitted a series of models as follows: (1) unadjusted associations with each participant characteristic and COVID-related occupational experience; (2) association of each COVID-related occupational experience, adjusted for the personal characteristics, which were also associated with the outcome (P < 0.1); and (3) to examine the independent association of COVID-related occupational experiences with adverse mental health, another model included all occupational experiences associated with the outcome (P < 0.1) under step 2 and personal characteristics. Missing data were addressed using listwise deletion, with n = 1866 participants (90% of total) contributing to the fully adjusted model,3 and by multiple imputation.
Sensitivity Analyses
Additional analyses were conducted as follows. To test sensitivity to the definition of work duration, absolute rather than relative work duration was substituted into the adjusted model. To address potential temporal variation, an analysis was limited to 1748 participants responding within the first 72 hours after the initial invitation. To further address missing data, the fully adjusted model was re-fit and estimates pooled from 10 imputations using multiple imputation by chained equations with augmented regression and including all independent and dependent variables in the imputation model. To further assess aspects related to experiencing COVID-19 symptoms, which may have been related to mental health, we re-fit the adjusted model using a 4-level variable related to the concept of “presenteeism,” that is, working “despite complaints and ill health that should prompt rest and absence from work.”17 Indicators for no symptoms, experienced symptoms but did not work, worked while sick but not in direct patient care, or worked while sick in direct patient care, were used in place of the dichotomous variable for COVID-19 symptoms. To examine whether the observed association with “other” shortages was related to specific factors, the dichotomous term for other shortages was replaced with dichotomous terms for each of the 4 specific types of other shortages.
To test for heterogeneity by mental health outcome for each COVID-related occupational experience, experience × outcome type product terms were added to the adjusted model separately for each experience variable, and heterogeneity was then evaluated based on a test of the joint hypotheses that all interaction terms were equal to 0. When this joint hypothesis test indicated statistically significant evidence for heterogeneity (P < 0.05), mental health outcome–specific adjusted odds ratios (aORs) and 95% confidence intervals (CIs) were calculated from the models including product terms.
All analyses used Stata 16.0 (StataCorp LLC, College Station, TX).
RESULTS
Population Characteristics
Characteristics and distribution of the COVID-19 pandemic-related occupational experiences of the study population, overall and by profession, are shown in Table 1 and Table, Supplemental Digital Content 1, http://links.lww.com/JOM/B86. Just under half were female, the majority between the ages of 40 and 59 years, and two thirds had their usual practice location in the NYC metropolitan area. Approximately three quarters were physicians (MD or DO), with primary care (30.2%), non-surgical specialties (19.9%), and pediatrics (14.7%) representing the most prevalent specialties. Forty-five percent reported having children younger than 18 years, and 32% answered the survey anonymously.
Regarding occupational experiences, 40% were redeployed or had a change of function. Reporting both increases (20.5%) and decreases (39.5%) in the number of hours worked in the past 2 weeks was common. Approximately half had worked with COVID-19 patients, and nearly one third (30.3%) had experienced symptoms themselves. One fifth reported that family or friends had died of COVID-19, and over one half were affected by PPE shortages.
Overall, the prevalence of negative mental health was presented as follows: depression, 13.4%; anxiety, 26.5%; stress, 29.3%; and anger, 7.7%. The counts and stratum-specific prevalence of each mental health outcome by pandemic-related occupational exposures are shown in Tables (Supplemental Digital Content 2, http://links.lww.com/JOM/B87 and Supplemental Digital Content 3, http://links.lww.com/JOM/B88).
Relationship of Participant Characteristics to Negative Mental Health
The unadjusted associations between participant characteristics and odds of negative mental health are shown in Table 2. Odds of negative mental health were higher among females than males, among younger versus older health care professionals, among those with usual practice locations in the NYC metropolitan area, among physician assistants and nurse practitioners/certified nurse midwives versus physicians, and among those specializing in critical care versus those in primary care. Having children younger than 18 years or answering the survey anonymously was not associated with the odds of negative mental health.
TABLE 2.
Prevalence of Anxiety, Depression, Anger, and Stress, and Crude Odds Ratios (ORs) and 95% Confidence Intervals (CIs) of Negative Mental Health According to Participant Characteristics Among New York State Health Care Workers Between April 28 and June 30, 2020
| Characteristic | Anxietya | Depressiona | Angera | Stressa | OR | 95% CI | P | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | SE | % | SE | % | SE | % | SE | |||||
| Female | 30.6 | [1.5] | 15.1 | [1.2] | 9.9 | [1.0] | 34.2 | [1.5] | 1.52 | (1.26, 1.85) | <0.001 | |
| Male | 22.4 | [1.6] | 12.1 | [1.3] | 5.8 | [0.90] | 24.6 | [1.7] | 1 | Ref | — | |
| Age category | ||||||||||||
| <40 | 34.1 | [2.4] | 15 | [1.7] | 10.1 | [1.5] | 36.8 | [2.4] | 1.28 | (1.03, 1.60) | 0.03 | |
| 40–59 | 26.8 | [1.7] | 14.6 | [1.4] | 7.5 | [1.0] | 31.5 | [1.7] | 1 | Ref | — | |
| ≥60 | 20 | [1.9] | 10.2 | [1.4] | 5.9 | [1.1] | 18.7 | [1.8] | 0.59 | (0.46, 0.75) | <0.001 | |
| NYC metro usual | ||||||||||||
| Yes | 28.8 | [1.5] | 14 | [1.1] | 7.9 | [0.9] | 30.3 | [1.5] | 1.28 | (1.05, 1.55) | 0.01 | |
| No | 21.7 | [1.6] | 11.7 | [1.3] | 6.5 | [1.0] | 27.4 | [1.8] | 1 | Ref | — | |
| Profession | ||||||||||||
| MD, DO | 24.6 | [1.3] | 11.6 | [0.9] | 6.8 | [0.7] | 26.3 | [1.3] | 1 | Ref | — | |
| NP, CNMW | 33 | [2.4] | 16.8 | [1.9] | 10.1 | [1.6] | 34.8 | [2.5] | 1.51 | (1.22, 1.86) | <0.001 | |
| PA | 30.4 | [4.2] | 21.3 | [4.0] | 10.4 | [2.8] | 42.1 | [4.5] | 1.73 | (1.22, 2.45) | 0.002 | |
| Specialty | ||||||||||||
| Primary care | 25.9 | [2.0] | 11.2 | [1.4] | 7 | [1.1] | 27.8 | [2.0] | 1 | Ref | — | |
| Pediatrics | 28.3 | [2.9] | 11 | [1.9] | 4.6 | [1.3] | 32.8 | [3.0] | 1.16 | (0.88, 1.54) | 0.30 | |
| Emergency | 24 | [3.7] | 13.3 | [3.0] | 11.1 | [3.0] | 29.1 | [4.0] | 1.03 | (0.70, 1.50) | 0.89 | |
| Critical Care | 35.9 | [4.9] | 20.8 | [4.2] | 14.5 | [4.0] | 39.9 | [5.0] | 1.74 | (1.17, 2.57) | 0.01 | |
| Non-surgical specialties | 27.6 | [2.5] | 14.8 | [2.0] | 6.8 | [1.3] | 30.1 | [2.6] | 1.14 | (0.87, 1.48) | 0.35 | |
| Surgery | 26.9 | [3.3] | 18.7 | [3.0] | 9.9 | [2.3] | 29.8 | [3.4] | 1.17 | (0.84, 1.63) | 0.35 | |
| Behavioral | 18.4 | [3.7] | 8.8 | [2.8] | 4.8 | [2.0] | 16.2 | [3.5] | 0.59 | (0.39, 0.89) | 0.01 | |
| Other | 0 | [0.0] | 0 | [0.0] | 6.7 | [6.6] | 5.7 | [5.7] | 0.06 | (0, 1.16) | 0.06 | |
| Has children younger than 18 yrs | ||||||||||||
| Yes | 27.4 | [1.8] | 13.3 | [1.3] | 7.4 | [1.0] | 32.5 | [1.9] | 1.17 | (0.97, 1.42) | 0.1 | |
| No | 25.8 | [1.4] | 13.5 | [1.2] | 7.9 | [0.9] | 26.6 | [1.4] | 1 | Ref | — | |
| Answered survey anonymously | ||||||||||||
| Yes | 25.8 | [2.0] | 13.8 | [1.6] | 7.5 | [1.2] | 30.1 | [2.1] | 1.01 | (0.83, 1.24) | 0.91 | |
| No | 26.8 | [1.3] | 13.2 | [1.0] | 7.8 | [0.8] | 28.9 | [1.4] | 1 | Ref | — | |
aWeighted percentages.
Association of COVID-19 Pandemic Occupational-Related Exposures With Negative Mental Health
The unadjusted and covariate adjusted associations between COVID-19 pandemic-related occupational experiences and negative mental health are shown in Table 3. Working in the same location but changing function and working with COVID-19 patients were each associated with increased odds of negative mental health in unadjusted models, but associations were no longer statistically significant after adjustment for participant characteristics. Involvement in triage decisions was associated with increased odds of negative mental health after adjustment for participant characteristics, but not after adjustment for other pandemic-related occupational experiences. Adjusting for participant characteristics and other pandemic-related occupational experiences, the odds of negative mental health outcomes was significantly increased among those who reported working more hours than usual in the past 2 weeks, who had family or friends who had died due to COVID-19, and who had COVID-19 symptoms, insufficient PPE, or who experienced other shortages. A model including the absolute rather than relative time worked over the past 2 weeks showed similar results for overwork (see Table, Supplemental Digital Content 4, http://links.lww.com/JOM/B89); restricting observations to responses received in the first 72 hours or addressing missing data with multiple imputation produced consistent findings (see Table, Supplemental Digital Content 5, http://links.lww.com/JOM/B90).
TABLE 3.
Unadjusted and Adjusted Associations of COVID-19 Pandemic Occupational-Related Experiences With Negative Mental Health Among New York State Health Care Workers Between April 28 and June 30, 2020
| Experience | Unadjusted | Adjusted for Participant Characteristicsa | Adjusted for Other Occupational Experiencesa,b | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| Redeployment/function change | |||||||||
| None | 1.00 | Ref | — | — | — | — | — | — | — |
| Same location, changed function | 1.35 | (1.08, 1.70) | 0.01 | 1.22 | (0.96, 1.56) | 0.10 | — | — | — |
| Redeployed | 1.13 | (0.87, 1.45) | 0.36 | 1.03 | (0.79, 1.35) | 0.82 | — | — | — |
| Hours worked in past 2 wks | |||||||||
| Less | 1.10 | (0.89, 1.37) | 0.38 | 1.06 | (0.85, 1.33) | 0.58 | 1.01 | (0.81, 1.27) | 0.92 |
| Same as usual | 1.00 | Ref | 1.00 | Ref | 1.00 | Ref | |||
| More | 1.65 | (1.29, 2.12) | <0.0001 | 1.58 | (1.21, 2.06) | 0.001 | 1.41 | (1.08, 1.85) | 0.01 |
| Worked with COVID-19 patients | 1.33 | (1.10, 1.61) | 0.003 | 1.18 | (0.95, 1.46) | 0.13 | — | — | — |
| Family or friends died | 1.37 | (1.09, 1.72) | 0.01 | 1.51 | (1.18, 1.92) | 0.001 | 1.43 | (1.12, 1.82) | 0.004 |
| COVID-19 symptoms | 1.97 | (1.62, 2.41) | <0.001 | 1.78 | (1.44, 2.19) | <0.001 | 1.64 | (1.33, 2.01) | <0.0001 |
| Patients died | 1.15 | (0.95, 1.40) | 0.15 | 1.07 | (0.86, 1.32) | 0.56 | — | — | — |
| Involved in triage decisions | 1.47 | (1.11, 1.96) | 0.01 | 1.36 | (1.00, 1.84) | 0.047 | 1.07 | (0.78, 1.47) | 0.66 |
| PPE shortages | 2.13 | (1.76, 2.58) | <0.001 | 2.04 | (1.67, 2.49) | <0.001 | 1.80 | (1.46, 2.21) | <0.0001 |
| Other shortages | 1.67 | (1.38, 2.03) | <0.001 | 1.62 | (1.33, 1.99) | <0.0001 | 1.31 | (1.06, 1.62) | 0.01 |
aAdjusted for sex, age, profession, specialty, and usual work location in the NYC metropolitan area.
bAlso adjusted for other experiences with estimates shown in the column.
Fifty percent of the population experienced symptoms, but did not work while sick, 15% worked while sick but not in direct patient care, and 35% worked in direct patient care while sick. Relative to not reporting symptoms, and after adjusting for participant characteristics and other pandemic-related occupational experiences, those presenteeism experiences were associated with odds ratios of negative mental health of the following: 1.28 (0.98–1.67), P = 0.07 for those with symptoms who did not work; 1.48 (0.99–2.22), P = 0.05 for those who worked while sick but not in direct patient care; and 2.29 (1.71–3.08), P < 0.001 for those who worked in direct patient care while sick, respectively (see Fig. 1).
FIGURE 1.
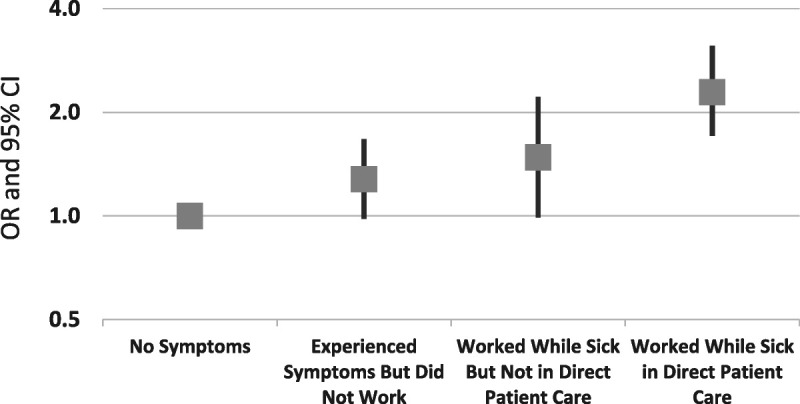
Adjusted odds ratios and 95% confidence intervals for the association between continued work in patient care while sick with COVID-19 symptoms and negative mental health, among New York State health care workers between April 28 and June 30, 2020. Estimates are adjusted for sex, age, profession, specialty, and usual work location in the NYC metropolitan area, relative number of hours worked in the past 2 weeks, having family/friends who died due to COVID-19, being involved in triage decisions, PPE shortages, and other shortages.
Adjusting for participant characteristics and other pandemic-related occupational exposures, negative mental health was increased among those who experienced shortages of personnel (aOR, 1.42; 95% CI, 1.10–1.85; P = 0.01), ventilators (aOR, 2.04; 95% CI, 1.05–3.96; P = 0.04), and beds (aOR, 2.20; 95% CI, 1.36–3.55; P = 0.001), but not test kits (aOR, 1.08; 95% CI, 0.85–1.38; P = 0.52).
Heterogeneity of Association Between Pandemic-Related Occupational Exposures and Negative Mental Health by Specific Mental Health Outcomes
There was evidence for statistically significant heterogeneity of associations for involvement in triage decision (P = 0.02, df = 3) and for other shortages (P = 0.04, df = 3) but not for the other tests of heterogeneity (P > 0.05). Mental health outcome–specific aORs and 95% CIs from these models are shown in Table, Supplemental Digital Content 6, http://links.lww.com/JOM/B91. As was the case for negative mental health overall, being involved in triage decisions was not significantly associated with any of the specific mental health outcomes in these adjusted models; other shortages were associated with significantly increased stress only.
DISCUSSION
In an on-line survey of licensed NYS health care providers during the first peak of the COVID-19 pandemic, we found that adverse mental health outcomes related to health care providers having COVID-19 symptoms were most pronounced among those who worked directly with patients while sick.
Several other circumstances that were independently associated with negative mental health outcomes could be classified as those that are modifiable by hospital policies and those that are not. The modifiable circumstances included increased recent work duration, shortages of PPE and other resources, as well as working with patients while sick. Those not modifiable in this way were loss of family or friends to the virus and health care workers experiencing COVID-19 symptoms themselves. We did not see strong evidence of heterogeneity in associations with respect to the specific mental health outcome.
Comparison to Other Findings
The personal characteristics associated with a higher risk of negative mental health—in particular, being female, younger, and a non-physician health care professional (nurse practitioner or physician assistant)—were in accord with the preponderance of findings from prior studies across a range of outbreaks, including COVID-19 internationally (reviewed in Sirois and Owens9). These studies also comport with our findings of risk associated with increased work hours, bereavement related to the virus, personal illness, and resource shortages.9,10 The role of working in patient care while experiencing symptoms oneself, on the other hand, has rarely been examined.
A limited number of other studies have specifically examined occupational factors related to the mental health of United States health care providers during the COVID-19 pandemic. Among faculty, staff, and fellows of a Midwestern university including clinical providers, exposure to COVID-19 and caring for patients with COVID-19 were risk factors for mental health outcomes.18 Caring for COVID-19 patients and lower PPE adequacy were associated with higher levels of self-reported stress at a separate Midwestern university.19 An on-line study of teaching hospitals in each of 4 US regions found that needing more social support was associated with significantly higher odds of probable psychiatric disorders in multivariable models, but that COVID-19 status, frontline status, change in roles, or change in hours is not.20 Among US health care providers who reported that they cared for COVID-19 patients in an intensive care unit during the initial US peak, emotional distress/burnout was most strongly associated with insufficient PPE access and was also related to personnel and respirator shortages, but not to shortages of intensive care unit beds.21 Finally, among those providing care to COVID-19 patients at a single NYC hospital, higher number of hours worked, lack of PPE, death or serious illness of coworker, and making difficult decisions in prioritizing patients were associated with increased symptoms of PTSD, depression, or generalized anxiety.22
The variation in the significance of specific factors associated with mental health outcomes across studies is likely impacted by differences in methods, including the exact combinations of exposures examined, and the covariates included in the models. However, contextual differences may also play a role, that is, equipment shortages may be more distressing when these shortages are more severe and sustained, and this differed by locale. Notably, the first wave surge in cases in NYC was particularly rapid and dramatic.1
Interpretation
Our findings suggest three specific areas associated with negative mental health impact on health care providers during a pandemic. First, the impact of personal exposure is demonstrated by the associations of mental health outcomes with participants’ own illness and with sickness and death of their family and friends. Second, the role of a breakdown of institutional protections is suggested by the associations of mental health outcomes with shortages of PPE and with working longer hours and/or while sick. Presenteeism has been associated with poorer self-rated and mental health.23 Highly prevalent among health care practitioners even before the pandemic, the reasons for presenteeism include a mix of systemic and sociocultural factors including difficulty finding coverage, concern about letting colleagues or patients down, and cultural expectations.24 However, to be clear, this study did not assess if sick health care workers were advised to stay home by their supervisors but chose to continue working, or if their continued working was an expectation.
Third, moral injury may be another element. Moral injury results from perpetrating or witnessing actions that violate one’s core beliefs and may involve a sense of betrayal by a trusted authority. Exposure to moral injury has been associated with increased risk of psychiatric symptoms.25,26 Although most studies have been related to military experiences,25,26 in the context of COVID, moral injury may result when, lacking sufficient material resources (ie, shortages of personnel and equipment) and with diminished personal reserves (ie, working for an increased duration and/or while ill), health care workers feel they are unable to adequately care for those for whom they are responsible.27 Moral injury during the COVID-19 pandemic has been previously documented in small samples of US health care workers.28 In this study, it may be an aspect of the findings that shortages of personnel and equipment, and caring directly for patients while sick themselves were related to mental health outcomes. Moral injury can be avoided or reduced by institutional policies and planning, but even when it cannot, treatment approaches may mitigate its effects on individual workers.
Strengths and Limitations
The strengths of this study include a large sample identified from a state-wide database of all licensed physicians, physician assistants, and nurse practitioners regardless of institution or practice setting; responses collected during the peak months of the first wave of the pandemic in NYS; availability of survey weights to make the findings more representative of the target population; use of validated screening instruments for depression and anxiety; and an analytic strategy to combine information across multiple mental health outcomes while accounting for their correlation within individuals.
Several limitations must be acknowledged. Although differential participation may potentially have biased results, the application of survey weights helped address the age, sex, and geographic distribution of respondents versus the target population. We were unable to address other factors that may have been associated with probability of participation. If people experiencing both mental health conditions and specific COVID-related occupational experiences were differentially more likely to participate, it may have biased our findings. However, because the survey covered a range of occupational and other factors related to the pandemic, it is unlikely that participation was driven by specific exposures. On the other hand, those more negatively impacted generally may have been more motivated to participate, therefore the prevalence of mental health conditions and COVID-related experiences may not generalize to the entire population. The study was cross-sectional, and we did not have information on preexisting mental health conditions. Therefore, reverse causation cannot be ruled out whereby professionals with underlying mental health concerns either differentially selected (eg, voluntarily changing work hours) or differentially reported their COVID-related occupational exposures. We did not have information about whether the outcomes were functionally impairing; further, stress and anger related to COVID-19 are not diagnoses. However, there was little significant heterogeneity of associations observed by the specific outcome. Finally, we had limited information on covariates, for example, race/ethnicity and income levels of participants. This may result in uncontrolled confounding; however, the concordance of key elements of our findings with those in other studies that have adjusted for these factors reduced the sway of that explanation.
Conclusions
In a sample drawn from all licensed physicians, nurse practitioners, and physician assistants in NYS during the first peak of the COVID-19 pandemic in the United States, personal exposure to infection with the virus, increased work duration, PPE/equipment shortages, and working in direct patient care while sick were associated with increased odds of negative mental health outcomes. A number of these circumstances are modifiable by changes in institutional and governmental policy. An important implication of these findings is that modifications such as stockpiling of PPE and other equipment, and maintaining adequate staffing including backup capacity may reduce the risks of adverse mental health impacts among physicians, nurse practitioners, and physician assistants in future pandemic situations. Whether these findings also extend to other categories of workers such as nurses and allied health care workers should be addressed in future research.
ACKNOWLEDGMENTS
The authors received no specific funding for this research. The authors thank the New York State Health Commissioner’s Office, the participants of the COVID-19 Healthcare Personnel Study, David P. Merle for programming the interview, and William Keating and Sarah Forthal for the editorial assistance.
Footnotes
Funding Sources: None to disclose. The study was designed and conducted pro bono by an ad hoc collaboration of investigators from Columbia University, New York State Psychiatric Institute, New York University, and City University of New York.
Conflict of Interest: None declared.
Ethical Considerations and Disclosure(s): The study was approved by the institutional review boards of the participating institutions, and a waiver of documentation of informed consent was obtained. Informed consent was obtained electronically from all participants before gaining access to the on-line survey.
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.joem.org).
Contributor Information
Michaeline Bresnahan, Email: Mab29@cumc.columbia.edu.
Megan Ryan, Email: Megan.Ryan@nyspi.columbia.edu.
George J. Musa, Email: George.Musa@nyspi.columbia.edu.
Lawrence Amsel, Email: Larry.Amsel@nyspi.columbia.edu.
Charles DiMaggio, Email: Charles.DiMaggio@nyulangone.org.
Howard F. Andrews, Email: Howard.Andrews@nyspi.columbia.edu.
Ezra Susser, Email: ess8@cumc.columbia.edu.
Guohua Li, Email: gl2240@cumc.columbia.edu.
David M. Abramson, Email: david.abramson@nyu.edu.
Barbara H. Lang, Email: bl2309@cumc.columbia.edu.
Christina W. Hoven, Email: Ch42@cumc.columbia.edu.
REFERENCES
- 1.Thompson CN Baumgartner J Pichardo C, et al. COVID-19 outbreak—New York City, February 29–June 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1725–1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.New York State Department of Health . New York State Statewide COVID-19 Fatalities by Age Group. 2022. Available at: http://health.data.ny.gov/d/du97-svf7/visualization. Accessed March 22, 2022.
- 3.Rothfeld M, Sengupta S, Goldstein J, Rosenthal BM. 13 Deaths in a day: an ‘apocalyptic’ coronavirus surge at an N.Y.C. Hospital. The New York Times. 2020. Available at: https://www.nytimes.com/2020/03/25/nyregion/nyc-coronavirus-hospitals.html. Accessed June 23, 2022. [Google Scholar]
- 4.Breazzano MP Shen J Abdelhakim AH, et al. New York City COVID-19 resident physician exposure during exponential phase of pandemic. J Clin Invest. 2020;130:4726–4733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brooks SK Webster RK Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly M. The pandemic’s psychological toll: an emergency physician’s suicide. Ann Emerg Med. 2020;76:A21–A24. [Google Scholar]
- 7.Schwartz DA, Connerney MA, Davila-Molina M, Tummalapalli SL. Resident mental health at the epicenter of the COVID-19 pandemic. Acad Med. 2021;96:e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PloS One. 2021;16:e0246454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sirois FM, Owens J. Factors associated with psychological distress in health-care workers during an infectious disease outbreak: a rapid systematic review of the evidence. Front Psychiatry. 2021;11:589545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. Brain Behav Immun Health. 2020;100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shechter A Diaz F Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DiMaggio C Abramson D Susser ES, et al. The COVID-19 Healthcare Personnel Study (CHPS): overview, methods, and preliminary findings. J Neurosurg Anesthesiol. 2022;34:148–151. [DOI] [PubMed] [Google Scholar]
- 13.DiMaggio C Abramson D Susser E, et al. The COVID-19 Healthcare Personnel Study (CHPS): overview, methods and preliminary report. medRxiv. 2020. [DOI] [PubMed] [Google Scholar]
- 14.Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58:163–171. [DOI] [PubMed] [Google Scholar]
- 15.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22:1596–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. [DOI] [PubMed] [Google Scholar]
- 17.Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness presenteeism. J Epidemiol Community Health. 2000;54:502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evanoff BA Strickland JR Dale AM, et al. Work-related and personal factors associated with mental well-being during the COVID-19 response: survey of health care and other workers. J Med Internet Res. 2020;22:e21366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huffman EM Athanasiadis DI Anton NE, et al. How resilient is your team? Exploring healthcare providers’ well-being during the COVID-19 pandemic. Am J Surg. 2021;221:277–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hennein R, Mew EJ, Lowe SR. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PloS One. 2021;16:e0246602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharma M Creutzfeldt CJ Lewis A, et al. Health-care professionals’ perceptions of critical care resource availability and factors associated with mental well-being during coronavirus disease 2019 (COVID-19): results from a US survey. Clin Infect Dis. 2020;72:e566–e576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feingold JH Peccoralo L Chan CC, et al. Psychological impact of the COVID-19 pandemic on frontline health care workers during the pandemic surge in New York City. Chronic Stress (Thousand Oaks). 2021;5:2470547020977891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skagen K, Collins AM. The consequences of sickness presenteeism on health and wellbeing over time: a systematic review. Soc Sci Med. 2016;161:169–177. [DOI] [PubMed] [Google Scholar]
- 24.Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin SE, Sammons JS. Reasons why physicians and advanced practice clinicians work while sick: a mixed-methods analysis. JAMA Pediatr. 2015;169:815–821. [DOI] [PubMed] [Google Scholar]
- 25.Griffin BJ Purcell N Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32:350–362. [DOI] [PubMed] [Google Scholar]
- 26.Williamson V, Stevelink SAM, Greenberg N. Occupational moral injury and mental health: systematic review and meta-analysis. Br J Psychiatry. 2018;212:339–346. [DOI] [PubMed] [Google Scholar]
- 27.Williamson V, Murphy D, Greenberg N. COVID-19 and Experiences of Moral Injury in Front-Line Key Workers. Oxford, United Kingdom: Oxford University Press; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hines SE, Chin KH, Glick DR, Wickwire EM. Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:488. [DOI] [PMC free article] [PubMed] [Google Scholar]


