Abstract
Aim
The present study aimed to investigate the construct structure behind the psychosocial response, behavioral response, prenatal depression, and post-traumatic stress disorder (PTSD) in pregnant women during the COVID-19 pandemic in China.
Method
The validated Chinese version of the Edinburgh Postnatal Depression Scale (EPDS), PTSD CheckList (PCL)-6, and two newly established scales for COVID-19-related psychological and behavioral responses were used. Structural equation modeling (SEM) analysis was applied to evaluate the structural relationships of psychological and behavioral responses during the COVID-19 pandemic.
Results
Of the 1,908 mothers who completed the questionnaires, 1,099 met the criteria for perinatal depression, and 287 were positively screened for PTSD, where 264 women exceed the cut-off points for both. Pregnant women with full-time or part-time jobs tended to have the lowest scores of EPDS (10.07 ± 5.11, P < 0.001) and stress levels (23.85 ± 7.96, P = 0.004), yet they were more likely to change their behavior in accordance with the COVID-19 outbreak (13.35 ± 3.42, P = 0.025). The structural model fit the data (χ2 = 43.260, p < 0.001) and resulted in satisfactory fit indices (CFI = 0.984, TLI = 0.959, RMSEA = 0.072, and χ2/df = 10.815), all path loadings were significant (p < 0.05). The SEM indicates that the level of QoL was attributable to the occurrence of PND, leading to PTSD, and COVID-19 related behavioral and psychological responses.
Conclusion
The inter-relationships between the COVID-19-related psychosocial and behavioral responses have been assessed, indicating that the pandemic increased the burden of perinatal depression. Psychoeducation, as well as other psychological interventions, may be needed to alleviate the COVID-19-based anxiety and increase their engagement in protective behaviors.
Keywords: COVID-19, pregnancy, perinatal depression, post-traumatic stress disorder, structural equating modeling
Introduction
A pneumonia-like respiratory system disease outbreak termed the coronavirus disease 2019 (COVID-19) caused by the newly identified coronavirus, the severe acute respiratory syndrome (SARS)-CoV-2, swept through China in early 2020. COVID-19 was officially announced as a global pandemic on 11th March (1). The COVID-19 pandemic has disrupted the lives of millions across the globe, resulting in more than 2 million deaths since January 2020 (2).
The outbreak of infectious diseases induces widespread anxiety (3). During the SARS outbreak in 2003, empirical studies on psychological responses of the general population to epidemics were reported (4–6). Panic over the COVID-19 outbreak resulted in the public over-purchasing and hoarding of necessities, including tissue paper, surgical masks, hand sanitizers, and disinfectants, though such infections do not typically result in death (7, 8). Beyond this, the levels of depression, anxiety, and post-traumatic stress disorder (PTSD) among the public have elevated, pertaining to the infectious disease and the uncertainty of the situation.
Nevertheless, reports of the psychological impact of infectious disease outbreaks on pregnant women have been rare. Pregnant women are particularly affected, as they are naturally concerned about the safety of their fetus and tend to overestimate the risk of contracting the disease (5, 9). Elevated stress level in pregnant women during the SARS outbreak was precipitated by the infection and the epidemic itself, quarantine, economic fallout, and lack of social and family support (3). Previous trauma and recent stressful life events were associated with anxiety and depression in perinatal period (3, 10), yet it impacts pregnancy and postpartum stages differently (11). Psychometric evidence of the Perceived Stress Scale has shown that pregnant women are more associated with depression with certain risk factors, namely unemployment, lower education level, perceived stress in the last month, and recent life adversity (12). Nevertheless, symptoms of both depression and PTSD are prevalent amongst post-delivery mothers (13, 14).
Our preliminary nationwide cross-sectional study on the psychological impact of COVID-19 on pregnant women has revealed a high prevalence of probable depression in prenatal depression (PND) (34%) and suspected PTSD (40%) (15). Although many studies have investigated the relationship between peripartum depression and PTSD in pregnant women, the construct relationship is still not fully elucidated, let alone the interactions during the COVID-19 pandemic (16, 17).
The COVID-19 situation is likely to generate additional stress for perinatal women (18–20). Current studies on COVID-19 have documented anxiety in pregnant women regarding themselves or their friends and family being infected during and after their pregnancy (15). Concerns about miscarriage and preterm births have also been reported, leading these women to consider altering their perinatal care routine, including postponing or canceling perinatal appointments. The implementation of physical distancing and quarantine guidelines might have further disrupted the modalities and delivery of routine prenatal care and impeded access to social support after childbirth (21–23).
Furthermore, the experiences of emotional insecurity may be acute (15, 24), where women might experience intense loneliness from the absence of companionship during the delivery or postpartum care. Hence, sufficient caregiving and other social support are much needed by both their mothers and family.
Coping skills have always been a precipitate and perpetuity for psychiatric disorders (25–27). Empirical evidence has indicated that suppressive, proactive, and avoidant coping strategies, such as behavioral disengagement and problem denial, are more prevalent among patients with psychiatric disorders (28–30), compared to healthy participants (31). At the same time, a systematic review has noted the susceptibility of perinatal women with psychological difficulties to avoidant behavioral patterns for stress coping (32, 33). Given that pregnant women are psychologically vulnerable under the pandemic, it is necessary to evaluate the roles of stress and behavioral responses manifested by their coping skills and their effects on perinatal mental health.
Since COVID-19 has a negative impact on pregnant women's perinatal mental health, the psychological demands of perinatal women need to be acknowledged. Based on our previous nationwide population-based cross-sectional survey, this study aims to investigate the possible role of different psychiatric diseases during the outbreak of COVID-19 and the influences on the behavioral changes and decision-making of prenatal examinations.
Therefore, a structural equation modeling (SEM) was defined to grasp the prediction of perinatal depression and PTSD during the COVID-19 outbreak. Based on the preceding literature review and objectives above, our primary hypotheses were as follows: (1) behavioral responses resulting from the pandemic are related to its psychological response, as well as probable PND and suspected PTSD; (2) behavioral responses and psychological responses resulting from the pandemic are interrelated to probable PND and suspected PTSD.
Methods
Study Design
A nationwide population-based cross-sectional study was conducted among pregnant women in China during the COVID-19 pandemic. Participants were invited to complete a web-based questionnaire. Participants were initially recruited from local hospitals across the nation via a hospital-based online education scheme for Chinese women during antenatal and postnatal periods. This online scheme allowed local hospitals to assess participating pregnant women's health conditions and provide primary care to their clients (via the Internet) during their pregnancy. Informed consent from each participant was obtained initially, prior to filling out the questionnaire. The data analyzed for this study was collected from 1908–2020, between February 13–16, from women in their second- or third-trimester of pregnancy.
Research Protocol
The study protocol was reviewed and approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (reference no: UW 20-252). All procedures were conducted in accordance with the Declaration of Helsinki.
Measurements
Participants were given the following questionnaire in Chinese in a structured online-based questionnaire format:
Demographic Data
Participants' age, marital status, educational level, occupation, primiparity, presence of complications during pregnancy, and history of depression were collected.
Depression in Pregnancy
Depression in pregnancy or PND was assessed using the 10-item Chinese version of the Edinburgh Postnatal Depression Scale (EPDS), which was designed to assess perinatal depression to identify pregnant women at risk of PND (34, 35). This screening tool consists of 10 items relating to enjoyment and happiness, feelings of blame, anxiety and fear, sleeping problems, sadness, crying, and thoughts of self-harm. Each item is rated on a four-point scale from 0 to 3, and all items are added to form an overall score ranging from 0 to 30. Reverse scoring also applied in EPDS. Respondents are required to answer each question based on their feelings in the past 7 days. Participants scoring 13 or above are at considerable risk for depression, where probable or moderate PND is classified accordingly if the diagnosis is confirmed (36), and it is suggested to seek medical attention. Participants who scored between 10–12, indicate the experience of depressive symptoms and are classified as possible PND, which would be termed as mild PND if the diagnosis is confirmed (37). The internal consistency of the questionnaire was satisfactory (Cronbach α coefficient = 0.8480, Kaiser-Meyer-Olkin (KMO) measures of sampling adequacy = 0.881).
Post-traumatic Stress
Post-traumatic stress was measured using the PTSD Checklist-Specific version (PCL-S) in Chinese (38). The PCL asks respondents to indicate their level of irritation (five-point format) in response to specific stressful life experiences in the past month (39). For this study, the stressful experience was standardized as “the COVID-19 outbreak since late December 2019.” We used the abbreviated six-item version in this study (40). The six-items were derived from the original 17-item version with two items from each of three clusters (i.e., re-experiencing, avoidance, and hyperarousal) and have been validated for psychometry properties (r = 0.96–0.97 with the original total score). When using ≥ 14 as the cut-off, the checklist showed a sensitivity of 0.8–0.95 and specificity of 0.69–0.76 based on diagnostic interviews. This study adopted ≥ 14 as the cut-off point to classify participants into low or high PTSD risk (40). Due to the ongoing outbreak during data collection, those at higher risk (≥14) were demoted as suspected PTSD. The internal consistency of the questionnaire was good (Cronbach α-coefficient = 0.8253, KMO measures of sampling adequacy = 0.819).
COVID-Related Psychological and Behavioral Responses
We also evaluated multiple psychological and behavioral responses to COVID-19, including anxiety about the infection of members within one's social network (five questions), and specific psychological responses (anxiety when staying at home, lack of security, and loss of freedom; three questions). The internal consistency of the questionnaire was good (Cronbach α-coefficient = 0.8957, KMO measures of sampling adequacy = 0.868).
The behavioral response included items about precautionary behaviors (handwashing, use of facemasks, wearing gloves, and housebound behaviors; four questions) and psycho-behavioral responses, particularly related to pregnancy (anxiousness about miscarriage and premature birth, fear of antenatal check-up and consultation, and cancellation and postponement of antenatal visit; six questions). The internal consistency of the questionnaire was good (Cronbach α-coefficient = 0.4379, KMO measures of sampling adequacy = 0.691).
Statistical Analyses
First, a descriptive statistical analysis of the main variables of interest was conducted, using central tendency (mean, median) and dispersion (standard deviation, interquartile interval) measures. In addition, preliminary regression analyses were performed to examine whether scores of scales differed by participants' demographics, and zero-order pair-wise correlations among them were reported. Finally, SEM, a type of multivariate analysis, was applied to confirm a theoretically built model that includes domains of post-traumatic stress experience, depression in pregnancy, COVID-19-related psychological and behavioral responses, as well as quality of life (QoL) domains.
In the first step, the model was designed and fitted with a well-defined research question. Next, the estimation and the significant levels for each parameter were obtained. Third, the assumed structure of the data was compared, and the goodness of fit measures for the model built were evaluated using multiple indices, including the chi-square statistic, the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), the χ2/df , and the Root Mean Square Error of Approximation (RMSEA) (41). CFI ranged between 0 and 1, with values > 0.90 suggesting a good fit; RMSEA is a measure of the discrepancy between the model and the data per degree of freedom, with values <0.5 indicating close fit and values between 0.5 and 0.8 suggesting acceptable fit (42); and χ2/df is a measure relating to the chi-square and degree of freedom, with the values less than three suggesting a good fit. If indicated, correlations between error terms were added and parameters were constrained to improve the model.
All analyses were conducted in R version 3.6.2. Statistical significance was set at p < 0.05.
Results
Demographic Characteristics
Table 1 summarizes the demographic characteristics of postpartum women completing the survey. Of the mothers completing the questionnaires (n = 1,908), 1,099 met the criteria for a positive screening for perinatal depression, and 287 met the criteria for a positive screening for PTSD, where 264 women exceed the cut-off points for both (Table 1). Moreover, the subsequent psychological and behavioral responses to the COVID-19 outbreak were designated as stress level and behavioral adjustment in the study and reported in Tables 2, 3, respectively. Married women were more likely to have PTSD experience and adopted preventive behaviors (13.27 ± 3.34, p = 0.011), yet single mothers had higher scores of EPDS (13.20 ± 5.78, p = 0.055). Pregnant women with full-time or part-time jobs tended to have the lowest scores of EPDS (10.07 ± 5.11, P < 0.001) and stress level (23.85 ± 7.96, p = 0.004), yet they were more likely to change their behavior in accordance with the outbreak of COVID-19 (13.35 ± 3.42, p = 0.025).
Table 1.
Descriptive statistics of the demographic characteristics.
| Demographic results (N = 1,908) | ||
|---|---|---|
| Age, mean (SD) | 28.88 (4.75) | |
| Whether in Hubei province, n (%) | Yes | 95 (5.0%) |
| No | 1,813 (95.0%) | |
| Education, n (%) | Primary school/ Junior Secondary school | 397 (20.8%) |
| Senior/ technical secondary school | 474 (24.8%) | |
| College/ University | 964 (50.5%) | |
| Graduate | 73 (3.8%) | |
| Marital state, n (%) | Single | 15 (0.8%) |
| Married/ cohabitation | 1,893 (99.2%) | |
| Gestation, median (IQR) | 2 (1, 2) | |
| Gravidity, median (IQR) | 0 (0, 1) | |
| Work, n (%) | Students/ not employed | 76 (4.0%) |
| Full-time/ part-time | 930 (48.7%) | |
| Housewife | 902 (47.3%) | |
| Scores of PCL-6, mean (SD) | 12.83 (4.17) | |
| Scores of EPDS, mean (SD) | 10.62 (5.21) | |
| Scores of Behavioral response, mean (SD) | 13.25 (3.36) | |
| Scores of Psychological response level, mean (SD) | 24.45(7.82) | |
| EQ-VAS, mean (SD) | 86.90 (14.22) | |
| Probable PND, n (%) | 1,099 (57.6%) | |
| Suspected PTSD, n (%) | 287 (15.0%) | |
| Any Family infected, n (%) | Yes | 2 (0.1%) |
| No | 1,906 (99.9%) | |
| Any Friend infected, n (%) | Yes | 11 (0.6%) |
| No | 1,897 (99.4%) | |
| Any Neighbor infected, n (%) | Yes | 40 (2.1%) |
| No | 1,868 (97.9%) | |
| Ever Depression, n (%) | Yes | 159 (8.3%) |
| No | 1,749 (91.7%) |
Table 2.
Demographic factors associated with the scores of scales.
| Educational level | Primary school/ Junior Secondary school (N = 397) | Senior/ technical secondary school (N = 474) | College/ University (N = 964) | Graduate (N = 73) | p-value |
|---|---|---|---|---|---|
| Scores of PTSD, mean (SD) | 12.89 (4.47) | 12.86 (3.95) | 12.83 (4.19) | 12.18 (3.69) | 0.6 |
| Scores of EPDS, mean (SD) | 11.39 (5.43) | 10.97 (4.94) | 10.30 (5.24) | 8.53 (4.45) | <0.001 |
| Suspected PTSD, n (%) | 61 (15.4%) | 73 (15.4%) | 146 (15.1%) | 7 (9.6%) | 0.62 |
| Probable PND, n (%) | 255 (64.2%) | 288 (60.8%) | 528 (54.8%) | 28 (38.4%) | <0.001 |
| Behavioral responses, mean (SD) | 13.21 (3.45) | 13.17 (3.29) | 13.30 (3.37) | 13.29 (3.20) | 0.89 |
| Psychological responses, mean (SD) | 25.50 (7.52) | 25.22 (6.91) | 23.82 (8.25) | 22.04 (7.90) | <0.001 |
| Occupational states | Students/ not employed (N = 76) | Full-time/ part-time (N = 930) | Housewife (N = 902) | p -value | |
| Scores of PTSD, mean (SD) | 12.64 (4.44) | 12.72 (4.11) | 12.95 (4.22) | 0.49 | |
| Scores of EPDS, mean (SD) | 11.96 (5.95) | 10.07 (5.11) | 11.09 (5.18) | <0.001 | |
| Suspected PTSD, n (%) | 9 (11.8%) | 127 (13.7%) | 151 (16.7%) | 0.13 | |
| Probable PND, n (%) | 50 (65.8%) | 491 (52.8%) | 558 (61.9%) | <0.001 | |
| Behavioral responses, mean (SD) | 12.26 (3.92) | 13.35 (3.42) | 13.23 (3.23) | 0.025 | |
| Psychological responses, mean (SD) | 24.76 (8.63) | 23.85 (7.96) | 25.04 (7.55) | 0.004 | |
| Marital status | Single (N = 15) | Married (N = 1,893) | p -value | ||
| Scores of PTSD, mean (SD) | 11.33 (4.75) | 12.84 (4.17) | 0.16 | ||
| Scores of EPDS, mean (SD) | 13.20 (5.78) | 10.60 (5.20) | 0.055 | ||
| Suspected PTSD, n (%) | 2 (13.3%) | 285 (15.1%) | 0.85 | ||
| Probable PND, n (%) | 11 (73.3%) | 1,088 (57.5%) | 0.22 | ||
| Behavioral responses, mean (SD) | 11.07 (4.67) | 13.27 (3.34) | 0.011 | ||
| Psychological responses, mean (SD) | 24.47 (7.93) | 24.45 (7.82) | 0.99 |
Table 3.
The pair-wise Pearson correlation of the measured variables.
| Variables | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | (14) | (15) | (16) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Scores of PCL−6 | 1.000 | |||||||||||||||
| (2) Scores of EPDS | 0.626*** | 1.000 | ||||||||||||||
| (3) Scores of Psychological response | 0.520*** | 0.504*** | 1.000 | |||||||||||||
| (4) Scores of Behavioral responses | 0.211*** | 0.211*** | 0.325*** | 1.000 | ||||||||||||
| (5) Age | 0.014 | −0.081*** | −0.068** | 0.132*** | 1.000 | |||||||||||
| (6) Education | −0.016 | −0.109*** | −0.108*** | 0.014 | 0.121*** | 1.000 | ||||||||||
| (7) Marital state | −0.032 | 0.044 | 0.000 | −0.058 | −0.035 | −0.060** | 1.000 | |||||||||
| (8) Number of gestations | 0.032 | 0.045 | 0.000 | 0.010 | 0.262*** | −0.232*** | 0.004 | 1.000 | ||||||||
| (9) Number of gravidities | 0.055 | 0.068** | 0.021 | 0.072** | 0.231*** | −0.275*** | 0.024 | 0.341*** | 1.000 | |||||||
| (10) Any pregnancy complications | 0.079* | 0.085*** | 0.044 | 0.028 | 0.063** | −0.014 | 0.006 | 0.027 | 0.017 | 1.000 | ||||||
| (11) Any family infected | −0.053 | −0.004 | 0.004 | 0.012 | 0.100*** | −0.014 | 0.181*** | 0.034 | 0.088*** | 0.040 | 1.000 | |||||
| (12) Any friend infected | −0.008 | 0.001 | −0.008 | −0.012 | 0.015 | −0.025 | 0.072** | 0.008 | 0.048 | −0.005 | 0.425*** | 1.000 | ||||
| (13) Any neighbor infected | 0.026 | 0.022 | 0.024 | 0.019 | 0.020 | 0.043 | 0.028 | −0.020 | 0.016 | 0.006 | 0.108*** | 0.037 | 1.000 | |||
| (14) Any depression history | 0.131*** | 0.204** | 0.054 | −0.012 | −0.057 | −0.025 | 0.016 | 0.019 | 0.036 | 0.030 | 0.049 | 0.002 | −0.004 | 1.000 | ||
| (15) QoL (EQVAS) | −0.363*** | −0.461*** | −0.218*** | −0.024 | 0.055 | 0.007 | −0.017 | 0.000 | 0.009 | −0.069** | −0.019 | −0.036 | 0.001 | −0.202*** | 1.000 | |
| (16) Whether in Hubei | 0.066** | 0.019 | 0.028 | 0.007 | 0.005 | −0.021 | 0.034 | −0.004 | −0.023 | 0.010 | 0.067** | 0.078*** | 0.236*** | −0.017 | 0.013 | 1.000 |
p<0.01,
p<0.05,
p<0.1.
The influence of demographic factors on the scores of scales was reported in Table 2, where the educational level, occupational status, and marital status were included. We found that women with lower educational levels tended to have higher scores of PCL-6, and EPDS scales as well as stress level and behavioral adjustment, and more were regarded as suspected PTSD and probable PND. Nevertheless, compared to the level-dependent pattern between education level and scores of scales, the occupational states were paradoxically associated with the scores. Pregnant women with full-time or part-time jobs tended to have the lowest scores of EPDS (10.0 ± 5.11, p < 0.001) and stress level (23.85 ± 7.96, p = 0.004), yet they were more likely to change their behavior in accordance with the outbreak of COVID-19 (13.35 ± 3.42, p = 0.025). Housewives had a higher level of PTSD experience but a medium level of EPDS scores. Still, married women were more likely to have PTSD experience and adopted preventive behaviors (13.27 ± 3.34, p = 0.011), yet the single mother had higher scores of EPDS (13.20 ± 5.78, p = 0.055).
Preliminary Analyses and Pearson Correlation Coefficients
Generalized linear modeling (GLM) multivariate test results showed that the four scores of the scales have distinct patterns of difference by marital status, employment status, education level, obstetrics history (gestation, gravidity, and any pregnancy complication history), any history of COVID-19 exposure (any history of friend, family, or neighbors infected), and whether in Wuhan (Supplementary Tables S1–4). First, age (Coef = −0.09, t-value = −3.22, p = 0.001), number of gravidities (Coef = 0.347, t-value = 3.94, p = 0.022), history of any pregnancy complications (Coef = 1.477, t-value = 3.94, p < 0.001), and education were significant predictors for the scores of EPDS (Supplementary Table S1), where a higher level of education associated with lower scores of EPDS. In addition, being in Hubei (Coef = 1.251, t-value = 2.77, p = 0.006), number of gravidity (Coef = 0.275, t-value = 2.25, p = 0.024), and history of any pregnancy complications (Coef = 1.08, t-value = 3.57, p < 0.001) served as significant predictors for the scores of PCL-6 (Supplementary Table S2). Moreover, the scores of the COVID-19-related psychological responses were significantly related to age (Coef = −0.088, t-value = −2.09, p = 0.037), history of any pregnancy complications (Coef = 1.229, t-value = 2.17, p = 0.118), and education level (Supplementary Table S3). Finally, age (Coef = 0.086, t-value = 4.79, p < 0.001), marital status (Coef = −1.951, t-value = −2.19, p = 0028), and number of gravidity (Coef = 0.229, t-value = 2.33, p = 0.02) served as significant predictors for the scores of COVID-19-related behavioral responses (Supplementary Table S4).
The correlation for all indicators is shown in Table 3. The scores of the four scales were significantly correlated, and the QoL, as measured by EQVAS, was also significantly correlated with the scores of PCL-6, EPDS, and COVID-19-related psychological responses. Specifically, past-history of depression was also found to significantly correlated with the scores of PCL-6 and scores of EPDS. Age was also significantly correlated with the scores of EPDS and scores of COVID-19-related psychological and behavioral responses. Moreover, being in Hubei Province, the epicenter of the COVID-19 pandemic in China, was found to be significantly correlated with the scores of PCL-6, and the history of any pregnancy complications was also found to be significantly correlated with the scores of PCL-6 and EPDS.
Structural Equation Modeling
Structural equation modeling was conducted to evaluate the proposed structural model. First, to evaluate the intercorrelation between pregnant women's psychological and behavioral responses during the COVID-19 pandemic. The QoL score was hypothesized to have direct and indirect effects on PND and PTSD, as well as psychological and behavioral responses. Second, the state of PND was hypothesized to have direct effects on the post-traumatic stress experience, psychological responses, and behavioral responses. Moreover, behavioral responses were hypothesized to be influenced by PND and directly influenced psychological responses.
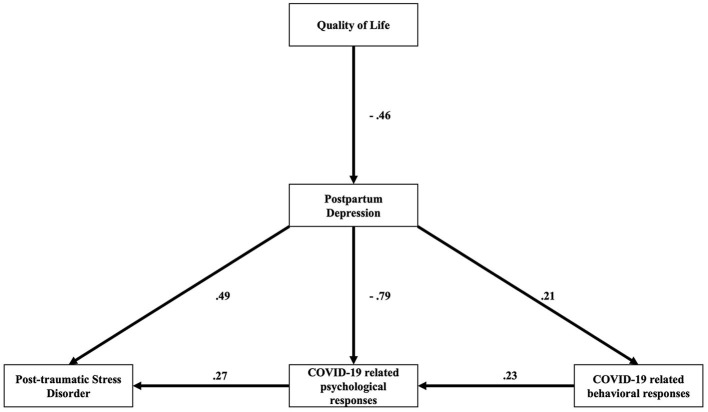
Figure 1 shows significant pathways of the final model. The structural model fit the data (χ2 = 43.260, p < 0.001) and resulted in the following satisfactory fit indices (CFI = 0.984, TLI = 0.959, RMSEA = 0.072, and χ2/df = 10.815). All path loadings were significant (p < 0.05), and the results of the SEM are reported in Table 4.
Figure 1.
The hypothesized model relating the scores of PCL-6, EPDS, and COVID-9-related psychological and behavioral. All path loadings were significant (p < 0.05).
Table 4.
Relationship between independent and dependent variables.
| Estimate | Standard errors | z-value | p-value | 95% Confidence interval | ||||
|---|---|---|---|---|---|---|---|---|
| Scores of PCL−6 | –> | Scores of Psychological responses | 0.147 | 0.011 | 13.959 | 0 | 0.126 | 0.167 |
| Scores of PCL−6 | –> | Scores of EPDS | 0.391 | 0.016 | 24.788 | 0 | 0.360 | 0.421 |
| Scores of Psychological responses | –> | Scores of Behavioral responses | 0.533 | 0.045 | 11.726 | 0 | 0.444 | 0.622 |
| Scores of Psychological responses | –> | Scores of EPDS | 0.682 | 0.029 | 23.282 | 0 | 0.625 | 0.740 |
| Scores of Behavioral responses | –> | Scores of EPDS | 0.136 | 0.014 | 9.452 | 0 | 0.108 | 0.165 |
| Scores of EPDS | –> | Scores of EQVAS | −0.169 | 0.007 | −22.712 | 0 | −0.184 | −0.154 |
| Scores of PCL−6 | ~~ | Scores of PCL−6 | 9.597 | 0.311 | 30.887 | 0 | 8.988 | 10.206 |
| Scores of Psychological responses | ~~ | Scores of Psychological responses | 42.503 | 1.376 | 30.887 | 0 | 39.806 | 45.200 |
| Scores of Behavioral responses | ~~ | Scores of Behavioral responses | 10.769 | 0.349 | 30.887 | 0 | 10.086 | 11.453 |
| Scores of EPDS | ~~ | Scores of EPDS | 21.367 | 0.692 | 30.887 | 0 | 20.011 | 22.722 |
Discussion
To our knowledge, this is the first SEM study based on real-world data from a nationwide study to examine the relationship between various psychological factors and behavioral changes in pregnant women during the COVID-19 outbreak. The survey was conducted during the peak (between February 13 and 16, 2020) of the COVID-19 outbreak in China. Our study demonstrates the relationship between post-traumatic experience, depression in pregnancy, and the interrelationship between behavioral and psychological responses in pregnant women.
The COVID-19 outbreak had profound psychological impacts on pregnant women. A substantial portion of pregnant women have demonstrated to have suspected PTSD, probable PPD symptoms, high-stress levels, and subsequent behavioral adjustment. As much as 24.8% of pregnant women considered themselves likely to be infected by SARS-CoV-2 (15). Incidents illustrating a biased risk assessment over COVID-19 could be seen in avoidance behavior, such as canceling and postponing antenatal check-up appointments. About 71.2% of pregnant women reported having canceled or postponed antenatal check-up appointments during the outbreak. These findings are consistent with a survey on psychological response, behavior, and attitudes of pregnant women to the SARS outbreak by Ng et al. (5) and Lee et al. (9). Although a recent investigation on the public's psychological responses during the initial stage of COVID-19 in China reported that most respondents believed the risk of contracting the infection during the outbreak was low (43), pregnant women we surveyed were highly stressed, possibly owing to the pressure of decision-making on the undergoing of antenatal examinations, risking viral exposure in hospital settings. Psychological effects brought about by public health measures may also contribute to stress production (44).
Secondly, demographic factors have been found to influence women's symptoms, as shown in the scores of scales in Table 4, where educational level, occupational status, and marital status were the most notable. Women with lower educational levels tended to have higher scores of PCL-6 and EPDS scales, as well as psychological and behavioral responses during the COVID-19 pandemic, where more than 15% and 60% of those with only primary school and junior secondary school education have been regarded as suspected PTSD and probable PND, respectively. Such findings correlate with the study by Hanna-Leena et al. (45), where they reported that the most important factors contributing to perinatal anxiety included employment and elective cesarean section, while educational levels played a minor role (45). Therefore, improving antenatal emotional well-being may have positive social and maternal care for optimal childbirth experiences, especially during the COVID-19 outbreak. A clinical trial by Jocelyn et al. (46) reported that pregnant women with psycho-education by trained midwives had an effective reduction of fear that may be associated with the delivery and elevated childbirth confidence (46). Hence, greater social support might also help to buffer depression and anxiety-related symptoms in pregnant women (47).
Psychologists have published a wide range of theories in attempt to explain the underlying mechanism of infectious outbreak-related anxiety and fear. Anxiety and fear are implicitly results of biased information processing (48), but also in explicit biases in the evaluation of risk and information (49, 50). When risks regarding an event are overestimated in its likelihood of occurrence or its severity, a maladaptive fear process can generate, leading to the irrationality of one's anticipatory response (51, 52).
As none of the 1908 participants had contracted the infection, the pregnant women may, in comparison to the public, have overestimated the risk of COVID-19. Nevertheless, their high-stress level should not be neglected. Disease outbreaks related to anxiety and panic are attributable to two factors: stigma on the infectious virus and fear of the unknown (50). The effect of the stigma attached to the virus is widely documented in population survey studies on outbreaks, including SARs, Ebola, and Zika. Fear of the unknown might be provoked by unforeseeable events (such as death or disabilities), the unknown nature of the virus, and economic paralysis (53, 54).
Moreover, healthcare authorities need to provide psychological support for those in need. Online and smartphone-based psychological interventions, including hotlines to provide crisis support should be considered. The content of these interventions needs to be modified to suit the needs of the pregnant women presenting with mental health difficulties during the pandemic. Physical symptoms, as a result of psychological distress should also be addressed. Symptoms such as headaches, fatigue, dizziness, high blood pressure, and breathing difficulties are often presented in people with mental illnesses, such as anxiety, depression, and PTSD. It is evident that those with poor health status and a history of chronic illness are more likely to experience psychological impacts as well as stress, anxiety, and depression amidst an outbreak (55). Health professionals should be aware of the symptoms above and provide early adequate psychological support and intervention. Moreover, healthcare authorities should be alert to possible long-term psychiatric sequelae, especially PTSD and PPD.
There are several limitations to this study. The questionnaire was self-administered and hence, reporting bias is possible. The study measured the stress level and behavioral adjustment using a newly developed questionnaire. Though we have tested the validity and reliability of the questionnaire, there still may be unfound bias and limited utility in reflecting the real conditions. The comprehension of the questionnaire by the respondents was not evaluated. It was not possible to evaluate psychometric performance of the questionnaire because the questionnaire is simply a collection of questions on how pregnant women reacted to the outbreak. However, the internal consistency of the questionnaire has been assessed and resulted in promising reliability. The psychological responses of pregnant women toward the infection were collected prior to its declaration as a pandemic. Thus, only the initial and intermediary responses were examined in the present study. Moreover, though information on education level and culture were collected, we failed to investigate the socioeconomic status or collect data on income. All the respondents in the study were pregnant Chinese women involved in an online teaching school, which may limit the homogeneity of the respondents. A longitudinal follow-up investigation is pending to examine the long-term psychological effects of this outbreak.
Conclusion
To date, the psychological stress of pregnant women under the COVID-19 pandemic have been underestimated. Our results contributed to elucidating the relationships between the COVID-19-related distress and the mental health of women in the perinatal period. Perinatal depression is associated with PTSD-like anxiety and may lead to COVID-19-related behavioral and psychological responses in pregnant women during the COVID-19 pandemic. Mental health surveillance in pregnant women is necessary. Psychoeducation, as well as other psychological interventions, may be needed to equip pregnant women and their family members with problem-solving and communication skills to alleviate COVID-19-related distress.
Significant Outcomes
Out of the 1,908 mothers who completed the questionnaires, 1,099 met the criteria for perinatal depression, and 287 were positively screened for PTSD where 264 women exceed the cut-off points for both.
Being in Hubei Province, the epicenter of the COVID-19 pandemic in China, was found to be significantly correlated with the scores of PCL-6, and the history of any pregnancy complications was also found to be significantly correlated with the scores of PCL-6 and EPDS.
Moreover, the scores of the COVID-19-related psychological responses were significantly related to age, history of any pregnancy complications, and education level.
Take-Home Messages
With the COVID-19 pandemic ongoing, and normalized regulatory stage enforced, the COVID-19 outbreak represented an additional factor that increased the burden of perinatal depression, and psychoeducation, as well as other psychological interventions, may be needed to improve their mental health.
Limitations
The questionnaire was self-administered, and hence, reporting bias is possible.
The study measured stress levels and behavioral adjustment using a newly developed questionnaire. Though we have tested the validity and reliability of the questionnaire, unfound bias and limited utility in reflecting actual conditions may remain.
Psychological responses of pregnant women toward the infection were collected prior to its declaration as a pandemic, and a follow-up investigation was not possible.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by UW 20-252. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
ZH and JC conceptualized the idea, established the questionnaire, and analyzed the data, as well as drafted the manuscript. YL, BA, TW, CZ, and W-KM drafted and revised the manuscript, while helping to perform the statistical analysis and produce the graphics. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by the City University of Hong Kong New Research Initiatives/Infrastructure Support from Central (APRC; grant number 9610589).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Glossary
Abbreviations
- SARS
Severe Acute Respiratory Syndrome
- COVID-19
Coronavirus disease 2019
- PTSD
post-traumatic stress disorder
- PND
prenatal depression
- SEM
structural equation modeling
- EPDS
Edinburgh Postnatal Depression Scale
- PCL-S
PTSD Checklist-Specific version
- QoL
quality of life
- CFI
Comparative Fit Index
- TLI
Tucker-Lewis Index
- RMSEA
Root Mean Square Error of Approximation.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.796567/full#supplementary-material
References
- 1.Organization WM . WHO Announces COVID-19 Outbreak a Pandemic 2020 Available online at: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed March 11, 2020).
- 2.Organization WM. Coronavirus Disease (COVID-19) Situation Report−164. (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200702-covid-19-sitrep-164.pdf?sfvrsn=ac074f58_2 (accessed July 2, 2020).
- 3.Person B, Sy F, Holton K, Govert B, Liang A, NCID, et al. Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis. (2004) 10:358. 10.3201/eid1002.030750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blendon RJ, Benson JM, DesRoches CM, Raleigh E. Taylor-Clark K. The public's response to severe acute respiratory syndrome in Toronto and the United States. Clin Infect Dis. (2004) 38:925–31. 10.1086/382355 [DOI] [PubMed] [Google Scholar]
- 5.Ng J, Sham A, Tang PL, Fung S. SARS: pregnant women's fears and perceptions. Br J Midwifery. (2004) 12:698–702. 10.12968/bjom.2004.12.11.16710 [DOI] [Google Scholar]
- 6.Leung GM, Ho L-M, Chan SK, Ho S-Y, Bacon-Shone J, Choy RY, et al. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin Infect Dis. (2005) 40:1713–20. 10.1086/429923 [DOI] [PubMed] [Google Scholar]
- 7.Fofana NK, Latif F, Sarfraz S, Bashir MF, Komal B. Fear and agony of the pandemic leading to stress and mental illness: an emerging crisis in the novel coronavirus (COVID-19) outbreak. Psychiatry Res. (2020) 291:113230. 10.1016/j.psychres.2020.113230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shorey S, Ang E, Yamina A, Tam C. Perceptions of public on the COVID-19 outbreak in Singapore: a qualitative content analysis. J Public Health. (2020) 42:665–71. 10.1093/pubmed/fdaa105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee DTS, Sahota D, Leung TN, Yip ASK, Lee FFY, Chung TKH. Psychological responses of pregnant women to an infectious outbreak: a case-control study of the 2003 SARS outbreak in Hong Kong. J Psychosom Res. (2006) 61:707–13. 10.1016/j.jpsychores.2006.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bianciardi E, Barone Y, Lo Serro V, De Stefano A, Giacchetti N, Aceti F, et al. Inflammatory markers of perinatal depression in women with and without history of trauma. Riv Psichiatr. (2021) 56:237–45. 10.1708/3681.36671 [DOI] [PubMed] [Google Scholar]
- 11.Bianciardi E, Vito C, Betrò S, De Stefano A, Siracusano A, Niolu C. The anxious aspects of insecure attachment styles are associated with depression either in pregnancy or in the postpartum period. Ann Gen Psychiatry. (2020) 19:51. 10.1186/s12991-020-00301-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saur AM, Dos Santos MA. Risk factors associated with stress symptoms during pregnancy and postpartum: integrative literature review. Women Health. (2021) 61:651–67. 10.1080/03630242.2021.1954132 [DOI] [PubMed] [Google Scholar]
- 13.Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. (2001) 15:232–40. 10.1046/j.1365-3016.2001.00345.x [DOI] [PubMed] [Google Scholar]
- 14.Soderquist J, Wijma K. Wijma B. Traumatic stress after childbirth: the role of obstetric variables. J Psychosom Obstet Gynaecol. (2002) 23:31–9. 10.3109/01674820209093413 [DOI] [PubMed] [Google Scholar]
- 15.Zhang CJ, Wu H, He Z, Chan NK, Huang J, Wang H, et al. Psychobehavioral responses, post-traumatic stress and depression in pregnancy during the early phase of COVID-19 outbreak. Psychiatr Res Clin Pract. (2020) 3:46–54. 10.1176/appi.prcp.20200019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Polachek IS, Harari LH, Baum M, Strous RD. Postpartum anxiety in a cohort of women from the general population: risk factors and association with depression during last week of pregnancy, postpartum depression and postpartum PTSD. Isr J Psychiatry Relat Sci. (2014) 51:128. [PubMed] [Google Scholar]
- 17.Hairston IS, Handelzalts JE, Assis C, Kovo M. Postpartum bonding difficulties and adult attachment styles: the mediating role of postpartum depression and childbirth-related PTSD. Infant Ment Health J. (2018) 39:198–208. 10.1002/imhj.21695 [DOI] [PubMed] [Google Scholar]
- 18.Berthelot N, Lemieux R, Garon-Bissonnette J, Drouin-Maziade C, Martel É, Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand. (2020) 99:848–55. 10.1111/aogs.13925 [DOI] [PubMed] [Google Scholar]
- 19.Cameron EE, Joyce KM, Delaquis CP, Reynolds K, Protudjer JL, Roos LE. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J Affect Disord. (2020) 276:765–74. 10.1016/j.jad.2020.07.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ceulemans M, Hompes T, Foulon V. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic: a call for action. Int J Gynaecol Obstet. (2020) 151:146–7. 10.1002/ijgo.13295 [DOI] [PubMed] [Google Scholar]
- 21.Corbett GA, Milne SJ, Hehir MP, Lindow SW, O'connell MP. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur J Obstet, Gynecol Reprod Biol. (2020) 249:96. 10.1016/j.ejogrb.2020.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thapa SB, Mainali A, Schwank SE, Acharya G. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstet Gynecol Scand. (2020) 99:817–8. 10.1111/aogs.13894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Y, Ma ZF. Psychological responses and lifestyle changes among pregnant women with respect to the early stages of COVID-19 pandemic. Int J Soc Psychiatry. (2021) 67:344–50. 10.1177/0020764020952116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liang P, Wang Y, Shi S, Liu Y, Xiong R. Prevalence and factors associated with postpartum depression during the COVID-19 pandemic among women in Guangzhou, China: a cross-sectional study. BMC Psychiatry. (2020) 20:1–8. 10.1186/s12888-020-02969-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annu Rev Clin Psychol. (2007) 3:377–401. 10.1146/annurev.clinpsy.3.022806.091520 [DOI] [PubMed] [Google Scholar]
- 26.Ullman SE, Peter-Hagene LC, Relyea M. Coping, emotion regulation, and self-blame as mediators of sexual abuse and psychological symptoms in adult sexual assault. J Child Sex Abus. (2014) 23:74–93. 10.1080/10538712.2014.864747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D. Family violence and COVID-19: increased vulnerability and reduced options for support. Int J Ment Health Nurs. (2020) 29:549–52. 10.1111/inm.12735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stanisławski K. The coping circumplex model: an integrative model of the structure of coping with stress. Front Psychol. (2019) 10:694. 10.3389/fpsyg.2019.00694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nielsen MB, Knardahl S. Coping strategies: a prospective study of patterns, stability, and relationships with psychological distress. Scand J Psychol. (2014) 55:142–50. 10.1111/sjop.12103 [DOI] [PubMed] [Google Scholar]
- 30.Carver CS, Connor-Smith J. Personality and coping. Annu Rev Psychol. (2010) 61:679–704. 10.1146/annurev.psych.093008.100352 [DOI] [PubMed] [Google Scholar]
- 31.Orzechowska A, Zajaczkowska M, Talarowska M, Gałecki P. Depression and ways of coping with stress: a preliminary study. Med Sci Monit. (2013) 19:1050. 10.12659/MSM.889778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guardino CM, Dunkel Schetter C. Coping during pregnancy: a systematic review and recommendations. Health Psychol Rev. (2014) 8:70–94. 10.1080/17437199.2012.752659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holubova M, Prasko J, Matousek S, Latalova K, Marackova M, Vrbova K, et al. Comparison of self-stigma and quality of life in patients with depressive disorders and schizophrenia spectrum disorders–a cross-sectional study. Neuropsychiatr Dis Treat. (2016) 12:3021. 10.2147/NDT.S121556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. BrJ Psychiatry. (1987) 150:782–6. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- 35.Boyd RC, Le H, Somberg R. Review of screening instruments for postpartum depression. Arch Womens Ment Health. (2005) 8:141–53. 10.1007/s00737-005-0096-6 [DOI] [PubMed] [Google Scholar]
- 36.Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. (2009) 119:350–64. 10.1111/j.1600-0447.2009.01363.x [DOI] [PubMed] [Google Scholar]
- 37.Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA psychiatry. (2013) 70:490–8. 10.1001/jamapsychiatry.2013.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu K, Chan S, Yiu VF. Psychometric properties and confirmatory factor analysis of the post-traumatic stress disorder checklist for Chinese survivors of road traffic accidents. East Asian Arch Psychiatry. (2008) 18:144. [Google Scholar]
- 39.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. (1996) 34:669–73. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- 40.Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther. (2005) 43:585–94. 10.1016/j.brat.2004.04.005 [DOI] [PubMed] [Google Scholar]
- 41.Hoyle RH. Structural Equation Modeling: Concepts, Issues, and Applications. Thousand Oaks, CA; London; New Delhi: Sage. (1995). [Google Scholar]
- 42.Brown MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res. (1993) 154:136. [Google Scholar]
- 43.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in china. Int J Environ Res Public Health. (2020) 17:1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet. (2020) 395:760–2. 10.1016/S0140-6736(20)30365-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Melender H-L. Experiences of fears associated with pregnancy and childbirth: a study of 329 pregnant women. Birth. (2002) 29:101–11. 10.1046/j.1523-536X.2002.00170.x [DOI] [PubMed] [Google Scholar]
- 46.Toohill J, Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. A randomized controlled trial of a psycho-education intervention by midwives in reducing childbirth fear in pregnant women. Birth. (2014) 41:384–94. 10.1111/birt.12136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kizilirmak A. Başer M. The effect of education given to primigravida women on fear of childbirth. Appl Nurs Res. (2016) 29:19–24. 10.1016/j.apnr.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 48.Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. (2007) 133:1. 10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- 49.Loewenstein G, Lerner J. The role of emotion in decision making. In: Davidson RJ, Goldsmith HH, Scherer KR, editors. The Handbook of Affective Science Oxford. England: Oxford University Press; (2003). [Google Scholar]
- 50.Cheng CJ. To be paranoid is the standard? Panic responses to SARS outbreak in the Hong Kong special administrative region. Asian Perspective. (2004) 28:67–98. 10.1353/apr.2004.0034 [DOI] [Google Scholar]
- 51.Jones MK, Menzies RG. Danger expectancies, self-efficacy and insight in spider phobia. Behav Res Ther. (2000) 38:585–600. 10.1016/S0005-7967(99)00076-5 [DOI] [PubMed] [Google Scholar]
- 52.Hofmann SG, Alpers GW, Pauli P. Phenomenology of panic and phobic disorders. In: Antony MM, Stein MB, editors. Oxford Handbook of Anxiety and Related Disorders. New York, NY: Oxford University Press; (2009) p. 34–46. [Google Scholar]
- 53.Lam T, Leung G, Chan B, Ho S, Ho L, Hedley A. Public Perceptions and Preventive Measures of Hong Kong Citizens Concerning Atypical (Coronavirus) Pneumonia. Faculty of Medicine, University of Hong Kong (2003). [Google Scholar]
- 54.Cheng C, Tang CS-K. The psychology behind the masks: psychological responses to the severe acute respiratory syndrome outbreak in different regions. Asian J Soc Psycol. (2004) 7:3–7. 10.1111/j.1467-839X.2004.00130.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mak IWC, Chu CM, Pan PC, Yiu MGC, Ho SC, Chan VL. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen Hosp Psychiatry. (2010) 32:590–8. 10.1016/j.genhosppsych.2010.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.