Abstract
With the development of the novel coronavirus disease 2019 (COVID-19) epidemic and the increase in cases, as a potential source of infection, the risk of close contact has gradually increased. However, few studies have analyzed the tracking and management of cross-regional personnel. In this study, we hope to understand the effectiveness and feasibility of existing close contact management measures in Chengdu, so as to provide a reference for further prevention and control of the epidemic. The close contact management mode and epidemiological characteristics of 40,425 close contacts from January 22, 2020, to March 1, 2022, in Chengdu, China, were analyzed. The relationship with index cases was mainly co-passengers (57.58%) and relatives (7.20%), and the frequency of contact was mainly occasional contact (70.39%). A total of 400 (0.99%) close contacts were converted into cases, which were mainly found in the first and second nucleic acid tests (53.69%), and the contact mode was mainly by sharing transportation (63.82%). In terms of close contact management time, both the supposed ((11.93 ± 3.00) days vs. (11.92 ± 7.24) days) and actual ((13.74 ± 17.47) days vs. (12.60 ± 4.35) days) isolation times in Chengdu were longer than those of the outer cities (P < 0.001). For the local clustered epidemics in Chengdu, the relationship with indexed cases was mainly colleagues (12.70%). The tracing and management of close contacts is a two-way management measure that requires cooperation among departments. Enhancing existing monitoring and response capabilities can control the spread of the epidemic to a certain extent.
Keywords: Close contact, Epidemiological characteristics, Tracing and management, Spatial distribution, Disease conversion
Graphical abstract

1. Introduction
The novel coronavirus disease 2019 (COVID-19) has been spreading contrary to expectations since the first report in December 2019, and its outbreak has posed a considerable threat to people around the world [1,2]. As of March 1, 2022, >436 million people have been infected, and 5.9 million have died. Fast access to cross-regional case and close contact information, and rapid identification and management of close contacts are of great significance to reduce the risk of infection in the population and controlling the spread of the epidemic [3,4].
In contrast to SARS CoV, the transmission of COVID-19 occurs in the precursor period of mild illness and daily activities, which contributes to the transmission of infection [5,6]. If the potentially infected person is not controlled in a timely manner, they will go to work and travel, potentially spreading the virus to their contacts and even internationally [7,8]. Drawing on the experience of control measures for influenza A (H1N1) in 2009 [9], since the begining of the outbreak of COVID-19, the local Centers for Disease Control and Prevention (CDC) has tracked all close contacts of confirmed COVID-19 cases, investigated contact history, tested nucleic acids, and tracked health status to prevent new cases and local transmission [10]. Jing [11] and Long [12] shared the prevention and control strategy of China, namely, actively discovering and identifying close contacts, and then quarantining and monitoring them, which effectively controlled the epidemic, and enabled Wuhan to be lifted after 76 days of lockdown. This has also laid the foundation for important achievements in China's phased epidemic prevention and control.
Our previous research has shown that the main contact mode between close contacts and index cases were domesticity and transportation [13]. Although the infection risk for individuals who share public transportation with infected cases was low, the number of people on public transportation was large and it was difficult to identify all close contacts, which may cause a large number of people to be infected in this situation [14,15]. In addition, previous studies have shown that family members were also an important source of close contacts in the epidemiology of infectious disease [16]. SARS-CoV-2 was more likely to spread among family members through coughing, sneezing, or direct contact with surfaces contaminated by the virus. They spend more time at home, resulting in a higher frequency and longer duration of unprotected exposure [15], which leads to a higher risk of secondary infection through family contact [17,18].
For instance, several studies have analyzed the epidemiological characteristics of close contact. However, these studies lack the tracking and management of cross-regional personnel. The investigation presented here expected to reveal the epidemiological characteristics of close contacts under isolation and control in Chengdu and other places in China. At the same time, we analyzed the possible infection risk factors for close contact, and provided a reference basis for evaluating and optimizing epidemic prevention and control strategies.
2. Materials and methods
2.1. Data source
According to the Chinese National Health Commission in the Protocol on Prevention and Control of COVID-19 (Edition 6) [14], close contact was defined as people who had not taken effective protection and had close contact with the confirmed or suspected cases (within 1 m) within 2 days prior to illness onset or 2 days before sampling taken of the asymptomatic carriers. Once close contact was confirmed, his relevant information was entered into the “COVID-19 Close Contact Information Management System of Chengdu” and maintained and managed by relevant personnel.
Epidemiological data of COVID-19 indexed cases were collected from January 22, 2020, to March 1, 2022. Close contacts who were quarantined due to COVID-19 were selected, including close contacts of related cases in Chengdu, and those investigated and managed outside Chengdu were also included.
2.2. Personnel classifications
Close contacts mainly included family members, relatives, friends, colleagues, classmates, medical workers, and service personnel. Relatives mainly referred to family members who lived with the case and other relatives who had close contact through meals and other forms. Co-passengers refers to people who take the same transportation (airplane, train, car, ship, etc.) and have closed contact (within 1 m), which includes carers and companions (family, colleagues, friends, etc.) on the same transportation. Medical personnel included patients in the same hospital ward, medical staff, and hospital staff who had not taken appropriate protective measures. While other personnel include friends and colleagues' contact with work or social life, individuals who provide business or life services for the indicated cases, and other occasional close contacts.
2.3. Close contact management
Close contacts were subject to centralized isolation for medical observation. The medical observation period was 14 days after the last unprotected contact with indexed cases. Close contacts at the centralized observation point should be strictly managed in a single room. Those who were not suitable for centralized isolation due to age, diseases, and other reasons were subject to home quarantine for medical observation.
During the observation period, the medical staff measured their body temperature twice a day and asked their health status, whether they had a fever, chills, dry cough, shortness of breath, dyspnea, chest tightness, conjunctival congestion, diarrhea, or abdominal pain, and completed the “Medical Observation Registration Form for Close Contacts of COVID-19”. On the 1st and 14th days of isolation, the medical staff collected nasal and/or throat swab samples from close contacts for nucleic acid testing, and the frequency of testing was adjusted according to the national scheme. If the swab test was positive or any symptoms were found, close contact was sent to a designated hospital for infection evaluation and diagnosis. Individuals whose samples were negative and showed no symptoms were exempted after the quarantine period expired.
2.4. Observation index
Close contact information of COVID-19 confirmed or suspected cases and asymptomatic carriers was collected, which included basic information about close contacts, relationships with related cases, observation methods, contact methods, exposure time, outcome, sampling, and testing information. In addition, relevant indicators of local clustered epidemics in Chengdu were also analyzed.
2.5. Statistical analysis
Retrospective data and relevant information were collected and recorded through the “COVID-19 Close Contact Information Management System of Chengdu” from January 22, 2020, to March 1, 2022. Excel (Microsoft Corp, WA, USA) was used to conduct preliminary data sorting. The average value was used to supplement the missing data in some indicators. The epidemiological and contact characteristics of close contacts were analyzed by SPSS of version 22.0 software (IBM Corp, NY, USA). Continuous variables were expressed as mean ± SD, and the differences between groups were expressed by independent sample t-test. While the categorical variables were expressed as counts and percentages, the differences between groups were analyzed by the chi-square test. In addition, the odds ratio (OR) and its 95% confidence interval (95% CI) were calculated. P < 0.05 was considered to be statistically significant. The spatial distribution of close contacts was described by ArcGIS of version 10.5 software (Environmental Systems Research Institute, Redlands, CA, USA).
3. Results
3.1. Close contact control strategy
For close contact management, the confidential data were confirmed by epidemiological investigation of indexed cases or big-data platforms of public security and transportation. After verification, the main information was entered into the “COVID-19 Close Contact Information Management System of Chengdu” system and pushed to relevant districts or other regions. Subsequently, the information was exchanged with the community, streets, and other departments. Meanwhile, close contacts were transferred to the isolated hotel for centralized management. In this process, coordination with other departments should be maintained, and the implementation of close contact management and release of isolation by the hotel should be tracked. All relevant information was entered into the system and maintained and managed by relevant staff (Fig. 1).
Fig. 1.
Management strategy for COVID-19 close contacts of Chengdu.
3.2. Close contact overview
Through the epidemiological investigation of indexed cases and the push of big-data information, as of March 1, 2022, Chengdu has received a total of 49,142 close contacts. Eventually, a total of 40,425 close contacts were included in the management through the screening of suspected cases, tracking time over 14 days, and incomplete information, of which 36,353 were in Chengdu and 4072 were outside Chengdu (Fig. 2).
Fig. 2.
The process of close contacts screening.
3.3. Analysis of COVID-19 in Chengdu
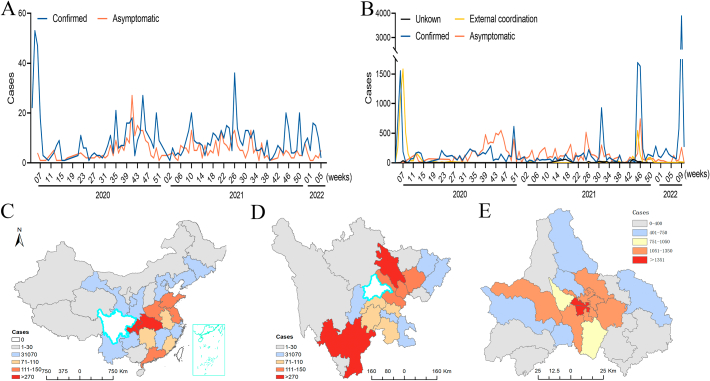
As of March 1, 2022, a total of 552 confirmed cases (67.20%) and 269 asymptomatic infection patients (32.80%) of COVID-19 were detected in Chengdu. The epidemic situation presented three peaks (Fig. 3 A). After April 2020, the cases were mainly imported from abroad (79.54%), and close contacts showed the same trend. Close contacts were mainly from confirmed cases and asymptomatic carriers, accounting for 39.20% and 39.54%, respectively (Fig. 3 B). Distribution of close contacts outside Chengdu showed dispersion from the center to the north and south (Fig. 3 C, D), while close contacts inside Chengdu showed a diffusion from the center to the surroundings (Fig. 3 E).
Fig. 3.
Distribution of close contacts. A, Time distribution of COVID-19 cases in Chengdu. B, Time distribution of close contacts. C, Distribution of close contacts in provinces of China. D, Distribution of close contacts in cities around Chengdu. E, Distribution of close contacts in Chengdu.
3.4. Basic characteristics of close contact
Among the 40,425 close contacts, 68.40% were male, with an average age of (34.26 ± 12.96) years, mainly in the 15–30-year-old age group (40.51%). No significant difference was found in the age groups between Chengdu and outside the city. The relationship between close contact and indexed cases was mainly co-passengers (57.58%) and relatives (7.20%), and the frequency of contact was mainly occasional (70.39%). A total of 37,237 (92.61%) close contacts were brought into centralized quarantine, and 40,025 (99.01%) close contacts were released from quarantine. During the centralized isolation period, a total of 400 (0.99%) closed contacts were transferred to confirmed cases or asymptomatic carriers (Table 1).
Table 1.
Basic characteristics of close contact.
Ref, reference category. Differences between groups were analyzed by chi-square test and the 95% CI were calculated.
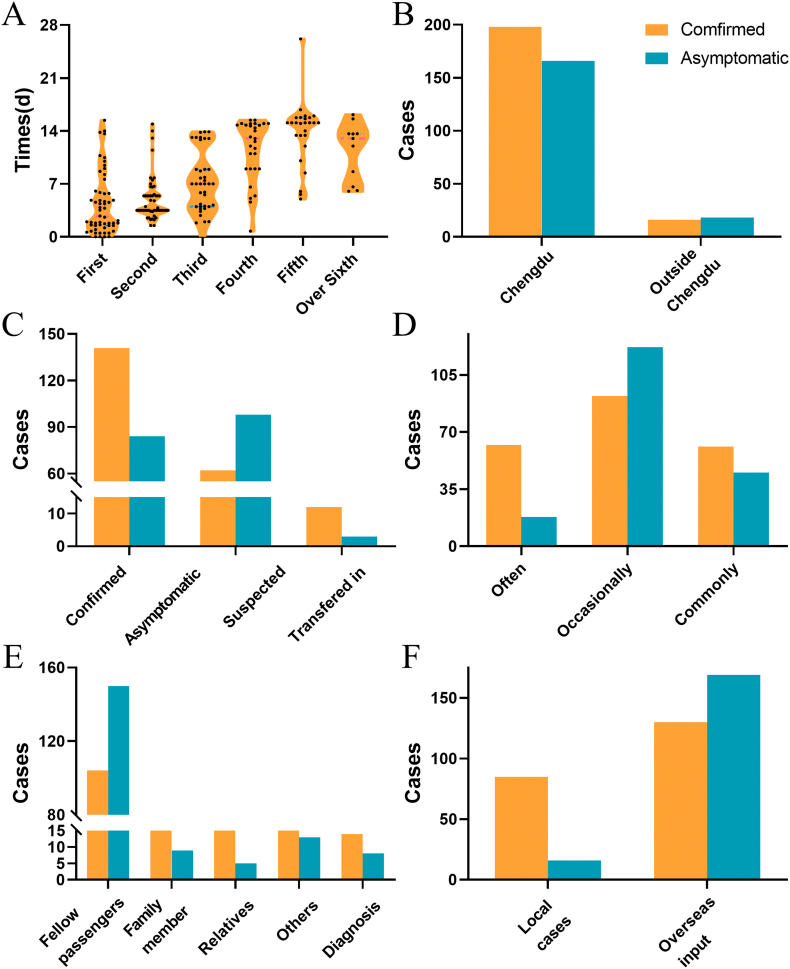
3.5. Close contacts converted to cases
A total of 400 cases were found among the close contacts, including 214 confirmed cases. The average age of the patients was 34.34 years (IQR: 25.00–41.00); 72.75% (291/400) were male. The average detection time of cases was 7.50 days, mainly in the first and second nucleic acid tests (53.69%) (Fig. 4 A). A total of 96.73% of the cases were related to contact with confirmed cases or asymptomatic infected persons (Fig. 4 C). The frequency of contact was mainly occasional contact (53.77%), which was mainly through shared transportation (63.82%) (Fig. 4 D, E). There was no significant difference in the incidence of close contacts between overseas imported patients (1.06%) and local cases (0.82%) (Fig. 4 F).
Fig. 4.
Close contacts converted to cases. A, Time detection of confirmed cases or asymptomatic infections. B, Division of close contacts transferred to cases. C, Source of transferred cases. D, Contact frequency with indexed cases. E, Relationship with indexed cases. F, Source distribution of indexed cases.
3.6. Time index comparison
Compared with close contacts outside Chengdu, the discovery time of close contacts in Chengdu was shorter ((2.11 ± 3.10) days vs. (2.62 ± 7.87) days) (Fig. 5 A). While the supposed quarantine time ((11.93 ± 3.00) days vs. (11.92 ± 7.24) days) and the actual isolation time ((13.74 ± 17.47) days vs. (12.60 ± 4.35) days) were longer, and the difference was statistically significant (P < 0.001) (Fig. 5 B, C).
Fig. 5.
Time index comparison. A, Close contact discovery time. B, Should have been quarantined time. C, Actual isolation time. Close contact discovery time = (start observation time) - (last contact time), Supposed quarantined time = (last contact time + 14 days) - (start observation time), Actual isolation time = (release isolation time) - (start observation time). Data were present as mean ± SD and analyzed by independent sample t-test. **P < 0.01, statistical difference from Chengdu.
3.7. Local epidemic analysis
After the epidemic became normalized, a total of four local clustered epidemics occurred in Chengdu. Of these, 84 cases were found, and 9239 close contacts were determined. The average age of close contact was (33.67 ± 12.96) years old, the relationship with the case was mainly colleagues (12.70%), and the frequency of contact was mainly occasional contact (74.20%). A total of 45 close contacts were converted into cases. In the four rounds of epidemics, there were no statistically significant differences in the relationship with cases, contact frequency, or isolation method, and control time (P < 0.001) (Table 2).
Table 2.
Analysis of local epidemic-related indicators (n = 9239).
| Indexes | Alternately |
H/χ2 | P | |||
|---|---|---|---|---|---|---|
| First(n = 665) | Second(n = 1031) | Third(n = 3181) | Fourth(n = 4362) | |||
| Gender | ||||||
| Male | 338 | 564 | 1900 | 2006 | 142.70 | <0.001 |
| Female | 327 | 467 | 1281 | 2356 | ||
| Age | 31.74 ± 16.81 | 35.77 ± 15.38 | 34.11 ± 14.27 | 32.72 ± 12.69 | 58.53 | <0.001 |
| Relationship with cases | ||||||
| Relative | 44 | 14 | 34 | 37 | 2726.17 | <0.001 |
| Colleague | 37 | 365 | 216 | 555 | ||
| Diagnosis | 30 | 0 | 3 | 20 | ||
| Fellow passengers | 27 | 110 | 82 | 11 | ||
| Interchange of time and space | 0 | 263 | 617 | 0 | ||
| Others | 527 | 279 | 2229 | 3739 | ||
| Management status | ||||||
| Centralized isolation | 644 | 949 | 3075 | 4294 | 288.38a | <0.001 |
| Home isolation | 18 | 9 | 15 | 57 | ||
| Hospital treatment | 2 | 4 | 3 | 10 | ||
| Others | 1 | 69 | 88 | 1 | ||
| Fate of close contacts | ||||||
| Released | 662 | 1030 | 3177 | 4325 | 25.92a | <0.001 |
| Confirmed cases | 3 | 0 | 2 | 30 | ||
| Asymptomatic | 0 | 1 | 2 | 7 | ||
| Contact frequency | ||||||
| Occasinally | 374 | 767 | 2282 | 3432 | 265.10 | <0.001 |
| General | 225 | 246 | 819 | 857 | ||
| Often | 66 | 18 | 80 | 73 | ||
| Time indexes | ||||||
| Discovery time | 3.432 ± 2.088 | 1.851 ± 1.134 | 4.043 ± 2.765 | 4.562 ± 6.305 | 150.75 | <0.001 |
| Should be quarantined | 10.58 ± 2.019 | 12.15 ± 1.140 | 9.955 ± 2.772 | 9.441 ± 6.308 | 151.14 | <0.001 |
| Actual isolation | 14.87 ± 0.9666 | 13.88 ± 2.457 | 14.80 ± 1.230 | 10.03 ± 3.551 | 17,957.73 | <0.001 |
Data were analyzed by Fisher exact probability method.
4. Discussion
Since the COVID-19 pandemic, Chengdu has carried out case investigation and disposal, close contact tracking, developed a close contact management system, and carried out the management mode of self-management and co-investigation for close contacts. To facilitate the isolation and control of close contact and understand their status, Chengdu CDC began to develop and maintain the “COVID-19 Close Contact Information Management System of Chengdu” since the beginning of the epidemic. To the best of my knowledge, this is the first city in China to establish a close contact management system, at least at the municipal level. At present, the efficient management and rapid information acquisition of the system have been recognized by Chengdu municipal government departments. Moreover, it is planned to integrate the system with the overall epidemic prevention and control platform in Chengdu and strive to promote it throughout the city. Through the circulation of indexed cases, as of March 1, 2022, Chengdu tracked and managed 40,425 close contacts. Among these, 36,353 were in Chengdu, while other cities and provinces assisted in the management of 1653 and 2419, respectively (Fig. 2).
Actually, it is a two-way management measure of close contact tracking and management. First, it helps to understand the transition states of close contact. Once a close contact was converted to a case, this may facilitate the rapid management and control of him, especially for close contact transferred to other places. Second, it is helpful to improve the feedback efficiency of the state information of close contact, and provide a reference for close contact release in time. In this study, 400 cases were found in a timely and accurate manner through the implementation of centralized medical management of close contacts, which reduced the possibility of second-generation cases, and fully demonstrated that the current management model in Chengdu is effective and feasible. Since it took a certain time to judge and analyze the close contact, and the information exchange with other regions was different from conventional communication, there was a certain time difference in time feedback, which inevitably led to the discovery time of close contact being different in Chengdu and other regions ((2.11 ± 3.10) days vs. (2.62 ± 7.87) days)(Fig. 5).
Based on the WHO and China's prevention and control management measures, Chengdu strictly controlled the community management time before April 2021. Compared with some domestic regions [19,20], the control time of close contact in Chengdu was extended by 7–14 days, which increased the possibility of finding potential cases during the isolation observation period. At the same time, according to the epidemic situation, China has continuously adjusted the prevention and control plan and increased the frequency of nucleic acid detection. Through this step, we more effectively found the possible cases and prevented the generation of second-generation cases. In this study, the secondary generation rate of close contact was 0.99%, which was lower than that in relevant studies [10,19]. In contrast to some studies [15,21], we found that 83.28% of the second-generation cases were co-passengers with indexed cases, which might be due to the different judgment methods of close contact.
Our data showed that 57.58% of close contacts had shared transportation experience with indexed cases, and 88.81% were passengers on the same flight (Table 1). Since April 2020, COVID-19 cases in Chengdu have mainly been imported from abroad. Different from local close contacts, these people have a relatively single track of activity and enter strict centralized isolation management after preliminary nucleic acid detection [22]. Moreover, with the assistance of airlines and public security, these people were easier to control. Therefore, the case discovery time was lower than that of local cases ((0.64 ± 1.21) days vs. (4.22 ± 4.88) days). Among the 400 s-generation cases, 63.75% (255/400) cases were on the same flight (Fig. 4E) and these may have been infected before departure.
It is worth noting that in most family environments, especially when COVID-19 indicated cases in the incubation period, it is difficult to achieve physical alienation and avoid direct oral communication [22]. Compared with published studies in other countries, once a confirmed case was found, the local CDC immediately isolated family contacts at designated locations, which may reduce the secondary incidence of family contacts [23]. In our study, family contacts accounted for 7.20%, and the secondary generation rate was 2.59%, which was lower than that in other cities in China (11.2%) [10] and the United States (10.5%) [24]. Due to the contact frequency between family members, reduction or neglect of personal protective equipment use, shared living and eating environment, and the continued existence of SARS-CoV-2 on different surfaces, it provides favorable conditions for the mutual spread of family members [25,26]. Therefore, in terms of management, centralized isolation should be adopted as much as possible to avoid further transmission among family members [10].
After the normalization of the epidemic situation in China, four large-scale local cluster epidemics occurred in Chengdu, and a total of 9239 close contacts were determined to be, of which 45 (0.49%) turned into cases. Given the increased transmission speed and risk of Delta virus strain, the concept of “four identical” was introduced for the judgment of close contact, that is, in the same space, same unit, same building, and with the patient four days before onset of disease was judged as close contact. Thus the range of close contacts has expanded, which may have a certain impact on the second-generation rate. Due to the unknown source of the epidemic and concealment of transmission in the early stage, these close contacts were different from an imported population from abroad. In addition, the relationship with the case was more diverse, which was mainly accompanied by colleagues (12.70%) and the interchange of time and space (9.52%).
This investigation had several limitations. As mentioned in our previous research, it is mainly reflected in information offset [13]. The reason lies in objective forgetting, subjective deliberate concealment, and incomplete information recall. At the same time, due to the presence of close contacts for >14 days, which suggested the co-investigation mechanism needs to be improved to further avoid the possibility of infection risk. In addition, we could not rule out the possibility that infected close contacts have another unknown source of infection before isolation, which may affect our conclusion to a certain extent. Furthermore, due to the lack of relevant data on vaccination before October 2020, considering the completeness of data, we did not include this part of data in the analysis. Finally, with the change in the prevention and control period, the determination and control methods of close contacts also changed, but the overall difference was small.
In summary, our present study indicates that fellow passengers and relatives were still the main sources of close contact in Chengdu. Follow-up research needs to strengthen the study on the close contact characteristics of different COVID-19 virus types, such as Delta and Omicron strains. For the government, it is necessary to continue to adhere to and optimize various scientific measures to establish risk level assessment standards for the management of close contacts.
Author contributions
Conceptualization: KY, JLD, XLT; Data creation: SFF, HL, YZ; Formal analysis: YY, ZJL; Methodology: SFF, SZ, LYW; Supervision: XLT, YY; Roles/Writing -original draft: KY, JLD; Writing - review & editing: LYW, RD.
Funding
This work was supported by the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences [grant number: 2020-PT330-005].
Declaration of Competing Interest
The authors declare there is no conflict of interest.
References
- 1.Chams N., Chams S., Badran R., Shams A., Araji A., Raad M., et al. COVID-19: a multidisciplinary review. Front. Public Health. 2020;8:383. doi: 10.3389/fpubh.2020.00383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilke L.G., Nguyen T.T., Yang Q., Hanlon B.M., Wagner K.A., Strickland P., et al. Analysis of the impact of the COVID-19 pandemic on the multidisciplinary management of breast cancer: review from the American Society of Breast Surgeons COVID-19 and mastery registries. Ann. Surg. Oncol. 2021;28(10):5535–5543. doi: 10.1245/s10434-021-10639-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paital B., Das K., Parida S.K. Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kraemer M.U.G., Pybus O.G., Fraser C., Cauchemez S., Rambaut A., Cowling B.J. Monitoring key epidemiological parameters of SARS-CoV-2 transmission. Nat. Med. 2021;27(11):1854–1855. doi: 10.1038/s41591-021-01545-w. [DOI] [PubMed] [Google Scholar]
- 5.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z., et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heymann David L., Shindo N. COVID-19: what is next for public health? Lancet. 2020;395(10224):542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China - key questions for impact assessment. N. Engl. J. Med. 2020;382(8):692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 8.Rocklov J., Sjodin H., Wilder-Smith A. COVID-19 outbreak on the diamond princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures. J. Travel Med. 2020;27(3) doi: 10.1093/jtm/taaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xinghuo Pang, Peng Yang, Shuang Li, Li Zhang, Lili Tian, Yang Li, et al. Pandemic (H1N1) 2009 among quarantined close contacts, Beijing, People’s Republic of China. Emerg. Infect. Dis. 2011;17(10):1824–1830. doi: 10.3201/eid1710.101344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu P., Ma M., Jing Q., Ma Y., Gan L., Chen Y., et al. Retrospective study identifies infection related risk factors in close contacts during COVID-19 epidemic. Int. J. Infect. Dis. 2021;103:395–401. doi: 10.1016/j.ijid.2020.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jing Q.L., Liu M.J., Zhang Z.B., Fang L.Q., Yuan J., Zhang A.R., et al. Household secondary attack rate of COVID-19 and associated determinants in Guangzhou, China: a retrospective cohort study. Lancet Infect. Dis. 2020;20(10):1141–1150. doi: 10.1016/S1473-3099(20)30471-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Long J., He R., Tian S., Luo Y., Ma M., Wang W., et al. Development and utility of a close contact information management system for the COVID-19 pandemic. BMC Public Health. 2021;21(1):2248. doi: 10.1186/s12889-021-12355-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang K., Deng J.L., Wang L., Jiang S., Lu R., Liu Z.J., et al. Tracing management and epidemiological characteristics of COVID-19 close contacts in cities around Chengdu, China. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.645798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.China OoNHCotPsRo . Clinical Infectious Diseases : an official publication of the Infectious Diseases Society of America. 2020. Notice on the Issue of Coronavirus Disease 2019 Prevention and Control Program (Trial Version 6) [Google Scholar]
- 15.Luo L., Liu D., Liao X., Wu X., Jing Q., Zheng J., et al. Contact settings and risk for transmission in 3410 close contacts of patients with COVID-19 in Guangzhou, China : a prospective cohort study. Ann. Intern. Med. 2020;173(11):879–887. doi: 10.7326/M20-2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wong J.J.M., Gan C.S., Kaushal S.H., Chuah S.L., Sultana R., Tan N.W.H., et al. Pediatric COVID-19 risk factors in Southeast Asia-Singapore and Malaysia: a test-negative case-control study. Am. J. Trop. Med. Hygiene. 2022;106(4):1113–1120. doi: 10.4269/ajtmh.21-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuba Y., Shingaki A., Nidaira M., Kakita T., Maeshiro N., Oyama M., et al. Characteristics of household transmission of COVID-19 during its outbreak in Okinawa, Japan from February to may 2020. Jpn. J. Infect. Dis. 2021;74(6):579–583. doi: 10.7883/yoken.JJID.2020.943. [DOI] [PubMed] [Google Scholar]
- 18.Park S.Y., Kim Y.M., Yi S., Lee S., Na B.J., Kim C.B., et al. Coronavirus disease outbreak in call center, South Korea. Emerg. Infect. Dis. 2020;26(8):1666–1670. doi: 10.3201/eid2608.201274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Y., Song S., Kao Q., Kong Q., Sun Z., Wang B. Risk of SARS-CoV-2 infection among contacts of individuals with COVID-19 in Hangzhou, China. Public Health. 2020;185:57–59. doi: 10.1016/j.puhe.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang L., Li Z., Liu X.X., Jiao H.T., Zhou L., Liu Q.J., et al. Analysis and evaluation of the isolation medicine observation for close contacts of coronavirus disease 2019 in Jinan City. J. Shandong Univ. (Health Sciences). 2020;58:12–16. [Google Scholar]
- 21.Kasper M.R., Geibe J.R. An outbreak of Covid-19 on an aircraft carrier. Reply. N. Engl. J. Med. 2021;384(10):976–977. doi: 10.1056/NEJMc2034424. [DOI] [PubMed] [Google Scholar]
- 22.Ng O.T., Marimuthu K., Koh V., Pang J., Linn K.Z., Sun J., et al. SARS-CoV-2 seroprevalence and transmission risk factors among high-risk close contacts: a retrospective cohort study. Lancet Infect. Dis. 2021;21(3):333–343. doi: 10.1016/S1473-3099(20)30833-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li W., Zhang B., Lu J., Liu S., Chang Z., Peng C., et al. Characteristics of household transmission of COVID-19. Clin. Infect. Dis. 2020;71(8):1943–1946. doi: 10.1093/cid/ciaa450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burke R.M., Midgley C.M., Dratch A., Fenstersheib M., Haupt T., Holshue M., et al. Active monitoring of persons exposed to patients with confirmed COVID-19 - United States, January-February 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69(9):245–246. doi: 10.15585/mmwr.mm6909e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hospital Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Madewell Z.J., Yang Y., Longini I.M., Jr., Halloran M.E., Dean N.E. Household transmission of SARS-CoV-2: a systematic review and Meta-analysis. JAMA Netw. Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31756. [DOI] [PMC free article] [PubMed] [Google Scholar]