Analysis of 995 civilian #casualties has shown that the EpiC Study population is suitable for conducting #PCC research. Based on caseloads, patient characteristics, injury profiles, and times to interventions, data from EpiC can be extrapolated to #military relevant contexts.
KEY WORDS: Trauma, prolonged care, mortality, morbidity
BACKGROUND
Civilian and military populations alike are increasingly faced with undesirable situations in which prehospital and definitive care times will be delayed. The Western Cape of South Africa has some similarities in capabilities, injury profiles, resource limitations, and system configuration to US military prolonged casualty care (PCC) settings. This study provides an initial description of civilians in the Western Cape who experience PCC and compares the PCC and non-PCC populations.
METHODS
We conducted a 6-month analysis of an ongoing, prospective, large-scale epidemiologic study of prolonged trauma care in the Western Cape (Epidemiology and Outcomes of Prolonged Trauma Care [EpiC]). We define PCC as ≥10 hours from injury to arrival at definitive care. We describe patient characteristics, critical interventions, key times, and outcomes as they may relate to military PCC and compare these using χ2 and Wilcoxon tests. We estimated the associations between PCC status and the primary and secondary outcomes using logistic regression models.
RESULTS
Of 995 patients, 146 experienced PCC. The PCC group, compared with non-PCC, were more critically injured (66% vs. 51%), received more critical interventions (36% vs. 29%), and had a greater proportionate mortality (5% vs. 3%), longer hospital stays (3 vs. 1 day), and higher Sequential Organ Failure Assessment scores (5 vs. 3). The odds of 7-day mortality and a Sequential Organ Failure Assessment score of ≥5 were 1.6 (odds ratio, 1.59; 95% confidence interval, 0.68–3.74) and 3.6 (odds ratio, 3.69; 95% confidence interval, 2.11–6.42) times higher, respectively, in PCC versus non-PCC patients.
CONCLUSION
The EpiC study enrolled critically injured patients with PCC who received resuscitative interventions. Prolonged casualty care patients had worse outcomes than non-PCC. The EpiC study will be a useful platform to provide ongoing data for PCC relevant analyses, for future PCC-focused interventional studies, and to develop PCC protocols and algorithms. Findings will be relevant to the Western Cape, South Africa, other LMICs, and military populations experiencing prolonged care.
LEVEL OF EVIDENCE
Therapeutic/care management; Level IV.

There are important parallels between prolonged civilian and combat casualty care in which the common aim is to bring effective care closer to the wounded and to provide sustained care for prolonged durations using limited resources.1,2 In civilian populations living in low- and middle-income countries specifically, prehospital delays more than 60 minutes contribute up to 20% excess mortality.3,4 Since 2008, medical evacuation in the US military has been designed to occur in less than 60 minutes (“golden hour”), thus contributing to the lowest combat mortality rate in history.2 However, in near future multidomain operations, delayed evacuations on the order of hours to days are anticipated; hence, there is a need to study prehospital and critical resuscitative care beyond conventional time periods.
Critical interventions, including essential medications and early surgical interventions, can avert death and disability.5,6 To yield the best outcomes, critical interventions, such as those needed for hemorrhage and airway control, should be initiated as soon as possible in the prehospital setting and continued upon arrival to a hospital.3,5,6 Furthermore, among patients with hemorrhage in noncompressible sites, prolonged times from injury to surgical intervention are directly associated with mortality.7–9 The recently published prolonged casualty care (PCC) guidelines define PCC as, “The need to provide patient care for extended periods of time when evacuation or mission requirements surpass available capabilities and/or capacity to provide that care.”10 Increasingly, civilian and military populations alike are faced with suboptimal operational conditions resulting in lengthy prehospital and definitive care times, putting casualties at risk for worse outcomes.2,11 Managing patients in prolonged, often resource-poor, situations requires contemporary training and care protocols that extend beyond current treatment algorithms.2 Nevertheless, a paucity of evidence-based clinical practice guidelines and protocols exists to guide patient management or to predict poor outcomes in prolonged care situations, in both civilian and military contexts.12 It is ideal, therefore, for research efforts to synergistically investigate parallels in military-civilian prolonged care and identify knowledge products that mutually benefit both populations.1
The ongoing large-scale Epidemiology and Outcomes of Prolonged Trauma Care (EpiC) study in the Western Cape of South Africa has established that the Western Cape civilian and US military PCC settings have some similarities in care capabilities, injury profiles, resource limitations, and system configurations.13–15 The EpiC study seeks to assess the effect of early trauma resuscitation on mortality and morbidity outcomes among severely injured adult patients. Importantly, the median time from injury to definitive care, measured in the EpiC cohort, is 10 hours.14 The EpiC study seeks to assess the effects of early resuscitation on postinjury mortality and morbidity in a civilian population with a high-prevalence of combat-relevant injuries.13 Findings will help fill critical scientific gaps relevant to military and civilian populations requiring PCC.16,17
The overarching purpose of this paper is to assess the suitability of the EpiC study population to conduct PCC-relevant research. We analyze the EpiC pilot data with the intent of providing an initial description of the subset of patients who experience PCC. We primarily seek to describe the patient caseload, patient characteristics, injury profiles, critical interventions, and key times of trauma casualties facing PCC within the EpiC data set. We also provide an exploratory comparison of the PCC and non-PCC cohorts.
PATIENTS AND METHODS
This is a secondary analysis of data that were prospectively collected, from March to August 2021, during the pilot phase of the EpiC study. The EpiC is a prospective multicenter observational study in the Western Cape of South Africa.
South Africa is among the countries with the highest postinjury mortality rates in the world (112 deaths per 100,000 population) and has eight times the mean mortality rate from interpersonal violence compared with the global average.18 As typical of many low- and middle-income countries, the Western Cape civilian health system is a high trauma, resource-constrained, referral-based system in which patients advance from the point of injury through a tiered system to definitive care, with prehospital care and transport provided via formal emergency medical services (EMSs). This trajectory and timeline conceptually parallel the care of those wounded in US military combat.14
The 10 sites participating in EpiC include 4 EMSs bases, 4 hospitals, and 2 forensic pathology laboratories. All sites belong to the same trauma “referral pathway” in which all patients requiring trauma, surgical, or subspecialty care receive escalating care at each facility culminating in the trauma center. The three nontrauma hospitals are deliberately located in geographically diverse and dispersed areas (dense urban, suburban, and rural) (Supplemental Digital Content, Supplementary Fig. 1, http://links.lww.com/TA/C539).13 In EpiC, demographic and clinical data are collected on included patients, defined as patients with trauma (external application of force to the body) who are 18 years and older with a clinical encounter at 1 of the 10 study sites. Exclusion criteria include prisoners, injury onset exceeding 24 hours before arrival at the first study site, stings, other forms of envenomation, toxicologic injuries, drownings, patients who are found deceased on scene, and/or patients transported via private EMSs agency.13 Data are collected by a team of trained research personnel using primary review of EMSs, hospital, and pathology records for each case. Probabilistic linking is used to link relevant clinical records as the patient traverses the trauma care system from injury to death or discharge from the hospital.19 Data are entered directly into a secure online research electronic database. The EpiC study provides a complete record from point of injury to outcomes of interest.
The primary outcome is all-cause 7-day mortality, which is defined as death in ambulance or within 7 days of injury. Patients discharged from the hospital within 7 days after injury are assumed to be alive. Secondary outcomes include hospital length of stay and organ failure assessed with the Sequential Organ Failure Assessment (SOFA) score.20 The SOFA score is calculated from the sum of points allocated from the assessment of the respiratory, cardiac, hepatic, renal, hematologic, and central nervous systems. A SOFA score of ≥5 denotes multiorgan failure and was used an indicator of morbidity (SOFA score of <5 is organ dysfunction). Sequential Organ Failure Assessment performs comparably with other trauma organ failure scores, and the data needed to compute a SOFA score are readily available in South Africa.21 In this paper, we defined PCC as at least 10 hours from injury to arrival at a definitive care facility (i.e., a hospital capable of providing definitive trauma surgical and critical care for the patient's injuries). Ten hours is a relevant cutoff time given it is the median time from injury to definitive care in this civilian setting.14 In a secondary analysis, we also present the patient characteristics using the military-relevant PCC cutoff of 4 hours or more from injury to arrival at surgically capable facility to correspond with definitions used in recent US military studies.22 To address absence of recorded injury times in the data, for individuals who are transported by EMSs, we impute injury time as the dispatch time, and for walk-ins (i.e., those who arrive without utilizing EMSs) who had a missing injury time, we stratify by critical versus noncritical injury type and impute the cohort median from the known injury times. A detailed list of EMSs and in-hospital critical interventions and medications used in this analysis are presented in Supplemental Digital Content (Supplementary Table 2A, http://links.lww.com/TA/C540, and Supplementary Table 2B, http://links.lww.com/TA/C541, respectively).
Descriptive statistics (medians, frequencies) were estimated overall and by PCC status. Comparisons of patient demographics and clinical characteristics between PCC and non-PCC patients were performed using χ2 tests for categorical variables and Wilcoxon tests for continuous variables. Logistic regression models were used to estimate odds ratios (ORs) and 95% confidence intervals for the association between PCC status and the primary and secondary outcomes. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
This study received ethics approval with a waiver of informed consent at the patient level (N20/03/036 project ID 14866). Strobe checklist was used to summarize the study findings (Supplemental Digital Content, Supplementary Data 1, http://links.lww.com/TA/C542).
RESULTS
There were 995 patients who satisfied the study eligibility criteria (Fig. 1). The median age across the study groups was 31 years, and 700 (70%) were male (Table 1). Figure 2 summarizes the elapsed median times and health system trajectory of all patients included in this study. The median time from injury to first hospital arrival was 1.9 hours (interquartile range [IQR], 1.4–2.6). The median time from injury to the first critical intervention was 3.2 hours (IQR, 2.1–5.9) postinjury. Transportation from the first hospital to definitive care by EMSs occurred on average 12.5 hours (IQR, 8.6–20.3) postinjury. At the trauma center, intensive trauma care was commenced 17.3 hours (IQR, 10.0–23.2) postinjury, and damage-control surgery was delivered at a median of 30.1 hours (IQR, 24.1–65.4) postinjury. There were 40 deaths (4%) overall, 2 prehospital and 38 in-hospital, which occurred at a median time of 10.1 hours (IQR, 3.1–56.2) postinjury.
Figure 1.

Patient enrollment flowchart.
TABLE 1.
Baseline Patient Characteristics for the Entire EpiC Study Population, and by Non-PCC Versus PCC (≥10 Hours) Subgroups
| All N = 995 |
Non-PCC n = 849 (85%) |
PCC n = 146 (15%) |
p | |
|---|---|---|---|---|
| Patient characteristics | ||||
| Age (median, Q1–Q3) | 31.5 (25.7–40.0) | 31.7 (25.5–40.0) | 30.7 (26.0–39.7) | 0.64 |
| Sex: male | 700 (70%) | 595 (70%) | 105 (72%) | 0.65 |
| Injury characteristics | ||||
| Penetrating injury | 455 (46%) | 399 (47%) | 56 (38%) | 0.053 |
| Dominant mechanism of injury: | ||||
| Firearm | 94 (9%) | 81 (10%) | 13 (9%) | |
| Struck/hit (i.e., blunt) | 196 (20%) | 168 (20%) | 28 (19%) | |
| Stabbing or cut | 312 (31%) | 273 (32%) | 39 (27%) | |
| Vehicular | 217 (22%) | 185 (22%) | 32 (22%) | |
| Fall/thermal/other | 160 (16%) | 130 (15%) | 30 (21%) | |
| Unknown | 16 (2%) | 12 (1%) | 4 (3%) | 0.45 |
| Severity measures | ||||
| TEWS score ≥ 7 | 137 (14%) | 103 (12%) | 34 (23%) | 0.0003 |
| SATS: Red | 384 (39%) | 304 (36%) | 80 (54%) | <0.0001 |
| NISS ≥15 | 138 (14%) | 93 (11%) | 45 (31%) | <0.0001 |
| AIS severity ≥ severe | 63 (6%) | 47 (6%) | 16 (11%) | 0.01 |
| GCS score ≤12 | 78 (8%) | 57 (7%) | 21 (15%) | 0.001 |
| Shock index ≥1 | 226 (23%) | 197 (23%) | 29 (20%) | 0.35 |
| Critical patient (meets any of the above severity measures) | 533 (54%) | 437 (51%) | 96 (66%) | 0.001 |
| AIS body regions with AIS severity score >1 | ||||
| Head | 256 (26%) | 158 (24%) | 98 (33%) | |
| Face | 54 (6%) | 36 (5%) | 18 (6%) | |
| Neck | 14 (1%) | 12 (2%) | 2 (1%) | |
| Thorax | 189 (20%) | 157 (23%) | 32 (11%) | |
| Abdomen | 106 (11%) | 81 (12%) | 25 (8%) | |
| Spine | 28 (3%) | 20 (9%) | 8 (3%) | |
| Upper extremity | 102 (11%) | 67 (10%) | 35 (12%) | |
| Lower extremity | 206 (21%) | 133 (20%) | 73 (25%) | |
| External | 13 (1%) | 8 (1%) | 5 (2%) | 0.0001 |
| Total | 968 (100%) | 672 (69%) | 296 (31%) | |
| Median (Q1–Q3) severity score | 3 (2–3) | 3 (2–3) | 3 (2–3) | 0.80 |
| Critical interventions received* | ||||
| Received any intervention during EMSs or at hospital, within 24 h of injury | 299 (30%) | 246 (29%) | 53 (36%) | 0.07 |
*Defined in Supplementary Tables 1A and 1B.
AIS, Abbreviated Injury Scale; GCS, Glasgow Coma Scale; NISS, New Injury Severity Score; SATS, South African Triage Scale; TEWS, Trauma Early Warning Score.
Figure 2.
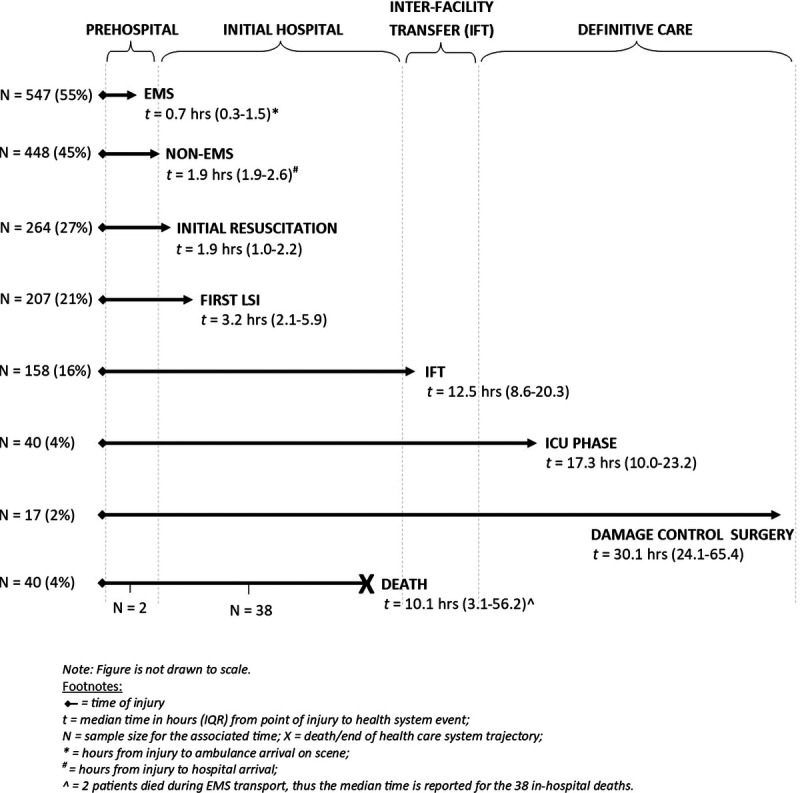
Median time (in hours) elapsed from injury to the start of key health system events for 995 trauma patients enrolled into the EpiC study from March to August 2021.
There were 146 patients (15%) who experienced PCC of at least 10 hours from time of injury until definitive care (Table 1). There was a greater proportion of penetrating injuries in the non-PCC group (47%), while the PCC group had a greater proportion of patients who were critical (i.e., higher physiologic and anatomic acuity scores, except for the shock index which was similar between groups). A greater proportion of those in the PCC compared with non-PCC group received at least one critical intervention prehospital or in-hospital (36% vs. 29%, respectively). There were 272 critical interventions performed during EMSs transport, the majority of which were breathing (44%) and circulatory interventions (42%), with fewer airway interventions (4%) or critical medications (11%) (Table 2). Prehospital interventions were mostly delivered within 1 hour of injury, whereas critical medications were delivered later, on average 2.2 hours from injury (i.e., for EMSs responses from the scene). In comparison, of the 494 in-hospital critical interventions, critical medications (51%) and breathing interventions (19%) were the most common, with a higher proportion of airway intervention (16%) than by EMSs transport. A surgical intervention was performed within the first 24 hours in 6% of cases and damage-control surgery in 4%. The median times from injury to nonoperative interventions were 2.4 to 5.2 hours, whereas operative interventions occurred later, between 5.1 and 8.9 hours postinjury.
TABLE 2.
Time From Injury to Key Clinical Intervention by PCC (≥10 Hours) and Non-PCC Subgroups of the EpiC Study
| Intervention Location | Intervention Type | PCC (n = 146) | Non-PCC (n = 849) | ||
|---|---|---|---|---|---|
| Total Interventions by Location, n (%) | Time From Injury, Median (IQR), h | Total Interventions by Location, n (%) | Time From Injury, Median (IQR), h | ||
| EMSs | Airway | 2 (4%) | 8.2 (0.6–15.8) | 6 (3%) | 0.7 (0.5–1.7) |
| Breathing | 25 (44%) | 4.5 (0.7–14.2) | 78 (36%) | 1.1 (0.7–4.5) | |
| Circulation | 24 (42%) | 0.8 (0.7–6.1) | 124 (58%) | 1.0 (0.7–1.9) | |
| Disability | 0 (0%) | N/A | 0 (0%) | N/A | |
| Medication | 6 (11%) | 11.0 (0.8–15.8) | 7 (3%) | 2.0 (0.9–2.3) | |
| Total | 57 (100%) | 215 (100%) | |||
| Nonsurgical hospital** | Airway | 0 (0%) | N/A | 3 (10%) | 1.6 (0.7–2.3) |
| Breathing | 1 (50%) | 2.4 (2.4–2.4) | 15 (52%) | 2.8 (1.9–4.0) | |
| Circulation | 0 (0%) | N/A | 1 (3%) | 23.5 (23.5–23.5) | |
| Medication | 1 (50%) | 2.1 (2.1–2.1) | 10 (34%) | 2.2 (1.6–3.2) | |
| Total | 2 (100%) | 29 (100%) | |||
| Light surgical hospital** | Airway | 15 (16%) | 3.5 (2.2–4.9) | 26 (10%) | 2.6 (1.5–3.6) |
| Breathing | 18 (19%) | 3.4 (2.2–4.9) | 62 (24%) | 2.4 (2.0–4.2) | |
| Circulation | 4 (4%) | 2.6 (1.7–3.7) | 4 (2%) | 3.8 (1.9–6.7) | |
| Medication | 48 (51%) | 3.5 (1.8–6.1) | 115 (45%) | 2.3 (1.7–4.0) | |
| Surgeries: | |||||
| DCR | 4 (4%) | 4.6 (4.3–9.0) | 11 (4%) | 3.3 (2.6–5.1) | |
| Surgical procedure* | 6 (6%) | 9.9 (4.5–20.4) | 37 (15%) | 8.7 (3.3–17.5) | |
| Total | 95 (100%) | 255 (100%) | |||
| Full surgical hospital** | Airway | 1 (25%) | 20.3 (20.3–20.3) | 11 (10%) | 2.2 (1.5–7.3) |
| Breathing | 0 (0%) | N/A | 16 (15%) | 2.2 (1.8–7.5) | |
| Circulation | 0 (0%) | N/A | 4 (4%) | 9.6 (2.4–18.5) | |
| Medication | 3 (75%) | 15.9 (12.4–22.0) | 55 (50%) | 4.5 (2.6–8.8) | |
| Surgeries: | |||||
| DCR | 0 (0%) | N/A | 10 (9%) | 12.3 (5.3–17.3) | |
| Surgical procedure* | 0 (0%) | N/A | 13 (12%) | 13.1 (8.6–13.2) | |
| Total | 4 (100%) | 109 (100%) | |||
*Surgical procedures within the first 24 hours in hospital.
**Nonsurgical hospital, Ceres Hospital; light-surgical hospital, Khayelitsha and Worcester Hospitals; full surgical hospital, Tygerberg Hospital.
DCR, damage-control surgery; N/A, not available.
Those in the PCC group were more likely to receive a critical intervention from EMSs or in hospital compared with non-PCC patients (OR, 1.40; 95% confidence interval [CI], 0.97–2.02; p = 0.08). The median time to receiving EMSs circulatory interventions was similar between PCC ≥10 hours and non-PCC patients (0.8 vs. 1.1 hours, respectively) (Table 2). Critical airway and breathing interventions, and critical medications for PCC patients occurred substantially (3–9 hours) longer than non-PCC patients, although the sample sizes were relatively small (n = 146 PCC; n = 849 non-PCC). Times to receiving critical interventions in-hospital were greater in the PCC group but to a lesser extent. The median time to receive a surgical procedure within 24 hours of hospitalization in the PCC group was 1 hour greater than the non-PCC group. The median time to receiving circulatory intervention both in EMSs and in-hospital was greater in the non-PCC group, as was time to damage-control surgery.
There was a greater proportion of 7-day mortality in the PCC ≥10 hour (4.8%) versus the non-PCC group (3.1%) (OR, 1.59; 95% CI, 0.68–3.74; p = 0.28) (table not presented). The PCC patients had a longer median hospital length of stay (3 vs. 1 day, p < 0.0001), a higher median SOFA score (5 vs. 3, p = 0.13), and greater odds of having a SOFA score of ≥5 within 7 days of injury (OR, 3.69; 95% CI, 2.11–6.42; p < 0.0001) (Table 3). In a multivariable regression model adjusting for critical versus noncritical injuries, there was no clinically meaningful effect of PCC ≥10 versus non-PCC.
TABLE 3.
Frequencies and Proportions of All EpiC Mortality and Morbidity-Related Outcomes Within 7 Days Postinjury, by Subgroups
| Outcomes | All | Non-PCC | PCC | p |
|---|---|---|---|---|
| N = 995 | n = 849 (85%) | n = 146 (15%) | ||
| 1O – Death in ambulance or within 7 d of injury, n (%)* | 33 (3.3%) | 26 (3.1%) | 7 (4.8%) | 0.28 |
| 2O – Death in ambulance or within 30 d of injury, n (%)* | 37 (3.7%) | 29 (3.4%) | 8 (5.5%) | 0.22 |
| 2O – Total hospital LOS (emergency department and in-patients) | 1 (1–3) | 1 (1–2) | 3 (2–9) | <0.0001 |
| 2O – LOS (in-patients only)** | 5 (3–11) | 4 (3–9) | 7 (3–12) | 0.003 |
| 2O – Worst SOFA score† | 4 (1–7) | 3 (1–7) | 5 (2–7) | 0.13 |
*Two non-PCC patients died during EMSs transport and were missing a mortality outcome.
**A total of 273 were admitted as in-patients (189 non-PCC and 83 with PCC).
†Of the patients, 86% were noncritical and appropriately missing a SOFA score, so medians are based on 141 individuals (100 non-PCC and 41 PCC).
1O, Primary outcome; 2O, secondary outcome; LOS, length of stay.
The patients with PCC defined as ≥4 hours (n = 260 [24%]; Supplemental Digital Content, Supplementary Table 2, http://links.lww.com/TA/C540) had similar distributions and trends of patient characteristics, injury characteristics, and severity measures as those defined using a PCC cutoff of ≥10 hours. The notable exceptions are that, while the PCC ≥4-hours cohort had a higher proportion of penetrating injuries (47%), the PCC ≥10-hours cohort (38%) had relatively more critical interventions delivered (42% vs. 36%, respectively) (Table 1; Supplemental Digital Content, Supplementary Table 2, http://links.lww.com/TA/C540). The PCC ≥4 hours had lower odds of mortality compared with the non-PCC group (OR, 0.9; 95% CI, 0.40–2.03; p = 0.80). The odds of SOFA score of ≥5 in the first 7 days was lower for PCC ≥4 hours versus non-PCC (OR, 3.18; 95% CI, 1.88–5.37; p < 0.001). In comparison with the PCC ≥10-hours definition, these ORs for mortality and SOFA score of ≥5 in the first 7 days were lower when defining PCC ≥4 hours. In concordance with the PCC ≥10-hours definition, the odds of receiving a critical intervention in EMSs or hospital was greater for the PCC ≥4 hours versus non-PCC group (OR, 2.02; 95% CI, 1.50–2.72; p < 0.001).
DISCUSSION
In our study population, PCC occurred in 15% to 25% of all cases, and patients were gravely injured, with 46% experiencing penetrating injuries, 36% critical in acuity, and a 5% mortality rate. Patients experiencing PCC had more critical injuries and had up to two times greater odds of receiving critical interventions, compared with those with non-PCC. Prehospital breathing and circulatory interventions, and in-hospital airway, breathing, and surgical interventions were commonly performed procedures in PCC situations. In terms of outcomes, those in the PCC group were admitted for longer durations in the hospital and experienced worse organ failure, as assessed by the SOFA score. There was a clinically meaningful 2% higher mortality among those with PCC.
A prior conceptual report described how the Western Cape civilian trauma profile and health care system can serve as a research equivalency model useful for studying interventions and outcomes directly relevant to military US military disrupted care situations or PCC.14 In this report, we advance that body of work by providing primary data collected during the pilot phase of the EpiC study to provide the first description of patient characteristics, injury patterns, interventions, and crude outcomes of patients experiencing PCC as a subset of the larger EpiC population.
The majority of trauma registries across the world are located in high-income countries, mostly in Europe and North America.23 In the United States, Germany, and Finland, for example, median times from injury to trauma center arrival are about 1 hour, which is substantively shorter than reported in EpiC and inadequate to study PCC.24 In addition, the US Department of Defense Trauma Registry overwhelmingly reflects care provided in non-PCC (conventional) scenarios and features very limited case series and reports of military casualties facing PCC.22,25 In low- and middle-income countries, which feature more prolonged care, trauma registries are sparse because they are challenging to implement and sustain, and where they exist, they are often constrained by limited data and often missing injury times and key resuscitative times.26,27 Limited institutional and facility-based registries exist in South Africa, which are typically restricted to academic facilities and private hospitals.28 Hence, EpiC is uniquely positioned to provide high-quality data relevant to South Africa, other low- and middle-income countries, and the US military to help advance care and policies relevant to PCC.
Although some mechanisms of injury in the Western Cape may differ from typical military trauma (e.g., blast injuries), the civilian population nonetheless is injured by many of the mechanisms seen with expeditionary and contingency military operations (e.g., firearms and stab wounds).14 The common physiology of hemorrhagic shock and traumatic brain injuries, for example, are well represented in the EpiC study and relevant to diverse trauma populations. The EpiC study will generate evidence regarding the relationship of promising interventions (e.g., tranexamic acid and blood products) with morbidity and mortality outcomes in a PCC context. Several US military and civilian studies have demonstrated improved survival with prompt neurosurgical interventions29 and blood transfusions, including one study that found that blood transfusion within 60 minutes of injury had 14% to 44% lower mortality and another that showed that 24-hour and 30-day mortality was 74% and 61%, respectively.30 However, PCC evidence is directly lacking from such studies. In our Western Cape population, the median time from injury to initiation of resuscitation was 1.9 hours, and 3.2 hours to first critical intervention. Damage-control surgery occurred much later, around 30 hours, with more than one in six patients receiving ongoing resuscitative care for more than 10 hours (the longest being 65 hours from injury). This corresponds well with the US military PCC timeframe of 4 to 72 hours.22 Despite these prolonged care situations, the 7-day mortality rate remained relatively low around 4% to 5% and comparable with other high-income country civilian trauma registry data.24 There are two potential explanations. The first is that the Western Cape trauma system is adept at providing resource-limited care for prolonged durations to sustain life until the casualty reaches definitive care. The second is a measurement artifact, that is, a selection bias imposed by the EpiC exclusion criteria. The EpiC study excludes those who arrive dead at an EpiC site (EMSs or hospital)—considering an early peak of trauma deaths exists within the first 4 hours postinjury, it is plausible that many severely injured patients simply did not reach EMSs or a hospital alive, that is, a survival bias.22 This will be further assessed in the EpiC study through a preventable mortality panel review. Notwithstanding, the comparatively favorable survival rate in EpiC is noteworthy and worthy of ongoing investigation.
Next, there is a dearth of literature reporting the association of organ failure among patients experiencing prolonged durations of resuscitation and protracted delays to definitive care. This is especially poignant among those with injury severities that are initially triaged as mild to moderate who may deliberately receive lengthier PCC and less aggressive resuscitation, only to develop sequela of their injuries several days postinjury resulting in protracted hospitalizations and disability. Crush syndrome is a classic example in which a relatively modest crush injury, upon initial assessment, can result in renal injury if there is suboptimal fluid resuscitation in the first 24 hours.31 The unadjusted organ failure estimates from this initial descriptive study show that the odds of having a high SOFA score in the first 7 days is almost four times higher in the PCC group than the non-PCC group. To our knowledge, there are no published reports assessing trends in postinjury organ failure specifically because of prolonged resuscitation. However, in the nontrauma literature, a similar trend was observed to ours in a study that compared critically ill patients with sepsis who were transferred to a tertiary care center after spending 24 hours or longer at an outside facility with those who had early triage. The authors reported that delayed transfer patients had higher SOFA scores.32 While not a traditional trauma scoring tool, SOFA was selected in EpiC by a 20-member expert panel33 as a trade-off between high feasibility of collecting the necessary clinical variables despite slightly lower performance characteristics compared with other trauma multiorgan failure scoring tools.21,34 The correlation of critical interventions with organ failure scores and trends, especially as they pertain to prolonged periods of resuscitation and delays to care, will be an ongoing area of focus in the EpiC study.
The findings of this initial descriptive study, although informative, carry several limitations. Two types of imputations were done for a large proportion of cases that were missing injury time—one for EMSs arrivals and another for non-EMSs patients. These imputations, although based on reasonable definitions, is plausible that a slightly lower proportion of patients experienced PCC; however, other administrative and research reports from the Western Cape support our timeframes.35,36 Next, there were relatively few EMSs critical interventions performed in this pilot data set, which limits the strength of those conclusions—future analyses of EpiC data will be based on larger EMSs samples to yield stronger evidence. In addition, almost one third of patient injuries were due to stab wounds, which are less representative of modern combat casualties. Last, the Western Cape civilian and US military trauma systems differ in terms of personnel capabilities, operational contexts, available resources, hospital lengths of stay, and other nuanced factors; hence, findings need to be carefully translated across contexts.
In conclusion, a subset of this South African civilian population, recruited by the EpiC study, appears to be suitable for studying prolonged care relevant to both civilians and the US military. These patients are frequently critically injured, often via penetrating trauma, and receive a diversity of critical interventions and operative interventions, yet they experience a similar in-hospital mortality rate to high-income country populations. In this cohort, casualties with longer durations of PCC have relatively worse mortality and organ failure compared with those experiencing shorter durations of PCC. The EpiC study will be a useful platform to provide ongoing data for PCC observational studies, to inform future interventional trials, and to develop PCC protocols and algorithms. This ongoing body of work will be relevant to populations in the Western Cape of South Africa and other low- and middle-income countries, as well as the combat-wounded facing prolonged evacuation and treatment.
Supplementary Material
AUTHORSHIP
N.-K.M.-M., K.S., and S.G.S. developed the study design. K.S. and B.B. conducted the primary data analyses. N.-K.M.-M., K.S., B.B., and N.K.B. drafted the initial manuscript. C.P., J.M.D., S.d.V., H.J.L., E.S., J.V., S.G.S., T.E.B., C.C., S.K., L.A.W., A.A.G., E.E.M., and V.S.B. provided key revisions and final edits.
ACKNOWLEDGMENTS
We thank the research site leads for their collaboration and support of this effort: Dr. Adeloye Adeniji, Dr. Karlien Doubell, Dr. Lesley Hodsdon, Dr. Hendrick Lategan, Dr. Denise Lourens, Dr. Suzan Mukonkole, Dr. Jeanette Verster, Dr. Shaheem de Vries, and the late Dr. Johan Dempers. We are appreciative of the Western Cape Government Department of Health of South Africa and the administrators at all study sites, for providing their institutional approvals and administrative support, respectively, required for this research study. We are thankful to several members of the US Department of Defense Joint Trauma System for offering valuable advice to strengthen the military relevance in the study approach and epidemiologic considerations.
This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Combat Casualty Care Research Program, Defense Medical Research, and Development Program under award number W81XWH1920055 and award number W81XWH2020042. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense.
DISCLOSURE
The authors declare no conflicts of interest.
The views expressed in this article are those of the authors and do not reflect the official policy or position of any listed institution, including the US Army Medical Department, US Department of the Army, US Department of Defense, or the US Government.
Footnotes
Published online: May 21, 2022.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Navneet Kaur Baidwan, Email: navneet.baidwan@cuanschutz.edu.
Brenda Beaty, Email: brenda.beaty@cuanschutz.edu.
Krithika Suresh, Email: krithika.suresh@cuanschutz.edu.
Julia M. Dixon, Email: julia.dixon@cuanschutz.edu.
Chandni Patel, Email: chandni.patel@cuanschutz.edu.
Shaheem de Vries, Email: Sdevries@pgwc.gov.za.
Hendrick J. Lategan, Email: hendrickjlategan@sun.ac.za.
Elmin Steyn, Email: esteyn@sun.ac.za.
Janette Verster, Email: jverster@sun.ac.za.
Maj Steven G. Schauer, Email: steven.g.schauer.mil@mail.mil.
Col Tyson E. Becker, Email: tyson.e.becker.mil@mail.mil.
Cord Cunningham, Email: c4.cunningham@gmail.com.
Sean Keenan, Email: sean.keenan1.ctr@mail.mil.
Ernest E. Moore, Email: Ernest.Moore@dhha.org.
Lee A. Wallis, Email: Lee.Wallis@uct.ac.za.
Adit A. Ginde, Email: adit.ginde@cuanschutz.edu.
Col Vikhyat S. Bebarta, Email: vikhyat.bebarta@cuanschutz.edu.
REFERENCES
- 1.Cohen AB, Davis M, Herman SEM. Prolonged field care research approach and its relevance to civilian medicine. Mil Med. 2021;186(5–6):123–128. [DOI] [PubMed] [Google Scholar]
- 2.Keenan S, Riesberg JC. Prolonged field care: beyond the “golden hour”. Wilderness Environ Med. 2017;28(2S):S135–S139. [DOI] [PubMed] [Google Scholar]
- 3.Shah B Krishnan N Kodish SR Yenokyan G Fatema K Burhan Uddin K, et al. Applying the Three Delays Model to understand emergency care seeking and delivery in rural Bangladesh: a qualitative study. BMJ Open. 2020;10(12):e042690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pham H, Puckett Y, Dissanaike S. Faster on-scene times associated with decreased mortality in Helicopter Emergency Medical Services (HEMS) transported trauma patients. Trauma Surg Acute Care Open. 2017;2(1):e000122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO . Guidelines for Essential Trauma Care 2004. Available at: https://www.who.int/violence_injury_prevention/publications/services/en/guidelines_traumacare.pdf. Accessed January 30, 2022.
- 6.Gauss T Ageron FX Devaud ML Debaty G Travers S Garrigue D, et al. Association of prehospital time to in-hospital trauma mortality in a physician-staffed emergency medicine system. JAMA Surg. 2019;154(12):1117–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang ZY Zhang HY Talmy T Guo Y Zhou SR Zhang LY, et al. Management of non-compressible torso hemorrhage: an update. Chin J Traumatol. 2021;24(3):125–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spahn DR Bouillon B Cerny V Coats TJ Duranteau J Fernández-Mondéjar E, et al. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Crit Care. 2013;17(2):R76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Curry N, Hopewell S, Dorée C, Hyde C, Brohi K, Stanworth S. The acute management of trauma hemorrhage: a systematic review of randomized controlled trials. Crit Care. 2011;15(2):R92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Remley M Loos P Riesberg J Montgomery H Drew B Keenan S, et al. Prolonged Casualty Care Guidelines 2021. Available at: https://jts.amedd.army.mil/assets/docs/cpgs/Prolonged_Casualty_Care_Guidelines_21_Dec_2021_ID91.pdf. Accessed Janaury 28, 2022.
- 11.Calvello EJ, Skog AP, Tenner AG, Wallis LA. Applying the lessons of maternal mortality reduction to global emergency health. Bull World Health Organ. 2015;93(6):417–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasmussen TE, Baer DG, Cap AP, Lein BC. Ahead of the curve: sustained innovation for future combat casualty care. J Trauma Acute Care Surg. 2015;79(4 Suppl 2):S61–S64. [DOI] [PubMed] [Google Scholar]
- 13.Mould-Millman NK Bebarta V Schauer SG Cunningham C Becker TE Moore EE, et al. Epidemiology and Outcomes of Combat-Relevant Prolonged Trauma Care: A Prospective Multicenter Prehospital Study in South Africa 2020–2024. University of Colorado at Denver Department of Defense, Defense Medical Research and Development Program. Funded on September 30, 2020. Available at: https://cdmrp.army.mil/search.aspx?LOG_NO=BA190049. Accessed May 26, 2022.
- 14.Mould-Millman NK Keenan S Dixon J Steyn E Lategan HJ de Vries S, et al. An innovative civilian research model to inform combat-relevant prolonged casualty care. U.S. Army Medical Journal. In press. Accepted October 14, 2021. [PubMed] [Google Scholar]
- 15.Schauer SG Long BJ Rizzo JA Walrath BD Baker JB Gillespie KR, et al. A conceptual framework for non-military investigators to understand the joint roles of medical care in the setting of future large scale combat operations. Prehosp Emerg Care. 2022;1–8. [DOI] [PubMed] [Google Scholar]
- 16.Zimmerman A Fox S Griffin R Nelp T Thomaz EBAF Mvungi M, et al. An analysis of emergency care delays experienced by traumatic brain injury patients presenting to a regional referral hospital in a low-income country. PLoS One. 2020;15(10):e0240528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitaker J O’Donohoe N Denning M Poenaru D Guadagno E Leather AJM, et al. Assessing trauma care systems in low-income and middle-income countries: a systematic review and evidence synthesis mapping the Three Delays framework to injury health system assessments. BMJ Glob Health. 2021;6(5):e004324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ. 2007;85(9):695–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sayers A, Ben-Shlomo Y, Blom AW, Steele F. Probabilistic record linkage. Int J Epidemiol. 2016;45(3):954–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cole E Gillespie S Vulliamy P Brohi K, Organ Dysfunction in Trauma (ORDIT) study collaborators . Multiple organ dysfunction after trauma. Br J Surg. 2020;107(4):402–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fröhlich M Wafaisade A Mansuri A Koenen P Probst C Maegele M, et al. Which score should be used for posttraumatic multiple organ failure? — comparison of the MODS, Denver- and SOFA- scores. Scand J Trauma Resusc Emerg Med. 2016;24(1):130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shackelford SA Del Junco DJ Riesberg JC Powell D Mazuchowski EL Kotwal RS, et al. Case-control analysis of prehospital death and prolonged field care survival during recent US military combat operations. J Trauma Acute Care Surg. 2021;91(2S Suppl 2):S186–S193. [DOI] [PubMed] [Google Scholar]
- 23.Bommakanti K, Feldhaus I, Motwani G, Dicker RA, Juillard C. Trauma registry implementation in low- and middle-income countries: challenges and opportunities. J Surg Res. 2018;223:72–86. [DOI] [PubMed] [Google Scholar]
- 24.Brinck T, Handolin L, Paffrath T, Lefering R. Trauma registry comparison: six-year results in trauma care in southern Finland and Germany. Eur J Trauma Emerg Surg. 2015;41(5):509–516. [DOI] [PubMed] [Google Scholar]
- 25.DeSoucy E Shackelford S Dubose JJ Zweben S Rush SC Kotwal RS, et al. Review of 54 Cases of Prolonged Field Care. J Spec Oper Med. 2017;17(1):121–129. [DOI] [PubMed] [Google Scholar]
- 26.Botchey IM Jr. Hung YW Bachani AM Paruk F Mehmood A Saidi H, et al. Epidemiology and outcomes of injuries in Kenya: a multisite surveillance study. Surgery. 2017;162(6S):S45–S53. [DOI] [PubMed] [Google Scholar]
- 27.Rosenkrantz L, Schuurman N, Hameed M. Trauma registry implementation and operation in low and middle income countries: a scoping review. Glob Public Health. 2019;14(12):1884–1897. [DOI] [PubMed] [Google Scholar]
- 28.Zhou J, Wang T, Belenkiy I, Hardcastle TC, Rouby JJ, Jiang B. Management of severe trauma worldwide: implementation of trauma systems in emerging countries: China, Russia and South Africa. Crit Care. 2021;25(1):286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tien HC, Jung V, Pinto R, Mainprize T, Scales DC, Rizoli SB. Reducing time-to-treatment decreases mortality of trauma patients with acute subdural hematoma. Ann Surg. 2011;253(6):1178–1183. [DOI] [PubMed] [Google Scholar]
- 30.Kotwal RS Howard JT Orman JA Tarpey BW Bailey JA Champion HR, et al. The effect of a golden hour policy on the morbidity and mortality of combat casualties. JAMA Surg. 2016;151(1):15–24. [DOI] [PubMed] [Google Scholar]
- 31.Abassi ZA, Hoffman A, Better OS. Acute renal failure complicating muscle crush injury. Semin Nephrol. 1998;18(5):558–565. [PubMed] [Google Scholar]
- 32.Loftus TJ Wu Q Wang Z Lysak N Moore FA Bihorac A, et al. Delayed interhospital transfer of critically ill patients with surgical sepsis. J Trauma Acute Care Surg. 2020;88(1):169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mould-Millman NK Mata LV Schauer SG Dixon J Keenan S Holcomb JB, et al. Defining combat-relevant endpoints for early trauma resuscitation research in a resource-constrained civilian setting. Med J (Ft Sam Houst Tex). 2021;Pb 8-21-07/08/09(Pb 8-21-07-08-09):3–14. [PubMed] [Google Scholar]
- 34.Hutchings L, Watkinson P, Young JD, Willett K. Defining multiple organ failure after major trauma: a comparison of the Denver, Sequential Organ Failure Assessment, and Marshall scoring systems. J Trauma Acute Care Surg. 2017;82(3):534–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vanderschuren M, McKune D. Emergency care facility access in rural areas within the golden hour? Western Cape case study. Int J Health Geogr. 2015;14:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Western Cape Injury Mortality Profile 2010–2016: Western Cape Government; 2018. Available at: https://www.westerncape.gov.za/assets/departments/health/mortality_profile_2016.pdf. Accessed January 30, 2022.


