Abstract
Worldwide, poultry infections by Salmonella are the cause of significant economic losses, not only due to reduced production (due to fowl typhoid disease), but also considering the efforts and control measures that must be constantly applied, especially due to zoonotic serovars. Poultry is a common reservoir of Salmonella and its transmission into the food chain is a risk for humans. The vaccination of layers plays an important role in the overall efforts to prevent Salmonella infections. An inactivated trivalent vaccine was prepared with S. Enteritidis, S. Typhimurium, and S. Infantis strains. Infection trials were performed to evaluate the efficacy of three vaccination schedules using inactivated and live S. Gallinarum 9R vaccines. For this purpose, at week 5 of life, one subcutaneous dose of live S. Gallinarum 9R vaccine (1–5 × 107 CFU) was given to Groups 1 and 2. At weeks 8 and 11 of life, chickens were also vaccinated with one (Group 1) or two (Groups 2 and 3) intramuscular doses of the inactivated oil-adjuvant trivalent vaccine (1 × 108 CFU/dose of each antigen). Group 4 consisted of chickens that remained unvaccinated (control). At week 14 of life, the efficacy of the vaccination plans was evaluated in three separate inoculation trials with S. Enteritidis, S. Typhimurium, or S. Infantis. After vaccination with the inactivated vaccine, homologous antibody production was observed, and after challenge, a significant reduction in the faecal shedding, invasion, and colonization of S. Typhimurium and S. Infantis was achieved by all vaccination schedules, while the vaccination with at least one dose of the live S. Gallinarum 9R vaccine was necessary to obtain such a significant protection against S. Enteritidis infection.
Keywords: Salmonella Enteritidis, Salmonella Typhimurium, Salmonella Infantis, inactivated vaccine, chickens
1. Introduction
Salmonella is a Gram-negative microorganism, widely dispersed in nature and often found in the intestinal tract of animals and humans [1]. There are more than 2600 serovars that differ in their antigenic formula, according to the traditional Kauffmann–White schema for the antigenic classification of salmonellae [2]. Worldwide, poultry infections by Salmonella are the cause of significant economic losses, not only due to reduced production, but also considering the efforts and control measures that must be constantly applied for human health [3]. Poultry is a common reservoir of Salmonella and its transmission into the food chain is a risk for public health [4]. Consequently, international markets have high sanitarian demands and many restrictions that apply to food safety and public health [5]. In the United States and Europe, despite these ongoing public health and regulatory efforts to prevent and control Salmonellosis, its prevalence has remained substantial. In EU countries, Salmonellosis is the second most commonly reported foodborne gastrointestinal infection in humans [6]. In the USA, non-typhoidal Salmonella spp. is responsible for 11% of all foodborne illnesses and has caused 35% of hospitalizations and 28% of total deaths [7]. S. Enteritidis is most frequently associated with egg-related outbreaks of salmonellosis, and S. Typhimurium is considered the principal causative agent of foodborne salmonellosis [8]. In Europe, these two Salmonella serovars, Enteritidis and Typhimurium, are specifically regulated in laying flocks in all member states [9]. In Argentina, S. Enteritidis and S. Typhimurium represented more than 50% of foods contaminants from 2000 to 2005, and since 2006, S. Typhimurium has been the most frequent serotype isolated from humans, animals, and foods [10]. Nevertheless, the exact cause of the predominance of these Salmonella serovars is not yet clearly understood [11]. However, in Australia, S. Infantis was the most prevalent among egg-laying flocks [12] as well as in Peru, where S. Infantis was by far the most frequently isolated serovar and a genetic association between S. Infantis strains from poultry meat and human clinical isolations was observed [13,14].
Preventing flock infection with Salmonella is a major interest not only for poultry but also to avoid the contamination of poultry products [15]. Once Salmonella is introduced into a flock of laying hens, further transmission occurs via contact with infected individuals and ingestion of faecal-contaminated materials, feed, and water [16,17,18]. The potential for contact transmission of Salmonella may be greater when birds are subjected to stress, especially during induced moulting [16,19].
By applying strict biosecurity measures, it might be possible to achieve Salmonella-free farms. These measures should include tight control of feed quality and very strict hygiene, as well as investments in the appropriate installations and equipment to avoid the infiltration of rodents, insects, and wild birds into the farm. Furthermore, multi-age rearing is not recommended as new birds are rapidly becoming infected by older ones. Nevertheless, this practice is still common in many developing countries [8,20]. Consequently, due to the high costs of the implementation of efficiency measures, it is unlikely to achieve these goals [21]. On the other hand, the widespread usage of antibiotics has led to the emergence of multiple antibiotic-resistant bacteria [22,23] and many restrictions on their use [24].
Vaccination plays an important role in biosecurity systems on chicken farms to prevent Salmonella infections [25], and it should increase the resistance of birds to infection, thus reducing horizontal transmission, faecal excretion, and the frequency of egg contamination [26]. Killed and live attenuated vaccines have been used for controlling Salmonella in poultry production with extensively proven efficacy [15,26,27]. Largely, these vaccines are commercialized, but in some South American countries, availability may vary due to local sanitarian registry processes [28,29]. Killed Salmonella vaccines greatly help to reduce S. Enteritidis prevalence when implemented in laying hens flocks. These vaccines are associated with a reduction in Salmonella load in faeces, internal tissues, and eggs as well as lower mortality, lesions, and clinical signs in different experimental models [30]. Despite the inability of inactivated vaccines to effectively elicit a protective cell-mediated immune response, and as some bacterial antigens might be lost during the inactivation, they are regarded as considerably safe and do not present any risk of introducing live vaccine strains into the food chain [26,28,31,32]. On the other hand, live vaccines stimulate cell-mediated and humoral immune responses as they often express a wider range of antigens [28,33]. These attenuated Salmonella strains contain mutations or deletions in essential genes that should result in a reduced virulence but enough to induce a protective immune response [28,31]. Certain live Salmonella vaccines can induce cross-protection between different serotypes such as the S. Gallinarum 9R strain [34], which can largely protect poultry against S. Gallinarum infections and offer protection against infections with S. Enteritidis [15,35]. Inactivated vaccines were efficient in decreasing S. Enteritidis in broiler breeders [36], and when following the combined application of both live and killed vaccines, the protection against infection exceeded the performance of either product administered separately [37,38,39]. Most of the commercial inactivated vaccines are composed of killed cells of S. Enteritidis and S. Typhimurium [31]; others include S. Infantis [39], S. Heidelberg, or even local or regional strains of a certain serovar of importance [40].
The present trials aimed to evaluate the efficacy of a trivalent inactivated vaccine prepared with antigens of S. Enteritidis, S. Typhimurium, or S. Infantis with or without an initial vaccination dose of live S. Gallinarum 9R vaccine after experimental inoculation of young layers with either S. Enteritidis, S. Typhimurium, or S. Infantis
2. Materials and Methods
2.1. Salmonella Strains
Three Salmonella strains from Peru were used; S. Enteritidis strain Q391 and S. Typhimurium strain Q782 were isolated from layers, while S. Infantis strain Q360 was isolated from broilers. These strains were used for the preparation of the Bacterin and for the experimental inoculations.
2.2. Chickens
Salmonella-free birds were used in the three trials (Table 1). One-day-old female chicks were housed immediately after hatching: in Trial 1, Hy-line chickens (Produss, Lima, Peru) while in Trials 2 and 3, Lohmann Brown chickens were used (La Camila, Entre Ríos, Argentina). Before entering the rearing facilities, every bird was wing-tagged and Salmonella-free status was confirmed by bacteriologically culturing of meconium samples from all birds. Afterwards, weekly cloacal swabs were randomly taken from ten chickens per group. These meconium samples and swabs were pooled into 40 mL of Tetrathionate broth supplemented with Brilliant Green (TB) (Oxoid, CM0029) and, after overnight incubation was sub-cultured onto XLD (Difco, 278850) + 0.46% Tergitol 4 (Sigma, 100H0494) (XLDT4) agar.
Table 1.
Vaccination and challenge. Schedule and number of birds. The chickens were vaccinated with the 9R vaccine and with the trivalent inactivated vaccine. At week 14 of life, in each trial, the chickens were inoculated by gavage into the crop with 0.5 mL of the correspondent strain.
| Group | Age of Vaccination (Weeks) | n | ||||
|---|---|---|---|---|---|---|
| Trial 1 | Trial 2 | Trial 3 | ||||
| Challenge Strain | ||||||
| 5 | 8 | 11 | S. Enteritidis | S. Typhimurium | S. Infantis | |
| 1 | 9R | - | Inactivated | 32 | 30 | 30 |
| 2 | 9R | Inactivated | Inactivated | 32 | 30 | 30 |
| 3 | - | Inactivated | Inactivated | 32 | 28 | 30 |
| 4 | - | - | - | 32 | 30 | 30 |
| Inoculation Dose (CFU) * | 1 × 107 | 4 × 107 | 6 × 107 | |||
* Colony-forming units.
2.3. Feed and Water
Animals received ad libitum Salmonella-free balanced food based on a vegetable protein diet, free from meat or fishmeal, without adding any antibiotics or coccidiostats. To ensure the absence of Salmonella spp. in feed, cultures of all batches using lactose broth were performed as previously described [41,42].
2.4. Vaccines and Vaccination
An oil-adjuvant (W/O/W), trivalent, inactivated vaccine was prepared using the three aforementioned Salmonella strains. Each strain was grown separately, inactivated with formalin 0.1% (v/v), and added to the vaccine at a final concentration of 1 × 108 colony-forming units (CFU)/dose. On the other hand, the commercial vaccine based on S. Gallinarum strain 9R (1–5 × 107 CFU/dose) also contained inactivated antigens of Escherichia coli (Inmuno Tifo C®, QUIMTIA SA, Lima, Peru).
Upon arrival, chicks were randomly distributed into four experimental groups as shown in Table 1. Birds of Groups 1 and 2 received one subcutaneous dose of the 9R vaccine at week 5 of life. Afterwards, at week 8 of life, the pullets of Groups 2 and 3 were intramuscularly vaccinated with the inactivated trivalent vaccine. Finally, at week 11 of life, all hens of Groups 1, 2, and 3 were vaccinated intramuscularly with the inactivated trivalent vaccine. The birds of Group 4 remained unvaccinated and were used as the negative control.
2.5. Preparation of the Inoculum and Avianization
Each Salmonella strain was thawed from liquid nitrogen and cultured onto an XLDT4 agar plate. After overnight incubation at 37 °C, one colony was used to seed a Brain Heart Infusion broth (BHI) (Oxoid, CM1135), which was incubated overnight at 37 °C. Before the beginning of the trials, the virulence of the three Salmonella strains was enhanced as previously described [43,44]. Briefly, each strain was inoculated by gavage into the crop using two Salmonella-free one-day-old chicks. After two days, these chicks were euthanized, and their livers and spleens were cultured onto XLDT4 plates that were processed as before. For standardization of the proceedings, the growth from the agar plates was collected, aliquoted, and kept frozen in liquid nitrogen until used.
2.6. Bacteriology
In all trials, individual cloacal swabs were cultured in 5 mL TB that was incubated for 48 h at 37 °C. After euthanasia, livers and spleens were macerated and diluted 1:1 (w/v) using sterile BHI, while caecum contents samples were diluted 1:2 (w/v) using TB in sterile plastic bags. After homogenizations, five log10 dilutions were prepared for each sample using BHI (for livers and spleens) or TB (for caecum content), which were incubated overnight for 48 h, respectively, at 37 °C. After incubation, all tubes were vortexed and subcultured onto XLDT4 agar plates as before. The presence of the challenge strain was registered for each tube.
2.7. Pre Trials
To establish the minimum infective dose 100% of each strain, a pre-trial was conducted. For each Salmonella strain, an inoculum was prepared as above, and two log10 dilutions (1:10 and 1:100) were prepared in sterile BHI. These dilutions were used to inoculate fifteen 12-week-old birds that were divided into three groups of five birds each. These birds were orally inoculated by gavage into the crop with 0.5 mL of one of the correspondent dilutions. On day 3 (Trials 2 and 3) or days 3 and 5 (Trial 1) post-inoculation, all birds were sampled by cloacal swabbing and euthanized. Livers and spleens were cultured as before. The results from the pre-trials are shown in Table S1.
2.8. Experimental Infections with Salmonella
Three infection trials were conducted. At week 14 of life, the hens were orally inoculated with the correspondent Salmonella strain with 0.5 mL of the inoculum by gavage into the crop (Table 1).
2.9. Cloacal Swabbing and Samplings
Individual cloacal swabs were taken from all birds on days 3, 6, 9, 12, and 15 post-challenge. In Trial 1, cloacal swabs were also taken on days 2, 4, and 7 post-challenge. Each swab was deposited into a tube containing 3 mL TB that was cultured as before. On days 3, 6, 9, 12, and 15 post-challenge, five (Trial 1) or six (Trials 2 and 3) birds from each group were sacrificed by decapitation. Livers, spleens, and caecum contents were cultured as above (without dilutions). Positive/negative results were recorded.
2.10. Serology
Blood samples were taken before the first vaccination at week 5 of life and approximately every 10 days until week 14 of life when birds were challenged. Thereafter, in Trial 1, blood samples were taken on day 15 post-challenge, while in Trials 2 and 3, blood samples were taken on days 3, 6, 9, 12, and 15 post-challenge. Blood was taken from the wing veins of the chickens using 2.5 mL syringes and 30G needles [45] and transferred into 5 mL plastic tubes. Afterwards, sera were separated and kept frozen at −20 °C in 1.5 mL tubes until usage. Tittering of anti-Salmonella antibodies was evaluated using ELISA kits Salm Gp D (https://www.biochek.com/poultry-elisa/salmonella-group-d-antibody-test-kit/ accessed on 30 June 2022) and Salm Gp B (https://www.biochek.com/poultry-elisa/salmonella-group-b-antibody-test-kit/, accessed on 30 June 2022, Biochek, Scarborough, ME, USA) specific for S. Enteritidis (Trial 1) and S. Typhimurium (Trial 2), respectively. On the other hand, in Trial 3, the anti-Salmonella antibodies titres in sera were evaluated by the micro-agglutination test (MAT) [46,47,48]. For that purpose, the S. Infantis was cultured in BHI broth, inactivated, centrifuged, resuspended in PBS + Thimerosal (0.01%), and adjusted to a final concentration of 1 × 109 bacteria/mL (0.5 at OD600m). Afterwards, sera samples were diluted at 1:10 and ten Log2 dilutions were prepared and incubated (overnight at 37 °C) with the inactivated antigen. Titres were calculated as the highest log2 dilution with a positive reaction.
2.11. Statistics
The chi-square test of independence was performed to compare de re-isolation rates of Salmonella sp. among the four experimental groups in each trial (significance level α = 0.05).
2.12. Animal Welfare
Handling of birds was performed according to the Guide for the Care and Use of Laboratory Animals [49], and euthanasia was performed according to the American Veterinary Medical Association’s Manual for euthanasia [50]. The performance of these trials was previously evaluated and approved by the Regional Council of the National Institute for Agro-Technology (CICUAE INTA CeRBAS), and the trials were performed accordingly (approvals numbers 01815 and 05016).
3. Results
3.1. Cloacal Swabs
The recovery rates of the challenge strains in the three trials are shown in Table 2. In Trial 1, significantly more cloacal swabs from the unvaccinated birds (Group 4) were positive for the challenge strain (140 positive swabs out of 191) in comparison with the other groups, with 124, 63, and 107 positive swabs from Groups 1, 2, and 3, respectively, which were also statistically different. Similarly, in trials 2 and 3, significantly more cloacal swabs from the unvaccinated birds (Group 4) were positive for the challenge strain (17/90 and 23/90, respectively) in comparison with the other groups in the same trial. In trial 2, only one positive swab (out of 81 samples) was obtained from birds of group 3, significantly lower than the ones from groups 1 and 2 (7/90 each). Furthermore, in trial 3, no statistical differences were found among groups 1, 2, and 3 (5/90, 3/90, and 5/90, respectively). Information about the daily results of samplings is available in Supplementary Table S2.
Table 2.
Cloacal swabs. Cloacal swabs were taken from all birds on days 3, 6, 9, 12, and 15 post-challenge. In Trial 1, cloacal swabs were also taken on days 2, 4, and 7 post-challenge.
| Group | Number of Positive Cloacal Swabs Samples | ||
|---|---|---|---|
| Trial 1 | Trial 2 | Trial 3 | |
| S. Enteritidis | S. Typhimurium | S. Infantis | |
| 1 | 124/191 a | 7/90 a | 5/90 a |
| 2 | 63/191 b | 7/90 a | 3/90 a |
| 3 | 106/191 c | 1/81 b | 5/90 a |
| 4 | 140/191 d | 17/90 c | 23/90 b |
a,b,c,d Isolation rates in the same column (trial) without common superscripts differ statistically using the chi2 test (p < 0.05).
3.2. Salmonella Recovery from Livers, Spleens, and Caecum Contents
The recovery rates from livers, spleens, and caecum content and the number of positive birds are presented in Table 3, while more information is available in Supplementary Table S3.
Table 3.
The total isolation rates of S. Enteritidis, S. Typhimurium, or S. Infantis from livers, spleens, and caecum contents after challenge. Samples were taken from five (Trial 1) or six (Trials 2 and 3) birds of each group on days 3, 6, 9, 12, and 15 post-challenge. A chicken was considered positive if at least one sample was positive.
| Number of Trial/Salmonella Strain | Group | n | Number of Positive Samples | Number of Positive Birds | |||
|---|---|---|---|---|---|---|---|
| Liver | Spleen | Caecum Contents | Total | ||||
| Trial 1 Salmonella Enteritidis | 1 | 25 | 8 a | 13 a | 20 ab | 41 a | 21 a |
| 2 | 25 | 7 a | 8 a | 15 a | 30 b | 18 a | |
| 3 | 25 | 18 b | 22 b | 22 b | 62 c | 23 ab | |
| 4 | 25 | 17 b | 24 b | 23 b | 64 c | 25 b | |
| Trial 2 Salmonella Typhimurium | 1 | 30 | 1 a | 1 a | 5 a | 7 a | 6 a |
| 2 | 30 | 2 a | 0 a | 4 a | 6 a | 6 a | |
| 3 | 28 | 4 a | 7 b | 6 a | 17 b | 11 a | |
| 4 | 30 | 10 b | 20 c | 13 b | 43 c | 23 b | |
| Trial 3 Salmonella Infantis | 1 | 30 | 3 a | 10 a | 13 a | 26 a | 18 a |
| 2 | 30 | 1 a | 8 a | 7 a | 16 a | 13 b | |
| 3 | 30 | 6 ab | 7 a | 6 a | 19 a | 13 b | |
| 4 | 30 | 13 b | 26 b | 23 b | 62 b | 29 c | |
a,b,c Isolation rates and the number of positive birds in the same column (for each trial) without common superscripts differ statistically using the Chi2 test (p < 0.05).
Trial 1. Significantly fewer positive livers and spleens from Groups 1 and 2 were found in comparison with those from Groups 3 and 4, which did not statistically differ among themselves. Similarly, fewer caecum contents from Group 2 were positive in comparison with those from Groups 3 and 4, which did not statistically differ among themselves. The recovery rate of S. Enteritidis from caecum contents in Group 1 did not differ statistically from the other three experimental groups. Overall, significantly fewer positive samples (30/75) were obtained from birds of Group 2 in comparison with the other three groups, followed by Group 1 (41/75), which was significantly lower in comparison with Groups 3 and 4 (62/75 and 64/75, respectively), which did not statistically differ among themselves. Furthermore, all of the chickens from Group 4 were positive, significantly more so than Groups 1 and 2. In Group 3, the number of positive birds did not statistically differ from the other groups.
Trial 2. Significantly more livers, spleen and caecum contents from Group 4 were positive in comparison with the other three vaccinated groups, which did not statistically differ among themselves, except for Group 3, which had significantly more positive spleens in comparison with Groups 1 and 2. The total recovery rate of Salmonella from all samples from birds of Group 1 (7/90) and Group 2 (6/90) did not statistically differ among themselves but were significantly lower in comparison with Group 3 (17/84), which was also significantly lower than the total recovery of S. Typhimurium from birds of Group 4 (43/90). All vaccinated groups presented significantly fewer positive birds in comparison with the unvaccinated Group 4.
Trial 3. Significantly more livers, spleen and caecum contents from Group 4 were positive in comparison with the other three vaccinated groups, which did not statistically differ among themselves, except for the livers from Group 3 that did not differ from the other groups. Overall, significantly more positive samples from the unvaccinated Group 4 (62/90) were recovered in comparison with the other three groups. In addition, there were more positive birds in the unvaccinated group in comparison with all of the vaccinated groups, while in Group 1, the number of positive birds was significantly higher than in Groups 2 and 3.
3.3. Serology
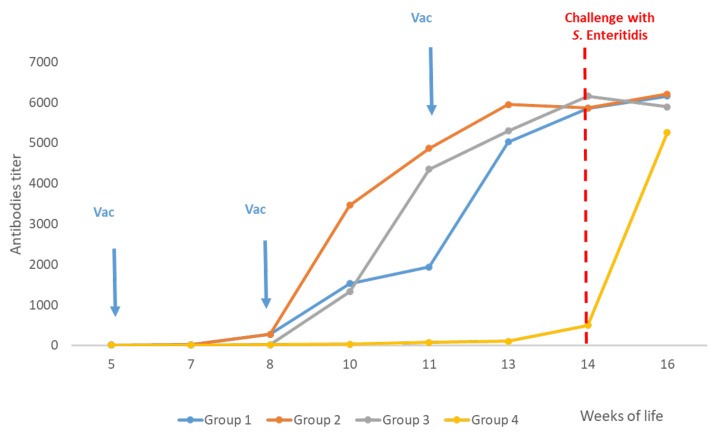
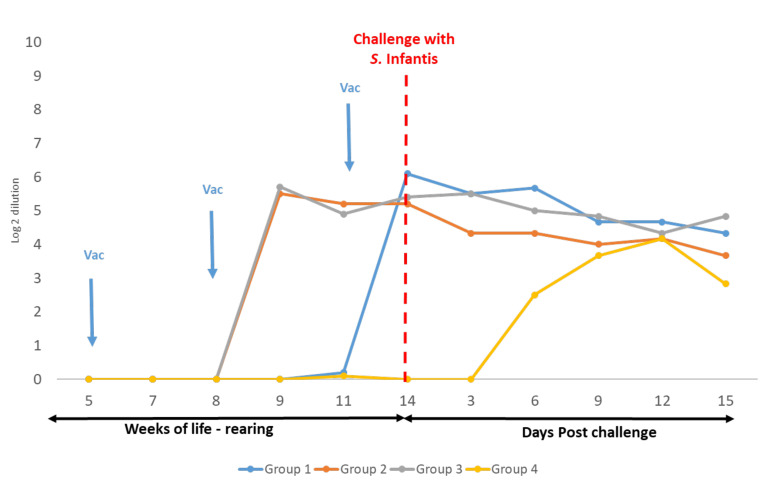
The ELISA results for Trials 1 and 2 are presented in Figure 1 and Figure 2, respectively, and MAT results for Trial 3 are available in Figure 3.
Figure 1.
Trial 1—Antibodies titres. Measurements of antibody titres in vaccinated and non-vaccinated chickens. Challenge with S. Enteritidis (SE) was carried out in week 14 of life (red line). Blood samples were taken approximately every 10 days starting at week 5 until week 16 of life (two weeks post-challenge) when all birds were euthanized. Sera were analysed by ELISA (Salm Gp D, Biochek).
Figure 2.
Trial 2—Antibodies titres. Measurements of antibody titres in vaccinated and non-vaccinated chickens. Challenge with S. Typhimurium (ST) was carried out in week 14 of life (red line). Blood samples were taken approximately every 10 days starting at week 5 of life, and after the challenge, samples were taken every three days until day 15 post-challenge, when all birds were euthanized. Sera were analysed by ELISA (Salm Gp B, Biochek).
Figure 3.
Trial 3—Micro-agglutination test (MAT). Measurements of titres in vaccinated (Groups 1, 2, and 3) and non-vaccinated (Group 4) chickens. Blood samples were taken approximately every 10 days starting at week 5 of life. Ten Log2 dilutions of each serum were incubated with antigens of S. Infantis. Antibody titres were calculated as the highest log2 dilution that reacted.
In Trials 1 and 2, the vaccination at week 5 of life with the live vaccine of Salmonella Gallinarum 9R caused a very low production of antibodies against S. Enteritidis or S. Typhimurium, respectively, which was evidenced only from week 10 of life (Group 1). Nevertheless, in Trial 3, a similar presence of antibodies against S. Infantis was not observed by MAT in this group.
On the other hand, in all trials, 10 days after the first vaccination with the inactivated vaccine at week 8 of life, antibody titres were detected in Groups 2 and 3. Similarly, in all trials, after the second vaccination with the inactivated vaccine at week 11 of life, homologous antibodies titres were also detected in Group 1. In Trials 1 and 3, on day 15 post-challenge, antibodies titres against S. Enteritidis or S. Infantis, respectively, from the unvaccinated chickens (Group 4) were similar to the three vaccinated groups. On the contrary, in Trial 2, antibodies against S. Typhimurium were very low in blood samples from the unvaccinated chickens taken after the challenge.
4. Discussion
Salmonella control in poultry farms should be based on the application of strict biosecurity measures. These include major efforts in controlling housing conditions, feed quality, strict hygiene, plagues control, contact with wildlife animals, and, where possible, avoiding multi-age rearing [8,20]. In many countries, these measures are too expansive and are not being implemented [21]. Vaccination against Salmonella-nonspecific host serovars was reported with variable success rates. Inactivated vaccines produce good immune responses but generally lack cross-protection against other serovars [37]. While vaccination with homologous serovars can show cross-protection within the same serologic group [51], multivalent inactivated vaccines, prepared from a mixture of strains from different serovars, provide an expanded spectrum of protection [39,52].
In South American countries, layers are commonly vaccinated with the 9R vaccines against fowl typhoid caused by S. Gallinarum [10]. Furthermore, cross-protection by the 9R vaccine against S. Enteritidis was reported as both serovars belong to the same serogroup [53]. The vaccination schedules that were tested in the present study consisted of vaccination with the live S. Gallinarum 9R in week 5 of life in combination with one or two doses of the inactivated trivalent vaccine in weeks 8 and 11 of life (Groups 1 and 2, respectively). Usually, vaccination with the 9R vaccine is administered at 8 weeks of age, but this vaccine could be administered as early as 4 weeks of life [54,55]. In the present study, vaccination with the 9R vaccine was administered at week 5 of life and no negative effects were observed, nor was the excretion of the vaccine strains detected in faecal samples.
Killed vaccines were associated with decreased incidences of S. Enteritidis infection in Dutch broiler breeder flocks and S. Enteritidis contamination in eggs from Japanese laying flocks [35,56]. In Trial 1, to obtain a significant reduction in the invasion and colonization of S. Enteritidis, the use of the live S. Gallinarum 9R vaccine with the addition of at least one dose of the inactivated trivalent vaccine was required. Nevertheless, there was a significant reduction in the number of samples positive for S. Typhimurium and S. Infantis (Trials 2 and 3, respectively) in comparison with the unvaccinated birds. This reduction was also observed in the number of positive birds (that had at least one positive sample after euthanasia). Furthermore, the protection afforded by two doses of the inactivated vaccine (Group 3) was good enough even without the previous vaccination with the live S. Gallinarum 9R vaccine (Groups 1 and 2). These results should not be surprising, as the use of the 9R vaccine did not protect against intestinal colonization by S. Typhimurium or S. Infantis [57]. In a similar trial, performed by Deguchi et al. (2009), using an inactivated vaccine with the same three Salmonella serovars, there was also a reduction in the number of S. Enteritidis, S. Typhimurium, S. Infantis, and S. Heidelberg from faeces, caecum colonization, and organ invasion. Nevertheless, the S. Enteritidis that was used was isolated from humans [39].
Environmental contamination, including floors, feeders, and drinkers is a result of the faecal shedding of Salmonella by infected hens [58]. In the present trials, the three vaccination schedules were helpful in significantly reducing the excretion of Salmonella, and thus contributing to the reduction in the dissemination of Salmonella on farms. El-Enbaawy et al. [47] used bivalent (S. Enteritidis and S. Typhimurium) and polyvalent (S. Enteritidis, S. Typhimurium, S. Infantis, and S. Meleagridis) inactivated vaccines and obtained a significant reduction in Salmonella excretion after a simultaneous challenge with these four serovars.
In the present trials, antibody production was evidenced after vaccination with the inactivated vaccines during rearing. These were measured by ELISA in Trials 1 and 2, showing the efficiency of the inactivated vaccine to produce antibodies against S. Enteritidis y S. Typhimurium, respectively. As no commercial ELISA was available for the detection of antibodies against S. Infantis, the blood samples from Trial 3 were processed by the MAT technique. This technique is not as accurate as ELISA, but it provides a good qualitative tool to compare the levels of antibody production among different vaccination schedules. Furthermore, it has some advantages of savings in time, space, and cost [46]. It was revealed that the inactivated vaccine enabled the production of antibodies against S. Infantis with similar levels that were detected by ELISA against S. Enteritidis and S. Typhimurium. After the challenge, in the three trials, homologous antibodies were produced in the unvaccinated birds. In Trials 1 and 3, the antibody titres of unvaccinated chickens against S. Enteritidis and S. Infantis, respectively, reached similar levels of antibodies in comparison with the vaccinated chickens. Hence, it was shown that the three vaccination schedules were efficient for producing enough antibodies, similar to the levels of antibodies that may be produced by the chickens when a pathogenic strain is introduced. Differently, after challenge with S. Typhimurium, the titres of antibodies in unvaccinated chickens were lower in comparison with the other vaccinated chickens (Trial 2). This is probably because more time was needed to reach the same levels of antibodies.
Under the conditions of this study, the results suggest that the inactivated trivalent Salmonella vaccine can be an effective tool for controlling S. Typhimurium and S. Infantis. It has also contributed to significantly reducing the excretion of S. Enteritidis. Nevertheless, the combination of the live 9R vaccine with at least one dose of the inactivated triple Salmonella vaccine filled this gap of protection against S. Enteritidis, achieving a significant reduction in faecal shedding. Furthermore, the use of one dose of the 9R vaccine with only one dose of the inactivated vaccines might be effective, and thus help to reduce the costs of vaccinations, especially in countries where high costs of vaccination might be a limiting factor.
Future trials should include challenges with pathogenic S. Gallinarum. It might also be interesting to compare the inactivated vaccine, which was prepared with local Peruvian strains, with other available inactivated multivalent vaccines that are prepared with international strains. Field trials in poultry farms with a history of Salmonella can also be included and may shed more light on the efficacy and duration of protection as well as antibodies production during the egg production period.
Acknowledgments
The authors wish to thank Abel Gulle and Cristian Gulle (INTA Balcarce, Argentina) for their assistance in the rearing of the birds and maintenance of the experimental units in INTA Balcarce. The authors also wish to thank Pablo Chacana from CICVyA (Buenos Aires, Argentina) for his guidance in using the microagglutination tests.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines10071113/s1, Table S1: Pre-trials to establish the minimum infective dose 100%, Table S2: Cloacal swabs, Table S3: The number of positive samples of livers, spleens, and caecum contents after challenges at week 14 of life in three experimental infection trials.
Author Contributions
Conceptualization, Y.D.H., M.C.-G. and A.M.-E.; Data Curation, Y.D.H., R.M., R.R., J.L.-G. and M.C.-G.; Formal Analysis, Y.D.H., S.A. and A.M.-E.; Investigation and Methodology, Y.D.H., M.C.-G., R.R., S.A., L.H.O., R.M., J.L., P.N., P.C., J.L.-G. and A.M.-E.; Funding Acquisition, Y.D.H., M.C.-G. and A.M.-E.; Project Administration, Y.D.H., M.C.-G. and A.M.-E.; Resources, Y.D.H., M.C.-G. and A.M.-E.; Supervision, Y.D.H., M.C.-G. and A.M.-E.; Validation, Visualization, Y.D.H. and A.M.-E.; Writing—Original Draft Preparation, Y.D.H. and A.M.-E.; Writing—Review and Editing, Y.D.H. and A.M.-E. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Handling of birds was performed according to the Guide for the Care and Use of Laboratory Animals [49], and euthanasia was performed according to the American Veterinary Medical Association’s Manual for euthanasia [50]. The performance of these trials was previously evaluated and approved by the Regional Council of the National Institute for Agro-Technology (CICUAE INTA CeRBAS), and the trails trials were per-formed accordingly (approvals numbers 01815 and 05016).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. These trials were conducted at the I&D Department of Quimtia SA (Lima, Peru) and at the laboratory of bacteriology of INTA EEA Balcarce (Balcarce, Buenos Aires, Argentina). All authors are employees of Quimtia SA or INTA. These trials were performed under a Technical Assistance Agreement between Quimtia SA and INTA (Balcarce, Argentina)-CAT#25101.
Funding Statement
These trials were conducted at the I&D Department of QUIMTIA SA Lima, Peru and in the Laboratory of Bacteriology of INTA Balcarce, Argentina under a Technical Assistance Agreement between QUIMTIA SA and INTA (CAT#25101). This research was funded by Quimtia S.A.—ProCiencia—CONCYTEC: Contrato N° 033-2019-Fondecyt-BM-INC.INV.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mahmoud B.S.M. In: Salmonella—A Dangerous Foodborne Pathogen. Barakat S.M.M., editor. InTech; Rijeka, Croatia: 2012. [Google Scholar]
- 2.Zou Q., Li R., Liu G., Liu S. Genotyping of Salmonella with Lineage-Specific Genes: Correlation with Serotyping. Int. J. Infect. Dis. 2016;49:134–140. doi: 10.1016/j.ijid.2016.05.029. [DOI] [PubMed] [Google Scholar]
- 3.Frenzen P.D., Riggs T.L., Buzby J.C., Breuer T., Roberts T., Voetsch D., Reddy S., FoodNet Working Group Salmonella Cost Estimate Updated Using FoodNet Data. FoodReviews. 1999;22:10–15. doi: 10.1128/AAC.03728-14. [DOI] [Google Scholar]
- 4.Batz M., Hoffmann S., Morris J.G. Disease-Outcome Trees, EQ-5D Scores and Estimated Annual Losses of Quality-Adjusted Life Years (QALYs) for 14 Foodborne Pathogens in the United States. Foodborne Pathog. Dis. 2014;11:395–402. doi: 10.1089/fpd.2013.1658. [DOI] [PubMed] [Google Scholar]
- 5.Gast R.K. Salmonella Infections. In: Saif Y., Fadly A., Glisson J., McDougald L., Nolan L., Swayne D., editors. Diseases of Poultry. Blackwell Publishing; Athens, GA, USA: 2008. pp. 619–674. [Google Scholar]
- 6.EFSA The European Union One Health 2020 Zoonoses Report. EFSA J. 2021;19:e06971. doi: 10.2903/j.efsa.2021.6971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scallan E., Hoekstra R.M., Angulo F.J., Tauxe R.V., Widdowson M.A., Roy S.L., Jones J.L., Griffin P.M. Foodborne Illness Acquired in the United States-Major Pathogens. Emerg. Infect. Dis. 2011;17:7–15. doi: 10.3201/eid1701.P11101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gast R.K. Microbiology of Shell Egg Production in the United States. In: Ricke C., Gast R.K., editors. Producing Safe Eggs: Microbial Ecology of Salmonella. Academic Press; London, UK: 2017. pp. 25–44. [Google Scholar]
- 9.EC Regulation (EC) No 2160/2003 of the European Parliament and of the Council. Off. J. Eur. Union. 2003;2003:1–15. [Google Scholar]
- 10.Bueno D.J., Soria M.A., Soria M.C., Procura F., Rodriguez F.I., Godano E.I. Egg Production Systems and Salmonella in South America. In: Ricke S.C., Gast R.K., editors. Producing Safe Eggs—Microbial Ecology of Salmonella. Academic Press—Nikki Levy; London, UK: 2017. pp. 87–110. [Google Scholar]
- 11.Gomez-Aldapa C.A., del Torres-Vitela R.M., Villaruel-Lopez A., Castro-Rosas J. The Role of Food in Salmonella Infections. In: Mahmoud B.S.M., editor. Salmonella—A Dangerous Foodborne Pathogen. InTech; Rijeka, Croatia: 2012. pp. 17–31. [Google Scholar]
- 12.Cox J., Woolcock J., Sartor A. In: The Significance of Salmonella, Particularly S. Infantis, to the Australian Egg Industry. Cox J.M., Woolcock J.B., Sartor A.L., editors. RIRDC Web Publication; Sydney, Australia: 2002. [Google Scholar]
- 13.Zamudio M.L., Meza A., Bailón H., Martinez-Urtaza J., Campos J. Experiencias En La Vigilancia Epidemiológica de Agentes Patógenos Transmitidos Por Alimentos a Través de Electroforesis En Campo Pulsado (PFGE) En El Perú. Rev. Peru. Med. Exp. Salud Publica. 2011;28:128–135. doi: 10.1590/S1726-46342011000100020. [DOI] [PubMed] [Google Scholar]
- 14.Walderama W., Quevedo M., Pastor J., Mantilla Y., Ortiz M. Estudio de Prevalencia de Serotipos de Salmonella En Granjas Avícolas Tecnificadas En El Perú—Parte 1. MAP. 2014;5:50–58. [Google Scholar]
- 15.Revolledo L., Ferreira A.J.P.P. Current Perspectives in Avian Salmonellosis: Vaccines and Immune Mechanisms of Protection. J. Appl. Poult. Res. 2012;21:418–431. doi: 10.3382/japr.2011-00409. [DOI] [Google Scholar]
- 16.Holt P.S., Mitchell B.W., Gast R.K. Airborne Horizontal Transmission of Salmonella Enteritidis in Molted Laying Chickens. Avian Dis. 1998;42:45–52. doi: 10.2307/1592575. [DOI] [PubMed] [Google Scholar]
- 17.Holt P.S. Horizontal Transmission of Salmonella Enteritidis in Molted and Unmolted Laying Chickens. Avian Dis. 1995;39:239–249. doi: 10.2307/1591865. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura M., Takagi M., Takahashi T., Suzuki S., Sato S., Takehara K. The Effect of the Flow of Air on Horizontal Transmission of Salmonella Enteritidis in Chickens. Avian Dis. 1997;41:354–360. doi: 10.2307/1592189. [DOI] [PubMed] [Google Scholar]
- 19.Palermo-Neto J., Quinteiro-Filho W.M., Ribeiro A., Ferraz-de-Paula V., Pinheiro M.L., Baskeville E., Akamine A.T., Astolfi-Ferreira C.S., Ferreira A.J.P., Gomes A.V. Overcrowding Stress Decreases Macrophage Activity and Increases Salmonella Enteritidis Invasion in Broiler Chickens. Avian Pathol. 2014;40:e30–e31. doi: 10.1016/j.bbi.2014.06.124. [DOI] [PubMed] [Google Scholar]
- 20.Davies R.H., Breslin M. Persistence of Salmonella Enteritidis Phage Type 4 in the Environment and Arthropod Vectors on an Empty Free-Range Chicken Farm. Environ. Microbiol. 2003;5:79–84. doi: 10.1046/j.1462-2920.2003.00387.x. [DOI] [PubMed] [Google Scholar]
- 21.Zhang-Barber L., Turner A.K., Barrow P.A. Vaccination for Control of Salmonella in Poultry. Vaccine. 1999;17:2538–2545. doi: 10.1016/S0264-410X(99)00060-2. [DOI] [PubMed] [Google Scholar]
- 22.Djordjevic S.P., Cain A.K., Evershed N.J., Falconer L., Levings R.S., Lightfoot D., Hall R.M. Emergence and Evolution of Multiply Antibiotic-Resistant Salmonella Enterica Serovar Paratyphi B D-Tartrate-Utilizing Strains Containing SGI1. Antimicrob. Agents Chemother. 2009;53:2319–2326. doi: 10.1128/AAC.01532-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glynn M.K.A., Bopp C., Dewitt W., Dabney P., Mokhtar M., Angullo F. Emergence of Multidrug-Resistant Salmonella Enterica Serotype Typhimurium DT104 Infections in the United States. N. Engl. J. Med. 1998;338:1333–1338. doi: 10.1056/NEJM199805073381901. [DOI] [PubMed] [Google Scholar]
- 24.Wegener H.C. Antibiotics in Animal Feed and Their Role in Resistance Development. Curr. Opin. Microbiol. 2003;6:439–445. doi: 10.1016/j.mib.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 25.Temelli S., Kahya S., Eyigor A., Carli K.T. Incidence of Salmonella Enteritidis in Chicken Layer Flocks in Turkey: Results by Real-Time Polymerase Chain Reaction and International Organization for Standardization Culture Methods. Poult. Sci. 2010;89:1406–1410. doi: 10.3382/ps.2010-00796. [DOI] [PubMed] [Google Scholar]
- 26.Gast R.K. Improving the Safety and Quality of Eggs and Egg Products. Volume 2. Woodhead Publishing; Sawston, UK: 2011. Pre-Harvest Measures to Control Salmonella in Laying Hens; pp. 120–145. [Google Scholar]
- 27.Cerquetti M.C., Gherardi M.M. Orally Administered Attenuated Salmonella Enteritidis Reduces Chicken Cecal Carriage of Virulent Salmonella Challenge Organisms. Vet. Microbiol. 2000;76:185–192. doi: 10.1016/S0378-1135(00)00235-2. [DOI] [PubMed] [Google Scholar]
- 28.Van Immerseel F., Methner U., Rychlik I., Nagy B., Velge P., Martin G., Foster N., Ducatelle R., Barrow P.A., Ducatelle R. Vaccination and Early Protection against Non-Host-Specific Salmonella Serotypes in Poultry: Exploitation of Innate Immunity and Microbial Activity. Epidemiol. Infect. 2005;133:959–978. doi: 10.1017/S0950268805004711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gast R.K. Serotype-Specific and Serotype-Independent Strategies for Preharvest Control of Food-Borne Salmonella in Poultry. Avian Dis. 2007;51:817–828. doi: 10.1637/8090-081807.1. [DOI] [PubMed] [Google Scholar]
- 30.De Cort W., Ducatelle R., Van Immerseel F. Preharvest Measures to Improve the Safety of Eggs. In: Ricke S.C., Gast R.K., editors. Producing Safe Eggs: Microbial Ecology of Salmonella. Elsevier; London, UK: 2016. pp. 259–280. [Google Scholar]
- 31.Desin T.S., Köster W., Potter A.A. Salmonella Vaccines in Poultry: Past, Present and Future. Expert Rev. Vaccines. 2013;12:87–96. doi: 10.1586/erv.12.138. [DOI] [PubMed] [Google Scholar]
- 32.Muotiala A., Hovi M., Mäkelä P.H. Protective Immunity in Mouse Salmonellosis: Comparison of Smooth and Rough Live and Killed Vaccines. Microb. Pathog. 1989;6:51–60. doi: 10.1016/0882-4010(89)90007-7. [DOI] [PubMed] [Google Scholar]
- 33.Babu U., Dalloul R.A., Okamura M., Lillehoj H.S., Xie H., Raybourne R.B., Gaines D., Heckert R.A. Salmonella Enteritidis Clearance and Immune Responses in Chickens Following Salmonella Vaccination and Challenge. Vet. Immunol. Immunopathol. 2004;101:251–257. doi: 10.1016/j.vetimm.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 34.Smith H.W.H. The Use of Live Vaccines in Experimental Salmonella Gallinarum Infection in Chickens with Observations on Their Interference Effect. J. Hyg. 1956;54:419–432. doi: 10.1017/S0022172400044685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feberwee A., de Vries T.S., Hartman E.G., de Wit J.J., Elbers A.R., de Jong W.A. Vaccination against Salmonella Enteritidis in Dutch Commercial Layer Flocks with a Vaccine Based on a Live Salmonella Gallinarum 9R Strain: Evaluation of Efficacy, Safety, and Performance of Serologic Salmonella Tests. Avian Dis. 2001;45:83–91. doi: 10.2307/1593015. [DOI] [PubMed] [Google Scholar]
- 36.Feberwee A., De Vries T.S., Elbers A.R.W., De Jong W.A. Results of a Salmonella Enteritidis Vaccination Field Trial in Broiler-Breeder Flocks in The Netherlands. Avian Dis. 2000;44:249–255. doi: 10.2307/1592537. [DOI] [PubMed] [Google Scholar]
- 37.Gast R.K. Paratyphoid Infections. In: Swayne D.E., Glisson J.R., McDougald L.R., Nolan L.K., Suarez D.L., Nair V., editors. Diseases of Poultry. John Wiley & Sons Inc.; Hoboken, NJ, USA: 2013. pp. 693–706. [Google Scholar]
- 38.Filho R.A.C.P., de Paiva J.B., Argüello Y.M.S., da Silva M.D., Gardin Y., Resende F., Junior A.B., Sesti L. Efficacy of Several Vaccination Programmes in Commercial Layer and Broiler Breeder Hens against Experimental Challenge with Salmonella Enterica Serovar Enteritidis. Avian Pathol. 2009;38:367–375. doi: 10.1080/03079450903183645. [DOI] [PubMed] [Google Scholar]
- 39.Deguchi K., Yokoyama E., Honda T., Mizuno K. Efficacy of a Novel Trivalent Inactivated Vaccine Against the Shedding of Salmonella in a Chicken Challenge Model. Avian Dis. 2009;53:281–286. doi: 10.1637/8516-110908-Reg.1. [DOI] [PubMed] [Google Scholar]
- 40.Aehle S., Curtiss R. Current and Future Perspectives on Development of Salmonella Vaccine Technologies. In: Rickie S.C., Gast R.K., editors. Producing Safe Eggs: Microbial Ecology of Salmonella. Academic Press; Cambridge, MA, USA: 2017. pp. 281–299. [Google Scholar]
- 41.Pascual Anderson M.D.R., Calderón Y., Pascual V. Investigación y Recuento de Enterobacteriaceae Lactosapositivas (Coliformes) In: Díaz de Santos S.A., editor. Microbiología Alimentaria: Metodología Analítica para Alimentos y Bebidas. Universidad de Alcalá; Madrid, Spain: 1992. pp. 17–20. [Google Scholar]
- 42.Huberman Y.D., Velilla A.V., Terzolo H.R. Evaluation of Different Live Salmonella Enteritidis Vaccine Schedules Administered during Layer Hen Rearing to Reduce Excretion, Organ Colonization, and Egg Contamination. Poult. Sci. 2019;98:2422–2431. doi: 10.3382/ps/pez003. [DOI] [PubMed] [Google Scholar]
- 43.Huberman Y.D., Terzolo H.R. Fowl Typhoid: Assessment of a Disinfectant Oral Dose to Reduce Horizontal Spread and Mortality. Avian Dis. 2008;52:320–323. doi: 10.1637/8105-090307-ResNote.1. [DOI] [PubMed] [Google Scholar]
- 44.Audisio M.C., Terzolo H.R. Virulence Analysis of a Salmonella Gallinarum Strain by Oral Inoculation of 20-Day-Old Chickens. Avian Dis. 2002;46:186–191. doi: 10.1637/0005-2086(2002)046[0186:VAOASG]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 45.Hoysak D.J., Weatherhead P.J. Sampling Blood from Birds: A Technique and an Assessment of Its Effect. Condor. 1991;93:746–752. doi: 10.2307/1368207. [DOI] [Google Scholar]
- 46.Williams J.E., Whittemore A.D. Serological Diagnosis of Pullorum Disease with the Microagglutination System. Appl. Microbiol. 1971;21:394–399. doi: 10.1128/am.21.3.394-399.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.El-Enbaawy M.I., Ahmed Z.A.M., Sadek M.A., Ibrahim H.M. Protective Efficacy of Salmonella Local Strains Representing Groups B, C, D and E in a Prepared Polyvalent Formalin Inactivated Oil Adjuvant Vaccine in Layers. Int. J. Microbiol. Res. 2013;4:288–295. doi: 10.5829/idosi.ijmr.2013.4.3.7681. [DOI] [Google Scholar]
- 48.Brown S.L., Klein G.C., McKinney F.T., Jones W.L. Safranin O-Stained Antigen Microagglutination Test for Detection of Brucella Antibodies. J. Clin. Microbiol. 1981;13:398–400. doi: 10.1128/jcm.13.2.398-400.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.National Research Council . Guide for the Care and Use of Laboratory Animals. 8th ed. Volume 46. The National Academies Press; Washington, DC, USA: 2011. [Google Scholar]
- 50.AVMA . Guidelines for the Euthanasia of Animals: 2013 Edition. AVMA; Schaumburg, IL, USA: 2013. 2013.0.1. [Google Scholar]
- 51.Revolledo L. Vaccines and Vaccination against Fowl Typhoid and Pullorum Disease: An Overview and Approaches in Developing Countries. J. Appl. Poult. Res. 2018;3:1–13. doi: 10.3382/japr/pfx066. [DOI] [Google Scholar]
- 52.Wigley P., Barrow P. Salmonella in Preharvest Chickens: Current Understanding and Approaches to Control. In: Rickie S.C., Gast R.K., editors. Producing Safe Eggs. Microbial Ecology of Salmonella. Academic Press; Cambridge, MA, USA: 2017. pp. 139–159. [Google Scholar]
- 53.Barrow P.A., Lovell M.A. Experimental Infection of Egg-Laying Hens with Salmonella Enteritidis Phage Type 4. Avian Pathol. 1991;20:335–348. doi: 10.1080/03079459108418769. [DOI] [PubMed] [Google Scholar]
- 54.Lee Y.J., Mo I.P., Kang M.S. Safety and Efficacy of Salmonella Gallinarum 9R Vaccine in Young Laying Chickens. Avian Pathol. 2005;34:362–366. doi: 10.1080/03079450500180895. [DOI] [PubMed] [Google Scholar]
- 55.OIE . OIE Terrestrial Manual. OIE; Paris, France: 2018. Fowl Typhoid and Pullorum Disease; pp. 1–17. [Google Scholar]
- 56.Toyota-Hanatani Y., Ekawa T., Ohta H., Igimi S., Hara-Kudo Y., Sasai K., Baba E. Public Health Assessment of Salmonella Enterica Serovar Enteritidis Inactivated-Vaccine Treatment in Layer Flocks. Appl. Environ. Microbiol. 2009;75:1005–1010. doi: 10.1128/AEM.01689-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Silva E., Snoeyenbos G., Weinack O., Smyser C. Studies on the Use of 9R Strain of Salmonella Gallinarum as a Vaccine in Chickens. Avian Dis. 1981;25:38–52. doi: 10.2307/1589825. [DOI] [PubMed] [Google Scholar]
- 58.Dewaele I., Van Meirhaeghe H., Rasschaert G., Vanrobaeys M., De Graef E., Herman L., Ducatelle R., Heyndrickx M., De Reu K. Persistent Salmonella Enteritidis Environmental Contamination on Layer Farms in the Context of an Implemented National Control Program with Obligatory Vaccination. Poult. Sci. 2012;91:282–291. doi: 10.3382/ps.2011-01673. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.