Abstract
This article is an observational and cross-sectional study that related the result obtained in the questionnaire for the evaluation of quality of life related to muscle mass (SarQoL) and the prevalence of sarcopenic pathology measured under the EWGSOP2 algorithm. Participants were 202 community-dwelling older adults living in Valencia, Spain. The prevalence of sarcopenia in men was 28.9%, while in women it was 26.2%. In the case of the SarQoL questionnaire, the mean score obtained for men was 75.5 and 72.6 for women, showing significant differences in both sexes between the results obtained by the group with and without sarcopenia. After the exhaustive data analysis, a high discriminative capacity for sarcopenic disease was found in the SarQoL questionnaire total score and in domains 2 (locomotion), 4 (functionality) and 5 (activities of daily living). In accordance with the existing controversy regarding the use of SARC-F as a screening method for sarcopenia, the authors pointed out the capacity of domain 2 (locomotion) in isolation as a possible screening method for this disease, exposing a high risk of suffering sarcopenia when scores in this domain were below 60 points. Further research is needed to develop new lines of research as these showed in this work, as well as new and easily applicable screening methods for sarcopenia in clinical practice, that allow a rapid detection of this disease in the community.
Keywords: sarcopenia, older adults, quality of life, SarQoL, older people, muscle strength
1. Introduction
Sarcopenia, according to the diagnostic criteria of the European Working Group on Sarcopenia in Older People (EWGSOP2) [1], is defined as a generalized and progressive skeletal muscle disorder that is associated with a higher probability of adverse outcomes including falls, fractures, physical disability and mortality. In this latest revision of sarcopenia’s definition, special attention is paid to muscle strength, which has been shown as a key factor in the prediction of disease-related adverse effects. In this latest revision of the disease definition, particular attention is paid to muscle strength, which has been shown to be the key factor in predicting disease-related adverse effects [2,3,4,5]. Sarcopenic pathology is related to age, its appearance being more common after the sixth decade of life [6,7]; despite this, with the implementation of better diagnostic resources, the increasing knowledge and value of the disease among the different health specialists, it is becoming increasingly common to find a greater number of cases in a younger population [8].
Traditionally, sarcopenia’s presence has been linked to health institutions [9,10,11,12], since most of the publications focused on institutionalized patients, who were more accessible to researchers and on whom it could be appreciated to a greater extent the effects of sarcopenia. Nowadays, some researchers stress the need to study sarcopenia in community-dwelling older adults [13,14,15,16,17], since, traditionally, the pathology in this population group was found to be underdiagnosed and may constitute a relevant point of action in terms of public health policies and prevention of higher sarcopenic stages, which through its complications could increase the risk of hospitalization notably [18,19].
At the same time, the analysis of perceived quality of life proved to be important for government and health institutions, since it allows health-related reforms planning according to the specific needs of the population [20].
Complications derived from sarcopenia are related, mainly, with mobility deterioration from patients as well as with a frailty increase, malnutrition, a progressive loss of autonomy and, globally, a decrease in perceived quality of life [20,21,22,23,24]. With the aim of evaluating quality of life and its relationship with muscle mass, in 2016, the SarQoL questionnaire [25] (Sarcopenia Quality of Life) was developed, which was validated for the Spanish population in 2020 [26,27].
This study aim was to evaluate possible differences in terms of quality of life quantified by the SarQoL questionnaire [27] in community-dwelling men and women depending on the presence of sarcopenic disease. Secondarily, researchers started from the hypothesis of the existence of a possible discriminatory capacity of sarcopenic pathology through the SarQoL total score [27] or any of its domains, and whether it can be used as an additional screening tool along with the SARC-F questionnaire [28] proposed by EWGSOP2 [1].
2. Material and Methods
2.1. Study Design and Recruitment of the Sample
Participants of this observational, descriptive and cross-sectional study were recruited in a center for the elderly in Benimaclet (Valencia), managed by Valencia City Council. This center collaborated with the University of Valencia together with the city council in the framework of the commitment acquired regarding the Chair of Healthy, Active and Participative Aging.
The study was sampled by convenience as no randomization method was used. The final sample obtained was of 202 community-dwelling adults over 65 years old; 38 (18.8%) of them were men and 164 were women (81.2%). The inclusion criteria applied to the participants for participation in the research were the following: being over 65 years of age, being enrolled in the center for the elderly where the study was conducted and having completed the informed consent and all phases of the study. The exclusion criteria were the following: presenting diseases that implied a severe deterioration of muscle mass (Parkinson’s, Alzheimer’s, severe cognitive impairment, stroke, muscular dystrophy and cancer) and/or being absent from the center on days on which the study was performed.
Participation in this study was voluntary; all participants completed the relevant informed consent for participation. This research met the standards established by the Declaration of Helsinki [29] and was approved by the bioethics committee of the University of Valencia (Spain) (n/1139186).
2.2. General Assessments
To study general sociodemographic variables of the participants, researchers used a specific ad-hoc questionnaire generated for the occasion. The variables studied were: sex, coexistence at home, age, blood pressure record, heart rate record and chronic diseases (hypertension, diabetes, osteoporosis and dyslipidemia).
2.2.1. Sarcopenia
Sarcopenia diagnosis was made using the latest EWGSOP2 standards [1]. As a result, the sample was divided into two groups: with sarcopenia and without sarcopenia. Participants in the sarcopenic group must have had probable, confirmed or severe sarcopenia, while the group without sarcopenia comprised the rest of the participants.
Handgrip Strength (Upper Body Strength) and Sit-to-Stand Test (Lower Body Strength)
To determine muscle strength, a diagnostic test targeting the two main body segments was performed. In the upper segment, a Jamar 5030J1 manual dynamometer, with a measurement scale of 0–90 kg/f and with an accuracy of ±2 kg, was used to determine the grip strength of the participants [1,30,31,32]. In the lower segment, the sit-to-stand test was performed [1,33] to assess the strength in the subjects’ legs. The cut-off points referred by the EWGSOP2 [1] were used for the categorization of the results.
Participants who showed low muscle strength in the upper body segment and/or low muscle strength in the lower segment were categorized as probable sarcopenia, with their amount of muscle mass evaluated in the next step of the algorithm presented by the EWGSOP2 [1].
Appendicular Skeletal Muscle Mass (ASMM)
Appendicular muscle mass was evaluated using the formula proposed by Kyle et al. [34] to obtain necessary data to complete the equation; the electrical bioimpedance measurement was used with a TANITA DC430MA-S scale (Tokyo, Japan) with a precision of 0.05 kg. In order to obtain accurate measurements, researchers implemented the latest recommendations for performing this technique [35].
According to the EWGSOP2 consensus [1], subjects who presented low muscle strength and also obtained ASMM values lower than 15 kg (muscle mass deficit) were considered sarcopenic confirmed cases; their physical performance was evaluated to determine the severity of the sarcopenic pathology.
Physical Performance (Gait Speed)
Physical performance of the participants was evaluated using the gait speed test [1,36]. This test consisted of measuring the time taken by the subjects to walk a distance of 4 m at a constant and habitual speed. According to the EWGSOP2 consensus [1], participants who presented low muscle strength, low muscle mass and values lower than 0.8 m/s (low physical performance) were categorized as subjects with severe sarcopenia, this being the maximum expression of the disease’s development.
2.2.2. Physical Activity Quantification
Researchers used the International Physical Activity Questionnaire Adapted for the Elderly (IPAQ-E) [37,38] with the study participants with the aim of evaluating the amount of daily mean metabolic equivalents (METS) that subjects were able to develop.
2.2.3. Frailty Status
The frailty of the subjects was evaluated using the Frailty Instrument for Primary Care of the Survey of Health, Aging and Retirement in Europe (SHARE-FI) [39]. This tool is validated for the Spanish population in the age range of the study participants [40].
The SHARE-FI instrument [40] consists of 5 sections that evaluate fatigue, appetite, manual grip muscle strength, functional difficulties and the frequency of physical activity performed; each item offers a numerical result that is processed through the calculator offered by the tool. Finally, it gives a categorization of the subject in three possible states: frail, pre-frail and non-frail.
2.2.4. Nutritional Status
The nutritional status of the participants was evaluated using the Self-MNA test [41] validated for populations older than 65 years [41,42]. This test was self-administered according to its original format; despite this, its completion was supervised by researchers in order to resolve any doubts that might arise among the participants.
The Self-MNA test [41] categorized participants into three states based on the final score obtained: normal nutritional status (12–14 points), risk of malnutrition (8–11 points) and malnutrition (0–7 points).
2.3. Quality of Life (SarQoL)
To assess participants’ quality of life, the Spanish translated version of the SarQoL questionnaire [27] was used, offered by developers. All the questions asked in this questionnaire, except 7, 14 and 22, use a Likert scale of frequency or intensity; in turn, these questions are categorized into seven domains that assess different dimensions related to quality of life: physical and mental health (D1), locomotion (D2), body composition (D3), functionality (D4), activities of daily living (D5), leisure activities (D6) and fears (D7). Each domain, as well as the total score of the questionnaire, is quantified on a scale from 0 to 100, in which a higher score implies a better quality of life.
The administration of this questionnaire was carried out by the researchers, who clarified and/or resolved the doubts that arose during its completion.
To obtain the corresponding detailed results of the questionnaires once completed with the participants’ information, researchers used the official platform offered by the creators (www.SarQoL.org, accessed on 25 June 2022). This questionnaire has strong internal consistency, as can be consulted in various publications [27,43,44,45].
2.4. Statistical Analysis
Statistical analysis was carried out using the IBM SPSS Statistics v. 24 software for Windows (IBM Corp., Armouk, NY, USA). The normality of the data was evaluated using the Shapiro–Wilk’s test. Descriptive statistics were calculated for sociodemographic variables (percentages or mean ± SD), results of the SarQoL questionnaire [27] and its domains (mean ± SD) and for the different variables related to physical performance, as well as the diagnosis of the sarcopenia (mean ± SD). The differences between groups with and without sarcopenic disease were determined using the Student’s t test and Mann–Whitney U test, establishing significant differences with p values ≤ 0.05 in all tests. The Spearman correlation model was used to evaluate the relationships between the different variables that make up the diagnosis of sarcopenia and the results obtained in the SarQoL questionnaire [27] and in its domains. Variables that showed significant differences were evaluated in a later step using a multiple linear regression model in order to observe their influence on the score obtained for each of the domains and on the total score of the SarQoL questionnaire [27].
Additionally, a ROC curve analysis model was developed where the ability to discriminate sarcopenia as a pathology through the total score of the SarQoL test [27] and the three most influential domains in the general result of the questionnaire was evaluated. Subsequently, knowing the specificity and sensitivity thresholds in the sarcopenia diagnosis of each score obtained in the total SarQoL questionnaire [27], researchers designed possible risk areas that would allow the use of this test as a diagnostic-preventive factor.
3. Results
The study sample was composed of a total of 202 subjects; the mean age was 73 ± 7 years. The youngest participant was a 65-year-old woman, and the oldest was an 85-year-old woman. Of the total sample, 7.4% had confirmed or severe sarcopenic pathology and 26.7% had some of the disease stages. The mean value obtained regarding participants’ total quality of life was 75.3 ± 10.1 points.
Table 1 summarizes general characteristics of the sample distributed by sex based on sarcopenic disease presence. In the men group, age showed significant differences in terms of the presence of sarcopenia; men who presented the disease were older. Regarding frailty, men and women who presented a pre-frail or frail state were more prevalent in the sarcopenic disease group (p = 0.015 and p = 0.001, respectively). In the nutritional aspect, significant differences (p = 0.017) were only found in the men group, where the results obtained showed a higher prevalence of malnutrition in the group of sarcopenic participants. No significant differences were found in terms of the prevalence of sarcopenia for BMI or chronic diseases under study in either sex. The quality of life of the participants analyzed through the SarQoL questionnaire [27] yielded significantly lower results in the sarcopenia group in both men and women, the values obtained in most of the domains of the questionnaire being significantly lower in the groups who presented the disease. Finally, the parameters related to physical activity studied showed significantly lower results in the sarcopenia groups regardless of sex, with the exception of the total amount of ASMM.
Table 1.
Characteristics of the study sample based on the presence of sarcopenia and the QoL.
| Total | Men | p-Value | Women | p-Value | |||
|---|---|---|---|---|---|---|---|
| WS * (N = 27) | S ** (N = 11) | WS * (N = 121) | S ** (N = 43) | ||||
| Age (years) | 73 ± 5 | 71 ± 4 | 75 ± 5 | 0.013 | 72 ± 5 | 74 ± 5 | 0.104 |
| Living arrangement | 0.230 | 0.062 | |||||
| With partner | 143 (70.8%) | 27 (100%) | 9 (81.8%) | 86 (71.1%) | 21 (48.8%) | ||
| With son | 5 (2.5%) | 0 (0%) | 0 (0%) | 3 (2.5%) | 2 (4.7%) | ||
| Alone | 6 (3%) | 0 (0%) | 2 (18.2%) | 3 (2.5%) | 1 (2.3%) | ||
| Other | 48 (23.7%) | 0 (0%) | 0 (0%) | 0.165 | 29 (24%) | 19 (44.2%) | 0.045 |
| Education | |||||||
| Elementary school or no degree | 170 (84.1%) | 19 (70.4%) | 11 (100%) | 100 (82.6%) | 40 (94%) | ||
| Secondary school | 22 (10.9%) | 8 (29.6%) | 0 (0%) | 12 (9.9%) | 2 (4.7%) | ||
| University or higher degree | 10 (5%) | 0 (0%) | 0 (0%) | 0.015 | 9 (7.4%) | 1 (2.3%) | 0.001 |
| Frailty status (score) | |||||||
| Non-frail | 85 (42.1%) | 18 (66.7%) | 4 (36.4%) | 54 (44.6%) | 9 (20.9%) | ||
| Pre-frail | 87 (43.1%) | 9 (33.3%) | 4 (36.4%) | 54 (44.6%) | 20 (46.5%) | ||
| Frail | 30 (14.8%) | 0 (0%) | 3 (37.3%) | 0.017 | 13 (10.7%) | 14 (32.6%) | 0.080 |
| Nutritional status (score) | |||||||
| Normal nourished | 127 (62.9%) | 22 (81.5%) | 4 (36.4%) | 76 (62.8%) | 25 (58.1%) | ||
| At risk of malnutrition | 4 (2%) | 0 (0%) | 0 (0%) | 1 (0.8%) | 3 (7%) | ||
| Malnourished | 71 (35.1%) | 5 (18.5%) | 7 (63.6%) | 44 (36.4%) | 15 (14.9%) | ||
| Body mass index (kg/m2) | 27.5 ± 4.2 | 28.2 ± 4.4 | 28.7 ± 4.9 | 0.800 | 27.2 ± 4.2 | 27.7 ± 4.1 | 0.500 |
| Comorbidities | |||||||
| Hypertension | 102 (50.5%) | 18 (66.7%) | 8 (72.7%) | 0.720 | 54 (44.6%) | 22 (51.2%) | 0.460 |
| Dyslipidemia | 90 (44.6%) | 14 (51.9%) | 5 (45.5%) | 0.620 | 51 (42.1%) | 20 (46.5%) | 0.720 |
| Diabetes mellitus 2 | 28 (13.9%) | 6 (22.2%) | 5 (45.5%) | 0.150 | 12 (9.9%) | 5 (11.6%) | 0.750 |
| Osteoporosis | 13 (6.4%) | 1 (3.7%) | 0 (0%) | 0.520 | 9 (7.4%) | 3 (7%) | 0.920 |
| SarQoL | |||||||
| Overall quality of life | 75.3 ± 10.1 | 81.2 ± 10.4 | 69.8 ± 12.5 | 0.006 | 76.9 ± 8.4 | 68.3 ± 9.6 | 0.000 |
| Physical and mental health | 75.7 ± 13.9 | 83.1 ± 12.7 | 69.3 ± 15.3 | 0.007 | 76.8 ± 12.7 | 69.6 ± 14.8 | 0.003 |
| Locomotion | 80.6 ± 15.7 | 86.5 ± 16.3 | 73 ± 15.9 | 0.025 | 83.6 ± 14.4 | 70.5 ± 13.7 | 0.000 |
| Body composition | 65.7 ± 14.9 | 76.2 ± 14.2 | 65.9 ± 15.7 | 0.076 | 64.2 ± 14.5 | 63.3 ± 14 | 0.710 |
| Functionality | 75.3 ± 13.4 | 80.3 ± 14.8 | 67.1 ± 15.3 | 0.018 | 77.9 ± 11.9 | 67.1 ± 11.7 | 0.000 |
| Activities of daily living | 72.4 ± 10.3 | 78.1 ± 10.3 | 65.7 ± 14.8 | 0.005 | 73.8 ± 8.3 | 66.6 ± 10.8 | 0.000 |
| Leisure activities | 67.9 ± 20 | 73.9 ± 19.2 | 60.5 ± 15.3 | 0.046 | 68.4 ± 20.3 | 64.6 ± 20.3 | 0.290 |
| Fears | 88.9 ± 17.5 | 94 ± 14 | 95.5 ± 10.1 | 0.750 | 89 ± 17.3 | 83.4 ± 20.2 | 0.110 |
| Physical activity parameters | |||||||
| METS (score) | 855.4 ± 420.3 | 1212.1 ± 644.6 | 821 ± 448.1 | 0.043 | 845 ± 342.9 | 669.5 ± 294.2 | 0.003 |
| ASMM (kg) | 17.8 ± 3.6 | 23.2 ± 2.9 | 23.1 ± 3.2 | 0.990 | 16.5 ± 2.4 | 16.6 ± 2.8 | 0.850 |
| Handgrip strength (kg) | 22.4 ± 7.7 | 35.6 ± 7 | 30.1 ± 5 | 0.023 | 21.4 ± 3.8 | 15.1 ± 4.3 | 0.000 |
| Gait speed (m/s) | 1.01 ± 0.22 | 1 ± 0.2 | 0.9 ± 0.2 | 0.043 | 1.1 ± 0.2 | 0.9 ± 0.2 | 0.000 |
| Sit to stand test (s) | 11.9 ± 3.6 | 10.8 ± 2.6 | 17.4 ± 3.4 | 0.000 | 10.5 ± 2.1 | 14.9 ± 4.4 | 0.000 |
* WS: Without sarcopenia; S **: Sarcopenia cases; Group differences: Chi square test or Fisher’s exact test for categorical data. t test or Mann–Whitney U test for continuous data; The data are presented in mean ± standard deviation or N (percentages); p-Value ≤ 0.05 shown in bold.
Relationships between main variables related to sarcopenia and the SarQoL questionnaire domains [27], as well as the total result obtained in the questionnaire, were analyzed according to sex and can be consulted in detail in Table 2.
Table 2.
Correlations between principal variables related with Sarcopenia and SarQoL Domains.
| Age | BMI | Weekly Physical Activity (METS) |
Appendicular Skeletal Muscle Mass |
Handgrip Strength | Sit to Stand Test | Gait Speed | ||
|---|---|---|---|---|---|---|---|---|
| Physical and mental health (D1) | Men | 0.341 | −0.291 | 0.422 | −0.13 | 0.133 | −0.565 | 0.363 |
| Women | −0.202 | −0.164 | 0.331 | −0.077 | 0.147 | −0.240 | 0.096 | |
| Locomotion (D2) | Men | −0.351 | −0.412 | 0.538 | −0.24 | 0.198 | −0.575 | 0.544 |
| Women | −0.247 | −0.284 | 0.424 | −0.106 | 0.328 | −0.381 | 0.351 | |
| Body composition (D3) | Men | −0.062 | −0.265 | 0.132 | −0.088 | −0.04 | −0.176 | −0.022 |
| Women | −0.235 | 0.123 | 0.195 | 0.079 | −0.059 | −0.039 | 0.104 | |
| Functionality (D4) | Men | −0.390 | −0.344 | 0.510 | −0.161 | 0.397 | −0.589 | 0.514 |
| Women | −0.198 | −0.301 | 0.267 | −0.153 | 0.267 | −0.396 | 0.384 | |
| Activities of daily living (D5) | Men | −0.361 | −0.365 | 0.331 | −0.224 | 0.269 | −0.422 | 0.413 |
| Women | −0.236 | −0.168 | −0.316 | −0.038 | 0.326 | −0.201 | −0.281 | |
| Leisure activities (D6) | Men | −0.232 | −0.16 | 0.387 | −0.074 | 0.251 | −0.262 | 0.097 |
| Women | −0.243 | 0.011 | 0.332 | 0.015 | 0.061 | −0.231 | 0.163 | |
| Fears (D7) | Men | −0.068 | −0.368 | 0.268 | −0.051 | 0.171 | −0.094 | 0.252 |
| Women | −0.106 | −0.238 | 0.016 | −0.13 | 0.072 | −0.192 | 0.255 | |
| SarQoL Total | Men | −0.350 | −0.423 | 0.521 | −0.21 | 0.33 | −0.592 | 0.513 |
| Women | −0.305 | −0.279 | 0.406 | −0.120 | 0.314 | −0.394 | 0.383 |
Pearson’s correlation coefficient for normally distributed data and Spearman’s correlation coefficient for data that are not normally distributed; p ≤ 0.05 results area shown in bold.
Thus, we can observe how all the variables, except the total amount of ASMM, showed significant differences regarding the correlations for the final result of the SarQoL questionnaire [27] regardless of sex. All variables related to sarcopenia diagnosis presented worse results, as seen with the lower score obtained in terms of quality of life. Domains three, six and seven were ones that showed the least significant correlations regardless of gender in terms of their result and their relationship with main variables related to sarcopenia diagnosis.
Table 3 shows the results of the multiple linear regression analysis for all of the SarQoL questionnaire domains and its total score. Most of the variables related to sarcopenia diagnosis presented worse results given the lower scores in the domains or in the total score of the SarQoL questionnaire [27]. This finding associated worse results in these variables with a worse score in terms of quality of life for the participants.
Table 3.
Multiple Linear Regression Analysis with Total and Domain Scores of SarQol as Dependent Variable.
| Independent Variable | Men | Independent Variable |
Women | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | Beta | T | p | R2 | Adjusted R2 | Model Significance |
B | SE | Beta | T | p | R2 | Adjusted R2 | Model Significance |
||
| D1 Physical and mental health | D1 Physical and mental health | ||||||||||||||||
| 1. Age | −0.323 | 0.509 | −0.999 | −0.364 | 0.53 | 0.44 | 0.37 | 0.001 | 1. Age | −0.306 | 0.210 | −0.116 | −1.455 | 0.148 | 0.152 | 0.13 | 0.0001 |
| 2. METS | 0.005 | 0.003 | 0.22 | 1.531 | 0.135 | 2. BMI | −0.441 | 0.245 | −0.135 | −1.802 | 0.074 | ||||||
| 3. Sit To Stand Test | −1.655 | 0.609 | −0.469 | −2.715 | 0.01 | 3. METS | 0.009 | 0.003 | 0.235 | 3.007 | 0.003 | ||||||
| 4. Gait Speed | 2.503 | 12.22 | 0.034 | 0.205 | 0.839 | 4. Sit To Stand Test | −0.595 | 0.302 | −0.151 | −1.970 | 0.051 | ||||||
| D2 Locomotion | D2 Locomotion | ||||||||||||||||
| 1. Age | −0.313 | 0.498 | −0.082 | −0.628 | 0.534 | 0.628 | 0.57 | 0.0001 | 1. Age | −0.460 | 0.208 | −0.154 | −2.215 | 0.028 | 0.339 | 0.323 | 0.0001 |
| 2. BMI | −1.568 | 0.424 | −0.411 | −3.703 | 0.001 | 2. BMI | −1.296 | 0.241 | −0.352 | −5.368 | 0.000 | ||||||
| 3. METS | 0.007 | 0.003 | 0.254 | 2.128 | 0.041 | 3. METS | 0.013 | 0.003 | 0.287 | 4.178 | 0.000 | ||||||
| 4. Sit To Stand Test | −0.634 | 0.598 | −0.154 | −0.106 | 0.297 | 4. Handgrip | 0.760 | 0.212 | 0.238 | 3.581 | 0.000 | ||||||
| 5. Gait Speed | 27.324 | 11.810 | 0.320 | 2.314 | 0.027 | ||||||||||||
| D3 Body Composition | D3 Body Composition | ||||||||||||||||
| 1. Age | −0.583 | 0.224 | −0.209 | −2.604 | 0.010 | 0.066 | 0.054 | 0.004 | |||||||||
| 2. METS | 0.004 | 0.003 | 0.097 | 1.209 | 0.228 | ||||||||||||
| D4 Functionality | D4 Functionality | ||||||||||||||||
| 1. Age | −0.134 | 0.527 | −0.038 | −0.254 | 0.801 | 0.6 | 0.522 | 0.0001 | 1. Age | −0.258 | 0.191 | −0.104 | −1.353 | 0.178 | 0.312 | 0.285 | 0.0001 |
| 2. BMI | −1.170 | 0.427 | −0.330 | −2.736 | 0.010 | 2. BMI | −0.898 | 0.213 | −0.293 | −4.214 | 0.000 | ||||||
| 3. METS | 0.006 | 0.003 | 0.239 | 1.894 | 0.068 | 3. METS | 0.004 | 0.003 | 0.116 | 1.632 | 0.105 | ||||||
| 4. Handgrip | 0.502 | 0.323 | 0.219 | 1.556 | 0.130 | 4. Handgrip | 0.286 | 0.188 | 0.107 | 1.515 | 0.132 | ||||||
| 5. Sit To Stand Test | −0.977 | 0.587 | −0.256 | −1.667 | 0.106 | 5. Sit To Stand Test | −0.916 | 0.287 | −0.247 | −3.192 | 0.002 | ||||||
| 6. Gait Speed | 15.118 | 11.875 | 0.191 | 1.273 | 0.212 | 6. Gait Speed | 6.286 | 4.680 | 0.112 | 1.343 | 0.181 | ||||||
| D5 Activities of Daily Living | D5 Activities of Daily Living | ||||||||||||||||
| 1. Age | −0.586 | 0.447 | −0.206 | −1.310 | 0.199 | 0.47 | 0.387 | 0.001 | 1. Age | −0.219 | 0.153 | −0.118 | −1.433 | 0.154 | 0.211 | 0.181 | 0.0001 |
| 2. BMI | −0.799 | 0.381 | −0.278 | −2.098 | 0.044 | 2. BMI | −0.388 | 0.171 | −0.169 | −2.267 | 0.025 | ||||||
| 3. METS | 0.003 | 0.003 | 0.146 | 1.023 | 0.314 | 3. METS | 0.005 | 0.002 | 0.159 | 2.086 | 0.039 | ||||||
| 4. Sit To Stand Test | −0.185 | 0.538 | −0.060 | −0.344 | 0.733 | 4. Handgrip | 0.434 | 0.151 | 0.217 | 2.868 | 0.005 | ||||||
| 5. Gait Speed | 22.902 | 10.618 | 0.356 | 2.157 | 0.039 | 5. Sit To Stand Test | −0.262 | 0.230 | −0.094 | −1.136 | 0.258 | ||||||
| 6. Gait Speed | 2.985 | 3.754 | 0.071 | 0.795 | 0.428 | ||||||||||||
| D6 Leisure Activities | D6 Leisure Activities | ||||||||||||||||
| 1. METS | 0.008 | 0.005 | 0.267 | 1.665 | 0.105 | 0.071 | 0.046 | 0.105 | 1. Age | −0.519 | 0.328 | −0.132 | −1.582 | 0.116 | 0.113 | 0.103 | 0.000 |
| 2. METS | 0.015 | 0.005 | 0.243 | 3.073 | 0.002 | ||||||||||||
| 3. Sit To Stand Test | −0.580 | 0.508 | −0.099 | −1.141 | 0.256 | ||||||||||||
| 4. Gait Speed | 0.509 | 8.009 | 0.006 | 0.063 | 0.949 | ||||||||||||
| D7 Fears | D7 Fears | ||||||||||||||||
| 1. BMI | −1.337 | 0.424 | −0.465 | −3.155 | 0.003 | 0.217 | 0.195 | 0.003 | 1. BMI | −0.761 | 0.329 | −0.174 | −2.311 | 0.022 | 0.117 | 0.101 | 0.0001 |
| 2. Sit To Stand Test | −0.591 | 0.452 | −0.112 | −1.307 | 0.193 | ||||||||||||
| 3. Gait Speed | 1.573 | 6.890 | 0.197 | 2.282 | 0.024 | ||||||||||||
| SarQol Total | SarQol Total | ||||||||||||||||
| 1. Age | −0.340 | 0.351 | −0.127 | −0.968 | 0.341 | 0.693 | 0.634 | 0.0001 | 1. Age | −0.289 | 0.135 | −0.157 | −2.137 | 0.034 | 0.375 | 0.351 | 0.0001 |
| 2. BMI | −1.115 | 0.285 | −0.414 | −3.918 | 0.000 | 2. BMI | −0.605 | 0.151 | −0.265 | −3.996 | 0.000 | ||||||
| 3. METS | 0.005 | 0.002 | 0.270 | 2.451 | 0.020 | 3. METS | 0.007 | 0.002 | 0.234 | 3.439 | 0.001 | ||||||
| 4. Handgrip | 0.251 | 0.215 | 0.144 | 1.169 | 0.251 | 4. Handgrip | 0.299 | 0.134 | 0.151 | 2.239 | 0.027 | ||||||
| 5. Sit To Stand Test | −0.607 | 0.390 | −0.209 | −1.556 | 0.130 | 5. Sit To Stand Test | −0.608 | 0.204 | −0.221 | −2.985 | 0.003 | ||||||
| 6. Gait Speed | 12.555 | 7.903 | 0.208 | 1.589 | 0.122 | 6. Gait Speed | 3.364 | 3.321 | 0.081 | 1.013 | 0.313 | ||||||
p ≤ 0.05 results area shown in bold.
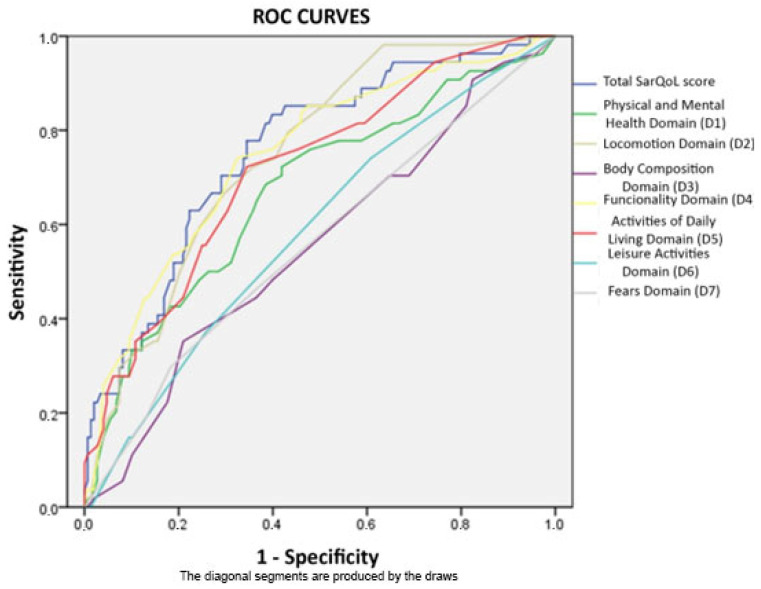
After what was observed in Table 2 and Table 3 and taking into account the high relationship between most of the variables related to sarcopenia and scores obtained in different domains and in the total SarQoL questionnaire score [27], researchers decided to perform an analysis of ROC curves in order to assess the discriminatory capacity of the questionnaire and its domains for the diagnosis of sarcopenia, regardless of sex; this model is shown in Figure 1 and can be consulted in detail in Table 4. Areas under the curve were greater than 0.7 for domains two, four and five and for the total SarQoL [27] score, this latter being the one that showed a greater discriminatory capacity for the diagnosis of sarcopenic disease (area under the curve: 0.756). Additionally, the authors performed the same test excluding patients with probable sarcopenia from the population with the disease (it can be seen in depth in Table 5).
Figure 1.
Multiple ROC curves developed for every SarQoL domain and total score.
Table 4.
ROC curves diagnostic performance values for each domain and total score of SarQoL questionnaire when it was used to discriminate sarcopenic pathology.
| Analyzed Variables | 95% Asymptotic Confidence Interval | |||
|---|---|---|---|---|
| Area | p-Value | Lower Limit | Upper Limit | |
| Total SarQoL score | 0.756 * | 0.000 | 0.682 | 0.83 |
| Physical and Mental Health Domain (D1) | 0.671 | 0.000 | 0.584 | 0.758 |
| Locomotion Domain (D2) | 0.749 * | 0.000 | 0.679 | 0.819 |
| Body Composition Domain (D3) | 0.554 | 0.244 | 0.464 | 0.644 |
| Functionality Domain (D4) | 0.746 * | 0.000 | 0.669 | 0.824 |
| Activities Of Daily Living Domain (D5) | 0.717 * | 0.000 | 0.638 | 0.796 |
| Leisure Activities Domain (D6) | 0.586 | 0.063 | 0.498 | 0.673 |
| Fears Domain (D7) | 0.559 | 0.202 | 0.467 | 0.65 |
* Area >0.70 is shown in bold.
Table 5.
ROC curves diagnostic performance values for each domain and total score of SarQoL questionnaire when it was used to discriminate sarcopenic pathology (only confirmed and severe cases).
| Analyzed Variables | 95% Asymptotic Confidence Interval | |||
|---|---|---|---|---|
| Area | p-Value | Lower Limit | Upper Limit | |
| Total SarQoL score | 0.685 | 0.014 | 0.556 | 0.815 |
| Physical and Mental Health Domain (D1) | 0.647 | 0.052 | 0.506 | 0.787 |
| Locomotion Domain (D2) | 0.696 | 0.009 | 0.576 | 0.817 |
| Body Composition Domain (D3) | 0.455 | 0.553 | 0.302 | 0.608 |
| Functionality Domain (D4) | 0.621 | 0.109 | 0.489 | 0.753 |
| Activities Of Daily Living Domain (D5) | 0.666 | 0.028 | 0.533 | 0.799 |
| Leisure Activities Domain (D6) | 0.661 | 0.032 | 0.530 | 0.793 |
| Fears Domain (D7) | 0.515 | 0.838 | 0.372 | 0.659 |
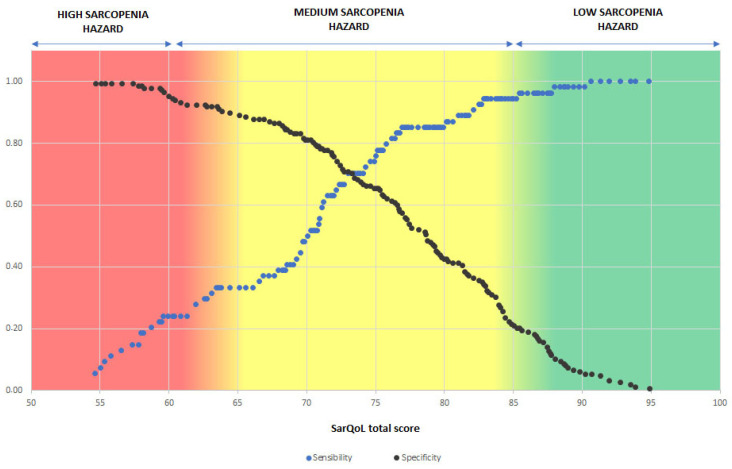
Taking into account the sensitivity and specificity in the sarcopenia diagnosis for each of the total scores of the questionnaire obtained, researchers delimited three risk areas in terms of the probability of suffering sarcopenia, regardless of sex, based on results obtained in the SarQoL questionnaire [27] test; this model can be consulted in Figure 2. Thus, obtaining a result of fewer than 60 points in the questionnaire would imply a high risk of suffering from sarcopenia; a result between 61 and 85 implies a moderate risk; and a score higher than 86 implies a low risk of suffering from sarcopenia.
Figure 2.
Sarcopenia hazard based on the result obtained in the SarQoL questionnaire, assessing the sensitivity and specificity for the scores obtained.
4. Discussion
The results of this study showed a significant relationship between quality of life quantified through the SarQoL test [27] and the presence of sarcopenia in the study subjects. As far as the authors know, this is the first article in which the SarQoL questionnaire [27] was used to quantify community-dwelling older people’s quality of life with or without sarcopenia. Furthermore, this work presents a pioneering approach in terms of evaluating the ability of the questionnaire to discriminate sarcopenic disease regardless of the participant’s sex in the total SarQoL score and its domains.
The updated EWGSOP2 algorithm [1] was used for the diagnosis of sarcopenia despite the existence of other diagnostic tools in the literature [46,47,48,49]. This algorithm is widely endorsed by the scientific community [11,14,50,51,52,53], being a reference in the great part of the world.
Our study used a sample size and yielded results similar to those obtained by Geerinck et al. [54] in their initial research to observe the feasibility of the SarQoL questionnaire as a screening method for sarcopenia. The cut-off score obtained in their study was 52.4 points when assessing the risk between low and high of suffering from the disease, while the researchers of this article placed it at 60 points. This difference could be due to the fact that the entire sample of the work presented by Geerinck et al. [54] was not collected outside health institutions or because no cases with probable sarcopenia were included in its intervention group.
Additionally, the area under the curve obtained by Geerinck et al. [54] for the total score of the SarQoL questionnaire was higher (0.771) than the score obtained by the researchers of this study when the same conditions were applied to the group with the disease (Table 5) or including the cases of probable sarcopenia (0.756).
Our work presented a prevalence of confirmed and severe sarcopenia similar to that found by Kim et al. [50] in community-dwelling older people using the algorithm proposed by EWGSOP2 [1]. Furthermore, consistent with Volpato et al. [55] and Cruz-Jentoft et al. [56], a significant relationship was found between age and the presence of sarcopenic pathology in men; this same relationship could not be demonstrated in women, unlike what was stated by other authors [57,58] in their studies. Significant differences were also found regarding the level of education and the prevalence of sarcopenia in women, with sarcopenia being more prevalent in women with primary education or without studies; this situation is similar to that expressed by Dorosty et al. [59] for both sexes in their publication, despite being an institutionalized population and having evaluated sarcopenic pathology following the EWGSOP recommendations [60] published in 2010. The significant increase in pre-frail and frail status in sarcopenic groups regardless of sex was found in our study, as in that presented by other authors [23,24,61]. Regarding chronic diseases studied, no significant differences were found when they were related to sarcopenia regardless of sex, although other authors [58,62] reported an osteoporosis increase in sarcopenic individuals.
Regarding quality of life, significant differences were found in the total score obtained in the SarQoL questionnaire [27], observing a worse quality of life in individuals with sarcopenia regardless of gender; this fact is also contemplated in publications made by other authors [20,45,63], despite not using the same tool for quantifying quality of life. Most of the SarQoL domains [27] presented worse scores in the group with sarcopenia, except in domain three (body composition) and seven (fears) in both groups, and domain six (leisure activities) also in the female group. These domains did not seem to have much influence on the quality of life of subjects with sarcopenic pathology. More studies are needed to broaden the discussion regarding this last statement.
The main variables for sarcopenia diagnosis showed significant differences when they were related to the total SarQoL score [27], with worse results in these variables obtained with participants with a lower quality of life. This situation was not manifested in the case of the ASMM, since it did not show significant differences when relating it to the score obtained in the questionnaire. The absence of a relationship between the amount of ASMM and quality of life seems to be in agreement with that expressed by other authors [2,3,4,5] regarding the need to reduce the relevance of this variable in the diagnosis of sarcopenia; in fact, the EWGSOP in its latest update [1] already introduced the importance of strength, physical performance or the quality of muscle mass against the detriment of the amount of ASMM as a diagnostic variable.
After consulting some publications in which the use of the SARC-F test [28] recommended by the EWGSOP2 [1] as a screening tool for sarcopenia was discussed, the authors detected some uncertainty regarding the current capacity of the test to detect early possible cases of sarcopenia [17,54,64]. That is why, after observing the significant differences in terms of quality of life between subjects living in the community with or without sarcopenic pathology, regardless of sex, and taking into account the purpose of this possible new adaptation of the SarQoL questionnaire, as well as the original function of the SARC-F as a screening questionnaire, the authors decided that it was relevant to include the subjects with probable sarcopenia within the group with sarcopenia in the study, since the early detection of a presarcopenic situation is also relevant in current medicine. The results obtained show that the total score of the questionnaire and domains two (locomotion), four (functionality) and five (activities of daily living), autonomously, would allow for detecting cases of sarcopenia. The development of risk intervals for sarcopenia detection was carried out based on the total SarQoL score [27], as it was the analyzed variable of the questionnaire that presented a greater area under the curve (0.756).
The SarQoL questionnaire [27] has an approximate duration of 10 min according to its developers. We consider that the total duration of the questionnaire can be an inconvenience for its use as a screening tool; for this reason, we suggest the use of domain 2 (locomotion) autonomously. This domain presented an area under the curve of 0.749, is composed by only 9 items and requires less time to complete. The authors suggest carrying out the SarQoL questionnaire in nursing or medicine primary care consultations with the vulnerable population over 65 years of age as a screening method at least once a year. If the value obtained is fewer than 85 points, researchers recommend performing the complete battery of tests for the diagnosis of sarcopenia explained in the EWGSOP2 [1] algorithm.
This study has severe limitations: the sampling carried out was non-random despite the voluntary nature of the participants; it was not multicenter; the small sample could lead the authors to bias in the results or some false-negative cases. Despite this, it also shows strengths: the application of the updated EWGSOP2 algorithm [1] in its entirety, the pioneering vision with which the discrimination capacity of the questionnaire for the diagnosis/prevention of sarcopenia is evaluated, as well as the use of a control group that allows comparing the differences between the sarcopenic and non-sarcopenic groups in community-dwelling older adults.
More research is needed to continue exploring: the ability of the SarQoL questionnaire [27] to detect sarcopenic disease early, its potential as a screening tool together with the SARC-F test [28] proposed by the EWGSOP2 [1] and the importance of the quality of life within sarcopenic disease, responding directly to the subjective assessment of patients regarding the limitations caused by this disease. Quality of life must be a direct feedback channel for the production of primary and secondary health policies that are as close as possible to the citizen and therefore to the future patient.
5. Conclusions
In summary, this study shows a significant reduction in the quality of life of sarcopenic community-dwelling subjects regardless of sex when evaluated using the EWGSOP2 diagnostic algorithm [1] and SarQoL questionnaire [27]. Participants presented significantly lower values for the main variables related with sarcopenia diagnosis when the results obtained in the analysis of quality of life were worse, except ASMM. The SarQoL [27], in its entirety, or using domains 2, 4 and 5 autonomously, demonstrated discriminatory capacity for sarcopenic pathology diagnosed under the EWGSOP2 algorithm [1], as well as a potential use as an element of population screening.
Author Contributions
Conceptualization, C.G.-E. and A.D.-G.; methodology, C.G.-E. and A.D.-G.; software, J.M.T.-B. and C.G.-E.; formal analysis, J.M.T.-B.; data curation, J.M.T.-B. and C.G.-E.; writing—original draft preparation, C.G.-E. and A.D.-G.; writing—review and editing, C.G.-E., A.D.-G., D.Z.R., J.J.F.-G. and J.M.S.; visualization, J.J.F.-G. and J.M.S.; supervision, J.J.F.-G., A.M.-G. and J.M.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Bioethics Committee of University of Valencia (UV-1139186, 21/05/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cruz-Jentoft A.J., Bahat G., Bauer J., Boirie Y., Bruyère O., Cederholm T., Cooper C., Landi F., Rolland Y., Sayer A.A., et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schaap L.A., van Schoor N.M., Lips P., Visser M. Associations of Sarcopenia Definitions, and Their Components, with the Incidence of Recurrent Falling and Fractures: The Longitudinal Aging Study Amsterdam. J. Gerontol. A Biol. Sci. Med. Sci. 2018;73:1199–1204. doi: 10.1093/gerona/glx245. [DOI] [PubMed] [Google Scholar]
- 3.Ibrahim K., May C., Patel H.P., Baxter M., Sayer A.A., Roberts H. A Feasibility Study of Implementing Grip Strength Measurement into Routine Hospital Practice (GRImP): Study Protocol. Pilot Feasibility Stud. 2016;2:27. doi: 10.1186/s40814-016-0067-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leong D.P., Teo K.K., Rangarajan S., Lopez-Jaramillo P., Avezum A., Orlandini A., Seron P., Ahmed S.H., Rosengren A., Kelishadi R., et al. Prognostic Value of Grip Strength: Findings from the Prospective Urban Rural Epidemiology (PURE) Study. Lancet Lond. Engl. 2015;386:266–273. doi: 10.1016/S0140-6736(14)62000-6. [DOI] [PubMed] [Google Scholar]
- 5.Alley D.E., Shardell M.D., Peters K.W., McLean R.R., Dam T.-T.L., Kenny A.M., Fragala M.S., Harris T.B., Kiel D.P., Guralnik J.M., et al. Grip Strength Cutpoints for the Identification of Clinically Relevant Weakness. J. Gerontol. A Biol. Sci. Med. Sci. 2014;69:559–566. doi: 10.1093/gerona/glu011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han A., Bokshan S.L., Marcaccio S.E., DePasse J.M., Daniels A.H. Diagnostic Criteria and Clinical Outcomes in Sarcopenia Research: A Literature Review. J. Clin. Med. 2018;7:70. doi: 10.3390/jcm7040070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roubenoff R., Hughes V.A. Sarcopenia: Current Concepts. J. Gerontol. A Biol. Sci. Med. Sci. 2000;55:716. doi: 10.1093/gerona/55.12.M716. [DOI] [PubMed] [Google Scholar]
- 8.Sayer A., Syddall H., Martin H., Patel H., Baylis D., Cooper C. The Developmental Origins of Sarcopenia. J. Nutr. Health Aging. 2008;12:427–432. doi: 10.1007/BF02982703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bravo-José P., Moreno E., Espert M., Romeu M., Martínez P., Navarro C. Prevalence of Sarcopenia and Associated Factors in Institutionalised Older Adult Patients. Clin. Nutr. ESPEN. 2018;27:113–119. doi: 10.1016/j.clnesp.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Cuesta F., Formiga F., Lopez-Soto A., Masanes F., Ruiz D., Artaza I., Salvà A., Serra-Rexach J.A., Rojano I., Luque X., et al. Prevalence of Sarcopenia in Patients Attending Outpatient Geriatric Clinics: The ELLI Study. Age Ageing. 2015;44:807–809. doi: 10.1093/ageing/afv088. [DOI] [PubMed] [Google Scholar]
- 11.Salvà A., Serra-Rexach J.A., Artaza I., Formiga F., Rojano I., Luque X., Cuesta F., López-Soto A., Masanés F., Ruiz D., et al. Prevalence of Sarcopenia in Spanish Nursing Homes: Comparison of the Results of the ELLI Study with Other Populations. Rev. Esp. Geriatr. Gerontol. 2016;51:260–264. doi: 10.1016/j.regg.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Bianchi L., Abete P., Bellelli G., Bo M., Cherubini A., Corica F., Di Bari M., Maggio M., Manca G.M., Rizzo M.R., et al. Prevalence and Clinical Correlates of Sarcopenia, Identified According to the EWGSOP Definition and Diagnostic Algorithm, in Hospitalized Older People: The GLISTEN Study. J. Gerontol. A Biol. Sci. Med. Sci. 2017;72:1575–1581. doi: 10.1093/gerona/glw343. [DOI] [PubMed] [Google Scholar]
- 13.Mayhew A.J., Amog K., Phillips S., Parise G., McNicholas P.D., de Souza R.J., Thabane L., Raina P. The Prevalence of Sarcopenia in Community-Dwelling Older Adults, an Exploration of Differences between Studies and within Definitions: A Systematic Review and Meta-Analyses. Age Ageing. 2019;48:48–56. doi: 10.1093/ageing/afy106. [DOI] [PubMed] [Google Scholar]
- 14.Simsek H., Meseri R., Sahin S., Kilavuz A., Bicakli D.H., Uyar M., Savas S., Sarac F., Akcicek F. Prevalence of Sarcopenia and Related Factors in Community-Dwelling Elderly Individuals. Saudi Med. J. 2019;40:568–574. doi: 10.15537/smj.2019.6.23917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bahat G., Tufan A., Kilic C., Karan M.A., Cruz-Jentoft A.J. Prevalence of Sarcopenia and Its Components in Community-Dwelling Outpatient Older Adults and Their Relation with Functionality. Aging Male Off. J. Int. Soc. Study Aging Male. 2018;23:424–430. doi: 10.1080/13685538.2018.1511976. [DOI] [PubMed] [Google Scholar]
- 16.Masanes F., Culla A., Navarro-Gonzalez M., Navarro-Lopez M., Sacanella E., Torres B., Lopez-Soto A. Prevalence of Sarcopenia in Healthy Community-Dwelling Elderly in an Urban Area of Barcelona (Spain) J. Nutr. Health Aging. 2012;16:184–187. doi: 10.1007/s12603-011-0108-3. [DOI] [PubMed] [Google Scholar]
- 17.Guillamón-Escudero C., Diago-Galmés A., Tenías-Burillo J.M., Soriano J.M., Fernández-Garrido J.J. Prevalence of Sarcopenia in Community-Dwelling Older Adults in Valencia, Spain. Int. J. Environ. Res. Public Health. 2020;17:9130. doi: 10.3390/ijerph17239130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X., Zhang W., Wang C., Tao W., Dou Q., Yang Y. Sarcopenia as a Predictor of Hospitalization among Older People: A Systematic Review and Meta-Analysis. BMC Geriatr. 2018;18:188. doi: 10.1186/s12877-018-0878-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sobestiansky S., Michaelsson K., Cederholm T. Sarcopenia Prevalence and Associations with Mortality and Hospitalisation by Various Sarcopenia Definitions in 85–89 Year Old Community-Dwelling Men: A Report from the ULSAM Study. BMC Geriatr. 2019;19:318. doi: 10.1186/s12877-019-1338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rizzoli R., Reginster J.-Y., Arnal J.-F., Bautmans I., Beaudart C., Bischoff-Ferrari H., Biver E., Boonen S., Brandi M.-L., Chines A., et al. Quality of Life in Sarcopenia and Frailty. Calcif. Tissue Int. 2013;93:101–120. doi: 10.1007/s00223-013-9758-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Puts M.T.E., Shekary N., Widdershoven G., Heldens J., Lips P., Deeg D.J.H. What Does Quality of Life Mean to Older Frail and Non-Frail Community-Dwelling Adults in the Netherlands? Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2007;16:263–277. doi: 10.1007/s11136-006-9121-0. [DOI] [PubMed] [Google Scholar]
- 22.Sieber C.C. Malnutrition and Sarcopenia. Aging Clin. Exp. Res. 2019;31:793–798. doi: 10.1007/s40520-019-01170-1. [DOI] [PubMed] [Google Scholar]
- 23.Cruz-Jentoft A.J., Kiesswetter E., Drey M., Sieber C.C. Nutrition, Frailty, and Sarcopenia. Aging Clin. Exp. Res. 2017;29:43–48. doi: 10.1007/s40520-016-0709-0. [DOI] [PubMed] [Google Scholar]
- 24.Greco E.A., Pietschmann P., Migliaccio S. Osteoporosis and Sarcopenia Increase Frailty Syndrome in the Elderly. Front. Endocrinol. Lausanne. 2019;10:255. doi: 10.3389/fendo.2019.00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beaudart C., Biver E., Reginster J.-Y., Rizzoli R., Rolland Y., Bautmans I., Petermans J., Gillain S., Buckinx F., Dardenne N., et al. Validation of the SarQoL®, a Specific Health-Related Quality of Life Questionnaire for Sarcopenia. J. Cachexia Sarcopenia Muscle. 2017;8:238–244. doi: 10.1002/jcsm.12149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fábrega-Cuadros R., Martínez-Amat A., Cruz-Díaz D., Aibar-Almazán A., Hita-Contreras F. Psychometric Properties of the Spanish Version of the Sarcopenia and Quality of Life, a Quality of Life Questionnaire Specific for Sarcopenia. Calcif. Tissue Int. 2020;106:274–282. doi: 10.1007/s00223-019-00635-9. [DOI] [PubMed] [Google Scholar]
- 27.Montero-Errasquín B., Vaquero-Pinto N., Sánchez-Cadenas V., Geerinck A., Sánchez-García E., Mateos-Nozal J., Ribera-Casado J.M., Cruz-Jentoft A.J. Spanish Translation, Cultural Adaptation and Validation of the SarQoL®: A Specific Health-Related Quality of Life Questionnaire for Sarcopenia. BMC Musculoskelet. Disord. 2022;23:191. doi: 10.1186/s12891-022-05125-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malmstrom T.K., Morley J.E. SARC-F: A Simple Questionnaire to Rapidly Diagnose Sarcopenia. J. Am. Med. Dir. Assoc. 2013;14:531–532. doi: 10.1016/j.jamda.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 29.World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 30.Hamasaki H., Kawashima Y., Katsuyama H., Sako A., Goto A., Yanai H. Association of Handgrip Strength with Hospitalization, Cardiovascular Events, and Mortality in Japanese Patients with Type 2 Diabetes. Sci. Rep. 2017;7:7041. doi: 10.1038/s41598-017-07438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trosclair D., Bellar D., Judge L.W., Smith J., Mazerat N., Brignac A. Hand-Grip Strength as a Predictor of Muscular Strength and Endurance. J. Strength Cond. Res. 2011;25:S99. doi: 10.1097/01.JSC.0000395736.42557.bc. [DOI] [Google Scholar]
- 32.Gopinath B., Kifley A., Liew G., Mitchell P. Handgrip Strength and Its Association with Functional Independence, Depressive Symptoms and Quality of Life in Older Adults. Maturitas. 2017;106:92–94. doi: 10.1016/j.maturitas.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 33.Cooper C., Fielding R., Visser M., van Loon L.J., Rolland Y., Orwoll E., Reid K., Boonen S., Dere W., Epstein S., et al. Tools in the Assessment of Sarcopenia. Calcif. Tissue Int. 2013;93:201–210. doi: 10.1007/s00223-013-9757-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kyle U.G., Genton L., Hans D., Pichard C. Validation of a Bioelectrical Impedance Analysis Equation to Predict Appendicular Skeletal Muscle Mass (ASMM) Clin. Nutr. Edinb. Scotl. 2003;22:537–543. doi: 10.1016/S0261-5614(03)00048-7. [DOI] [PubMed] [Google Scholar]
- 35.Alvero-Cruz J.R., Correas Gómez L., Ronconi M., Fernández Vázquez R., Porta i Manzañido J. La Bioimpedancia Eléctrica Como Método de Estimación de La Composición Corporal, Normas Prácticas de Utilización. Rev. Andal. Med. Deporte. 2011;4:167–174. [Google Scholar]
- 36.Studenski S., Perera S., Patel K., Rosano C., Faulkner K., Inzitari M., Brach J., Chandler J., Cawthon P., Connor E.B., et al. Gait Speed and Survival in Older Adults. JAMA J. Am. Med. Assoc. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubio Castañeda F.J., Tomas Aznar C. Medición de La Actividad Física En Personas Mayores de 65 Años Mediante El IPAQ-E: Validez de Contenido, Fiabilidad y Factores Asociados. Rev. Esp. Salud Pública. 2017;91 [PubMed] [Google Scholar]
- 38.Roman-Viñas B., Serra-Majem L., Hagströmer M., Ribas-Barba L., Sjöström M., Segura-Cardona R. International Physical Activity Questionnaire: Reliability and Validity in a Spanish Population. Eur. J. Sport Sci. 2010;10:297–304. doi: 10.1080/17461390903426667. [DOI] [Google Scholar]
- 39.Salaffi F., Di Carlo M., Carotti M., Farah S., Giovagnoni A. Frailty Prevalence According to the Survey of Health, Ageing and Retirement in Europe-Frailty Instrument (SHARE-FI) Definition, and Its Variables Associated, in Patients with Symptomatic Knee Osteoarthritis: Findings from a Cross-Sectional Study. Aging Clin. Exp. Res. 2021;33:1519–1527. doi: 10.1007/s40520-020-01667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Romero Ortuño R. El Instrumento de Fragilidad Para Atención Primaria de La Encuesta de Salud, Envejecimiento y Jubilación En Europa (SHARE-FI): Resultados de La Muestra Española. Rev. Esp. Geriatría Gerontol. 2011;46:243–249. doi: 10.1016/j.regg.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 41.Donini L.M., Marrocco W., Marocco C., Lenzi A. Validity of the Self- Mini Nutritional Assessment (Self- MNA) for the Evaluation of Nutritional Risk. A Cross- Sectional Study Conducted in General Practice. J. Nutr. Health Aging. 2018;22:44–52. doi: 10.1007/s12603-017-0919-y. [DOI] [PubMed] [Google Scholar]
- 42.Cuerda C., Álvarez J., Ramos P., Abánades J.C., García-de-Lorenzo A., Gil P., De-la-Cruz J.J. Prevalence of Malnutrition in Subjects over 65 Years of Age in the Community of Madrid. The DREAM + 65 Study. Nutr. Hosp. 2016;33:101. doi: 10.20960/nh.101. [DOI] [PubMed] [Google Scholar]
- 43.Beaudart C., Edwards M., Moss C., Reginster J.-Y., Moon R., Parsons C., Demoulin C., Rizzoli R., Biver E., Dennison E., et al. English Translation and Validation of the SarQoL®, a Quality of Life Questionnaire Specific for Sarcopenia. Age Ageing. 2017;46:271–276. doi: 10.1093/ageing/afw192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beaudart C., Locquet M., Reginster J.-Y., Delandsheere L., Petermans J., Bruyère O. Quality of Life in Sarcopenia Measured with the SarQoL®: Impact of the Use of Different Diagnosis Definitions. Aging Clin. Exp. Res. 2018;30:307–313. doi: 10.1007/s40520-017-0866-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsekoura M., Kastrinis A., Katsoulaki M., Billis E., Gliatis J. Sarcopenia and Its Impact on Quality of Life. Adv. Exp. Med. Biol. 2017;987:213–218. doi: 10.1007/978-3-319-57379-3_19. [DOI] [PubMed] [Google Scholar]
- 46.Chen L.-K., Woo J., Assantachai P., Auyeung T.-W., Chou M.-Y., Iijima K., Jang H.C., Kang L., Kim M., Kim S., et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020;21:300–307.e2. doi: 10.1016/j.jamda.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 47.Rodriguez-Rejon A.I., Artacho R., Puerta A., Zuñiga A., Ruiz-Lopez M.D. Diagnosis of Sarcopenia in Long-Term Care Homes for the Elderly: The Sensitivity and Specificity of Two Simplified Algorithms with Respect to the EWGSOP Consensus. J. Nutr. Health Aging. 2018;22:796–801. doi: 10.1007/s12603-018-1004-x. [DOI] [PubMed] [Google Scholar]
- 48.Studenski S., Peters K., Alley D., Cawthon P., Mclean R., Harris T., Ferrucci L., Guralnik J., Fragala M., Kenny A., et al. The FNIH Sarcopenia Project: Rationale, Study Description, Conference Recommendations, and Final Estimates. J. Gerontol. A Biol. Sci. Med. Sci. 2014;69:547–558. doi: 10.1093/gerona/glu010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fielding R.A., Vellas B., Evans W.J., Bhasin S., Morley J.E., Newman A.B., Abellan van Kan G., Andrieu S., Bauer J., Breuille D., et al. Sarcopenia: An Undiagnosed Condition in Older Adults. Current Consensus Definition: Prevalence, Etiology, and Consequences. International Working Group on Sarcopenia. J. Am. Med. Dir. Assoc. 2011;12:249–256. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim M., Won C.W. Prevalence of Sarcopenia in Community-Dwelling Older Adults Using the Definition of the European Working Group on Sarcopenia in Older People 2: Findings from the Korean Frailty and Aging Cohort Study. Age Ageing. 2019;48:910–916. doi: 10.1093/ageing/afz091. [DOI] [PubMed] [Google Scholar]
- 51.Patel H.P., Syddall H.E., Jameson K., Robinson S., Denison H., Roberts H.C., Edwards M., Dennison E., Cooper C., Aihie Sayer A. Prevalence of Sarcopenia in Community-Dwelling Older People in the UK Using the European Working Group on Sarcopenia in Older People (EWGSOP) Definition: Findings from the Hertfordshire Cohort Study (HCS) Age Ageing. 2013;42:378–384. doi: 10.1093/ageing/afs197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang M., Liu Y., Zuo Y., Tang H. Sarcopenia for Predicting Falls and Hospitalization in Community-Dwelling Older Adults: EWGSOP versus EWGSOP2. Sci. Rep. 2019;9:17636. doi: 10.1038/s41598-019-53522-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martone A.M., Bianchi L., Abete P., Bellelli G., Bo M., Cherubini A., Corica F., Di Bari M., Maggio M., Manca G.M., et al. The Incidence of Sarcopenia among Hospitalized Older Patients: Results from the Glisten Study. J. Cachexia Sarcopenia Muscle. 2017;8:907–914. doi: 10.1002/jcsm.12224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Geerinck A., Dawson-Hughes B., Beaudart C., Locquet M., Reginster J.-Y., Bruyère O. Assessment of the Performance of the SarQoL® Questionnaire in Screening for Sarcopenia in Older People. Aging Clin. Exp. Res. 2021;33:2149–2155. doi: 10.1007/s40520-021-01913-z. [DOI] [PubMed] [Google Scholar]
- 55.Volpato S., Bianchi L., Cherubini A., Landi F., Maggio M., Savino E., Bandinelli S., Ceda G.P., Guralnik J.M., Zuliani G., et al. Prevalence and Clinical Correlates of Sarcopenia in Community-Dwelling Older People: Application of the EWGSOP Definition and Diagnostic Algorithm. J. Gerontol. A Biol. Sci. Med. Sci. 2014;69:438–446. doi: 10.1093/gerona/glt149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cruz-Jentoft A.J., Landi F., Schneider S.M., Zúñiga C., Arai H., Boirie Y., Chen L.-K., Fielding R.A., Martin F.C., Michel J.-P., et al. Prevalence of and Interventions for Sarcopenia in Ageing Adults: A Systematic Review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS) Age Ageing. 2014;43:748–759. doi: 10.1093/ageing/afu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Messier V., Rabasa-Lhoret R., Barbat-Artigas S., Elisha B., Karelis A.D., Aubertin-Leheudre M. Menopause and Sarcopenia: A Potential Role for Sex Hormones. Maturitas. 2011;68:331–336. doi: 10.1016/j.maturitas.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 58.Cevei M., Onofrei R.R., Cioara F., Stoicanescu D. Correlations between the Quality of Life Domains and Clinical Variables in Sarcopenic Osteoporotic Postmenopausal Women. J. Clin. Med. 2020;9:441. doi: 10.3390/jcm9020441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dorosty A., Arero G., Chamar M., Tavakoli S. Prevalence of Sarcopenia and Its Association with Socioeconomic Status among the Elderly in Tehran. Ethiop. J. Health Sci. 2016;26:389–396. doi: 10.4314/ejhs.v26i4.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cruz-Jentoft A.J., Baeyens J.P., Bauer J.M., Boirie Y., Cederholm T., Landi F., Martin F.C., Michel J.-P., Rolland Y., Schneider S.M., et al. Sarcopenia: European Consensus on Definition and Diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Marcell T.J. Sarcopenia: Causes, Consequences, and Preventions. J. Gerontol. A Biol. Sci. Med. Sci. 2003;58:911. doi: 10.1093/gerona/58.10.M911. [DOI] [PubMed] [Google Scholar]
- 62.Tarantino U., Baldi J., Celi M., Rao C., Liuni F.M., Iundusi R., Gasbarra E. Osteoporosis and Sarcopenia: The Connections. Aging Clin. Exp. Res. 2013;25:93–95. doi: 10.1007/s40520-013-0097-7. [DOI] [PubMed] [Google Scholar]
- 63.Chen L.-K., Liu L.-K., Woo J., Assantachai P., Auyeung T.-W., Bahyah K.S., Chou M.-Y., Chen L.-Y., Hsu P.-S., Krairit O., et al. Sarcopenia in Asia: Consensus Report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 2014;15:95–101. doi: 10.1016/j.jamda.2013.11.025. [DOI] [PubMed] [Google Scholar]
- 64.Dodds R.M., Murray J.C., Robinson S.M., Sayer A.A. The Identification of Probable Sarcopenia in Early Old Age Based on the SARC-F Tool and Clinical Suspicion: Findings from the 1946 British Birth Cohort. Eur. Geriatr. Med. 2020;11:433–441. doi: 10.1007/s41999-020-00310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.