Abstract
The mammalian heart is a four-chambered organ with systemic and pulmonary circulations to deliver oxygenated blood to the body, and a tightly regulated genetic network exists to shape normal development of the heart and its associated major arteries. A key process during cardiovascular morphogenesis is the septation of the outflow tract which initially forms as a single vessel before separating into the aorta and pulmonary trunk. The outflow tract connects to the aortic arch arteries which are derived from the pharyngeal arch arteries. Congenital heart defects are a major cause of death and morbidity and are frequently associated with a failure to deliver oxygenated blood to the body. The Pax transcription factor family is characterised through their highly conserved paired box and DNA binding domains and are crucial in organogenesis, regulating the development of a wide range of cells, organs and tissues including the cardiovascular system. Studies altering the expression of these genes in murine models, notably Pax3 and Pax9, have found a range of cardiovascular patterning abnormalities such as interruption of the aortic arch and common arterial trunk. This suggests that these Pax genes play a crucial role in the regulatory networks governing cardiovascular development.
Keywords: Pax3, Pax9, cardiovascular development
1. Cardiovascular Development
The heart is the very first organ to form in development and is responsible for providing the embryo with a sufficient supply of blood, via the aortic arch arteries, to support its growth. Different cells of diverse embryonic origins make up the cardiovascular system. The heart is mostly comprised from mesodermal cells with a contribution from the endoderm for specification and differentiation [1]. Multiple studies have shown that the heart is formed from distinct populations of progenitor cells termed the primary and secondary heart fields (reviewed in [2,3]). Briefly, cells from the first heart field form the left ventricle and are involved in atria formation, whereas cells from the second heart field contribute to formation of the outflow tract, right ventricle and atria. Initially, the outflow tract of the heart is formed with a single lumen, which subsequently becomes divided into the separate aorta and pulmonary trunk following the formation and remodelling of the outflow tract cushions; the precursors to the unidirectional valves that prevent blood flowing back to the heart. A protrusion from the dorsal wall of the aortic sac also contributes to the septation of the outflow tract, along with neural crest cells (NCC) which migrate to these tissues [4]. The aorta is transferred to the left ventricle and the pulmonary trunk links with the right ventricle.
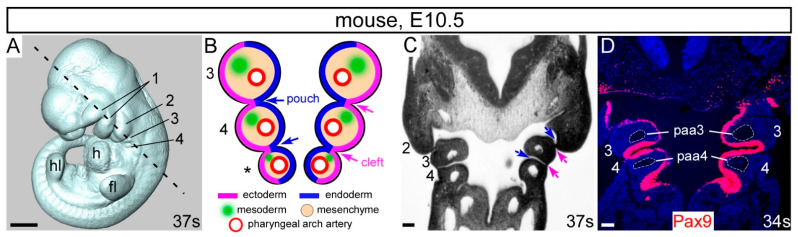
The aortic arch arteries, which comprise the aorta, subclavian and carotid arteries, are derived from the pharyngeal arch arteries which form within the pharyngeal arches. The pharyngeal arches are transient, evolutionary conserved structures in embryonic development and resemble bilateral pairs of swellings surrounding the embryonic foregut, developing in a rostral to caudal sequence [5] (Figure 1A). They are composed of diverse embryonic cell types, with an outer layer of ectoderm, an internal layer of endoderm, and a mesenchymal core composed of both NCC and mesoderm. Each arch is demarcated by endodermal pharyngeal pouches and ectodermal pharyngeal clefts (Figure 1B,C). The pharyngeal arches give rise to disparate specialist structures including vasculature, bone, cartilage, muscle and nerves, and derivatives of the third and fourth pharyngeal pouches: the thymus, thyroid and parathyroid glands, and the ultimobranchial bodies [5].
Figure 1.
The pharyngeal arches. (A) Mouse embryo at E10.5 with 37 somites (s) with the pharyngeal arches 1–4 labelled. (B) Schematic coronal overview of the tissues and structures of the 3rd, 4th and ultimate (*) pharyngeal arches. Pharyngeal arches are numbered, and pharyngeal pouches (blue arrows) and pharyngeal clefts (pink arrows) indicated. Each pharyngeal arch is filled with neural crest-derived mesenchyme. (C) Coronal section of the embryo in (A) with the section plane shown with a dotted line. (D) Coronal section of an E10.5 embryo immuno-stained with an anti-Pax9 antibody, specifically labelling the pharyngeal endoderm. The 3rd and 4th pharyngeal arch arteries are indicated. Abbreviations: ec, ectoderm; en, endoderm; fl, forelimb bud h, heart; hl, hindlimb bud; paa, pharyngeal arch artery. Scale bar: 500 µm in (A), 100 µm in (C,D).
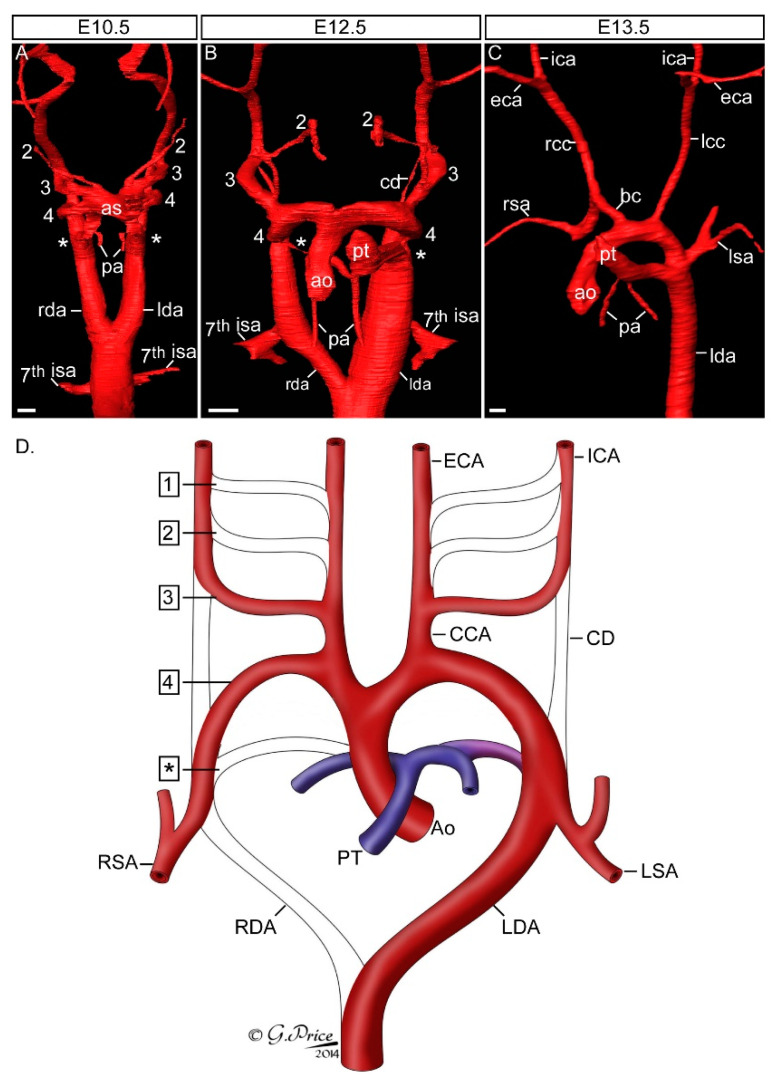
In mammals there are five pairs of pharyngeal arch arteries, numbered one to four, plus the ultimate artery of the pulmonary arch [6,7]. These arteries form sequentially within the mesenchyme of each pharyngeal arch and link the aortic sac to the dorsal aorta but are not all present at the same time in development. Together, they represent the foundations of the mature circulatory system, and undergo complex remodelling to produce the final asymmetric structure of the aortic arch arteries (Figure 2). This process starts with the first and second arch arteries forming first, at embryonic day (E) 8.5 in the mouse, but become interrupted shortly after with their distal parts subsequently forming the mandibular and hyoid arteries, and the proximal parts becoming the base of the external carotid arteries [7,8]. The third arch arteries form next (Figure 2A), and with extensive growth of the embryo in the anterior-posterior axis, remodel into the common carotid arteries and proximal parts of the internal carotid arteries. The distal parts of the internal carotids are formed from the paired dorsal aorta anterior to the carotid duct, which is the segment of the dorsal aorta between the third and fourth arch arteries and this involutes during the remodelling process. The fourth arch arteries on the right and left develop into distinct arch arteries. On the right, the fourth arch artery becomes the proximal portion of the right subclavian artery in conjunction with the right seventh intersegmental artery. The left fourth arch artery develops into the aortic arch. The ultimate arch artery is the last to form but the first to remodel (Figure 2B). On the right, following rotation and septation of the outflow tract, the vessel thins and disappears. On the left, the ultimate artery becomes the arterial duct, entering the descending aorta level with the left subclavian artery which is formed from the left seventh intersegmental artery (Figure 2C,D). This connection, present only in the foetus, allows blood to bypass the non-functioning, fluid filled lungs and closes shortly after birth, to allow for the delivery of deoxygenated blood to the lungs.
Figure 2.
Development of the aortic arch arteries. Mouse embryos were processed for high resolution episcopic microscopy [9] and the acquired datasets used to make three-dimensional reconstructions with Amira software. (A) At the E10.5 stage the mouse embryo has symmetrical pairs of pharyngeal arch arteries. The first arch artery has remodelled and is no longer visible, the second is interrupted, and the third, fourth and ultimate (*) arch arteries are symmetrical, of equal size and connect the aortic sac (as) with the paired left and right dorsal aorta (lda, rda). The future subclavian arteries, the 7th intersegmental arteries (isa), emanate from the paired dorsal aorta near the point of bifurcation. (B) By E12.5 remodelling of the pharyngeal arch arteries is underway. The outflow tract has separated into the aorta (ao) and pulmonary trunk (pt), the ultimate artery (*) has thinned on the right and expanded on the left. The region of the dorsal aorta between the third and fourth arteries, the carotid duct (cd), is involuting. The right dorsal aorta caudal to the 7th intersegmental artery is regressing. (C) At the fetal stage, E13.5 in the mouse, the arch arteries have completed remodelling to produce the mature aortic arch arteries configuration. (D) Schematic showing the pharyngeal arch arteries (numbered, on the (left)) and the arteries they develop into (labelled, on the (right)). Abbreviations: ao, aorta; as, aortic sac; bc, brachiocephalic artery; cca, common carotid artery; cd, carotid duct; eca, external carotid artery; ica, internal carotid artery; isa, intersegmental artery; lcc, left common carotid; lda, left descending aorta; lsa, left subclavian artery; pa, pulmonary artery; pt, pulmonary trunk; rcc, right common carotid; rda, right descending aorta; rsa, right subclavian artery. Scale bar, 100 µm. Figure adapted from [7].
NCC are a multipotent population of neuroectoderm derived cells that delaminate from the dorsal portion of the neural tube, undergo an epithelial-to-mesenchymal transition and migrate to target destinations where they differentiate into key cell types such as melanocytes, smooth muscle cells, craniofacial cartilage and bone and the peripheral nervous system. A sub-population of NCC, the cardiac neural crest cells (cNCC), migrate ventrally through the third, fourth and ultimate pharyngeal arches and contribute to outflow tract septation, formation of the valves and differentiate into the smooth muscle cells that invest around the aortic arch arteries that emanate from the heart [10]. In order to migrate, cNCC must navigate complex cellular and molecular interactions to reach their destination. The extracellular matrix regulates the movement of cNCC through the embryo along an equilibrium of permissive substrate components such as fibronectin and laminin, and non-permissive components such as proteoglycans [11].
2. Congenital Heart Defects
Congenital heart defects are a major driver of morbidity in childhood, with global incidence rates of approximately 0.8–1.2% in live-born infants [12,13], affecting the heart itself, the outflow tract region, or the aortic arch arteries. They are usually haemodynamically compatible with embryonic and foetal development as oxygenation of the blood by the lungs is not required. It is only following birth that abnormalities of the heart and the aortic arch arteries prevent oxygenated blood being delivered to the whole body. For example, when the outflow tract fails to separate into the aorta and pulmonary trunk, a single lumen tract remains, known as a common arterial trunk (also known as persistent truncus arteriosus) [14]. Another outflow tract defect, is where the aorta is not transferred to the left ventricle and remains in communication with the right ventricle along with the pulmonary trunk, giving double outlet right ventricle [15]. If the fourth pharyngeal arch arteries do not form correctly this can result in interruption of the aortic arch and an aberrant, frequently retro-oesophageal, right subclavian artery [7]. The importance of cNCC in cardiovascular development was illustrated by the surgical ablation of the neural crest prior to its migration that resulted in conotruncal abnormalities such as common arterial trunk and aortic arch artery patterning defects [16,17]. Furthermore, genetic ablation of NCC using diphtheria toxin or thymidine kinase sensitivity also results in cardiovascular outflow tract and aortic arch artery abnormalities [18,19,20].
3. Pax Genes in Development
All members of the Pax gene family contribute to organ development during embryogenesis through a wide range of actions influencing cell fate, apoptosis and differentiation [21,22]. The Pax genes are regulators of gene expression and are characterised by a highly conserved DNA binding paired domain and a C-terminal transcriptional regulatory domain [23]. The Pax genes are further subdivided depending on the presence or absence of additional motifs such as an octapeptide region and a paired-type homeodomain. Pax proteins are essential for eye, kidney, thyroid, skeleton, muscle, lymphocyte and pancreas endocrine cell formation, but only Pax3 and Pax9 have been found to be crucial in cardiovascular development.
3.1. Pax3 in Cardiovascular Development
The genetic alteration of Pax3 in mouse models causes defects associated with neural crest derivatives and cardiovascular malformations. Pax3 is a 479 amino acid protein which maps to chromosome 1 in the mouse and has 97.5% homology at the protein level to human PAX3, which is found on chromosome 2. The Pax3 protein contains a paired-domain, octapeptide motif, and a paired-type homeodomain (Table 1). Pax3 mRNA transcripts are first identified from E6.5 in mouse embryo development and localised to the dorsal section of the neuroepithelium and part of the dermomyotome by E8.5. Pax3 becomes more widely expressed throughout other parts of the embryo, such as the NCC, between E9.5 and E12.5 and Pax3 transcripts are no longer expressed by E17.5 [24,25].
Table 1.
Structure and expression of Pax genes discussed in this review.
| Gene | Protein Domains | Class | Human | Mouse | Expression | Human Cardiac Defects | ||
|---|---|---|---|---|---|---|---|---|
| Paired | Oct | Homeo | ||||||
| Pax1 |
|
1 | 20p11 | 2 | Pharyngeal endoderm, sclerotome | None | ||
| Pax9 | 14q12-13 | 12 | PAD, IAA, BAV, VSD | |||||
| Pax3 |
|
3 | 2q35 | 1 | Neural crest cells, dermomyotome | ASD, VSD | ||
| Pax7 | 1p36 | 4 | None | |||||
Abbreviations: ASD, atrial septal defect; BAV, bicuspid aortic valve; IAA, interrupted aortic arch; Homeo, paired-type homeodomain; Oct, octapeptide; PAD, patent arterial duct; VSD, ventricular septal defect.
3.1.1. Splotch Mouse Models
Pax3 is the gene affected in mice where the Splotch locus has been mutated. Mice homozygous for Splotch mutations display a range of defects affecting the neural tube, NCC and their derivatives, making Splotch mutant mice a widely used model to study defects of neural tube development, such as spina bifida, exencephaly, and Waardenburg syndrome [26]. The most prominent cardiovascular phenotype seen across the range of Splotch mutant embryos is the failure of outflow tract septation resulting in common arterial trunk [4]. It is the role of Pax3 within the NCCs that is critical for outflow tract septation, as well as other NCC dependent organs derived from the pharyngeal arches. A key characteristic shared by all variants of Splotch heterozygous mutant mice is the presence of a white spot on the belly, caused by improper Pax3 regulation of NCC-derived melanocyte development [27].
Multiple mutations of the Splotch locus, encompassing alterations or deletions that include Pax3, have been identified and are known as Splotch (Sp, Sp1H, Sp2H, Sp4H), Splotch-retarded (Spr) and Splotch-delayed (Spd) (Table 2) [28,29,30,31,32], with many other Splotch and “Splotch-like” mutations also having been studied [29,33,34,35,36,37]. The Sp and Spd mutations arose spontaneously, and the others were induced through x-ray mutagenesis although Sp1H and Sp2H likely share the same mutation as both were isolated from the same mutagenised male [26,31]. Mice homozygous for the Sp mutation, and also the Sp1H and Sp2H mutations, die at day 14 of gestation with defects affecting the lumbosacral and cranial neural tube, neural crest-derived tissues and the cardiovascular system [38,39,40,41]. Mice frequently present with a common arterial trunk emanating from the right ventricle and accompanied by an interventricular communication (or ventricular septal defect). The cardiovascular phenotype, however, may vary depending on the mutation within the Splotch locus, or the genetic background of the mice analysed. For example, on a mixed C3H/101 × C57Bl6 background, the majority of Sp1H homozygous mutants have common arterial trunk, although occasionally some embryos may only present with double outlet right ventricle [42]. Mutant Sp1H embryos also display aortic arch artery patterning defects such as abnormal regression of the ultimate arch artery, retro-oesophageal right subclavian artery and aberrant formation of the common carotid arteries, although these are seen with variable penetrance [42]. Defects affecting the derivatives of the third and fourth pharyngeal arches are also observed in Sp1H mutants, including aberrant positioning or non-formation of the thymus, absent ultimobranchial bodies, and malformations affecting the thyroid and parathyroid glands [42]. The Sp2H allele also causes variable penetrance of cardiovascular defects in homozygous mutants. Although all Sp2H/Sp2H mutants, on a mixed C3H/101 × CBA/Ca background, present with neural tube defects, either spina bifida, exencephaly, or both, only 60% of mutants have an outflow tract defect, with the majority having a common arterial trunk, and a minority with double outlet right ventricle, all associated with an interventricular communication. The remaining 40% of Sp2H/Sp2H mutants do not have cardiovascular defects but die perinatally with signs of cardiac failure [43]. The caudal pharyngeal arch arteries are also hypoplastic [44].
Table 2.
Pax3 mutant alleles.
| Allele | Mutation in Pax3 | Cardiovascular Defect When Homozygous |
Reference |
|---|---|---|---|
| Sp | Splice acceptor site in intron 3. Exon 4 not translated. | CAT, VSD | [40,45] |
| Sp1H | 32bp deletion in exon 5 |
CAT, DORV, VSD, abnormal arch arteries a |
[42] |
| Sp2H | CAT, DORV, VSD, arch arteries, congestive heart failure a |
[43,44] | |
| Sp4H | Deletion on Chromosome 1 between Epha4 and Cul3 (3.1 Mb) | ND, early embryonic death | [46] |
| Spd | Pax3 G42R | DORV, VSD | [26] |
| Spr | Deletion on Chromosome 1 between Vil1 and Akp3 (12.6 Mb) | ND, early embryonic death | [47] |
| Pax3 Δ 5 | Deletion of exon 5 | CAT, VSD, absent left ultimate arch artery |
[20] |
| Pax3 Δ 5 ;AP-2aCre | Deletion of exon 5 in NCC |
DORV, VSD | |
| Pax3Cre | Replacement of exon 1 with Cre | CAT, DORV, VSD a | [48] |
| Pax3neo | Neomycin cassette inserted in intron 5 (hypomorphic allele) |
No cardiovascular defects | [49] |
| Pax3neo;Pax3 Δ 5 ;Pax7+/− |
Pax3 hypomorph (10%) and Pax7 heterozygous (50%) |
CAT, DORV, VSD a | [50] |
| Pax3neo;Pax3 Δ 5 ;Pax7−/− | Pax3 hypomorph (10%) and Pax7-null | CAT, VSD | |
| Pax3NCE | Deletion of NCC enhancer element |
CAT, VSD | [51] |
| Pax3-FKHR | Pax3-Foxo1 fusion protein |
CAT, DORV, VSD | [52] |
a defects are not fully penetrant. Abbreviations: CAT, common arterial trunk; DORV, double outlet right ventricle; NCC, neural crest cell; ND, not determined; TV, tricuspid valve; VSD, ventricular septal defect.
Mutant mice with a large chromosomal deletion that includes the Splotch locus die early in development, before the cardiovascular system has formed. Mice homozygous for the Sp4H mutation have arrested development around E6.0 and an increased proportion of embryo resorptions are seen [29,46]. This early lethality of Sp4H mutants is believed to be influenced by the deletion of another gene within the affected region rather than solely due to the loss of Pax3, since the null allele found in Sp1H and Sp2H mutant mice does not cause early embryonic death [46]. For example, mice deficient for Cul3, which is in the deleted region, die before E7.5 with defects in mitosis [53]. Spr homozygotes are lethal before the preimplantation stage of development [45] possibly due to the deletion of surrounding flanking markers such as Vil1 and Inha, which are essential for the progression to implantation [45,47].
Of all the Splotch mutations, the Spd phenotype can be described as the least severe, with homozygous mutants typically surviving to full term before dying perinatally with a reduction in the size and number of spinal ganglia [54]. Spina bifida also develops due to the abnormality in interactions between the layers of embryonic tissues leading to faults with neural tube closure. Spd homozygous mutants also typically present with double outlet right ventricle, and in Sp1H/Spd double heterozygous compound mutants around 50% of fetuses had common arterial trunk [54].
3.1.2. Pax3 Mouse Models
An engineered genetic alteration of the Pax3 allele that deletes exon 5 (Pax3Δ5), creating a premature stop codon and loss of the Pax3 homeodomain, is genetically analogous to the Sp2H allele [55]. Homozygous mutants, on a C57BL6 background, display a cardiovascular phenotype of common arterial trunk and interventricular communication with 100% penetrance at E14.5 [20]. In these mutants, malformations of the caudal pharyngeal arch arteries were seen at E11.5, with abnormal regression of the left ultimate arch artery in the mutants which may explain the formation of the common arterial trunk [20]. Additionally, cNCC migration was disorganized with reduced numbers seen in the pharyngeal arches and outflow tract [20].
Through targeting of cDNA sequences of the transcription factor Forkhead Box O1 (FKHR) in the Pax3 locus of mouse embryonic stem cells, a Pax3-FKHR knock-in allele and consequential Pax3-FKHR fusion protein was generated [52]. In this fusion protein, the C-terminal transcriptional transactivation sequence of Pax3 is replaced with the bisected DNA binding domain of FKHR, which is a stronger transactivating sequence, giving the fusion protein the ability to bind homeodomain sites alone. Interestingly, heterozygous offspring of the chimeric mice were found to die at around the time of birth with a range of developmental abnormalities including cardiovascular defects partially resembling those seen in Sp2H mice [43]. The fusion protein was expressed at a significantly reduced level compared to the wild-type expression of Pax3 in embryogenesis, suggesting that a dominant negative effect on the Pax3 gene is contributing to the observed phenotype. It was deduced that the cause of neonatal death was a combination of defects such as ventricular septal defects and tricuspid valve insufficiency, ultimately causing congestive heart failure.
A novel Splotch allele was created by replacing the first exon of Pax3 with the Cre recombinase gene. Homozygous mutants on a mixed C57BL/6 × 129Sv genetic background displayed the typical Splotch phenotype although the outflow tract defects of common arterial trunk and double outlet right ventricle observed were not fully penetrant [48]. The Pax3Cre allele also allowed for lineage tracing and identified novel Pax3 expression in hindgut and urogenital epithelium.
3.1.3. Pax3 Interaction with Pax7
Mutant mice with a hypomorphic allele of Pax3 (Pax3neo), which produces only 20% of normal transcripts when homozygous, do not have neural tube or cardiovascular defects [49]. Pax3neo;Pax3Δ5 mutants with 10% of normal Pax3 levels, however, have neural tube defects, but the outflow tract of the heart was septated normally [50]. Pax3 shares some overlapping embryonic expression domains with Pax7 in NCC (9,10). Although both these genes share a similar protein structure (Table 1), Pax7-null mice are phenotypically unaffected [56]. Pax3 acts to repress Pax7 in normal development as in Pax3 mutants Pax7 is upregulated [50,56]. Mice double null for Pax3 and Pax7 die earlier than Pax3-nulls at E11.5 with more severe neural tube defects, suggesting redundancy between these two genes [57]. Compound mutant mice were engineered to produce 10% levels of Pax3 and reduced amounts of Pax7 [50]. In Pax3neo;Pax3Δ5;Pax7+/− embryos common arterial trunk and double outlet right ventricle phenotypes were observed in half of the mutants examined. When embryos were produced that were also deficient for Pax7 (i.e., Pax3neo;Pax3Δ5;Pax7−/−), however, all of the mutants presented with common arterial trunk. This study therefore demonstrated that a threshold of Pax3 expression of >10% is required for correct outflow tract formation, and Pax7 compensates for loss of Pax3 in cardiovascular development through upregulated expression [50].
3.1.4. Pax3 Interaction with Foxd3
Foxd3 is a forkhead transcription factor, and similar to Pax3, is an early regulator of neural crest progenitor cells. Foxd3 deficiency results in early embryonic lethality at around E6.5 [58], and conditional deletion from the NCC leads to a reduction in the number of NCC and cardiovascular defects such as abnormal aortic arch arteries and common arterial trunk in a minority of mutants [59,60]. When Pax3 expression is heterozygous in conjunction with Foxd3 loss in the NCC, however, common arterial trunk is seen in all mutants [60] and resembles the phenotype seen in the NCC ablation model [18]. Foxd3 directly binds to enhancers in the Pax3 locus [61] and Foxd3 expression is also reduced in Pax3Sp/Sp mutants [62], suggesting it functions downstream of Pax3 and therefore may be involved in a feedback loop mechanism.
3.1.5. Pax3 Interaction with Msx2
Msx2 is a transcription factor expressed in a range of tissues and organs, including the dorsal neural tube and the neural crest [63]. Msx2-deficient mice have defects in endochondral bone formation as well as aberrant tooth and mammary gland development [64]. Msx2 is functionally redundant with Msx1 (which interacts with Pax9 as described below), and mice lacking both Msx2 and Msx1 have cardiovascular defects [65,66,67]. Whilst Splotch mutants die at E13.5, Pax3;Msx2 double null mutants survive to the neonatal stage and do not present with cardiovascular defects [68]. In normal development, Pax3 binds to the promoter of Msx2 to repress its expression in a NCC-specific manner, and in the absence of Pax3, Msx2 is upregulated and disrupts NCC development [68].
3.1.6. Pax3 Interaction with Sox10
Sox10, an SRY-box transcription factor, physically interacts with Pax3 [69] and mutations in both genes are known to be involved in Waardenburg syndrome in humans [70]. Patients typically present with NCC related defects such as hearing loss and pigmentation abnormalities, and in rare cases, also congenital heart abnormalities such as atrial and ventricular septal defects [71,72].
3.1.7. Pax3 Interaction with Tbx18
Tbx18 physically interacts with Pax3 to cooperatively regulate gene expression in the paraxial mesoderm [73]. Tbx18 deficient mice die perinatally with multiple defects that include the pleuropericardial membranes, the sinus node, epicardium and coronary vasculature of the heart [74,75,76,77].
3.1.8. Pax3 and Neural Crest Cells
RNA analysis experiments have demonstrated that the expression of Pax3 can be used as a marker of cNCC in the mouse embryo until the time of their entry into the outflow tract [43]. In homozygous Sp2H/Sp2H embryos the mutant variant of Pax3 is expressed in the neural tube, but migration of cNCC at E10.5 is defective with reduced cell numbers seen to migrate through the third, fourth and ultimate pharyngeal arches and a failure to arrive at their intended destination in the outflow tract [43]. The role of Pax3 in the migration and function of cNCC seems to be cell autonomous, as homozygous Sp/Sp mutant mice, with a transgenic overexpression of Pax3 in cNCC driven by a 1.6kb Pax3 regulatory region, allowed for a phenotypic rescue of neural tube closure and cardiac developmental defects [40]. Conditional deletion of Pax3 from the neural crest, however, does not fully recapitulate the common arterial trunk defect [20]. When Pax3 is deleted using the Wnt1Cre allele, which is active in migrating NCC, no outflow tract defects were seen, although just over half of all mutants displayed exencephaly. When an AP-2aCre allele was used, which is active earlier within the neural folds, all mutant embryos developed double outlet right ventricle and died perinatally. Pax3 is therefore required as a neural border specifier that is essential for premigratory NCC induction [78]. NCC in Splotch mutant mice proliferate normally but show altered migratory characteristics indicating that Pax3 is required for cNCC migration, perhaps through chemotropic responses to migratory cues or through the directionality and persistence of cell movement [79]. This may be controlled through an inhibition of p53 dependent processes during cNCC migration as it has been shown that neural tube closure defects and an increased rate of apoptosis in Sp/Sp embryos is p53 dependent [80,81]. Interestingly, the inactivation of p53 in Pax3-deficient embryos (i.e., Pax3−/−;p53−/−) leads to a rescue of the cNCC migration and outflow tract septation defects seen in Pax3-null embryos [81]. Furthermore, Pax3 inhibits p53 protein stability through stimulation of ubiquitination and degradation pathways independently of DNA-binding and transcriptional regulation [82]. Taken together, this suggests that Pax3 acts in the cNCC to inhibit p53-dependent processes that lead to apoptosis, thus allowing for optimal migration of cNCC to enable normal septation of the outflow tract of the heart. The upstream region of the Pax3 gene in mice contains two evolutionary conserved elements that are vital for Pax3 expression in the neural crest [83,84]. Mice engineered to replace this neural crest element (NCE), with a loxP flanked neomycin cassette, creates a null or severely hypomorphic Pax3 allele and homozygous mutants develop neural tube defects and common arterial trunk, thereby recapitulating the phenotype seen in the majority of Splotch mutants [51]. When the neomycin gene is removed, however, homozygous Pax3NCE mutant mice develop normally indicating that the neomycin cassette itself was disrupting Pax3 expression.
3.2. Pax9 in Cardiovascular Development
Pax9 is a transcription factor important for multiple aspects of embryogenesis, controlling craniofacial, skeletal and pharyngeal development [85,86] and has more recently been shown to be crucial for cardiovascular morphogenesis [87,88,89]. In humans, PAX9 is found on chromosome 14 and consists of 342 amino acids, with an N-terminal paired DNA-binding domain, an octapeptide motif, but no additional homeodomain (Table 1). In the mouse, Pax9 is found on chromosome 12 and has 343 amino acids. Human and mouse PAX9 have 98% homology at the protein level.
3.2.1. Pax9 in the Pharyngeal Endoderm
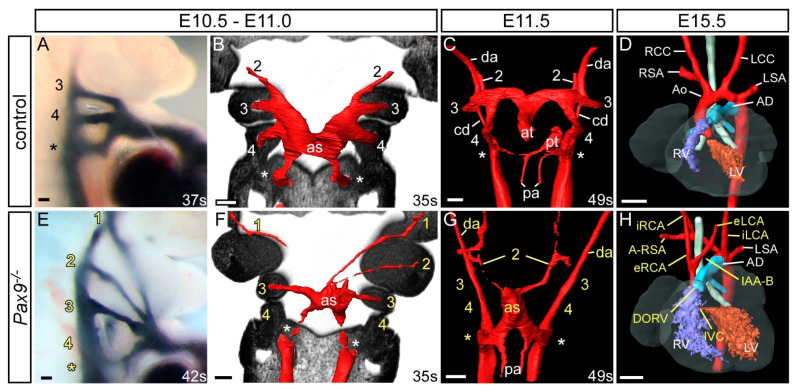
Pax9 is expressed throughout the developing embryo beginning at E8.5 in the mouse in the foregut epithelium and becoming specific to the pharyngeal endoderm by E9.5 (Figure 1D). Pax9 is expressed in the endoderm of the first four pharyngeal pouches by mid-embryogenesis, before eventually being expressed throughout the developing embryo in the craniofacial region and skeleton [90]. In equivalently staged human embryos, however, expression was only seen in the third and fourth pouches [91]. Pax9 is critical for skeletal and craniofacial development as mice deficient for Pax9 die perinatally with preaxial digit duplications, cleft secondary palate and oligodontia. Pax9-null mice also lack the thymus, parathyroids and ultimobranchial bodies, all derivatives of the third and fourth pharyngeal pouches which arrest in development by E11.5 [85]. Mice deficient for Pax9 on a C57Bl/6 genetic background die neonatally from severe cardiovascular defects, which include double-outlet right ventricle, interrupted aortic arch, retroesophageal origin of the right subclavian artery, and absent common carotid arteries (Figure 3) [88]. They also have hypoplasia of the ascending aorta and bicuspid aortic valve. The phenotypes involving the aortic arch and the subclavian artery are due to bilateral failure of the fourth arch arteries to form (Figure 3E–G). Although no complete vessel is observed, it is possible to find isolated endothelial cells within the fourth arches. The absence of the common carotid arteries reflects the collapse of the third arch arteries (Figure 3E–G). These vessels form bilaterally, but by E11.5, during the phase of remodelling, the vessels begin to degenerate, at least in part, through the lack of investment of the smooth muscle cells derived from the neural crest. This may relate directly to the significant reduction in the number of NCC migrating into the pharyngeal arches. Indeed, in another genetic mouse model where Msx1 haploinsufficiency was coupled with Pax9 deficiency (see below), the number of migrating NCC was normalized, the arteries of the third arch were invested with smooth muscle cells, and the common carotid arteries were preserved [89]. Interestingly, on a CD1 genetic background, Pax9-null mice had a significantly lower incidence of double outlet right ventricle and bicuspid aortic valve compared to those on the C57Bl/6 background, although the penetrance of arch artery defects was similar [89]. This suggests that genetic modifiers may play a role in the penetrance of the Pax9 related outflow tract defects, perhaps by influencing second heart field progenitor cells. Inactivation of Pax9 in NCC using Wnt1Cre mice and Pax9-floxed alleles caused cleft secondary palate and tooth agenesis and revealed that the Pax9 expressing mesenchymal cells of the nose, palate, and teeth are derived from NCC [92]. Pax9, however, does not have a cell autonomous role within the cNCC, as Wnt1Cre conditional deletion of Pax9 does not result in any cardiovascular defects [88].
Figure 3.
Cardiovascular developmental defects in Pax9-null mouse embryos. Control (A–D) and Pax9-null (Pax9−/−; E–H) mouse embryos were collected at different developmental stages and analysed for cardiovascular defects using intracardiac ink injections (A,E), high resolution episcopic microscopy (B,C,F,G) and magnetic resonance imaging (D,H). Control embryos at E10.5-E11.0 have the 3rd, 4th and ultimate (*) arch arteries patent to ink, are symmetrical in appearance and the 1st and 2nd have remodelled at this stage (A,B). In equivalently staged Pax9-null embryos the arch arteries are abnormal, with the 1st and 2nd persisting, the 3rd thin and the 4th absent (E,F). At E11.5 the caudal arch arteries of control embryos start to remodel, with the outflow tract septated and the right ultimate arch artery (*) regressing (C), whereas in Pax9-null embryos outflow tract septation is delayed, the 3rd arch arteries have collapsed and the 1st and/or 2nd persist (G). By E15.5 the pharyngeal arch arteries have remodelled into the adult aortic arch artery configuration (D). Pax9-null embryos show multiple defects (H) including aberrant right subclavian artery (A-RSA), interrupted aortic arch (IAA), abnormal right and left internal and external carotid arteries (i/eRCA, i/eLCA) and double outlet right ventricle (DORV) with interventricular communication (IVC). Somite numbers (s) are indicated. Abbreviations: AD, arterial duct; as, aortic sac; at, aortic trunk; cd, carotid duct; da, dorsal aorta; LCC, left common carotid artery; LSA, left subclavian artery; LV, left ventricle; pa, pulmonary artery; pt, pulmonary trunk; RCC, right common carotid artery; RSA, right subclavian artery; RV, right ventricle. Scale bar: 100 µm in (A–C) and (E–G), 500 µm in (D,H). Figure adapted from [88].
In normal development, the arteries of the first and second arches have usually remodelled by E10.5 but in Pax9-null mutants these vessels aberrantly persist, being observed either bilaterally or unilaterally (Figure 3E,F) [88]. Whether expression of Pax9 is directly important for this aspect of remodelling, or if the changes are a consequence of the altered haemodynamics due to absence of the arteries of the fourth arch and collapse of those of the third, is currently unknown. Alteration of blood flow at mid-embryogenesis in both the mouse and chick has been shown to affect the morphogenesis of the arch arteries [93,94]. In the absence of the third and fourth arch arteries in the Pax9-null mutants, it is the persisting arteries of the first or second arches that form the external carotid arteries, which then arise directly from the ascending aorta (Figure 3H). The internal carotid arteries take their origin directly from the dorsal aorta, this vessel retaining its continuity due to the failure of involution of the carotid duct.
Cardiovascular developmental defects have been associated with patients harbouring chromosomal abnormalities such as deletions and translocations that include PAX9 Table 1). Patent foramen ovale, patent arterial duct and pulmonary hypertension have all been reported [95,96,97], alongside craniofacial defects or oligodontia. One particularly interesting case featured a patient with cardiovascular phenotypes similar to the Pax9-deficient mouse, with interrupted aortic arch, a bicuspid aortic valve, hypoplastic aorta and a ventricular septal defect [98]. The patient had a small (105kb) hemizygous deletion at 14q13 which removed just three genes: PAX9, NKX2-1 and NKX2-8. Mice deficient for either Nkx2-1 or Nkx2-9 (which is the NKX2-8 gene in mice) do not display any cardiovascular abnormalities [99,100]. PAX9, therefore, may be considered as a potential candidate gene for human congenital cardiac defects.
3.2.2. Pax9 Interaction with Tbx1
It is unlikely that Pax9 acts alone in the origination of signalling events from the pharyngeal endoderm. Instead, it is expected to function in a genetic network with co-regulated genes, as has been demonstrated by studies looking at the transcriptome of Tbx1-null embryos [101,102] where Pax9 was identified as being one of the many genes downregulated in this model. Analysis of the Pax9-null pharyngeal arch transcriptome revealed a reduction in Tbx1 expression, as well as a significant overlap with genes differentially expressed in Tbx1-null embryos, suggesting that Tbx1 and Pax9 might share a genetic network [88].
Hemizygosity of Tbx1 is understood to underly the cardiovascular defects in 22q11 Deletion Syndrome patients. Also known as DiGeorge Syndrome, this is the most common microdeletion syndrome with an incidence of 1:4000 births, and patients display a wide range of clinical pathologies including congenital cardiovascular defects [103,104]. Mice null for Tbx1 display cardiovascular developmental defects such as common arterial trunk, caused by the failure of the pharyngeal apparatus to form normally [105,106]. Mice heterozygous for Tbx1 present with defective fourth arch artery formation which leads to interruption of the aortic arch in a minority of mice, but aberrant right subclavian artery is more frequently seen [7,107]. To test for a genetic interaction between Pax9 and Tbx1, mice heterozygous for each gene were crossed together [88]. Only two Pax9;Tbx1 double heterozygous mice were identified at weaning (the expected number was 42), with the majority subsequently found to die on the day of birth with a much higher incidence of interruption of the aortic arch than seen in Tbx1 heterozygous mice. Tbx1 is expressed in all three germ layers of the pharyngeal arches—the endoderm, mesoderm and ectoderm. To confirm the site of the potential Tbx1-Pax9 interaction, a novel conditional Pax9Cre allele was created in mice and used in conjunction with Tbx1-floxed allele mice. Mice with a heterozygous conditional deletion of Tbx1 in the endoderm, which was simultaneously heterozygous for Pax9, displayed cardiovascular defects thereby demonstrating a functional interaction between the two genes in the pharyngeal endoderm [88].
3.2.3. Pax9 Interaction with Gbx2
The transcription factor Gbx2 is downregulated in Tbx1-null embryos [102] and has also been shown to genetically interact with Tbx1 [108]. Gbx2 is expressed in the pharyngeal endoderm concomitantly with Pax9 and Tbx1, and Gbx2 expression is downregulated in the pharyngeal pouch endoderm in Pax9-null embryos at E9.5 [87,88]. Given the identified functional relationship between Pax9 and Tbx1, the potential for Gbx2 to be a shared downstream target in a regulatory network with these genes was explored. A proportion of mice null for Gbx2 display cardiovascular defects such as aberrant right subclavian artery, double outlet right ventricle and interrupted aortic arch [109] although the latter defect was not observed in our study, but a left-right patterning defect was identified, with these differences attributed to the use of a different Gbx2 mutant allele [87]. In our study we investigated a genetic interaction between Pax9 and Gbx2 and found that fewer Pax9;Gbx2 double heterozygous mice than expected survived to weaning (59 observed, 77 expected) and had cardiovascular defects including interrupted aortic arch and aberrant right subclavian artery. When Gbx2-null mice were combined with Pax9 heterozygosity (i.e., Gbx2−/−;Pax9+/−) there was a statistically significant increase in the incidence of cardiovascular defects in total, and interrupted aortic arch specifically. Moreover, common arterial trunk was also observed in complex compound mutants (i.e., Gbx2−/−;Pax9+/− and Gbx2+/−;Pax9−/−), a defect not seen in either Pax9-null or Gbx2-null embryos. Collectively our data demonstrated that Pax9 and Gbx2 genetically interact in cardiovascular development, with defects seen in double heterozygous mice, and novel and more severe cardiovascular defects in compound mutants [87].
3.2.4. Pax9 Interaction with Msx1
Pax9 is co-expressed with Msx1 during craniofacial development, and mice null for Msx1 display overlapping palate and tooth phenotypes with Pax9-deficient mice [85,110]. Msx1 is a highly conserved homeobox gene that plays a role in transcriptional regulation in early development. Unlike Pax9-null mice, however, Msx1-null mice have a phenotypically normal cardiovascular system [110], despite being expressed in the endocardial cushions at E10.5 [111]. Msx1 is functionally redundant with Msx2, and mice deficient for Msx1 and Msx2 (i.e., Msx1−/−;Msx2−/−) die in late gestation with outflow tract defects as well as craniofacial malformations [65,66,67]. Msx1 and Pax9 proteins interact in in vitro assays [112], and compound Pax9 and Msx1 mutant mice demonstrate a synergistic interaction between these two proteins affecting lip and tooth development [113,114]. Pax9 and Msx1 are not co-expressed in the same cell types in the pharyngeal region at mid-embryogenesis in the mouse, however, as Pax9 is restricted to the endoderm, and Msx1 to NCC [85,89,111,115]. These two genes, however, do appear to influence cardiovascular development, despite the lack of overlapping expression in the pharyngeal arches, with Msx1 haploinsufficiency modifying the Pax9-null cardiovascular phenotype. In Pax9-null mice the fourth arch artery fails to form and the third arch arteries collapse, concomitant with a reduction in cNCC migration to the pharyngeal arches [88]. As described above, this leads to aortic arch artery defects such as interrupted aortic arch and retro-oesophageal right subclavian artery, from the absent fourth arch arteries, and absent common carotid arteries, from the loss of the third arch arteries. In mice deficient for Pax9 and simultaneously heterozygous for Msx1 (i.e., Pax9−/−;Msx1+/−), a significant reduction in the incidence of interrupted aortic arch and retro-oesophageal right subclavian artery when compared to Pax9-null mice was found [89]. Conversely, there was a significant increase in the less severe arch artery defects of cervical origins of the right subclavian artery and aortic arch. These latter defects arise when the fourth arch arteries are absent, but the third arch arteries are maintained and the carotid ducts persist, and these cervical vessels are theoretically compatible with a functional systemic circulation. These phenotypes were coupled with a rescue of the cNCC migrating into the third pharyngeal arches and therefore able to stabilise the third arch arteries by differentiating into the smooth muscle cells that envelop the remodelling vessels [89]. Pax9−/−;Msx1+/− mutant mice, however, did not survive after birth possibly through breathing defects associated with defective hyoid bone and thyroid cartilage formation [89]. Whilst it can be deduced that Msx1 and Pax9 interact in cardiovascular development, the mechanisms underlying this interaction are yet to be uncovered and it is anticipated that there are further genetic interactions involving other key genes involved in this.
3.2.5. Pax9 Gene Dosage
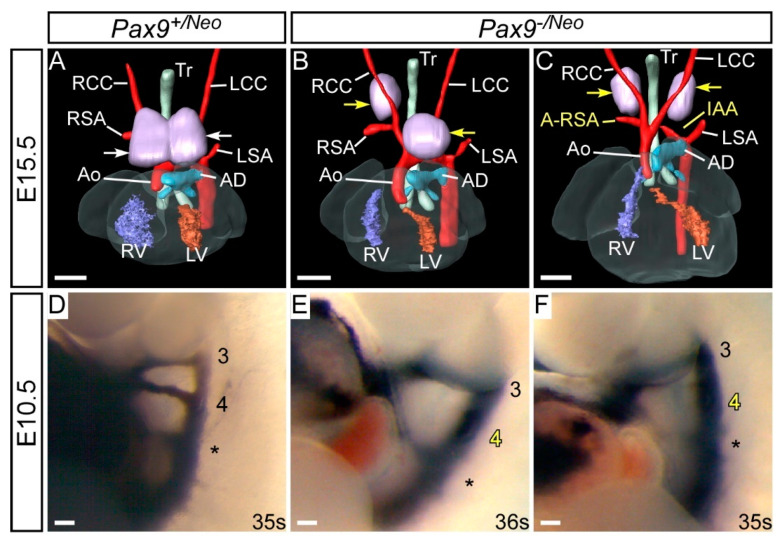
Pax9-heterozygous mice (i.e., Pax9+/−) are healthy and viable, suggesting that haploinsufficiency of Pax9 does not affect development. We reasoned that a further reduction in Pax9 levels may reveal a dosage sensitivity threshold that is crucial for correct cardiovascular development, as has been described with genetically altered Tbx1 alleles in mice [116]. Reduced levels of Pax9 were achieved using a hypomorphic allele of Pax9, which has a neomycin resistance cassette inserted between the second and third coding exons [117]. Mice homozygous for the hypomorphic allele (Pax9neo/neo) have ~20% of wild type Pax9 mRNA transcript levels and develop normally, except for displaying oligodontia. Interestingly mice heterozygous for the null allele have 32% of wild type Pax9 mRNA transcript levels instead of the predicted 50% levels. This indicates there are as yet undescribed feedback mechanisms at the molecular level that regulate Pax9 transcription during development. When the hypomorphic allele mice are crossed with Pax9+/− mice, the resulting Pax9−/neo mice have less than 10% wild type Pax9 mRNA levels [117] and, on a C57Bl/6 genetic background, do not survive long after birth.
To investigate these mice in more detail for a cause of death we examined Pax9−/neo embryos at E15.5 by magnetic resonance imaging (n = 14) and by intracardiac ink injection at E10.5 (n = 3). At E15.5, 64% of mutants (9/14) had a detectable cardiovascular defect, which all involved an aberrant right subclavian artery, either alone (3/14), with interrupted aortic arch (4/14), a right sided aorta (1/14), or double outlet right ventricle (1/14) (Figure 4B,C). All mutants presented with an abnormal thymus, where the lobes were either split and asymmetrically placed (9/14), hypoplastic (3/14) or absent (2/14). At E10.5, all fourth pharyngeal arch arteries (two per embryo, left and right) of the Pax9−/neo mutant embryos were abnormal, being either hypoplastic (1/6) or absent (5/6) (Figure 4E,F). These data demonstrated that even with very low levels of Pax9 mRNA, the cardiovascular system can develop without a high penetrance of abnormalities, although it is not known why all Pax9−/neo mutants die perinatally when a proportion show no signs of a severe arterial duct-dependent cardiovascular defect. It is, however, possibly due to the same mechanism that causes the death of Pax9;Msx1 mutants described above, but this requires further investigation. All embryos at E10.5 displayed bilateral fourth arch artery defects, but this incidence was not reflected in the mutants at E15.5, where only 64% had defects derived from the fourth arch arteries. This is analogous to the situation in Tbx1-heterozygous mice, where significantly fewer foetuses and neonates have fourth arch artery defects compared to those at mid-gestation suggesting that this vessel has the capacity to recover during development [7].
Figure 4.
Developmental defects in Pax9-hypomorphic mouse embryos. Pax9+/Neo control (A,D) and Pax9−/Neo mutant (B,C,E,F) mouse embryos were collected and analysed for cardiovascular defects using magnetic resonance imaging at E15.5 (A–C) and intracardiac ink injections at E10.5 (D–F). (A) Control embryo with normal cardiovascular anatomy and thymus lobes (white arrows). Pax9−/Neo mutant embryos have normal arch arteries (B) or display fourth pharyngeal arch artery derived defects such as aberrant right subclavian artery and interruption of the aortic arch (C). The thymus lobes are frequently abnormal (yellow arrows; (B,C)). (D) The third (3), fourth (4) and ultimate (*) pharyngeal arch arteries are of equivalent size and patent to ink in control embryos. (E,F) In stage-matched Pax9−/Neo mutant embryos the fourth arch arteries are frequently absent. Somite numbers (s) are indicated. Abbreviations: AD, arterial duct; Ao, aorta; A-RSA, aberrant right subclavian artery; IAA, interrupted aortic arch; RCC, LCC, right/left common carotid artery; RSA, LSA, right/left subclavian artery; RV, LV, right/left ventricle; Tr, trachea. Scale bar: 500 µm in (A–C), 100 µm in (D–F).
3.2.6. Pax1 Does Not Interact with Pax9 in Cardiovascular Development
Pax1 has a similar protein structure (Table 1) and high sequence homology to Pax9, they share promoter binding sites [90] and have overlapping expression in the pharyngeal endoderm in a range of organisms [86,118,119,120,121]. Pax1-null mice have skeletal defects affecting the vertebral column, sternum and scapula [122]. Mice homozygous null for Pax1 and Pax9 display developmental defects of the vertebral bodies, intervertebral discs and ribs [86], a more severe phenotype, therefore, than seen in Pax1-null mice. Patients suffering from Jarcho-Levin syndrome have severe skeletal defects and have reduced levels of Pax1 and Pax9 protein expression [123]. Using genetically mutated mice we have looked to see if Pax1 and Pax9 interact in cardiovascular development. We found that the heart and arch arteries of Pax1-null mice are normal, and loss of one or two Pax1 alleles in the context of Pax9 deficiency, does not alter the typical Pax9-null cardiovascular phenotype (Figure 5). Pax1 and Pax9 therefore do not genetically interact in cardiovascular development.
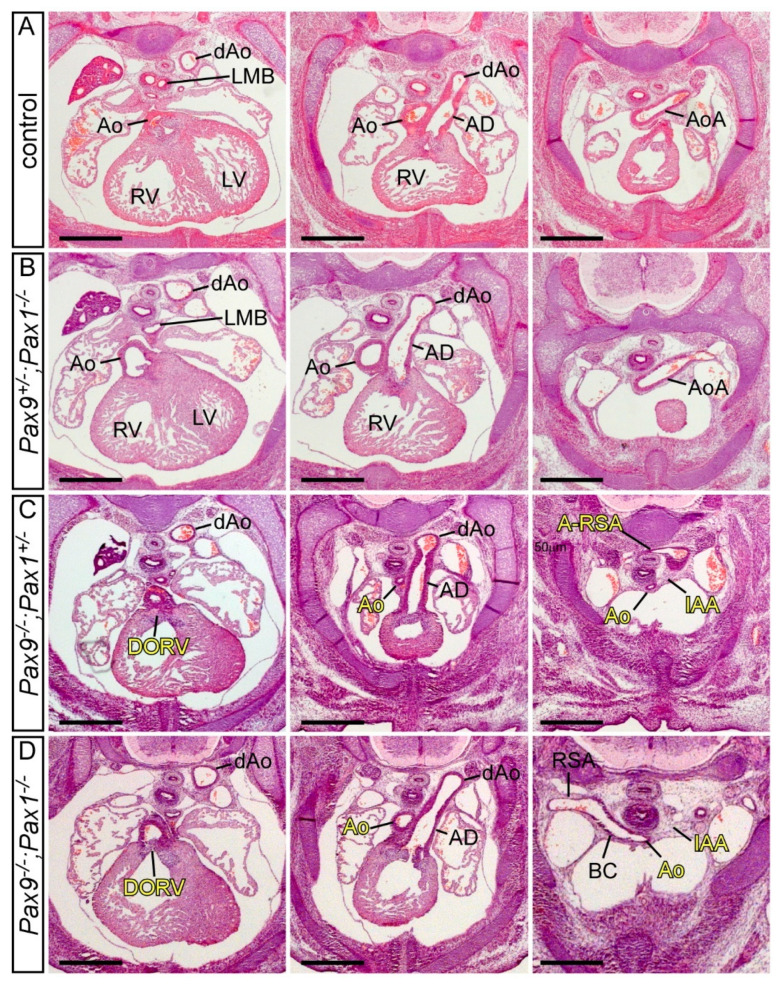
Figure 5.
Pax1 and Pax9 do not genetically interact in cardiovascular development. Transverse haematoxylin and eosin-stained sections of E14.5 embryos. (A) Control embryo with normal outflow tract and arch artery morphology with the aorta arising from the left ventricle and the aortic arch crossing over the left main bronchus to join the dorsal aorta. (B) Embryo null for Pax1 heterozygous for Pax9 (Pax9+/−; Pax1−/−) with normal cardiovascular development comparable to the control. (C) Embryo heterozygous for Pax1 and null for Pax9 (Pax9−/−;Pax1+/−) displaying the typical cardiovascular defects seen in Pax9-null embryos. The aorta arises aberrantly from the right ventricle producing a double outlet right ventricle (DORV). The aorta is hypoplastic, with an interruption of the aortic arch (IAA) and an aberrant retro-oesophageal right subclavian artery (A-RSA). (D) Homozygous Pax9;Pax1 null embryo (Pax9−/−;Pax1−/−) also with the typical Pax9-null cardiovascular defects, except with a normal right subclavian artery. Abbreviations: Ao, aorta; AoA, aortic arch; AD, arterial duct; BC, brachiocephalic artery; dAo, dorsal aorta; LMB, left main bronchus; LV, left ventricle; RSA, right subclavian artery; RV, right ventricle. Scale bar: 500 μm.
4. Concluding Remarks
Despite the Pax family consisting of nine genes all involved in embryonic development, only Pax3 and Pax9 play major roles in cardiovascular development involving NCC deficiencies, but through expression in different tissues. Pax3 acts cell autonomously in the NCC and is crucial for their migration and the subsequent septation of the outflow tract. In contrast, Pax9 is vital for pharyngeal arch artery morphogenesis possibly through influencing NCC migration non-cell autonomously to the pharyngeal arches. Pax9, furthermore, is also a major contributor in a complex genetic regulatory pathway underpinning morphogenesis of the aortic arch arteries that originates within the pharyngeal endoderm.
Author Contributions
R.E.S. and S.D.B. wrote and revised the manuscript. R.S. and H.M.P. reviewed and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Mice were used in accordance with the permissions on our project licence P0CD9CAB6 obtained from the UK Home Office under the revised Animals (Scientific Procedures) Act 1986, and all experimental protocols were approved by the Animal Welfare and Ethical Review Body at Newcastle University.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by research grants from the British Heart Foundation (FS/08/016/24741, PG/16/39/32115, FS/16/8/31984, PG/20/15/35041, FS/PhD/20/29032).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lough J., Sugi Y. Endoderm and heart development. Dev. Dyn. 2000;217:327–342. doi: 10.1002/(SICI)1097-0177(200004)217:4<327::AID-DVDY1>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 2.Stutt N., Song M., Wilson M.D., Scott I.C. Cardiac specification during gastrulation—The Yellow Brick Road leading to Tinman. Semin. Cell Dev. Biol. 2022;127:46–58. doi: 10.1016/j.semcdb.2021.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Kelly R.G. Molecular Mechanism of Congenital Heart Disease and Pulmonary Hypertension. Springer; Singapore: 2020. Advances in the Second Heart Field; pp. 301–307. [Google Scholar]
- 4.Anderson R.H., Chaudhry B., Mohun T.J., Bamforth S.D., Hoyland D., Phillips H.M., Webb S., Moorman A.F., Brown N.A., Henderson D.J. Normal and abnormal development of the intrapericardial arterial trunks in humans and mice. Cardiovasc. Res. 2012;95:108–115. doi: 10.1093/cvr/cvs147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Graham A., Richardson J. Developmental and evolutionary origins of the pharyngeal apparatus. Evodevo. 2012;3:24. doi: 10.1186/2041-9139-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson R.H., Bamforth S.D., Gupta S.K. How best to describe the pharyngeal arch arteries when the fifth arch does not exist? Cardiol. Young. 2020;30:1708–1710. doi: 10.1017/S1047951120003807. [DOI] [PubMed] [Google Scholar]
- 7.Anderson R.H., Bamforth S.D. Morphogenesis of the Mammalian Aortic Arch Arteries. Front. Cell Dev. Biol. 2022;10:892900. doi: 10.3389/fcell.2022.892900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hiruma T., Nakajima Y., Nakamura H. Development of pharyngeal arch arteries in early mouse embryo. J. Anat. 2002;201:15–29. doi: 10.1046/j.1469-7580.2002.00071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weninger W.J., Geyer S.H., Martineau A., Galli A., Adams D.J., Wilson R., Mohun T.J. Phenotyping structural abnormalities in mouse embryos using high-resolution episcopic microscopy. Dis. Models Mech. 2014;7:1143–1152. doi: 10.1242/dmm.016337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hutson M.R., Kirby M.L. Neural crest and cardiovascular development: A 20-year perspective. Birth Defects Res. C Embryo Today. 2003;69:2–13. doi: 10.1002/bdrc.10002. [DOI] [PubMed] [Google Scholar]
- 11.Henderson D.J., Copp A.J. Role of the extracellular matrix in neural crest cell migration. J. Anat. 1997;191:507–515. doi: 10.1046/j.1469-7580.1997.19140507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burn J., Goodship J. Congenital heart disease. In: Rimoin D.L., Connor J.M., Pyeritz R.E., Korf B.R., editors. Principles and Practice of Medical Genetics. Churchill Livingstone; London, UK: 2002. [Google Scholar]
- 13.Hoffman J.I., Kaplan S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002;39:1890–1900. doi: 10.1016/S0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 14.Johnson A.-L., Bamforth S.D. Molecular Pathways and Animal Models of Truncus Arteriosus. In: Rickert-Sperling S., Kelly R.G., Driscoll D.J., editors. Congenital Heart Diseases: The Broken Heart. Springer; Vienna, Austria: 2016. pp. 569–576. [Google Scholar]
- 15.Anderson R.H., Bamforth S.D., Spicer D.E., Henderson D.J., Chaudhry B., Brown N.A., Mohun T.J. Development and Maldevelopment of the Ventricular Outflow Tracts. In: Lacour-Gayet F., Bove E.L., Hraška V., Morell V.O., Spray T.L., editors. Surgery of Conotruncal Anomalies. Springer International Publishing; Cham, Switzerland: 2016. pp. 27–59. [Google Scholar]
- 16.Kirby M.L., Turnage K.L., 3rd, Hays B.M. Characterization of conotruncal malformations following ablation of “cardiac” neural crest. Anat. Rec. 1985;213:87–93. doi: 10.1002/ar.1092130112. [DOI] [PubMed] [Google Scholar]
- 17.Bockman D.E., Redmond M.E., Waldo K., Davis H., Kirby M.L. Effect of neural crest ablation on development of the heart and arch arteries in the chick. Am. J. Anat. 1987;180:332–341. doi: 10.1002/aja.1001800403. [DOI] [PubMed] [Google Scholar]
- 18.Porras D., Brown C.B. Temporal-spatial ablation of neural crest in the mouse results in cardiovascular defects. Dev. Dyn. 2008;237:153–162. doi: 10.1002/dvdy.21382. [DOI] [PubMed] [Google Scholar]
- 19.Ivanova A., Signore M., Caro N., Greene N.D., Copp A.J., Martinez-Barbera J.P. In vivo genetic ablation by Cre-mediated expression of diphtheria toxin fragment A. Genesis. 2005;43:129–135. doi: 10.1002/gene.20162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olaopa M., Zhou H.-m., Snider P., Wang J., Schwartz R.J., Moon A.M., Conway S.J. Pax3 is essential for normal cardiac neural crest morphogenesis but is not required during migration nor outflow tract septation. Dev. Biol. 2011;356:308–322. doi: 10.1016/j.ydbio.2011.05.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lang D., Powell S.K., Plummer R.S., Young K.P., Ruggeri B.A. PAX genes: Roles in development, pathophysiology, and cancer. Biochem. Pharmacol. 2007;73:1–14. doi: 10.1016/j.bcp.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 22.Chi N., Epstein J.A. Getting your Pax straight: Pax proteins in development and disease. Trends Genet. 2002;18:41–47. doi: 10.1016/S0168-9525(01)02594-X. [DOI] [PubMed] [Google Scholar]
- 23.Underhill D.A. PAX Proteins and Fables of Their Reconstruction. Crit. Rev. Eukar. Gene. 2012;22:161–177. doi: 10.1615/CritRevEukarGeneExpr.v22.i2.70. [DOI] [PubMed] [Google Scholar]
- 24.Goulding M.D., Chalepakis G., Deutsch U., Erselius J.R., Gruss P. Pax-3, a novel murine DNA binding protein expressed during early neurogenesis. EMBO J. 1991;10:1135–1147. doi: 10.1002/j.1460-2075.1991.tb08054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Henderson D.J., Ybot-Gonzalez P., Copp A.J. Over-expression of the chondroitin sulphate proteoglycan versican is associated with defective neural crest migration in the Pax3 mutant mouse (splotch) Mech. Dev. 1997;69:39–51. doi: 10.1016/S0925-4773(97)00151-2. [DOI] [PubMed] [Google Scholar]
- 26.Vogan K.J., Epstein D.J., Trasler D.G., Gros P. The splotch-delayed (Spd) mouse mutant carries a point mutation within the paired box of the Pax-3 gene. Genomics. 1993;17:364–369. doi: 10.1006/geno.1993.1333. [DOI] [PubMed] [Google Scholar]
- 27.Epstein J.A., Shapiro D.N., Cheng J., Lam P.Y., Maas R.L. Pax3 modulates expression of the c-Met receptor during limb muscle development. Proc. Natl. Acad. Sci. USA. 1996;93:4213–4218. doi: 10.1073/pnas.93.9.4213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dickie M.M. New Splotch Alleles in the Mouse. J. Hered. 1964;55:97–101. doi: 10.1093/oxfordjournals.jhered.a107317. [DOI] [PubMed] [Google Scholar]
- 29.Cattanach B.M., Rasberry C. Enhanced specific-locus mutation response of 101/H male mice to single, acute X-irradiation. Mutat. Res. 1994;311:77–84. doi: 10.1016/0027-5107(94)90075-2. [DOI] [PubMed] [Google Scholar]
- 30.Auerbach R. Analysis of the developmental effects of a lethal mutation in the house mouse. J. Exp. Zool. 1954;127:305–329. doi: 10.1002/jez.1401270206. [DOI] [Google Scholar]
- 31.Beechey C., Searle A. Mutations at the Sp locus. Mouse News Lett. 1986;75:28. [Google Scholar]
- 32.Russell W. Splotch, a new mutation in the house mouse, Mus-musculus. Genetics. 1947;32:102. [Google Scholar]
- 33.Ohno T., Maegawa T., Katoh H., Miyasaka Y., Suzuki M., Kobayashi M., Horio F. A new missense mutation in the paired domain of the mouse Pax3 gene. Exp. Anim. 2017;66:245–250. doi: 10.1538/expanim.17-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rasberry C., Cattanach B.M. A new mutation at the Ph locus. Mouse Genome. 1994;92:504–505. [Google Scholar]
- 35.Guo X.L., Ruan H.B., Li Y., Gao X., Li W. Identification of a novel nonsense mutation on the Pax3 gene in ENU-derived white belly spotting mice and its genetic interaction with c-Kit. Pigment Cell Melanoma Res. 2010;23:252–262. doi: 10.1111/j.1755-148X.2010.00677.x. [DOI] [PubMed] [Google Scholar]
- 36.Xiao Y., Zhang L., He K., Gao X., Yang L., He L., Ma G., Guo X. Characterization of a novel missense mutation on murine Pax3 through ENU mutagenesis. J. Genet. Genomics. 2011;38:333–339. doi: 10.1016/j.jgg.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 37.Bogani D., Warr N., Elms P., Davies J., Tymowska-Lalanne Z., Goldsworthy M., Cox R.D., Keays D.A., Flint J., Wilson V., et al. New semidominant mutations that affect mouse development. Genesis. 2004;40:109–117. doi: 10.1002/gene.20071. [DOI] [PubMed] [Google Scholar]
- 38.Moase C.E., Trasler D.G. Spinal ganglia reduction in the splotch-delayed mouse neural tube defect mutant. Teratology. 1989;40:67–75. doi: 10.1002/tera.1420400109. [DOI] [PubMed] [Google Scholar]
- 39.Grim M., Halata Z., Franz T. Schwann cells are not required for guidance of motor nerves in the hindlimb in Splotch mutant mouse embryos. Anat. Embryol. 1992;186:311–318. doi: 10.1007/BF00185979. [DOI] [PubMed] [Google Scholar]
- 40.Li J., Liu K.C., Jin F., Lu M.M., Epstein J.A. Transgenic rescue of congenital heart disease and spina bifida in Splotch mice. Development. 1999;126:2495–2503. doi: 10.1242/dev.126.11.2495. [DOI] [PubMed] [Google Scholar]
- 41.Epstein J.A. Pax3, neural crest and cardiovascular development. Trends Cardiovasc. Med. 1996;6:255–260. doi: 10.1016/S1050-1738(96)00110-7. [DOI] [PubMed] [Google Scholar]
- 42.Franz T. Persistent truncus arteriosus in the Splotch mutant mouse. Anat. Embryol. 1989;180:457–464. doi: 10.1007/BF00305120. [DOI] [PubMed] [Google Scholar]
- 43.Conway S.J., Henderson D.J., Copp A.J. Pax3 is required for cardiac neural crest migration in the mouse: Evidence from the splotch (Sp2H) mutant. Development. 1997;124:505–514. doi: 10.1242/dev.124.2.505. [DOI] [PubMed] [Google Scholar]
- 44.Bradshaw L., Chaudhry B., Hildreth V., Webb S., Henderson D.J. Dual role for neural crest cells during outflow tract septation in the neural crest-deficient mutant Splotch(2H) J. Anat. 2009;214:245–257. doi: 10.1111/j.1469-7580.2008.01028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goulding M., Sterrer S., Fleming J., Balling R., Nadeau J., Moore K.J., Brown S.D., Steel K.P., Gruss P. Analysis of the Pax-3 gene in the mouse mutant splotch. Genomics. 1993;17:355–363. doi: 10.1006/geno.1993.1332. [DOI] [PubMed] [Google Scholar]
- 46.Fleming J., Pearce A., Brown S.D., Steel K.P. The Sp4H deletion may contain a new locus essential for postimplantation development. Genomics. 1996;34:205–212. doi: 10.1006/geno.1996.0267. [DOI] [PubMed] [Google Scholar]
- 47.Epstein D.J., Malo D., Vekemans M., Gros P. Molecular characterization of a deletion encompassing the splotch mutation on mouse chromosome 1. Genomics. 1991;10:89–93. doi: 10.1016/0888-7543(91)90488-Z. [DOI] [PubMed] [Google Scholar]
- 48.Engleka K.A., Gitler A.D., Zhang M., Zhou D.D., High F.A., Epstein J.A. Insertion of Cre into the Pax3 locus creates a new allele of Splotch and identifies unexpected Pax3 derivatives. Dev. Biol. 2005;280:396–406. doi: 10.1016/j.ydbio.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 49.Zhou H.M., Wang J., Rogers R., Conway S.J. Lineage-specific responses to reduced embryonic Pax3 expression levels. Dev. Biol. 2008;315:369–382. doi: 10.1016/j.ydbio.2007.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhou H.M., Conway S.J. Pax3 Hypomorphs Reveal Hidden Pax7 Functional Genetic Compensation in Utero. J. Dev. Biol. 2022;10:19. doi: 10.3390/jdb10020019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Degenhardt K.R., Milewski R.C., Padmanabhan A., Miller M., Singh M.K., Lang D., Engleka K.A., Wu M., Li J., Zhou D., et al. Distinct enhancers at the Pax3 locus can function redundantly to regulate neural tube and neural crest expressions. Dev. Biol. 2010;339:519–527. doi: 10.1016/j.ydbio.2009.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lagutina I., Conway S.J., Sublett J., Grosveld G.C. Pax3-FKHR knock-in mice show developmental aberrations but do not develop tumors. Mol. Cell Biol. 2002;22:7204–7216. doi: 10.1128/MCB.22.20.7204-7216.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Singer J.D., Gurian-West M., Clurman B., Roberts J.M. Cullin-3 targets cyclin E for ubiquitination and controls S phase in mammalian cells. Genes Dev. 1999;13:2375–2387. doi: 10.1101/gad.13.18.2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Franz T. The Splotch (Sp1H) and Splotch-delayed (Spd) alleles: Differential phenotypic effects on neural crest and limb musculature. Anat. Embryol. 1993;187:371–377. doi: 10.1007/BF00185895. [DOI] [PubMed] [Google Scholar]
- 55.Koushik S.V., Chen H., Wang J., Conway S.J. Generation of a conditional loxP allele of the Pax3 transcription factor that enables selective deletion of the homeodomain. Genesis. 2002;32:114–117. doi: 10.1002/gene.10051. [DOI] [PubMed] [Google Scholar]
- 56.Mansouri A., Stoykova A., Torres M., Gruss P. Dysgenesis of cephalic neural crest derivatives in Pax7−/− mutant mice. Development. 1996;122:831–838. doi: 10.1242/dev.122.3.831. [DOI] [PubMed] [Google Scholar]
- 57.Mansouri A., Gruss P. Pax3 and Pax7 are expressed in commissural neurons and restrict ventral neuronal identity in the spinal cord. Mech. Dev. 1998;78:171–178. doi: 10.1016/S0925-4773(98)00168-3. [DOI] [PubMed] [Google Scholar]
- 58.Hanna L.A., Foreman R.K., Tarasenko I.A., Kessler D.S., Labosky P.A. Requirement for Foxd3 in maintaining pluripotent cells of the early mouse embryo. Genes Dev. 2002;16:2650–2661. doi: 10.1101/gad.1020502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Teng L., Mundell N.A., Frist A.Y., Wang Q., Labosky P.A. Requirement for Foxd3 in the maintenance of neural crest progenitors. Development. 2008;135:1615–1624. doi: 10.1242/dev.012179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nelms B.L., Pfaltzgraff E.R., Labosky P.A. Functional interaction between Foxd3 and Pax3 in cardiac neural crest development. Genesis. 2011;49:10–23. doi: 10.1002/dvg.20686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kubic J.D., Little E.C., Kaiser R.S., Young K.P., Lang D. FOXD3 Promotes PAX3 Expression in Melanoma Cells. J. Cell Biochem. 2016;117:533–541. doi: 10.1002/jcb.25306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dottori M., Gross M.K., Labosky P., Goulding M. The winged-helix transcription factor Foxd3 suppresses interneuron differentiation and promotes neural crest cell fate. Development. 2001;128:4127–4138. doi: 10.1242/dev.128.21.4127. [DOI] [PubMed] [Google Scholar]
- 63.Davidson D. The function and evolution of Msx genes: Pointers and paradoxes. Trends Genet. 1995;11:405–411. doi: 10.1016/S0168-9525(00)89124-6. [DOI] [PubMed] [Google Scholar]
- 64.Satokata I., Ma L., Ohshima H., Bei M., Woo I., Nishizawa K., Maeda T., Takano Y., Uchiyama M., Heaney S., et al. Msx2 deficiency in mice causes pleiotropic defects in bone growth and ectodermal organ formation. Nat. Genet. 2000;24:391–395. doi: 10.1038/74231. [DOI] [PubMed] [Google Scholar]
- 65.Ishii M., Han J., Yen H.Y., Sucov H.M., Chai Y., Maxson R.E., Jr. Combined deficiencies of Msx1 and Msx2 cause impaired patterning and survival of the cranial neural crest. Development. 2005;132:4937–4950. doi: 10.1242/dev.02072. [DOI] [PubMed] [Google Scholar]
- 66.Chen Y.H., Ishii M., Sun J., Sucov H.M., Maxson R.E., Jr. Msx1 and Msx2 regulate survival of secondary heart field precursors and post-migratory proliferation of cardiac neural crest in the outflow tract. Dev. Biol. 2007;308:421–437. doi: 10.1016/j.ydbio.2007.05.037. [DOI] [PubMed] [Google Scholar]
- 67.Chen Y.H., Ishii M., Sucov H.M., Maxson R.E., Jr. Msx1 and Msx2 are required for endothelial-mesenchymal transformation of the atrioventricular cushions and patterning of the atrioventricular myocardium. BMC Dev. Biol. 2008;8:75. doi: 10.1186/1471-213X-8-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kwang S.J., Brugger S.M., Lazik A., Merrill A.E., Wu L.-Y., Liu Y.-H., Ishii M., Sangiorgi F.O., Rauchman M., Sucov H.M., et al. Msx2 is an immediate downstream effector of Pax3 in the development of the murine cardiac neural crest. Development. 2002;129:527–538. doi: 10.1242/dev.129.2.527. [DOI] [PubMed] [Google Scholar]
- 69.Lang D., Epstein J.A. Sox10 and Pax3 physically interact to mediate activation of a conserved c-RET enhancer. Hum. Mol. Genet. 2003;12:937–945. doi: 10.1093/hmg/ddg107. [DOI] [PubMed] [Google Scholar]
- 70.Bondurand N., Pingault V., Goerich D.E., Lemort N., Sock E., Le Caignec C., Wegner M., Goossens M. Interaction among SOX10, PAX3 and MITF, three genes altered in Waardenburg syndrome. Hum. Mol. Genet. 2000;9:1907–1917. doi: 10.1093/hmg/9.13.1907. [DOI] [PubMed] [Google Scholar]
- 71.Wang D., Ren G.F., Zhang H.Z., Yi C.Y., Peng Z.J. A de novo 2q35-q36.1 deletion incorporating IHH in a Chinese boy (47,XYY) with syndactyly, type III Waardenburg syndrome, and congenital heart disease. Genet. Mol. Res. 2016;15:gmr15049060. doi: 10.4238/gmr15049060. [DOI] [PubMed] [Google Scholar]
- 72.Banerjee A.K. Waardenburg’s syndrome associated with ostium secundum atrial septal defect. J. R. Soc. Med. 1986;79:677–678. doi: 10.1177/014107688607901121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Farin H.F., Mansouri A., Petry M., Kispert A. T-box protein Tbx18 interacts with the paired box protein Pax3 in the development of the paraxial mesoderm. J. Biol. Chem. 2008;283:25372–25380. doi: 10.1074/jbc.M802723200. [DOI] [PubMed] [Google Scholar]
- 74.Wu S.P., Dong X.R., Regan J.N., Su C., Majesky M.W. Tbx18 regulates development of the epicardium and coronary vessels. Dev. Biol. 2013;383:307–320. doi: 10.1016/j.ydbio.2013.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wiese C., Grieskamp T., Airik R., Mommersteeg M.T., Gardiwal A., de Gier-de Vries C., Schuster-Gossler K., Moorman A.F., Kispert A., Christoffels V.M. Formation of the sinus node head and differentiation of sinus node myocardium are independently regulated by Tbx18 and Tbx3. Circ. Res. 2009;104:388–397. doi: 10.1161/CIRCRESAHA.108.187062. [DOI] [PubMed] [Google Scholar]
- 76.Greulich F., Farin H.F., Schuster-Gossler K., Kispert A. Tbx18 function in epicardial development. Cardiovasc. Res. 2012;96:476–483. doi: 10.1093/cvr/cvs277. [DOI] [PubMed] [Google Scholar]
- 77.Norden J., Grieskamp T., Christoffels V.M., Moorman A.F., Kispert A. Partial absence of pleuropericardial membranes in Tbx18- and Wt1-deficient mice. PLoS ONE. 2012;7:e45100. doi: 10.1371/journal.pone.0045100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Milet C., Maczkowiak F., Roche D.D., Monsoro-Burq A.H. Pax3 and Zic1 drive induction and differentiation of multipotent, migratory, and functional neural crest in Xenopus embryos. Proc. Natl. Acad. Sci. USA. 2013;110:5528–5533. doi: 10.1073/pnas.1219124110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Epstein J.A., Li J., Lang D., Chen F., Brown C.B., Jin F., Lu M.M., Thomas M., Liu E., Wessels A., et al. Migration of cardiac neural crest cells in Splotch embryos. Development. 2000;127:1869–1878. doi: 10.1242/dev.127.9.1869. [DOI] [PubMed] [Google Scholar]
- 80.Pani L., Horal M., Loeken M.R. Rescue of neural tube defects in Pax-3-deficient embryos by p53 loss of function: Implications for Pax-3- dependent development and tumorigenesis. Genes Dev. 2002;16:676–680. doi: 10.1101/gad.969302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Morgan S.C., Lee H.Y., Relaix F., Sandell L.L., Levorse J.M., Loeken M.R. Cardiac outflow tract septation failure in Pax3-deficient embryos is due to p53-dependent regulation of migrating cardiac neural crest. Mech. Dev. 2008;125:757–767. doi: 10.1016/j.mod.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang X.D., Morgan S.C., Loeken M.R. Pax3 stimulates p53 ubiquitination and degradation independent of transcription. PLoS ONE. 2011;6:e29379. doi: 10.1371/journal.pone.0029379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pruitt S.C., Bussman A., Maslov A.Y., Natoli T.A., Heinaman R. Hox/Pbx and Brn binding sites mediate Pax3 expression in vitro and in vivo. Gene Expr. Patterns. 2004;4:671–685. doi: 10.1016/j.modgep.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 84.Milewski R.C., Chi N.C., Li J., Brown C., Lu M.M., Epstein J.A. Identification of minimal enhancer elements sufficient for Pax3 expression in neural crest and implication of Tead2 as a regulator of Pax3. Development. 2004;131:829–837. doi: 10.1242/dev.00975. [DOI] [PubMed] [Google Scholar]
- 85.Peters H., Neubuser A., Kratochwil K., Balling R. Pax9-deficient mice lack pharyngeal pouch derivatives and teeth and exhibit craniofacial and limb abnormalities. Genes Dev. 1998;12:2735–2747. doi: 10.1101/gad.12.17.2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Peters H., Wilm B., Sakai N., Imai K., Maas R., Balling R. Pax1 and Pax9 synergistically regulate vertebral column development. Development. 1999;126:5399–5408. doi: 10.1242/dev.126.23.5399. [DOI] [PubMed] [Google Scholar]
- 87.Stothard C.A., Mazzotta S., Vyas A., Schneider J.E., Mohun T.J., Henderson D.J., Phillips H.M., Bamforth S.D. Pax9 and Gbx2 Interact in the Pharyngeal Endoderm to Control Cardiovascular Development. J. Cardiovasc. Dev. Dis. 2020;7:20. doi: 10.3390/jcdd7020020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Phillips H.M., Stothard C.A., Shaikh Qureshi W.M., Kousa A.I., Briones-Leon J.A., Khasawneh R.R., O’Loughlin C., Sanders R., Mazzotta S., Dodds R., et al. Pax9 is required for cardiovascular development and interacts with Tbx1 in the pharyngeal endoderm to control 4th pharyngeal arch artery morphogenesis. Development. 2019;146:dev177618. doi: 10.1242/dev.177618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Khasawneh R.R., Kist R., Queen R., Hussain R., Coxhead J., Schneider J.E., Mohun T.J., Zaffran S., Peters H., Phillips H.M., et al. Msx1 haploinsufficiency modifies the Pax9-deficient cardiovascular phenotype. BMC Dev. Biol. 2021;21:14. doi: 10.1186/s12861-021-00245-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Neubuser A., Koseki H., Balling R. Characterization and developmental expression of Pax9, a paired-box-containing gene related to Pax1. Dev. Biol. 1995;170:701–716. doi: 10.1006/dbio.1995.1248. [DOI] [PubMed] [Google Scholar]
- 91.Farley A.M., Morris L.X., Vroegindeweij E., Depreter M.L., Vaidya H., Stenhouse F.H., Tomlinson S.R., Anderson R.A., Cupedo T., Cornelissen J.J., et al. Dynamics of thymus organogenesis and colonization in early human development. Development. 2013;140:2015–2026. doi: 10.1242/dev.087320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kist R., Greally E., Peters H. Derivation of a mouse model for conditional inactivation of Pax9. Genesis. 2007;45:460–464. doi: 10.1002/dvg.20295. [DOI] [PubMed] [Google Scholar]
- 93.Yashiro K., Shiratori H., Hamada H. Haemodynamics determined by a genetic programme govern asymmetric development of the aortic arch. Nature. 2007;450:285–288. doi: 10.1038/nature06254. [DOI] [PubMed] [Google Scholar]
- 94.Hogers B., DeRuiter M.C., Gittenberger-de Groot A.C., Poelmann R.E. Extraembryonic venous obstructions lead to cardiovascular malformations and can be embryolethal. Cardiovasc. Res. 1999;41:87–99. doi: 10.1016/S0008-6363(98)00218-1. [DOI] [PubMed] [Google Scholar]
- 95.Hayashi S., Yagi M., Morisaki I., Inazawa J. Identical deletion at 14q13.3 including PAX9 and NKX2-1 in siblings from mosaicism of unaffected parent. J. Hum. Genet. 2015;60:203–206. doi: 10.1038/jhg.2014.123. [DOI] [PubMed] [Google Scholar]
- 96.Shapira S.K., Anderson K.L., Orr-Urtregar A., Craigen W.J., Lupski J.R., Shaffer L.G. De novo proximal interstitial deletions of 14q: Cytogenetic and molecular investigations. Am. J. Med. Genet. 1994;52:44–50. doi: 10.1002/ajmg.1320520109. [DOI] [PubMed] [Google Scholar]
- 97.Schuffenhauer S., Leifheit H.J., Lichtner P., Peters H., Murken J., Emmerich P. De novo deletion (14)(q11.2q13) including PAX9: Clinical and molecular findings. J. Med. Genet. 1999;36:233–236. doi: 10.1136/jmg.36.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Santen G.W., Sun Y., Gijsbers A.C., Carre A., Holvoet M., Haeringen A., Lesnik Oberstein S.A., Tomoda A., Mabe H., Polak M., et al. Further delineation of the phenotype of chromosome 14q13 deletions: (positional) involvement of FOXG1 appears the main determinant of phenotype severity, with no evidence for a holoprosencephaly locus. J. Med. Genet. 2012;49:366–372. doi: 10.1136/jmedgenet-2011-100721. [DOI] [PubMed] [Google Scholar]
- 99.Pabst O., Rummelies J., Winter B., Arnold H.H. Targeted disruption of the homeobox gene Nkx2.9 reveals a role in development of the spinal accessory nerve. Development. 2003;130:1193–1202. doi: 10.1242/dev.00346. [DOI] [PubMed] [Google Scholar]
- 100.Kimura S., Hara Y., Pineau T., Fernandez-Salguero P., Fox C.H., Ward J.M., Gonzalez F.J. The T/ebp null mouse: Thyroid-specific enhancer-binding protein is essential for the organogenesis of the thyroid, lung, ventral forebrain, and pituitary. Genes Dev. 1996;10:60–69. doi: 10.1101/gad.10.1.60. [DOI] [PubMed] [Google Scholar]
- 101.Liao J., Aggarwal V.S., Nowotschin S., Bondarev A., Lipner S., Morrow B.E. Identification of downstream genetic pathways of Tbx1 in the second heart field. Dev. Biol. 2008;316:524–537. doi: 10.1016/j.ydbio.2008.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ivins S., Lammerts van Beuren K., Roberts C., James C., Lindsay E., Baldini A., Ataliotis P., Scambler P.J. Microarray analysis detects differentially expressed genes in the pharyngeal region of mice lacking Tbx1. Dev. Biol. 2005;285:554–569. doi: 10.1016/j.ydbio.2005.06.026. [DOI] [PubMed] [Google Scholar]
- 103.Morrow B.E., McDonald-McGinn D.M., Emanuel B.S., Vermeesch J.R., Scambler P.J. Molecular genetics of 22q11.2 deletion syndrome. Am. J. Med. Genet. Part A. 2018;176:2070–2081. doi: 10.1002/ajmg.a.40504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Papangeli I., Scambler P. The 22q11 deletion: DiGeorge and velocardiofacial syndromes and the role of TBX1. Wiley Interdiscip. Rev. Dev. Biol. 2013;2:393–403. doi: 10.1002/wdev.75. [DOI] [PubMed] [Google Scholar]
- 105.Jerome L.A., Papaioannou V.E. DiGeorge syndrome phenotype in mice mutant for the T-box gene, Tbx1. Nat. Genet. 2001;27:286–291. doi: 10.1038/85845. [DOI] [PubMed] [Google Scholar]
- 106.Vitelli F., Morishima M., Taddei I., Lindsay E.A., Baldini A. Tbx1 mutation causes multiple cardiovascular defects and disrupts neural crest and cranial nerve migratory pathways. Hum. Mol. Genet. 2002;11:915–922. doi: 10.1093/hmg/11.8.915. [DOI] [PubMed] [Google Scholar]
- 107.Lindsay E.A., Baldini A. Recovery from arterial growth delay reduces penetrance of cardiovascular defects in mice deleted for the DiGeorge syndrome region. Hum. Mol. Genet. 2001;10:997–1002. doi: 10.1093/hmg/10.9.997. [DOI] [PubMed] [Google Scholar]
- 108.Calmont A., Ivins S., Van Bueren K.L., Papangeli I., Kyriakopoulou V., Andrews W.D., Martin J.F., Moon A.M., Illingworth E.A., Basson M.A., et al. Tbx1 controls cardiac neural crest cell migration during arch artery development by regulating Gbx2 expression in the pharyngeal ectoderm. Development. 2009;136:3173–3183. doi: 10.1242/dev.028902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Byrd N.A., Meyers E.N. Loss of Gbx2 results in neural crest cell patterning and pharyngeal arch artery defects in the mouse embryo. Dev. Biol. 2005;284:233–245. doi: 10.1016/j.ydbio.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 110.Satokata I., Maas R. Msx1 deficient mice exhibit cleft palate and abnormalities of craniofacial and tooth development. Nat. Genet. 1994;6:348–356. doi: 10.1038/ng0494-348. [DOI] [PubMed] [Google Scholar]
- 111.Papoutsi T., Odelin G., Moore-Morris T., Puceat M., de la Pompa J.L., Robert B., Zaffran S. Msx1(cre) (ERT) (2) knock-In allele: A useful tool to target embryonic and adult cardiac valves. Genesis. 2015;53:337–345. doi: 10.1002/dvg.22856. [DOI] [PubMed] [Google Scholar]
- 112.Ogawa T., Kapadia H., Wang B., D’Souza R.N. Studies on Pax9-Msx1 protein interactions. Arch. Oral Biol. 2005;50:141–145. doi: 10.1016/j.archoralbio.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 113.Nakatomi M., Ludwig K.U., Knapp M., Kist R., Lisgo S., Ohshima H., Mangold E., Peters H. Msx1 deficiency interacts with hypoxia and induces a morphogenetic regulation during mouse lip development. Development. 2020;147:dev189175. doi: 10.1242/dev.189175. [DOI] [PubMed] [Google Scholar]
- 114.Nakatomi M., Wang X.P., Key D., Lund J.J., Turbe-Doan A., Kist R., Aw A., Chen Y., Maas R.L., Peters H. Genetic interactions between Pax9 and Msx1 regulate lip development and several stages of tooth morphogenesis. Dev. Biol. 2010;340:438–449. doi: 10.1016/j.ydbio.2010.01.031. [DOI] [PubMed] [Google Scholar]
- 115.Goupille O., Saint Cloment C., Lopes M., Montarras D., Robert B. Msx1 and Msx2 are expressed in sub-populations of vascular smooth muscle cells. Dev. Dyn. 2008;237:2187–2194. doi: 10.1002/dvdy.21619. [DOI] [PubMed] [Google Scholar]
- 116.Zhang Z., Baldini A. In vivo response to high-resolution variation of Tbx1 mRNA dosage. Hum. Mol. Genet. 2008;17:150–157. doi: 10.1093/hmg/ddm291. [DOI] [PubMed] [Google Scholar]
- 117.Kist R., Watson M., Wang X., Cairns P., Miles C., Reid D.J., Peters H. Reduction of Pax9 gene dosage in an allelic series of mouse mutants causes hypodontia and oligodontia. Hum. Mol. Genet. 2005;14:3605–3617. doi: 10.1093/hmg/ddi388. [DOI] [PubMed] [Google Scholar]
- 118.Wallin J., Eibel H., Neubuser A., Wilting J., Koseki H., Balling R. Pax1 is expressed during development of the thymus epithelium and is required for normal T-cell maturation. Development. 1996;122:23–30. doi: 10.1242/dev.122.1.23. [DOI] [PubMed] [Google Scholar]
- 119.Muller T.S., Ebensperger C., Neubuser A., Koseki H., Balling R., Christ B., Wilting J. Expression of avian Pax1 and Pax9 is intrinsically regulated in the pharyngeal endoderm, but depends on environmental influences in the paraxial mesoderm. Dev. Biol. 1996;178:403–417. doi: 10.1006/dbio.1996.0227. [DOI] [PubMed] [Google Scholar]
- 120.Ogasawara M., Shigetani Y., Hirano S., Satoh N., Kuratani S. Pax1/Pax9-Related genes in an agnathan vertebrate, Lampetra japonica: Expression pattern of LjPax9 implies sequential evolutionary events toward the gnathostome body plan. Dev. Biol. 2000;223:399–410. doi: 10.1006/dbio.2000.9756. [DOI] [PubMed] [Google Scholar]
- 121.Sanchez R.S., Sanchez S.S. Characterization of pax1, pax9, and uncx sclerotomal genes during Xenopus laevis embryogenesis. Dev. Dyn. 2013;242:572–579. doi: 10.1002/dvdy.23945. [DOI] [PubMed] [Google Scholar]
- 122.Wilm B., Dahl E., Peters H., Balling R., Imai K. Targeted disruption of Pax1 defines its null phenotype and proves haploinsufficiency. Proc. Natl. Acad. Sci. USA. 1998;95:8692–8697. doi: 10.1073/pnas.95.15.8692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bannykh S.I., Emery S.C., Gerber J.K., Jones K.L., Benirschke K., Masliah E. Aberrant Pax1 and Pax9 expression in Jarcho-Levin syndrome: Report of two Caucasian siblings and literature review. Am. J. Med. Genet. Part A. 2003;120A:241–246. doi: 10.1002/ajmg.a.20192. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.