Abstract
Background:
Patients undergoing bilateral autologous breast reconstruction may benefit from increased flap volume using bilateral stacked deep inferior epigastric perforator (DIEP) and profunda artery perforator (PAP) flaps. Our aim was to characterize the donor site morbidity and patient-reported outcomes in four-flap breast reconstruction.
Methods:
Retrospective review was performed for all patients undergoing four-flap breast reconstruction by two surgeons between January 2010 and September 2021. Outcome measures including the BREAST-Q reconstructive module, the lower extremity functional scale (LEFS), inpatient surgical site pain scores by numeric pain rating scale (NPRS), and a postoperative subjective survey comparing donor sites were obtained. Four-flap BREAST-Q scores were compared with bilateral DIEP and bilateral PAP patients.
Results:
A total of 79 patients undergoing four-flap breast reconstruction were identified. Four-flap BREAST-Q scores (n = 56) were similar to bilateral DIEP and bilateral PAP reconstruction patients. Long-term survey outcomes from the LEFS demonstrated improved score trend after 6 months. Mean instances of donor site pain location recorded at the abdomen were significantly higher than the thigh during the postoperative admission. Subjective survey data revealed more long-term donor site pain at the PAP site, a patient preference for the DIEP donor site, and easier postoperative care for the DIEP donor site.
Conclusions:
This is the largest consecutive series of four-flap breast reconstruction outcomes reported to date. BREAST-Q scores in four-flap patients demonstrate overall patient satisfaction that is similar to both bilateral DIEP and bilateral PAP reconstruction patients. The DIEP donor site appears to be preferred by patients over the PAP donor site.
Takeaways
Question: What are the donor site morbidity and patient-reported outcomes in four-flap breast reconstruction?
Findings: BREAST-Q scores in four-flap patients demonstrate overall patient satisfaction similar to both bilateral DIEP and bilateral PAP reconstruction patients.
Meaning: Patients who require more volume for breast reconstruction have a safe choice in four-flap reconstruction that demonstrated similar satisfaction as DIEP and PAP reconstruction patients.
INTRODUCTION
Patients undergoing bilateral autologous breast reconstruction may benefit from multiple perforator flaps in a four-flap configuration for appropriate volume, ptosis, and avoidance of prosthesis.1–3 The senior authors have previously reported their experience with four-flap breast reconstruction using bilateral stacked deep inferior epigastric perforator (DIEP) and profunda artery perforator (PAP) flaps.1,4 Early experience suggests an acceptable microsurgical risk and donor site morbidity profile.
Patient-reported outcome measures are critical in understanding patient perception and quality of life with autologous breast reconstruction.5–7 This is especially relevant when determining the appropriate choice of secondary or stacked flaps in selected patients.8 With regard to donor site morbidity, the most common donor site complications among four-flap patients include delayed wound healing and dehiscence, hematoma, and seroma.1,9 However, there is a paucity of data describing the quality of life and postoperative experience among four-flap patients. Four-flap breast reconstruction patients are also a unique population in which to directly compare abdominal and posterior thigh donor site outcomes within the same patient population. Our aim was to review patient-reported outcome measures in four-flap breast reconstruction patients and to compare abdominal and posterior thigh donor site subjective outcomes within this cohort.
METHODS
Between January 2010 and September 2021, a retrospective chart review was performed of all patients undergoing four-flap breast reconstruction by the two senior cosurgeons (N.T.H. and S.S.T.) at a single academic medical center. Following institutional review board approval, all data were collected within REDCap.10 Patient demographics, including age, body mass index, history of cancer, radiation therapy, chemotherapy, medical comorbidities, and social history, were recorded. All four-flap patients were invited to complete the BREAST-Q module and lower extremity functional scale (LEFS) at 3-, 6-, 12-, 18-, 24-, and greater than 24-month time points.11 Rasche scores were calculated for each of the postoperative BREAST-Q questions. Patients with missing responses to specific questions were removed from the analysis of that question, and kept for the analysis of completed questions. An additional nonvalidated postoperative survey was administered to assess subjective thigh aesthetic improvement, and to directly compare donor site pain, preference, and ease of postoperative care. For the purposes of data analysis, the most recent scores were used for comparisons.
For surgical site pain analysis between four-flap patients, patient numeric pain rating scale (NPRS) and pain location were recorded by nursing staff into the electronic medical record during the postoperative inpatient admission. Pain scores were recorded every 2 hours in the surgical intensive care unit, and every 4 hours after floor transfer. If no pain was present, a score of 0 was documented. Mean pain scores were calculated per donor anatomic location (abdomen, thighs, and breasts), along with the number of recorded pain instances per anatomic site. As an example, if the recorded pain score was documented as 7 to the abdomen out of the 0–10 scale, one count of abdominal pain was recorded. Similarly, if both abdominal pain and thigh pain were documented for the pain score, each donor site received one count of recorded pain instance.
We then performed a comparative analysis of BREAST-Q scores of four-flap patients to bilateral DIEP and bilateral PAP patients as reference populations. All patients undergoing bilateral DIEP or bilateral PAP reconstruction within the study timeframe were reviewed. Patients were excluded from analysis if there was no response to BREAST-Q survey invitation. Estimated marginal means were obtained and adjusted for age, BMI, follow-up survey time, radiation, and neoadjuvant and adjuvant chemotherapy. Bilateral PAP patient LEFS scores were also obtained as a comparison to the four-flap group. Finally, normative BREAST-Q scores were obtained for all preoperative patients with available preoperative BREAST-Q surveys undergoing any reconstruction type (implant-based, autologous, unilateral, or bilateral) after invitation following the initial consult. These normative patients were then compared with the postoperative BREAST-Q scores of the three surgical groups (four-flap, DIEP, and PAP). Statistical significance was set at a P value less than 0.05 for all tests. All statistics were performed using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
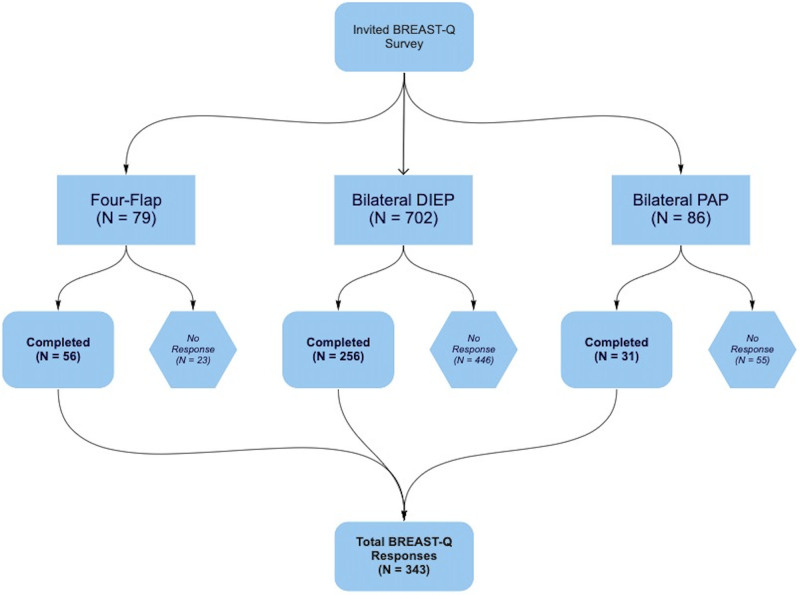
A total of 79 patients undergoing four-flap breast reconstruction were identified, with a median clinic follow-up time of 23 months. Completed BREAST-Q module was available for 56 patients, and completed LEFS was available for 60 patients. Inpatient postoperative NPRS pain score data were available for 60 patients. For bilateral DIEP flap patient comparison, 702 patients were identified, of which 256 patients had completed BREAST-Q data. For bilateral PAP patients, 86 patients were identified with 31 with completed BREAST-Q data, and 46 with completed LEFS data. A flowchart for patient inclusion is shown in Figure 1. Mean BREAST-Q postoperative survey time was 18.6 ± 10.4 months for four-flap patients, 16.9 ± 10.7 months for bilateral DIEP patients, and 16.4 ± 9.9 months for bilateral PAP patients, and was not statistically significant between groups (P = 0.518). Patient demographic data for patients with completed BREAST-Q data are shown in Table 1.
Fig. 1.
BREAST-Q patient flowchart.
Table 1.
Summary of Patient Demographics and History
| Characteristics | Group | ||
|---|---|---|---|
| Four-flap | PAP | DIEP | |
| (N = 56) | (N = 31) | (N = 256) | |
| Age at flap procedure | |||
| Mean ± SD | 50.4 ± 9.3 | 47.4 ± 10 | 51.48 ± 9.2 |
| Median (IQR) | 49 (45.8–59.0) | 46 (41–56) | 52 (45–58.3) |
| BMI for flap procedure* | |||
| Mean ± SD | 25.8 ± 3.7 | 24.7 ± 4.1 | 40 ± 5.6 |
| Median (IQR) | 25.4 (23.0–28.9) | 24.1 (22.7–25.6) | 30.4 (26.63. 34.2) |
| Race | |||
| White | 43 | 22 | 172 |
| Asian | 1 | 0 | 5 |
| Black | 2 | 2 | 33 |
| Hispanic | 5 | 7 | 37 |
| Other | 5 | 0 | 9 |
| HTN* | |||
| No | 49 | 29 | 196 |
| Yes | 7 | 2 | 60 |
| Diabetes | |||
| No | 55 | 30 | 244 |
| Yes | 1 | 1 | 12 |
| Autoimmune | |||
| No | 50 | 30 | 241 |
| Yes | 6 | 1 | 15 |
| History of abdominal surgery | |||
| No | 18 | 9 | 75 |
| Yes | 38 | 22 | 181 |
| History of cosmetic breast surgery* | |||
| No | 48 | 28 | 243 |
| Yes | 8 | 3 | 13 |
| History of DVT or PE | |||
| No | 55 | 28 | 242 |
| Yes | 1 | 3 | 14 |
| History of miscarriage | |||
| No | 55 | 31 | 252 |
| Yes | 1 | 0 | 4 |
| Family history or hematologic diagnosis of hypercoagulability | |||
| No | 53 | 29 | 244 |
| Yes | 3 | 2 | 12 |
| Prophylactic mastectomy due to genetic mutation | |||
| No | 47 | 30 | 215 |
| Yes | 9 | 1 | 41 |
| Radiation* | |||
| No | 25 | 13 | 170 |
| Yes | 31 | 18 | 86 |
| Neoadjuvant chemotherapy | |||
| No | 39 | 24 | 184 |
| Yes | 17 | 7 | 72 |
| Adjuvant chemotherapy | |||
| No | 46 | 23 | 181 |
| Yes | 10 | 8 | 75 |
| Procedure time cut to closure (min)* | |||
| Mean ± SD | 530.6 ± 111.5 | 358.6 ± 188.8 | 387.2 ± 162.1 |
| Median (IQR) | 524 (464.0–611.5) | 312 (256.5. 433.5) | 364.5 (272.5–450) |
| Length of stay (d)* | |||
| Mean ± SD | 3.9 ± 1.2 | 3 ± 1 | 3.4 ± 2 |
| Median (IQR) | 4 (3–5) | 3 (2–3) | 3 (2–4) |
For categorical variables, P values were obtained using the Chi-square test or Fisher exact test. For continuous variables, P values were obtained using one-way ANOVA or nonparametric Kruskal–Wallis rank sum test.
*Denotes statistical significance.
ANOVA, analysis of variance; DVT, deep venous thrombosis; HTN, hypertension; PE, pulmonary embolism.
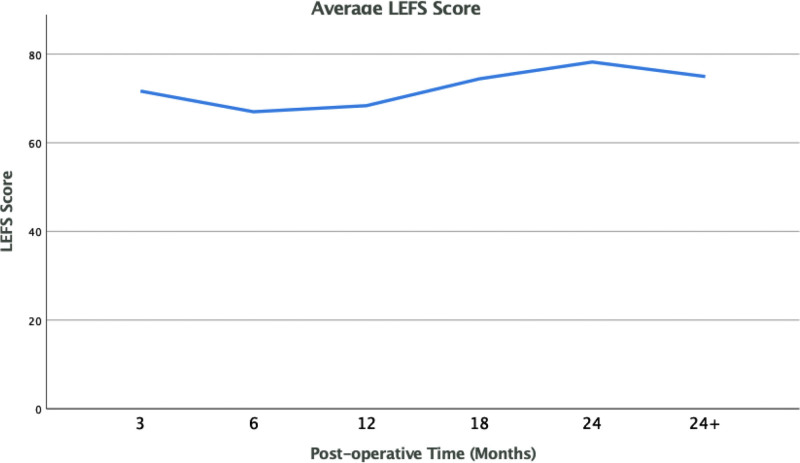
Four-flap BREAST-Q results demonstrated estimated marginal mean Rasch score of satisfaction with breasts of 79.0 ± 18.2, psychosocial well-being 86.4 ± 18.4, physical well-being chest 84.3 ± 16.6, physical well-being abdomen 77.0 ± 21.5, and sexual well-being 64.9 ± 25.7. For postoperative patient experience measures, four-flap patients demonstrated satisfaction with information 85.2 ± 18.2, satisfaction with surgeon 94.2 ± 12.8, satisfaction with medical team 97.9 ± 7.1, and satisfaction with office staff 99.2 ± 3.64. When compared with bilateral DIEP patients and bilateral PAP patients, there was no difference in EMM scores for each of the outcome measures. The remainder of the results are shown in Table 2. Survey outcomes from the LEFS (n = 60) among four-flap patients demonstrated a most recent mean score of 92.4% (SD, 10.9), with score trend over time shown in Figure 2. For bilateral PAP patients, the most recent mean score was 90.4% (SD, 12.45), which was not statistically significant (P = 0.7895).
Table 2.
Summary of BREAST-Q Scores with DIEP Flap as the Reference
| BREAST-Q (N = 352) | Mean ± SD | EMM | P |
|---|---|---|---|
| Postoperative satisfaction with breasts | |||
| DIEP | 73.4 ± 23.2 | 74.2 | Ref |
| Four-flap | 79.0 ± 18.2 | 78.2 | 0.737 |
| PAP | 69.3 ± 19.3 | 66.1 | 0.205 |
| Postoperative psychosocial well-being | |||
| DIEP | 75.9 ± 25.2 | 76.4 | Ref |
| Four-flap | 86.4 ± 18.4 | 85.0 | 0.072 |
| PAP | 71.0 ± 21.4 | 68.9 | 0.348 |
| Postoperative physical well-being: chest | |||
| DIEP | 82.6 ± 18.1 | 83.3 | Ref |
| Four-flap | 84.3 ± 16.6 | 82.3 | 1 |
| PAP | 83.1 ± 16.2 | 81.0 | 1 |
| Postoperative physical well-being: abdomen | |||
| DIEP | 71.2 ± 19.3 | 71.9 | Ref |
| Four-flap | 77.0 ± 21.5 | 73.8 | 1 |
| PAP | 68.3 ± 30.6 | 66.7 | 1 |
| Postoperative sexual well-being | |||
| DIEP | 54.6 ± 29.8 | 56.0 | Ref |
| Four-flap | 64.9 ± 25.7 | 62.1 | 0.704 |
| PAP | 54.0 ± 29.8 | 48.9 | 0.753 |
| Postoperative patient experience: satisfaction with information | |||
| DIEP | 78.4 ± 19.2 | 79.8 | Ref |
| Four-flap | 85.2 ± 18.2 | 82.2 | 1 |
| PAP | 85.0 ± 17.5 | 79.2 | 1 |
| Postoperative patient experience: satisfaction with surgeon | |||
| DIEP | 91.6 ± 19.3 | 92.0 | Ref |
| Four-flap | 94.2 ± 12.8 | 93.5 | 1 |
| PAP | 95.8 ± 18.4 | 93.0 | 1 |
| Postoperative patient experience: satisfaction with medical team | |||
| DIEP | 95.7 ± 13.6 | 95.9 | Ref |
| Four-flap | 97.9 ± 7.1 | 97.5 | 1 |
| PAP | 96.6 ± 10.7 | 95.5 | 1 |
| Postoperative patient experience: satisfaction with office staff | |||
| DIEP | 97.0 ± 11.5 | 97.2 | Ref |
| Four-flap | 99.2 ± 3.64 | 98.7 | 1 |
| PAP | 99.1 ± 3.9 | 97.8 | 1 |
The EMMs were adjusted for age, BMI, follow-up survey time (continuous variable; values include 3, 6, 12, 24, and 30), radiation, neoadjuvant chemotherapy, and adjuvant chemotherapy.
EMM values were compared post hoc using Bonferroni test.
EMM, estimated marginal mean.
Fig. 2.
Lower extremity functional scale trend in four-flap patients.
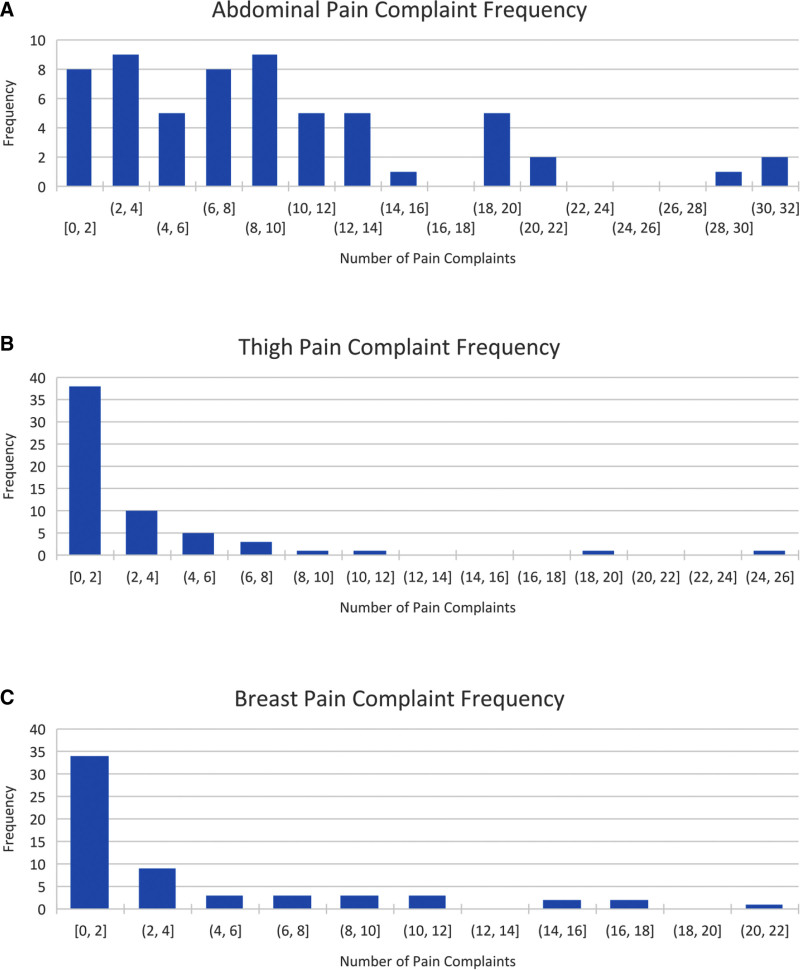
With regard to donor site pain, mean instances of donor site pain location recorded at the abdomen (9.72 instances; 95% CI, 7.78–11.66) were significantly higher than the thigh (2.82 instances; 95% CI, 1.63–4.00) during the postoperative admission (P ≤ 0.0001). The distribution of donor site complaint frequency between abdomen, thigh, and breast sites is shown in Figure 3. Mean pain score severity by NPRS was statistically similar between abdomen, thigh, and breast surgical sites.
Fig. 3.
Number of pain complaints per surgical location. A–C, Four-flap inpatient admission distribution of donor site complaint frequency of recorded instances of pain for the abdomen, thigh, and breast.
Postoperative donor site survey results were completed in 45 patients and are shown in Table 3. More than half of patients reported aesthetic improvement of the thighs (56.1%). With regard to donor site pain, 50% reported more pain to the PAP donor site, and 33.3% reported equal pain between PAP and DIEP donor sites. The DIEP donor site was preferred to the PAP in 55.6% of patients, with equal preference among 33.3%. A majority of patients did not have limitation in daily living (73.2%) and would make the same decision for four-flap reconstruction (87.3%).
Table 3.
Postoperative Survey and Donor Site Comparison among Four-flap Patients
| Do you feel your thighs were aesthetically improved? | Frequency | Percent |
| Yes | 32 | 56.1 |
| No | 16 | 28.1 |
| Same | 9 | 15.8 |
| Do you feel your buttock shape was aesthetically improved? | Frequency | Percent |
| Yes | 15 | 26.3 |
| No | 20 | 35.1 |
| Same | 22 | 38.6 |
| Is your thigh sensation changed? | Frequency | Percent |
| Same | 23 | 39.7 |
| Increased | 5 | 8.6 |
| Decreased | 30 | 51.7 |
| Which donor site caused more pain? | Frequency | Percent |
| DIEP | 9 | 16.7 |
| PAP | 27 | 50 |
| Both equal | 18 | 33.3 |
| Which donor site do you prefer? | Frequency | Percent |
| DIEP | 30 | 55.6 |
| PAP | 7 | 13 |
| Both equal | 17 | 31.5 |
| Which donor site was easier to care for? | Frequency | Percent |
| DIEP | 40 | 78.4 |
| PAP | 3 | 5.9 |
| Both equal | 8 | 15.7 |
| Does either donor site limit your daily living? | Frequency | Percent |
| DIEP | 6 | 10.7 |
| PAP | 7 | 12.5 |
| Both | 2 | 3.6 |
| Neither | 41 | 73.2 |
| Would you make the same decision for four-flap reconstruction? | Frequency | Percent |
| Yes | 48 | 87.3 |
Normative BREAST-Q data for all available BREAST-Q modules among any preoperative patients (n = 202) undergoing any reconstruction were compared with the BREAST-Q scores for each of the three postoperative surgical groups (four-flap, DIEP, and PAP), as shown in Table 4. BREAST-Q scores increased for all categories compared with normative preoperative patients with the exception of abdominal well-being, which decreased postoperatively across all three surgical groups. Reliability and validity statistics are included in the appendix.
Table 4.
Comparisons of BREAST-Q Survey between Preoperative and Postoperative Groups
| Breast-Q | Normative Group (N = 202) | Postgroup | P | ||
|---|---|---|---|---|---|
| Four-flap | PAP | DIEP | |||
| (N = 56) | (N = 31) | (N = 256) | |||
| Postoperative satisfaction with breasts | |||||
| Mean ± SD | 48.2 ± 23.5 | 79.7 ± 18.2 | 69.3 ± 19.3 | 73.4 ± 23.4 | Kruskal–Wallis rank sum test <0.001* |
| Median (IQR) | 48.0 (34–58) | 82.0 (69–92) | 71 (54–84) | 78 (58.25–92) | |
| Postoperative psychosocial well-being equivalent | |||||
| Mean ± SD | 64.4 ± 21.5 | 86.4 ± 18.4 | 71.0 ± 21.4 | 75.9 ± 25.2 | Kruskal–Wallis rank sum test <0.001* |
| Median (IQR) | 64.0 (48–80) | 93.0 (76.25–100) | 69.0 (56.5–90) | 83.0 (58–100) | |
| Postoperative physical well-being: chest | |||||
| Mean ± SD | 76.8 ± 23.3 | 84.3 ± 16.6 | 83.1 ± 16.2 | 82.6 ± 18.1 | Kruskal–Wallis rank sum test = 0.179 |
| Median (IQR) | 80.0 (64–100) | 88.0 (79–100) | 88.0 (78–92) | 88.0 (76–96) | |
| Postoperative physical well-being: abdomen | |||||
| Mean ± SD | 80.4 ± 20.7 | 77.0 ± 21.5 | 68.3 ± 30.6 | 71.2 ± 19.3 | Kruskal–Wallis rank sum test ≤0.001* |
| Median (IQR) | 76 (69–100) | 81.0 (62–100) | 66.0 (52.5–83) | 69.0 (58–81) | |
| Postoperative sexual well-being | |||||
| Mean ± SD | 48.2 ± 23.8 | 64.9 ± 25.9 | 54.0 ± 29.8 | 54.6 ± 30.3 | Kruskal–Wallis rank sum test = 0.002* |
| Median (IQR) | 48.0 (31–66) | 54.0 (53–80.25) | 57.5 (33.25–71) | 53.0 (31–74) | |
Each survey question may have missing data between two groups.
*Indicates statistical significance.
DISCUSSION
Increased patient choice for prophylactic mastectomy has led to higher rates of bilateral mastectomy over time.12 Options for autologous bilateral breast reconstruction in patients with inadequate abdominal tissue for body-appropriate reconstruction are limited. Fat grafting following breast reconstruction is often insufficient to achieve large increases in volume, requires serial operations, and is associated with palpable masses and increased postreconstruction imaging.13,14 Furthermore, vascularized adipocutaneous tissue does not undergo anticipated resorption seen in fat grafting due to diffusion-limited oxygenation.15 Patients undergoing radiation therapy after bilateral mastectomy often choose to avoid implant-associated complications. Furthermore, secondary placement of implants after abdominal-based reconstruction is shown to have high rates of infection and implant loss.16 The use of four-flap reconstruction provides adequate tissue for both envelope and volume allowing for ptosis and the feel of a natural breast.
We present the largest series of four-flap breast reconstruction outcomes to date, and the first series of patient-reported outcome measures for four-flap patients. Our results demonstrate that BREAST-Q scores for four-flap patients are comparable to bilateral DIEP flap patients and bilateral PAP patients. Overall, these results are encouraging for patients who may require additional stacked flap configuration for body-appropriate reconstruction. The addition of a second donor site and increased complexity of surgery does not seem to change the final patient outcome as measured by BREAST-Q when compared with bilateral DIEP flaps or bilateral PAP flaps.
Patients are indicated for four-flap reconstruction if there is insufficient abdominal tissue for body-appropriate reconstruction. As expected in our cohort, patients undergoing four-flap reconstruction have a lower BMI when compared with bilateral DIEP patients. In our experience, we find that patients tend to have a reciprocal phenotype of either abdominal or thigh adiposity. In light of this, a patient-centered approach based on each patient’s ideal donor site for tissue transfer is critical for aesthetic reconstruction and donor site management.17
The BREAST-Q module does not address alternative donor sites including the posterior thigh, gluteal, and lumbar regions used in autologous reconstruction. The BREAST-Q module has been used to evaluate alternative lumbar and superior gluteal artery perforator flaps in a nonvalidated questionnaire by substituting abdominal donor site to lumbar and gluteal areas, respectively.8 In our study, rather than substitute donor site word for word and altering the BREAST-Q, we administered the standard BREAST-Q module to all patients and administered a different survey to compare donor sites of alternative regions, in our case the posterior thigh. To further characterize thigh donor sites in these patients, we have previously reported the LEFS scores for patients undergoing PAP flap reconstruction.7 The LEFS is a validated patient reported outcome measures initially used in musculoskeletal conditions and is scored on a maximum of 80 with a minimum level of detectable change of nine points (90% confidence).18,19 Our results showed that four-flap patients had an overall high average LEFS score above 73 with an increasing score trend over time, which is comparable to our bilateral PAP patients in this series and similar to our previously published series on PAP flap reconstruction only patients.7
Four-flap patients are a unique population in which to subjectively compare the experience of both abdominal and thigh donor sites within the same patient. Our analysis of inpatient pain scales demonstrated no differences in the severity of pain between these two donor sites. When analyzing the frequency of pain recorded by location, there was a significantly higher number of abdominal pain instances recorded than the thigh during admission. In contrast, results for our postoperative donor site survey showed that 50% of patients reported that the PAP donor site caused more pain than the abdomen, with 33.3% reporting equal pain between PAP and DIEP donor sites. We hypothesize the immediate postoperative difference to be due to increased muscle spasm of the rectus abdominus muscle from physiologic respiratory motion, coughing, and core abdominal movements. We attribute the patient survey difference of higher PAP pain to increased ambulation once at home and increased donor site contact through use of a commode. The location of the PAP donor site is more difficult to reach and cumbersome with thigh compression garments, with the vast majority of patients reporting ease of care preference for the DIEP donor site over the PAP.
Though most patients felt that their thigh aesthetic appearance was improved, a small majority preferred the DIEP donor site over the PAP overall. This is likely due to the poor scar quality of the PAP closure, given high skin tension from wide beveling of the flap for volume. A majority of patients undergoing four-flap reconstruction would make the same decision again; however, 12.7% of our patients would not make the same reconstructive decision again. We hypothesize that this may reflect unrealistic expectations rather than true regret rate in some patients, but our survey does not specifically elucidate reasons for regret for four-flap surgery and is an area for further research. Scar quality was not specifically assessed in our study and is a limitation. Additional limitations of our study include variance of NPRS inpatient pain score assessment and documentation, low bilateral PAP flap BREAST-Q responses preventing matching, and relatively short-term follow-up. Finally, though institutional BREAST-Q normative data have been previously described, further data are needed to determine generalizability of our population to other geographic or institutional settings.20
CONCLUSIONS
We present the largest series of four-flap breast reconstructive outcomes to date. A highly selected group of patients may require four-flap reconstruction for appropriate envelope, volume, and natural ptosis. Four-flap breast reconstruction provides equivalent BREAST-Q outcomes to bilateral DIEP or bilateral PAP patients. Patients initially report higher frequency of pain to the abdomen during admission, but higher overall pain to the thighs on subjective survey. The majority of patients experienced aesthetic improvement of the thighs and more ease of care for the abdomen, with the vast majority reporting satisfied results with four-flap breast reconstruction.
Footnotes
Published online 25 July 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Ethical approval: Institutional review board approval was obtained for the study. All procedures performed in this study were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
REFERENCES
- 1.Haddock NT, Suszynski TM, Teotia SS. Consecutive bilateral breast reconstruction using stacked abdominally based and posterior thigh free flaps. Plast Reconstr Surg. 2021;147:294–303. [DOI] [PubMed] [Google Scholar]
- 2.Mayo JL, Allen RJ, Sadeghi A. Four-flap breast reconstruction: bilateral stacked DIEP and PAP flaps. Plast Reconstr Surg Glob Open. 2015;3:e383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rozen WM, Patel NG, Ramakrishnan VV. Increasing options in autologous microsurgical breast reconstruction: four free flaps for ‘stacked’ bilateral breast reconstruction. Gland Surg. 2016;5:255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haddock NT, Cho MJ, Teotia SS. Comparative analysis of single versus stacked free flap breast reconstruction: a single-center experience. Plast Reconstr Surg. 2019;144:369e–377e. [DOI] [PubMed] [Google Scholar]
- 5.Hunsinger V, Hivelin M, Derder M, et al. Long-term follow-up of quality of life following DIEP flap breast reconstruction. Plast Reconstr Surg. 2016;137:1361–1371. [DOI] [PubMed] [Google Scholar]
- 6.Allen RJ, Jr, Sobti N, Patel AR, et al. Laterality and patient-reported outcomes following autologous breast reconstruction with free abdominal tissue: an 8-year examination of BREAST-Q data. Plast Reconstr Surg. 2020;146:964–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haddock NT, Teotia SS. Consecutive 265 profunda artery perforator flaps: refinements, satisfaction, and functional outcomes. Plast Reconstr Surg Glob Open. 2020;8:e2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Opsomer D, Vyncke T, Ryx M, et al. Comparing the lumbar and SGAP flaps to the DIEP flap using the BREAST-Q. Plast Reconstr Surg. 2020;146:276e–282e. [DOI] [PubMed] [Google Scholar]
- 9.Cho MJ, Teotia SS, Haddock NT. Classification and management of donor-site wound complications in the profunda artery perforator flap for breast reconstruction. J Reconstr Microsurg. 2020;36:110–115. [DOI] [PubMed] [Google Scholar]
- 10.Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Q-Portfolio. BREAST-Q User Manual Version 1.0. Available at http://qportfolio.org/score-breast-q-breast-cancer-2/. Accessed February 2016. [Google Scholar]
- 12.Sabel MS, Kraft CT, Griffith KA, et al. Differences between breast conservation-eligible patients and unilateral mastectomy patients in choosing contralateral prophylactic mastectomies. Breast J. 2016;22:607–615. [DOI] [PubMed] [Google Scholar]
- 13.Cason RW, Shammas RL, Broadwater G, et al. The influence of fat grafting on breast imaging after postmastectomy reconstruction: a matched cohort analysis. Plast Reconstr Surg. 2020;146:1227–1236. [DOI] [PubMed] [Google Scholar]
- 14.Groen JW, Negenborn VL, Twisk DJWR, et al. Autologous fat grafting in onco-plastic breast reconstruction: a systematic review on oncological and radiological safety, complications, volume retention and patient/surgeon satisfaction. J Plast Reconstr Aesthet Surg. 2016;69:742–764. [DOI] [PubMed] [Google Scholar]
- 15.Suszynski TM, Rohrich RJ, Sieber DA, et al. Bioengineered approach to the design of a fat graft based on mathematical modeling that predicts oxygen delivery. Plast Reconstr Surg. 2019;143:1648–1655. [DOI] [PubMed] [Google Scholar]
- 16.Alhefzi M, Voineskos SH, Coroneos CJ, et al. Secondary implant augmentation in the subpectoral plane following abdominal-based perforator flaps for breast reconstruction. Plast Reconstr Surg Glob Open. 2020;8:e3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haddock NT, Suszynski TM, Teotia SS. An Individualized patient-centric approach and evolution towards total autologous free flap breast reconstruction in an academic setting. Plast Reconstr Surg Glob Open. 2020;8:e2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehta SP, Fulton A, Quach C, et al. Measurement properties of the lower extremity functional scale: a systematic review. J Orthop Sports Phys Ther. 2016;46:200–216. [DOI] [PubMed] [Google Scholar]
- 19.Binkley JM, Stratford PW, Lott SA, et al. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79:371–383. [PubMed] [Google Scholar]
- 20.Klifto KM, Aravind P, Major M, et al. Differences between breast cancer reconstruction and institutionally established normative data using the BREAST-Q reconstruction module: a comparative study. Plast Reconstr Surg. 2020;145:1371–1379. [DOI] [PubMed] [Google Scholar]