Abstract
Background
During prehospital anaesthesia, oxygen delivery to the brain might be inadequate to match the oxygen consumption, with unknown long‐term functional outcomes. We aimed to evaluate the feasibility of monitoring cerebral oxygenation during prehospital anaesthesia and determining the long‐term outcomes.
Methods
We performed a prospective observational feasibility study in two helicopter emergency medical services units. Frontal lobe regional oxygen saturation (rSO2) of adult patients undergoing prehospital anaesthesia was monitored with near‐infrared spectroscopy (NIRS) by a Nonin H500 oximeter. The outcome was evaluated with a modified Rankin Scale (mRS) at 30 days and 1 year. Health‐related quality of life (HRQoL) was measured with a 15D instrument at 1 year.
Results
Of 101 patients enrolled, 83 were included. The mean baseline rSO2 was 79% (73–84). Desaturation for at least 5 min to rSO2 below 50% or a decrease of 10% from baseline occurred in four (5%, 95% CI 2%–12%) and 19 (23%, 95% CI 15–93) patients. At 1 year, 32 patients (53%, 95% CI 41–65) achieved favourable neurological outcomes. The median 15D score was 0.889 (Q1–Q3, 0.796–0.970).
Conclusion
Monitoring cerebral oxygenation with a hand‐held oximeter during prehospital anaesthesia and collecting data on functional outcomes and HRQoL are feasible. Only half of the patients achieved a favourable functional outcome. The effects of cerebral oxygenation on outcomes during prehospital critical care need to be assessed in future studies.
Keywords: cerebral oxygenation, helicopter emergency, medical services, near‐infrared spectroscopy, prehospital anaesthesia
Editorial Comment.
Severely ill patients undergoing prehospital anaesthesia are at risk of cerebral oxygen deprivation. This study assessed a mixed prehospital population in need of anaesthesia and subsequent transportation to hospital by helicopter. In these patients, hand‐held near‐infrared spectrometry of the forehead was feasible and provided signals were consistent with mild and severe desaturation events in 23% and 5% of patients, respectively. Near‐infrared spectroscopy may be an additional noninvasive monitoring option to help the guide supportive therapy in the prehospital setting.
1. INTRODUCTION
Prehospital anaesthesia is a routine procedure in many services providing prehospital critical care. 1 Many patients undergoing prehospital anaesthesia may be at risk of receiving inadequate oxygen delivery to match their cerebral oxygen consumption due to, for example, traumatic brain injury (TBI), intracerebral haemorrhage, seriously compromised haemodynamics or prolonged seizures. General anaesthesia and endotracheal intubation enable controlled ventilation in order to lower the intracranial pressure (ICP) and enhance the cerebral perfusion pressure. 2 However, the procedure also carries several risks. These include not only failure to intubate and other immediate complications related to intubation but also disturbance of haemodynamics and oxygenation. 3 Furthermore, anaesthesia itself may impair cerebral autoregulation and compromise cerebral oxygen delivery. 4 On the other hand, anaesthetic agents decrease the cerebral metabolic demand of oxygen—except a common induction agent in prehospital critical care, ketamine, that increases metabolic rate. 4 Accordingly, it seems that the quality of prehospital anaesthesia plays a central role in achieving a favourable outcome. Anaesthesiologist‐provided prehospital care appears to significantly improve outcomes, whereas poorly provided prehospital anaesthesia and uncontrolled ventilation seem to significantly increase the mortality of TBI patients. 5
Near‐infrared spectroscopy (NIRS) offers the possibility to noninvasively measure the tissue oxygen saturation of the brain. The method has been shown to be feasible in TBI patients and anaesthetised patients in the prehospital setting. 6 , 7 Furthermore, the NIRS values of TBI patients during intensive care are associated with cerebral perfusion pressure and survival. 8 As a noninvasive technology, NIRS is the only one potentially suitable to monitor the cerebral oxygenation of patients anaesthetised in a prehospital setting. Nonetheless, this monitoring modality has some major limitations, including extracerebral contribution to the NIRS signal. 9 Moreover, only the oxygenation of the frontal lobe is measured, and thus, adequate oxygenation of the whole brain cannot be ensured. 10
The association between NIRS values during general anaesthesia and the neurological outcome of patients has not been studied in a prehospital setting. In order to carry out an observational multicentre study (NCT04144803) determining whether cerebral oxygenation deficiency during prehospital anaesthesia is associated with functional outcomes, quality of life or mortality in patients, we performed this observational pilot study to (a) estimate the incidence of cerebral desaturation events during prehospital anaesthesia and (b) assess the feasibility of data collection using a new, hand‐held NIRS monitor in helicopter emergency medical services (HEMS) settings, and long‐term follow‐up including functional outcome.
2. METHODS
2.1. Study design
This prospective observational study was carried out in two helicopter emergency medical services (HEMS) units in Finland. Adult patients undergoing prehospital anaesthesia following routine clinical practice were monitored with NIRS to observe the occurrence of cerebral desaturation events (CDEs). Monitoring started before the induction of general anaesthesia and ended at hospital arrival. Subsequently, the study patients were interviewed at 30 days and 1 year to define neurological outcomes and quality of life. The study protocol was approved by the ethical committee of Helsinki University Hospital (HUS/757/2019) and also by the hospital districts medically responsible for the HEMS units participating in the study. The study protocol was published prior to the study on clinicaltrials.gov (NCT03948711). Clinical investigation of medical devices for human subjects—Good Clinical Practice (ISO 14155:2011)—was followed in conducting the study. The results are reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement. 11
2.2. Study setting
The national HEMS service has been described previously. 12 The HEMS responds almost solely to primary missions and does not have a role in interfacility transfers. The HEMS units who recruited the patients are staffed with a physician (mostly senior anaesthesiologists), a HEMS crew member (nurse paramedic or firefighter with extensive additional training in aviation and prehospital critical care) and a pilot. They are capable, for example, of rapid sequence intubation and prehospital anaesthesia, thoracic decompression, and prehospital blood transfusion. The anaesthetics available for induction of anaesthesia in the units include esketamine, propofol and midazolam. The two latter are also used for maintaining anaesthesia. Fentanyl can be combined with anaesthetics.
HEMS is publicly funded in Finland. HEMS units are dispatched by an emergency dispatcher among other EMS and rescue units according to predefined criteria. The most common types of missions are major trauma, cardiac arrest, and unconsciousness for any reason (e.g., intracranial haemorrhage or drug overdose). The majority of the patients are escorted by ground ambulance to the hospital, while patients from longer distances are transported by helicopter. Both units use rapid response cars in case of weather conditions preventing the use of helicopters or in situations where the patient can be more rapidly reached by car. The patients are transported to public hospitals using electronic patient record systems accessible by the HEMS physicians. All six HEMS bases in Finland have entered detailed data on every mission into the national HEMS database since 2012.
2.3. Participants
All adult patients encountered by the HEMS units and undergoing prehospital anaesthesia were screened for eligibility. Inclusion criteria were age ≥18 years and sedation or anaesthesia provided for endotracheal intubation. Exclusion criteria were cardiac arrest at the time of induction, physical barriers to NIRS measurement (e.g., forehead laceration), situations where the patient was not escorted to the hospital by HEMS physicians, workload being too high to ensure standard levels of clinical care at the time of recruiting, known special vulnerability (mental disability, patients in nursing homes, prisoners and forensic psychiatric patients) and known or evident pregnancy.
2.4. Variables
A cerebral desaturation event (CDE) was predefined as cerebral regional oxygen saturation (rSO2) ≤50% for at least 5 min. However, due to the lack of previous literature and the pilot nature of the current study, different cut‐offs of CDEs were explored.
The feasibility of the device was evaluated by (a) measuring the success rate of monitoring and (b) the proportion of artefact‐free records from the whole monitoring period. As a safety endpoint, we compared the on‐scene times of patients fulfilling the inclusion criteria treated by the study units during the study period and the same timeframe in the previous 2 years.
The clinical outcome measures included 30‐day and 12‐month mortality, neurological outcome at 30 days and 1 year and health‐related quality of life (HRQoL) at 1 year. Neurological outcomes were measured using a modified Rankin Scale (mRS) 13 and mRS ≤ 2, corresponding to independent functionality in daily activities, was defined as a favourable outcome. The HRQoL was measured using a 15D instrument 14 in which an ordinal score from zero to five is assigned for 15 dimensions of quality of life: mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, usual activities, mental function, discomfort and symptoms, depression, distress, vitality and sexual activity.
2.5. Study procedures
The NIRS data were collected using a Nonin H500 one‐channel near‐infrared spectroscopy monitor (Nonin Inc.). The sensors used were Model 8204CA single‐patient use, non‐sterile, disposable regional oximetry sensors with EQUANOX Technology (Nonin Medical Inc.). The sensors were connected to the signal processor using an INT‐100 interface cable (Nonin Medical Inc.). In the H500 oximetry system, the signal processor is connected to the display unit with Bluetooth technology. The system uses four wavelengths (730, 760, 810 and 880 nanometres) to estimate haemoglobin–oxygen saturation. The display unit displays the rSO2 value with a graphic trend. The values are stored every second in the device and can be transferred to a USB memory stick afterwards. The software of the monitoring device was updated by the manufacturer after the inclusion of 65 patients. At the time of the study, the device was not yet commercially available nor CE‐marked. The devices were rented, and the sensors were purchased from the manufacturer for study purposes. The manufacturer did not provide any financial support and did not participate in planning, conducting, analysing or reporting the results.
The NIRS monitor was connected to the patient by placing a sensor on the left forehead of the patient in accordance with the manufacturer's manual. Wet or bloody skin was dried before application. The data were stored in the device and exported afterwards to the study database by study personnel. Monitoring was initiated at least 1 min before induction of anaesthesia and continued to hospital arrival. Otherwise, the monitoring and treatment followed standard practice.
Clinical personnel from the HEMS units were trained in three phases. First, the study protocol was presented face to face, and questions were discussed. Second, the personnel received hands‐on training on the use of the device. Last, video‐assisted training was used to demonstrate the investigational measurements to be carried out in a clinical situation. During the training, it was emphasised to the participants that no clinical decision is allowed based on the rSO2 values, but the changes in rSO2 may encourage the clinician to re‐evaluate the other clinical and vital signs. At the beginning of the study, a study nurse was present at the HEMS bases to instruct physicians and paramedics on the use of the device in real clinical situations.
Informed consent before monitoring was neither feasible nor required by the ethical committee. Patients were contacted by the study nurse at 30 days and asked for informed consent. In case of disability of the patient, next of kin was contacted for consent. According to the advice of the ethical committee, the relatives of deceased patients were not contacted. If a patient declined participation in the study, the data were not included in the analyses, and the patient was not interviewed to define neurological outcomes. The legislation on the delayed consent process requires that patients can be expected to benefit from being recruited in the study. In this case, the benefit was monitoring capabilities exceeding the standards of care. Consequently, the blinding of clinicians to rSO2 readings was not possible and they were instructed to review other parameters if they observed significant changes in NIRS values. However, actions based solely on changes of NIRS were not allowed.
After obtaining consent, the neurological outcome was evaluated by telephone interview using mRS by a study nurse who was certified to assess mRS using a worldwide standardised and harmonised certification program. Telephone interviews have previously been validated in scoring for neurological functional outcomes. 13 A good neurological outcome was defined as mRS ≤2, corresponding with independence in daily activities. If a patient or next of kin could not be reached, the mRS was obtained from hospital records when available.
2.6. Other data sources
The case report form (CRF) was integrated into the national HEMS database. 12 A CRF was generated automatically for every patient fulfilling the inclusion criteria and served also as a screening log. Physicians were asked to enter a reason for exclusion or to fill out the CRF for included patients. Patient characteristics, vital signs, data on airway management according to Sunde et al. 15 and other interventions were copied automatically from the routinely registered data to the CRF. The adverse event report form was incorporated into the CRF.
Data on hospital stays were gathered from electronic patient records. Discharge day and discharge diagnoses were abstracted by the investigators.
The study sites were regularly visited, and adherence to the protocol, adequate completion of CRFs and appropriate use of the investigational device were verified. During the study, frequent connection failures between the NIRS monitor and signal processor appeared, leading to patient exclusions by the treating physician and to missing data for some included patients. This issue was resolved with a software update by the device manufacturer during the study and did not affect the data quality otherwise.
Based on expert consensus, we aimed to include 100 patients from two HEMS bases. We considered this sample adequate to demonstrate the feasibility of the data collection methods and to reconfirm the main study sample size estimation.
2.7. Statistical methods
As the distribution of most variables was skewed, data are reported as median and quartiles Q1 and Q3. In the analyses, we compared rSO2 to the baseline, defined as mean rSO2 before induction of anaesthesia. The on‐scene time of the HEMS team was compared to previous years with the Kruskal–Wallis test. For proportions, 95% confidence intervals (95% CIs) were calculated using Wilson–Brown analysis. The 15D HRQoL scores were evaluated according to Sintonen et al. 14 to give an index score ranging from 0 (dead) to 1 (no problems) for each dimension. Missing 15D data were not imputed since the aim of the study was the assessment of the feasibility of data collection and conclusions according to HRQoL cannot be made from this small sample. All statistical analyses were performed using GraphPad Prism version 9.0 for MacOS (GraphPad Software).
3. RESULTS
During the study period, 128 eligible patients were encountered by the HEMS units. Of these, 101 patients were enrolled and 83 were included in the analyses (Figure 1). The characteristics of the patients are presented in Table 1. The median duration of NIRS monitoring was 51 (Q1–Q3 42–63) minutes.
FIGURE 1.
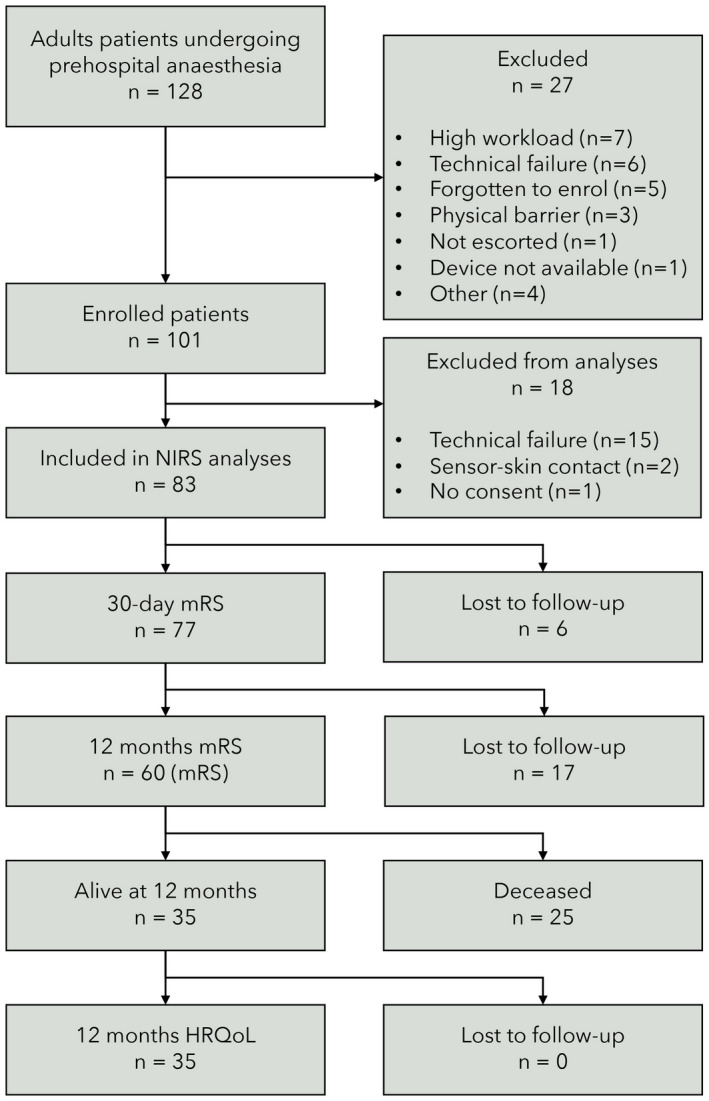
Flow chart of the study population
TABLE 1.
Characteristics of the patients. Continuous variables are presented as median (Q1–Q3). The categoric data are reposted as n (%)
| All patients (n = 83) | Missing data | |
|---|---|---|
| Age, years | 60 (41–69) | 0 |
| Sex, male | 51 (61) | 0 |
| Vital signs when encountered by the HEMS team | ||
| Heart rate; beats per minute | 102 (80–123) | 8 |
| Systolic blood pressure; mm Hg | 135 (112–159) | 10 |
| Respiratory rate; per minute | 20 (16–25) | 27 |
| Oxygen saturation; % | 98 (93–99) | 11 |
| Glasgow Coma Score | 3 (3–6) | 10 |
| Patient category | ||
| OHCA (post‐resuscitation) | 22 (27) | |
| Neurological (excl. stroke) | 19 (23) | |
| Trauma | 15 (18) | |
| Intoxication | 12 (14) | |
| Stroke | 10 (12) | |
| Respiratory failure | 3 (4) | |
| Other | 2 (2) | |
Abbreviations: HEMS, helicopter emergency medical services; OHCA, out‐of‐hospital cardiac arrest (patients anesthetised and enrolled after return of spontaneous circulation).
3.1. Feasibility of NIRS
The NIRS monitoring was successful in 83 patients 83% (95% CI 74–89). The reasons for failure were technical in 15 cases and poor sensor‐skin contact in 2 cases. Additionally, six technical failures, for example, empty battery of the device, occurred before enrolment of the patient. The proportion of artefact‐free monitoring time was 94.5% of the total monitoring time (median 99.1% per patient; Q1–Q3, 93.8–99.8%). The on‐scene time of eligible patients during the study period was similar to patients (n = 279) fulfilling the inclusion criteria and treated within the same timeframe in the previous 2 years in the participating HEMS units (median 31 [25–40] vs. 30 [21–38] minutes, p = .068).
3.2. Cerebral oxygenation
Baseline rSO2 before induction of anaesthesia was available in 73 patients. The reasons for missing baseline included failure to press event marker at the time of induction, artefact in the NIRS signal during the baseline due to sensor‐skin contact, and the period between initiation of the monitoring and induction of anaesthesia was <60 s. The median baseline rSO2 was 79% (Q1–Q3, 73–84) and ranged from 19% to 100%.
Desaturation to absolute rSO2 below 50% for at least 5 min occurred in four patients (5%, 95% CI 2%–12%). The trends of rSO2 during prehospital anaesthesia are shown in Figure 2. Of these patients, one had pulseless electrical activity after intubation, two had hypotension (systolic blood pressure 60–74 mmHg) and one was normotensive. Relative drops of 10%, 20% and 30% from baseline for at least 5 min were occurred in 19 (23%, 95% CI 15–93), 4 (5%, 95% CI 2–12) and 1 (1%, 95% CI 0–7) patients, respectively.
FIGURE 2.
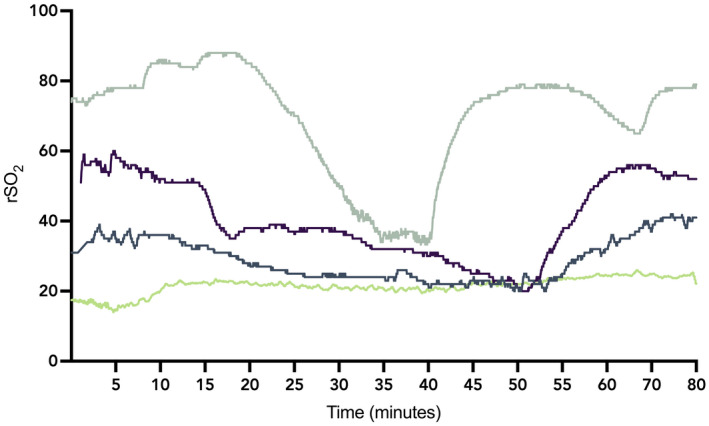
Cerebral oxygen saturation (rSO2) trends of the patients (n = 4) with predefined cerebral desaturation event of rSO2<50% for ≥5 min
The distribution of rSO2 values during prehospital anaesthesia in individuals with a 10% drop from baseline for at least 5 min is presented in Figure 3. In these patients, values were visibly under the baseline during most of the prehospital care time.
FIGURE 3.
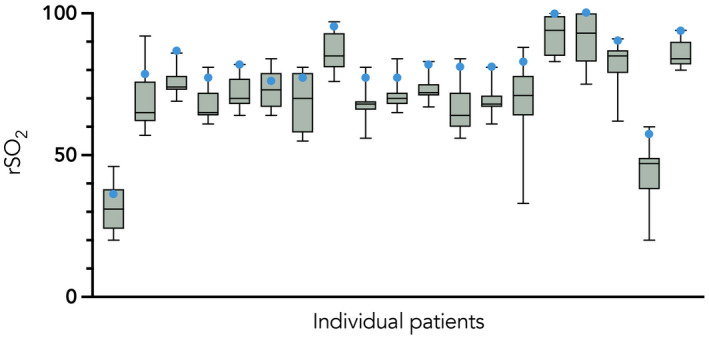
The distribution of rSO2 values during prehospital anaesthesia in patients with cerebral desaturation events, defined as a 10% drop from baseline for at least 5 min. Each box and whiskers represents an individual patient. The baseline before induction of anaesthesia is marked with a circle
3.3. Outcome
Twenty (24%, 95% CI 16–23) patients were deceased at 30 days and 25 (30%, 95% CI 21–41) patients at 1 year. Of the survivors, six patients (10%) were lost to follow‐up for mRS at 30 days and 23 patients (40%) for mRS and 15D at 1 year. Favourable neurological outcomes were achieved in 43 patients (56%, 95% CI −66) at 30 days and 32 patients (53%, 95% CI 41–65) at 1 year. The majority of the survivors achieved good functional outcomes, whereas severe disability was rare (Figure 4). HRQoL was measured in 35 survivors. The 15D score was 0.889 (Q1‐Q3, 0.796 to 0.970). The HRQoL in different dimensions is presented in Figure 5.
FIGURE 4.
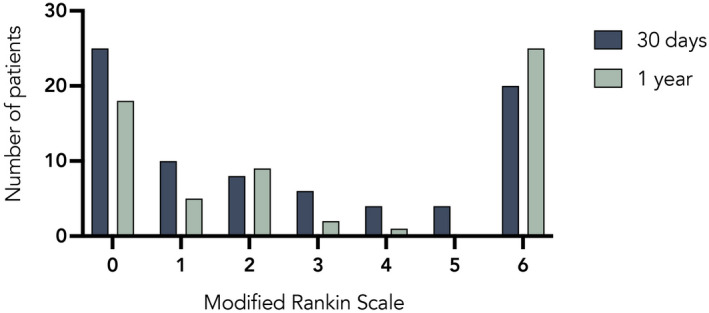
Functional outcomes measured using a modified Rankin Scale (mRS) at 30 days (n = 77) and 1 year (n = 60) after prehospital anaesthesia. 0 denotes normal functional capability, whereas 6 denotes death. A favourable neurological outcome was defined as mRS ≤ 2
FIGURE 5.
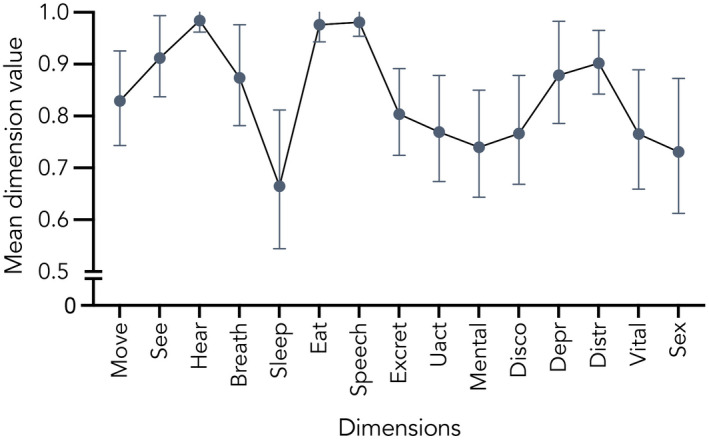
Health‐related quality of life at 1 year after prehospital anaesthesia measured with 15D instrument. Presented as mean with 95% confidence interval. For all other dimensions, n = 35, except sex (n = 32)
3.4. Association between cerebral oxygenation and outcome
No association was observed between outcomes at 30 days and CDEs of different severity levels (Figure 6).
FIGURE 6.
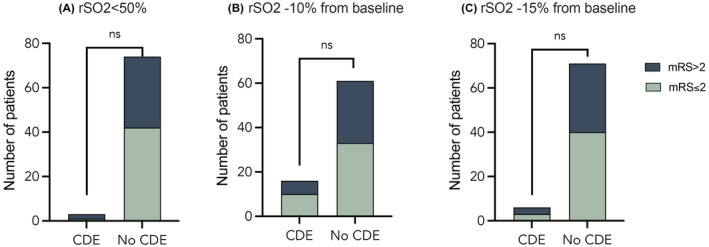
Functional outcome measured with a modified Ranking Scale (mRS) at 30 days after prehospital anaesthesia in patients with and without cerebral desaturation events (CDEs). Different definitions of reginal cerebral oxygen saturation (rSO2) levels of at least 5 min are presented in panels A–C
4. DISCUSSION
This study demonstrates the feasibility of data collection during prehospital anaesthesia with a Nonin H500 hand‐held oximeter as well as follow‐up to determine the functional outcome and HRQoL after prehospital critical care. Furthermore, five per cent of patients met the predefined criteria of CDE. This pilot study was not powered to explore the association between cerebral oxygenation and outcome. However, we observed variation in rSO2 changes during anaesthesia, and approximately only half of the patients were alive and functionally independent at 30 days.
Outcome after critical illness or severe trauma can be measured with multiple domains ranging from physiological variables to functional status and HRQoL. 16 These more complex outcomes are important because many survivors after prehospital critical care represent patient groups characterised by risk of significantly impaired functionality, for example, severe TBI or intracerebral bleeding. 17 , 18 The current study is one of the very rare ones in prehospital critical care reporting these more complex outcomes instead of mortality alone. Furthermore, a sufficient length of follow‐up is important. We have recently reported significant over‐mortality in patients treated by HEMS teams compared to the normal population, even 1‐to‐3 years after a critical incident. 19 In the current study, we observed a low frequency of severe disability in the survivors. The HRQoL in this study was higher than recently reported—for example, in patients with Parkinson's disease or head and neck cancer. 20 , 21 However, the results need to be interpreted cautiously because of the small sample size.
The hand‐held oximeter investigation showed a high rate of artefact‐free monitoring during prehospital care. There is evident need for development of monitoring alternatives in prehospital critical care. These have remained unchanged for decades and include blood pressure, peripheral oxygen saturation, capnography and observations of diameter and reactivity of the pupils. All of these are indirect surrogates of cerebral perfusion and ICP. Most importantly, they do not confirm adequate oxygen delivery. In the prehospital setting, cerebral oxygenation may be threatened in many anaesthetised patients, for example, patients with TBI or stroke, leading to potentially insufficient cerebral perfusion pressure. 22 Likewise, patients successfully resuscitated from out‐of‐hospital cardiac arrest (OHCA) are characterised by post‐resuscitation myocardial stunning, making them hemodynamically unstable, 23 and by altered cerebral autoregulation, 24 both of which threaten adequate cerebral oxygenation. Modern prehospital critical care offers multiple possibilities to improve the ratio of cerebral oxygen delivery and consumption. These include controlled mechanical ventilation, sedation and analgesia, inotropes and vasoactives, intravenous fluids and packed red blood cells. 25
NIRS carries several advantages. It is non‐invasive, easy to use and attainable in the challenging prehospital environment, as demonstrated by the current study as well as previous studies using different monitoring devices. 6 , 7 , 26 Despite its simplicity, it yields insight into a better understanding of the sufficiency of cerebral perfusion pressure and cerebral perfusion. 8 , 27 It even enables defining an individual autoregulatory perfusion pressure range by plotting rSO2 with mean arterial pressure or calculating a cerebral oxygenation (COx) index. 28 , 29 However, multiple factors affect NIRS readings, making them difficult to interpret. 10 It is important to note that even though NIRS is used in multiple patient groups during surgery or intensive care, there is no strong evidence on the association of rSO2 and clinically meaningful outcomes. In particular, no evidence of the advantage of NIRS‐guided therapy compared to standard therapy exists. The NIRS technology itself possesses some uncertainties. The influence of changes in extracranial oxygen saturation cannot be excluded. Furthermore, the algorithms used in the calculation of rSO2 differ between the manufacturers, and not all of these have been published, making a comparison between the devices and studies difficult.
We observed a significant decrease in cerebral rSO2 after the induction of anaesthesia in some patients. The potential explanations include decreased perfusion pressure or cardiac output caused by anaesthetics, hypercapnia during the baseline recording and altered cerebral autoregulation due to anaesthesia. Hypoxia and hypotension are frequently observed in patients undergoing prehospital anaesthesia and airway management. 3 The clinical significance of this finding cannot be evaluated based on this study since it is not powered to detect any association with the outcome. Prehospital anaesthesia is a routine practice performed by trained prehospital physicians and is likely to be beneficial to a majority of patients. 30 However, the findings of the current study raise concern that cerebral oxygenation of some patients may be impaired by the procedure, with potentially harmful consequences. The same phenomenon can occur in hospital practice as well. Future studies are needed to assess the association between cerebral oxygen saturation and outcome.
This study has several strengths. First, the enrolment rate was relatively high, and thus, the study patients represent the actual patient mix undergoing prehospital anaesthesia by HEMS teams. Second, the treatment of the patients followed routine practice, and thus, the results characterise the consequences of the current practice. However, the clinical personnel were not blinded to NIRS values because of regulatory requirements related to the delayed consent process. Thus, we cannot exclude the possibility that the rSO2 readings influenced the treatment of the patients although it was emphasised in training not to make conclusions based on these values. The main limitations also include the fact that only one brain hemisphere was monitored due to the technical characteristics of the device. The sample size was appropriate regarding the aims of the study, but the association of cerebral oxygenation and outcome cannot be explored based on this study. Furthermore, the NIRS values in therapy guidance cannot be evaluated based on this study design. Not all patients could be reached, which can have an effect on the mRS and 15D assessments. Loss to follow‐up was higher at 1 year.
This pilot study was carried out to evaluate the feasibility of data collection with a new NIRS device and on HRQoL and functional outcome in long‐term follow‐up. We aimed to estimate the incidence of CDEs as well as neurological outcomes of the patients to refine the study protocol of the forthcoming main study. The main study is currently in recruiting and aims to assess the association between cerebral oxygenation and neurological outcome (NCT04144803).
5. CONCLUSIONS
Monitoring cerebral oxygenation during prehospital anaesthesia with a Nonin H500 oximetry device and collection of patient‐centred long‐term outcome data after prehospital critical care are feasible. Substantial variation in cerebral oxygenation exists between patients during prehospital anaesthesia. The mortality of the patients is high, but the survivors achieve good functional capability in most cases. The clinical significance of these findings needs to be assessed in the future by an adequately powered study.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
Nurmi J, Laukkanen‐Nevala P, Kirves H, et al. Cerebral oxygen desaturation events during and functional outcomes after prehospital anaesthesia: A prospective pilot study. Acta Anaesthesiol Scand. 2022;66:750–758. doi: 10.1111/aas.14066
Funding information
This work was funded by Helsinki University Hospital (state funding, VTR TYH2019243) and by FinnHEMS Research and Development Unit.
REFERENCES
- 1. Gellerfors M, Fevang E, Bäckman A, et al. Pre‐hospital advanced airway management by anaesthetist and nurse anaesthetist critical care teams: a prospective observational study of 2028 pre‐hospital tracheal intubations. Br J Anaesth. 2028;120(5):1103–1109. doi: 10.1016/j.bja.2017.12.036 [DOI] [PubMed] [Google Scholar]
- 2. Stocchetti N, Carbonara M, Citerio G, et al. Severe traumatic brain injury: targeted management in the intensive care unit. Lancet Neurol. 2017;16:452‐464. doi: 10.1016/S1474-4422(17)30118-7 [DOI] [PubMed] [Google Scholar]
- 3. Sunde GA, Sandberg M, Lyon R, et al. Hypoxia and hypotension in patients intubated by physician staffed helicopter emergency medical services ‐ a prospective observational multi‐centre study. BMC Emerg Med. 2017;17:1‐10. doi: 10.1186/s12873-017-0134-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Slupe AM, Kirsch JR. Effects of anesthesia on cerebral blood flow, metabolism, and neuroprotection. J Cereb Blood Flow Metab. 2018;38:2192‐2208. doi: 10.1177/0271678X18789273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pakkanen T, Nurmi J, Huhtala H, Silfvast T. Prehospital on‐scene anaesthetist treating severe traumatic brain injury patients is associated with lower mortality and better neurological outcome. Scand J Trauma Resusc Emerg Med. 2019;27:1‐7. doi: 10.1186/s13049-019-0590-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Weatherall A, Poynter E, Garner A, Lee A. Near‐infrared spectroscopy monitoring in a pre‐hospital trauma patient cohort: an analysis of successful signal collection. Acta Anaesthesiol Scand. 2019;71:838. doi: 10.1111/aas.13444 [DOI] [PubMed] [Google Scholar]
- 7. Ångerman S, Kirves H, Nurmi J. A before‐and‐after observational study of a protocol for use of the C‐MAC videolaryngoscope with a Frova introducer in pre‐hospital rapid sequence intubation. Anaesthesia. 2018;73:348‐355. doi: 10.1111/anae.14182 [DOI] [PubMed] [Google Scholar]
- 8. Dunham CM, Ransom KJ, Flowers LL, Siegal JD, Kohli CM. Cerebral hypoxia in severely brain‐injured patients is associated with admission Glasgow Coma Scale score, computed tomographic severity, cerebral perfusion pressure, and survival. J Trauma. 2004;56(3):482–491. doi: 10.1097/01.ta.0000114537.52540.95 [DOI] [PubMed] [Google Scholar]
- 9. Weigl W, Milej D, Janusek D, et al. Application of optical methods in the monitoring of traumatic brain injury: a review. J Cereb Blood Flow Metab. 2016;36(11):1825‐1843. doi: 10.1177/0271678X16667953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ghosh A, Elwell C, Smith M. Review article: Cerebral near‐infrared spectroscopy in adults: a work in progress. Anesth Analg. 2012;115(6):1373‐1383. doi: 10.1213/ANE.0b013e31826dd6a6 [DOI] [PubMed] [Google Scholar]
- 11. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806. doi: 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Saviluoto A, Björkman J, Olkinuora A, et al. The first seven years of nationally organized helicopter emergency medical services in Finland – the data from quality registry. Scand J Trauma Resusc Emerg Med. 2020;28:46. doi: 10.1186/s13049-020-00739-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Janssen PM, Visser NA, Mees SMD, Klijn CJM, Algra A, Rinkel GJE. Comparison of telephone and face‐to‐face assessment of the modified Rankin Scale. Cerebrovasc Dis. 2010;29:137‐139. doi: 10.1159/000262309 [DOI] [PubMed] [Google Scholar]
- 14. Sintonen H. The 15D instrument of health‐related quality of life: properties and applications. Ann Med. 2001;33:328‐336. doi: 10.3109/07853890109002086 [DOI] [PubMed] [Google Scholar]
- 15. Sunde GA, Kottmann A, Heltne JK, et al. Standardised data reporting from pre‐ hospital advanced airway management – a nominal group technique update of the Utstein‐style airway template. Scand J Trauma Resusc Emerg Med. 2018;26:1‐16. doi: 10.1186/s13049-018-0509-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Measuring BN, Illness OAC. Measuring outcomes after critical illness. Crit Care Clin. 2018;34:515‐526. doi: 10.1016/j.ccc.2018.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Oie L, Madsbu M, Solheim O, et al. Functional outcome and survival following spontaneous intracerebral hemorrhage: a retrospective population‐based study. Brain Behav. 2018;8:e01113. doi: 10.1002/brb3.1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McCrea MA, Giacino JT, Barber J, et al. Functional outcomes over the first year after moderate to severe traumatic brain injury in the prospective, longitudinal TRACK‐TBI Study. JAMA Neurol. 2021;78(8):982‐992. doi: 10.1001/jamaneurol.2021.2043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Björkman J, Laukkanen‐Nevala P, Olkinuora A, Pulkkinen I, Nurmi J. Short‐term and long‐term survival in critical patients treated by helicopter emergency medical services in Finland: a registry study of 36,715 patients. BMJ Open. 2021;11:e045642. doi: 10.1136/bmjopen-2020-045642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Aro K, Bäck L, Loimu V, et al. Trends in the 15D health‐related quality of life over the first year following diagnosis of head and neck cancer. Eur Arch Oto‐Rhino‐l. 2016;273:2141‐2150. doi: 10.1007/s00405-015-3732-4 [DOI] [PubMed] [Google Scholar]
- 21. Haapaniemi TH, Sotaniemi KA, Sintonen H, Taimela E. The generic 15D instrument is valid and feasible for measuring health related quality of life in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2004;75:976. doi: 10.1136/jnnp.2003.015693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Leinonen V, Vanninen R, Rauramaa T. Raised intracranial pressure and brain edema. Handb Clin Neurol. 2017;145:25‐37. doi: 10.1016/B978-0-12-802395-2.00004-3 [DOI] [PubMed] [Google Scholar]
- 23. Stub D, Bernard S, Duffy SJ, Kaye DM. Post cardiac arrest syndrome: a review of therapeutic strategies. Circulation. 2011;123:1428‐1435. doi: 10.1161/CIRCULATIONAHA.110.988725 [DOI] [PubMed] [Google Scholar]
- 24. Sundgreen C, Larsen FS, Herzog TM, Knudsen GM, Boesgaard S, Aldershvile J. Autoregulation of cerebral blood flow in patients resuscitated from cardiac arrest. Stroke. 2001;32:128‐132. doi: 10.1161/01.STR.32.1.128 [DOI] [PubMed] [Google Scholar]
- 25. Reid BO, Rehn M, Uleberg O, Krüger AJ. Physician‐provided prehospital critical care, effect on patient physiology dynamics and on‐scene time. Eur J Emerg Med. 2018;25:114‐119. doi: 10.1097/MEJ.0000000000000432 [DOI] [PubMed] [Google Scholar]
- 26. Schewe J‐C, Thudium MO, Kappler J, et al. Monitoring of cerebral oxygen saturation during resuscitation in out‐of‐hospital cardiac arrest: a feasibility study in a physician staffed emergency medical system. Scand J Trauma Resusc Emerg Med [internet]. 2014;22:58. http://sjtrem.biomedcentral.com/articles/10.1186/s13049-014-0058-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Taussky P, O’Neal B, Daugherty WP, et al. Validation of frontal near‐infrared spectroscopy as noninvasive bedside monitoring for regional cerebral blood flow in brain‐injured patients. Neurosurg Focus. 2012;32:E2. doi: 10.3171/2011.12.FOCUS11280 [DOI] [PubMed] [Google Scholar]
- 28. Brady KM, Mytar JO, Lee JK, et al. Monitoring cerebral blood flow pressure autoregulation in pediatric patients during cardiac surgery. Stroke. 2010;41:1957‐1962. doi: 10.1161/STROKEAHA.109.575167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chan B, Aneman A. A prospective, observational study of cerebrovascular autoregulation and its association with delirium following cardiac surgery. Anaesthesia. 2019;74(1):33‐44. doi: 10.1111/anae.14457 [DOI] [PubMed] [Google Scholar]
- 30. Lockey DJ, Crewdson K, Lossius HM. Pre‐hospital anaesthesia: the same but different. Br J Anaesth. 2014;113:211‐219. doi: 10.1093/bja/aeu205 [DOI] [PubMed] [Google Scholar]


