Abstract
The Audiology Practice Standards Organization (APSO) has published its second audiology standard. This second standard is focused on adult hearing aid fittings. These standards put forward information about verification that should be completed on hearing aids before, during, and after a fitting. Validation following the verification of the hearing aids to ensure patient satisfaction with the devices is also included in the standards. The goal of this article is to provide clinicians with the guidelines related to hearing aid verification and validation while also providing information about how to put these standards into clinical practice.
Keywords: hearing aid verification, validation, real-ear measures
STANDARDS DISCUSSED
9. An assessment of initial product quality is completed, using standard electroacoustic measures to verify either manufacturer or published specifications.
10. Hearing aids are fitted so that various input levels of speech result in verified ear canal output that meets the frequency-specific targets provided by a validated prescriptive method. The frequency-specific maximum power output is adjusted to optimize the patient's residual dynamic range and ensure that the output does not exceed the patient's loudness discomfort levels.
11. Following individualized verification of hearing aid gain and output, if the fitting is not acceptable to the patient, minor deviations in gain and output may be necessary.
Fitting a hearing aid without utilizing verification and validation can be likened to driving a car without a speedometer and without a destination in mind. Hearing aid programming software can give approximations for the output of a hearing aid or functionality in different environments; however, verification is required to ensure that the goal of the hearing aid fitting (returning audibility across frequency and input level by meeting evidence-based targets) is achieved. Hearing loss is a common condition that has detrimental effects on quality of life 1 and appropriately fitted hearing aids can reduce the impact of hearing loss. Verification is key in determining if a hearing aid is functioning adequately and is fit with that patient's hearing loss and ear canal characteristics 2 in mind.
Currently, the use of real-ear probe microphone measurements is the most efficient, accurate way to verify that the output of the hearing aid is meeting evidence-based targets across frequency and input levels. The use of verification techniques in audiology clinics has been widely discussed in hearing health care forums. Mueller and Picou have completed many surveys regarding the use of real-ear probe microphone measurements for verification purposes and for the past 25 years, the results indicate that 34 to 53% of respondents use this verification technique. 3 The 2020 American Academy of Audiology (AAA) Member Connect Survey was recently conducted and showed a majority (68%) of AAA members have real-ear probe microphone measurement equipment and use it consistently. 4 These surveys indicate that rates of consistent use of verification equipment may be increasing; however, there is room for improvement.
Clinicians who choose not to verify that hearing output has met evidence-based targets using standard equipment for this purpose often list the cost of the equipment, time, and lack of benefit as barriers to use. Former president of the AAA, Catherine Palmer, suggested that clinicians not verifying the output of hearing aid fittings (i.e., using real-ear probe microphone verification) are practicing unethically and in opposition to the AAA Code of Ethics. 5 Patient satisfaction supports the importance of verifying the function and fitting of hearing aids. Research has found that more testing (including real-ear verification) completed during a hearing aid fitting appointment improves a patient's satisfaction with their hearing aids. 6 7 Following verification of the hearing aid output to target, patient validation is another component to ensure the hearing aids are meeting the needs and expectations of the patient. Validation is an objective (e.g., hearing in noise) or subjective measure (e.g., perceived benefit) provided by the wearer of the hearing aids. 8 Both verification and validation confirm the patient has access to needed acoustic information and that the patient is receiving quality hearing health care. 9 Following the release of the APSO standards for adult hearing aid fittings, we will review how these standards can be put into practice for hearing aid verification and validation.
9. An assessment of initial product quality is completed, using standard electroacoustic measures to verify either manufacturer or published specifications.
10. Hearing aids are fitted so that various input levels of speech result in verified ear canal output that meets the frequency-specific targets provided by a validated prescriptive method. The frequency-specific maximum power output (MPO) is adjusted to optimize the patient's residual dynamic range and ensure that the output does not exceed the patient's loudness discomfort levels.
11. Following individualized verification of hearing aid gain and output, if the fitting is not acceptable to the patient, minor deviations in gain and output may be necessary.
BEFORE PATIENT ARRIVAL
The minimum standard, according to the APSO, prior to a hearing aid fitting is to assess that the hearing aids meet the standard electroacoustic measurements provided by the manufacturer. 10 The American National Standards Institute (ANSI) S3.22–1976 Standard Specification of Hearing Aid Characteristics 11 was created to ensure manufacturers would test their hearing aids and report the results on a set of standard measurements. The ANSI hearing aid standard outlines what measurements should be conducted and an acceptable tolerance range for each measurement.
In 2009, ANSI S3.22.2009 12 created an Automatic Gain Control (AGC) test protocol to test various functions of a hearing aid sequentially. This protocol can be loaded on verification equipment to measure maximum output, high-frequency average output, average gain at a moderate intensity, distortion, internal noise, and attack and release times. These measurements and parameters are important for manufacturers and clinicians to ensure hearing aids are uniform and are performing to expectations. These standards were further updated and revised in ANSI S3.22–2014.
When hearing aids are shipped from each manufacturer, a printout of the ANSI information is included; however, some clinicians dismiss this information. A reason for the rejection of this information is a possible lack of education regarding hearing aid verification measurements and the equipment that performs these tests. Furthermore, some hearing healthcare providers are unable to test the hearing aids in their office due to the lack of verification equipment, as was discussed previously.
ANSI Protocol
When new hearing aids arrive at the clinic, electroacoustic analysis (EAA) needs to be completed. Clinicians should be checking the hearing aids upon their arrival because research has revealed that new hearing aids can largely be noncompliant with ANSI standards. 14 The hearing aids must be set to the appropriate test settings before running the ANSI test on the verification equipment. To accomplish this, the hearing aids must be connected to the corresponding fitting software to set the hearing aid to its ANSI gain setting. These settings might not be easy to locate at a glance. Most major manufacturers have this gain setting under a technical or ANSI measurements section. Upon switching the hearing aid into its ANSI gain setting, an ANSI protocol can be run on the hearing aid using the verification equipment. See Fig. 1 for an example of how a clinician would couple a RIC hearing aid for ANSI testing. After testing is completed, it is very important to remember to return the hearing aid to its previous settings or “first-fit” the device for the patient. This ensures the patient does not have full-on gain hearing aids in their ears when they arrive for their fitting appointment.
Figure 1.

Example of how to couple a hearing aid to a test box for ANSI testing (courtesy of Audioscan).
Directional Microphone Verification
Directional microphones in theory provide an improved signal-to-noise ratio (SNR) by attenuating sounds from the back allowing the patient to focus on the sounds coming from the front. For this to happen, the back and front omnidirectional microphones must be at a fixed distance and matched in sensitivity. Unfortunately, the MEMS microphones used in hearing aids can have drift (i.e., mismatch in sensitivity) due to debris, microphone damage, or environmental factors. 15 Verification equipment allows clinicians to assess the sensitivity of the front and back hearing aid microphones while the hearing aid is in the directional setting. You will follow the instructions of your equipment for this measurement.
When utilizing the Verifit 1 or 2 from Audioscan to complete directional microphone testing, two lines appear on the screen. See Fig. 2 for an illustration of this measurement. To determine that directional microphones are functioning appropriately, we are looking for the separation of the dark green and light green lines. The darker line should be at a higher level than the thinner, lighter line if the directional microphones are functioning. If there is no separation of these lines, there are a few things to troubleshoot. Before running the test, it is important to activate the directional microphones in the programming software. In addition, clinicians should be aware of the SNR that is being used during the testing. If the SNR level is set too high, the hearing aids might not allow the directional microphones to be active. Lowering the SNR level might improve the situation and allow for the directional microphones to be engaged in signal processing.
Figure 2.

Measurement of directional microphone performance (courtesy of Audioscan).
One should always check the positioning of the hearing aid(s) in the test box to ensure the placement is following the manufacturer's guidance. If a lighter curve appears above the darker line, the hearing aid microphones may have been wired incorrectly. This creates issues for the patient's perception. Finally, if you are unable to get the measurements to separate after completing troubleshooting, the devices might require cleaning or manufacturer's repair.
AFTER PATIENT ARRIVAL
Real Ear to Coupler Difference
After certifying the function of the hearing aids, they are ready to be fit on the patient. Verification equipment, specifically on-ear probe microphone equipment, is used to obtain a variety of measures. One important measure is the real ear to coupler difference (RECD) which is the difference in decibels, as a function of frequency between the sound pressure level (SPL) at a specified measurement point in the ear canal and the SPL in a 2-cc coupler, for a specified input signal. The 2-cc coupler represents the ear canal volume of the average white adult male. RECD allows the measurement equipment to convert the audiometric information collected during testing from dB HL to dB SLP. With this information, the verification equipment provides the SPL thresholds for the evidence-based fitting algorithms to use when producing targets across frequency and input levels.
The use of RECD to accurately produce targets for a hearing aid fitting is widely accepted in pediatric hearing aid fitting given the understanding that a pediatric ear is likely to be much smaller than an average adult ear and that ignoring this difference will lead to inaccurate hearing aid fittings. If the goal is to fit to evidence-based targets, then the targets need to be accurate, and to accomplish this RECD would need to be used to convert HL to SPL data specific to an individual for any patient regardless of age given that most ears are not average.
To complete RECDs is a simple process that does take some practice to master. Most verification systems have a similar process, but some subtle differences are discussed in the equipment's manual or user guide. Generally, the process begins with ensuring the equipment is calibrated and ready to begin gathering data. The RECD transducer is first measured attached to the coupler to obtain the “coupler” part of the RECD measurement. Next, it is important to complete otoscopy to check and see if the ear canal is free from major obstructions. The probe module is placed on the ear with the reference microphone facing outward. Next, a probe tube is inserted into the ear canal to an appropriate depth, within 2 to 5 mm of the eardrum. At this depth, the black marker on the probe tube is seated within the intertragal notch (see Fig. 3 ).
Figure 3.
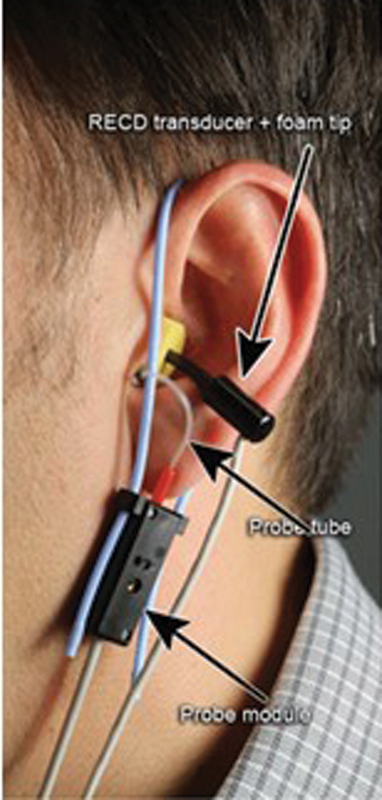
Depiction of correct real ear to coupler difference (RECD) transducer and probe tube placement (courtesy of Audioscan).
The RECD transducer with a foam tip is then similarly placed in the ear canal if an insert was used for audiometric testing. Finally, the measure can be taken. Before using this measure to continue the hearing aid fitting process, be sure to examine it for some possible issues. When the ear canal measurement is significantly lower than expected in the low frequencies, there may be a leak in the ear canal seal. If there is a lower than expected response in only the high frequencies, then there is possibly an issue with the probe tube. Check that the probe tube is clear and that the probe tube placement is correct. When in doubt try repositioning the probe module, tube, and RECD transducer. Fig. 4 shows an example of what a typical RECD response looks like. The top two responses show the coupler response and the real-ear response. These results are then subtracted from each other and the result is the RECD, which is displayed near the bottom with the average RECD.
Figure 4.

Real ear to coupler difference (RECD) measurement (courtesy of Audioscan).
The next step includes measuring the output of the hearing aid across frequency and input level, call the real-ear aided response (REAR). Before completing this measure, an evidence-based fitting formula must be selected to generate the appropriate output targets.
HEARING AID PRESCRIPTIVE FITTING APPROACHES
NAL-NL2 is the current iteration of the National Acoustics Laboratory fitting formula. NAL-NL2 was created to fit current wide dynamic range compression hearing aids by providing targets across frequency specific to input levels (i.e., differing gain depending on input). Its goal is to make speech intelligible and have overall comfortable loudness. This aim is driven by the principle that these factors are most often important for hearing aid users but is also driven by the fact that less information is available about how to adjust the gain to optimize other parameters such as localization, tonal quality, detection of environmental sounds, and naturalness. This version also takes the age, gender, hearing aid experience, language, and compressor speed into consideration. This fitting formula is typically used with adults who are fit with hearing aids later in life.
The desired sensation level (DSL) method is used to fit hearing aids by ensuring that speech is amplified to audible levels without allowing loud sounds to be uncomfortable. DSL v.5 [i/o] is commonly used for pediatric hearing aid fittings; however, the adult version is appropriate for adult fittings. The use of DSL targets is recommended if the patient was previously fit as a child using DSL targets. DSL-A targets are used for adult hearing aid fittings (acquired hearing loss), while the DSL-C targets are used for children (congenital hearing loss). The adult targets are approximately 7 dB lower (quieter) than the child targets. The current iteration of DSL is DSL v.5.
REAR PROCEDURES
After choosing a fitting formula and completing RECD, the targets are individualized to the patient and the process of the hearing aid fitting can continue. The REAR is a measure that records the output of the hearing aid at or near the eardrum. During this measure, speech-like signals are presented at levels that are considered to be soft, moderate, and loud in the sound field and the output SPL from the hearing aid in the ear canal is displayed against the patient's threshold in dB SPL and targets derived from an evidence-based fitting formula. The overall goal of completing this test is to ensure sounds are audible, comfortable, and maintain appropriate loudness for soft, moderate, and loud sounds. These goals all together allow for improved speech understanding and satisfaction with the devices.
To complete the REAR, the process is similar but different from that of measuring the RECD. The probe microphone tube is placed down the ear canal close to the tympanic membrane.
The hearing aid is then carefully inserted with the probe tube in the ear canal. It is important to make sure that the tube is not pushed in further while inserting the earmold or hearing aid receiver/dome. To prevent this, the clinician can hold the tube against the ear lobe while inserting the hearing aid. If the probe tube is inserted too deeply, the patient might experience discomfort or pain if it hits the tympanic membrane. In addition, inappropriate hearing aid insertion may cause the probe tube to bend and/or face the ear canal wall and result in an inaccurate REAR.
Next, it is important to ensure the speaker is positioned to allow for reliable and accurate probe microphone measurements. Some systems have internal and external speakers. The internal sound-field speaker is a built-in speaker and is not convenient for on-ear measures, especially for pediatric patients. The external speaker is especially helpful when completing real-ear measures because it is adjustable. These speakers may become overdriven because of the creation of standing waves from nearby walls and reflective surfaces. When selecting a location for the verification equipment, consider placing it away from reflective surfaces. The speaker should be positioned at a distance of 18 to 24 inches, or about a forearm's length, from the middle of the head.
Once the speakers, hearing aid, and probe tube are determined to be in the correct orientation, the process of REAR begins. The hearing aid should be connected to the corresponding programming software so that changes can be made to the gain for soft, moderate, and loud sounds to match the measured output to the targets displayed on the measurement screen. Using the verification equipment allows clinicians to present various signals to the patient. Current nonlinear hearing aids require complex speech signals to get a better understanding of hearing aid function. 16 One of the most common signals used during real-ear measures is the International Speech Test Signal (ISTS). This signal is non-intelligible speech that uses speech from six different languages and is shaped to the long-term average speech spectrum (LTASS). Some providers use the “carrot passage” or “rainbow passage”; however, it should be noted these measures only utilize English speech.
After selecting the stimulus parameters, the measurement can begin. Some clinicians prefer to start with the soft or moderate input level. It does not matter and is up to personal preference. In addition, some clinicians prefer to present at 50, 65, and 80 dB, while others increase in increments of 10 dB (55, 65, and 75 dB). Again, this is a matter of personal preference and both methods give a valid response of what is happening at soft, moderate, and loud intensities because the generated targets will be specific to the input levels that are chosen. A measure of the MPO of the hearing aid should be completed. This also can be considered the output SPL at 90 dB SPL input. If responses do not match the targets, make appropriate programming changes to the hearing aid(s). In addition, the MPO should never pass the levels of the Uncomfortable Loudness Level (UCL) to ensure patient comfort and safety. Sometimes the targets generated will be below the patient's threshold because the hearing threshold is at a level that does not allow audibility.
PATIENT BENEFIT
Verification allows clinicians to ensure that the goal of the hearing aid fitting has been met—producing an audible signal across frequency and input levels. Clinicians without verification equipment fit hearing aids using manufacturer first fit and participant report; however, research has confirmed these methods are not as effective as real-ear measures in ensuring the goals of a hearing aid fitting have been met. 17 18
Furthermore, Abrams and colleagues completed a questionnaire of hearing aid users wearing devices programmed to NAL-NL1 targets with minor adjustments and devices programmed to the manufacturer's first fit. 18 The verified fittings produced a higher perceived benefit. This increase in patient benefit is likely related to audibility. Patients fit with verified hearing aid acoustic responses performed better on tests measuring word recognition and other measures at a soft intensity. 19 In the same study, they determined that participants preferred their devices when programmed with the verified settings. Additional studies have confirmed that real-ear probe microphone measures support audibility and patient satisfaction. 20 21
Real-ear measurements add time to a fitting appointment; however, the established benefits of this process cannot be overstated. An industry-wide survey concluded that completing real-ear probe microphone measurements reduces the number of adjustment visits a patient makes to the clinic. 22 The added cost and time of completing these measurements are negligible when considering the added benefit to the patient and the practice. Reducing additional programming appointments opens up availability for providers to complete other appointments to support new and returning patients. It also reduces the burden on the patient and their potential caregivers, as they do not have to return as regularly for adjustments. In summary, real-ear probe microphone measurements are used to verify that the hearing aid output matches evidence-based targets to ensure audibility which is the basis for all hearing aid fittings.
POST-FITTING ADJUSTMENTS AND COUNSELING
Once the verification process has been completed, clinicians typically ask the patient about how the hearing aids are sounding. This is the time when minor adjustments to address perceptual complaints take place. New hearing aid users might comment on the loudness of the hearing aids. In these cases, it is allowable to reduce the overall gain to a level that is more comfortable but still provides good audibility. The adaptation manager is very useful in cases like this because the gain can be set to slowly increase over a set period to finally match the verified fitting. It is important to remind the patient that they have been hearing through a filter (their hearing loss) for an extended period of time and the brain needs to adjust to this new sound.
Patients might also report issues with the sound of their own voice. These are issues related to low-frequency gain and venting. Gain can be lowered in the low frequencies to try to resolve this perceptual complaint; however, an acoustic modification might be advised—increasing the vent size in the earmold or swapping the dome for a more open fitting. It is important to note that if a change like this is completed, real-ear probe microphone measures should be completed again to ensure audibility. Once the patient is happy with the volume and balance of their hearing aids, the clinician needs to complete orientation and counseling.
This is also a time to remind the patient of the purpose of hearing aids and the aural rehabilitation process. The ultimate goal when fitting hearing aids is to improve a patient's communication competence. Patients do not care about hearing pure tones in a sound booth; they want to be able to communicate with their loved ones and take part in activities they used to enjoy. Improving the communication competence of the patient will also improve the quality of life of those around them. The patient must know that they will not have perfect hearing, but they will be given technology and aural rehabilitative techniques to improve their communication competence to be able to communicate with those close to them.
Once the hearing aids are set to the point where the patient is happy and knows about their devices, clinicians should run a frequency/gain (or output) curve on the devices after all adjustments have been made. It is useful to keep in the patient's chart to refer to when hearing aid function is in question. If a patient complains that their hearing aid is not working like it used to, but the gain curve has not changed, and other electroacoustic measures are consistent, it might not be a hearing aid issue. Clinicians can start to resolve this complaint by completing an otoscopic examination, basic hearing aid troubleshooting, and/or re-test the patient's hearing. See Fig. 5 to see an instance of why completing this measure is very useful.
Figure 5.

Illustration of how hearing aid output can decline overtime and usefulness of test box measures to confirm patient reports and troubleshoot hearing aid performance.
VALIDATION
Validation occurs after the patient has adjusted to the newly returned audibility. Validation measures should be tailored to the individual's goals for the hearing aid fitting and aural rehabilitation plan. Validation measures whether the patient's goals have been achieved. In the analogy provided at the beginning of this article, validation is about whether you go to where you were planning to go. Validation can be measured with objective testing (e.g., speech in noise improvement) or with subjective measures that may sample benefit, satisfaction, meeting expectations, etc.
CONCLUSION
Hearing aid verification and validation are essential to the adult hearing aid fitting process. Improved audibility verified by real-ear probe microphone measures to ensure that output is meeting evidence-based targets. After verification, clinicians use their knowledge of sound and clinical experience to adjust the devices to resolve perceptual complaints. Patients on average prefer verified and validated hearing aid fittings and return to the clinic less for follow-up visits. When patients are doing better, clinicians and office staff have more time to complete daily tasks and see patients with more complex needs.
Footnotes
Conflict of Interest None declared.
References
- 1.Palmer C V, Mulla R, Dervin E, Coyan K C. HearCARE: hearing and communication assistance for resident engagement. Semin Hear. 2017;38(02):184–197. doi: 10.1055/s-0037-1601574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hear well in a noisy world: hearing aids, hearing protection & more. Consum Rep. 2009;74(07):32–37. [PubMed] [Google Scholar]
- 3.Mueller H G, Picou E M. Survey examines popularity of real-ear probe-microphone measures. Hear J. 2010;63(05):27–28. [Google Scholar]
- 4.Zitelli L, Jedlicka D, Scagline T, Cody Leslie, Reitz A, Palmer C.The results are in: 2020 member survey of the use of real-ear probe microphone measurements. Audiol Today 2020. Accessed April 10, 2022 at:https://www.audiology.org/news-and-publications/audiology-today/articles/online-feature-the-results-are-in-2020-member-survey-of-the-use-of-real-ear-probe-microphone-measurements/
- 5.Palmer C V. Best practice: It's a matter of ethics. Audiol Today. 2009;21(05):31–35. [Google Scholar]
- 6.Kochkin S, Beck D L, Christensen L A. MarkeTrak VIII: The impact of the hearing healthcare professional on hearing aid user success. Hear Rev. 2010;(04):12–34. [Google Scholar]
- 7.Beck D L.Do real-ear measurements make a real difference to patient outcomes? 2010. Accessed April 10, 2022 at:www.audiology.org/news/interviews/Pages/20090119a.aspx
- 8.Guidelines for hearing aid fitting for adults Am J Audiol 19987015–13.26649513 [Google Scholar]
- 9.Jorgensen L E. Verification and validation of hearing aids: opportunity not an obstacle. J Otol. 2016;11(02):57–62. doi: 10.1016/j.joto.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.S2 1 Hearing Aid Fitting for Adult & Geriatric Patients. APSO - Current StandardsPublished May 2, 2021 at:https://www.audiologystandards.org/standards/display.php?id=102
- 11.American National Standards Institute (ANSI) Specifications of Hearing Aid CharacteristicsANSI 3.22–1976.New York, NY: ANSI; 1976 [Google Scholar]
- 12.American National Standards Institute (ANSI) Specification of Hearing Aid CharacteristicsANSI 3.22–2009.New York, NY: ANSI; 2009 [Google Scholar]
- 13.American National Standards Institute (ANSI) Specification of Hearing Aid CharacteristicsANSI 3.22–2014.New York, NY: ANSI; 2014 [Google Scholar]
- 14.Holder J T, Picou E M, Gruenwald J M, Ricketts T A. Do modern hearing aids meet ANSI standards? J Am Acad Audiol. 2016;27(08):619–627. doi: 10.3766/jaaa.15027. [DOI] [PubMed] [Google Scholar]
- 15.Thompson S. Dual microphones or directional-plus-omni: which is best? High Perf Hear Sol. 1999;3:31–35. [Google Scholar]
- 16.Valente M. New York: Thieme; 2002. Hearing Aids: Standards, Options, and Limitations. 2nd ed. [Google Scholar]
- 17.Mueller H G. Probe microphone measurements: 20 years of progress. Trends Amplif. 2001;5(02):35–68. doi: 10.1177/108471380100500202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abrams H B, Chisolm T H, McManus M, McArdle R. Initial-fit approach versus verified prescription: comparing self-perceived hearing aid benefit. J Am Acad Audiol. 2012;23(10):768–778. doi: 10.3766/jaaa.23.10.3. [DOI] [PubMed] [Google Scholar]
- 19.Sanders J, Stoody T M, Weber J E, Mueller H G. Manufacturer's NAL-NL2 fittings fail real-ear verification. Hear Rev. 2015;21(03):24. [Google Scholar]
- 20.Valente M, Oeding K, Brockmeyer A, Smith S, Kallogjeri D. Differences in word and phoneme recognition in quiet, sentence recognition in noise, and subjective outcomes between manufacturer first-fit and hearing aids programmed to NAL-NL2 using real-ear measures. J Am Acad Audiol. 2018;29(08):706–721. doi: 10.3766/jaaa.17005. [DOI] [PubMed] [Google Scholar]
- 21.Amlani A M, Pumford J, Gessling E. Improving patient perception of clinical services through real-ear measurements. Can Audiol. 2016:4–5. [Google Scholar]
- 22.Bratt G W, Rosenfeld M AL, Peek B F, Kang J, Williams D W, Larson V. Coupler and real-ear measurement of hearing aid gain and output in the NIDCD/VA Hearing Aid Clinical Trial. Ear Hear. 2002;23(04):308–315. doi: 10.1097/00003446-200208000-00006. [DOI] [PubMed] [Google Scholar]


