Abstract
Background: Fructose providing excess calories in the form of sugar sweetened beverages (SSBs) increases markers of non-alcoholic fatty liver disease (NAFLD). Whether this effect holds for other important food sources of fructose-containing sugars is unclear. To investigate the role of food source and energy, we conducted a systematic review and meta-analysis of controlled trials of the effect of fructose-containing sugars by food source at different levels of energy control on non-alcoholic fatty liver disease (NAFLD) markers. Methods and Findings: MEDLINE, Embase, and the Cochrane Library were searched through 7 January 2022 for controlled trials ≥7-days. Four trial designs were prespecified: substitution (energy-matched substitution of sugars for other macronutrients); addition (excess energy from sugars added to diets); subtraction (excess energy from sugars subtracted from diets); and ad libitum (energy from sugars freely replaced by other macronutrients). The primary outcome was intrahepatocellular lipid (IHCL). Secondary outcomes were alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Independent reviewers extracted data and assessed risk of bias. The certainty of evidence was assessed using GRADE. We included 51 trials (75 trial comparisons, n = 2059) of 10 food sources (sugar-sweetened beverages (SSBs); sweetened dairy alternative; 100% fruit juice; fruit; dried fruit; mixed fruit sources; sweets and desserts; added nutritive sweetener; honey; and mixed sources (with SSBs)) in predominantly healthy mixed weight or overweight/obese younger adults. Total fructose-containing sugars increased IHCL (standardized mean difference = 1.72 [95% CI, 1.08 to 2.36], p < 0.001) in addition trials and decreased AST in subtraction trials with no effect on any outcome in substitution or ad libitum trials. There was evidence of influence by food source with SSBs increasing IHCL and ALT in addition trials and mixed sources (with SSBs) decreasing AST in subtraction trials. The certainty of evidence was high for the effect on IHCL and moderate for the effect on ALT for SSBs in addition trials, low for the effect on AST for the removal of energy from mixed sources (with SSBs) in subtraction trials, and generally low to moderate for all other comparisons. Conclusions: Energy control and food source appear to mediate the effect of fructose-containing sugars on NAFLD markers. The evidence provides a good indication that the addition of excess energy from SSBs leads to large increases in liver fat and small important increases in ALT while there is less of an indication that the removal of energy from mixed sources (with SSBs) leads to moderate reductions in AST. Varying uncertainty remains for the lack of effect of other important food sources of fructose-containing sugars at different levels of energy control.
Keywords: alanine aminotransferase, aspartate aminotransferase, intrahepatocellular lipid, non-alcoholic fatty liver disease, sugars, sugar-sweetened beverages
1. Introduction
Sugars consumption has been implicated in the development of non-alcoholic fatty liver disease (NAFLD), the leading form of chronic liver disease worldwide [1] and its associated downstream metabolic diseases including obesity, type 2 diabetes, hypertension, and dyslipidemia [2,3]. There is a specific focus on fructose because of its unique metabolism where it bypasses negative feedback control and acts as an unregulated substrate for de novo lipogenesis, which can stimulate liver fat accumulation [4,5]. Clinical Practice guidelines for the prevention and management of NAFLD recommend a reduction in fructose in addition to weight loss and increased exercise [6].
The evidence to support recommendations to reduce fructose derives largely from trials of overfeeding using sugar-sweetened beverages. An earlier systematic review and meta-analysis of controlled feeding trials [7] of sugar-sweetened beverages (SSBs) showed that when consumed at high doses providing excess calories, there was a significant increase in the NAFLD markers intrahepatocellular lipid (IHCL) and alanine aminotransferase (ALT). However, when fructose-containing SSBs were consumed in matched isocaloric substitution for other carbohydrates, there was no effect on NAFLD markers [7].
It is unknown whether the effects seen for SSBs providing excess energy hold for other important food sources of fructose-containing sugars at different levels of energy control on NAFLD markers. There is evidence on other cardiometabolic outcomes that the harmful effects seen for SSBs do not hold for other food sources of fructose-containing sugars, whereas some (fruit) may even show benefit [8,9,10,11].
To investigate the role of food source and energy control in the prevention and management of NAFLD, we conducted a systematic review and meta-analysis of controlled trials to assess the certainty of evidence for the effect of different food sources of fructose-containing sugars at different energy control levels on intrahepatocellular lipid (IHCL), as well as alanine aminotransferase (ALT), and aspartate aminotransferase (AST).
2. Materials and Methods
We followed the Cochrane Handbook for Systematic Reviews of Interventions (v6.1) [12] for the conduct of our systematic review and meta-analysis and reported our results following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13] (Supplementary Table S1). The study protocol is registered at ClinicalTrials.gov (NCT02716870).
2.1. Data Sources and Search Strategy
We conducted a systematic search in MEDLINE, Embase, and the Cochrane Central Register of Controlled Studies databases through 7 January 2022. Supplementary Tables S2 and S3 present the search strategy based on the PICOTS framework, there were no language restrictions. Validated filters from the McMaster University Health Information Research Unit were applied to limit the database search to controlled studies only [14]. The searches were supplemented with manual searches of the reference list of included studies.
2.2. Study Selection
We included randomized and non-randomized controlled feeding trials in humans of all health backgrounds and ages, with intervention periods ≥7 days investigating the effect of orally consumed fructose-containing sugars from various food sources compared with control diets that were free of fructose or at least 5 g lower in fructose-containing sugars on at least one NAFLD marker (IHCL, ALT, or aspartate aminotransferase (AST)). We excluded studies of liquid meal replacement interventions and studies of interventions or comparators of rare sugars that contain fructose (e.g., isomaltulose, melezitose, or turanose) or were low calorie epimers of fructose (e.g., allulose, tagatose, sorbose). Reports were initially excluded based on review of their titles and abstracts by a single reviewer. Those reports that remained were then excluded based on review of the full text reports by at least 2 reviewers (DL, LC, SAC, FAY, AC, QL, XQ, AA) independently, leaving the final set of reports to be included in our syntheses. We prespecified four study designs based on energy control: (1) ‘substitution’ trials, in which energy from the food sources of fructose-containing sugars was substituted for other non-fructose-containing macronutrients under energy matched conditions; (2) ‘addition’ trials, in which excess energy from the food sources of fructose-containing sugars was added to the background diet compared to the same diet alone without the excess energy (with or without the use of non-nutritive/low-calorie sweeteners to match sweetness); (3) ‘subtraction’ trials, in which energy from the food sources of fructose-containing sugars was subtracted from background diets compared with the original background diets through displacement by water or low-calorie sweeteners or elimination altogether; and (4) ‘ad libitum’ trials, in which energy from the food sources of fructose-containing sugars was freely replaced (usually within reasonable limits, e.g., intake required to be between 75 and 125% of predicted daily energy requirements) with other non-fructose-containing macronutrients without any strict control of either the study foods or the background diets, allowing for free replacement of energy. In reports containing more than one eligible trial comparison, we included them as separate trial comparisons.
2.3. Data Extraction
At least two reviewers (DL, LC, SA-C) independently extracted data from eligible studies. Relevant information included food source of fructose-containing sugars, number of participants, setting, participant health status, study design, level of feeding control, randomization, comparator, fructose-containing sugars type, macronutrient profile of the diets, follow-up duration, energy balance, funding source and outcome data. Supplementary Table S4 shows the code definitions for the different food sources of fructose-containing sugars. Authors were contacted for missing outcome data when it was indicated that an NAFLD marker was measured but not reported. In the absence of outcome data and inability to obtain the original data from authors, values were extracted from figures using Plot Digitizer [15] where available.
2.4. Risk of Bias Assessment
Included studies were assessed for risk of bias independently and in duplicate by at least 2 reviewers (DL, LC, SA-C) using the Cochrane Risk of Bias Tool [12]. Assessment was done across six domains of bias (sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and other). Risk of bias for each domain was assessed as either “low” (proper methods taken to reduce bias), “high” (improper methods creating bias) or “unclear” (insufficient information provided). The “other” domain applied only to crossover trials, “high” risk of bias was given when there was no washout between interventions, otherwise the trial was rated as “low”. Reviewer discrepancies were resolved by consensus or arbitration by the senior author (JLS).
2.5. Outcomes
The primary outcome was IHCL. Secondary outcomes were ALT and AST. Mean differences (MDs) between the intervention and control arm and their standard errors (SEs) were extracted for each eligible trial comparison. If unavailable, they were derived from available data using published formulas [12]. Mean pairwise difference in change-from-baseline values were preferred over end values. When median data were provided, they were converted to mean data with corresponding variances using methods developed by Luo et al. (2018) [16] and Wan et al. (2014) [17]. When no variance data were available, the standard deviation (SD) was borrowed from a trial similar in size, participants and nature of intervention [18].
2.6. Data Syntheses and Analyses
We used STATA software, v16.1 (StataCorp, College Station, TX, USA) for all analyses. As our primary research question was to assess the effect of different food sources of fructose-containing sugars at different energy control levels, we performed separate pairwise meta-analyses for each of the four prespecified designs by energy control level (substitution, addition, subtraction and ad libitum trials) and assessed the interaction between food sources of fructose-containing sugars within each energy control level using the Cochrane Handbook’s recommended standard Q-test for subgroup differences (significance at p < 0.10) [19,20,21].
The principal effect measures were the mean pair-wise differences in change from baseline (or alternatively, end differences) between the food sources of fructose-containing sugars arm and the comparator arm (significance at p < 0.05). Data were analyzed using the generic inverse variance method with DerSimonian and Laird random-effects model [12,22]. A fixed effects model was used when only <5 trial comparisons were available [17]. Paired analyses were applied to all crossover trials with the use of a within-individual correlation coefficient between treatment of 0.5 [23,24,25]. Data were expressed as standardized mean differences (SMDs) for IHCL since the available data were reported in various units, and MDs for ALT and AST, with 95% confidence intervals (CIs). Standardized mean difference (SMD) was calculated for each study where the difference between two treatment and control means were divided by the standard deviation pooled across both groups [26]. A pooled SD from baseline reporting % liver fat was used to convert the IHCL SMD to % liver fat for clinical interpretation. To mitigate a unit-of-analysis error, when arms of trials with multiple intervention or control arms were used more than once, the corresponding sample size was divided by the number of times it was used for calculation of the standard error [12].
Heterogeneity was assessed by visual inspection of the forest plots and using the Cochran Q statistic and quantified using the I2 statistic [12]. We considered an I2 ≥ 50% and PQ < 0.10 as evidence of substantial heterogeneity [12]. Sources of heterogeneity were explored by sensitivity analyses, including influence analysis, altering pairwise comparison correlation coefficient and subgroup analyses. The influence analysis systematically removed each trial comparison from the meta-analysis with recalculation of the summary effect estimate. A trial whose removal explained the heterogeneity or changed the significance, direction, or magnitude (by more than the minimally important difference (MIDs) for IHCL (5% of the baseline in SMD units (0.26) due to variability in assessment measurement tools), ALT (2.85 U/L) [27], and AST (2.55 U/L) [27] of the effect was considered an influential trial. To determine whether the overall results were robust to the use of different correlation coefficients in crossover trials, we also conducted sensitivity analyses using correlation coefficients of 0.25 and 0.75. If ≥10 trials were available [20,28] we conduced subgroup analyses to explore sources of heterogeneity using meta-regression (significance at p < 0.05). A priori subgroup analyses were conducted by participant health status, age, randomization, energy balance, baseline outcome levels, fructose sugars type, comparator type, study design, follow-up, feeding control, fructose-containing sugars dose, and funding. Post-hoc subgroup analyses were conducted by sugars regulatory designation and type of imputation performed for deriving variances. Meta-regression analyses were used to assess the significance of each subgroup categorically and, when applicable, as a continuous exposure.
If ≥6 trial comparisons were available [29], then we assessed linear and non-linear (restricted cubic splines) dose–response relationships (significance at p < 0.05) using meta-regression. We also assessed non-linear dose–response threshold effects with three prespecified spline knots at public health thresholds of 5% [30,31], 10% [31,32], and 25% [33] total energy from fructose-containing sugars.
If ≥10 trials were available, then we assessed publication bias by visual inspection of contour-enhanced funnel plots and formal testing with Egger’s [34] and Begg’s [35] tests (significance at p < 0.10) [36]. If there was evidence of publication bias, then we adjusted for funnel plot asymmetry and assessed for small-study effects by imputing the missing trial data using the Duval and Tweedie trim-and-fill method [37].
2.7. Certainty of the Evidence
The certainty of the evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach and software (GRADEpro GDT, McMaster University and Evidence Prime Inc., Hamilton, ON, Canada) [38]. The assessments were conducted by at least two independent reviewers and discrepancies were resolved by consensus or arbitration by the senior author (JLS). The evidence was rated as high, moderate, low, or very low certainty. The included controlled trials were initially rated as high certainty by default and then downgraded or upgraded based on pre-specified criteria. Reasons for downgrading the evidence included risk of bias (assessed by the Cochrane Risk of Bias Tool [12]), inconsistency (substantial unexplained inter-study heterogeneity, I2 > 50% and p < 0.10), indirectness (presence of factors that limit the generalizability of the results), imprecision (the 95% CI for effect estimates overlap the MIDs for benefit or harm), and publication bias (significant evidence of small study effects). The reason for upgrading the evidence was presence of a significant dose–response gradient [39,40,41,42,43,44].
3. Results
3.1. Search Results
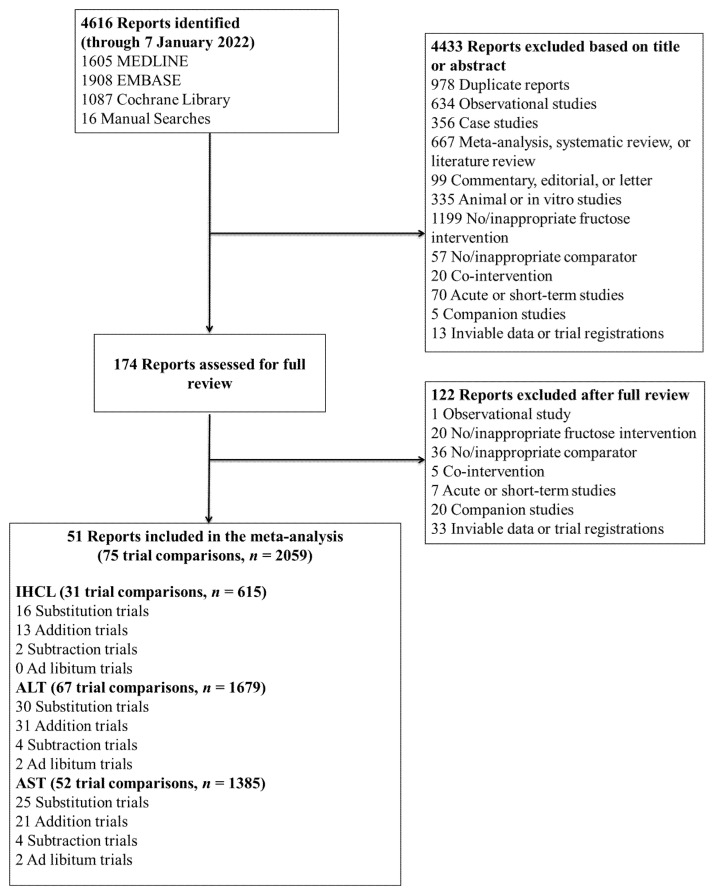
Figure 1 shows the flow of the literature. We retrieved 4616 reports from databases and manual searches, 4433 of which were excluded based on the title or abstract. Of the 174 reports reviewed in full text, 51 reports of controlled feeding trials (75 trial comparisons, n = 2059) met the eligibility criteria [45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94]. These trials included ten different food sources of fructose-containing sugars (SSBs; sweetened dairy alternative (soy); 100% fruit juice; fruit; dried fruit; mixed fruit forms; sweets and desserts; added nutritive (caloric) sweetener; honey; and mixed sources (with SSBs)) across four energy control levels: substitution (35 trial comparisons); addition (39 trial comparisons); subtraction (4 trial comparisons); and ad libitum (2 trial comparisons). The mixed sources food category includes those trials in which the intervention included more than one of the food sources (e.g., SSBs and fruits). For the present meta-analysis, all trials categorized as mixed sources included SSBs in the dietary prescription. Out of the ten authors who were contacted for missing NAFLD outcome data, five responded and provided unpublished data [47,49,69,70,81].
Figure 1.
Flow of the literature for the effect of different food sources of fructose-containing sugars and NAFLD risk markers. ALT = alanine aminotransferase; AST = aspartate aminotransferase; IHCL = intrahepatocellular lipid.
3.2. Trial Characteristics
Table 1 and Supplementary Table S5 show the trial characteristics. Trial sizes ranged from a median of 12 participants (range 5–15) in subtraction trials to 92 participants (range 92–92) in ad libitum trials. Participants were predominantly healthy mixed weight or overweight/obese (based on BMI criteria) with some participants who had NAFLD or diabetes. There were proportionally more males than females for subtraction and addition trials, but proportionately more females for subtraction and ad libitum. Most participants were younger adults with ages ranging from a median of 28.7 (range: 28–29) years in subtraction trials to 38 (range: 8–59) years in substitution trials. Most trials were conducted in an outpatient setting (50–100%) and performed in European countries. Most substitution and ad libitum trials were parallel (62% and 100%, respectively), whereas addition trials were mostly crossover (56%) and subtraction trials were equal in crossover and parallel design. Feeding control was mostly supplemented for substitution (66%), addition (87%), subtraction (50%), and all ad libitum (100%) trials. Most studies were randomized (50–91%), whereas ad libitum trials were non-randomized (100%). The dose of fructose-containing sugars ranged from a median of 12% (1–42%) in addition trials to 20% (1–42%) of total energy intake in substitution trials. The follow-up duration ranged from a median of four weeks (range 1–52 weeks) in substitution trials to 88 weeks (88–88) in ad libitum trials. The comparators for substitution trials were mostly glucose (12/35, 34%), diet alone for addition trials (22/39, 56%), and non-nutritive sweetener for all subtraction and ad libitum trials (4/4, 100% and 2/2, 100%, respectively). SSBs was the main food source for substitution (13/35, 37%), addition (20/39, 51%), and subtraction (4/4, 100%) trials, whereas mixed sources were used in all ad libitum trials (2/2, 100%). Most trials were funded by agency sources across for substitution and addition trials (government, not-for-profit health agency, or university sources) (54% and 69%, respectively), agency and industry sources for subtraction trials (50%), and no funding was reported for ad libitum trials.
Table 1.
Summary of trial characteristics a.
| Trial Characteristics | Substitution Trials |
Addition Trials |
Subtraction Trials |
Ad Libitum Trials |
|---|---|---|---|---|
| Trial comparisons (n) | 35 | 39 | 4 | 2 |
| Participants (median n ((range)) | 29 (7–102) | 23 (6–91) | 12 (5–15) | 92 (92–92) |
| Health status (n trials) | NW = 5; MW = 7; OW/OB = 17; MetS = 1; NAFLD = 5 | NW = 9; MW = 9; OW/OB = 4; DM2 = 3; NAFLD = 1; Other = 5 | MW = 1; OW/OB = 3 | MW = 2 |
| Sex ratio (% male:female) b | 62:38 | 61:39 | 25:75 | 35:65 |
| Age (years; median (range)) b | 38 (7.7–59) | 36.2 (21.7–58.9) | 28.7 (28.3–29.1) | 29 (29–29) |
| Age category ratio (%; adult:children:mixed) b | 86:14:0 | 100:0:0 | 100:0:0 | 100:0:0 |
| Country (n trials) | 1 Brazil; 1 Denmark; 5 Finland; 2 Germany; 1 Greece; 2 Iran; 1 Sweden; 4 Switzerland; 7 UK; 8 USA; 1 Netherlands | 1 China; 8 Denmark; 1 Germany; 2 Iran; 4 Malaysia; 2 Netherlands; 1 Pakistan; 1 Sweden; 8 Switzerland; 1 UK; 2 USA | 2 Switzerland; 2 USA | 2 Finland |
| Setting ratio (%; inpatients:outpatients:inpatients/outpatients) | 9:88:3 | 8:87:5 | 50:50:0 | 0:100:0 |
| Baseline IHCL (% liver fat; median (range)) c | 5.7 (2.6–16.5) | 4.1 (1.6–9.7) | 2.9 (2.6–3.3) | NR |
| Baseline ALT (U/L; median (range)) d | 23 (5.2–116.6) | 25 (16.4–46.9) | 28.5 (21.6–39.7) | NR |
| Baseline AST (U/L; median (range)) e | 25 (7.9–68.8) | 26 (18–37) | 24.7 (21.6–27.9) | NR |
| Trial design ratio (%; crossover:parallel) | 37:62 | 56:44 | 50:50 | 0:100 |
| Feeding control ratio (%; met:sup:DA:met/sup) | 22:66:11:3 | 5:87:0:8 | 50:50:0:0 | 0:100:0:0 |
| Randomization ratio (%; yes:no:partial) f | 91:9:0 | 85:15:0 | 50:50:0 | 0:0:100 |
| Fructose-containing sugar dose (% of total energy intake; median (range)) | 20 (1–42) | 12.2 (1.2–35) | 16.3 (15–22.5) | 14.4 (14–14.7) |
| Follow-up duration (median n (range) of weeks) | 4 (1–52) | 1 (1–24) | 7 (1.7–12) | 88 (88–88) |
| Funding sources (%; A:I:A+I:NR) | 54:40:0:6 | 69:3:26:3 | 50:0:50:0 | 0:0:0:100 |
| Fructose-containing sugar type (n trials) | Fructose = 11; fruit = 8; HFCS = 2; sucrose = 14 | Fructose = 13; sucrose = 7; honey = 5; HFCS = 1; fruit = 13 | Sucrose = 4 | Fructose = 1; sucrose = 1 |
| Sugar regulatory designation (n trials) | Naturally occurring = 7; added = 18; mixed = 10 | Naturally occurring = 13; added = 26 | Added = 2; mixed = 2 | Mixed = 2 |
| Comparator (n trials) | NNS = 1; fat = 8; glucose = 12; lactose = 2; starch = 5; mixed comparator = 9 | NNS = 6; diet alone = 22; fat = 1; water = 3; other = 7 | NNS = 4 | NNS = 2 |
| Food sources of fructose-containing sugars (n trials) | SSB = 13; sweetened dairy alternative (soy) = 1; 100% fruit juice = 2; fruit = 2; dried fruit = 3; honey = 1; sweets and desserts = 3; mixed sources (with SSBs) = 10 | SSB = 20; 100% fruit juice = 7; fruit = 4; dried fruit = 2; honey = 5; sweets and desserts = 1 | SSB = 2; mixed sources (with SSBs) = 2 | Mixed sources (with SSBs) = 2 |
A = agency; A+I = agency and industry; ALT = alanine aminotransferase; AST = aspartate aminotransferase; Pre-CVD = pre-cardiovascular disease; DA = dietary advice; DM2 = type-2 diabetes mellitus; HIV = human immunodeficiency virus; I = industry; IHCL = intrahepatocellular lipid; met = metabolically controlled; MetS = metabolic syndrome; MW = mixed weight; NAFLD = non-alcoholic fatty liver disease; No = number; NR = not reported; NW = normal weight; OB = obese; ODM2 = overweight or obese type-2 diabetes mellitus; OW = overweight; SSBs = sugar-sweetened beverages; sup = supplemented; UK = United Kingdom; USA = United States of America. a Values are rounded to nearest whole number except for baseline NAFLD outcomes. b Based on trials which report data. c Based on trial comparisons that reported baseline data (n = 21 trials missing baseline IHCL substitution trials and n = 20 trials missing baseline IHCL addition trials). Baseline % liver fat was calculated by multiplying the baseline standardized mean difference of IHCL and baseline standard deviation of all trial comparisons that reported % liver fat. d Based on trial comparisons that reported baseline data (n = 9 trials missing baseline ALT substitution trials; n = 14 trials missing for baseline ALT addition trials; and n = 2 trials missing for baseline ALT ad libitum trials). e Based on trial comparisons that reported baseline data (n = 13 trials missing baseline AST substitution trials; n = 19 trials missing baseline AST addition trials; and n = 2 trials missing for baseline ALT ad libitum trials). f Partial randomization was assigned to a trial comparison which randomized only selected participants.
3.3. Risk of Bias
Supplementary Figures S1–S11 show a summary of the risk of bias assessments of the included trials. Most trials were assessed as having unclear risk of bias in random sequence generation (41/75, 55%), allocation concealment (46/75, 61%), and incomplete outcome data domains (47/75, 63%) due to poor reporting, while most were low risk of bias in blinding (47/75, 63%), selective outcome reporting (47/75, 63%), and other (carry-over effects) risk of bias (62/75, 83% domains. Few studies were assessed as having high risk of bias, for random sequence generation (12/75, 12%), allocation concealment (15/75, 20%), blinding of participants and personnel (3/75, 4%), incomplete outcome data (0/75, 0%), selective outcome reporting (2/75, 3%), and other (carry-over effects) (13/75, 17%) risk of bias domains, respectively. Thus, there was no overall serious risk of bias in any trial comparisons except for ad libitum trial comparisons which had 100% (both two trial comparisons) high risk of bias rating for sequence generation and allocation concealment.
3.4. Primary Outcome
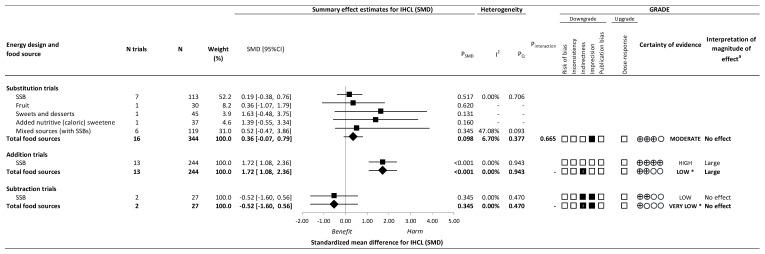
Figure 2 and Supplementary Figures S12–S14 present the effect of different food sources of fructose-containing sugars on IHCL at four levels of energy control. Total fructose-containing sugars resulted in a large increase in IHCL for addition trials (13 trials; SMD: 1.72; 95% CI: 1.08, 2.36, PSMD < 0.001; no heterogeneity, I2 = 0.00%, PQ = 0.943), whereas there was no effect in substitution trials (16 trials; SMD: 0.36; 95% CI: −0.07, 0.79; PSMD = 0.098; no substantial heterogeneity, I2 = 6.70%, PQ = 0.377) or subtraction trials (2 trials; SMD: −0.52; 95% CI: −1.60, 0.56; PSMD = 0.345; no heterogeneity, I2 = 0.00%, PQ = 0.470). No ad libitum trials were available for IHCL.
Figure 2.
Summary plot for the effect of important food sources of fructose-containing sugars on intrahepatocellular lipid (IHCL). Data are weighted standardized mean differences (95% confidence intervals) for summary effects of individual food sources and total food sources on IHCL. Analyses conducted by generic, inverse variance random effects models (at least five trials available) or fixed effects models (fewer than five trials available). Between-study heterogeneity was assessed by the Cochrane Q statistic, where PQ < 0.100 is considered statistically significant, and quantified by the I2 statistic, where I2 ≥ 50% is considered evidence of substantial heterogeneity. The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) of randomized controlled trials are rated as “High” certainty of evidence and can be downgraded by five domains and upgraded by one domain. The white squares represent no downgrades, while filled black squares indicate a single downgrade or upgrades for each outcome, and the black square with a white “2” indicates a double downgrade for each outcome. CI = confidence interval; GRADE = Grading of Recommendations, Assessment, Development and Evaluation; IHCL = intrahepatocellular lipid; N = number; SMD = standardized mean difference; SSB = sugar-sweetened beverage. a For the interpretation of the magnitude, we used the MIDs to assess the importance of magnitude of our point estimate using the effect size categories according to new GRADE guidance. * Where there was a significant interaction by food source in substitution and addition trials and SSBs and mixed sources were the sole food sources in subtraction and ad libitum trials, we performed the GRADE analysis for each individual food source. To convert SMD to % liver fat, multiply the SMD by the baseline pooled standard deviation, 0.71%.
There was evidence of influence by food source on IHCL in addition and subtraction trials. Although we were unable to assess interaction by food source at these levels of energy control, the large increase in IHCL in the addition trials and no effect in IHCL in the subtraction trials was specific to a single food source: SSBs. There was no evidence of interaction by food source in the substitution trials (p = 0.665).
3.5. Secondary Outcomes
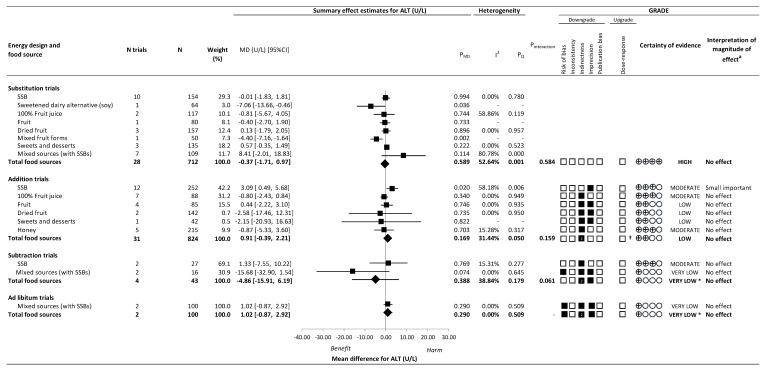
Figure 3 and Supplementary Figures S15–S18 present the effect of different food sources of fructose-containing sugars on ALT. There was no effect of total fructose-containing sugars on ALT in substitution trials (28 trials; MD: −0.37 U/L; 95% CI: −1.71, 0.97; PMD = 0.589; substantial heterogeneity, I2 = 52.64%, PQ = 0.001), addition trials (31 trials; MD: 0.91 U/L; 95% CI: −0.39, 2.21; PMD = 0.169; no substantial heterogeneity, I2 = 31.44%, PQ = 0.050), subtraction trials (4 trials; MD: −4.86 U/L; 95% CI: −15.91, 6.19; PMD = 0.388; no substantial heterogeneity, I2 = 38.84%, PQ = 0.179), or ad libitum trials (2 trials; MD: 1.02 U/L; 95% CI: −0.87, 2.92; PMD = 0.290; no heterogeneity, I2 = 0.00%, PQ = 0.509).
Figure 3.
Summary plot for the effect of important food sources of fructose-containing sugars on alanine aminotransferase (ALT). Data are weighted mean differences (95% confidence intervals) for summary effects of individual food sources and total food sources on ALT. Analyses conducted by generic, inverse variance random effects models (at least five trials available) or fixed effects models (fewer than five trials available). Between-study heterogeneity was assessed by the Cochrane Q statistic, where PQ < 0.100 is considered statistically significant, and quantified by the I2 statistic, where I2 ≥ 50% is considered evidence of substantial heterogeneity. The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) of randomized controlled trials are rated as “High” certainty of evidence and can be downgraded by five domains and upgraded by one domain. The white squares represent no downgrades, while filled black squares indicate a single downgrade or upgrades for each outcome, and the black square with a white “2” indicates a double downgrade for each outcome. ALT = alanine aminotransferase; CI = confidence interval; GRADE = Grading of Recommendations, Assessment, Development and Evaluation; MD = mean difference; N = number; SMD = standardized mean difference; SSB = sugar-sweetened beverage. a For the interpretation of the magnitude, we used the MIDs to assess the importance of magnitude of our point estimate using the effect size categories according to new GRADE guidance. † Not upgraded for dose–response (see Table S7 for details). * Where there was a significant interaction by food source in substitution and addition trials and SSBs and mixed sources were the sole food sources in subtraction and ad libitum trials, we performed the GRADE analysis for each individual food source. To convert U/L to ukat/L, multiply U/L by 0.0167.
In addition trials, although the test for interaction by food sources was not significant (p = 0.159), we considered there to be an influence by food source on ALT as SSBs contributed the majority (42.4%) of the weight in the overall analysis. SSBs (12 trials; MD: 3.09 U/L; 95% CI: 0.49, 5.68 U/L; PMD = 0.020; substantial heterogeneity, I2 = 58.18%, PQ = 0.006) resulted in an increase in ALT, but other food sources were not significant and showed variable directions of effect estimates. There was evidence of influence by food source on ALT in subtraction trials (p = 0.061), although neither food source (SSBs nor mixed sources [with SSBs]) showed an effect on ALT. Even though we were unable to assess an interaction by food source in ad libitum trials, the non-significant effect was specific to a sole food source: mixed sources (with SSBs). There was no evidence of interaction by food source in substitution trials (p = 0.584).
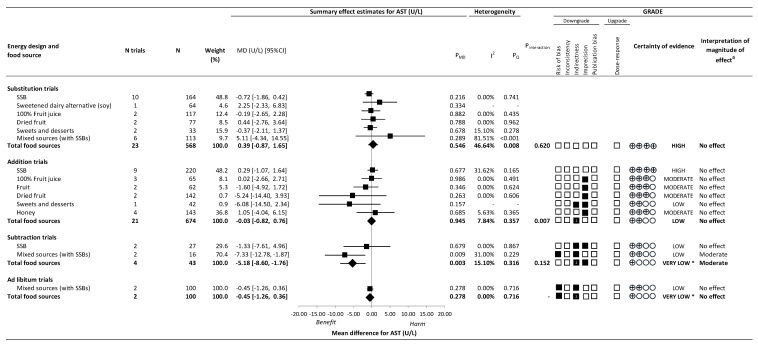
Figure 4 and Supplementary Figures S19–S22 present the effect of different food sources of fructose-containing sugars on AST.
Figure 4.
Summary plot for the effect of important food sources of fructose-containing sugars on aspartate aminotransferase (AST). Data are weighted mean differences (95% confidence intervals) for summary effects of individual food sources and total food sources on ALT. Analyses conducted by generic, inverse variance random effects models (at least five trials available) or fixed effects models (fewer than five trials available). Between-study heterogeneity was assessed by the Cochrane Q statistic, where PQ < 0.100 is considered statistically significant, and quantified by the I2 statistic, where I2 ≥ 50% is considered evidence of substantial heterogeneity. The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) of randomized controlled trials are rated as “High” certainty of evidence and can be downgraded by five domains and upgraded by one domain. The white squares represent no downgrades, while filled black squares indicate a single downgrade or upgrades for each outcome, and the black square with a white “2” indicates a double downgrade for each outcome. AST = aspartate aminotransferase; CI = confidence interval; GRADE = Grading of Recommendations, Assessment, Development and Evaluation; MD = mean difference; N = number; SMD = standardized mean difference; SSB = sugar-sweetened beverage. a For the interpretation of the magnitude, we used the MIDs to assess the importance of magnitude of our point estimate using the effect size categories according to new GRADE guidance. * Where there was a significant interaction by food source in substitution and addition trials and SSBs and mixed sources were the sole food sources in subtraction and ad libitum trials, we performed the GRADE analysis for each individual food source. To convert U/L to ukat/L, multiply U/L by 0.0167.
Total fructose-containing sugars resulted in a decrease in AST for subtraction trials (4 trials; MD: −5.18 U/L; 95% CI: −8.60, −1.76; PMD = 0.003; no substantial heterogeneity I2 = 15.10%, PQ = 0.316). There was no significant effect of total fructose-containing sugars independent of food source on AST in substitution (23 trials; MD: 0.39 U/L; 95% CI: −0.87, 1.65; PMD = 0.546; no substantial heterogeneity, I2 = 46.64%, PQ = 0.008), addition (21 trials; MD: −0.03 U/L; 95% CI: −0.82, 0.76; PMD = 0.945; no substantial heterogeneity I2 = 7.84%, PQ = 0.357), or ad libitum (2 trials; MD: −0.45 U/L; 95% CI: −1.26, 0.36; PMD = 0.278; no heterogeneity I2 = 0.00%, PQ = 0.716) trials.
There was evidence of interaction by food source on AST in addition trials (p = 0.007), although none of the food sources showed an effect on AST. We considered there to be evidence of influence by food source in subtraction trials was mixed sources (with SSBs) showed significant reduction in AST (2 trials; MD: −7.33 U/L; 95% CI: −12.78, −1.87 U/L; PMD = 0.009; no substantial heterogeneity, I2 = 31.00%, PQ = 0.229) while SSBs alone did not. In ad libitum trials, the non-significant effect was specific to a sole food source: mixed sources (with SSBs). There was no significant effect of interaction by food source in the substitution trials (p = 0.620).
3.6. Sensitivity Analyses
Supplementary Figures S23–S33 present the influence analyses for total fructose-containing sugars at the four levels of energy control. The systematic removal of a single trial provided partial explanation of the evidence of substantial heterogeneity for ALT in substitution trials [56,78,81].
Supplementary Figures S34–S47 present the influence analyses for individual food sources for those analyses that showed evidence of an interaction or influence by food source. Removal of a single trial resulted in a change in direction of the effect of ALT in subtraction trials [48] and AST in substitution [68] and addition trials [68].
Supplementary Table S6 shows sensitivity analyses in which different correlation coefficients (0.25 and 0.75) were used for paired analyses of crossover trials. The use of these different correlation coefficients did not alter the direction, magnitude, or significance of the effect or evidence for heterogeneity for any outcomes across food sources and levels of energy control. The three exceptions where the use of a correlation of 0.75 led to substantial heterogeneity for the effect of mixed sources (with SSBs) on SSBs on AST addition trials (9 trials, I2 = 51.46%, PQ = 0.036).
Supplementary Figures S48–S61 present the subgroup analyses for all outcomes except subtraction and ad libitum trials as <10 trial comparisons were available for analyses. For the primary outcome IHCL, there was no evidence of significant effect modification by any subgroup category. Secondary outcomes ALT and AST showed significant effect modification in at least one of the following: health status, age, baseline outcome, randomization, energy balance, fructose sugars type, comparator, study design, follow-up, feeding control, dose, regulatory designation, funding, type of mean difference, sugar form matrix, data source, sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome data, and other carry-over effects. Subgroup analyses by addition ALT trials for SSBs showed no significant effect modification by any subgroup category except for follow-up, feeding control, and blinding. No subgroup analyses were performed for any other individual food sources where there was a significant interaction or influence by food source or when SSBs or mixed sources were the sole food sources as <10 trials were available in these analyses.
3.7. Dose–Response Analyses
Supplementary Figures S62–S88 present linear and non-linear dose–response analyses. There was no dose response for the effect of total fructose-containing sugars on IHCL or AST in substitution and addition trials. A significant positive linear dose–response gradient was found for the effect of total food sources of fructose-containing sugars on ALT in addition trials (coeflinear = 0.153 U/L (0.035, 0.271) per 1%E, Plinear = 0.011). No significant dose response was detected for the effect of any food source which was assessed (≥6 trial comparisons). Dose–response analyses were not performed on subtraction and ad libitum trials (<6 trials).
3.8. Publication Bias
Supplementary Figures S89–S99 present the publication bias assessments for all outcomes. There was evidence of funnel plot asymmetry and small study effects for IHCL, ALT and AST in substitution and addition trials (Begg’s test p < 0.05; Egger’s test p < 0.05). Adjustment for funnel plot asymmetry with the imputation of missing trials by the Duval and Tweedie trim-and-fill method, however, did not alter the direction, magnitude, or significance of the effect, suggesting that there was no meaningful influence of publication bias on the results. No evidence of publication bias was detected in addition ALT trials by SSBs. Publication bias could not be assessed in subtraction or ad libitum comparisons, or for food sources where there was significant interaction by food source, as there were <10 trials available for these analyses.
3.9. GRADE Assessment
Figure 2, Figure 3 and Figure 4 and Supplementary Tables S7 and S8 present the GRADE assessments. The certainty of evidence for the effect of total fructose-containing sugars on IHCL was moderate in substitution trials, low in addition trials, and very low in subtraction trials, owing to double downgrades for indirectness in the addition and subtraction trials and single downgrades for imprecision in the substitution and subtraction trials. The certainty of evidence for the effect of total fructose-containing sugars on secondary outcomes was high for the lack of effect on ALT and AST in the substitution trials and low to very low for the lack of effect on ALT and AST across the other levels of energy control, with the exception of the reduction on AST in subtraction trials, owing to double downgrades for indirectness and a single downgrade for risk of bias or imprecision.
Because SSBs were the sole food source in addition and subtraction trials for IHCL, and we detected an interaction or influence by food source in the addition, subtraction, and ad libitum trials for ALT and AST, we assessed the certainty of evidence for each of the food sources in these analyses. The certainty of evidence was high for the effect of SSBs (large increase) on IHCL in the absence of any downgrades, and moderate for the effect of SSBs (small important increase) on ALT, owing to a single downgrade for imprecision in addition trials; and low for the effect of the removal of mixed sources (with SSBs) (moderate reduction) on AST owing to downgrades for serious risk of bias and indirectness in subtraction trials. For all other food sources, the certainty of evidence varied from moderate to very low owing to downgrades for risk of bias, indirectness, and/or imprecision.
4. Discussion
We conducted a systematic review and meta-analysis of 51 studies (75 trial comparisons) in 2059 predominantly healthy mixed weight or overweight/obese younger adult participants that assessed the effect of 10 different food sources of fructose-containing food sources (sugar-sweetened beverages [SSBs]; sweetened dairy alternative; 100% fruit juice; fruit; dried fruit; mixed fruit sources; sweets and desserts; added nutritive sweetener; honey; and mixed sources [with SSBs]) with a median dose of 12% (range 1% to 35%) to 20% (range 1% to 42%) of total energy intake across four different levels of energy control over a median follow-up of 1 to 88 weeks. We showed that total fructose-containing sugars led to a clinically meaningful, moderate relative increase of 10% from baseline IHCL levels in IHCL in addition trials, whereas there was a moderate reduction of 19% in AST in subtraction trials. Total fructose-containing sugars had no other effects. There was evidence of influenced by food source in these analyses. SSBs providing 27% to 30% excess energy led to a moderate increase in IHCL of 10% (as the sole food source) and a small important increase in ALT of 11% in addition trials, whereas the removal of energy from mixed sources (with SSBs) resulted in a moderate reduction of 28% in AST in subtraction trials.
4.1. Findings in Relation to the Literature
Our findings are in agreement with a previous systematic review and meta-analysis by Chiu et al. 2014 [7] in which addition studies of fructose-containing sugars, in the form of SSBs, were found to harmfully affect IHCL and ALT levels. Our results show harm for IHCL which relates to ~0.7% liver fat as well as a significant harmful increase in ALT in SSB addition trials. Chiu et al. [7] also demonstrated that in substitution trials, where energy is matched, fructose-containing sugars from SSBs did not significantly change IHCL and ALT, which corresponds with our findings. Another systematic review and meta-analysis by Chung et al. 2014 [95] found a non-significant difference on ALT and AST in addition trials comparing fructose and glucose diets. We also did not find a significant effect on AST in addition trials of SSBs, and this may be due to the fewer number of studies available (9 vs. 13 and 12 in the IHCL and ALT analyses, respectively).
Our data are also congruent with several systematic review and meta-analyses of prospective cohort studies that investigated the effects of elevated fructose-containing SSB consumption on NAFLD risk. A meta-analysis [96] of seven observational studies (six cross-sectional and one cohort study, n = 4639) found that compared with those who did not consume SSB, up to one serving per day was associated with a 53% increased risk of NAFLD (risk ratio 1.53 (95% CI: 1.34, 1.75). Similarly, a systematic review and meta-analysis of four cross-sectional studies (n = 6326) found that daily consumption of SSBs was associated with a 40% increased risk in NAFLD compared to the group not consuming any SSBs [97]. In contrast, an observational study in older Finnish adults demonstrated an inverse association between NAFLD risk and fructose intake [98], where the main food source of fructose-containing sugars was consumed in the form of fruit rather than SSBs. We found no significant effect of fruit on any NAFLD markers, though our confidence in these effect estimates is limited due to indirectness and imprecision, and only included data from one to three small trials.
4.2. Potential Mechanisms
Supplementary Table S9 shows several mechanisms that have been proposed to explain the effects of fructose-containing sugars and NAFLD markers. Briefly, the consumption of SSBs as excess calories may stimulate disruptions in hepatic fatty acid metabolism, the various effects shown could be due to the different food matrices/forms of food sources of fructose-containing sugars, and subtraction trials resulting in no effect on NAFLD outcomes could be due to energy compensation.
4.3. Strengths and Limitations
Our systematic review and meta-analysis has several strengths. First, the literature search and selection methods were comprehensive and reproducible. Second, the synthesized data were derived from all the available evidence from controlled interventions, providing a large body of evidence (51 studies, 75 trials comparisons, n = 2059), which minimizes bias and increases precision. Third, our approach included a comprehensive exploration of possible sources of heterogeneity. Fourth, none of our analysis had substantial unexplained heterogeneity. Fifth, we evaluated the shape and strength of the dose–response relationships. Finally, the overall certainty of the evidence was assessed by GRADE.
There were also several limitations. First, there was evidence of serious risk of bias in the ad libitum trials of ALT and AST. The two available ad libitum trials were neither randomized nor concealed the allocation of treatment groups to participants, thereby increasing the risk of bias in the measured effects. Second, there was evidence of very serious indirectness in several analyses. There was significant interaction or influence by food source for ALT and AST in addition trials and thus we double downgraded total fructose-containing sugars in these analyses for indirectness. Another source of indirectness was the limited number of food sources of fructose-containing sugars available for some analyses. SSBs and/or mixed sources (with SSBs) was the sole food source in addition and subtraction trials of IHCL and ad libitum trials for ALT and AST. The lack of alternate food sources limits our ability to explore interactions by food source and is thus unclear whether these effects hold for other important fructose-containing food sources. In some analyses with few trials, we downgraded for indirectness due to limited generalizability. Another source of indirectness may have been that we were unable to differentiate between NAFLD and non-alcoholic steatohepatitis (NASH) as the effects of fructose-containing sugars could differ based on NAFLD status. All obtained studies with NAFLD participants did not diagnose for NASH except Vos et al. 2009 [83], where seven pediatric participants were confirmed to have NASH from a liver biopsy and there was no effect between the NASH and NAFLD participants. Finally, there was evidence of serious imprecision in the effect of total fructose-containing sugars on IHCL in the substitution and subtraction trials with the 95% confidence intervals crossing the prespecified minimally important differences on either side of unity. Thus, we cannot rule out clinically important benefit and/or harm for these NAFLD outcomes.
Weighing the strengths and limitations, the certainty of the evidence was high and moderate for the increasing effect of SSBs providing excess energy on IHCL and ALT, respectively, in addition trials, low for the decreasing effect of the removal of energy from mixed sources (with SSBs) on AST, and generally low to moderate for all other comparisons.
4.4. Implications
Our findings have implications for public health and clinical practice. General dietary guidelines and clinical practice guidelines for obesity, diabetes, and cardiovascular disease have shifted away from a focus on single nutrients to a focus on foods and dietary patterns [99,100,101,102]. Clinical practice guidelines for NAFLD have also shifted in this direction recommending a Mediterranean dietary pattern, although there is still a recommendation to avoid fructose intake irrespective of the food source [6]. Understanding the differential effects of food sources of fructose-containing sugars on NALFD markers aligns with this approach to nutrition and health in the prevention and management of NAFLD. The evidence supports reducing the consumption of SSBs as a source of excess energy, while it does not support avoidance of food sources such as 100% fruit juice, dried fruit, mixed fruit, or plant-based dairy alternative, all of which are part of one or more therapeutic dietary pattens such as Mediterranean, Dietary Approaches to Stop Hypertension (DASH), vegetarian, Portfolio, and low-glycemic index dietary patterns [102].
5. Conclusions
In conclusion, the effect of fructose-containing sugars on markers of NAFLD appears mediated by both energy control and food source in predominantly mixed weight or overweight/obese younger adults. The evidence provides a good indication that SSBs providing excess energy at high doses lead to large increases liver fat and small important increases in ALT, whereas there is a less of an indication that the removal of energy from mixed sources (with SSBs) results in moderate reductions in AST. Varying uncertainty remains for the lack of effect of other important food sources of fructose-containing sugars such as fruit, 100% fruit juice, dried fruit, mixed fruit sources, sweetened dairy alternatives, sweets and desserts, and mixed sources at different levels of energy control. The main sources of uncertainty in the evidence are imprecision and indirectness (most of the interventions were limited to SSBs). There is a need for more large high-quality randomized trials that assess a broader variety of food sources of fructose-containing sugars (e.g., fruit, dairy and grain-based products) should be explored in future studies at different levels of energy control to address these issues. In the meantime, our findings suggest policy and guideline makers should consider the role of energy and food matrix in recommendations for sugars in NAFLD prevention and management.
Acknowledgments
Aspects of this work were presented at The St. Michael’s Hospital Research Training Centre’s 2019 Trainee Research Day, Toronto, ON, Canada, The Canadian Nutrition Society 2021 Virtual Thematic Conference, The American Society of Nutrition 2021 Live Online Conference, and the International Symposium on Diabetes and Nutrition 2021 Virtual Conference.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14142846/s1 [103,104,105].
Author Contributions
Research design (project conception, development of overall research plan, and study oversight), J.L.S., L.C., V.L.C., S.B.M., V.S.M., A.E.-S., R.J.d.S., T.M.S.W., L.A.L., C.W.C.K. and D.J.A.J.; research conduct (hands-on conduct of the experiments and data collection), D.L., L.C., S.A.-C., F.A.-Y., A.C., Q.L., X.Q. and A.A.; data analysis and statistical analysis, D.L., L.C., T.A.K., A.Z. and F.A.-Y.; writing—review and editing, D.L., L.C. and J.L.S.; study supervision, D.J.A.J. and J.L.S.; D.L., L.C. and J.L.S. had primary responsibility for the final content and take responsibility for the integrity of the data and the accuracy of the data analysis. All the authors contributed to the critical revision of the manuscript for important intellectual content. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethics approval not required.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data available upon request.
Conflicts of Interest
Declaration of interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf. DL reports receiving a stipend from University of Toronto Department of Nutritional Sciences Graduate Student Fellowship, University of Toronto Fellowship in Nutritional Sciences, University of Toronto Supervisor’s Research Grant—Early Researcher Awards, and Dairy Farmers of Canada Graduate Student Fellowships; a scholarship from St. Michael’s Hospital Research Training Centre, and a University of Toronto School of Graduate Studies Conference Grant. LC was a Mitacs-Elevate post-doctoral fellow jointly funded by the Government of Canada and the Canadian Sugar Institute. She was previously employed as a casual clinical coordinator at INQUIS Clinical Research, Ltd. (formerly Glycemic Index Laboratories, Inc.), a contract research organization. SA-C has received funding from CIHR Canadian Graduate Scholarship-Master’s and Doctoral, the Loblaw Food as Medicine Award, and the Ontario Graduate Scholarship. TAK has received research support from the Canadian Institutes of Health Research (CIHR), the International Life Science Institute (ILSI), and National Honey Board. He has been an invited speaker at the Calorie Control Council Annual meeting for which he has received an honorarium. He was funded by a Toronto 3D Postdoctoral Fellowship Award. AZ is a part-time Research Associate at INQUIS Clinical Research, Ltd., a contract research organization, and has received funding from a BBDC Postdoctoral Fellowship. AC and AA have received funding from a Toronto 3D MSc Scholarship award. FA-Y is a part-time Research Assistant at INQUIS Clinical Research, Ltd., a contract research organization. VSM has received funding from the Canada Research Chairs Program; Connaught New Researcher Award, University of Toronto; The Joannah & Brian Lawson Centre for Child Nutrition, University of Toronto; Temerty Faculty of Medicine Pathway Grant, University of Toronto; Canada Foundation for Innovation; Ontario Research Fund, and reports personal fees from the City and County of San Francisco and from Kaplan Fox & Kilsheimer, LLP, outside the submitted work. RJdS has served as an external resource person to the World Health Organization’s Nutrition Guidelines Advisory Group on trans fats, saturated fats, and polyunsaturated fats. The WHO paid for his travel and accommodation to attend meetings from 2012–2017 to present and discuss this work. He has presented updates of this work to the WHO in 2022. He has also done contract research for the Canadian Institutes of Health Research’s Institute of Nutrition, Metabolism, and Diabetes, Health Canada, and the World Health Organization for which he received remuneration. He has received speaker’s fees from the University of Toronto, and McMaster Children’s Hospital. He has held grants from the Canadian Institutes of Health Research, Canadian Foundation for Dietetic Research, Population Health Research Institute, and Hamilton Health Sciences Corporation as a principal investigator, and is a co-investigator on several funded team grants from the Canadian Institutes of Health Research. He has served as an independent director of the Helderleigh Foundation (Canada). He serves as a member of the Nutrition Science Advisory Committee to Health Canada (Government of Canada), and a co-opted member of the Scientific Advisory Committee on Nutrition (SACN) Subgroup on the Framework for the Evaluation of Evidence (Public Health England).TMSW was previously part owner, and now is an employee of INQUIS and received an honorarium from Springer/Nature for being an Associate Editor of the European Journal of Clinical Nutrition. CWCK has received grants or research support from the Advanced Food Materials Network, Agriculture and Agri-Foods Canada, Almond Board of California, American Pistachio Growers, Barilla, Calorie Control Council, Canadian Institutes of Health Research, Canola Council of Canada, International Nut and Dried Fruit Council, International Tree Nut Council Research and Education Foundation, Loblaw Brands, Pulse Canada, Saskatchewan Pulse Growers and Unilever; has received in-kind research support from the Almond Board of California, American Peanut Council, Barilla, California Walnut Commission, Kellogg Canada, Loblaw Companies, Quaker (PepsiCo), Primo, Unico, Unilever, WhiteWave Foods; has received travel support or honorariums from the American Peanut Council, American Pistachio Growers, Barilla, California Walnut Commission, Canola Council of Canada, General Mills, International Nut and Dried Fruit Council, International Pasta Organization, Loblaw Brands Ltd., Nutrition Foundation of Italy, Oldways Preservation Trust, Paramount Farms, Peanut Institute, Pulse Canada, Sabra Dipping, Saskatchewan Pulse Growers, Sun-Maid, Tate & Lyle, Unilever and White Wave Foods; has served on the scientific advisory board for the International Tree Nut Council, International Pasta Organization, Lantmannen, McCormick Science Institute, Oldways Preservation Trust, Paramount Farms and Pulse Canada; is a member of the International Carbohydrate Quality Consortium, executive board member of the Diabetes and Nutrition Study Group of the European Association for the Study of Diabetes; is on the Clinical Practice Guidelines Expert Committee for Nutrition Therapy of the European Association for the Study of Diabetes; and is a director of the Toronto 3D Knowledge Synthesis and Clinical Trials Foundation. DJAJ has received research grants from Saskatchewan & Alberta Pulse Growers Associations, the Agricultural Bioproducts Innovation Program through the Pulse Research Network, the Advanced Foods and Material Network, Loblaw Companies Ltd., Unilever Canada and Netherlands, Barilla, the Almond Board of California, Agriculture and Agri-food Canada, Pulse Canada, Kellogg’s Company, Canada, Quaker Oats, Canada, Procter & Gamble Technical Centre Ltd., Bayer Consumer Care, Springfield, NJ, Pepsi/Quaker, International Nut & Dried Fruit Council (INC), Soy Foods Association of North America, the Coca-Cola Company (investigator initiated, unrestricted grant), Solae, Haine Celestial, the Sanitarium Company, Orafti, the International Tree Nut Council Nutrition Research and Education Foundation, the Peanut Institute, Soy Nutrition Institute (SNI), the Canola and Flax Councils of Canada, the Calorie Control Council, the Canadian Institutes of Health Research (CIHR), the Canada Foundation for Innovation (CFI)and the Ontario Research Fund (ORF). He has received in-kind supplies for trials as a research support from the Almond board of California, Walnut Council of California, American Peanut Council, Barilla, Unilever, Unico, Primo, Loblaw Companies, Quaker (Pepsico), Pristine Gourmet, Bunge Limited, Kellogg Canada, WhiteWave Foods. He has been on the speaker’s panel, served on the scientific advisory board and/or received travel support and/or honoraria from Nutritional Fundamentals for Health (NFH)-Nutramedica, Saint Barnabas Medical Center, The University of Chicago, 2020 China Glycemic Index (GI) International Conference, Atlantic Pain Conference, Academy of Life Long Learning, the Almond Board of California, Canadian Agriculture Policy Institute, Loblaw Companies Ltd., the Griffin Hospital (for the development of the NuVal scoring system), the Coca-Cola Company, Epicure, Danone, Diet Quality Photo Navigation (DQPN), Better Therapeutics (FareWell), Verywell, True Health Initiative (THI), Heali AI Corp, Institute of Food Technologists (IFT), Soy Nutrition Institute (SNI), Herbalife Nutrition Institute (HNI), Saskatchewan & Alberta Pulse Growers Associations, Sanitarium Company, Orafti, the American Peanut Council, the International Tree Nut Council Nutrition Research and Education Foundation, the Peanut Institute, Herbalife International, Pacific Health Laboratories, Barilla, Metagenics, Bayer Consumer Care, Unilever Canada and Netherlands, Solae, Kellogg, Quaker Oats, Procter & Gamble, Abbott Laboratories, Dean Foods, the California Strawberry Commission, Haine Celestial, PepsiCo, the Alpro Foundation, Pioneer Hi-Bred International, DuPont Nutrition and Health, Spherix Consulting and WhiteWave Foods, the Advanced Foods and Material Network, the Canola and Flax Councils of Canada, Agri-Culture and Agri-Food Canada, the Canadian Agri-Food Policy Institute, Pulse Canada, the Soy Foods Association of North America, the Nutrition Foundation of Italy (NFI), Nutra-Source Diagnostics, the McDougall Program, the Toronto Knowledge Translation Group (St. Michael’s Hospital), the Canadian College of Naturopathic Medicine, The Hospital for Sick Children, the Canadian Nutrition Society (CNS), the American Society of Nutrition (ASN), Arizona State University, Paolo Sorbini Foundation and the Institute of Nutrition, Metabolism and Diabetes. He received an honorarium from the United States Department of Agriculture to present the 2013 W.O. Atwater Memorial Lecture. He received the 2013 Award for Excellence in Research from the International Nut and Dried Fruit Council. He received funding and travel support from the Canadian Society of Endocrinology and Metabolism to produce mini cases for the Canadian Diabetes Association (CDA). He is a member of the International Carbohydrate Quality Consortium (ICQC). His wife, Alexandra L Jenkins, is a director and partner of INQUIS Clinical Research for the Food Industry, his 2 daughters, Wendy Jenkins and Amy Jenkins, have published a vegetarian book that promotes the use of the foods described here, The Portfolio Diet for Cardiovascular Risk Reduction (Academic Press/Elsevier 2020 ISBN:978-0-12-810510-8)and his sister, Caroline Brydson, received funding through a grant from the St. Michael’s Hospital Foundation to develop a cookbook for one of his studies. JLS has received research support from the Canadian Foundation for Innovation, Ontario Research Fund, Province of Ontario Ministry of Research and Innovation and Science, Canadian Institutes of health Research (CIHR), Diabetes Canada, American Society for Nutrition (ASN), International Nut and Dried Fruit Council (INC) Foundation, National Honey Board (the U.S. Department of Agriculture [USDA] honey “Checkoff” program), Institute for the Advancement of Food and Nutrition Sciences (IAFNS), Pulse Canada, Quaker Oats Center of Excellence, The United Soybean Board (the USDA soy “Checkoff” program), The Tate and Lyle Nutritional Research Fund at the University of Toronto, The Glycemic Control and Cardiovascular Disease in Type 2 Diabetes Fund at the University of Toronto (a fund established by the Alberta Pulse Growers), The Plant Protein Fund at the University of Toronto (a fund which has received contributions from IFF), and The Nutrition Trialists Fund at the University of Toronto (a fund established by an inaugural donation from the Calorie Control Council). He has received food donations to support randomized controlled trials from the Almond Board of California, California Walnut Commission, Peanut Institute, Barilla, Unilever/Upfield, Unico/Primo, Loblaw Companies, Quaker, Kellogg Canada, WhiteWave Foods/Danone, Nutrartis, and Dairy Farmers of Canada. He has received travel support, speaker fees and/or honoraria from ASN, Danone, Dairy Farmers of Canada, FoodMinds LLC, Nestlé, Abbott, General Mills, Nutrition Communications, International Food Information Council (IFIC), Calorie Control Council, International Sweeteners Association, and International Glutamate Technical Committee. He has or has had ad hoc consulting arrangements with Perkins Coie LLP, Tate & Lyle, Phynova, and INQUIS Clinical Research. He is a former member of the European Fruit Juice Association Scientific Expert Panel and former member of the Soy Nutrition Institute (SNI) Scientific Advisory Committee. He is on the Clinical Practice Guidelines Expert Committees of Diabetes Canada, European Association for the study of Diabetes (EASD), Canadian Cardiovascular Society (CCS), and Obesity Canada/Canadian Association of Bariatric Physicians and Surgeons. He serves or has served as an unpaid member of the Board of Trustees and an unpaid scientific advisor for the Carbohydrates Committee of IAFNS. He is a member of the International Carbohydrate Quality Consortium (ICQC), Executive Board Member of the Diabetes and Nutrition Study Group (DNSG) of the EASD, and Director of the Toronto 3D Knowledge Synthesis and Clinical Trials foundation. His spouse is an employee of AB InBev. QL, XQ, SBM, VLC, AE-S, and LAL declare no competing interests. There are no products in development or marketed products to declare.
Funding Statement
This work was supported by Diabetes Canada (CS-5-15-4771-JS) and the Canadian Institutes of Health Research (funding reference number, 129920). The Diet, Digestive tract, and Disease (3-D) Centre, funded through the Canada Foundation for Innovation (CFI) and the Ministry of Research, and Innovation’s Ontario Research Fund (ORF), provided the infrastructure for the conduct of this project. DL was funded by a St. Michael’s Hospital Research Training Centre Scholarship. LC was funded by a Mitacs-Elevate Postdoctoral Fellowship Award. SA-C was funded by a CIHR Canada Graduate Scholarships Master’s Award, the Loblaw Food as Medicine Graduate Award, and the Ontario Graduate Scholarship. TAK was funded by a Toronto 3D Foundation Postdoctoral Fellowship Award. AZ was funded by a BBDC Postdoctoral Fellowship. AC and AA were funded by Toronto 3D Foundation MSc Scholarship Awards. DJAJ was funded by the Government of Canada through the Canada Research Chair Endowment. JLS was funded by a PSI Graham Farquharson Knowledge Translation Fellowship, Diabetes Canada Clinician Scientist award, CIHR INMD/CNS New Investigator Partnership Prize, and Banting & Best Diabetes Centre Sun Life Financial New Investigator Award.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bellentani S., Marino M. Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD) Ann. Hepatol. 2009;8((Suppl. 1)):S4–S8. doi: 10.1016/S1665-2681(19)31820-4. [DOI] [PubMed] [Google Scholar]
- 2.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 3.Lelis D.D.F., Andrade J.M.O., Almenara C.C.P., Broseguini-Filho G.B., Mill J.G., Baldo M.P. High fructose intake and the route towards cardiometabolic diseases. Life Sci. 2020;259:118235. doi: 10.1016/j.lfs.2020.118235. [DOI] [PubMed] [Google Scholar]
- 4.Campos V.C., Tappy L. Physiological handling of dietary fructose-containing sugars: Implications for health. Int. J. Obes. 2016;40((Suppl. 1)):S6–S11. doi: 10.1038/ijo.2016.8. [DOI] [PubMed] [Google Scholar]
- 5.Sun S.Z., Empie M.W. Fructose metabolism in humans—What isotopic tracer studies tell us. Nutr. Metab. 2012;9:89. doi: 10.1186/1743-7075-9-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.European Association for the Study of the Liver, European Association for the Study of Diabetes, European Association for the Study of Obesity EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016;64:1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Chiu S., Sievenpiper J.L., de Souza R., Cozma A.I., Mirrahimi A., Carleton A.J., Ha V., Di Buono M., Jenkins A.L., Leiter L.A., et al. Effect of fructose on markers of non-alcoholic fatty liver disease (NAFLD): A systematic review and meta-analysis of controlled feeding trials. Eur. J. Clin. Nutr. 2014;68:416–423. doi: 10.1038/ejcn.2014.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choo V.L., Viguiliouk E., Mejia S.B., Cozma A.I., Khan T.A., Ha V., Wolever T.M.S., Leiter L.A., Vuksan V., Kendall C.W.C., et al. Food sources of fructose-containing sugars and glycaemic control: Systematic review and meta-analysis of controlled intervention studies. BMJ. 2018;363:k4644. doi: 10.1136/bmj.k4644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayoub-Charette S., Chiavaroli L., Liu Q., Khan T.A., Zurbau A., Au-Yeung F., Cheung A., Ahmed A., Lee D., Choo V.L., et al. Different Food Sources of Fructose-Containing Sugars and Fasting Blood Uric Acid Levels: A Systematic Review and Meta-Analysis of Controlled Feeding Trials. J. Nutr. 2021;151:2409–2421. doi: 10.1093/jn/nxab144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Q., Chiavaroli L., Ayoub-Charette S., Khan T., Au-Yeung F., Cheung A., Lee D., Ahmed A., Mejia S.B., de Souza R.J., et al. Important Food Sources of Fructose-Containing Sugars and Blood Pressure: A Systematic Review and Meta-Analysis of Controlled Trials. Curr. Dev. Nutr. 2021;5((Suppl. 2)):1056. doi: 10.1093/cdn/nzab053_049. [DOI] [Google Scholar]
- 11.Chiavaroli L., Cheung A., Ayoub-Charette S., Ahmed A., Lee D., Au-Yeung F., McGlynn N., Ha V., Khan T., Mejia S.B., et al. Important Food Sources of Fructose-Containing Sugars and Adiposity: A Systematic Review and Meta-Analysis of Controlled Feeding Trials. Curr. Dev. Nutr. 2021;5((Suppl. 2)):1017. doi: 10.1093/cdn/nzab053_010. [DOI] [PubMed] [Google Scholar]
- 12.Higgins J.P., Thomas T.J., Chandler J., Cumpston M., Li T., Page M.J., Welch V.A. Cochrane Handbook for Systematic Reviews of Interventions. Wiley; Hoboken, NJ, USA: 2020. [(accessed on 2 June 2022)]. Version 6.1 [Internet] Available online: https://training.cochrane.org/cochrane-handbook-systematic-reviews-interventions#how-to-cite. [Google Scholar]
- 13.Page M.J., Moher D., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilczynski N.L., Morgan D., Haynes R.B., Hedges T. An overview of the design and methods for retrieving high-quality studies for clinical care. BMC Med. Inform. Decis. Mak. 2005;5:20. doi: 10.1186/1472-6947-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Source Forge Plot Digitizer. 2001. [(accessed on 18 January 2022)]. Available online: http://plotdigitizer.sourceforge.net/
- 16.Luo D., Wan X., Liu J., Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2018;27:1785–1805. doi: 10.1177/0962280216669183. [DOI] [PubMed] [Google Scholar]
- 17.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Furukawa T.A., Barbui C., Cipriani A., Brambilla P., Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. J. Clin. Epidemiol. 2006;59:7–10. doi: 10.1016/j.jclinepi.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. Introduction to Meta-Analysis. John Wiley & Sons; Oxford, UK: 2009. [Google Scholar]
- 20.Borenstein M., Higgins J.P. Meta-analysis and subgroups. Prev. Sci. 2013;14:134–143. doi: 10.1007/s11121-013-0377-7. [DOI] [PubMed] [Google Scholar]
- 21.Deeks J.J., Higgins J.P., Altman D.G. Cochrane Handbook for Systematic Reviews of Interventions. Wiley; Hoboken, NJ, USA: 2019. Cochrane Statistical Methods Group. Analysing data and undertaking meta-analyses; pp. 241–284. [Google Scholar]
- 22.Der Simonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.Elbourne D.R., Altman D.G., Higgins J., Curtin F., Worthington H., Vail A. Meta-analyses involving cross-over trials: Methodological issues. Int. J. Epidemiol. 2002;31:140–149. doi: 10.1093/ije/31.1.140. [DOI] [PubMed] [Google Scholar]
- 24.Follmann D., Elliott P., Suh I., Cutler J. Variance imputation for overviews of clinical trials with continuous response. J. Clin. Epidemiol. 1992;45:769–773. doi: 10.1016/0895-4356(92)90054-Q. [DOI] [PubMed] [Google Scholar]
- 25.Balk E.M., Earley A., Patel K., Trikalinos T.A., Dahabreh I.J. AHRQ Methods for Effective Health Care. Empirical Assessment of Within-Arm Correlation Imputation in Trials of Continuous Outcomes. Agency for Healthcare Research and Quality; Rockville, MD, USA: 2012. [PubMed] [Google Scholar]
- 26.Hedges L., Olkin I. Statistical Methods in Meta-Analysis. Academic Press; Cambridge, MA, USA: 2019. [Google Scholar]
- 27.Tietz N.W., Carl A.B., Edward R.A. Tietz Textbook of Clinical Chemistry. 2nd ed. Saunders; Philadelphia, PA, USA: 1994. [Google Scholar]
- 28.Thompson S.G., Higgins J.P. How should meta-regression analyses be undertaken and interpreted? Stat. Med. 2002;21:1559–1573. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]
- 29.Fu R., Gartlehner G., Grant M., Shamliyan T., Sedrakyan A., Wilt T.J., Griffith L., Oremus M., Raina P., Ismaila A., et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the Effective Health Care Program. J. Clin. Epidemiol. 2011;64:1187–1197. doi: 10.1016/j.jclinepi.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization . Guideline: Sugars Intake for Adults and Children. World Health Organization; Geneva, Switzerland: 2015. [(accessed on 11 January 2022)]. Available online: http://apps.who.int/iris/bitstream/handle/10665/149782/9789241549028_eng.pdf;jsessionid=F9FAD19E165BB45830BA1A484FC6FD93?sequence=1. [Google Scholar]
- 31.Scientific Advisory Committee on Nutrition Carbohydrates and Health: Scientific Advisory Committee on Nutrition. [(accessed on 11 January 2022)];2015 Available online: https://www.gov.uk/government/publications/sacn-carbohydrates-and-health-report#:~:text=The%20Scientific%20Advisory%20Committee%20on%20Nutrition%20(%20SACN%20)%20was%20asked%20by,2%20diabetes%2C%20bowel%20health%20and.
- 32.United States Department of Health and Human Services and United States Department of Agriculture . 2015–2020 Dietary Guidelines for Americans. 8th ed. United States Department of Health and Human Services and United States Department of Agriculture; Washington, DC, USA: 2015. [(accessed on 11 January 2022)]. Available online: http://health.gov/dietaryguidelines/2015/guidelines/ [Google Scholar]
- 33.Institute of Medicine . Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. The National Academies Press; Washington, DC, USA: 2005. [(accessed on 11 January 2022)]. Available online: https://www.nap.edu/catalog/10490/dietary-reference-intakes-for-energy-carbohydrate-fiber-fat-fatty-acids-cholesterol-protein-and-amino-acids. [Google Scholar]
- 34.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Begg C.B., Mazumdar M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 36.Sterne J.A., Gavaghan D., Egger M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J. Clin. Epidemiol. 2000;53:1119–1129. doi: 10.1016/S0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- 37.Duval S., Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 38.Schünemann H.B.J., Guyatt G.O.A. GRADE Handbook. 2013. [(accessed on 2 June 2022)]. Available online: https://handbook-5-1.cochrane.org.
- 39.Andrews J., Guyatt G., Oxman A.D., Alderson P., Dahm P., Falck-Ytter Y., Nasser M., Meerpohl J., Post P.N., Kunz R., et al. GRADE guidelines: Going from evidence to recommendations: The significance and presentation of recommendations. J. Clin. Epidemiol. 2013;66:719–725. doi: 10.1016/j.jclinepi.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 40.Brunetti M., Shemilt I., Pregno S., Vale L., Oxman A.D., Lord J., Sisk J., Ruiz F., Hill S., Guyatt G.H., et al. GRADE guidelines: Considering resource use and rating the quality of economic evidence. J. Clin. Epidemiol. 2013;66:140–150. doi: 10.1016/j.jclinepi.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 41.Guyatt G.H., Oxman A.D., Schünemann H.J. GRADE guidelines-an introduction to the 10th–13th articles in the series. J. Clin. Epidemiol. 2013;66:121–123. doi: 10.1016/j.jclinepi.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 42.Guyatt G., Oxman A.D., Sultan S., Brozek J., Glasziou P., Alonso-Coello P., Atkins D., Kunz R., Montori V., Jaeschke R., et al. GRADE guidelines: Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J. Clin. Epidemiol. 2013;66:151–157. doi: 10.1016/j.jclinepi.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 43.Guyatt G.H., Oxman A.D., Santesso N., Helfand M., Vist G., Kunz R. GRADE guidelines: Preparing summary of findings tables-binary outcomes. J. Clin. Epidemiol. 2013;66:158–172. doi: 10.1016/j.jclinepi.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 44.Guyatt G.H., Thorlund K., Oxman A.D., Walter S.D., Patrick D., Furukawa T.A. GRADE guidelines: Preparing summary of findings tables and evidence profiles-continuous outcomes. J. Clin. Epidemiol. 2013;66:173–183. doi: 10.1016/j.jclinepi.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 45.Aeberli I., Gerber P.A., Hochuli M., Kohler S., Haile S.R., Gouni-Berthold I. Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: A randomized controlled trial. Am. J. Clin. Nutr. 2011;94:479–485. doi: 10.3945/ajcn.111.013540. [DOI] [PubMed] [Google Scholar]
- 46.Agebratt C., Ström E., Romu T., Dahlqvist-Leinhard O., Borga M., Leanderson P., Nystrom F.H. A Randomized Study of the Effects of Additional Fruit and Nuts Consumption on Hepatic Fat Content, Cardiovascular Risk Factors and Basal Metabolic Rate. PLoS ONE. 2016;11:e0147149. doi: 10.1371/journal.pone.0147149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Banini A.E., Boyd L.C., Allen J.C., Allen H.G., Sauls D.L. Muscadine grape products intake, diet and blood constituents of non-diabetic and type 2 diabetic subjects. Nutrition. 2006;22:1137–1145. doi: 10.1016/j.nut.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 48.Kreis R., Boesch C.H., Campos V., Schneiter P., Despland C., Brandejsky V., Tappy L., Chiolero A. Sugar and artificially sweetened beverages and intrahepatic fat: A randomized controlled trial. Obes. (Silver Spring) 2015;23:2335–2339. doi: 10.7892/boris.80128. [DOI] [PubMed] [Google Scholar]
- 49.Claesson A.L., Holm G., Ernersson A., Lindström T., Nystrom F.H. Two weeks of overfeeding with candy, but not peanuts, increases insulin levels and body weight. Scand. J. Clin. Lab. Investig. 2009;69:598–605. doi: 10.1080/00365510902912754. [DOI] [PubMed] [Google Scholar]
- 50.Cox C.L., Stanhope K.L., Schwarz J.M., Graham J.L., Hatcher B., Griffen S.C., Bremer A.A., Berglund L., McGahan J.P., Keim N.L., et al. Consumption of fructose- but not glucose-sweetened beverages for 10 weeks increases circulating concentrations of uric acid, retinol binding protein-4, and gamma-glutamyl transferase activity in overweight/obese humans. Nutr. Metab. 2012;9:68. doi: 10.1186/1743-7075-9-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jin R., Welsh J.A., Le N.-A., Holzberg J., Sharma P., Martin D.R., Vos M.B. Dietary Fructose Reduction Improves Markers of Cardiovascular Disease Risk in Hispanic-American Adolescents with NAFLD. Nutrients. 2014;6:3187–3201. doi: 10.3390/nu6083187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Johnston R.D., Stephenson M.C., Crossland H., Cordon S.M., Palcidi E., Cox E., Taylor M.A., Aithal G., Macdonald I. No Difference Between High-Fructose and High-Glucose Diets on Liver Triacylglycerol or Biochemistry in Healthy Overweight Men. Gastroenterology. 2013;145:1016–1025.e2. doi: 10.1053/j.gastro.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 53.Koopman K.E., Caan M.W., Nederveen A.J., Pels A., Ackermans M.T., Fliers E., La Fleur S.E., Serlie M.J. Hypercaloric diets with increased meal frequency, but not meal size, increase intrahepatic triglycerides: A randomized controlled trial. Hepatology. 2014;60:545–553. doi: 10.1002/hep.27149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lê K.A., Faeh D., Stettler R., Ith M., Kreis R., Vermathen P., Tappy L. A 4-wk high-fructose diet alters lipid metabolism without affecting insulin sensitivity or ectopic lipids in healthy humans. Am. J. Clin. Nutr. 2006;84:1374–1379. doi: 10.1093/ajcn/84.6.1374. [DOI] [PubMed] [Google Scholar]
- 55.Lê K.A., Ith M., Kreis R., Faeh D., Bortolotti M., Tran C., Tappy L. Fructose overconsumption causes dyslipidemia and ectopic lipid deposition in healthy subjects with and without a family history of type 2 diabetes. Am. J. Clin. Nutr. 2009;89:1760–1765. doi: 10.3945/ajcn.2008.27336. [DOI] [PubMed] [Google Scholar]
- 56.Lehtonen H.-M., Suomela J.-P., Tahvonen R., Vaarno J., Venojärvi M., Viikari J., Kallio H. Berry meals and risk factors associated with metabolic syndrome. Eur. J. Clin. Nutr. 2010;64:614–621. doi: 10.1038/ejcn.2010.27. [DOI] [PubMed] [Google Scholar]
- 57.Ngo Sock E.T., Lê K.A., Ith M., Kreis R., Boesch C., Tappy L. Effects of a short-term overfeeding with fructose or glucose in healthy young males. Br. J. Nutr. 2010;103:939–943. doi: 10.1017/S0007114509992819. [DOI] [PubMed] [Google Scholar]
- 58.Ravn-Haren G., Dragsted L.O., Buch-Andersen T., Jensen E.N., Jensen R.I., Németh-Balogh M., Paulovicsová B., Bergström A., Wilcks A., Licht T.R., et al. Intake of whole apples or clear apple juice has contrasting effects on plasma lipids in healthy volunteers. Eur. J. Nutr. 2013;52:1875–1889. doi: 10.1007/s00394-012-0489-z. [DOI] [PubMed] [Google Scholar]
- 59.Ahmed T., Sadia H., Khalid A., Batool S., Janjua A. Report: Prunes and liver function: A clinical trial. Pak. J. Pharm. Sci. 2010;23:463–466. [PubMed] [Google Scholar]
- 60.Alavinejad P., Alavinejad F.F.P., Farsi F., Rezazadeh A., Mahmoodi M., Hajiani E., Masjedizadeh A.R., Mard S.A., Neisi N., Hoseini H., et al. The Effects of Dark Chocolate Consumption on Lipid Profile, Fasting Blood Sugar, Liver Enzymes, Inflammation, and Antioxidant Status in Patients with Non-Alcoholic Fatty Liver Disease: A Randomized, Placebo-Controlled, Pilot study. J. Gastroenterol. Hepatol. Res. 2015;4:1858–1864. doi: 10.17554/j.issn.2224-3992.2015.04.589. [DOI] [Google Scholar]
- 61.Amagase H., Sun B., Nance D.M. Immunomodulatory effects of a standardized Lycium barbarum fruit juice in Chinese older healthy human subjects. J. Med. Food. 2009;12:1159–1165. doi: 10.1089/jmf.2008.0300. [DOI] [PubMed] [Google Scholar]
- 62.Bahrami M., Ataie-Jafari A., Hosseini S., Foruzanfar M.H., Rahmani M., Pajouhi M. Effects of natural honey consumption in diabetic patients: An 8-week randomized clinical trial. Int. J. Food Sci. Nutr. 2009;60:618–626. doi: 10.3109/09637480801990389. [DOI] [PubMed] [Google Scholar]
- 63.Chiu S., Siri-Tarino P., Bergeron N., Suh J.H., Krauss R.M. A Randomized Study of the Effect of Replacing Sugar-Sweetened Soda by Reduced Fat Milk on Cardiometabolic Health in Male Adolescent Soda Drinkers. Nutrients. 2020;12:405. doi: 10.3390/nu12020405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Eslami O., Shidfar F., Maleki Z., Jazayeri S., Hosseini A.F., Agah S., Ardiyani F. Effect of Soy Milk on Metabolic Status of Patients with Nonalcoholic Fatty Liver Disease: A Randomized Clinical Trial. J. Am. Coll. Nutr. 2019;38:51–58. doi: 10.1080/07315724.2018.1479990. [DOI] [PubMed] [Google Scholar]
- 65.Niri Z.I., Shidfar F., Jabbari M., Zarrati M., Hosseini A., Malek M. The effect of dried Ziziphus vulgaris on glycemic control, lipid profile, Apo-proteins and hs-CRP in patients with type 2 diabetes mellitus: A randomized controlled clinical trial. J. Food Biochem. 2020;45:e13193. doi: 10.1111/jfbc.13193. [DOI] [PubMed] [Google Scholar]
- 66.Kaliora A.C., Kokkinos A., Diolintzi A., Stoupaki M., Gioxari A., Kanellos P.T., Dedoussis G.V.Z., Vlachogiannakos J., Revenas C., Ladas S.D., et al. The effect of minimal dietary changes with raisins in NAFLD patients with non-significant fibrosis: A randomized controlled intervention. Food Funct. 2016;7:4533–4544. doi: 10.1039/C6FO01040G. [DOI] [PubMed] [Google Scholar]
- 67.Kanellos P.T., Kaliora A.C., Protogerou A., Tentolouris N., Perrea D.N., Karathanos V.T. The effect of raisins on biomarkers of endothelial function and oxidant damage; an open-label and randomized controlled intervention. Food Res. Int. 2017;102:674–680. doi: 10.1016/j.foodres.2017.09.061. [DOI] [PubMed] [Google Scholar]
- 68.Kelsay J.L., Behall K.M., Holden J.M., Prather E.S. Diets high in glucose or sucrose and young women. Am. J. Clin. Nutr. 1974;27:926–936. doi: 10.1093/ajcn/27.9.926. [DOI] [PubMed] [Google Scholar]
- 69.Lehtonen H.-M., Suomela J.-P., Tahvonen R., Yang B., Venojärvi M., Viikari J., Kallio H. Different berries and berry fractions have various but slightly positive effects on the associated variables of metabolic diseases on overweight and obese women. Eur. J. Clin. Nutr. 2011;65:394–401. doi: 10.1038/ejcn.2010.268. [DOI] [PubMed] [Google Scholar]
- 70.Luukkonen P.K., Sädevirta S., Zhou Y., Kayser B., Ali A., Ahonen L., Lallukka S., Pelloux V., Gaggini M., Jian C., et al. Saturated Fat Is More Metabolically Harmful for the Human Liver Than Unsaturated Fat or Simple Sugars. Diabetes Care. 2018;41:1732–1739. doi: 10.2337/dc18-0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Maersk M., Belza A., Stødkilde-Jørgensen H., Ringgaard S., Chabanova E., Thomsen H., Pedersen S.B., Astrup A., Richelsen B. Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: A 6-mo randomized intervention study. Am. J. Clin. Nutr. 2012;95:283–289. doi: 10.3945/ajcn.111.022533. [DOI] [PubMed] [Google Scholar]
- 72.Mäkinen K.K., Scheinin A. Turku sugar studies XIII: Effect of the diet on certain clinico-chemical values of serum. Acta Odontol. Scand. 1976;34:371–380. doi: 10.3109/00016357609004648. [DOI] [PubMed] [Google Scholar]
- 73.Nier A., Brandt A., Conzelmann I.B., Özel Y., Bergheim I. Non-Alcoholic Fatty Liver Disease in Overweight Children: Role of Fructose Intake and Dietary Pattern. Nutrients. 2018;10:1329. doi: 10.3390/nu10091329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ribeiro C., Dourado G., Cesar T. Orange juice allied to a reduced-calorie diet results in weight loss and ameliorates obesity-related biomarkers: A randomized controlled trial. Nutrition. 2017;38:13–19. doi: 10.1016/j.nut.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 75.Silbernagel G., Machann J., Unmuth S., Schick F., Stefan N., Häring H.U., Fritsche A. Effects of 4-week very-high-fructose/glucose diets on insulin sensitivity, visceral fat and intrahepatic lipids: An exploratory trial. Br. J. Nutr. 2011;106:79–86. doi: 10.1017/S000711451000574X. [DOI] [PubMed] [Google Scholar]
- 76.Sobrecases H., Lê K.-A., Bortolotti M., Schneiter P., Ith M., Kreis R., Boesch C., Tappy L. Effects of short-term overfeeding with fructose, fat and fructose plus fat on plasma and hepatic lipids in healthy men. Diabetes Metab. 2010;36:244–246. doi: 10.1016/j.diabet.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 77.Parry S.A., Rosqvist F., Mozes F.E., Cornfield T., Hutchinson M., Piche M.-E., Hülsmeier A.J., Hornemann T., Dyson P., Hodson L. Intrahepatic Fat and Postprandial Glycemia Increase After Consumption of a Diet Enriched in Saturated Fat Compared with Free Sugars. Diabetes Care. 2020;43:1134–1141. doi: 10.2337/dc19-2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Purkins L., Love E.R., Eve M.D., Wooldridge C.L., Cowan C., Smart T.S., Johnson P.J., Rapeport G. The influence of diet upon liver function tests and serum lipids in healthy male volunteers resident in a Phase I unit. Br. J. Clin. Pharmacol. 2004;57:199–208. doi: 10.1046/j.1365-2125.2003.01969.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schell J., Betts N.M., Lyons T.J., Basu A. Raspberries Improve Postprandial Glucose and Acute and Chronic Inflammation in Adults with Type 2 Diabetes. Ann. Nutr. Metab. 2019;74:165–174. doi: 10.1159/000497226. [DOI] [PubMed] [Google Scholar]
- 80.Schwarz J.-M., Noworolski S.M., Wen M.J., Dyachenko A., Prior J.L., Weinberg M.E., Herraiz L.A., Tai V.W., Bergeron N., Bersot T.P., et al. Effect of a High-Fructose Weight-Maintaining Diet on Lipogenesis and Liver Fat. J. Clin. Endocrinol. Metab. 2015;100:2434–2442. doi: 10.1210/jc.2014-3678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schwimmer J.B., Ugalde-Nicalo P., Welsh J.A., Angeles J.E., Cordero M., Harlow K.E. Effect of a Low Free Sugar Diet vs Usual Diet on Nonalcoholic Fatty Liver Disease in Adolescent Boys: A Randomized Clinical Trial. JAMA. 2019;321:256–265. doi: 10.1001/jama.2018.20579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Umpleby A.M., Shojaee-Moradie F., Fielding B., Li X., Marino A., Alsini N., Isherwood C., Jackson N., Ahmad A., Stolinski M., et al. Impact of liver fat on the differential partitioning of hepatic triacylglycerol into VLDL subclasses on high and low sugar diets. Clin. Sci. 2017;131:2561–2573. doi: 10.1042/CS20171208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vos M.B., Weber M.B., Welsh J., Khatoon F., Jones D.P., Whitington P.F., McClain C.J. Fructose and Oxidized Low-Density Lipoprotein in Pediatric Nonalcoholic Fatty Liver Disease: A Pilot Study. Arch. Pediatr. Adolesc. Med. 2009;163:674–675. doi: 10.1001/archpediatrics.2009.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zakaria Z., Abidin Z.F.Z., Gan S.H., Hamid W.Z.W.A., Mohamed M. Effects of honey supplementation on safety profiles among postmenopausal breast cancer patients. J. Taibah Univ. Med. Sci. 2018;13:535–540. doi: 10.1016/j.jtumed.2018.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dikariyanto V., Smith L., Francis L., Robertson M., Kusaslan E., O’Callaghan-Latham M., Palanche C., D’Annibale M., Christodoulou D., Basty N., et al. Snacking on whole almonds for 6 weeks improves endothelial function and lowers LDL cholesterol but does not affect liver fat and other cardiometabolic risk factors in healthy adults: The ATTIS study, a randomized controlled trial. Am. J. Clin. Nutr. 2020;111:1178–1189. doi: 10.1093/ajcn/nqaa100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Simons N., Veeraiah P., Simons P.I.H.G., Schaper N.C., Kooi M.E., Schrauwen-Hinderling V.B., Feskens E.J.M., van der Ploeg E.M.C. Effects of fructose restriction on liver steatosis (FRUITLESS); A double-blind randomized controlled trial. Am. J. Clin. Nutr. 2021;113:391–400. doi: 10.1093/ajcn/nqaa332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tang S.P., Wan Yusuf W.N., Abd Aziz C.B., Mustafa M., Mohamed M. Effects of Six-Month Tualang Honey Supplementation on Physiological and Biochemical Profiles in Asymptomatic, Treatment-naïve HIV-infected Patients. Trop. J. Nat. Prod. Res. 2020;4:1116–1123. [Google Scholar]
- 88.Porikos K.P., Van Itallie T.B. Diet-induced changes in serum transaminase and triglyceride levels in healthy adult men: Role of sucrose and excess calories. Am. J. Med. 1983;75:624–630. doi: 10.1016/0002-9343(83)90444-8. [DOI] [PubMed] [Google Scholar]
- 89.Alemán J.O., Henderson W.A., Walker J.M., Ronning A., Jones D.R., Walter P.J., Daniel S.G., Bittinger K., Vaughan R., MacArthur R., et al. Excess dietary fructose does not alter gut microbiota or permeability in humans: A pilot randomized controlled study. J. Clin. Transl. Sci. 2021;5:e143. doi: 10.1017/cts.2021.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Debray F.-G., Seyssel K., Fadeur M., Tappy L., Paquot N., Tran C. Effect of a high fructose diet on metabolic parameters in carriers for hereditary fructose intolerance. Clin. Nutr. 2021;40:4246–4254. doi: 10.1016/j.clnu.2021.01.026. [DOI] [PubMed] [Google Scholar]
- 91.Kojadinovic M., Glibetic M., Vucic V., Popovic M., Vidovic N., Debeljak-Martacic J., Arsic A. Short-Term Consumption of Pomegranate Juice Alleviates Some Metabolic Disturbances in Overweight Patients with Dyslipidemia. J. Med. Food. 2021;24:925–933. doi: 10.1089/jmf.2020.0122. [DOI] [PubMed] [Google Scholar]
- 92.Ponce O., Benassi R., Cesar T. Orange juice associated with a balanced diet mitigated risk factors of metabolic syndrome: A randomized controlled trial. J. Nutr. Intermed. Metab. 2019;17:100101. doi: 10.1016/j.jnim.2019.100101. [DOI] [Google Scholar]
- 93.Sigala D.M., Hieronimus B., Medici V., Lee V., Nunez M.V., Bremer A.A., Cox C.L., Price C.A., Benyam Y., Chaudhari A.J., et al. Consuming Sucrose- or HFCS-sweetened Beverages Increases Hepatic Lipid and Decreases Insulin Sensitivity in Adults. J. Clin. Endocrinol. Metab. 2021;106:3248–3264. doi: 10.1210/clinem/dgab508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tutino V., De Nunzio V., Milella R.A., Gasparro M., Cisternino A.M., Gigante I., Lanzilotta E., Iacovazzi P.A., Lippolis A., Lippolis T., et al. Impact of Fresh Table Grape Intake on Circulating microRNAs Levels in Healthy Subjects: A Significant Modulation of Gastrointestinal Cancer-Related Pathways. Mol. Nutr. Food Res. 2021;65:2100428. doi: 10.1002/mnfr.202100428. [DOI] [PubMed] [Google Scholar]
- 95.Chung M., Ma J., Patel K., Berger S., Lau J., Lichtenstein A.H. Fructose, high-fructose corn syrup, sucrose, and nonalcoholic fatty liver disease or indexes of liver health: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2014;100:833–849. doi: 10.3945/ajcn.114.086314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wijarnpreecha K., Thongprayoon C., Edmonds P., Cheungpasitporn W. Associations of sugar and artificially sweetened soda with nonalcoholic fatty liver disease: A systematic review and meta-analysis. QJM Int. J. Med. 2016;109:461–466. doi: 10.1093/qjmed/hcv172. [DOI] [PubMed] [Google Scholar]
- 97.Asgari-Taee F., Zerafati-Shoae N., Dehghani M., Sadeghi M., Baradaran H.R., Jazayeri S. Association of sugar sweetened beverages consumption with non-alcoholic fatty liver disease: A systematic review and meta-analysis. Eur. J. Nutr. 2019;58:1759–1769. doi: 10.1007/s00394-018-1711-4. [DOI] [PubMed] [Google Scholar]
- 98.Kanerva N., Sandboge S., Kaartinen N.E., Männistö S., Eriksson J.G. Higher fructose intake is inversely associated with risk of nonalcoholic fatty liver disease in older Finnish adults. Am. J. Clin. Nutr. 2014;100:1133–1138. doi: 10.3945/ajcn.114.086074. [DOI] [PubMed] [Google Scholar]
- 99.Sievenpiper J.L., Dworatzek P.D. Food and Dietary Pattern-Based Recommendations: An Emerging Approach to Clinical Practice Guidelines for Nutrition Therapy in Diabetes. Can. J. Diabetes. 2013;37:51–57. doi: 10.1016/j.jcjd.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 100.Pearson G.J., Thanassoulis G., Anderson T.J., Barry A.R., Couture P., Dayan N., Wray W. 2021 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in Adults. Can. J. Cardiol. 2021;37:1129–1150. doi: 10.1016/j.cjca.2021.03.016. [DOI] [PubMed] [Google Scholar]
- 101.Wharton S., Lau D.C., Vallis M., Sharma A.M., Biertho L., Campbell-Scherer D., Adamo K., Alberga A., Bell R., Boulé N., et al. Obesity in adults: A clinical practice guideline. Can. Med. Assoc. J. 2020;192:E875–E891. doi: 10.1503/cmaj.191707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sievenpiper J.L., Chan C.B., Dworatzek P.D., Freeze C., Williams S.L. Nutrition Therapy. Can. J. Diabetes. 2018;42((Suppl. 1)):S64–S79. doi: 10.1016/j.jcjd.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 103.Santesso N., Glenton C., Dahm P., Garner P., Akl E.A., Alper B., Brignardello-Petersen R., Carrasco-Labra A., De Beer H., Hultcrantz M., et al. GRADE guidelines 26: Informative statements to communicate the findings of systematic reviews of interventions. J. Clin. Epidemiol. 2019;119:126–135. doi: 10.1016/j.jclinepi.2019.10.014. [DOI] [PubMed] [Google Scholar]
- 104.Balshem H., Helfand M., Schunemann H.J., Oxman A.D., Kunz R., Brozek J., Vist G.E., Falck-Ytter Y., Meerpohl J., Norris S., et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011;64:401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 105.Wang Y.F., Chiavaroli L., Roke K., DiAngelo C., Marsden S., Sievenpiper J. Canadian Adults with Moderate Intakes of Total Sugars have Greater Intakes of Fibre and Key Micronutrients: Results from the Canadian Community Health Survey 2015 Public Use Microdata File. Nutrients. 2020;12:1124. doi: 10.3390/nu12041124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available upon request.