Abstract
Background:
Autologous reconstruction techniques can provide a long-lasting natural breast reconstruction for patients. This study aimed to further investigate outcomes in the conversion of breast implant reconstruction into a lipofilled mini dorsi flap, focusing on reviewing its techniques, efficiency, and final results.
Methods:
Over 3 years, we performed a number of breast implant replacements via the lipofilled mini dorsi flap technique. The artificial implants were replaced to a deepithelized flap. The efficiency and tolerance of the technique were evaluated by the whole surgical team, and the achieved results were also analyzed by the patients in terms of postoperative pain, functional impact, and the softness of the reconstructed breast by comparing their prior condition to the lipofilled mini dorsi flap condition at least 9 months after operation.
Results:
Forty-seven consecutive operations were prospectively studied. The mean ± standard deviation volume of the removed implants was 348.66 ± 86.54 mL. The mean volume of fat injected was 284.13 ± 62.94 mL. The procedure’s average duration was 108.93 ± 17.65 minutes. The surgical team evaluated the results as very satisfactory in 32 cases (68.1%), satisfactory in 15 cases (31.9%), and moderately satisfactory or unsatisfactory in zero cases (0.0%). Eighteen patients (38.3%) evaluated their reconstruction as very good, while 20 patients (42.6%) considered their reconstruction as good, four (8.5%) as average, and zero (0.0%) as insufficient.
Conclusion:
According to our experience, the lipofilled mini dorsi flap is a simple, less invasive, and quick procedure to convert breast implants into natural breast reconstruction.
Takeaways
Question: Is it possible to replace a breast reconstruction with prosthesis for a site, without aesthetic and motor impairment?
Findings: Over 3 years, we performed 47 breast implant replacements with the lipofilled mini dorsi flap. It is a simple, minimally invasive and quick procedure for conversion of breast implants into natural breast reconstruction.
Meaning: The lipofilled mini dorsi flap is a feasible technique for women who wish to exchange a breast reconstruction with prosthesis for a natural looking flap.
INTRODUCTION
Breast reconstruction using a prosthesis is the most widely used technique for breast reconstruction. This is a simple technique that provides satisfactory results in most cases. Along the way, complications or deterioration of the results may appear, requiring further operations to remove or replace the implant.1–3
In recent years, the perception of breast implant reconstruction has been negatively impacted in France by the broad media coverage of breast implant-associated risks, such as silicone leakage after rupture, the poly implant prostheses breast implant scandal, and the risk of breast implant-associated anaplastic large cell lymphoma. For those patients who want reconstruction but do not want breast implants, autologous reconstruction is the only possible option, associated with the removal of the opposite breast augmentation implant.
We have developed an innovative breast reconstruction technique using an autologous, lipofilled, deepithelized mini dorsi flap, which was initially used as a natural prosthesis in immediate breast reconstruction.4 This single-stage technique, which combines a very limited dorsal flap and lipofilling,5–9 was offered to eligible patients who needed or wanted an accurate revision of their breast implant reconstruction. The research we have developed is oriented toward assessing the efficiency, tolerance, and results of lipofilled mini dorsi flap cases in these patients.
METHODS
This was a prospective and nonrandomized study that included patients with breast cancer, invasive or in situ, and patients with genetic mutations who had undergone skin-sparing or nipple-sparing breast operation reconstructed with an inflated tissue expander or silicone-based implant, in addition to an artificial prosthesis replacement with lipofilled mini dorsi flap. All operations and proceedings regarding this study were performed and assessed by the same surgical team between May 2017 and May 2020 at Institut Européen du Sein des Deux Rives.
Patient Selection
The inclusion criteria were the presence of a breast implant with indications for implant exchange or removal. Our team numbered the definitive prostheses and expanders of patients and also those cases with a previously radiated chest wall. The exclusion criteria were the absence of a palpable latissimus dorsi, active smoking status, inadequate fat surplus for liposuction, and the presence of cosmetic breast augmentation implants. Patients who underwent radiotherapy after the lipofilled mini dorsi flap for local recurrence were also excluded.
In this context, the offer to replace the artificial prosthesis with a lipofilled mini dorsi flap was welcomed by our patients who sometimes found the associated liposuction an additional benefit. Operation was performed for patients who had a standard body shape suitable for a lipofilled mini dorsi flap, such as those with a favorable pinch test, adequate skin, fat surplus outside the mastectomy scar, and donor sites for fat harvesting.
Surgical Technique
The surgical technique is similar to that described in the case of immediate breast reconstruction,4 but included a few variations. The default patient positioning was supine and slightly lateralized with a flexed and abducted arm (Fig. 1). In all cases, the previous implants were in a retropectoral position, while the lipofilled mini dorsi flap was in a prepectoral position. At the thoracic level, the operation began with subcutaneous tissue dissection in the anterior portion of the pectoral muscle for the superior section of the reconstruction and the anterior portion of the periprosthetic capsule for the inferior section of the reconstruction. The detachment surface was adjusted depending on the width and height of the opposite breast and the positioning of the future inframammary fold.
Fig. 1.
The patient is put in the supine position, slightly lateralized, and the arm is positioned in flexion and abduction.
Liposuction was performed simultaneously by a second surgeon followed by fat harvesting, preparation, and grafting techniques.4 Lipofilling of the pectoral muscle must be initiated immediately after detachment, as it is easier to perform when the implant remains located at the same place. This is more limited than in immediate breast reconstruction, due to variable pectoral muscle wasting or retraction, which frequently occurs after using a prosthesis. The breast implant was then removed with a partial lower capsulectomy. (See Video 1 [online], which displays lipofilling of the major pectoral muscle and breast implant removal.)
Video 1. displays lipofilling of the major pectoral muscle and breast implant removal.
The lower part was closed if the prosthetic pocket was lower than the future inframammary fold. Thereafter, the capsule was stitched while tightening the pectoral muscle, repositioning it to its usual precostal position.
The isolation of the descending branch of the thoracodorsal pedicle, which vascularizes the lipofilled mini dorsi flap, is an easy procedure in the absence of radiotherapy or even after it, facilitating dissection of the lipofilled mini dorsi flap.
Dissection begins with an incision from the previously marked skin to the fascia superficialis (Fig. 1). The anterior dissection of the latissimus dorsi, below the subcutaneous tissue, was limited to an anterior muscle portion that was 5 cm wide and 12 cm long. The fat graft was then injected into the muscle before the flap release.
In this technique, approximately 80% of the latissimus dorsi, as well as its tendon and the transverse branch of the thoracodorsal pedicle, are preserved. This very limited muscle dissection led the surgical team to name this technique the “mini dorsi” flap. (See Video 2 [online], which displays dissection, preparation, and placement of the latissimus dorsi flap.)
The inferior section, followed by the posterior section of the lipofilled muscular strip, meets the superior limit of the dorsal muscle dissection. The mini dorsi flap, pedicled by the descending branch of the thoracodorsal artery, is rotated forward, maintaining its attachment to the thoracic wall at the level of the anastomosis between the vascular pedicle of the serratus anterior and the descending branch of the thoracodorsal artery, avoiding traction to the thoracodorsal vascular pedicle. After the mini dorsi flap is prepared, the corresponding skin is deepithelized. (See Video 2 [online].)
Video 2. displays dissection, preparation and placement of the latissimus dorsi flap.
Lipofilling of the subcutaneous tissue, which is rarely used in immediate reconstruction, can easily increase the reconstruction volume, particularly in the upper part. (See Video 2 [online].) The flap is positioned as a natural prosthesis, with its muscular portion at the lower internal site of the breast and the deepithelized portion at the upper external site. Symmetry procedures on the contralateral side are possible during the same operation, extending its duration. In complicated cases or under circumstances where the surgeon and patient aim to better improve the reconstruction outcomes, lipofilling was repeated at least 2 months after operation to increase the volume of the reconstructed breast.
Evaluation Criteria
Efficiency (volume achieved to replace the prosthesis) and tolerance (incidence of hematoma, infection, flap necrosis, and seroma) were assessed by the surgical team, considering the cosmetic results in accordance with their satisfaction level gathered into four clusters: very satisfactory, satisfactory, moderately satisfactory, and unsatisfactory. All data concerning the results were collected at least 9 months after the procedure.
The results were evaluated by patients before (with breast implant) and after (with a lipofilled mini dorsi flap) their procedures, with at least a 9-month interval, through a questionnaire to assess pain (score range, 1–10; with 1 for no pain and 10 for maximum pain), functional discomfort (score range, 1–6; with 1 for maximum discomfort and 6 for no discomfort), and the reconstruction consistency (1, hard; 2, firm; and 3, soft). The cosmetic results were evaluated following four definitions (4, very good; 3, good; 2, average; and 1, insufficient). This analysis established a comparison between the previous breast implant and the subsequent lipofilled mini dorsi flap. We simplified the survey by focusing on the four points that we identified as essential.
Three additional questions to further evaluate patients’ satisfaction were included at the end of the survey:
“Do you feel like you have regained a real breast rather than a breast reconstruction?”
“If you could do it again, would you do so?”
“Would you recommend this surgical procedure to another patient?”
Statistical Analysis
Data processing, database double entry, review, and analysis were performed using SPSS version 18.0. [SPSS Inc. Released 2009. PASW Statistics for Windows, version 18.0. Chicago: SPSS Inc.]. Quantitative data were expressed as mean and standard error of the mean (±SEM), or by median and 95% confidence interval (95% CI). Qualitative variables were described as absolute (n) and relative (n%) frequencies. The Shapiro–Wilk test was used to determine the normality of data distribution. When applicable, comparisons between the implant and dorsal groups were performed using the Student t test for independent samples, and the Mann–Whitney test or chi-square test with adjusted residual analysis. The level of significance was set at 5% for all analyses.
RESULTS
We performed 270 lipofilled mini dorsi flap reconstructions: 195 (72%) patients underwent immediate reconstruction and 75 (28%) underwent a secondary reconstruction between May 2017 and May 2020. Among the 75 cases, 26 were reconstructions after mastectomy without reconstruction, and 49 were breast implants replaced with a lipofilled mini dorsi flap in 44 patients. Three patients underwent bilateral conversion from a breast implant to a lipofilled mini dorsi flap in two separate operations (with a 2–7-month interval between both sides). In the 47 lipofilled mini dorsi flap reconstructions studied, the implant was definitive for 32 cases (68.1%) and received an inflated expander in the other 15 cases (31.9%). In the series of 44 patients, 47 consecutive operations were prospectively studied.
Two patients were excluded due to skin recurrence after total mastectomy followed by prosthesis reconstruction; therefore, they were exposed to postoperative radiotherapy. Considering this situation, the postoperative irradiation did not allow us an objective outcome comparison between the previous reconstruction with a prosthesis (without radiotherapy) and the minidorsal (irradiated). Eleven of the 47 patients were irradiated before flap conversion.
The median interquartile range (IQR) age was 55 (46–65) years, ranging from 35 to 74 years, but a substantial portion of 30 patients (50.8%) were aged 60 years or older. The median (IQR) body mass index was 23.75 (21.35–26.35) kg/m2, ranging from 20.00 to 36.00 kg/m2 (Table 1). Chest wall radiotherapy was performed in 11 reconstructions (23.4%) with a prosthesis. None of the patients had an acellular dermis matrix.
Table 1.
Characteristics of the Series: Indications
| Variable | Total (N = 47) |
|---|---|
| Age (y), md (IQR) | 55.00 (46.00–65.00) |
| (minimum–maximum) | (35.00–74.00) |
| Body mass index (kg/m2), md (IQR) | 23.75 (21.30–26.35) |
| (minimum–maximum) | (20.00–36.00) |
| missing, n (%) | 3 (6.4) |
| Type of operation, n (%) | |
| Tissue expander to dorsal | 15 (31.9) |
| Prosthesis to dorsal | 32 (68.1) |
| Radiotherapy before, n (%) | |
| Yes | 1 (23.4) |
| No | 36 (76.6) |
| Indications, n (%) | |
| Prosthesis rupture | 9 (19.1) |
| Pain | 19 (40.4) |
| Patient desire | 19 (40.4) |
| G Baker III | 7 (14.9) |
| G Baker II | 3 (6.4) |
| G Baker I | 9 (19,1) |
%, relative frequency; G, grade; IQR, interquartile range (percentiles 25th–75th); md, median; n, absolute frequency.
Indications for implant removal included cases with implant ruptures (nine cases) or disabling pain (19 cases). The other 19 patients underwent operation by personal desire: seven cases of Baker grade III capsular contracture, three cases of grade II, and nine cases of grade I were observed in this group (Table 1). Some patients experienced significant breast-implant-associated discomfort, spontaneously or during pectoral muscle mobilization. Implant removal was an option in cases of asymmetry of the opposite breast that developed over time. It was also an option for patients with expanders and a small contralateral breast who did not want to augment the opposite breast through prosthesis, which is necessary to ensure symmetry.
The mean ± standard deviation (SD) volume of the removed implant was 348.66 ± 86.54 mL. The mean ± SD volume of fat injected was 284.13 ± 62.94 mL. In 14 out of 37 cases, a symmetry procedure on the contralateral side was performed in the same operation as the lipofilled mini dorsi flap. There were seven cases of removal of breast augmentation prostheses, three cases of mastopexy, and four cases of reduced mammoplasty of more than 150 g. In general, the mean ± SD duration of the procedure was 108.93 ± 17.65 minutes, ranging from 74.00 to 146.00 minutes. The shortest duration of the procedure was in cases without operation on the contralateral breast (mean ± SD, 104.07 ± 16.42 minutes; ranging from 74.00 to 145.00 minutes), while the maximum time was in cases with contralateral operation of breast reduction (≥150 g) (mean ± SD, 134.00 ± 8.98 min; ranging from 125.00 to 146.00 min) (Table 2).
Table 2.
Characteristics of the Series: Operation
| Variable | Total (N = 47) |
|---|---|
| Size of implant (g), mean ± SD | 348.66 ± 86.54 |
| (minimum–maximum) | (90.00–515.00) |
| Missing, n (%) | 6 (12.8) |
| LPF total (g), mean ± SD | 284.13 ± 62.94 |
| (minimum–maximum) | (160.00–490.00) |
| Contralateral operation, n (%) | |
| No | 33 (70.2) |
| Prosthesis removal | 7 (14.9) |
| Mastopexy and breast reduction (<150 g) | 3 (6.4) |
| Breast reduction (≥150 g) | 4 (8.5) |
| Operative time (min) | |
| General operative time, mean ± SD | 108.93 ± 17.65 |
| (minimum–maximum) | (74.00–146.00) |
| Missing, n (%) | 4 (8.5) |
| No contralateral operation, mean ± SD | 104.07 ± 16.42 |
| (minimum–maximum) | (74.00–145.00) |
| Missing, n (%) | 3 (9.1) |
| Contralateral operation prosthesis removal, mean ± SD | 114.71 ± 12.93 |
| (minimum–maximum) | (95.00–138.00) |
| Contralateral operation mastopexy or breast reduction (<150 g), md (IQR) | 111.50 (95.00–128.00) |
| (minimum–maximum) | (95.00–128.00) |
| Missing, n (%) | 1 (33.3) |
| Contralateral operation breast reduction (≥150 g), mean ± SD | 134.00 ± 8.98 |
| (minimum–maximum) | (125.00–146.00) |
%, relative frequency; IQR, interquartile range (percentiles 25th–75th); LPF, liposuctioned fat; md, median; n, absolute frequency; SD, standard deviation.
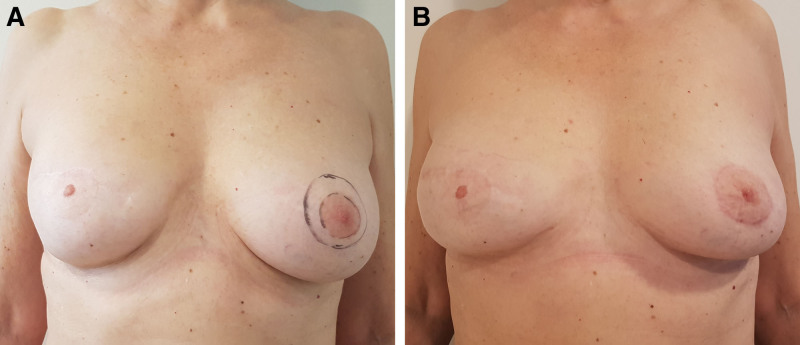
Minimal pain was observed at the postoperative follow-up. Arm abduction, which is at least at 90 degrees right after operation, was on average fully recovered within a month. Depending on the degree of complications of the case and the demands of the patients, one to three additional lipofilling sessions were performed in 25 cases (53.2%) (Table 3). Normally, breast reconstruction aims to obtain good symmetry with the opposite breast. In analyzing a total of 47 cases, 40 of them (85%) reached the desired symmetry as the result of one or two procedures. The other 22 cases (46.8%) presented good symmetry immediately keeping a stable result after a minimum period of 3 months. In cases with a previous augmentation of the opposite breast, the contralateral implant was removed. In 18 (38.3%) cases, a second lipofilling session was needed, most of which had underwent previous radiotherapy. Areolar reconstruction was performed when required (Fig. 2).
Table 3.
Additional Operations
| Variable | Total (N = 47) |
|---|---|
| No. operations, n (%) | |
| 1 | 22 (46.8) |
| 2 | 18 (38.3) |
| 3 | 5 (10.6) |
| 4 | 2 (4.3) |
%, relative frequency; n, absolute frequency,.
Fig. 2.
Lipofilled mini dorsi flap after expander on nonradiated chest wall, in two stages: (A) before and (B) after in the frontal view.
In cases of hypertrophy or ptosis on the contralateral side, reduction mammoplasties or mastopexies had to be performed. These procedures produced no complications that required further operation. No flap necrosis, hematoma, postoperative pulmonary symptoms, or infection was noted. During postoperative monitoring, a moderate seroma was often found with a median (IQR) volume of 70.00 (50.00–100.00) mL and was consequently drained.
In terms of cosmetic results, pain, functional impact, and consistency of reconstruction, a significant improvement was observed when comparing the lipofilled mini dorsi flap cases to breast implants cases. Thirty patients (63.8%) assessed their cosmetic results with a prosthesis as insufficient or average, while 38 patients (80.8%) assessed theirs as good or very good after the lipofilling mini dorsi flap procedure. The pain felt with the breast implant [median (IQR), 4.50 (2.00–6.00)] had practically disappeared with the lipofilled mini dorsi flap [median (IQR), 1.00 (1.00–2.00)]. Functional capacity was also improved through the lipofilled mini dorsi flap procedure (median [IQR] minimal discomfort at the dorsal area was 6.00 [4.00–6.00], while at the breast implant placement, it was 4.00 [3.00–5.00]). In 41 cases (87.2%), the consistency of the reconstructed breast was hard or firm using breast implants, whereas it was soft in 34 cases (72.3%) through the lipofilled mini dorsi flap (Table 4).
Table 4.
Patient Evaluation
| Variable | Implant (N = 47) | Dorsal (N = 47) | * P |
|---|---|---|---|
| Cosmetic result, n (%) | |||
| Insufficient | 7 (14.9) | 0 (0.0) | ≤0.0001 |
| Average | 23 (48.9) | 4 (8.5) | |
| Good | 11 (23.4) | 20 (42.6) | |
| Very good | 1 (2.1) | 18 (38.3) | |
| Missing | 5 (10.6) | 5 (10.6) | |
| Pain, md (IQR) | 4.50 (2.00–6.00) | 1.00 (1.00–2.00) | ≤0.0001 |
| (minimum–maximum) | (1.00–10.00) | (1.00–5.00) | |
| Missing, n (%) | 5 (10.6) | 5 (10.6) | |
| Functional discomfort, md (IQR) | 4.00 (3.00–5.00) | 6.00 (4.00–6.00) | ≤0.0001 |
| (minimum–maximum) | (2.00–6.00) | (2.00–6.00) | |
| Missing, n (%) | 5 (10.6) | 5 (10.6) | |
| Consistency of reconstruction, n (%) | |||
| Hard | 27 (57.4) | 0 (0.0) | ≤0.0001 |
| Firm | 14 (29.8) | 8 (17.0) | |
| Soft | 1 (2.1) | 34 (72.3) | |
| Missing | 5 (10.6) | 5 (10.6) | |
*Chi-squared test with adjusted residual analysis or Mann–Whitney test. Significance set at 5%.
Bold numbers indicate association between categories.
%, relative frequency; IQR, interquartile range (percentiles 25th–75th); md, median; n, absolute frequency; p, statistical index of significance.
The surgical team evaluated the results as very satisfactory in 32 (68.1%) cases, with an average result in 15 (31.9%) cases and an unsatisfactory result in zero (0.0%) cases. Patients felt that they had regained a real breast in a total of 42 cases (89.4%). Forty-two (89.4%) patients would do it again and 41 (87.2%) patients would recommend this technique to another patient (Table 5).
Table 5.
Patient and Surgeon Satisfaction
| Variable | Total (N = 47) |
|---|---|
| Surgeon impression, n (%) | |
| Good | 15 (31.9) |
| Very good | 32 (68.1) |
| Sense of a real breast, n (%) | |
| No | 0 (0.0) |
| Yes | 42 (89.4) |
| Missing | 5 (10.6) |
| Do it again? n (%) | |
| No | 0 (0.0) |
| Yes | 42 (89.4) |
| missing | 5 (10.6) |
| Do you recommend it? n (%) | |
| Yes | 41 (87.2) |
| No | 6 (12.8) |
| Missing | 0 (0.0) |
%, relative frequency; n, absolute frequency.
DISCUSSION
In our experience, the lipofilled mini dorsi flap technique is perfectly adapted to convert breast implant reconstruction into natural breast reconstruction. Patients frequently want a natural-looking breast, possibly identical to their previous one, with no size augmentation. This trend has been reinforced by the strong media coverage of the complications associated with breast implants, such as capsular contracture, rupture, and silicone leakage. The poly implant prostheses scandal triggered widespread misgivings on the safety of breast implants.10,11 Finally, the risk of breast implant-associated anaplastic large cell lymphoma, which received extensive media coverage in France at the beginning of 2019, and the subsequent ban on texturized implants, has had a truly stressful impact on patients with texturized implants, and has deterred others who were eligible for breast implant reconstruction.12–16
The lipofilled mini dorsi flap technique is a good option in this context. Our study indicated an improvement in patients’ quality of life (cosmetic results, postoperative pain, and functional capacity), and all results were assessed as good or very good by the surgical team. Given that this is an autologous reconstruction, the outcome should remain stable over time, whereas the satisfaction rate for breast implants in the long run is only 60%.17–20
We also observed an absence of complications due to minimal detachment and the partial removal of the latissimus dorsi, with volume provided by lipofilling. The lipofilled mini dorsi flap technique is minimally invasive compared to traditional latissimus dorsi reconstruction or the transverse rectus abdominis musculocutaneous flap.21–26 This technique is reliable (0% failure in our series), reproducible, and quickly performed (average duration is 108 minutes) compared with microsurgery.27–30 Substitution of the breast implant through several sessions of lipofilling is a worthwhile option for patients with the right body shape and sufficient motivation to undergo several operations.31,32
Iterative breast implant reconstruction (with capsulectomy in the case of capsular contracture) is a simpler option than the lipofilled mini dorsi flap technique, but exposes patients to more severe early complications (infection or exposure to the prosthesis), leading to reconstruction failure in addition to the usual later complications,33,34 particularly after radiotherapy.35-37 After the conversion of breast implants, only two patients were irradiated due to cancer recurrence in this study. This number of patients was limited and did not permit our team to evaluate the clinical effects of this procedure. The lipofilled mini dorsi flap can be irradiated, and this has been subject to other publications on immediate reconstruction.4
Compared with breast implants, lipofilled mini dorsi flap reconstruction has the advantage of being performed in the prepectoral position. This is beneficial for patients who no longer feel discomfort when contracting the chest muscles, which is a disadvantage for retropectoral prostheses.38,39 The lipofilled mini dorsi flap is softer and more flexible than breast implants, which can give patients the impression that they have regained a “real breast,” and not the mere volume provided by a breast implant. The newly reconstructed breast was more natural and softer to touch. This explains the high degree of patient satisfaction.
The use of a dermal matrix to cover the breast implant has been proposed by surgical teams. This appears to be an interesting option, particularly for repositioning the breast implant in front of the chest muscle.17,40 However, the high cost of this procedure is a limiting factor in the French national health system.
CONCLUSIONS
According to our experience, the lipofilled mini dorsi flap technique is the primary choice for breast implant replacement (silicone or expander) in breast reconstruction. Our study showed excellent patient tolerance and high-level satisfaction with the cosmetic outcome, associated with less pain, improved functional capacity, and the impression of having regained a realistic, soft, and natural breast. The lipofilled mini dorsi flap is a straightforward and autologous solution to replace artificial prostheses, which is in line with patients’ current preferences.
ACKNOWLEDGMENTS
We would like to warmly thank Mr. Charles Francisco Ferreira for the data statistical processing. We would like to thank Editage (www.editage.com) for English language editing.
Footnotes
Published online 25 July 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Ho Quoc C, Delay E. Reconstruction mammaire après mastectomie [breast reconstruction after mastectomy]. J Gynecol Obstet Biol Reprod. 2013;42:29–39. [DOI] [PubMed] [Google Scholar]
- 2.Coriddi M, Shenaq D, Kenworthy E, et al. Autologous breast reconstruction after failed implant-based reconstruction: evaluation of surgical and patient-reported outcomes and quality of life. Plast Reconstr Surg. 2019;143:373–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clemens MW, Brody GS, Mahabir RC, et al. How to diagnose and treat breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg. 2018;141:586e–599e. [DOI] [PubMed] [Google Scholar]
- 4.Piat JM, Tomazzoni G, Giovinazzo V, et al. Lipofilled mini dorsi flap: an efficient less invasive concept for immediate breast reconstruction. Ann Plast Surg. 2020;85:369–375. [DOI] [PubMed] [Google Scholar]
- 5.Ho Quoc C, Carrabin N, Meruta A, et al. [Lipofilling and breast cancer: literature review in 2015?]. J Gynecol Obstet Biol Reprod (Paris). 2015;44:812–817. [DOI] [PubMed] [Google Scholar]
- 6.Ho Quoc C, Dias LPN, Braghiroli OFM, et al. Oncological safety of lipofilling in healthy BRCA carriers after bilateral prophylactic mastectomy: a case series. Eur J Breast Health. 2019;15:217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ho Quoc C, Taupin T, Guérin N, et al. Volumetric evaluation of fat resorption after breast lipofilling. Ann Chir Plast Esthet. 2015;60:495–499. [DOI] [PubMed] [Google Scholar]
- 8.Ho Quoc C, Piat JM, Carrabin N, et al. Breast reconstruction with fat grafting and BRAVA pre-expansion: efficacy evaluation in 45 cases. Ann Chir Plast Esthet. 2016;61:183–189. [DOI] [PubMed] [Google Scholar]
- 9.Brondi RS, de Oliveira VM, Bagnoli F, et al. Autologous breast reconstruction with the latissimus dorsi muscle with immediate fat grafting: long-term results and patient satisfaction. Ann Plast Surg. 2019;82:152–157. [DOI] [PubMed] [Google Scholar]
- 10.Greco C. The poly implant prothèse breast prostheses scandal: embodied risk and social suffering. Soc Sci Med. 2015;147:150–157. [DOI] [PubMed] [Google Scholar]
- 11.Fenoll C, Leclère FM, Hivelin M, et al. [Poly Implant Prothèse (PIP) incidence of complications in breast reconstructive surgery: a retrospective comparative analysis]. Ann Chir Plast Esthet. 2015;60:478–483. [DOI] [PubMed] [Google Scholar]
- 12.Clemens MW, Nava MB, Rocco N, et al. Understanding rare adverse sequelae of breast implants: anaplastic large-cell lymphoma, late seromas, and double capsules. Gland Surg. 2017;6:169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nava MB, Adams WP, Jr, Botti G, et al. MBN 2016 aesthetic breast meeting BIA-ALCL consensus conference report. Plast Reconstr Surg. 2018;141:40–48. [DOI] [PubMed] [Google Scholar]
- 14.Jaffe ES, Ashar BS, Clemens MW, et al. Best practices guideline for the pathologic diagnosis of breast implant-associated anaplastic large-cell lymphoma. J Clin Oncol. 2020;38:1102–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cardoso MJ, Wyld L, Rubio IT, et al. EUSOMA position regarding breast implant associated anaplastic large cell lymphoma (BIA-ALCL) and the use of textured implants. Breast. 2019;44:90–93. [DOI] [PubMed] [Google Scholar]
- 16.Collett DJ, Rakhorst H, Lennox P, et al. Current risk estimate of breast implant-associated anaplastic large cell lymphoma in textured breast implants. Plast Reconstr Surg. 2019;143:30S–40S. [DOI] [PubMed] [Google Scholar]
- 17.Potter S, Conroy EJ, Cutress RI, et al. ; iBRA Steering Group; Breast Reconstruction Research Collaborative. Short-term safety outcomes of mastectomy and immediate implant-based breast reconstruction with and without mesh (iBRA): a multicentre, prospective cohort study. Lancet Oncol. 2019;20:254–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fracon S, Renzi N, Manara M, et al. Patient satisfaction after breast reconstruction: implants vs. autologous tissues. Acta Chir Plast. 2018;59:120–128. [PubMed] [Google Scholar]
- 19.Reinders FCJ, Young-Afat DA, Batenburg MCT, et al. Higher reconstruction failure and less patient-reported satisfaction after post mastectomy radiotherapy with immediate implant-based breast reconstruction compared to immediate autologous breast reconstruction. Breast Cancer. 2020;27:435–444. [DOI] [PubMed] [Google Scholar]
- 20.Colohan S, Wong C, Lakhiani C, et al. The free descending branch muscle-sparing latissimus dorsi flap: vascular anatomy and clinical applications. Plast Reconstr Surg. 2012;130:776e–787e. [DOI] [PubMed] [Google Scholar]
- 21.Saint-Cyr M, Nagarkar P, Schaverien M, et al. The pedicled descending branch muscle-sparing latissimus dorsi flap for breast reconstruction. Plast Reconstr Surg. 2009;123:13–24. [DOI] [PubMed] [Google Scholar]
- 22.Sowa Y, Numajiri T, Nakatsukasa K, et al. Comparison of morbidity-related seroma formation following conventional latissimus dorsi flap versus muscle-sparing latissimus dorsi flap breast reconstruction. Ann Surg Treat Res. 2017;93:119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim H, Wiraatmadja ES, Lim SY, et al. Comparison of morbidity of donor site following pedicled muscle-sparing latissimus dorsi flap versus extended latissimus dorsi flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2013;66:640–646. [DOI] [PubMed] [Google Scholar]
- 24.Massenburg BB, Sanati-Mehrizy P, Ingargiola MJ, et al. Flap failure and wound complications in autologous breast reconstruction: a national perspective. Aesthetic Plast Surg. 2015;39:902–909. [DOI] [PubMed] [Google Scholar]
- 25.Berthet G, Faure C, Dammacco MA, et al. Tolerance of latissimus dorsi in immediate breast reconstruction without implant to radiotherapy. J Plast Reconstr Aesthet Surg. 2018;71:15–20. [DOI] [PubMed] [Google Scholar]
- 26.Adams WP, Jr, Lipschitz AH, Ansari M, et al. Functional donor site morbidity following latissimus dorsi muscle flap transfer. Ann Plast Surg. 2004;53:6–11. [DOI] [PubMed] [Google Scholar]
- 27.Bennett KG, Qi J, Kim HM, et al. Comparison of 2-year complication rates among common techniques for postmastectomy breast reconstruction. JAMA Surg. 2018;153:901–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramelli E, Ruffenach L, Bruant-Rodier C, et al. [Surgical revision in case of DIEP failure in breast reconstruction]. Ann Chir Plast Esthet. 2019;64:320–325. [DOI] [PubMed] [Google Scholar]
- 29.Seidenstuecker K, van Waes C, Munder BI, et al. DIEAP flap for safe definitive autologous breast reconstruction. Breast. 2016;26:59–66. [DOI] [PubMed] [Google Scholar]
- 30.Ochoa O, Garza R, III, Pisano S, et al. Prospective longitudinal patient-reported satisfaction and health-related quality of life following DIEP flap breast reconstruction: relationship with body mass index. Plast Reconstr Surg. 2019;143:1589–1600. [DOI] [PubMed] [Google Scholar]
- 31.Kellou K, Lequesne J, Georgescu D, et al. [Limitations of breast reconstruction using exclusive lipofilling: a retrospective study over 10 years]. Gynecol Obstet Fertil Senol. 2019;47:347–351. [DOI] [PubMed] [Google Scholar]
- 32.Kronowitz SJ, Mandujano CC, Liu J, et al. Lipofilling of the breast does not increase the risk of recurrence of breast cancer: a matched controlled study. Plast Reconstr Surg. 2016;137:385–393. [DOI] [PubMed] [Google Scholar]
- 33.Riggio E, Toffoli E, Tartaglione C, et al. Local safety of immediate reconstruction during primary treatment of breast cancer. Direct-to-implant versus expander-based surgery. J Plast Reconstr Aesthet Surg. 2019;72:232–242. [DOI] [PubMed] [Google Scholar]
- 34.Frey JD, Choi M, Salibian AA, et al. Comparison of outcomes with tissue expander, immediate implant, and autologous breast reconstruction in greater than 1000 nipple-sparing mastectomies. Plast Reconstr Surg. 2017;139:1300–1310. [DOI] [PubMed] [Google Scholar]
- 35.Lee KT, Mun GH. Prosthetic breast reconstruction in previously irradiated breasts: a meta-analysis. J Surg Oncol. 2015;112:468–475. [DOI] [PubMed] [Google Scholar]
- 36.Spear SL, Boehmler JH, Bogue DP, et al. Options in reconstructing the irradiated breast. Plast Reconstr Surg. 2008;122:379–388. [DOI] [PubMed] [Google Scholar]
- 37.Bachour Y, Oei LJ, Van der Veen AJ, et al. The influence of radiotherapy on the mechanical properties of silicone breast implants. Plast Reconstr Surg Glob Open. 2018;6:e1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vidya R, Tafazal H, Salem F, et al. Management based on grading of animation deformity following implant-based subpectoral breast reconstruction. Arch Plast Surg. 2018;45:185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eck DL, Nguyen DC, Barnes LL, et al. Treatment of breast animation deformity in implant-based reconstruction with selective nerve ablation. Aesthetic Plast Surg. 2018;42:1472–1475. [DOI] [PubMed] [Google Scholar]
- 40.Sobti N, Ji E, Brown RL, et al. Evaluation of acellular dermal matrix efficacy in prosthesis-based breast reconstruction. Plast Reconstr Surg. 2018;141:541–549. [DOI] [PubMed] [Google Scholar]