Abstract
Introduction
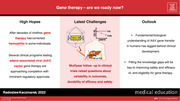
Haemophilia therapy has evolved from rudimentary transfusion‐based approaches to an unprecedented level of innovation with glimmers of functional cure brought by gene therapy. After decades of misfires, gene therapy has normalized factor (F)VIII and factor (F)IX levels in some individuals in the long term. Several clinical programmes testing adeno‐associated viral (AAV) vector gene therapy are approaching completion with imminent regulatory approvals.
Discussion
Phase 3 studies along with multiyear follow‐up in earlier phase investigations raised questions about efficacy as well as short‐ and long‐term safety, prompting a reappraisal of AAV vector gene therapy. Liver toxicities, albeit mostly low‐grade, occur in the first year in at least some individuals in all haemophilia A and B trials and are poorly understood. Extreme variability and unpredictability of outcome, as well as a slow decline in factor expression (seemingly unique to FVIII gene therapy), are vexing because immune responses to AAV vectors preclude repeat dosing, which could increase suboptimal or restore declining expression, while overexpression may result in phenotoxicity. The long‐term safety will need lifelong monitoring because AAV vectors, contrary to conventional wisdom, integrate into chromosomes at the rate that calls for vigilance.
Conclusions
AAV transduction and transgene expression engage the host immune system, cellular DNA processing, transcription and translation machineries in ways that have been only cursorily studied in the clinic. Delineating those mechanisms will be key to finding mitigants and solutions to the remaining problems, and including individuals who cannot avail of gene therapy at this time.
Keywords: AAV, cure, gene therapy, genotoxicity, haemophilia, liver toxicity
1. HAEMOPHILIA THERAPY: FROM EVOLUTION TO REVOLUTION
Haemophilia A and B are caused by deficiencies of coagulation factor VIII (FVIII) and factor IX (FIX), respectively. Haemophilia therapy has gone a long way since its humble beginnings. Most of that journey led to better ways of replacing the missing factor through incremental improvements in transfusion medicine, biochemistry and molecular biology. In 1840, Samuel Lane made the earliest successful attempt at treating symptoms of hemophilia. 1 The treatment was whole blood and it continued to be the only remotely effective therapy until the 1920s when plasma transfusion was first used to control bleeding, but it did not become a common practice until the 1950s. The efficacy of plasma transfusions was still limited because bleeding control required high volumes, running the risk of circulatory overload. Two major technological breakthroughs secured a foothold for more meaningful progress. The first one was the successful isolation of albumin by cold ethanol precipitation in the 1940s by Edwin Cohn, providing the proof of concept that one could isolate therapeutic proteins from plasma on a large scale. 2 The next major milestone was the discovery that a cold precipitate that forms following the slow thaw of frozen plasma contains high factor FVIII activity. 3 This cryoprecipitate could be easily separated from the rest of the plasma and infused from a closed‐bag system, which enabled local preparation and significantly reduced infusion volume, permitting administration of higher doses of FVIII without overloading the patients with fluids. Importantly, cryoprecipitation was able to be integrated into the plasma fractionation workflow. This, together with a number of chromatographic protein purification techniques that came along, allowed for efficient isolation of multiple plasma proteins in the form of concentrates, including FVIII and FIX, which could be freeze dried, stored in a refrigerator and used at home. The two seminal processes, cold ethanol fractionation and cryoprecipitation are still used in modern plasma fractionation. 4
Refinements in the chromatographic purification techniques produced an array of FVIII and FIX clotting factor concentrates, whose purity increased over time from < 1% of total protein to ∼99% purity by the end of 1980s. 5
Inadvertently, large‐scale manufacture from plasma pools, including plasma from as many as over a hundred thousand individuals and the widespread use of clotting factor concentrates, facilitated the spread of hepatitis B and C, and human immunodeficiency viruses (HBV, HCV and HIV), which altogether took lives of many thousands of individuals in the haemophilia community. 6 The catastrophe stymied the adoption of prophylaxis and conditioned the patients for many years to feel that danger was lying in wait.
The generation of high‐purity FVIII and FIX concentrates was pivotal for cloning the F8 and F9 genes in 1984 and 1982, respectively. 7 , 8 , 9 , 10 , 11 , 12 Efforts were well afoot to that end and intensified when the HIV disaster unfolded, which substantiated the urgent need to develop safer treatment products, leading to regulatory approvals of the first recombinant FVIII and FIX products in 1992 and 1997, respectively. Also, the successful cloning and expression of the F8 and F9 genes raised the prospect of ultimately designing a functional cure for haemophilia in the form of gene therapy.
In the 1990s and 2000s, growing access to safe recombinant and plasma‐derived clotting factor concentrates, which had largely rebuilt trust with the community thanks to the unblemished viral safety record since the introduction of viral reduction measures in the manufacture, prompted a reappraisal of prophylaxis in recognition of the unmet need for better bleeding protection. 13 Prophylaxis has improved outcomes and become a standard of care in children, but did so at the cost of increased treatment burden and fell short of eliminating all joint damage. Peaks and troughs in factor levels mean that patients still spend a considerable amount of time at factor levels that are incapable of preventing all spontaneous or subclinical bleeds. The 2010s ushered into the market a wave of extended half‐life (EHL) clotting factor concentrates that have facilitated prophylaxis by affording fewer infusions and higher troughs, especially for patients with haemophilia B. 14 The same decade also saw a number of non‐factor therapies enter the clinic, one of which, the bispecific antibody emicizumab, has already been commercialized and improved outcomes in patients with and without inhibitors, which are currently the most serious complication of treatment. 15 All or most of these new treatments offer easier (subcutaneous) and less frequent administration, and for the first time break the paradigm of seesaw pharmacokinetics, representing a molecular revolution in tapping into the coagulation system to restore hemostasis. 16 However, they have vastly different mechanisms of action, do not normalize hemostasis and cannot be measured using the legacy assays that have long been established in the factor replacement therapy. 17 Thus, the pursuit of better modalities and, ultimately, a cure have persisted.
2. HOPES AND LETDOWNS IN GENE THERAPY FOR HEMOPHILIA
The last decade also saw the first evidence that gene therapy for haemophilia A and B has the potential to normalize factor levels in the long term due to several adeno‐associated viral (AAV) vector gene therapy programs making some headway. The path toward that point has been long, winding and littered with roadblocks. The concept of gene therapy emerged 50 years ago. 18 The idea of using a virus as a gene transfer tool was born soon after when Terheggen and coworkers made an attempt to correct arginase deficiency by intravenous administration of the Shope papillomavirus into three hyperargininemic patients. 19 , 20 They failed, but the idea remained attractive and several years after the F8 and F9 had been cloned, the nascent field of haemophilia gene therapy was using retroviral vectors for successful gene transfer in primary human cell lines that were then implanted into small and large laboratory animals. 21 , 22 , 23 , 24 Some of those early experiments produced long‐term but low‐level expression in the animals, or vice versa. Yet, the results were reassuring enough to continue testing several viral vectors throughout most of the 1990s. Systemically administered adenoviral vectors produced transient therapeutic and supratherapeutic levels of factors for weeks and months in mice and dogs, but immune responses were limiting the duration of expression and precluded repeat administrations. 25 , 26 , 27
Advance to the clinic became tangible when the prototypical AAV2 vector induced stable FIX expression upon intramuscular or intraportal injection in mice, and subsequently in dogs with haemophilia B. 28 , 29 , 30 , 31 , 32 , 33 Although AAV looked like a favourite to enter clinical trials, the first human gene therapy study evaluated a non‐viral approach by implanting autologous fibroblasts transfected with the FVIII gene into omentum, closely followed by a trial that systemically delivered a retroviral vector encoding FVIII. 34 , 35 , 36 Both misfired, producing transient factor level increases within the moderate haemophilia range in some participants. 37 , 38 Two AAV2 haemophilia B trials followed, using the vectors that showed promise in mice and dogs, one injecting the vector in the muscle, the other in the portal vein. 39 , 40 In the muscle trial, FIX levels were stable but subtherapeutic, whereas in the liver trial the levels were therapeutic but transient. 41 , 42 One more flop occurred, when a study injecting an adenoviral vector encoding FVIII saw a modest and transient FVIII increase with liver enzyme elevations in the first individual, and the whole field went back to the drawing board. 37 For AAV, which still looked like the safest and most promising vector, the first clinical failures identified obstacles that had not been seen in the preclinical animal studies. Expression in the muscle seemed safe but saturable, which made the dose escalation impractical and necessitated dozens of intramuscular injections to achieve detectable factor levels. Expression in the liver rose to appreciable 10–12% but dropped to baseline within 10 weeks and the decline was accompanied by transaminitis. 43 The apparent liver toxicity of AAV was disheartening because of the prevalence of liver disease in the community. Thus, although hepatocyte was known to be the natural cellular source of FIX, these worries kept the interest in other targets alive. In subsequent studies, biopsies from a muscle‐dosed individual showed that transgene expression could last in humans for many years. 42 On the liver front, it turned out that expression loss and transaminitis resulted from cytotoxic cellular immune responses targeting AAV capsid antigens presented by transduced hepatocytes, showing that the problem could be druggable. 41 , 44 Also, in favour of the liver, animal studies suggested that hepatocyte FIX gene transfer could induce immune tolerance toward FIX. 45 , 46 Importantly, the gamut of AAV serotypes that could be used to target haemophilia was growing. 47
3. NEW HOPES AND OLD (AND NEW) WORRIES
In 2010, after several years of hiatus, gene therapy for haemophilia returned to the clinic with a verve, when several haemophilia B patients received AAV8‐FIX, and whose FIX expression was rescued with a course of corticosteroids when their transaminases started to rise. 48 This pioneering effort has informed a slew of subsequent trials evaluating AAV vectors encoding FIX or FVIII. 16 , 49 They all administer AAV vectors targeting the liver in a single bolus intravenous injection. The initial haemophilia B studies delivered transgenes encoding wild‐type FIX and saw FIX increases within moderate and lower mild ranges. 50 , 51 Better results came with the inclusion of the hyperactive Padua variant FIX, which harbours a single amino acid substitution and has since been used in all leading haemophilia B trials. 52 , 53 The change revs up FIX activity 5‐10‐fold, affording higher FIX levels without increasing the vector dose. Thus, the same vector doses as those used in wild‐type FIX trials boosted the achieved FIX increases to upper mild and normal FIX ranges. 54 , 55 , 56
The same team that ushered haemophilia B gene therapy back into the clinic designed several AAV vectors encoding B domain‐deleted (BDD) FVIII, one of which was selected for clinical development and became BMN 270 in 2014, now in Phase 3. 57 , 58 , 59 , 60 It was the first clinical trial that achieved normal FVIII levels in some individuals, and several other studies soon followed having similar success with different vectors. 61 , 62 , 63 , 64 Four clinical programs have advanced to Phase 3 with some early phase studies having multiyear data. 57 , 62 , 65 , 66
After decades of disappointments, the first gene therapies for haemophilia A and B are nearing commercialization, and thus the long‐awaited cure has come within reach but not for everyone. Data from larger groups of patients enrolled in Phase 3 studies have substantiated several concerns about variability, the durability of efficacy, and safety that emerged at earlier stages. In all trials, FVIII and FIX expression is highly variable, to the point that means and medians poorly represent levels achieved by individuals, from no response at all to moderate increase to levels across mild haemophilia and normal ranges, and far above the upper limit of normal. 61 , 67 , 68 , 69 Most individuals show elevations of liver enzymes, particularly alanine aminotransferase (ALT). These elevations are the most common, albeit asymptomatic, adverse event, typically managed with corticosteroids (as in the original 2010 trial) and other forms of immunosuppression. They are generally considered mild and transient, 1‐3‐fold above the upper limit of normal, but in some participants went up as high as 10–20 times over the upper limit of normal or persisted for months and as long as over a year. In haemophilia B trials, some but not all of these cases correlate with cytotoxic T cell response toward capsid proteins and they variably respond to immunosuppression. Haemophilia A studies rarely found evidence of immunotoxicity and responses to immunosuppression are even less consistent. Yet, in haemophilia A individuals, ALT seems to rise more often and be somewhat dose‐dependent. In a Phase 3 study of valoctocogene roxaparvovec (BMN 270) administering the largest vector dose in the field (6e13 vg/kg), 115 out of 134 dosed individuals had ALT elevations, 106 of whom received corticosteroids, and 39 other immunosuppression. 69 The durability of efficacy has been clearly different between FVIII and FIX studies. For FIX, transgene expression has been durable. Participants of the original 2010 trial have maintained stable FIX expression and more recent trials using FIX‐Padua AAV constructs seem to be following the same pattern. 70 In contrast, FVIII levels continue to decline and after 5 years have dropped five‐fold from the mean 57.7 (median 47.8) to 11.6 (8.2) IU/dL (measured with chromogenic substrate assay) in the longest‐running FVIII trial. 58 , 71
The causes of transaminase elevations, extreme expression variability and long‐term decline remain unclear. Some expression variability is expected due to the mechanism of gene therapy. Unlike protein biologics, manufacture of which can be fine‐tuned outside the body in bioreactors, biosynthesis of the same molecules upon gene transfer requires that the vector reaches the target cell, enters the cytoplasm, traffics to the nucleus, uncoats its genetic payload, which then undergoes complex reassembly to permit transcription and translation of the transgene product, which then goes through multiple maturation steps before it exits the cell to perform its function. Each of these steps may depend on individual sets of genetic and environmental factors. Some of these steps might be regulable with existing pharmaceuticals, which could partially reduce the variability of expression but probably not eliminate it. 72 Although the vast majority of individuals have shown reduced bleeding rates and remained off replacement therapy, this variability is concerning because factor level is the key determinant in the success of gene therapy, while individual outcomes are unpredictable and nonadjustable. 73 Universal development of high‐titre and cross‐reactive anti‐AAV antibodies, which can persist for at least 15 years, precludes repeat dosing in patients with suboptimal response, even with other serotypes. 74 , 75 Potential solutions, such as plasma‐exchange or proteolytic antibody depletion are at early stages of development or difficult to integrate in routine practice. Conversely, patients on the other side of the variability spectrum are faced with the risk of phenotoxicity insofar that supraphysiological factor levels may lead to thrombosis. High factor levels prompted the recent pause of a FVIII gene therapy program and prophylactic anticoagulation in some individuals as well as acute anticoagulation in a participant of a FIX gene therapy trial. 76 , 77 , 78 This issue also begets discussion of the ‘right’ target factor level (or range) for gene therapy. One train of thought maintains that gene therapy should aspire to cure and the cure is factor level in the normal range (50‐150%). The teleological justification would be that evolution favoured the FVIII 50–150% range because we need it to prevent any bleeding whatsoever. However, teleological arguments are not necessarily correct and supporters of targeting subnormal levels lament the loss of cardioprotective effect with higher expression and point to the elimination of joint bleeds seen at levels over ∼15%. 79 , 80 , 81 Bleeding rates observed in the gene therapy studies to date have supported the latter view.
Since the seminal discovery of cytotoxic T cell‐mediated killing of transduced hepatocytes, nonclinical research on immune responses to AAV gene therapy has painted a much more complex picture, elements of which have already manifested in the clinic pointing to potential mitigants. 41 , 44 , 82 Toll‐like receptor 9 (TLR9)‐mediated sensing of vector DNA cargo has emerged as a key mechanism triggering immunotoxicity and expression loss. 83 , 84 , 85 TLR9 is an innate immune sensor of unmethylated CpG sequences in DNA, which are a pathogen‐associated molecular pattern (PAMP). The most advanced clinical programs stripped their vectors of those elements, but the latest three failed trials inadvertently enriched their DNA constructs in CpG sequences leading to FIX expression loss within three months from dosing that could not be rescued with immunosuppression. Removal of CpG sequences from non‐coding elements of the expression cassette, such as promoters and inverted‐terminal repeats (ITRs), is difficult. The remainder potentially contributes to residual immunogenicity of otherwise CpG‐depleted constructs, manifesting as transaminase elevations that variably respond to immunosuppression and correlate with vector dose. 84 , 86 , 87 , 88 Additional causes of these elevations, such as vector impurities (e.g. empty or defective capsids, encapsidated extraneous DNA, adventitious agents) have not been ruled out. 89 , 90 , 91 AAV transduction is an extremely inefficient process, with ∼99% of vector perishing in the cellular garbage disposal pathways before settling in the nucleus. 72 , 92 , 93 Excess empty capsids could further burden the already strained mechanism. 90 The discontinued study of BAX 335 suggested that interleukin‐6 receptor (IL‐6R) is a promising target for AAV immunotoxicity mitigation. 83 , 84 Non‐clinical research has identified several other targets that may be fertile for clinical translation, including interleukin‐1 (IL‐1), interleukin‐6 (IL‐6), type I interferon, CD40‐CD40L co‐stimulation and the mammalian target of rapamycin (mTOR). 82 , 94 , 95
In FVIII trials, presumably nonimmune transaminase elevations and the relatively slow (multiyear) decline of FVIII levels may originate from unique challenges of the FVIII biosynthesis and FVIII AAV vectorology. Unlike FIX, FVIII is primarily produced by the liver sinusoidal endothelial cells (LSECs), not by hepatocytes. 96 Yet, AAV vectors encoding FVIII target hepatocytes, and thus FVIII transgene expression is ectopic. FVIII is a large and complex glycoprotein, notoriously difficult to express in heterologous cells even compared to other similarly sized and structured proteins, the reasons of which are incompletely understood. Several bottlenecks have been proposed to explain the poor FVIII expression, including transcription‐repressing elements in the F8 gene, tendency to misfold, aggregate and degrade, the requirement for specific receptor complex (lectin, mannose binding 1/multiple coagulation factor deficiency protein 2, or LMAN1‐MCFD2) to traverse the cellular secretory pathway and poor stability in the absence of von Willebrand factor (VWF). 97 , 98 Misfolded FVIII activates unfolded protein response, which can lead to cellular stress and death. 99 , 100 FVIII tolerates engineering within the B domain (which is naturally excised during activation anyway), removal of which has improved expression and permitted inclusion in AAV transgene cassettes, producing constructs of ∼5 kb as compared to > 7 kb for the full‐length FVIII. 101 However, BDD‐FVIII transgenes still exceed the optimal AAV capsid packaging limit. Vector packaging efficiency dramatically drops with transgene extension beyond 4.7 kb, which results in a mixture that consists mostly of vectors harbouring truncated cassettes. 102 , 103 Some fragmented AAV undergo repair in the nucleus and may be assembled into functional monomeric and concatemeric circular episomes by the cellular DNA processing machinery, which is essential for the establishment of persistent transgene expression. 104 , 105 , 106 , 107 , 108 However, this form of gene transfer results in extra loss of transgene from the administered vector dose and adds to the already tall order of managing a sudden influx of hundreds of thousands of vector particles per hepatocyte, the impact of which is unknown. Thus, FVIII gene therapy is a compromise between transgene cassette size and vector dose necessary to induce meaningful transgene expression.
4. REDUCING UNCERTAINTY
The causes and mitigants of wide variability, waning efficacy (for haemophilia A) and liver toxicity have not been sufficiently studied, and thus the advance of gene therapies toward commercialization has outpaced our fundamental biological understanding of AAV gene transfer in humans (Table 1). This will need to be rectified to ensure safety and the best possible outcomes at the current state of the art. Minimizing AAV ‘wastage’ throughout its journey to the nucleus and improving factor expression could lower vector doses by logs, thus potentially further reducing toxicities. The dose is likely critical as toxicities grow in frequency and severity with increased vector dosing, and in gene therapy for other conditions that delivered vector doses exceeding e14 vg/kg (higher than in any haemophilia study) included complement activation, cytopaenias and severe hepatotoxicity, likely representing part of the continuum of clinical immune responses. More transparency and data sharing as well as timely publication of animal and clinical data, including negative results, would help find solutions. Failed studies may offer important learnings as exemplified by the recent publication of the discontinued BAX 335 program. 84 Liver biopsies at different time points after vector dosing will be critical to understanding AAV gene transfer biology in humans. Also, the field needs standardization. For instance, clinical trials use two types of assays to measure pre‐existing immunity to AAV vectors: ELISA‐based total antibody assay and transduction inhibition assay, neither of which has been standardized. This is more obvious and troubling for the transduction inhibition assay because the results determine anti‐AAV neutralizing antibody titres and eligibility for gene therapy. Clinical trials have used vastly different assay conditions (if reported at all), making the results incomparable across the field. For example, different multiplicities of infection (MOI) that have been used by one haemophilia A and one haemophilia B trial could produce over ∼60‐fold different titres for the same vector (assuming all other conditions were the same). Vector production and purification may add to the variation because inactive viral particles may lead to underestimated antibody titres. Nevertheless, vector dose and serum volume are some of the key parameters of the transduction inhibition assay and changes in reporting these would bring some clarity. One way of minimizing the variation could be to report the presence of transduction inhibitors as the number of AAV particles that are neutralized per volume of serum instead of neutralizing antibody titers. 109 Another assay issue concerns discrepancies between one‐stage (OSA) and chromogenic substrate assays (CSA) when measuring transgene‐expressed factor levels. OSA overestimates coagulation in FVIII gene therapy by ∼1.6‐fold because transgene‐expressed BDD‐FVIII speeds up early activation of factor X but does not increase overall thrombin generation, so CSA seems more reliable. 110 , 111 Discrepancies have also emerged in FIX trials, but these appear to be inherent to FIX‐Padua enhanced kinetics and unrelated to in vivo transgene expression. 112 , 113 , 114
TABLE 1.
Key challenges facing AAV‐mediated gene therapy for haemophilia
| Efficacy | Safety |
|---|---|
|
|
| Related research questions requiring further study |
|---|
|
The long‐term safety of AAV gene therapy for haemophilia has so far been favourable both in the clinic and large animal models but needs continued attention. 115 , 116 , 117 , 118 AAV have long been misperceived as non‐integrating vectors due to the formation of episomes and the low rate of chromosomal integration estimated between .1 and 1.0%. However, in absolute terms, this may still result in millions of integration events in the liver with vector doses ranging from trillions to quadrillions (e12‐e15) of particles, raising questions about genotoxicity and oncogenicity risks. 119 , 120 Although the evidence of risk is limited to neonatal or liver‐damaged rodents, it merits vigilance and long‐term, preferably lifelong monitoring of gene therapy recipients. 120 , 121 , 122 , 123 , 124 Comprehensive genetic analysis of hepatocellular carcinoma (HCC) recently found in a FIX gene therapy trial participant found no evidence that gene transfer caused the malignancy, but integration events were found in .027% of cells in the tumour sample, confirming that integrations do occur. 125 Importantly, despite their hepatotropism and liver‐specific expression AAV vectors may transduce other tissues, so monitoring should be geared toward detecting other potential toxicities. 126 , 127 A framework of known unknowns has been proposed to organize thinking around the short‐ and long‐term safety, and help address the uncertainties. 119 Hopefully, the growing attention and calls to action on these matters will galvanize the field to pursue answers. 120 , 128 , 129 , 130
5. CHASING THE DREAM OF GENE THERAPY
Gene therapy has long held the promise of the ultimate cure that would provide lifelong haemophilia correction upon a single intervention. Does the state of the art match the dream? It might for some because haemophilia B individuals continue to have stable factor levels for years. For haemophilia A, the ‘cure’ appears temporary. Despite imperfections, first market approvals are imminent. Several subgroups in the community are missing out on the opportunity altogether, including females, children, patients with current or past inhibitors, and, most of all, individuals with preexisting anti‐AAV immunity. Globally, 85% of people with haemophilia may not have ready access to gene therapy based on the current price estimations, while it would offer the only viable solution for those living in resource‐limited jurisdictions without immediate prospects for improvement. 131 , 132 , 133 , 134 , 135 Future nonclinical, clinical and organizational efforts should aspire to include those long underserved and underprivileged groups. As a new technology, gene therapy presents unique challenges for healthcare providers who will be introducing and delivering it to the patients. Initiatives toward formulating principles and providing guidance are afoot. 136 , 137 , 138 , 139 AAV gene therapy has proven itself as a powerful platform for therapeutic gene transfer, as evidenced by almost 150 clinical trials registered to date and several regulatory approvals, but it has room for improvement and will continue to evolve. 140 , 141 , 142 Due diligence in addressing uncertainties will be paramount for the haemophilia community, who have endured a difficult safety legacy and failed hopes.
Ideal gene therapy for haemophilia will be the endpoint of the perennial struggle to close the gap between how much haemostatic correction a therapy can provide and how much is needed to live a life independent from treatment. The current state of the art brings us remarkably close to that goal, but actually getting there will take more time and innovation.
CONFLICTS OF INTEREST
RK conceived of and wrote the manuscript. RK received research funding from Bayer Hemophilia Awards Program.
Kaczmarek R. Gene therapy – are we ready now? Haemophilia. 2022;28(Suppl. 4):35–43. 10.1111/hae.14530
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- 1. Lane S. Haemorrhagic diathesis. Successful transfusion of blood. Lancet. 1840;35(896):185‐188. [Google Scholar]
- 2. Cohn EJ, Strong LE, Hughes WL, et al. Preparation and properties of serum and plasma proteins; a system for the separation into fractions of the protein and lipoprotein components of biological tissues and fluids. J Am Chem Soc. 1946;68(3):459‐475. [DOI] [PubMed] [Google Scholar]
- 3. Pool JG, Hershgold EJ. High potency anti‐haemophilic factor prepared from cryoglobulin precipitate. Nat Publ Gr. 1964;203:312. [DOI] [PubMed] [Google Scholar]
- 4. Burnouf T. Modern plasma fractionation. Transfus Med Rev. 2007;21(2):101‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burnouf T. An overview of plasma fractionation. Ann Blood. 2018;3:33‐33. [Google Scholar]
- 6. Evatt BL. The tragic history of AIDS in the hemophilia population, 1982–1984. J Thromb Haemost. 2006;4(11):2295‐2301. [DOI] [PubMed] [Google Scholar]
- 7. Ling G, Tuddenham EGD. Factor VIII: the protein, cloning its gene, synthetic factor and now – 35 years later – gene therapy; what happened in between?. Br J Haematol. 2020;189(3):400‐407. [DOI] [PubMed] [Google Scholar]
- 8. Choo KH, Gould KG, Rees DJG, Brownlee GG, Molecular cloning of the gene for human anti‐haemophilic factor IX. Nat. 1982;299(5879):178‐180. [DOI] [PubMed] [Google Scholar]
- 9. Toole JJ, Knopf JL, Wozney JM, et al. Molecular cloning of a cDNA encoding human antihaemophilic factor. Nat. 1984;312(5992):342‐347. [DOI] [PubMed] [Google Scholar]
- 10. Gitschier J, Wood WI, Goralka TM, et al. Characterization of the human factor VIII gene. Nat. 1984;312(5992):326‐330. [DOI] [PubMed] [Google Scholar]
- 11. Vehar GA, Keyt B, Eaton D, et al. Structure of human factor VIII. Nature. 1984;312(5992):337‐342. [DOI] [PubMed] [Google Scholar]
- 12. Wood WI, Capon DJ, Simonsen CC, et al. Expression of active human factor VIII from recombinant DNA clones. Nat. 1984;312(5992):330‐337. [DOI] [PubMed] [Google Scholar]
- 13. Manco‐Johnson MJ, Abshire TC, Shapiro AD, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med. 2007;357(6):535‐544. [DOI] [PubMed] [Google Scholar]
- 14. Von Mackensen S, Kalnins W, Krucker J, et al. Haemophilia patients’ unmet needs and their expectations of the new extended half‐life factor concentrates. Haemophilia. 2017;23(4):566‐574. [DOI] [PubMed] [Google Scholar]
- 15. Callaghan MU, Negrier C, Paz‐Priel I, et al. Long‐term outcomes with emicizumab prophylaxis for hemophilia A with or without FVIII inhibitors from the HAVEN 1–4 studies. Blood. 2021;137(16):2231‐2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Butterfield JSS, Hege KM, Herzog RW, Kaczmarek R. A Molecular Revolution in the Treatment of Hemophilia. Mol Ther. 2020;28(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Peyvandi F, Kenet G, Pekrul I, et al. Laboratory testing in hemophilia: impact of factor and non‐factor replacement therapy on coagulation assays. J Thromb Haemost. 2020:0‐2. [DOI] [PubMed] [Google Scholar]
- 18. Wirth T, Parker N, Ylä‐Herttuala S. History of gene therapy. Gene. 2013;525(2):162‐169. [DOI] [PubMed] [Google Scholar]
- 19. Terheggen HG, Lowenthal A, Lavinha F, et al. Unsuccessful trial of gene replacement in arginase deficiency. Z Kinderheilkd. 1975;119(1):1‐3. [DOI] [PubMed] [Google Scholar]
- 20. Rogers S, Lowenthal A, Terheggen HG, Columbo JP. Induction of arginase activity with the Shope papilloma virus in tissue culture cells from an argininemic patient. J Exp Med. 1973;137(4):1091‐1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Palmer Td, Thompson Ar, Miller Ad. Production of human factor IX in animals by genetically modified skin fibroblasts: potential therapy for hemophilia B. Blood. 1989;73(2):438‐445. [PubMed] [Google Scholar]
- 22. Hoeben RC, Van Der Jagt RC, Schoute F, et al. Expression of functional factor VIII in primary human skin fibroblasts after retrovirus‐mediated gene transfer. J Biol Chem. 1990;265(13):7318‐7323. [PubMed] [Google Scholar]
- 23. Dwarki VJ, Belloni P, Nijjar T, et al. Gene therapy for hemophilia A: production of therapeutic levels of human factor VIII in vivo in mice. Proc Natl Acad Sci U S A. 1995;92(4):1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kay MA, Rothenberg S, Landen CN, et al. In vivo gene therapy of hemophilia B: sustained partial correction in factor IX‐deficient dogs. Science (80‐). 1993;262(5130):117‐119. [DOI] [PubMed] [Google Scholar]
- 25. Walter J, You Q, Hagstrom JN, Sands M, High KA. Successful expression of human factor IX following repeat administration of adenoviral vector in mice. Proc Natl Acad Sci U S A. 1996;93(7):3056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kay MA, Landen CN, Rothenberg SR, et al. In vivo hepatic gene therapy: complete albeit transient correction of factor IX deficiency in hemophilia B dogs. Proc Natl Acad Sci U S A. 1994;91(6):2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Connelly S, Gardner Jm, Lyons Rm, Mcclelland A, Kaleko M. Sustained expression of therapeutic levels of human factor VIII in mice. Blood. 1996;87(11):4671‐4677. [PubMed] [Google Scholar]
- 28. Herzog RW, Hagstrom JN, Kung S‐H, et al. Stable gene transfer and expression of human blood coagulation factor IX after intramuscular injection of recombinant adeno‐associated virus. Proc Natl Acad Sci U S A. 1997;94(11):5804‐5809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Herzog RW, Yang EY, Couto LB, et al. Long‐term correction of canine hemophilia B by gene transfer of blood coagulation factor IX mediated by adeno‐associated viral vector. Nat Med. 1999;5(1):56‐63. [DOI] [PubMed] [Google Scholar]
- 30. Snyder RO, Miao C, Meuse L, et al. Correction of hemophilia B in canine and murine models using recombinant adeno‐associated viral vectors. Nat Med. 1999;5(1):64‐70. [DOI] [PubMed] [Google Scholar]
- 31. Snyder RO, Miao CH, Patijn GA, et al. Persistent and therapeutic concentrations of human factor IX in mice after hepatic gene transfer of recombinant AAV vectors. Nat Genet. 1997;16(3):270‐276. [DOI] [PubMed] [Google Scholar]
- 32. Linden RM, Woo SLC. AAVant‐garde gene therapy. Nat Med. 1999;5(1):21‐22. [DOI] [PubMed] [Google Scholar]
- 33. Trials and tribulations. Nat Genet. 2000;24(3):201‐202. [DOI] [PubMed] [Google Scholar]
- 34. Roth DA, Tawa NE, O'brien JM, Treco DA, Selden RF. Nonviral transfer of the gene encoding coagulation factor VIII in patients with severe hemophilia A. N Engl J Med. 2001;344(23):1735‐1742. [DOI] [PubMed] [Google Scholar]
- 35. Powell JS, Ragni MV, White GC, et al. Phase 1 trial of FVIII gene transfer for severe hemophilia A using a retroviral construct administered by peripheral intravenous infusion. Blood. 2003;102(6):2038‐2045. [DOI] [PubMed] [Google Scholar]
- 36. White GC, Roberts HR. Gene Therapy for Hemophilia: a Step Closer to Reality. Mol Ther. 2000;1(3):207‐208. [DOI] [PubMed] [Google Scholar]
- 37. Nathwani AC, Davidoff AM, Tuddenham EGD. Prospects for gene therapy of haemophilia. Haemophilia. 2004;10(4):309‐318. [DOI] [PubMed] [Google Scholar]
- 38. Pierce GF. Uncertainty in an era of transformative therapy for haemophilia: addressing the unknowns. Haemophilia. 2021;27(S3):103‐113. [DOI] [PubMed] [Google Scholar]
- 39. Kay MA, Manno CS, Ragni MV, et al. Evidence for gene transfer and expression of factor IX in haemophilia B patients treated with an AAV vector. Nat Genet. 2000;24(3):257‐261. [DOI] [PubMed] [Google Scholar]
- 40. Manno CS, Chew AJ, Hutchison S, et al. AAV‐mediated factor IX gene transfer to skeletal muscle in patients with severe hemophilia B. Blood. 2003;101(8):2963‐2972. [DOI] [PubMed] [Google Scholar]
- 41. Manno CS, Pierce GF, Arruda VR, et al. Successful transduction of liver in hemophilia by AAV‐Factor IX and limitations imposed by the host immune response. Nat Med. 2006;12(3):342‐347. [DOI] [PubMed] [Google Scholar]
- 42. Jiang H, Pierce GF, Ozelo MC, et al. Evidence of multiyear factor IX expression by AAV‐mediated gene transfer to skeletal muscle in an individual with severe hemophilia B. Mol Ther. 2006;14(3):452‐455. [DOI] [PubMed] [Google Scholar]
- 43. High K. Gene transfer for hemophilia: can therapeutic efficacy in large animals be safely translated to patients?. J Thromb Haemost. 2005;3(8):1682‐1691. [DOI] [PubMed] [Google Scholar]
- 44. Mingozzi F, Maus MV, Hui DJ, et al. CD8(+) T‐cell responses to adeno‐associated virus capsid in humans. Nat Med. 2007;13(4):419‐422. [DOI] [PubMed] [Google Scholar]
- 45. Mingozzi F, Liu Yi‐L, Dobrzynski E, et al. Induction of immune tolerance to coagulation factor IX antigen by in vivo hepatic gene transfer. J Clin Invest. 2003;111(9):1347‐1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dobrzynski E, Fitzgerald JC, Cao O, Mingozzi F, Wang L, Herzog RW. Prevention of cytotoxic T lymphocyte responses to factor IX‐expressing hepatocytes by gene transfer‐induced regulatory T cells. Proc Natl Acad Sci U S A. 2006;103(12):4592‐4597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jiang H, Lillicrap D, Patarroyo‐White S, et al. Multiyear therapeutic benefit of AAV serotypes 2, 6, and 8 delivering factor VIII to hemophilia A mice and dogs. Blood. 2006;108(1):107‐115. [DOI] [PubMed] [Google Scholar]
- 48. Nathwani AC, Tuddenham EGD, Rangarajan S, et al. Adenovirus‐associated virus vector‐mediated gene transfer in hemophilia B. N Engl J Med. 2011;365(25):2357‐2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Perrin GQ, Herzog RW, Markusic DM. Update on clinical gene therapy for hemophilia. Blood. 2019;133(5):407‐414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Nathwani AC, Reiss UM, Tuddenham EGD, et al. Long‐Term Safety and Efficacy of Factor IX Gene Therapy in Hemophilia B. N Engl J Med. 2014;371(21):1994‐2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Miesbach W, Meijer K, Coppens M, et al. Gene therapy with adeno‐associated virus vector 5‐human factor IX in adults with hemophilia B. Blood. 2018;131(9):1022‐1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Simioni P, Tormene D, Tognin G, et al. X‐Linked Thrombophilia with a Mutant Factor IX (Factor IX Padua). N Engl J Med. 2009;361(17):1671‐1675. [DOI] [PubMed] [Google Scholar]
- 53. Chang J, Jin J, Lollar P, et al. Changing residue 338 in human factor IX from arginine to alanine causes an increase in catalytic activity. J Biol Chem. 1998;273(20):12089‐12094. [DOI] [PubMed] [Google Scholar]
- 54. George LA, Sullivan SK, Rasko JEJ, et al. Efficacy and Safety in 15 Hemophilia B Patients Treated with the AAV Gene Therapy Vector Fidanacogene Elaparvovec and Followed for at Least 1 Year. Blood. 2019;134(1):3347‐3347. [Google Scholar]
- 55. Chowdary P, Shapiro S, Makris M, et al. A Novel Adeno Associated Virus (AAV) Gene Therapy (FLT180a) Achieves Normal FIX Activity Levels in Severe Hemophilia B (HB) Patients (B‐AMAZE Study). ISTH 2020 Congress Abstracts.
- 56. Von DA, A G, Castaman G, et al. Etranacogene dezaparvovec (AMT‐061 phase 2b): normal/near normal FIX activity and bleed cessation in hemophilia B. Blood Adv. 2019;3(21):3241‐3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pasi KJ, Rangarajan S, Mitchell N, et al. Multiyear follow‐up of aav5‐hfviii‐sq gene therapy for hemophilia a. N Engl J Med. 2020;382(1):29‐40. [DOI] [PubMed] [Google Scholar]
- 58. Rangarajan S, Walsh L, Lester W, et al. AAV5–Factor VIII Gene Transfer in Severe Hemophilia A. N Engl J Med. 2017;377(26):2519‐2530. [DOI] [PubMed] [Google Scholar]
- 59.BioMarin Announces Selection of Factor VIII Gene Therapy Drug Development Candidate BMN 270 for the Treatment of Hemophilia A. 1/13/2014. https://investors.biomarin.com/2014‐01‐13‐BioMarin‐Announces‐Selection‐of‐Factor‐VIII‐Gene‐Therapy‐Drug‐Development‐Candidate‐BMN‐270‐for‐the‐Treatment‐of‐Hemophilia‐A
- 60. High KH, Nathwani A, Spencer T, Lillicrap D. Current status of haemophilia gene therapy. Haemophilia. 2014;20 Suppl 4(S4):43‐49. [DOI] [PubMed] [Google Scholar]
- 61. George L, Eyster E, Ragni M, et al. Phase I/II Trial of SPK‐8011: Stable and Durable FVIII Expression After AAV Gene Transfer for Hemophilia A ‐ ISTH 2020 Congress Abstracts.
- 62. George LA, Monahan PE, Eyster ME, et al. Multiyear Factor VIII Expression after AAV Gene Transfer for Hemophilia A. N Engl J Med. 2021;385(21):1961‐1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Nathwani AC, Tuddenham E, Chowdary P, et al. GO‐8: preliminary Results of a Phase I/II Dose Escalation Trial of Gene Therapy for Haemophilia a Using a Novel Human Factor VIII Variant. Blood. 2018;132(1):489‐489. [Google Scholar]
- 64. Pipe SW, Ferrante F, Reis M, et al. First‐in‐Human Gene Therapy Study of AAVhu37 Capsid Vector Technology in Severe Hemophilia A ‐ BAY 2599023 has Broad Patient Eligibility and Stable and Sustained Long‐Term Expression of FVIII. Blood. 2020;136(1):44‐45. [Google Scholar]
- 65. Lisowski L, Staber JM, Wright JF, Valentino LA. The intersection of vector biology, gene therapy, and hemophilia. Research and Practice in Thrombosis and Haemostasis. 2021(February):1‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. George LA, Sullivan SK, Giermasz A, et al. Hemophilia B Gene Therapy with a High‐Specific‐Activity Factor IX Variant. N Engl J Med. 2017;377(23):2215‐2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Pipe SW, Leebeek FW, Recht M, et al. 52 Week Efficacy and Safety of Etranacogene Dezaparvovec in Adults with Severe or Moderate‐severe Hemophilia B: Data from the Phase 3 HOPE‐B Gene Therapy Trial ‐ ISTH 2021 Congress Abstracts.
- 68. Leebeek FW, Miesbach W, Recht M, et al. Clinical Outcomes in Adults with Hemophilia B with and without Pre‐existing Neutralizing Antibodies to AAV5: 6 Month Data from the Phase 3 Etranacogene Dezaparvovec HOPE‐B Gene Therapy Trial ‐ ISTH 2021 Congress Abstracts.
- 69. Ozelo MC, Mahlangu J, Pasi KJ, et al. Efficacy and Safety of Valoctocogene Roxaparvovec Adeno‐associated Virus Gene Transfer for Severe Hemophilia A: Results from the Phase 3 GENEr8‐1 Trial ‐ ISTH 2021 Congress Abstracts.
- 70. Nathwani AC. Gene therapy for hemophilia. Hematology. 2019;2019(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Pasi KJ, Rangarajan S, Robinson TM, et al. Hemostatic Response is Maintained for up to 5 Years Following Treatment with Valoctocogene Roxaparvovec, an AAV5‐hFVIII‐SQ Gene Therapy for Severe Hemophilia A ‐ ISTH 2021 Congress Abstracts.
- 72. Dhungel BP, Bailey CG, Rasko JEJ. Journey to the Center of the Cell: tracing the Path of AAV Transduction. Trends Mol Med. 2020;27(2):1‐13. [DOI] [PubMed] [Google Scholar]
- 73. Iorio A, Skinner MW, Clearfield E, et al. Core outcome set for gene therapy in haemophilia: results of the coreHEM multistakeholder project. Haemophilia. 2018;24(4):e167‐72. [DOI] [PubMed] [Google Scholar]
- 74. Fitzpatrick Z, Leborgne C, Barbon E, et al. Influence of Pre‐existing Anti‐capsid Neutralizing and Binding Antibodies on AAV Vector Transduction. Mol Ther Methods Clin Dev. 2018;9:119‐129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Leborgne C, Barbon E, Alexander JM, et al. IgG‐cleaving endopeptidase enables in vivo gene therapy in the presence of anti‐AAV neutralizing antibodies. Nat Med 2020 267. 2020;26(7):1096‐1101. [DOI] [PubMed] [Google Scholar]
- 76. https://www.hemophilia.org/news/fda‐places‐the‐pfizersangamo‐therapeutics‐phase‐3‐affine‐haemophilia‐a‐gene‐therapy‐study‐on‐clinical‐hold
- 77. https://chscontact.ca/dangerously‐high‐fix‐levels‐reported‐in‐hemophilia‐b‐gene‐therapy
- 78. Kaczmarek R, Herzog RW. Treatment‐induced hemophilic thrombosis?. Mol Ther. 2022;30(2):505‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Makris M. Gene therapy 1·0 in haemophilia: effective and safe, but with many uncertainties. Lancet Haematol. 2020;7(3):e186‐88. [DOI] [PubMed] [Google Scholar]
- 80.den Uijl IEM, Mauser Bunschoten EP, Roosendaal G, et al. Clinical severity of haemophilia A: does the classification of the 1950s still stand?. Haemophilia. 2011;17(6):849‐853. [DOI] [PubMed] [Google Scholar]
- 81. Van Der Valk P, Makris M, Fischer K, et al. Reduced cardiovascular morbidity in patients with hemophilia: results of a 5‐year multinational prospective study. Blood Adv. 2022;6(3):902‐908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Shirley JL, De Jong YP, Terhorst C, Herzog RW. Immune Responses to Viral Gene Therapy Vectors. Mol Ther. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. George LA. No CpGs for AAVs?. Blood. 2021;137(6):721‐723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Konkle BA, Walsh CE, Escobar MA, et al. BAX 335 hemophilia B gene therapy clinical trial results: potential impact of CpG sequences on gene expression. Blood. 2021;137(6):763‐774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Wright JF. Codon Modification and PAMPs in Clinical AAV Vectors: the Tortoise or the Hare?. Mol Ther. 2020;28(3):701‐703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Wright JF. Quantification of CpG Motifs in rAAV Genomes: avoiding the Toll. Mol Ther. 2020;28(8):1756‐1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Ronzitti G, Gross DA, Mingozzi F. Human Immune Responses to Adeno‐Associated Virus (AAV) Vectors. Front Immunol. 2020;11(April):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Verdera HC, Kuranda K, Mingozzi F. AAV Vector Immunogenicity in Humans : a Long Journey to Successful Gene Transfer. Mol Ther. 2020;28(3):723‐746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Kotin RM, Wright JF. Recombinant Adeno‐Associated Virus Quality Control for Non‐Clinical and Clinical Vectors: how an Unregulated Commercial Sector Can Compromise Development of New Gene Therapies. Hum Gene Ther. 2019;30(12):1447‐1448. [DOI] [PubMed] [Google Scholar]
- 90. Wright JF. Quality Control Testing, Characterization and Critical Quality Attributes of Adeno‐Associated Virus Vectors Used for Human Gene Therapy. Biotechnol J. 2021;16(1). [DOI] [PubMed] [Google Scholar]
- 91. Kaczmarek R. Do adventitious viruses carried by insect cell lines producing AAV vectors pose a safety risk in gene therapy?. Haemophilia. 2018;24(6):843‐844. [DOI] [PubMed] [Google Scholar]
- 92. Grimm D, Pandey K, Nakai H, Storm TA, Kay MA. Liver transduction with recombinant adeno‐associated virus is primarily restricted by capsid serotype not vector genotype. J Virol. 2006;80(1):426‐439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Vincent‐Lacaze N, Snyder RO, Gluzman Ré, Bohl D, Lagarde C, Danos O. Structure of adeno‐associated virus vector DNA following transduction of the skeletal muscle. J Virol. 1999;73(3):1949‐1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Shirley JL, Keeler GD, Sherman A, et al. Type I Interferon Sensing by Conventional Dendritic Cells and CD4+ T Help are both Requisite for Cross‐priming of AAV Capsid‐specific CD8+ T Cells. Mol Ther. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Rogers GL, Shirley JL, Zolotukhin I, et al. Plasmacytoid and conventional dendritic cells cooperate in crosspriming AAV capsid‐specific CD8+ T cells. Blood. 2017;129(24):3184‐3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Shahani T, Covens K, Lavend'homme R, et al. Human liver sinusoidal endothelial cells but not hepatocytes contain factor VIII. J Thromb Haemost. 2014;12(1):36‐42. [DOI] [PubMed] [Google Scholar]
- 97. Kumar SR. Industrial production of clotting factors: challenges of expression, and choice of host cells. Biotechnol J. 2015;10(7):995‐1004. [DOI] [PubMed] [Google Scholar]
- 98. Zhang B, Kaufman RJ, Ginsburg D. LMAN1 and MCFD2 form a cargo receptor complex and interact with coagulation factor VIII in the early secretory pathway. J Biol Chem. 2005;280(27):25881‐25886. [DOI] [PubMed] [Google Scholar]
- 99. Malhotra JD, Miao H, Zhang K, et al. Antioxidants reduce endoplasmic reticulum stress and improve protein secretion. Proc Natl Acad Sci U S A. 2008;105(47):18525‐18530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Poothong J, Pottekat A, Siirin M, et al. Factor VIII exhibits chaperone‐dependent and glucose‐regulated reversible amyloid formation in the endoplasmic reticulum. Blood. 2020;135(21):1899‐1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Sandberg H, Almstedt A, Brandt J, et al. Structural and functional characteristics of the B‐domain‐deleted recombinant factor VIII protein, r‐VIII SQ. Thromb Haemost. 2001;85(1):93‐100. [PubMed] [Google Scholar]
- 102. Dong B, Nakai H, Xiao W. Characterization of genome integrity for oversized recombinant AAV vector. Mol Ther. 2010;18(1):87‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Kyostio‐Moore S, Berthelette P, Piraino S, et al. The impact of minimally oversized adeno‐associated viral vectors encoding human factor VIII on vector potency in vivo. Mol Ther ‐ Methods Clin Dev. 2016;3:16006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Penaud‐Budloo M, Le Guiner C, Nowrouzi A, et al. Adeno‐associated virus vector genomes persist as episomal chromatin in primate muscle. J Virol. 2008;82(16):7875‐7885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Nakai H, Yant SR, Storm TA, Fuess S, Meuse L, Kay MA. Extrachromosomal recombinant adeno‐associated virus vector genomes are primarily responsible for stable liver transduction in vivo. J Virol. 2001;75(15):6969‐6976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Duan D, Sharma P, Yang J, et al. Circular intermediates of recombinant adeno‐associated virus have defined structural characteristics responsible for long‐term episomal persistence in muscle tissue. J Virol. 1998;72(11):8568‐8577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Hirsch ML, Agbandje‐Mckenna M, Jude Samulski R. Little vector, big gene transduction: fragmented genome reassembly of adeno‐associated virus. Mol Ther. 2010;18(1):6‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Hirsch ML, Wolf SJ, Samulski RJ. Delivering Transgenic DNA Exceeding the Carrying Capacity of AAV Vectors. Methods Mol Biol. 2016;1382:21‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Weber T. Anti‐AAV Antibodies in AAV Gene Therapy: current Challenges and Possible Solutions. Front Immunol. 2021;12(March):1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Rosen S, Tiefenbacher S, Robinson M, et al. Activity of transgene‐produced B‐domain‐deleted factor VIII in human plasma following AAV5 gene therapy. Blood. 2020;136(22):2524‐2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Ragni M. Gene‐produced FVIII: measure for measure. Blood. 2020;136(22):2483‐2484. [DOI] [PubMed] [Google Scholar]
- 112. Robinson MM, George LA, Carr ME, et al. Factor IX assay discrepancies in the setting of liver gene therapy using a hyperfunctional variant factor IX‐Padua. J Thromb Haemost. 2021;19(5):1212‐1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Samelson‐Jones BJ, Finn JD, Raffini LJ, et al. Evolutionary insights into coagulation factor IX Padua and other high‐specific‐activity variants. Blood Adv. 2021;5(5):1324‐1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Samelson‐Jones BJ, Finn JD, George LA, Camire RM, Arruda VR. Hyperactivity of factor IX Padua (R338L) depends on factor VIIIa cofactor activity. JCI Insight. 2019;4(14). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Batty P, Rimmer E, Brown C, et al. Long Term Safety and Efficacy of Adeno‐associated Viral Gene Therapy in a Canine Hemophilia A Model. ISTH Congress; 2019. [Google Scholar]
- 116. Batty P, Lillicrap D. Gene therapy for hemophilia : current status and laboratory consequences. Int J Lab Hematol [Internet]. 2021;43(April):117‐123. [DOI] [PubMed] [Google Scholar]
- 117. Nguyen GN, Everett JK, Kafle S, et al. A long‐term study of AAV gene therapy in dogs with hemophilia A identifies clonal expansions of transduced liver cells. Nat Biotechnol. 2021;39(1):47‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Venditti CP. Safety questions for AAV gene therapy. Nat Biotechnol. 2021;39(1):24‐26. [DOI] [PubMed] [Google Scholar]
- 119. Pierce GF, Iorio A. Past, present and future of haemophilia gene therapy: from vectors and transgenes to known and unknown outcomes. Haemophilia. 2018;24(6):60‐67. Suppl. [DOI] [PubMed] [Google Scholar]
- 120. Kaczmarek R, Pierce GF, Noone D, O'mahony B, Page D, Skinner MW. Eliminating Panglossian thinking in development of AAV therapeutics. Mol Ther. 2021;29(12):3325‐3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Dalwadi DA, Torrens L, Abril‐Fornaguera J, et al. Liver Injury Increases the Incidence of HCC following AAV Gene Therapy in Mice. Mol Ther. 2021;29(2):680‐690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Dalwadi DA, Calabria A, Tiyaboonchai A, et al. AAV integration in human hepatocytes. Mol Ther. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Konkle BA, Recht M, Hilger A, et al. The critical need for postmarketing surveillance in gene therapy for haemophilia. Haemophilia. 2020(March):1‐6. [DOI] [PubMed] [Google Scholar]
- 124. Konkle B, Pierce G, Coffin D, et al. Core data set on safety, efficacy, and durability of hemophilia gene therapy for a global registry: communication from the SSC of the ISTH. J Thromb Haemost. 2020;18(11):3074‐3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liver Safety Case Report from the Phase 3 HOPE‐B Gene Therapy Trial in Adults with Hemophilia B ‐ ISTH Congress Abstracts.
- 126. Hordeaux J, Buza EL, Jeffrey B, et al. MicroRNA‐mediated inhibition of transgene expression reduces dorsal root ganglion toxicity by AAV vectors in primates. Sci Transl Med. 2020;12(569):9188. [DOI] [PubMed] [Google Scholar]
- 127. Mueller C, Berry JD, Mckenna‐Yasek DM, et al. SOD1 Suppression with Adeno‐Associated Virus and MicroRNA in Familial ALS. N Engl J Med. 2020;383(2):151‐158. [DOI] [PubMed] [Google Scholar]
- 128. Pierce GF. Gene therapy for hemophilia: anticipating the unexpected. Blood Adv. 2020;4(15):3788‐3788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Herzog RW, Pierce GF. Liver Gene Therapy: reliable and Durable?. Mol Ther. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Pierce GF, Kaczmarek R, Noone D, O'mahony B, Page D, Skinner MW. Gene therapy to cure haemophilia: is robust scientific inquiry the missing factor?. Haemophilia. 2020;26(6):931‐933. [DOI] [PubMed] [Google Scholar]
- 131. Pierce GF, Coffin D, Lillicrap D, et al. The 1st WFH Gene Therapy Round Table: understanding the landscape and challenges of gene therapy for haemophilia around the world. Haemophilia. 2019;25(2):189‐194. [DOI] [PubMed] [Google Scholar]
- 132. Pierce GF, Pasi KJ, Coffin D, et al. Towards a global multidisciplinary consensus framework on haemophilia gene therapy: report of the 2nd World Federation of Haemophilia Gene Therapy Round Table. Haemophilia. 2020;26(3):443‐449. [DOI] [PubMed] [Google Scholar]
- 133. Ragni M. Royal gene therapy at a royal cost. Blood. 2021;138(18):1645‐1646. [DOI] [PubMed] [Google Scholar]
- 134. Bolous NS, Chen Y, Wang H, et al. The cost‐effectiveness of gene therapy for severe hemophilia B: a microsimulation study from the United States perspective. Blood. 2021;138(18):1677‐1690. [DOI] [PubMed] [Google Scholar]
- 135. Stonebraker JS, Bolton‐Maggs PHB, Brooker M, et al. The World Federation of Hemophilia Annual Global Survey 1999–2018. Haemophilia. 2020;26(4):591‐600. [DOI] [PubMed] [Google Scholar]
- 136. Miesbach W, Pasi KJ, Pipe SW, et al. Evolution of haemophilia integrated care in the era of gene therapy: treatment centre's readiness in United States and EU. Haemophilia. 2021(December 2020):1‐4. [DOI] [PubMed] [Google Scholar]
- 137. Miesbach W, O'Mahony B, Key NS, et al. How to discuss gene therapy for haemophilia? A patient and physician perspective. Haemophilia. 2019;hae.13769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Sidonio RF, Pipe SW, Callaghan MU, Valentino LA, Monahan PE, Croteau SE. Blood Reviews Discussing investigational AAV gene therapy with hemophilia patients : a guide. Blood Rev. 2021;47(November 2020):100759. [DOI] [PubMed] [Google Scholar]
- 139. Pipe SW. Delivering on the promise of gene therapy for haemophilia. Haemophilia. 2021;27(S3):114‐121. Suppl 3. [DOI] [PubMed] [Google Scholar]
- 140. Kuzmin DA, Shutova MV, Johnston NR, et al. The clinical landscape for AAV gene therapies. Nat Rev Drug Discov. 2021;20(3):173‐174. [DOI] [PubMed] [Google Scholar]
- 141. Wang D, Tai PWL, Gao G. Adeno‐associated virus vector as a platform for gene therapy delivery. Nat Rev Drug Discov. 2019;18(5):358‐378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Bulcha JT, Wang Yi, Ma H, Tai PWL, Gao G. Viral vector platforms within the gene therapy landscape. Signal Transduct Target Ther. 2021;6(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


