Abstract
Introduction/Aims
In response to coronavirus disease 2019 (COVID‐19) pandemic restrictions int 2020, our face‐to‐face (F2F) multidisciplinary neuromuscular clinic (NMC) transitioned to widespread use of telehealth (TH). This study aimed to (1) understand parent/guardian, child, and clinician perceptions of TH; (2) examine TH‐related changes in clinical activity; and (3) use these findings to inform a future model of care for the NMC.
Methods
A clinical audit was undertaken to examine clinical activity throughout 2018–2020. Online surveys were distributed to clinicians and parents of children attending the NMC via TH in 2020. A working group of clinicians created a checklist to guide a future hybrid model of TH and F2F care.
Results
Total clinical activity in 2020 was maintained from previous years; 62.8% of all appointments occurred via TH, and 82.3% of patients attended NMC by TH at least once. Ninety‐nine parents (30.6% response rate), 52 children, and 17 clinicians (77% response rate) responded to the survey. All groups reported better interaction when F2F compared to TH. Eighty percent of parents identified advantages of TH and reported lower levels of stress. A lack of “hands‐on” physical assessment was identified by parents and clinicians as a TH limitation. Most families (68.1% of parents; 58.8% of children) and all clinicians indicated a preference for a mix of TH and F2F NMC appointments in the future.
Discussion
This study has informed a checklist to guide future TH use in a new hybrid model of care. Further investigation is required to assess health impacts of TH use in pediatric neuromuscular care.
Keywords: COVID‐19, multidisciplinary, neuromuscular, paediatric, telehealth

Abbreviations
- F2F
face‐to‐face, in person
- NMC
neuromuscular clinic
- TH
telehealth
1. INTRODUCTION
The complex care required for children and adolescents with neuromuscular disorders is typically co‐ordinated in tertiary hospital outpatient clinics in which healthcare clinicians provide high quality multidisciplinary care in line with international recommendations. 1 , 2 , 3 , 4 , 5 , 6 Typically, this care is offered via face‐to‐face (F2F) patient consultations, which are essential for the physical examination and assessments described as best practice.
In response to the coronavirus disease 2019 (COVID‐19) global pandemic, lockdowns and other government‐mandated public health restrictions were used to control disease spread in Australia. Consequently, most healthcare was delivered remotely via telehealth (TH) throughout much of 2020. The shift to TH was consistent with pandemic management in many other countries and was facilitated by increased Australian government funding and the extension of eligibility for TH funding to include metropolitan residents. 7 , 8 , 9 , 10 However, the clinicians and patient families from the neuromuscular clinic (NMC) expressed concerns regarding the quality of care that could be provided via TH.
The use of technology to support patient care is not new, and video‐based TH has been available for use in our center since 2015, albeit with limited uptake prior to the pandemic. There is growing evidence that TH is acceptable to and feasible for adults with neuromuscular disease, and feasible and effective for neurologists managing children with various neurological conditions. 11 , 12 , 13 , 14 , 15 Less is known about TH in pediatric multidisciplinary clinics, including pediatric NMCs. With potential ongoing use of TH post‐pandemic, it is important to explore whether TH is appropriate in a pediatric neuromuscular population and if key stakeholders are satisfied with the care provided in 2020.
The primary aim of this study was to evaluate perceptions of TH use in the NMC from children, parents, and clinicians via an online survey. We hypothesized that families and clinicians would prefer in‐person clinical visits. Secondary aims were to (1) examine TH‐related changes in clinical activity via a clinical audit and (2) use the survey findings to inform a future hybrid model of care for the NMC.
2. METHODS
2.1. Setting
The NMC at The Royal Children's Hospital in Melbourne, Australia, is a weekly multidisciplinary clinic that provides care to 500+ children and adolescents from south‐eastern Australia. Since 2008, children have attended the clinic in‐person where, in a single day, they attend up to eight appointments with various medical, nursing, and allied health clinicians, as well as essential investigations (eg, lung‐function testing, blood tests, x‐rays). Between March and October 2020, only newly diagnosed or unstable patients were seen F2F with most attending NMC via TH. From October 2020 onward, there was a mix of TH and F2F appointments within each NMC.
2.2. Ethics
This project received ethics approval from the Human Research Ethics Committee at The Royal Children's Hospital (HREC 65359). Participants gave consent within the online survey; parents or guardians gave consent for their children to participate.
2.3. Participants
Parents/guardians (hereafter referred to as parents) and their child/ren were eligible to participate if they attended NMC via TH between 11th March and 16th December 2020. Children were eligible to answer a survey if they were aged 8 y or older. Clinicians (neurologists, respiratory physicians, an orthopedic surgeon, a psychiatrist, a genetic counsellor, a clinical nurse specialist, physiotherapists, an occupational therapist, an orthotist, dietitians, and a social worker) and administrators who work in the NMC were also invited to participate.
Families were excluded if they could not be contacted by email.
2.4. Procedures
2.4.1. Surveys
An online survey was used to assess perceptions of TH by key clinic stakeholders. Separate surveys were developed for parents, children, clinicians and NMC administrators and distributed using REDCap (Vanderbilt University), a secure online survey tool hosted by the Murdoch Children's Research Institute.
Survey questions were drafted following plain language principles, reviewed by NMC clinicians for face validity and piloted by members of the research team (n = 5).
Survey questions and a summary of survey contents are provided as Supporting Information File S1 and Table S1, which are available online. Surveys included a combination of multiple choice, sliding scale, and free text responses. Parents and clinicians were asked about the technology, engagement, stress, and value of TH, as well as background information questions to characterize the sample. Children were asked about their feelings and how hard it was to talk to clinicians during TH and F2F appointments, rating items using the Wong‐Baker faces ordinal scale, which scores from happiest face (1) to saddest face (7). 16 All groups were asked about their preferred future model of care.
Surveys were distributed via email. Parents were asked to complete the survey once per child based on their most recent NMC appointment, whereas clinicians were asked to respond based on their clinic experience since commencement of TH use.
Anonymous survey responses were collected and stored electronically using REDCap. The survey was open for 4 months from 22 September 2020 until 23 January 2021.
2.4.2. Audit of NMC scheduling
A clinical audit was conducted from January 2018 to December 2020 inclusive. Information regarding overall annual NMC patient numbers and attendance was extracted from the electronic medical record (number of patients accessing NMC, total number NMC appointments, number of patients attending NMC by TH, number of patients who “did not attend” one or more appointments). Additional information (number of NMC per year, patients scheduled per NMC, total appointments scheduled per NMC) was extracted from the departmental NMC lists. These data were used to determine if TH affected the level of clinical activity.
2.4.3. Developing a future hybrid model of care
A working group of clinicians (the study authors) used the survey findings from parent, child, and clinician groups; clinical audit data; published standards of care and their clinical experience to develop a pilot checklist to guide future allocation of TH and F2F appointments. Draft versions of the checklist were circulated via email to the wider NMC clinical team and edits made until consensus was achieved.
2.5. Analysis
Survey responses (complete and incomplete) were exported to Stata V16 for analysis (StataCorp. 2019. Stata Statistical Software: Release 16.; StataCorp LLC). Descriptive statistics were used to summarize and characterize survey responses. Regional postcode data were entered into the Australian Bureau of Statistics Socio‐economic Indexes for Areas (SEIFA; https://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa) product to describe the socioeconomic spread of parent respondents. SEIFA scores range from 0 to 100, with the higher the score, the higher the socioeconomic background.
Fisher's exact test (two‐sided) was used to test for associations between age, diagnosis, travel time, and preferred future model of care.
3. RESULTS
3.1. TH survey
3.1.1. Survey respondents
The parent/guardian survey was distributed to 323 families of whom 99 answered at least some questions (30.6% response rate). These families came from 75 different postal codes, representing all socioeconomic deciles in the Australian population, although skewed to higher socioeconomic status (median [interquartile range {IQR}] = 68 [42]). Participants were located across the three states serviced by the NMC (predominantly Victoria but also southern New South Wales and Tasmania), including metropolitan, regional, and rural locations. Parents reported a range of diagnoses for their children (Figure 1) and 14% had more than one child attending NMC. The median age of the children was 11 (IQR, 7; range, 2–18) y. Thirty‐five percent of families reported usually traveling for more than 2 h to attend NMC in‐person. The most common reason for TH NMC appointments was routine clinical care (92.4%).
FIGURE 1.
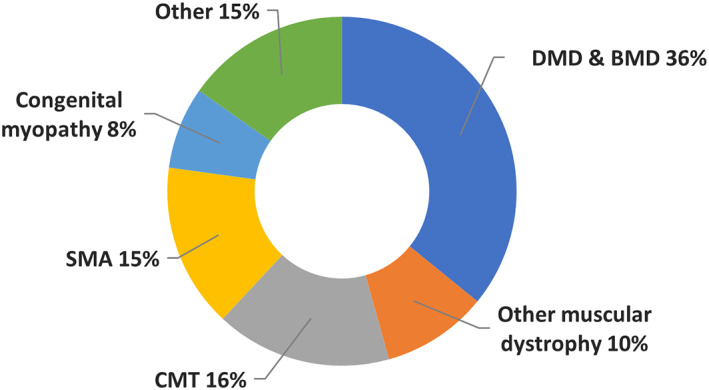
NM diagnoses reported by parents/guardians for their children. DMD, Duchenne muscular dystrophy; BMD, Becker muscular dystrophy; SMA, spinal muscular atrophy; CMT, Charcot–Marie–Tooth disease; “Other” includes myasthenic syndromes, chronic inflammatory demyelinating polyneuropathy (CIDP), undiagnosed, and unspecified; “Other muscular dystrophy” includes facioscapulohumeral (FSHD), congenital, and unspecified muscular dystrophies
Of the 68 children eligible by age to answer the child survey questions, 52 (76.5%; median age, 14 y; IQR, 6) received parental consent and completed the survey questions.
The clinician survey was distributed to 22 clinicians of whom 17 responded (77% response rate) representing 9 of the 11 health professions in the NMC. Specifically, responses were received for neurologist, respiratory physician, physiotherapist, occupational therapist, dietitian, nurse, social worker, genetic counsellor, and orthotist. There was no response for orthopedic surgeon or psychiatrist. The NMC administrators' survey was distributed to and answered by two clinic administrators.
3.1.2. TH appointments
Parents reported that their child had between one and sevenappointments (median, 3; IQR, 2) with different clinicians during a single afternoon of their TH NMC. The most commonly seen clinicians were neurologists (by 80.8% of children), physiotherapists (60.6%), respiratory physicians (43.4%), and the occupational therapist (36.4%). A typical appointment took 20–30 min per clinician. Clinicians reported that they had between one and eight patients scheduled for TH per clinic but usually failed to connect with one or two patients, mostly due to patient non‐attendance online.
3.1.3. TH technology
TH appointments were predominantly delivered by the Healthdirect Australia® video call system (92%) with telephone calls used for a minority of appointments. Perceptions of the technology are shown in Figure 2. Most families (57.3%) reported no technical issues in using TH, with some reports of poor sound (11.7%), poor visuals (10.7%), and Internet dropping out (12.6%). Conversely, intermittent connection and call quality issues were reported by more than 70% of clinicians. For 82.4% of families, all TH appointments took place as planned.
FIGURE 2.
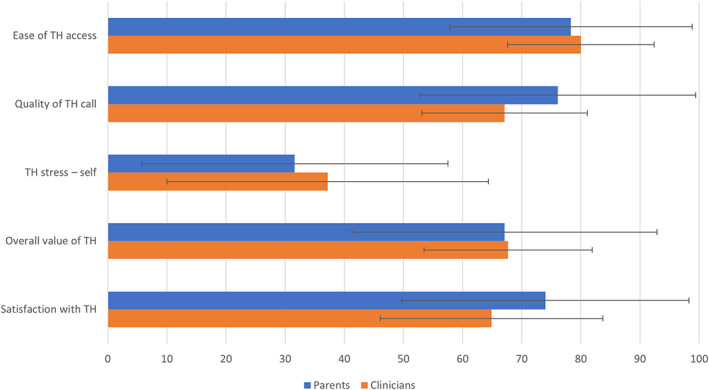
Sliding scale responses (out of 100) for parent/guardian and clinician groups. Mean values with error bars indicating standard deviation. Higher values represent positive findings except for stress where a lower value indicates less stress
3.1.4. TH stress and engagement
Parents reported that they found TH appointments less stressful (31.6 [25.9]/100 mean [SD], sliding scale) than F2F appointments (42.7 [27.6]/100), with 50.5% reporting no stress with TH. Parents rated their children's stress with TH (31.7 [26.6]/100) and F2F appointments (39.6 [28.0]/100) as similar to their own experience. TH stressors included managing child well‐being or behavior during the appointment (17.5%) and talking to someone via a screen (13.4%). Clinicians reported variable levels of stress, with 35.3% reporting that TH was more stressful than F2F NMC; the greatest cause of clinician stress was concern about providing a good clinical service via TH (77.8%).
Just over half of parents reported that their child interacted better with clinicians F2F (51.7%) with one‐third reporting equal interaction during TH and F2F appointments. Children themselves reported similar feelings during each appointment type (TH: median 3, 62.3% reported happy; F2F: median 3, 66.7% happy) but found it easier to talk with clinicians in person (F2F: median 3, 82.4% happy; TH: median 4, 43.1% happy). In TH appointments, clinicians found it easier to engage successfully with parents (rating engagement 76.8 [12.0]/100 on a sliding scale) than with children (59.8 [16.6]/100).
Despite the virtual format of TH appointments, most families reported that their children were asked to perform a physical activity for assessment (61.5%) such as walking, other gross motor activities, demonstrating range of motion, breathing and coughing, upper limb tests including handwriting. Physical activities were most commonly requested by the physiotherapist (reported by 42.4% of respondents). Twelve clinicians (70.5%; neurologists, respiratory physician, physiotherapists, occupational therapist, dietitians) reported that they undertook some form of physical assessment via TH and rated this as moderately (58.6 [12.4]/100) effective. Consistent with previous reports, certain functional tests were reported to be well suited to remote assessment (eg, timed rise from floor test and Egen Klassifikation version 2) and the ability to visually assess home environments for access, safety, and equipment was an advantage. 17 , 18 Other adaptive practices were used by NMC clinicians as they gained experience with TH. These included: getting parents to move the camera (eg, to the floor to assess child's foot posture); using household items to perform testing (eg, food cans from the pantry for timed can stack test); using clinician camera to demonstrate a movement or exercise to the patient; measuring joint angles off the screen using a goniometer.
3.1.5. Satisfaction with TH
More than 90% of families reported that some (41.8%) or all (52.8%) of their child's issues were addressed during their TH appointments. A lack of physical or “hands on” assessment was specifically identified in free text comments as a limitation of TH by 18 families (18.2%) and eight clinicians (47.1%).
The overall value of TH was rated 67 (25.8)/100 with 80% of families reporting advantages of TH, including reduced travel time (66.0%), no waiting in the waiting room (53.4%), and no parking costs (50.5%). Only six parents indicated that were worried about catching COVID‐19 and two parents commented that they preferred TH because their child was not exposed to other infections. All clinicians identified benefits of TH, including improved patient attendance (70.6%), time management (58.8%), and flexible working arrangements (52.9%). Clinicians noted that a small number of families who were previously “non‐attenders,” engaged successfully with TH appointments. Some advantages of seeing families' home environments online were noted (eg, to assess the need for bathroom modifications or identify safety issues).
3.1.6. Preferred future model of care
Figure 3 describes the preferred future model of care. Two thirds of families (68.1% of parents and 58.8% of children) preferred to have a mix of TH and F2F NMC appointments. Less than one third of families (28.6% of parents and 29.4% of children) and no clinicians wished to revert to only F2F appointments. There was an association between patient age and preferred model of care (p = .03) with parents of primary school‐aged children (6–12 y) more likely to favor F2F appointments. There was no association with diagnosis (p = .10) or travel time (p = .90). Clinician preference was for a mix of TH and F2F but with a majority F2F. Families were most likely to choose a future TH appointment for their child with a neurologist (37.4%) or dietitian (37.4%) and least likely to choose TH review with an orthopedic surgeon (10.1%) or physiotherapist (11.1%).
FIGURE 3.
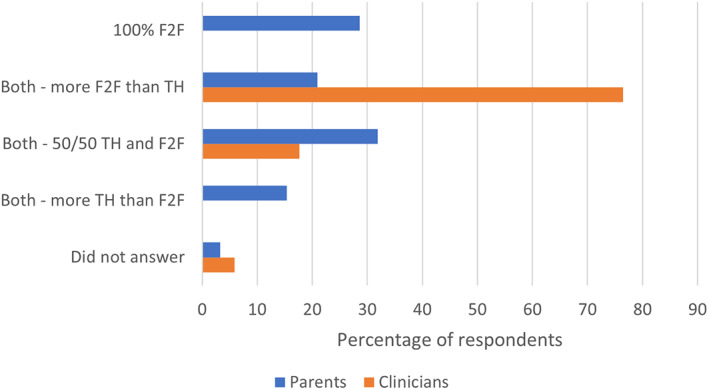
Preferences for future model of care
Clinicians commented that children who are well known to them, whose condition is stable, and who require a standard review without physical measures are best suited to TH.
3.1.7. Administering TH clinics
Administrators reported increased demands on their time associated with switching to a TH model and challenges scheduling a multidisciplinary clinic on this platform. Particularly challenging was scheduling a mix of TH and F2F appointment types on the same day and arranging for TH patients to access investigations, for example, blood tests and x‐rays, at an alternate healthcare service local to their home.
3.2. Clinical audit
An audit of NMC clinical activity from 2018 to 2020 inclusive revealed that the numbers of annual appointments was very similar across the 3 y; however, the incidence of patients with “did not attend” or missed appointments was 13% lower in 2020 (Table 1). Typically, 11–12 clinicians from different disciplines attended each NMC, while zero to four patients failed to attend one or more of their scheduled appointments in any given clinic. In 2020, 62.8% of all NMC appointments were scheduled for TH and 80% of patients attended NMC via TH at least once.
TABLE 1.
Clinical activity in the NMC by year
| Clinical activity by year | |||
|---|---|---|---|
| 2020 | 2019 | 2018 | |
| NM clinics per year (N) | 45 | 46 | 44 |
| Patients accessing NMC per year (N) | 470 | 473 | 440 |
| Total appointments scheduled per year (N) | 2661 | 2714 | 2604 |
| NMC scheduled visits per patient per year (mean) | 2.0 | 2.1 | 1.9 |
| Total appointments per patient per year (mean) | 5.7 | 5.7 | 5.9 |
|
Patients scheduled per NMC Mean (range) |
21 (10–34) |
20 (2–34) |
19 (6–28) |
|
Total appointments per NMC Mean (range) |
59 (29–92) |
59 (6–93) |
59 (15–91) |
| Patients attending NMC by TH at least once N (% of total) | 387 (82.3%) | 1 (0.2%) | 0 |
| Patients who “did not attend” ≥1 NMC appointment | 203 (43.2%) | 267 (56.4%) | 247 (56.1%) |
N, number; NMC, neuromuscular clinic (typically comprises multiple appointments); appointment, a consultation with a single clinician.
3.3. Future model of care
A checklist was developed to guide future allocation of TH and F2F appointments (Figure 4).
FIGURE 4.
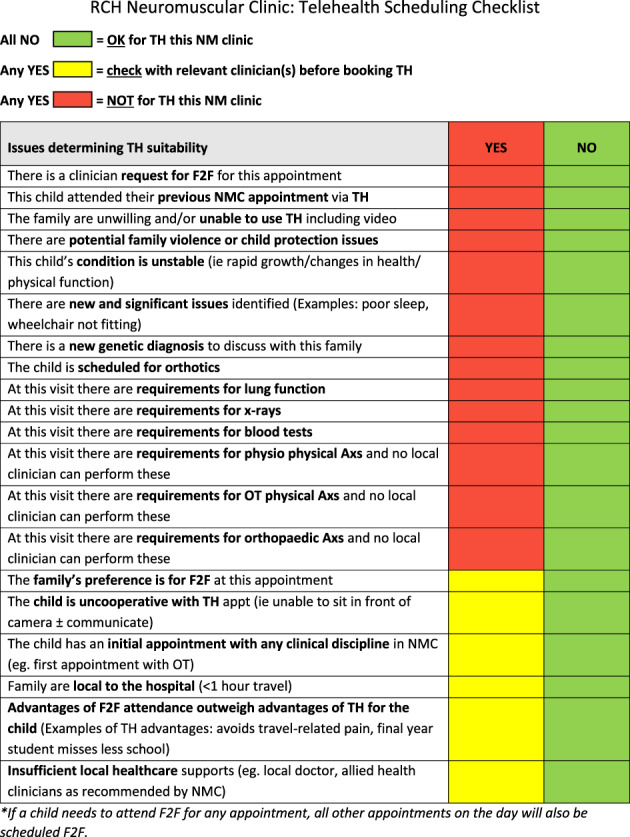
TH patient selection checklist
4. DISCUSSION
This research has highlighted that TH is an acceptable component of care in a large multidisciplinary pediatric NMC. All groups of survey participants (parents, children, and clinicians) reported positive aspects of TH use and were clear that they wanted TH to be an ongoing part of the NMC in the future. The clinical audit provided reassuring confirmation that similar numbers of children were seen in NMC over 2020 despite COVID‐19 restrictions placed on our practice.
Our initial hypothesis that families and clinicians would prefer to return to F2F appointments was not confirmed by the surveys when participants were asked about preferred future models of care. This is consistent with similar widespread patient acceptance and identification of TH benefits previously reported. 11 , 12 , 15 , 19 Acknowledging the limitations in physical assessment with TH, parents understandably indicated a preference for future TH appointments with clinicians such as the dietitian and social worker who rely less on physical assessment than other clinicians, such as orthopedic surgeons and physiotherapists. Clinicians indicated a high level of concern about compromised quality of care associated with TH due to the limited assessment of musculoskeletal issues, physical, and respiratory function. However, clinicians also acknowledged the convenience of TH for families and that, with experience, it was possible to do more with TH than was initially apparent. Where a child had good healthcare supports in their local community (eg, general practitioner, physiotherapist, and/or occupational therapist), these local clinicians could support the NMC TH appointment by providing information from their F2F interactions either prior to or during the TH encounter. 20 Emerging technologies that integrate physical assessments,such as homebased spirometry, with virtual healthcare platforms may further support TH in the future. 12 , 14 , 20 , 21
Consistent survey results suggest that, despite the positive aspects of TH that were identified, in‐person F2F engagement between children and clinicians was still preferable to most clinicians and one‐third of families. Although TH is a useful additional tool, we believe it should not fully replace F2F appointments.
Video‐based TH technology has been available in our center since 2015, however was rarely used in the NMC prior to March 2020. Possible reasons for this include a lack of TH training, previous geographically restricted funding criteria, clinician reluctance, as well as a belief that optimal clinical care can only occur in person. 8 , 9 , 10 This is despite some families traveling long distances to attend appointments with associated travel costs, time burden, and disruption to family lives. Parents reported few technical difficulties with TH; by the time they answered the survey relating to a single appointment they had had 6 mo of experience with remote work and schooling and felt comfortable using online platforms. Clinicians were reporting about their overall experience using TH over several weeks of NMC, which likely explains their higher rate of connection and call quality issues. Similar technical issues have been reported previously. 15 The slightly lower rate of “did not attend” or missed appointments in 2020 suggests that overall TH was not a barrier to NMC attendance and in some cases may even have facilitated attendance.
Based on survey findings and clinician reports we recommend that children who are well known to NMC, whose condition is stable, who attended their previous NMC appointment F2F, and who can use the technology effectively are best suited to TH. Conversely, TH is not recommended for children whose condition is rapidly changing, who require specialized tests (such as lung function tests or medical imaging), who are considered vulnerable, or those whose most recent appointment was also via TH. These recommendations have informed the NMC hybrid model checklist to guide appropriate allocation of TH and F2F appointments (Figure 4). This checklist is currently being trialed by administrators and clinicians in the NMC.
Limitations of this project include surveying families and clinicians on a single occasion thereby relying on recall of their TH experience. The survey instrument was developed specifically for this study and its psychometric properties are, therefore, unknown. Responses to this survey were skewed toward families from higher socioeconomic regions. These same families are likely to be more comfortable with online communication as they have responded to an email and answered an online survey to participate. They may, therefore, have more positive impressions of healthcare delivered online using TH. Families without an email contact were not included in the survey. Although families from non‐English speaking backgrounds had interpreters online to facilitate their successful participation in TH appointments, they are less likely to have responded to the survey as questions were available in English only. Similarly, the online consent process may have limited participation by those with cognitive deficits. Information about gender and racial distribution was not collected (in part to protect anonymity); therefore, we are unable to determine how well these different groups were represented in this survey.
Direct health‐related sequelae from the use of TH were not assessed in this study. For some of the children in the NMC who have attended more than one consecutive NMC appointment via TH, which may span 12 mo or more, there are concerns being expressed by clinicians and families that issues, such as contractures, scoliosis, and respiratory decline, have progressed unchecked over this period with delays to therapeutic interventions. Further investigation is required to confirm and quantify these anecdotal reports.
TH is a feasible and useful option for multidisciplinary pediatric neuromuscular care when there is limited access to in‐person appointments. Families and clinicians reported benefits associated with the use of TH; however, care is needed to ensure that quality and standards of care are not compromised. The checklist may assist with optimizing healthcare post‐pandemic in a new hybrid model of care using TH and F2F appointments. Further research is needed to determine direct health sequelae associated with the longer‐term use of TH in pediatric NMCs.
ETHICAL PUBLICATION STATEMENT
We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
CONFLICT OF INTERESTS
Dr Yiu reports grants from National Health and Medical Research Council of Australia, during the conduct of the study. The remaining authors had no conflict of interest.
Supporting information
File S1
Table S1
ACKNOWLEDGMENTS
This work was supported by The Royal Children's Hospital Foundation. We thank all the members of the Neuromuscular Clinic team for their support and contributions, and all the parents and children who answered the survey questions. Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
Carroll K, Adams J, de Valle K, et al. Delivering multidisciplinary neuromuscular care for children via telehealth. Muscle & Nerve. 2022;66(1):31‐38. doi: 10.1002/mus.27557
Funding information Royal Children's Hospital Foundation
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neuro. 2018;17:251‐267. doi: 10.1016/s1474-4422(18)30024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol. 2018;17:347‐361. doi: 10.1016/s1474-4422(18)30025-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 3: primary care, emergency management, psychosocial care, and transitions of care across the lifespan. Lancet Neurol. 2018;17:445‐455. doi: 10.1016/s1474-4422(18)30026-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mercuri E, Finkel RS, Muntoni F, et al. Diagnosis and management of spinal muscular atrophy: part 1: recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscul Disord. 2018;28:103‐115. doi: 10.1016/j.nmd.2017.11.005 [DOI] [PubMed] [Google Scholar]
- 5. Finkel RS, Mercuri E, Meyer OH, et al. Diagnosis and management of spinal muscular atrophy: part 2: pulmonary and acute care; medications, supplements and immunizations; other organ systems; and ethics. Neuromuscul Disord. 2018;28:197‐207. doi: 10.1016/j.nmd.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 6. Wang CH, Dowling JJ, North K, et al. Consensus statement on standard of care for congenital myopathies. J Child Neurol. 2012;27:363‐382. doi: 10.1177/0883073812436605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Doraiswamy S, Abraham A, Mamtani R, Cheema S. Use of telehealth during the COVID‐19 pandemic: scoping review. J Med Internet Res. 2020;22:e24087. doi: 10.2196/24087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leochico CFD. Adoption of telerehabilitation in a developing country before and during the COVID‐19 pandemic. Ann Phys Rehabil Med. 2020;63:563‐564. doi: 10.1016/j.rehab.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cohen BH, Busis NA, Ciccarelli L. Coding in the world of COVID‐19: non‐face‐to‐face evaluation and management care. Continuum (Minneap Minn). 2020;26:785‐798. doi: 10.1212/con.0000000000000874 [DOI] [PubMed] [Google Scholar]
- 10. Veerapandiyan A, Connolly AM, Finkel RS, et al. Spinal muscular atrophy care in the COVID‐19 pandemic era. Muscle Nerve. 2020;62:46‐49. doi: 10.1002/mus.26903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Geronimo A, Wright C, Morris A, Walsh S, Snyder B, Simmons Z. Incorporation of telehealth into a multidisciplinary ALS clinic: feasibility and acceptability. Amyotroph Lateral Scler Frontotemporal Degener. 2017;18:555‐561. doi: 10.1080/21678421.2017.1338298 [DOI] [PubMed] [Google Scholar]
- 12. Haulman A, Geronimo A, Chahwala A, Simmons Z. The use of telehealth to enhance care in ALS and other neuromuscular disorders. Muscle Nerve. 2020;61:682‐691. doi: 10.1002/mus.26838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Henderson RD, Hutchinson N, Douglas JA, Douglas C. Telehealth for motor neurone disease. Med J Aust. 2014;201:31. doi: 10.5694/mja14.00170 [DOI] [PubMed] [Google Scholar]
- 14. Penry VB, Mehta RG, Sadeghifa F. Teleneurology for neuromuscular conditions. Pract Neurol. 2020;June:54‐58. [Google Scholar]
- 15. Rametta SC, Fridinger SE, Gonzalez AK, et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID‐19 pandemic. Neurology. 2020;95:e1257‐e1266. doi: 10.1212/wnl.0000000000010010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Baker CM and Wong DL. Q.U.E.S.T.: a process of pain assessment in children (continuing education credit). Orthop Nurs 1987; 6: 11–21. January 1, 1987. [PubMed] [Google Scholar]
- 17. Montes J, Eichinger KJ, Pasternak A, Yochai C, Krosschell KJ. A post pandemic roadmap toward remote assessment for neuromuscular disorders: limitations and opportunities. Orphanet J Rare Dis. 2022;17:5. doi: 10.1186/s13023-021-02165-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Garibaldi M, Siciliano G, Antonini G. Telemedicine for neuromuscular disorders during the COVID‐19 outbreak. J Neurol. 2021;268:1‐4. doi: 10.1007/s00415-020-10063-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hooshmand S, Cho J, Singh S, Govindarajan R. Satisfaction of telehealth in patients with established neuromuscular disorders. Front Neurol. 2021;12:667813. doi: 10.3389/fneur.2021.667813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Howard IM, Kaufman MS. Telehealth applications for outpatients with neuromuscular or musculoskeletal disorders. Muscle Nerve. 2018;58:475‐485. doi: 10.1002/mus.26115 [DOI] [PubMed] [Google Scholar]
- 21. Geronimo A, Simmons Z. Evaluation of remote pulmonary function testing in motor neuron disease. Amyotroph Lateral Scler Frontotemporal Degener. 2019;20:348‐355. doi: 10.1080/21678421.2019.1587633 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File S1
Table S1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


