Abstract
Type 2 diabetes mellitus (T2DM), a common disease with a complex etiology in the world, is an important risk factor for severe cardiovascular and cerebrovascular diseases. However, treatments of T2DM are mainly based on Western medicine, whose severe side effects make traditional Chinese medicine (TCM) therapy more appealing to patients and clinicians. The overall clinical evidence for different TCM therapies in the treatment of T2DM is still unclear. This study aimed to adopt the evidence-mapping method and integrate the evidence from various researches on this topic, to depict the whole picture of TCM therapies for T2DM. This review included searches of PubMed, Embase, Web of Science, and three major Chinese literature databases (CNKI, VIP, and Wanfang) from inception to November 18, 2021. Two independent reviewers screened the literature, extracted information, and evaluated the quality of all included studies. A systematic review was subsequently performed. In total, 47 studies were reviewed, of which 46 studies (97.9%) were from China and 1 (2.1%) was from Canada. The evidence map was conducted according to different TCM therapies, including herbs or herbal extracts, compounds, powders, decoctions, pills, external treatment, basic theories and treatment principles of TCM, proprietary Chinese medicines, and unspecified TCM integrated therapies. According to the AMSTAR-2 scoring results, 4 papers were rated as high quality, 11 were low quality, and 32 were very low quality. Outcome indicators mainly focused on FBG, HbA1c, 2-h PBG, TC, TG, LDL-C, etc. The results showed that different types of TCM treatment had different improvement effects on the outcome indicators of T2DM. More consistent benefits were observed in the improvement of FBG, HbA1c, and 2-h PBG with treatment regimens based on basic theories and treatment principles of TCM, decoctions and pills, and unspecified TCM integrated therapies. Among herbs, ginger and Coptis root showed more improvement in all outcomes. Compounds, powders, and external treatment showed relatively consistent beneficial effects on the improvement of FBG. No serious adverse events were reported. Overall, the current evidence map provided an intuitive overview of the beneficial effects of TCM therapies in the treatment of type 2 diabetes. This study can be used as a reference for the clinical application of traditional Chinese medicine in T2DM, but due to the low-quality level of the included studies, it should be treated with caution in clinical practices.
1. Introduction
Type 2 diabetes mellitus (T2DM) is a common disease with a complex etiology around the world. The current development of diabetes has far exceeded expectations. The World Health Organization (WHO) reported that approximately 300 million people will suffer from diabetes in 2025 [1–3]. The trend of diabetes prevalence in China is the same as in the rest of the world. The prevalence of diabetes in Chinese adults as defined by WHO criteria increased from 9.7% in 2007 to 11.2% in 2017. In the April of 2020, a study showed that the prevalence of diabetes in Chinese adults was 12.8% and the total number of diabetic patients was about 129.8 million [4].
Diabetes is also an important risk factor for severe cardiovascular and cerebrovascular diseases, and T2DM can cause a variety of complications if blood glucose levels were not controlled, resulting in a serious decline in quality of life and high outpatient and inpatient costs. Real-time monitoring and effective control are required to reduce its burden.
Treatments for T2DM are mainly via Western medicine (antidiabetic drugs such as insulin and metformin) and lifestyle modification. However, severe side effects from medications make TCM complementary and alternative therapies more attractive to patients and clinicians [1, 5]. These TCM treatments include proprietary Chinese medicine, decoctions, pills, powders, herbal medicine, external treatment, and others [5].
A large number of systematic reviews and meta-analyses have been published on the TCM treatment for T2DM, and researchers often conducted clinical trials on a certain type of Chinese herbal medicine, proprietary Chinese medicine, and Chinese medicine compounds to verify its clinical effectiveness. However, the overall clinical evidence for different TCM classifications in the treatment of T2DM remains unclear.
Therefore, this study aims to reevaluate systematic reviews and meta-analyses, adopt the evidence mapping method, integrate the evidence from various research, and comprehensively sort out the problems in the research topic, thus depicting the whole picture of the research field [6]. No evidence map of T2DM has been published in the field of TCM. Therefore, this study used an evidence map to systematically retrieve the relevant literature (SRs) on the clinical treatment of T2DM, in order to better understand the distribution of evidence in this field and provide readers with more valuable and integrative evidence.
2. Materials and Methods
2.1. Search Strategy
Publication search was conducted in PubMed, Embase, Web of Science, and 3 major Chinese literature databases, including CNKI, VIP, and Wanfang Data (Supplementary Table 1 to Supplementary Table 6). A manual search of the unpublished literature (including conference proceedings, theses and dissertations, and gray literature) was also performed. The search time frame was from the inception to November 18, 2021, and the language was restricted to Chinese and English.
2.2. Inclusion Criteria
Inclusion criteria were as follows:
All meta-analyses and/or systematic reviews (SRs) on TCM treatments for T2DM were included.
Types of studies included in the SRs and meta-analyses should be RCTs.
Participants were diagnosed with T2DM, and there were no restrictions on age, gender, complications, or previous treatment.
The type of intervention was the use of at least one TCM therapy. There were no limitations on dosage, duration, and combined therapy.
The control group could be standard Western medicine treatment, placebo, or no treatment.
Primary outcomes included HbA1c, 2-h PBG, and FBG; secondary outcomes included BMI, HDL-C, HOMA-IR, LDL-C, TC, TG, INS, 2 h postprandial insulin, time to target blood glucose, average insulin dose, ISI, HOMA-β, hypoglycemia occurrence frequency/rate, clinical efficacy, TCM syndrome, etc.
No limitations were imposed on the study design or publication type.
2.3. Exclusion Criteria
(1) Clinical experts' experience, (2) clinical trial protocols, (3) meeting abstracts, (4) unavailable full text, (5) redundant publication, (6) fundamental research or pharmacological research of Chinese herbal medicine, and (7) animal studies were excluded.
2.4. Study Selection and Data Extraction
The authors (WY and DZL) screened the titles and abstracts of all retrieved references after removing duplicates, and the full text was obtained for further screening. WY checked all the eligible studies, and any disagreements were solved by a discussion with DZL, ZYG, and LN. The data extraction was conducted by WY and DZL and then validated by ZYG. The extracted information recorded was the title, authors, publication year, name of TCM, types of research included, the number of research included, interventions, controls, outcomes, effect value, etc. Disagreements were resolved by discussion, and a consensus was reached through a third party.
2.5. Quality Assessment
Two independent reviewers evaluated the quality of included studies. A measurement tool to assess SRs (AMSTAR-2) [7], which consists of 16 items, was used to evaluate the methodological quality of all the included SRs. For each item, when the evaluation criteria were completely satisfied, the result was “yes.” When the criteria were partially met, the evaluation result was “partially yes.” When no relevant information was reported in the SRs, the result was “no.” The key entries were 2, 4, 7, 9, 11, 13, and 15 [8]. If no or only one noncritical item failed, the quality level was high. If more than one noncritical item was not met, the quality level was medium. If one key item was not met, the quality rating was low. If more than one key item was not met, the quality level was very low.
2.6. Data Synthesis and Presentation
The quantitative description was conducted in Microsoft Excel 365. Data summary and analysis were shown as text and charts, distribution of the development trend was depicted as a line chart [9], and the distribution of evidence as bubble plots was conducted in python3 (matplotlib, pandas) [10].
3. Results
3.1. Literature Screening Process and Results
An initial review of 865 relevant sources was conducted. After removing duplicates, 566 studies were identified. After screening the titles and abstracts, 93 studies were retained. After screening the articles in full text, we further excluded 46 records, so a total of 47 studies [11–57] were reviewed (Figure 1).
Figure 1.
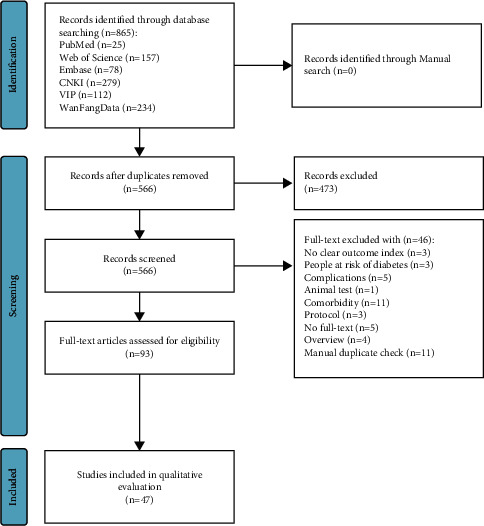
Literature screening process and results.
3.2. The Basic Information of the Included Literature
The basic information of the included literature is listed in Table 1; 46 studies (97.9%) were from China [11–33, 35–57], and 1 (2.1%) was from Canada [34]. According to different TCM therapies, they were divided into herbs or herbal extracts, compounds, powders, decoctions, pills, external treatment, basic theories and treatment principles of TCM, proprietary Chinese medicines, and unspecified TCM integrated therapies (Table 2). According to the AMSTAR-2 scoring results, 4 papers were assessed as high quality, 11 were low quality, and 32 were very low quality (Supplementary Table 7).
Table 1.
The basic information of TCM treatment for T2DM.
| Author | Country | Research department | TCM treatment | Contains ingredients/contents | Number of RCTs included |
|---|---|---|---|---|---|
| Zhipeng Hu 2021 [11] | China | Affiliated Hospital of Chengdu University of Chinese Medicine | Huanglian Jiedu decoction | Phellodendron chinense Schneid. Rutaceae (Huáng B˘ai) and Gardenia jasminoides Ellis Rubiaceae (Zhi Zĭ). | 9 |
| Dingyuan Zhong 2016 [12] | China | Guangzhou University of Chinese Medicine | Unspecified TCM therapy | — | 13 |
| Jiarong Lan 2015 [13] | China | Wenzhou Hospital of TCM, Zhejiang University of TCM | Coptis root | — | 27 |
| Xue Wang 2015 [14] | China | Shandong University of TCM | Tonifying spleen and Qi herbs | Buzhong Yiqi decoction Flavored, Buzhong Yiqi decoction modified, spleen-invigorating, hypoglycemic decoction, spleen-invigorating, and Qi-reducing decoction, spleen-invigorating and Qi-reducing Chinese medicine, spleen-reducing sugar decoction, spleen-invigorating, and Qi-reducing TCM, self-made health spleen hypoglycemic formula, Jianpi Jiangtang decoction, “pancrease kangxiao” capsules, Chinese herbs for strengthening spleen and Qi | 11 |
| Haibo Huang 2015 [15] | China | Hunan University of TCM | Liuwei Dihuang Wan | — | 8 |
| Yongzhong Wang 2015 [16] | China | The First Affiliated Hospital of Anhui University of TCM | Xiaoke pills | — | 15 |
| Xiaodong Han 2014 [17] | China | Hebei Medical University | Compound of nourishing Qi, replenishing Yin, and activating blood flow | — | 19 |
| Chi Xiao 2014 [18] | China | Dalian Medical University | Yuquan powder | — | 10 |
| Xiu-Feng Yan 2014 [19] | China | Guang'anmen Hospital | Three-typed syndrome differentiation (TTSD) | — | 19 |
| Lu sun 2012 [20] | China | Guangdong Provincial Hospital of TCM | Kidney-tonifying and blood-activating TCM compound treatment | — | 15 |
| Winnie Chen 2012 [21] | China | Guangdong University of Chinese Medicine | Jinqi Jiangtang tablets, Qihuang capsules | — | 17 |
| Jinlan Peng 2013 [22] | China | Department of Endocrinology, Pu'ai Hospital, Tongji Medical College, Huazhong University of Science and Technology | Jinqi Jiangtang tablets | Astragalus, Huanglian, and honeysuckle | 6 |
| Pu Run 2013 [23] | China | Department of Pharmacy Management and Clinical Pharmacy, School of Pharmacy, Peking University Medical Center | Liuwei Dihuang Wan | — | 16 |
| Luyao Zhang 2019 [24] | China | Beijing University of Chinese Medicine | Compound of nourishing Qi, replenishing Yin, activating blood flow | — | 17 |
| External treatment of TCM : nourishing Qi, replenishing Yin, activating blood flow | — | 5 | |||
| Yongzhong Wang 2014 [25] | China | Anhui University of TCM, First Affiliated hospital | Xiaoke pills | — | 17 |
| Jie Zhu 2018 [26] | China | The Second Clinical College, Nanjing University of Chinese Medicine, Nanjing, Jiangsu 210023, China | Ginger | — | Qualitative 12, meta 10 |
| Jingyan Yan 2018 [27] | China | Jiangxi University of TCM Research Center for the Development of Differentiated Basic Theories of TCM | Recipe for clearing stomach and intestines (Gegen Qinlian Decoction/Bai-hu decoction) | — | 24 |
| Yuqing Liang 2018 [28] | China | School of TCM, Jinan University | Strengthen spleen and reduce phlegm Chinese medicine | Shenling Baizhu powder modified, Wuling powder modified, TCM decoction for strengthening spleen and dampness, modification and subtraction of Jianpi Yiqi Huazhuo Fang, Heqi powder, Xiaoke Jianpi capsule, Wuling powder modification, and subtraction, Shenling Baizhu powder modified, modified Wuling powder, modified Shenling Baizhu powder, invigorating the spleen and removing dampness | 12 |
| Wei Zhang 2018 [29] | China | Yinchuan Hospital of TCM | Xiaoke recipe | — | 18 |
| Yue Cheng 2018 [30] | China | T2DM | TCM compound | — | 14 |
| Chongqi Ma 2017 [31] | China | North China University of Technology | TCM nutritional therapy | — | 11 |
| Linlin Kong 2012 [32] | China | School of Business Administration, Shenyang Pharmaceutical University | TCM methods | Compound pancreatic Suling, Liu Wei di Huang Wan, Xian Hu capsules, low phenolic cotton seed capsules, anti-thirst spirit, Tui Na Chiropractic | 7 |
| Multitherapeutic combination | 12 | ||||
| Tingting Shao 2009 [33] | China | Chengdu University of Chinese Medicine | Unspecified TCM therapy | 12 | |
| Dugoua Jean-Jacques 2007 [34] | Canada | Cassia bark | cassia bark | 3 | |
| X. Wang 2014 [35] | China | Key Laboratory of Endocrinology, Ministry of Health, Department of Endocrinology, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Sciences | Green tea or green tea extract | Green tea or green tea extract | 7 |
| Xiaolin Zhang 2020 [36] | China | College of Acupuncture and Massage, Changchun University of Chinese Medicine | Tui Na (massage therapy) | Chinese massage (CM) | 10 |
| Chunli Piao 2020 [37] | China | Institution of Shenzhen Hospital, Guangzhou University of Chinese medicine | Tianqi Jiangtang capsules | Tianqi hypoglycemic capsules | 8 |
| Xitao Ma [38] | China | Chengdu University of Traditional Chinese Medicine | Banxia Xiexin decoction with addition | — | 9 |
| Jiahui Hu 2020 [39] | China | Beijing University of Chinese Medicine | Chinese patent medicine | Liu Wei di Huang Wan, Xiao Xie Wan, Jin Li da, Ginseng-Astragalus hypoglycemic granules/capsules/tablets (abbreviated as Ginseng-Astragalus hypoglycemic), Tian Qi hypoglycemic capsules/granules/tablets | 42 |
| Jiahui Hu 2020 [40] | China | Beijing University of Chinese Medicine | Treating proprietary Chinese medicines and prescriptions from the perspective of the liver | Prosperity san\diversion of the liver and qi herbs\nourishing Yin and draining the liver herbs\liver and spleen harmonizing decoction\detoxification and liver regulating formula\digestion and liver clearing drink\Dan Gardenia prosperity san\liver clearing and heart diarrhea decoction\added flavor da Chai Hu granules\sugar Min Ling Wan\liver diarrhea and dampness formula | 13 |
| Ying Fu 2020 [41] | China | Nanjing University of Chinese Medicine | Unspecified TCM therapy | Huanglian Su, clearing heat, benefiting Qi and invigorating blood, clearing liver and lungs, Jinmai warming gall bladder, Huangzen Tang, Dahuang Huanglian diarrhea heart, Ge Gen cenlian Tang, Warming Yang, benefiting Qi and invigorating blood, clearing heat, invigorating blood, and resolving phlegm, Fuhe liver, and benefiting spleen | 13 |
| Huijuan Gao 2019 [42] | China | Yuquan Hospital, Tsing Hua University, | Jinqi Jiangtang tablets | Jinqi Jiangtang tablet | 17 |
| Fangyan Huang 2019 [43] | China | Youjiang Medical University for Nationalities | Ginger | Zingiber officinale | 8 |
| Fengmei Lian 2019 [44] | China | Department of Endocrinology, Guang'anmen Hospital, | Jinlida granules | Jinlida granules | 15 |
| Yujiao Zheng 2021 [45] | China | Department of Endocrinology, Guang' anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China | Banxia Xiexin granules | (Pinelliae Rhizoma 12 g, Scutellariae Radix 9 g, Coptidis Rhizoma 3 g, Ginseng Radix et Rhizoma 9 g, Zingiberis Rhizoma 9 g, Glycyrrhizae Radix et Rhizoma 9 g, Jujubae fructus 9 g), | 4 |
| Compound of Ginseng | Ginseng Radix et Rhizoma 10 g, Astragali Radix 30 g, Corni fructus Radix 10 g, Rehmanniae Radix 15 g, Salviae et Rhizoma 6 g) | ||||
| Gegen Qinlian decoction | (Puerariae Lobatae Radix, Scutellariae Radix, Coptidis Rhizoma, Glycyrrhizae Radix et rhizoma), | ||||
| Tonifying Qi and strengthening spleen decoction | AMC herbal formula (Anemarrhenae rhizoma, Momordica charantia, Coptidis rhizoma, Salviae miltiorrhizae Radix et Rhizoma, fermentum Schisandrae chinensis fructus, and Zingiberis Rhizoma) | ||||
| Xu Zhou 2021 [46] | China | Evidence-Based Medicine Research Center, Jiangxi University of TCM, Nanchang, 330004, China. | Acupuncture | Acupuncture | 21 |
| Zhipeng Hu 2021 [47] | China | Hospital of Chengdu University of TCM, Chengdu, China | Jingui Shenqi pills | Rehmannia glutinosa (Gaertn.) DC. (dì Huáng), Orobanchaceae; dioscorea oppositifolia L. (Huái Shān Yào), Dioscoreaceae; cornus officinalis siebold (Shān Zhū Yú), Cornaceae; alisma plantago-aquatica L. (Zé Xiè), Alismataceae; Smilax glabra roxb. (Fú Líng), Smilacaceae; Paeonia × suffruticosa Andrews. (Mŭ dān Pí), Paeoniaceae; Neolitsea cassia (L.) Kosterm. (Guì Zhī), Lauraceae; and Aconitum carmichaelii debeaux, Ranunculaceae. | 14 |
| Jiang Li 2021 [48] | China | Dongzhimen Hospital Affiliated to Beijing University of Chinese Medicine, Beijing, China. | Heat-clearing method | Astragalus, yam, poria, atractylodes, and Ginseng; Coptis, rhubarb, Radix Scutellariae, sophora flavescens, and honeysuckle | 15 |
| Guohua Mu 2021 [49] | China | Beijing University of Chinese Medicine | Coptis-cassia bark | Huanglian-cassia bark | 6 |
| Aiping Deng 2021 [50] | China | Heilongjiang University of TCM | TCM decoctions | Benefiting Qi and nourishing Yin, hypoglycemic and sensitizing decoction ∗ 2, dan gardenia and lipid regulating decoction, beneficial Yin and dampness Chinese herbs, strengthening the spleen and kidneys, clearing phlegm and blood, warming the Yang and strengthening the spleen method, strengthening the spleen and benefiting Qi Chinese herbs, Tonifying the organs and enlarging the ligaments, Erzhu Xia Lan Tang, beneficial Qi and nourishing Yin and clearing heat, dispelling pancreatic resistance, warming the Yang and strengthening the spleen decoction, Ling Gui Jie Gan Tang | 14 |
| Zhiyuan deng 2020 [51] | China | Guangzhou University of Chinese Medicine First Clinical School of Medicine | Jinqi Jiangtang tablets | Golden Astragalus hypoglycemic tablets | 10 |
| Jiaxing Tian 2019 [52] | China | Tian, Jiaxing Department of Endocrinology, Guang'anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China | Unspecified TCM therapy | Pueraria mirifica powder, argyle sugar health tablets, anti-thirst pill, Kai Yu Qing heat and lowering turbidity formula, Tian Qi lowering sugar capsules, Jin Li da, sugar min Ling pill, Wu Mei formula, Tang Ke soft capsules, Pueraria Mirifica Scutellaria Tang, Huang Lian Su | 12 |
| Siyi Zhao 2019 [53] | China | Siyi Zhao, School of Acupuncture and Rehabilitation Clinical Medicine, Guangzhou University of TCM | Liuwei Dihuang Wan (soup) | Cornus officinalis, Chinese Yam, radix Rehmanniae, Radix Zeligae, dampi, poria | 20 |
| Tingting Guo [54] | China | Department of Pharmacy, Affiliated Hospital of Changchun University of TCM | Unspecified TCM therapy | — | 12 |
| Huiping Tian 2019 [55] | China | Department of Pharmacy, The First Affiliated Hospital of Xi'an Jiaotong University | Replenishing Qi nourishing Yin method | Yiqi Yangyin recipe, Sanqi dan granules, Yiqi Yangyin clearing heat and blood activating TCM, Yiqi Yangyin Huoxue Tongluo decoction, Yiqi Yangyin decoction, Quyi Difang decoction, Yiqi Yangyin Huoxue decoction, sugar kidney 1 no. Fang, Yiqi Yangyin Qingre Huoxue Fang | 13 |
| Yanling Dai 2019 [56] | China | School of Nursing, Fujian University of TCM; People's Hospital of Fujian University of TCM | TCM diet therapy + conventional therapy | — | 12 |
| Replenishing Qi and nourishing Yin diet therapy + conventional treatment | |||||
| Nonreplenishing Qi and nourishing Yin diet therapy + conventional treatment | |||||
| Yuming Gu 2018 [57] | China | Shandong University of TCM | Chromium-containing Chinese medicine Tianmai Xiaoke tablets | Tianmai Xiaoke tablet contains chromium picolinate (1.6 mg per tablet, equal to 200 μg of chromium), Tianhuafen (Radix Trichosanthis, snake gourd root), Maidong (radix ophiopogonis, Dwarf Lilyturf tuber), and Wuweizi (fructus Schisandrae Chinensis) | 7 |
Table 2.
TCM therapy classification.
| Classification | Content |
|---|---|
| Herbs or herbal extracts | Ginger, cassia bark, green tea or green tea extract, Coptis root, Coptis-cassia bark |
| Compounds | Compound of nourishing Qi, replenishing Yin, activating blood flow compound of Ginseng-Astragalus |
| Powder | Yuquan powder, Jinlida Granules, Banxia Xiexin Granules |
| Decoction | Xiaoke recipe, recipe for clearing stomach and intestines (Gegen Qinlian decoction/Baihu decoction), Huanglian Jiedu decoction, Banxia Xiexin decoction with addition, Gegen Qinlian decoction, Tonifying Qi and strengthening spleen decoction |
| External treatment | Acupuncture, Tui Na (massage therapy) |
| Pills | Xiaoke pills, Liuwei Dihuang Wan, Jingui Shenqi pill |
| Pills or decoction | Liuwei Dihuang Wan (soup) |
| Basic theories and treatment principles of TCM | External treatment of TCM, replenishing Qi and nourishing Yin diet therapy + conventional treatment, replenishing Qi nourishing Yin method, heat-clearing method, tonifying spleen, and Qi herbs, strengthen spleen and reduce phlegm Chinese medicine, nonreplenishing Qi and nourishing Yin diet therapy + conventional treatment, treating proprietary Chinese medicines and prescriptions from the perspective of the liver, kidney-tonifying and blood-activating TCM compound treatment, three-typed syndrome differentiation (TTSD) |
| Proprietary Chinese medicines | Tianqi Jiangtang capsules, Jinqi Jiangtang tablets, Qihuang capsules, Jinqi Jiangtang tablets, chromium-containing Chinese medicine Tianmai Xiaoke tablets |
| Integrated TCM therapies | TCM methods, TCM nutritional therapy, TCM diet therapy + conventional therapy, unspecified TCM therapy, TCM decoction, TCM compound, Chinese patent medicine, multitherapeutic combination |
3.3. Bibliometric Information and Characteristics of the Included RCTs
In Figure 2, the increasing overall trend in the number of studies was demonstrated. Before 2010, reviews were conducted sporadically. The number increased rapidly after 2010, with up to 144 systematic reviews published in one year.
Figure 2.
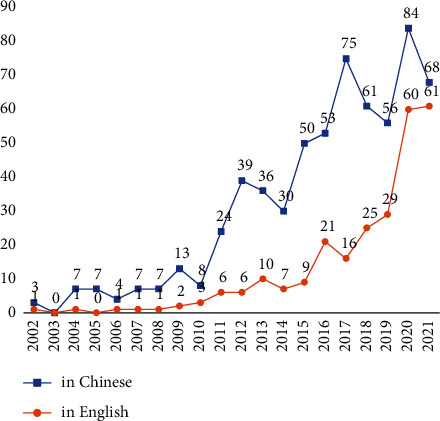
Number of the systematic review publications on TCM treatment for T2DM.
Table 3 shows the outcome indicators of TCM treatments of T2DM, the number of systematic reviews corresponding to the different indicators, and the number of comparative analyses with other control measures.
Table 3.
Number of studies and comparative analysis corresponding to different outcome indicators.
| Outcomes | Number of studies | Number of meta-analyses compared to the control group |
|---|---|---|
| HbA1c | 40 | 56 |
| 2-h PBG | 33 | 40 |
| BMI | 7 | 8 |
| FBG | 42 | 71 |
| HDL-C | 9 | 12 |
| HOMA-IR | 9 | 11 |
| LDL-C | 14 | 16 |
| TC | 21 | 31 |
| TG | 21 | 35 |
| INS | 11 | 11 |
| 2 h postprandial insulin | 3 | 3 |
| Blood sugar target time | 2 | 2 |
| Average insulin dose | 1 | 1 |
| ISI | 7 | 7 |
| HOMA-β | 5 | 5 |
| Number/rate of hypoglycemia | 3 | 3 |
| Clinical efficacy | 13 | 16 |
| TCM syndrome | 10 | 10 |
| Follow-up | 1 | 1 |
| Sleep quality | 1 | 1 |
| Plasma viscosity | 1 | 1 |
| Fibrinogen | 1 | 1 |
| Quality of life | 1 | 1 |
3.4. Effects of the TCM Therapies on T2DM
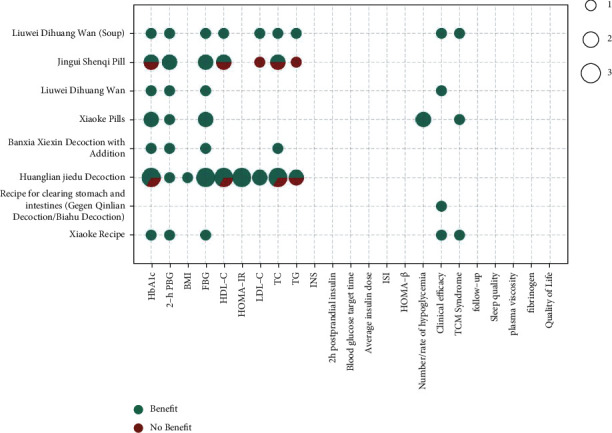
The metrics of clinical outcomes and intervention are shown in Figures 3–8 according to different TCM classifications. The consistent beneficial effect according to the systematic reviews and meta-analysis are shown in dark green. Nonmeaningful outcomes are shown in dark red, and the numbers of intervention-control comparisons for each outcome are shown as the bubble area.
Figure 3.
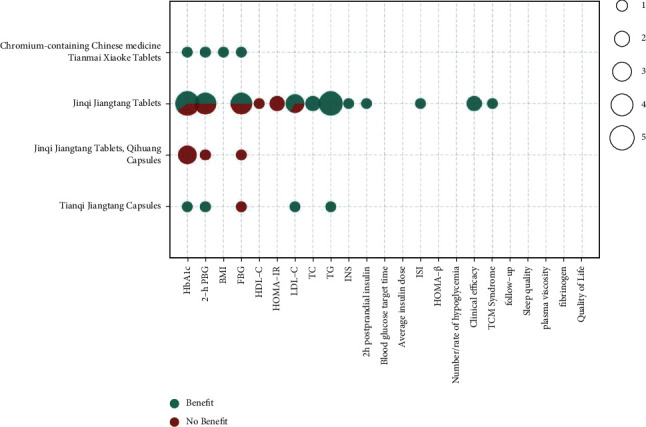
Outcomes and effects of proprietary Chinese medicines (horizontal axis: T2DM outcome indicators; ordinate: TCM; dark green color: beneficial effect; dark red color: nonbeneficial effect; bubble area: number of meta-analysis for intervention-control comparisons).
Figure 4.
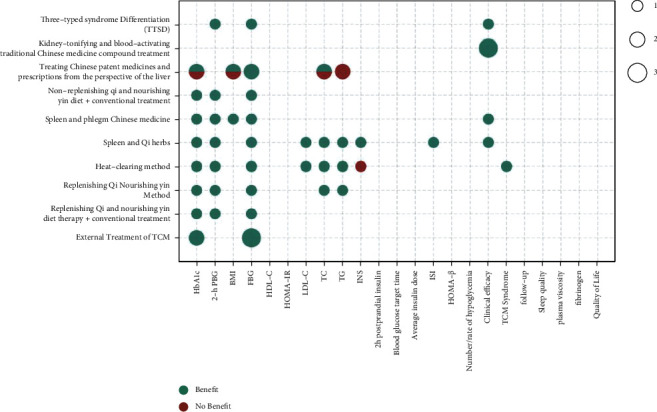
Outcomes and effects of basic theories and treatment principles of TCM.
Figure 5.
Outcomes and effects of decoctions and pills.
Figure 6.
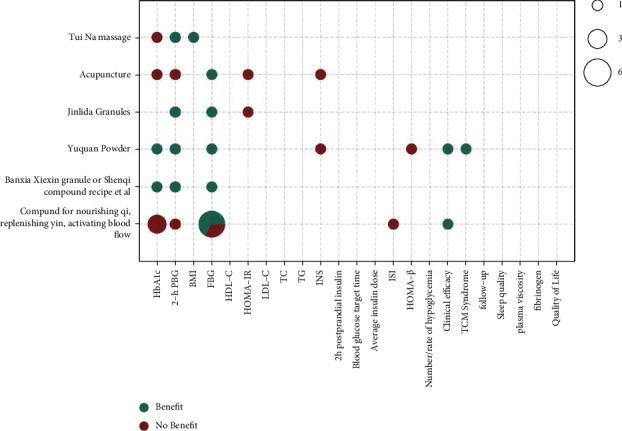
Outcomes and effects of compounds, powder, and external treatment methods (Banxia Xiexin granules, compound of Ginseng-Astragalus, tonifying Qi and strengthening spleen decoction, and Gegen Qinlian decoction.).
Figure 7.
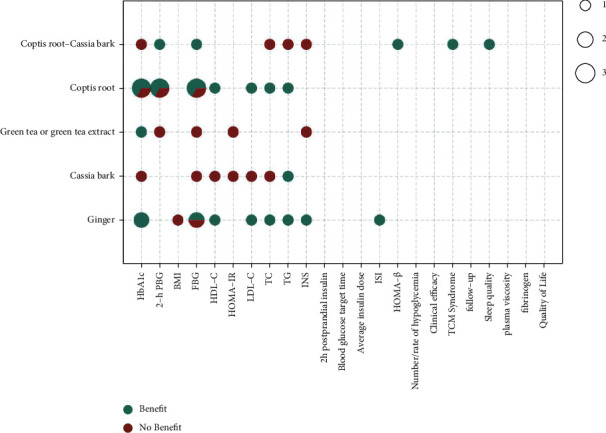
Outcomes and effects of herbal medicines.
Figure 8.
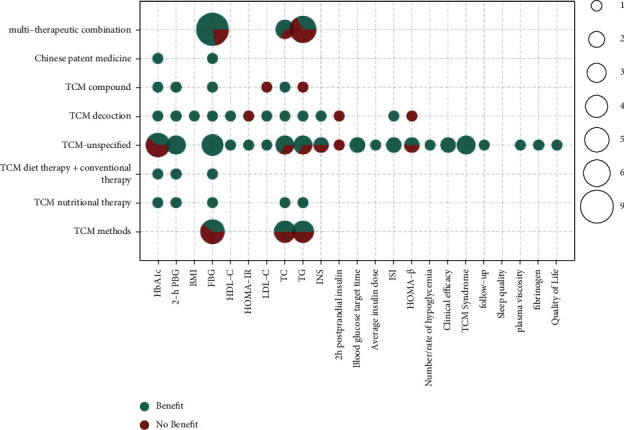
Outcomes and effects of integrated TCM therapies.
3.5. Proprietary Chinese Medicines
Of the 47 included systematic reviews, a total of 6 papers [21, 22, 37, 42, 51, 57] compared the effects of TCMs such as Tianqi Jiangtang capsules, Jinqi Jiangtang tablets, Jinqi Jiangtang tablets and Qihuang capsules, and chromium-containing Chinese herbal medicine Tianmai Xiaoke tablets on the treatment of T2DM by meta-analysis. Improvements in various outcome indicators did not show a more consistent beneficial effect than conventional or placebo therapy alone. Improvements in glycosylated hemoglobin (5/10), 2-hour postprandial glucose (4/7), and FBG (3/7) showed beneficial effects in only half of the studies, with consistent beneficial effects only on TG (6/6).
3.6. Basic Theories and Treatment Principles of TCM
A total of 10 [14, 17, 19, 20, 24, 28, 40, 48, 55, 56] of the 47 included systematic reviews compared the effectiveness of basic theories and treatment principles of TCM, including external treatment of TCM, nourishing Qi, replenishing yin, activating blood flow, replenishing Qi and nourishing yin diet therapy + conventional treatment, replenishing Qi nourishing yin method, heat-clearing method, tonifying spleen, and Qi herbs, strengthening the spleen, and reducing phlegm Chinese medicine, nonreplenishing Qi, and nourishing yin diet therapy + conventional treatment, treating proprietary Chinese medicines and prescriptions from the perspective of the liver, kidney-tonifying and blood-activating TCM compound treatment, and TTSD on the treatment of T2DM by meta-analysis. Improvements in all outcome indicators relative to conventional therapy or placebo therapy alone showed consistent beneficial effects. Improvements in glycated hemoglobin (9/10), 2-hour postprandial glucose (7/7), FBG (12/12), and clinical outcomes (6/6) were all highly beneficial. There were also beneficial effects on the improvements of BMI, LDL-C, TC, INS, ISI, and TCM syndrome.
3.7. Decoctions and Pills
A total of 11 [11, 15, 16, 23, 25, 27, 29, 38, 45, 47, 53] of the 47 included systematic reviews compared the effects of Xiaoke recipe, the recipe for clearing stomach and intestines (Gegen Qinlian decoction/Baihu decoction), Huanglian Jiedu decoction, Banxia Xiexin decoction with addition, Xiaoke pills, Liuwei Dihuang Wan, Jingui Shenqi pill, and Liuwei Dihuang Wan (soup) on the treatment of T2DM by meta-analysis. Improvements in all outcome indicators relative to conventional therapy or placebo therapy alone showed consistent beneficial effects. Improvements in glycated hemoglobin (9/11), 2-hour postprandial glucose (8/8), FBG (11/11), HOMA-IR (3/3), clinical outcomes (4/4), and TCM symptoms (3/3) were all highly beneficial. It was also beneficial for the improvements of BMI, HDL-C, LDL-C, TC, TG, and incidence of hypoglycemia.
3.8. Compounds, Powder, and External Treatment Methods
Of the 47 included systematic reviews, a total of 6 papers [24, 36, 44–46] compared the efficacy of the compound of nourishing Qi, replenishing yin, and activating blood flow, a compound of Ginseng-Astragalus, Yuquan powder, Jinlida granules, Banxia Xiexin granules, acupuncture, and Tui Na on the treatment of T2DM by meta-analysis. The overall beneficial effect on improvements of all outcome indicators was not significant relative to conventional or placebo therapy alone. There was a consistent improvement effect on FBG (8/10), with some beneficial effects on BMI, clinical outcomes, and TCM syndrome. However, there were inconsistent and insignificant improvement effects on glycated hemoglobin (2/7), 2-hour postprandial glucose (4/6), HOMA-IR (0/2), INS (0/2), ISI (0/1), and HOMA- β (0/1).
3.9. Herbal Medicine
A total of 6 [13, 26, 34, 35, 43, 49] of the 47 included systematic reviews compared the effects of ginger, cassia bark, green tea or green tea extract, Coptis root, and Coptis-cassia bark by meta-analysis for the treatment of T2DM. Coptis root showed beneficial effects on glycated hemoglobin, 2-hour postprandial glucose, FBG, HDL-C, TC, and TG in 10 of 13 meta-analyses. Ginger showed beneficial effects on glycated hemoglobin, FBG, HDL-C, LDL-C, TC, TG, INS, and ISI in 9 of 11 meta-analyses.
3.10. Integrated TCM Therapies
A total of 11 [58, 76–79, 85, 87, 96, 98, 100, 102] of the 47 included systematic evaluations compared the effects of unspecified TCM, including TCM methods such as Baduanjin, TCM nutritional therapy, TCM diet and conventional therapy, other unspecified TCM, TCM decoction, TCM compound, Chinese patent medicine, and multitherapeutic combination on T2DM by meta-analysis. Relative to conventional therapies alone, the integrated TCM therapies showed a more consistent beneficial effect on the improvement of glycosylated hemoglobin (7/10), with only 3 unspecified TCMs being insignificant in the 10 comparative studies. They showed a completely consistent beneficial effect on the improvement of 2-hour postprandial glucose (7/7) and showed a more consistent beneficial effect on the improvement of fasting glucose (18/23), with 2 insignificant multitherapeutic combinations and 3 insignificant TCM methods. The improvement in TC showed a more consistent beneficial effect (9/13); 2 TCM methods were not significant, 1 TCM were unspecified, and 1 multitherapeutic combination was not significant. For the improvement in TG, only half of the studies showed a beneficial effect (8/16), and for improvement in 2 hours' postprandial insulin, the integrated TCM therapies did not show a beneficial effect. The effects of TCM compound, Chinese patent medicine, and TCM unspecified on improving BMI, HDL-C, HOMA-IR, LDL-C, INS, blood glucose target time, average insulin dose, ISI, HOMA-β, number/rate of hypoglycemia, and clinical efficacy, TCM syndrome, follow-up, sleep quality, plasma viscosity, fibrinogen, and quality of life all had beneficial effects.
3.11. Adverse Events
In the intervention group using TCM therapies, there were few reports of adverse reactions, most of which were incidental cases, and no serious adverse reactions were reported. Zhipeng Hu [11] remarked that one RCT reported one case of headache, three cases of nausea and vomiting, one case of dizziness, and one case of dry cough in the TCM treatment group and one RCT reported one case of hypoglycemia and four cases of mild nausea and loss of appetite, which then gradually disappeared. Jiarong Lan [13] mentioned that no serious adverse reactions affecting vital organs occurred during the experiment. The incidence of adverse reactions was dose-dependent. Chi Xiao [18] noted that one RCT reported one case of the hypoglycemic reaction occurred in the TCM treatment group after 2 weeks of treatment, while 2 cases occurred in the control group. Some RCT studies reported possible GI adverse reactions in both the TCM treatment and control groups [21]. One RCT reported a total of 3 cases of gastrointestinal (GI) adverse reactions, but none of them required special treatment [22]. It has been summarized [24] that some RCTs reported the occurrence of adverse reactions, such as mild nausea and vomiting, mild gastrointestinal discomfort, mild hypoglycemia, skin pruritus, and mild tingling in the ear in a few patients. Jiahui Hu [39, 40], Huijuan Gao [42], Aiping Deng [50], and Jiaxing Tian [52] noted that there was no statistically significant difference in the incidence of adverse reactions between the TCM treatment group and the control group. Ying Fu [41] mentioned that the studies involved all GI reactions. Another review concluded [47] that hypoglycemic events were reported in the RCT studies, but there was no significant difference between the control group (6 cases) and the TCM treatment group (5 cases). Jiang Li [48] alluded that one RCT reported 6 cases of hyperthermia in the control group and 4 cases of vomiting in the TCM group, and another RCT reported one case of hypoglycemia in both groups. One literature reported the incidence of GI adverse reactions in the TCM group was 2.5% while that in the control group was 7.5% [48]. It has been indicated [53] that the combination of Liu Wei Di Huang Wan (soup) with metformin for T2DM has the potential to reduce the adverse effects of metformin. Yuming Gu [57] mentioned that the common adverse events in the TCM group were gastrointestinal symptoms (nausea/vomiting, bloating, and diarrhea), neurological symptoms, and hypoglycemia. However, no significant abnormalities in blood, liver, or kidney functions were seen in all studies.
4. Discussion
4.1. Summary of Findings
The evidence map for TCM treatments of T2DM was developed based on 47 SRs and meta-analyses, providing an evidence overview of the impact of different TCM therapies on different outcomes. The included literature was for patients with only T2DM but not comorbidities and complications. There were many systematic reviews on Coptis root, Jinqi Jiangtang tablets, Liuwei Dihuang pills, Xiaoke pills, and methods of nourishing Qi, replenishing yin, and activating blood flow. The outcome indicators mainly focus on FBG, HbA1c, 2-h PBG, TC, TG, and LDL-C. The results showed that different types of TCM treatments had different improvement effects on the outcome indicators of T2DM. More consistent benefits were observed in the improvement of the primary outcomes with basic theories and treatment principles of TCM, decoctions and pills, and unspecified TCM integrated therapies. Among the herbal medicine, ginger and Coptis root showed benefits in all outcomes. The improvement of FBG was more consistent with compounds, powders, and external treatment. No report of serious adverse reactions has been found, but mild gastrointestinal reactions were common, such as nausea, vomiting, abdominal distension, and diarrhea, and they did not require special treatments.
4.2. Differences from Previous Studies
The method of using the evidence map to provide evidence summary has been used in the treatment of hypertension with TCM [55], and there have been reviews published in English on the treatment of diabetes with TCM [1]. This paper is the first evidence map systematic review on the treatment of T2DM with TCM.
4.3. Limitations
The study has some limitations. First, most systematic reviews of TCM research were published in Chinese, which may have publication bias. Second, in all SRs and meta-analyses included, only a few studies were of high quality, and most were of low or very low quality.
4.4. Implications for Future Research
The study provides enlightenment for the future TCM treatments of diabetes and related academic research. First, the results of FBG showed the most consistent beneficial effect among different TCM treatments, which was beneficial for long-term control and prevention of complications. Second, in most of the included SRs and meta-analyses, TCM therapies were used in combination with conventional Western medicine treatment, but the different combinations of TCM and Western medicine may achieve different results and further clinical studies are needed. Third, a few studies found that TCM may reduce the side-effects of Western medicine, but the evidence was not clear enough. The interaction between TCM and Western medicine needs to be explored.
4.5. Implications for Clinical Practice
In China, emphasizing the application of both TCM and Western medicine has become a national strategy. But in clinical practice, the indications of TCM therapies are currently too broad, and the current evidence cannot convince clinicians to choose a specific treatment method. The evidence map shows that the external treatment of TCM, replenishing Qi and nourishing yin diet therapy + conventional treatment, replenishing Qi nourishing yin method, heat-clearing method, tonifying spleen and Qi herbs, strengthening the spleen and reducing phlegm Chinese medicine, nonreplenishing Qi and nourishing yin diet therapy + conventional treatment, TTSD, Xiaoke recipe, Banxia Xiexin decoction, Xiaoke pills, Liuwei Dihuang Wan (soup), and chromium-containing Chinese herbal medicine Tianmai Xiaoke tablets have a relatively clear application value for hypoglycemia and can be used as a careful reference for making diagnosis and treatment plans in clinical practice. However, the combined usage, administration time, and duration of TCM therapies still need to be further explored. Given the promising findings in the evidence map from this paper, the use of these TCM therapies may become more widespread if supported by further well-designed trials or real-world studies.
5. Conclusions
Overall, the evidence map provides an intuitive overview of the beneficial effects of TCM therapies in the treatment of T2DM. This study can be used as a reference for the clinical application of TCM in T2DM, but due to the relatively low-quality level of the included studies, it is recommended to be used with caution in clinical practice. This study also enlightens the future research direction of evidence-based medicine and further study about the clinical application of TCM.
Acknowledgments
This study was funded by the National Natural Science Foundation of China (No. 82004213) and the Project of Sichuan Provincial Department of Science and Technology (No. 2021YFH0191).
Contributor Information
Yonggang Zhang, Email: jebm_zhang@yahoo.com.
Nian Li, Email: linian@wchscu.cn.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Supplementary Materials
Supplementary Table 1: search strategy of CNKI (279). Supplementary Table 2: search strategy of VIP (112). Supplementary Table 3: search strategy of Wanfang Data (234). Supplementary Table 4: search strategy of PubMed (25). Supplementary Table 5: search strategy of Web of Science (157). Supplementary Table 6: search strategy of Embase (78). Supplementary Table 7: AMSTAR-2 scoring results.
References
- 1.Liu M., Liu Z., Xu B., Zhang W., Cai J. Review of systematic reviews and meta-analyses investigating traditional Chinese medicine treatment for type 2 diabetes mellitus. Journal of Traditional Chinese Medicine . 2016;36(5):555–563. doi: 10.1016/s0254-6272(16)30074-7. [DOI] [PubMed] [Google Scholar]
- 2.Yang W., Lu J., Weng J., et al. Prevalence of diabetes among men and women in China. New England Journal of Medicine . 2010;362(12):1090–1101. doi: 10.1056/nejmoa0908292. [DOI] [PubMed] [Google Scholar]
- 3.Xu Y., Li M. W., Jiang H., et al. Prevalence and control of diabetes in Chinese adults. JAMA . 2013;310(9):p. 948. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 4.Li Y. Z., Teng D., Shi X., et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American diabetes association: national cross sectional study. BMJ . 2020;369:p. m997. doi: 10.1136/bmj.m997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nahas R., Moher M. Complementary and alternative med-icine for the treatment of type 2 diabetes. Canadian Family Physician . 2009;55(6):591–596. [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Y., Wang B., Ju C., et al. Traditional Chinese medicine for essential hypertension: a clinical evidence map. Evidence-Based Complementary and Alternative Medicine . 2020;2020(14):17. doi: 10.1155/2020/5471931.5471931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shea B. J., Reeves B. C., Wells G., et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ . 2017;358 doi: 10.1136/bmj.j4008.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang F. Y., Shen A. M., Zeng X. T., Qiang W., Jin Y. An introduction to AMSTAR 2: a critical appraisal tool for systematic reviews. Chinese Journal of Evidence-Based Cardiovascular Medicine . 2018;10(1):14–18. [Google Scholar]
- 9.Yang M., Zhu S. J., Shen C., et al. Clinical application of Chinese herbal injection for cancer care: evidence-mapping of the systematic reviews, meta-analyses, and randomized controlled trials. Frontiers in Pharmacology . 2021;12 doi: 10.3389/fphar.2021.666368.666368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ming X. Read and Write Periodical . Berlin, Germany: Springer; 2018. The application of python in plotting. [Google Scholar]
- 11.Hu Z., Yang M., Liu Y., et al. Effect of Huang-Lian Jie-Du decoction on glucose and lipid metabolism in type 2 diabetes mellitus: a systematic review and meta-analysis. Frontiers in Pharmacology . 2021;12 doi: 10.3389/fphar.2021.648861.648861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhong D. Y. Meta-Analysis of Traditional Chinese Medicine Combined with Insulin Pump in the Treatment of Type 2 Diabetes Mellitus . Guangzhou, China: Guangzhou University of Chinese Medicine; 2016. [Google Scholar]
- 13.Lan J., Zhao Y., Dong F., et al. Meta-analysis of the effect and safety of berberine in the treatment of type 2 diabetes mellitus, hyperlipemia and hypertension. Journal of Ethnopharmacology . 2015;161:69–81. doi: 10.1016/j.jep.2014.09.049. [DOI] [PubMed] [Google Scholar]
- 14.Wang X., Li X. Meta analysis on the therapeutic effect of Yiqi Jianpi method on type 2 diabetes. Chinese Medicine Herald . 2015;21(18):82–85. [Google Scholar]
- 15.Huang H. B., Li J., Xiao Z. Z., Xiang Z. J. A systematic review of the efficacy of Liuwei Dihuang pills in the treatment of type 2 diabetes. Hunan Journal of Traditional Chinese Medicine . 2015;31(09):139–141. [Google Scholar]
- 16.Wang Y. Z., Li Y., Li X., Luo H., Jiang H., Li Y. Efficacy and safety of Xiaoke Pill versus glibenclamide in the treatment of type 2 diabetes mellitus: a systematic review. Chinese Pharmacy . 2015;26(36):5110–5113. [Google Scholar]
- 17.Han X. A Systematic Review on the Treatment of Type 2 Diabetes Mellitus with Yiqi Yangyin Huoxue Recipe . Shijiazhuang, China: Hebei Medical University; 2014. [Google Scholar]
- 18.Xiao C. Meat Analysis of Randomized Controlled Trials of Yuquan Powder in the Treatment of Type 2 Diabetes . Dalian, China: Dalian Medical University; 2014. [Google Scholar]
- 19.Yan X. F., Ni Q., Wei J. P., Lin L. A systematic review and meta-analysis of type 2 diabetes mellitus treatment based on the “three-typed syndrome differentiation” theory in Chinese medicine. Chinese Journal of Integrative Medicine . 2014;20(8):633–640. doi: 10.1007/s11655-013-1462-2. [DOI] [PubMed] [Google Scholar]
- 20.Sun L., Fan G. J. A systematic review on the treatment of type 2 diabetes mellitus with traditional Chinese medicines for invigorating the kidney and activating blood. Proceedings of the 14th National Diabetes Congress of Traditional Chinese Medicine; Zhengzhou, Henan, China, 2012. [Google Scholar]
- 21.Chen W. N., Liu Z. L., Zhang C., et al. Chinese medicines for treatment of type 2 diabetes: a systematic review of randomized controlled trials. China Journal of Traditional Chinese Medicine Information . 2012;19(01):21–24+28. [Google Scholar]
- 22.Peng J. L., Yin P., Wang B., Ding Y. F. Efficacy and safety of Jinqi Jiangtang tablet in treatment of type 2 diabetes mellitus. Medicine Herald . 2013;32(06):796–800. [Google Scholar]
- 23.Pu R., Geng X. N., Yu F., Liang H. G., Shi L. W. Liuwei Dihuang pills enhance the effect of western medicine in treating type 2 diabetes: a meta-analysis of randomized controlled trials. Chinese Journal of Integrative Medicine . 2013;19(10):783–791. doi: 10.1007/s11655-013-1591-7. [DOI] [PubMed] [Google Scholar]
- 24.Zhang L. Y. A Systematic Review on the Treatment of Type 2 Diabetes Mellitus by Nourishing Qi, Nourishing Yin and Activating Blood . Beijing, China: Beijing University of Traditional Chinese Medicine; 2019. [Google Scholar]
- 25.Wang Y. Z., Li Y., Li X., Luo H., Li Y., Xia L. Z. A systematic review of Xiaoke pills versus glyburide in the treatment of type 2 diabetes mellitus. Proceedings of the 2014 Academic Annual Meeting of the Hospital Pharmacy Branch of the Chinese Society of Traditional Chinese Medicine, the 2014 International Academic Conference of the Chinese Medicine Professional Committee of the World Federation of Chinese Medicine and the Inaugural Meeting of the Beijing Pharmacists Association Chronic Disease Prevention and Pharmacy Professional Committee; Beijing, China, 2014. [Google Scholar]
- 26.Zhu J., Chen H., Song Z., Wang X., Sun Z. Effects of ginger (Zingiber officinale Roscoe) on type 2 diabetes mellitus and components of the metabolic syndrome: a systematic review and meta-analysis of randomized controlled trials. Evidence-Based Complementary and Alternative Medicine . 2018;2018:11. doi: 10.1155/2018/5692962.5692962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yan J. Y., Li B., Zeng Z. J. A meta-analysis of treating T2D from the Eryang therapy. Traditional Chinese Medicine Clinical Research . 2018;10(19):139–143. [Google Scholar]
- 28.Liang Y. Q., Han L., Liang Z., Mai J. J., Li L. Y. Clinical Efficacy of spleen-invigorating and phlegm-relieving traditional Chinese medicine combined with hypoglycemic western medicine in treatment of overweight/obese type 2 diabetes mellitus: a meta-analysis. Journal of Hunan University of Traditional Chinese Medicine . 2018;38:1043–1048. [Google Scholar]
- 29.Zhang W., Lei M. Therapeutic efficacy of Xiaoke formula in the treatment of type 2 diabetes mellitus with Qi and Yin Deficiency: a meta-analysis. Chinese Pharmacy . 2018;29(20):2851–2855. [Google Scholar]
- 30.Cheng Y., Lai Y. W., Gao T. S. Meta-analysis of clinical efficacy of Chinese herb medicine in treatment of type 2 diabetes mellitus with dampness heat and spleen deficiency. Clinical Journal of Traditional Chinese Medicine . 2018;30(02):264–269. [Google Scholar]
- 31.Ma C. Q., Hao Z. M. Meta-analysis of medical nutrition treatment in the type 2 diabetes comprehensive management. Diabetes New World . 2017;20:23–25. [Google Scholar]
- 32.Kong L. L., Zhang F. Meta analysis on randomized controlled study comparing traditional Chinese medicine and integrative medicine with western medicine in the treatment of type 2 diabetes. Chinese Drug Evaluation . 2012;29(01):41–47. [Google Scholar]
- 33.Shao T. T. Effect of Traditional Chinese Medicine Combining with Metformin on Type 2 Diabetes: A Systematic Review of Randomized Evidence . Chengdu, China: Chengdu University of Traditional Chinese Medicine; 2009. [Google Scholar]
- 34.Dugoua J. J., Seely D., Perri D., et al. From type 2 diabetes to antioxidant activity: a systematic review of the safety and efficacy of common and cassia cinnamon bark this article is one of a selection of papers published in this special issue (part 1 of 2) on the safety and efficacy of natural health products. Canadian Journal of Physiology and Pharmacology . 2007;85(9):837–847. doi: 10.1139/y07-080. [DOI] [PubMed] [Google Scholar]
- 35.Wang X., Tian J., Jiang J., et al. Effects of green tea or green tea extract on insulin sensitivity and glycaemic control in populations at risk of type 2 diabetes mellitus: a systematic review and meta-analysis of randomised controlled trials. Journal of Human Nutrition and Dietetics . 2014;27(5):501–512. doi: 10.1111/jhn.12181. [DOI] [PubMed] [Google Scholar]
- 36.Zhang X., Cao D., Yan M., Liu M. The feasibility of Chinese massage as an auxiliary way of replacing or reducing drugs in the clinical treatment of adult type 2 diabetes: a systematic review and meta-analysis. Medicine (Baltimore) . 2020;99(34) doi: 10.1097/md.0000000000021894.e21894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Piao C., Zhang Q., Jin D., et al. Treatment of type 2 diabetes with Tianqi Jiangtang capsule: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) . 2020;99(21) doi: 10.1097/md.0000000000019702.e19702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ma X. T. Clinical Investigation of Supplemented Banxiaxiexin Decoction on Glucose Control in Patients with Type 2 Diabetes and Spleen Deficiency and Stomach Heat Syndrome . Chengdu, China: Chengdu University of Traditional Chinese Medicine; 2020. [Google Scholar]
- 39.Hu J. H., Qian H. N., Bai X. F., Huang Z. H., Yang F. Network meta-analysis of the effectiveness of different Chinese patent medicines combined with metformin in the treatment of type 2 diabetes. Journal of Traditional Chinese Medicine . 2020;61:2163–2173. [Google Scholar]
- 40.Hu J. H., Qian H. N., Yang F., Huang Z. H., Bai X. F. Systematic review on the efficacy and safety of the prescription for the treatment from liver on type 2 diabetes mellitus. World Traditional Chinese Medicine . 2020;15(18):2709–2716. [Google Scholar]
- 41.Fu Y. Systematically Evaluate the Effect of Chinese Medicine on the Intestinal Flora of Patients with Type 2 Diabetes . Nanjing, China: Nanjing University of Chinese Medicine; 2020. [Google Scholar]
- 42.Gao H., Yang Y., Deng J., Liang J., Zhang W., Feng X. A systematic review and meta-analysis on the efficacy and safety of traditional Chinese patent medicine Jinqi Jiangtang tablet in the treatment of type 2 diabetes. Complementary Therapies in Medicine . 2019;47 doi: 10.1016/j.ctim.2019.01.016.102021 [DOI] [PubMed] [Google Scholar]
- 43.Huang F. Y., Deng T., Meng L. X., Ma X. L. Dietary ginger as a traditional therapy for blood sugar control in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine (Baltimore) . 2019;98(13) doi: 10.1097/md.0000000000015054.e15054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lian F., Jin D., Bao Q., Zhao Y., Tong X. Effectiveness of traditional Chinese medicine Jinlida granules as an add-on therapy for type 2 diabetes: a system review and meta-analysis of randomized controlled trials. Journal of Diabetes . 2019;11(7):540–551. doi: 10.1111/1753-0407.12877. [DOI] [PubMed] [Google Scholar]
- 45.Zheng Y., Ding Q., Wei Y., et al. Effect of traditional Chinese medicine on gut microbiota in adults with type 2 diabetes: a systematic review and meta-analysis. Phytomedicine . 2021;88 doi: 10.1016/j.phymed.2020.153455.153455 [DOI] [PubMed] [Google Scholar]
- 46.Zhou X., Chen J. Efficacy and safety of acupuncture and related techniques for type 2 diabetes mellitus: a systematic review of 21 randomised controlled trials. Metabolism . 2021;116 doi: 10.1016/j.metabol.2020.154519.154519 [DOI] [Google Scholar]
- 47.Hu Z., Liu X., Yang M. Evidence and potential mechanisms of Jin-Gui Shen-Qi Wan as a treatment for type 2 diabetes mellitus: a systematic review and meta-analysis. Frontiers in Pharmacology . 2021;12 doi: 10.3389/fphar.2021.699932.699932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jiang L., Wang S., Zhao J., et al. Qingre Yiqi method along with oral hypoglycemic drugs in treating adults with type 2 diabetes mellitus: a systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine . 2021;2021:11. doi: 10.1155/2021/4395228.4395228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mu G. Clinical Application of Coptis Chinensis-Cassia Bark in the Treatment of T2DM and its Effect on BA/TGR5/GLP-1 Pathway Based on Intestinal Flora . Beijing, China: Beijing University of Traditional Chinese Medicine; 2021. [Google Scholar]
- 50.Deng A. P. Effect of Traditional Chinese Medicine Combined with Metformin on Treating Insulin Resistance in Type 2 Diabetes Mellitus: A Meta-Analysis . Harbin, China: Heilongjiang University of Traditional Chinese Medicine; 2021. [Google Scholar]
- 51.Deng Z. Y., Wang M. J., Fan Y. H., Liu M. Meta-analysis of effect of Jinqi Jiangtang Tablets on treating insulin resistance in type 2 diabetes. Zhongguo Zhongyao Zazhi . 2020;45(1):188–195. doi: 10.19540/j.cnki.cjcmm.20190401.502. [DOI] [PubMed] [Google Scholar]
- 52.Tian J., Jin D., Bao Q., et al. Evidence and potential mechanisms of traditional Chinese medicine for the treatment of type 2 diabetes: a systematic review and meta-analysis. Diabetes, Obesity and Metabolism . 2019;21(8):1801–1816. doi: 10.1111/dom.13760. [DOI] [PubMed] [Google Scholar]
- 53.Zhao S. Y., Huang F., Feng Z. T., et al. Meta-analysis and trial sequential analysis of Liuwei Dihuang Pills (Tang) combined with metformin in the treatment of type 2 diabetes. Chinese Journal of Hospital Pharmacy . 2019;39(11):1158–1165. [Google Scholar]
- 54.Guo T. T. Meta-analysis of intensive treatment of type 2 diabetes mellitus with traditional Chinese medicine combined with insulin pump. Diabetes New World . 2019;22:51–52. [Google Scholar]
- 55.Tian H. P., Ren L., Yao H. P., Zhang L., Feng W. Y. Effect of the Qi-boosting and Yin-nourishing (Yi Qi Yang Yin) treatment as an adjuvant treatment of type 2 diabetes mellitus. A Meta-analysis World Chinese Medicine . 2019;14(05):1192–1197. [Google Scholar]
- 56.Dai Y. L., Liu W. N., Pang S. Q., Yang L., Li M. L. A systematic review of the effects of traditional Chinese medicine diet on blood glucose and quality of life in patients with type 2 diabetes. Journal of Guangxi University of Traditional Chinese Medicine . 2019;22(01):140–146. [Google Scholar]
- 57.Gu Y., Xu X., Wang Z., et al. Chromium-containing traditional Chinese medicine, Tianmai Xiaoke tablet, for newly diagnosed type 2 diabetes mellitus: a meta-analysis and systematic review of randomized clinical trials. Evidence-Based Complementary and Alternative Medicine . 2018;2018:8. doi: 10.1155/2018/3708637.3708637 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1: search strategy of CNKI (279). Supplementary Table 2: search strategy of VIP (112). Supplementary Table 3: search strategy of Wanfang Data (234). Supplementary Table 4: search strategy of PubMed (25). Supplementary Table 5: search strategy of Web of Science (157). Supplementary Table 6: search strategy of Embase (78). Supplementary Table 7: AMSTAR-2 scoring results.


