Abstract
Mandibular resections decision is one of the most important steps in oral cavity malignant or nonmalignant lesions associated with the mandible. The role of mandibular reconstruction is not only for cosmesis, but it is also indicated for functional rehabilitation such as swallowing, phonetics, and for facial symmetrical. Even though the free tissue transfer is considered a gold standard for mandibular reconstruction, the importance of nonvascularized bone grafts (NVBGs) such as fibula, calvarium, rib, sternum, and iliac are still persisting in mandibulectomies condition like patient who have not taken radiotherapy or not willing to undergo radiotherapy or not fit for free tissue transfer and provides a good contour of mandibular replacement. The success rate of NVBG depends upon patient selection, preoperative planning, and meticulous nursing care. Addition to NVBG, regional flaps such as pectoralis major myocutaneous (PMMC) flap will help in soft-tissue replacement of the defect as well as it will help in the situation where primary closure and airtight closure is not possible. This case report will discuss in detail about the management of anterior segmental mandibulectomy due to oncological resection and reconstruction with NVBG with fibula and PMMC.
Keywords: Mandibular resections, nonvascularized bone graft, pectoralis major myocutaneous flap, postoperative follow-up
INTRODUCTION
Mandibular resections followed by pathology or due to a trauma will lead to loss of continuity and results in loss of function and facial asymmetry.[1,2] Mandibular bone involving in pathological process is similar to the other bones in the body, and in many times, mandibular resections will be associated with or without the surrounding soft tissues.[3] Mandibular resections can be classified into either total or partial, in view of partial mandibulectomy; they are further classified into segmental, hemi, subtotal, unilateral free end, bounded unilateral segmental, marginal, and bounded bilateral mandibulectomy.[4] Usually, the choice of mandibular reconstructions for patients with malignant tumors will be alloplastic with osteosynthesis system to provide mechanical stabilization and to prevent the dislocation of mandibular stump caused by scarring.[5] The use of autogenous bone grafting such as nonvascularized from calvarium, rib, ilium, tibia, fibula, scapula, and radius is seen in the literature. Whereas over the period of 30 years, after the use of microvascular osseous free tissue transfer from fibula, scapula, iliac crest, and radius are having success rate of 90%.[6] The facial deformity reconstruction should be viewed in soft-tissue and hard-tissue replacement.[7] This report discuss about a 42-year-old male who had diagnosed with carcinoma of lower alveolus involving the midline, floor of mouth, and management of the deformity with the use of nonvascularized fibula and pectoralis major myocutaneous (PMMC) flap for the soft-tissue coverage for the defect in detail.
CASE REPORT
A 42-year-old gentle male, a daily wager, tobacco chewer, and ex-smoker with Eastern Co-operative Oncology Group Performance Status with no comorbidity, who had reported on December 2017, at oral cancer foundation, Karpaga Vinayaga Institute of Medical and Dental Sciences, Chengalpet District, Tamil Nadu, India, with a complaint of ulcer in the lower jaw for the past 45 days, incisional biopsy was done, histopathologically diagnosed with well-differentiated squamous cell carcinoma of the lower alveolus. On clinical examination, a ulceroinfiltrative lesion present in the lower alveolus with involvement of gingivobuccal sulcus from either side of the canine, floor of the mouth with subcutaneous skin involvement of submental region and no significant neck nodes in the neck [Figure 1a-c]. On radiological examination, contrast-enhanced computed tomography of the head and neck was taken, and it reveals ill-defined heterogeneous lesion with anterior mandibular bone erosion, involving mylohyoid muscle and loss of fat planes were noted in the submental region. Enlarged neck nodes were noted in right level IB region. Orthopantogram (OPG) reveals ill-defined radiolucency from left canine to right canine region, which is illustrating with a destructive lesion and floating tooth on the left side of the mandible [Figure 1c and d]. Based on clinical and radiological findings, the patient has cT4aN1M0 (AJCC 7th EDN) staging. Planned for curative intent of treatment, the patient was explained and choice of free tissue transfer for mandibular reconstruction. However, in the view of patient unacceptance and financial status, free tissue transfer fibula reconstruction was deferred. Ethic informed consent was obtained in before surgery. The patient was treated with composite resection (full-thickness wide excision of anterior mandible from first premolar on either side of the mandible as segmental mandibulectomy + floor of mouth excision), bilateral comprehensive neck dissection [Figure 2a-f]. Reconstruction was done with harvestment of nonvascularized bone grafts (NVBGs) fibula from the left leg measuring 6.5 cm, and fixation was done with 1–2 mm (4 hole) plates in the right side, 1–2 mm (2 hole) plates in the left side, and 6 numbers of 2 mm × 8 mm long screws [Figure 3a-e]. Bipaddled PMMC flap was harvested for soft-tissue coverage for NVBG, metronidazole was given, two layer water tight closure and air tight pressure drain was given in the neck and donor sites. The patient was on nasogastric tube feeding until 17 days, postoperative care with routine oral hygiene and follow-up. Excisional biopsy was reported as well-differentiated squamous cell carcinoma with all margins of free tumor and staged as pT4aN1. The patient was advised for adjuvant radiotherapy; however, the patient declined for it due to personal reason. The last follow-up was recorded in May 2018. On the 1st and 3rd month postoperative follow-up, OPG was revealed good bone formation in the left side as compared to the right side [Figure 3f] and donor site of fibula region shows no abnormalities other than bone harvest defect [Figure 3g].
Figure 1.
Preoperative pictures (from right top to down). (a and b) Extraoral clinical picture showing skin induration, (c) Intraoral picture of ulceroinfiltrative lesion involving floor of the mouth and lower alveolus, (d) Orthopantomogram, (e) CECT scan of the head and neck with axial and sagittal view
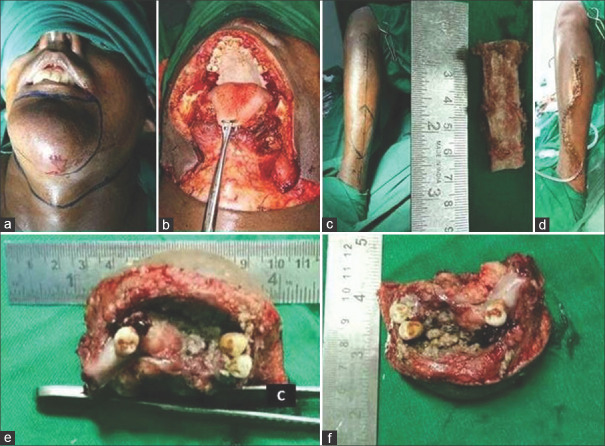
Figure 2.
Intra operative pictures (from right top to down). (a) Incision marking and (b) post excision defect, (c) harvestment of nonvascularized bone graft of fibula of 6.5 cm from left leg (d) closure of donor site with drain, (e and f) Specimen picture of full thickness wide excision of skin of chin with anterior segmental mandibulectomy and floor of the mouth with adequate margin
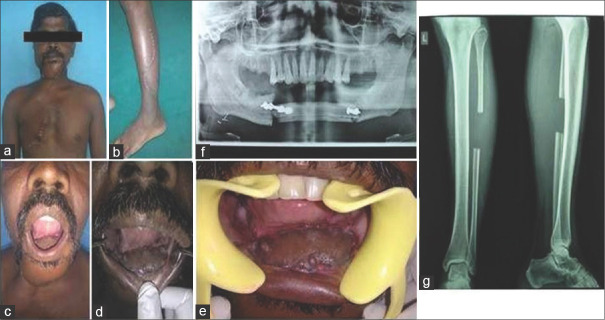
Figure 3.
(a and b) Postoperative pictures. (c and d) 1 month postoperative intraoral picture, (e) 3 month postoperative intra oral picture, (f) 3 month postoperative orthopantomogram, (g) 3 month postoperative anteroposterior and lateral view radiograph of the left leg
DISCUSSION
Surgical treatment is the primary choice of treatment in majority of head-and-neck squamous cell carcinoma (HNSCC). Recently, many reconstruction methods were performed by oncosurgeons to improve the outcomes. Reconstruction of segmental mandibular defects with NVBG and miniplate fixation has been found to improve the outcome in HNOSCC. The use of extensive soft-tissue coverage replaces the loss of soft tissue and absence of infection in the graft-recipient site.[1] The presented case demonstrated the use of nonvascularized fibula bone for mandibular bone replacement and PMMC flap for soft-tissue replacement in the extraoral chin region.
Mandibular resections due to oncology and nononcological reasons such as squamous cell carcinoma, ameloblastoma, Pindborg tumor, adenomatoid odontogenic tumor, central giant cell granuloma, odontogenic myxoma, dentigerous cyst, and odontogenic keratocyst.[6] These resection have higher success rate with autogeneous reconstruction for better functional outcome.[6] Szpindor had illustrated the 84% success rate of autogenous reconstruction in HNOSCC reconstruction surgery.[8] In our case, the patient had underwent composite resection as segmental mandibulectomy, wide local excision of floor of mouth, and full-thickness wide excision of the skin involving chin for the disease of squamous cell carcinoma of lower alveolus involving floor of the mouth. We included both canines are included along the midline. Reconstruction of large defects with free osseous tissue transfer was opted for reconstruction. There are various factors which may influence the technique outcome. These factors include socioeconomic status, nutrition, no comorbidities, quality of the vessels, vascularity of the recipient site and expertise, available time in the operating room, surgeon's skills, and preference and limited facilities.[9]
NVBG reconstruction has the chance of compromised vascularization; however, blood supply from periosteum, endosteum, and surrounding soft tissue can take care of this issue.[10] In this report, NVBG of 6.5 cm size was harvested with periosteum on both the distal and proximal ends and is used for miniplate fixation on either end of the mandible. Apart from mechanical stability given by plate and bone combination, intraoral and extraoral covering plays a major role in reconstruction.[5] The presence of dead spaces, salivary leak, and eventual contamination can lead to infection of the graft site and loss of graft.[2] This complication can be prevented providing metronidazole wash intraoperatively, watertight two-layer closure with drains, systemic antibiotics perioperatively, povidone-iodine gargle 6th hourly and on nasogastric feeds for 12 days. NVBG is contraindicated in patients treated with radiation therapy and adjuvant radiotherapy.[2] The patient was discharged on the 17th postoperative day (POD), followed up for 4 months. The orthopantamogram was taken on the 1st month POD and 3rd month POD, revealed partial radiodensity, and good radiodensity in the right side and left side, respectively. Clinically, graft was stable and no evidence of mobility or abnormality at the end of the 4th month POD which was the last follow-up of the patient.
CONCLUSION
NVBG can be used in segmental mandibular defects considering its higher success rate and less complication. NVBG is a good option with better outcome in cases of limited source for surgery or when patients is not fit free tissue transfer.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bai XF, Wushou A, Zheng J, Li G. An alternative approach for mandible reconstruction. J Craniofac Surg. 2013;24:e195–8. doi: 10.1097/SCS.0b013e3182802269. [DOI] [PubMed] [Google Scholar]
- 2.Moura LB, Carvalho PH, Xavier CB, Post LK, Torriani MA, Santagata M, et al. Autogenous non-vascularized bone graft in segmental mandibular reconstruction: A systematic review. Int J Oral Maxillofac Surg. 2016;45:1388–94. doi: 10.1016/j.ijom.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Chim H, Salgado CJ, Mardini S, Chen HC. Reconstruction of mandibular defects. Semin Plast Surg. 2010;24:188–97. doi: 10.1055/s-0030-1255336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adelusi EA. Classification of mandibulectomy/mandibular defects. World J Oral Maxillofac Surg. 2019;2:1032. [Google Scholar]
- 5.Maurer P, Eckert AW, Kriwalsky MS, Schubert J. Scope and limitations of methods of mandibular reconstruction: A long-term follow-up. Br J Oral Maxillofac Surg. 2010;48:100–4. doi: 10.1016/j.bjoms.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Rana M, Warraich R, Kokemüller H, Lemound J, Essig H, Tavassol F, et al. Reconstruction of mandibular defects-Clinical retrospective research over a 10-year period. Head Neck Oncol. 2011;3:23. doi: 10.1186/1758-3284-3-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallace CG, Wei FC. The current status, evolution and future of facial reconstruction. Chang Gung Med J. 2008;31:441–9. [PubMed] [Google Scholar]
- 8.Szpindor E. Evaluation of the usefulness of autogenic bone grafts in reconstruction of the mandible. Ann Acad Med Stetin. 1995;41:155–69. [PubMed] [Google Scholar]
- 9.Gadre PK, Ramanojam S, Patankar A, Gadre KS. Nonvascularized bone grafting for mandibular reconstruction: myth or reality? J Craniofac Surg. 2011;22:1727–35. doi: 10.1097/SCS.0b013e31822e633b. [DOI] [PubMed] [Google Scholar]
- 10.Akbay E, Aydogan F. Reconstruction of isolated mandibular bone defects with non-vascularized corticocancellous bone autograft and graft viability. Auris Nasus Larynx. 2014;41:56–62. doi: 10.1016/j.anl.2013.07.002. [DOI] [PubMed] [Google Scholar]