Abstract
Sensory impairment is common in older age and may be associated with intra- and interpersonal struggles. Treatment and intervention efforts may be hampered by functional difficulties or unwillingness to receive face-to-face mental health services. The current study seeks to assess the efficacy of an online psychological intervention for older adults with sensory loss and their spouses in Denmark, using a two-arm, parallel-group, randomized controlled trial study design. Participants will be randomly assigned to the intervention group or waiting list control group. The intervention consists of four digital, sequential modules that contain psychoeducation and Acceptance and Commitment Therapy inspired therapeutic activities. Individuals will be assessed at baseline, 6 weeks, and 10 weeks post-baseline, and for the intervention group only, at 18-weeks. The outcomes are well-being (primary), relationship satisfaction (secondary), and depressive symptoms (tertiary). The data will be analyzed using multilevel modeling to account for non-independence of data (nesting within participant and within couple). This is the first randomized controlled trial study of an online psychological intervention for older adults with sensory loss and their spouses and it will provide valuable knowledge regarding whether internet-delivered intervention is effective for this population group.
Keywords: Sensory loss, Hearing impairment, Vision impairment, Digital intervention, Acceptance and commitment therapy
Highlights
-
•
Sensory impairment is associated with reduced individual and relational well-being.
-
•
First digital intervention for older adults with sensory impair and their spouse
-
•
Based on ACT principles, program consists of 4 digital learning modules.
-
•
Program may provide more flexible and cost-effective treatment alternatives.
In it together: using acceptance and commitment therapy to treat distress among older adults with sensory loss and their spouses
Impairments in hearing and/or vision are common in older age. Within Europe, the prevalence rates of hearing and vision impairment are approximately 20–40 % (Roth et al., 2011; Viljanen et al., 2013). Because of ageing populations and widespread increases in known sensory loss-related risk factors such as diabetes, it is expected that the prevalence of sensory loss will only increase, as will its associated mental health burden (Rein et al., 2009; Wallhagen et al., 1997).
With sensory impairment comes increased communication difficulties, social isolation, and psychological distress, for the impaired person and their spouse (Lehane et al., 2017; Lehane et al., 2018a). Further, older adults with sensory loss and their spouses are known to have greater risk of mental health difficulties, such as depression and anxiety, compared to their sighted and hearing counterparts (Lehane et al., 2018a). Perhaps due to emotional contagion, when the impaired person reports depression, partners are also more likely to experience depression (Goodman and Shippy, 2002). Moreover, both partners report decreased relationship satisfaction and greater relationship inequity, in part due to reduced and poorer communication and loss of shared activities (Lehane et al., 2017). Consequently, these negative outcomes make the development of interventions that target individual and relational well-being in this population a research and societal priority (Lehane et al., 2016).
One psychological evidence-based treatment for chronic illness-related distress is Acceptance and Commitment Therapy (ACT; Harris, 2006; Podina et al., 2018). The aim of ACT is to foster greater psychological flexibility, such that people are better able to respond adaptively to challenges and to maintain active engagement with one's own life (Dindo et al., 2017). Psychological flexibility is achieved through 1) being present in the moment, that is, bringing full awareness and engagement to current experiences, with openness, interest, and receptiveness, 2) stepping back from negative thoughts and recognize that they are transient events that will pass (cognitive defusion), and 3) making room for unpleasant feelings and thoughts, without resisting them or giving them undue attention (acceptance and willingness). This should facilitate a recognition that 4) thoughts, feelings, and actions are context-dependent, and does not constitute an identity or essence of self (self as context), that 5) it is important to clarify what is important and what one's core goals are (values), and 6) that one can take effective action to achieve one's goals or live by one's values (committed action) (Dindo et al., 2017; Hayes et al., 2006; Podina et al., 2018). Within the ACT model, workability is a key process to effect change; that is, to help people develop greater (non-judgmental) awareness of behaviors, and whether those behaviors “work” to effectively solve the problem, or simply provide short-term symptom relief. Identification of “unworkable” behavioral patterns should then motivate behavioral changes aligning with one's values and goals (Dindo et al., 2017; Hayes et al., 2006).
By virtue of its focus on acceptance and workability, as opposed to change, ACT is an especially suitable treatment for distress related to chronic conditions (Dindo et al., 2017; Feliu-Soler et al., 2018), including sensory loss, where people's fears are often grounded in the realities of their own/spouse's health condition. Indeed, research suggests that acceptance of sensory impairment by both the self and the partner is associated with reduced psychological distress (Lehane et al., 2018b; Yorgason et al., 2007). Support for the use of ACT in the context of hearing loss was found in a recent pilot intervention trial, which showed promising results with significant psychological gains in the treatment group (Molander et al., 2018). However, the trial included a small sample, did not include those with vision loss or dual-sensory loss, or spouses, did not focus on elderly persons, and involved one-to-one therapist-client contact. Thus, it is unclear whether the findings are reliable and generalizable to a larger population and to older adults and their spouses. Furthermore, interventions requiring one-to-one client contact cannot easily be scaled to entire populations/large cohorts and integrated into current care systems at a reasonable cost, and thus, run the risk of not being implemented, regardless of their promising potential. For these reasons, we sought to create a short digital intervention, aimed at older adults with sensory loss and their romantic partners.
The intervention was conceptualized to be applicable across a range of partner impairment constellations (e.g., whether only one or both partners are impaired, and whether there is single or dual sensory impairment for one or both partners). Moreover, as both partners in a couple may experience negative effects (from either their partner's impairment or their own), we wished to create an intervention that focused on individual and couple well-being and adjustment. Though the intervention targets relational functioning, the intervention was constructed such that individuals complete it individually. The intervention consists of 4 digital learning modules, which are accessed online from a computer, mobile device, or tablet. Each module takes 20–30 min to complete. The modules are sequentially ordered and time locked; a new module is opened, when 7 days have passed since the previous module was completed. Fig. 1 provides an overview of module topics and content. All materials in the intervention are provided in text format only, but with associated speak for those with vision impairment. The objective is to provide a combination of psychoeducation and therapeutic activities, inspired by Acceptance and Commitment Therapy (Harris, 2009a, Harris, 2009b) and positive psychology (Seligman et al., 2005). The activities seek to increase insight into thoughts, feelings, and behaviors, as well as provide participants with an opportunity to develop plans for behavior change. A participant can skip an exercise within a module, if desired; skipping is done by simply clicking the next button on the relevant pages. Module 1 covers living with sensory loss, including information about the prevalence of sensory loss and normalization of the thoughts and feelings that come with the experience. The “Bulls Eye” (Harris, 2009a) activity then encourages participants to focus on what is important to them (their values) and to assess whether and how they may live according to those values. Module 2 covers the connection between thoughts, feelings, and actions. The objective is to highlight to participants that negative thoughts occur and to be comfortable with these (defusion and acceptance). The two activities (“Join the Dots” and “Struggling versus Opening Up”; Harris, 2009a) seek to bring awareness to adaptive and maladaptive coping strategies that participants may use when experiencing negative or unwanted thoughts and feelings. Module 3 covers how a sensory impairment may affect the dynamics between partners, including communication and displays of affection. The activities (“Appreciating your Partner” and “Value-Guided Actions”; Harris, 2009b) allow the participants to consider positive features of the partner and the relationship, and to develop a plan for how to connect with the partner (values and committed action). Module 4 serves to summarize the learning objectives of Modules 1, 2, and 3, as well as to allow participants to develop an action plan for the future (values and committed action).
Fig. 1.
In It Together: intervention structure and content.
At the end of modules 1, 2, and 3, participants are provided with the option to choose from two optional homework exercises that seek to reinforce the material covered in the module. Participants can choose to complete none, one, or both homework assignments. These homework assignments can be completed individually or in collaboration with the partner. The instructions are provided via a short video (text-based, with voice-over), and the assignment is to be completed over the course of the week before the next module opens up. Participants can print the homework exercise and complete it on paper, or they can log into the intervention platform and enter their answers in the module. They also have the opportunity to provide feedback on whether they completed the homework exercise and if so, what went well or poorly. In providing feedback regarding the homework exercise, participants can request a response from a person with a degree in psychology. Participants can also connect with the person through a “mailbox”, where they can post anonymous questions or stories about anything they choose; posts are visible to other platform users, though only the psychologist can respond.
To investigate the effects of our digital intervention, we employ a longitudinal randomized controlled trial study design. We mainly seek to improve well-being and relationship satisfaction and reduce depressive symptoms among older individuals, aged 60 and older, with hearing and/or vision impairment and their partners.
We have developed the following primary hypotheses:
H1
Those in the intervention group will report significantly greater well-being as compared to those in the control group at 6 and 10 weeks post-baseline.
H2
Those in the intervention group will report significantly higher relationship satisfaction as compared to those in the control group at 6 and 10 weeks post-baseline.
H3
Those in the intervention group will report significantly lower depression symptomology as compared to those in the control group at 6 and 10 weeks post-baseline.
We also developed the following secondary hypotheses:
H4
Those in the intervention group will report significantly greater acceptance (i.e., psychological flexibility) as compared to those in the control group at 6 and 10 weeks post-baseline.
H5
Those in the intervention group will report significantly greater satisfaction with communication with partner, as compared to those in the control group at 6 and 10 weeks post-baseline.
The study will contribute with knowledge regarding the acceptability and efficaciousness of a short digital intervention for aiding elderly people with sensory impairment and their spouses with their psychosocial well-being.
1. Method
1.1. Eligibility criteria and sample size
We have obtained a random sample of individuals and their spouse from Danish Agency of Health Research Services, who pulled person register numbers from the Central Person Registry (CPR). The register contains individual person register numbers, as well as information regarding familial associations (e.g., spousal relationships) and addresses. We provided the following specifications in obtaining our sample: People had to be 1) Danish citizens, 2) 60 years of age or older, 3) registered as residing at the same address in Denmark, and 4) married or registered partners (for individuals in same-sex relationships) with each other.
Additional eligibility criteria will be assessed via self-report at the baseline survey (please see doi:10.17605/OSF.IO/5WTR3 for question wording). These include 5) being able to read and write in Danish, 6) being in a relationship with their partner for 1 year or longer, and 7) perceiving that they or their partner has a sensory impairment (hearing, sight, or dual-sensory impairment) that affects their daily life. Answers to questions regarding sensory impairment will be provided for hearing and sight separately. Participants are ineligible for the study if they report receiving psychological therapy or intervention.
We conducted an a priori power analysis to determine the required minimum sample size for an independent samples t-test (comparison of the intervention and control groups at the 6-week assessment), using the formulas presented by Clifton et al. (2019).1 We elected to power the study to detect differences for depression, our tertiary outcome, using the results of Molander et al. (2018) as a basis for our calculations (e.g., estimate of variability in the data), as they represented a comparable study (i.e., employed the same outcome measure and did an ACT-based intervention for hearing impaired individuals). The calculations were performed in Excel (shared at doi:10.17605/OSF.IO/5WTR3). The power analyses suggested that we will need 251 units (couples; ~125 couples per group) to detect a Cohen's d effect of 0.35, at power = 0.80 and an alpha level = 0.05. We anticipate a small to moderate effect (d = 0.35), as it may be difficult to affect depressive symptoms through a brief online intervention. Thus, we elected to power ourselves to find a more difficult-to-detect effect.
Based on previous experience in digital intervention research (e.g., Hald et al., 2020), we expect an attrition rate of 70 %. Thus, we calculated that we need to recruit 839 couples to participate. Furthermore, based on past research that recruited participants from a similarly aged population (elderly men, over the age of 60), we expect an invitation response rate of roughly 15 % (Grønkjær et al., 2019). Thus, we further calculated that we would need to invite 5593 couples. As the invitation response rate may vary from the previous study, we requested information on 6000 couples from the Danish Agency of Health Research Services.
We elected to conduct a run-in period using 1000 couples (500 couples from the intervention control and 500 couples from the control group), to examine whether there were any issues with the intervention platform and study flow. We discovered a flow issue that prevented participants from progressing through the intervention. In programming the intervention, the module completion point (from which the system would unlock the next module, after a delay of 7 days) was set to be upon completion of the homework, however, as the homework was optional, participants who elected not to complete the homework were prevented from progressing to the next module. This flow error was rectified and the module completion point was set to the conclusion page (see Fig. 1). Thus, the final invitation sample size is 5000 couples (10,000 people).
1.2. Ethical approval and protocol registration
All procedures in this study are in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. We received ethical approval from the University of Copenhagen Research Ethics Committee for Science and Health (protocol number 504-0225/20-5000), as well as from the Danish Data Protections Agency. The study was exempt from further ethical evaluations following the rules and regulations as set forth by the Scientific Ethical Committees of Denmark (i.e., national ethics approval was not required).
The protocol is registered with clinicaltrials.gov prior to data collection (ClinicalTrials.gov Identifier: NCT04781608) as well as on Open Science Framework (doi:10.17605/OSF.IO/5WTR3).
1.3. Procedure
Upon receipt of the random sample from the Danish Agency of Health Research Services and prior to invitation into the study, participants are assigned to the intervention group or the waitlist control group; assignment occur at the couple level, such that both partners are in the same group (intervention or control). As the sample is randomly selected from the population and arrive in random order, assignment to condition is random.
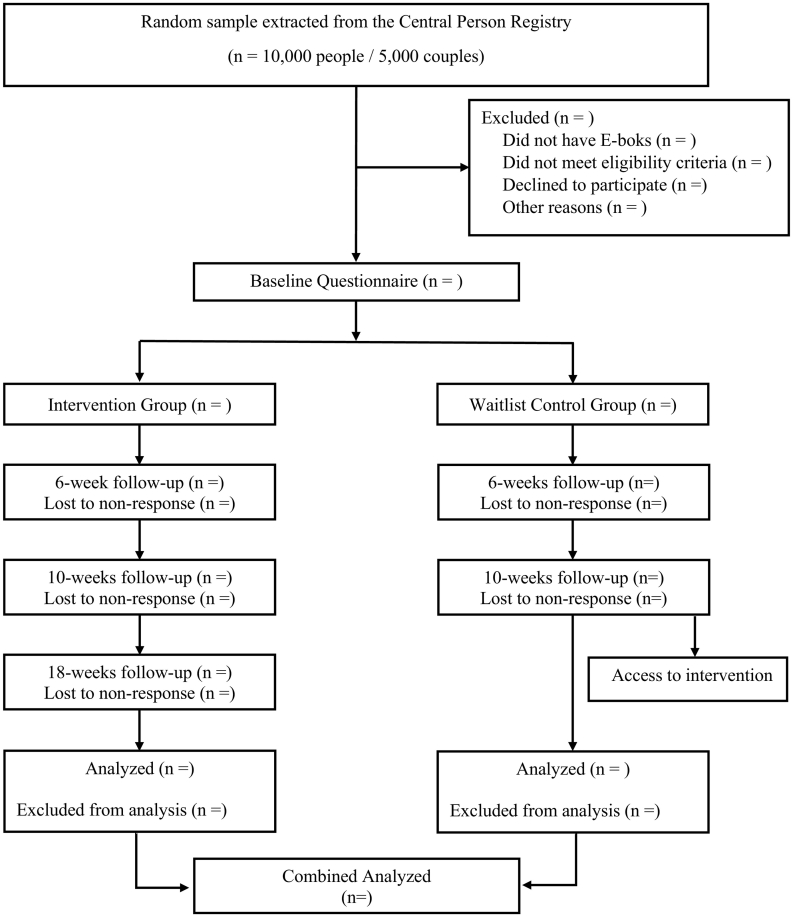
Participants receive an invitation letter through their individual national online mailbox (e-Boks; a secure electronic mailbox used to receive digital mail from the public and private sector, such as one's bank). The invitation letter indicates that invitees are eligible for study participation, regardless of their level of impairment, as long as the participants feels that the impairment affects their daily lives. Moreover, invitees are assured that they can participate, even if their partner does not wish to do so. The invitation letter includes a link to an informational page that describes the study aims and procedures. It also provides a link to the screening survey, which assesses eligibility for the study, as well as a custom username and password to be entered into the survey and used to access the intervention platform. Each partner in the couple is provided individual login information to the platform and to the surveys. Those that do not meet the eligibility criteria are thanked for their interest and routed out of the study.2 Those that meet the eligibility criteria are routed on to the consent form, which describe the study content and procedure, and that participation is voluntary. Those that provide study consent proceed to the demographic questions and the baseline survey. Within the baseline survey, participants provide a private e-mail address (not shared with the partner)3 to be used to send follow-up surveys at 6 weeks, 10 weeks, and for the intervention group only, 18 weeks post-baseline. Upon completion of the baseline survey, those in the intervention group are provided with the link to the intervention platform directly on screen and in an e-mail to their private e-mail address. Those in the waitlist control condition are informed that they will receive access to the platform after the 10-week survey (please see CONSORT diagram, Fig. 2).
Fig. 2.
CONSORT diagram.
Participants in the intervention group are informed that the intervention platform consist of four modules to be completed one week apart, for a total of 4 weeks. They receive reminder e-mails 3 days before they are to do a module (reminder emails sent out before module 2, 3, and 4), as well as on the day of the module. Although the instructions tell the participants of this schedule, they are able to take longer to complete the 4 modules (i.e., access to the intervention is not restricted after 4 weeks).
1.4. Measures
Participants will complete the below set of questionnaires at all time points (baseline, 6 weeks, 10 weeks, and 18 weeks), with the exception of the eligibility criteria and demographics questions, which will only be assessed at baseline. The measures document and codebook, with both English and Danish language versions of the items, can be found on doi:10.17605/OSF.IO/5WTR3.
1.4.1. Demographic questions
1.4.1.1. General demographic questions
Participants report on their gender, the gender of their romantic partner, age of romantic partner, and their highest level of education. Additionally, we ask whether anyone is helping them to complete the survey, with instructions that the partner must not be the helper. Moreover, participants are asked about potential comorbid issues using a validated checklist (Teglbjærg et al., 2018); the list comprises 18 physical and psychological conditions, such as diabetes, arthritis, dementia, or chronic depression. Participants respond whether they (1) have the condition currently, (2) have had the condition, but do not have it currently, or (3) have never had the condition.
1.4.1.2. Sight impairment questions
Participants are asked whether they usually wear glasses or contacts, 1) how good their vision is in general, 2) when seeing at a distance, and 3) when seeing up close (with or without glasses, as they would normally do). They are also asked whether they use any other aids and what the reason for their impairment is, if they know. These questions are taken from the Danish language version of the Survey of Health, Ageing and Retirement in Europe (SHARE) project (http://www.share-project.org/home0.html).
1.4.1.3. Hearing impairment questions
Participants are asked whether they normally wear a hearing aid, 1) how good their hearing is in general, and 2) whether it is difficult to follow a conversation when there is background noise (e.g., from a TV or radio), 3) in a conversation with multiple people, and 4) in a conversation one-on-one. They are also asked whether they use any other aids and what the reason for their impairment is, if they know. These questions are taken from the Danish language version of the Survey of Health, Ageing and Retirement in Europe (SHARE) project (http://www.share-project.org/home0.html).
1.4.2. Outcomes measures
1.4.2.1. Well-being
The 5-item WHO well-being measure is used in its Danish version (Bech, 1999, Bech, 2012). Participants are asked to what extent the statements reflect how they have felt over the last two weeks, and the statements are rated on a scale ranging from “at no time” (0) to “all the time” (5). An example item includes “I have felt active and vigorous.” Well-being serves as our primary outcome.
1.4.2.2. Relationship satisfaction
The 4-version of the Couple Satisfaction Index (CSI; Funk and Rogge, 2007) is used to measure relationship satisfaction, our secondary outcome. The items assess participants' feelings of happiness and satisfaction with the relationship. An example item includes “In general, how satisfied are you with your relationship?” and the response options range from “not at all” (0) to “completely” (5). The first and last author translated the items from English to Danish.
1.4.2.3. Depression
Depression is measured using the Danish version of the 9-item Patient Health Questionnaire (PHQ-9). The statements map onto DSM-IV criteria for depression and can therefore be used as a screening tool (Kroenke and Spitzer, 2002; Kroenke et al., 2001). Participants are asked to what extent the statements reflect how they have felt over the last two weeks and the statements are rated on a “not at all” (0) to “nearly every day” (3) scale. An example item includes “Feeling down, depressed, or hopeless?” Depression serves as our tertiary outcome.
1.4.3. Process measures
1.4.3.1. Acceptance
The Acceptance and Commitment theory construct of acceptance is measured using the Danish version of the 7-item Acceptance and Action Questionnaire (Bond et al., 2011; Hoffman et al., 2018). Items are rated on a scale ranging from “Never true” (1) to “always true” (6), and an example item includes “I worry about not being able to control my worries and feelings.”
1.4.3.2. Communication with partner
To assess communication, we use the 12-item Couple Communication Satisfaction Scale (Jones et al., 2018). As no Danish translation exists, the first and third author and a research assistant translated the scale. The scale assesses satisfaction with own and partner contributions to conversations, own emotional experiences and partner responsiveness during conversations, and conversation characteristics, such as frequency of conversation and variety of topics. An example item includes “The balance between what I give and receive when communicating”. Items are rated on a “not at all satisfied” (1) to “extremely satisfied” (5) scale.
1.4.3.3. Impact of sensory impairment
The Impact of Illness Questionnaire (Klimidis et al., 2001) is used to assess the extent to which participants perceive that their sensory impairment affects their daily functioning over the past 3 months. Statements are rated on a scale from “not at all” (0) to “fully” (3). An example item includes “To what extent (if at all) has your capacity to meet family obligations or expectations been reduced by your sensory impairment?” The impact of illness scale was chosen for its greater focus on socio-emotional challenges, as these may be particularly prevalent and salient to individuals with sensory loss and more relevant for psychological intervention, rather than issues related to physical impairment (bathing and dressing, cooking; issues addressed by the Activities of Daily Life scale, Lawton and Brody, 1969). As no Danish translation exists, the first and third author and a research assistant translated the scale.
1.4.4. User variables
The digital platform provides information regarding completion of modules, the feedback participants provide about homework completion and their requests for feedback from a (non-licensed) psychologist. “Module completion” is defined within the digital platform as viewing the conclusion page (see https://osf.io/39gj6/ for an overview of the number of pages per module and their titles), while “homework completion” is participant self-reported.
Each module also asks participants whether the experience of the module was positive or negative (“very negative” (1) to “very positive” (7)) and to what degree the module was useful to them (“Not at all” (1) to “To a very high degree” (5)).
1.5. Statistical analyses
We will begin by assessing the number of dyads in the study, as well as the attrition rate over time. Given the potential nesting of participants within couple, all analyses will be conducted within a multilevel modeling framework, accounting for dyadic interdependence in the data. As participants are able to participate, even if their partner do not, in all analyses, we will use the individual participant's responses as the unit of analysis. Attrition bias analyses will be conducted, comparing participants who only complete baseline to those who remain in the study after baseline, using multilevel logistic regression, with drop-out as the outcome and baseline sociodemographic and psychological variables as predictors.
To examine the effectiveness of the intervention, multilevel regressions will be conducted to examine group differences in H1) well-being, H2) relationship satisfaction, and H3) depression at 6 and 10 weeks post-baseline. Group member (intervention vs. control) and time (baseline, 6 weeks, and 10 weeks) will be entered as categorical predictors, and the model will be specified to allow for interdependence due to nesting of responses within participants and participants within couple (i.e., longitudinal actor-partner interdependence modeling [APIM]; Cook and Kenny, 2005; Kenny et al., 2006). Thus, in these analyses, participant responses are the unit of analysis. Initial analyses will be based on the intention-to-treat principle (Gupta, 2011). Sensitivity analyses (Thabane et al., 2013) will be conducted to adjust for participants' self-reported sensory impairment (vision and hearing assessed separately), gender, age, educational level, and impact of sensory impairment; additionally, given the potential for a large attrition rate, we will also conduct the analyses on complete cases only.
2. Discussion
For many, sensory impairment is associated with increased interpersonal difficulties, social isolation, trouble with communication, and intra-personal difficulties, such as loneliness, depression, and psychological distress (Lehane et al., 2017; Lehane et al., 2018b). Thus, psychosocial interventions that target individual and relational well-being are a research and societal priority (Lehane et al., 2016). This protocol represents, to our knowledge, a first attempt at examining the effectiveness of a digital intervention in improving well-being, relationship satisfaction, and depression symptomology among the heterogeneous population of older individuals with sensory loss and their spouses, using an RCT study design.
There are some limitations to the study. For one, study attrition may be significant and may occur for several reasons. Participants may make typos when entering their e-mail address into the baseline survey, which may prevent them from receiving study-related information and links to follow-up surveys. Moreover, some people may report a sensory impairment that affects their daily life, but not perceive that the intervention is of relevance or value to them. Relatedly, one partner in the couple may report an impairment (for themselves or the partner), though the other partner does not (for neither themselves nor their partner); thus, it may be that this will reduce our ability to recruit couples. And some participants may elect to drop out of the study due to lack of cognitive and emotional resources (e.g., “it is too much for me to do right now”). Moreover, for some older people, digital help may not be acceptable, as not all older people are adept at navigating a computer and web-browser, which may prevent them from using the service. However, as populations age, more people will be computer-native and thus, able to access and use a digital intervention. Lastly, there may be self-selection into the study, as many studies have found that those with better health, higher education and income, and of female gender are more likely to seek treatment (Wellstead, 2011) and to participate in research studies (Søgaard et al., 2004).
In sum, the present study will contribute to the extant knowledge about effectiveness of digital interventions, with a specific focus on older adult with sensory impairment and their spouses. As there is currently no digital aid available to this population, the present study is a first mover that seeks to offer a more cost-effective evidence-based scalable psychological help for people with sensory impairment (and their spouses), who may need it.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
This work was supported by ‘VELUX FONDEN’ (to the first author) under Grant No. 00022361.
We did not calculate power as change from baseline, as we did not have sufficient information regarding the standard error for the mean change score. Moreover, we elected to estimate power for a between-subjects test, rather than a within-subjects or a dyadic test, as we had insufficient information for estimating power for such tests.
It is possible for one partner in the couple to be eligible for study participation and the other to not be eligible. Given that participants are able to sign up asynchronously, that eligibility is based on own perceptions of their/their partner's sensory impairment, and that participants had to provide individual consent and contact information, we are unable to direct both partners to participate.
Participants are instructed that if they share an e-mail address with their partner and wish to participate in the study, they have to contact the study team, who then manually set up individual e-mails to the participants. The e-mails were clearly marked with the name of the person, so that participants know which e-mail is addressed to them and which link to click.
Contributor Information
Camilla S. Øverup, Email: Camilla.oeverup@sund.ku.dk.
Gert Martin Hald, Email: ghald@sund.ku.dk.
References
- Bech P. Health-related quality of life measurements in the assessment of pain clinic results. Acta Anaesthesiol. Scand. 1999;43(9):893–896. doi: 10.1034/j.1399-6576.1999.430906.x. [DOI] [PubMed] [Google Scholar]
- Bech P. John Wiley & Sons; 2012. Clinical Psychometrics. [Google Scholar]
- Bond F.W., Hayes S.C., Baer R.A., Carpenter K.M., Guenole N., Orcutt H.K., Waltz T., Zettle R.D. Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: a revised measure of psychological inflexibility and experiential avoidance. Behav. Ther. 2011;42(4):676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Clifton L., Birks J., Clifton D.A. Comparing different ways of calculating sample size for two independent means: a worked example. Contemp.Clin.Trials Commun. 2019;13 doi: 10.1016/j.conctc.2018.100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook W.L., Kenny D.A. The Actor-Partner Interdependence Model: a model of bidirectional effects in developmental studies. Int. J. Behav. Dev. 2005;29(2):101–109. doi: 10.1080/01650250444000405. [DOI] [Google Scholar]
- Dindo L., Van Liew J.R., Arch J.J. Acceptance and commitment therapy: a transdiagnostic behavioral intervention for mental health and medical conditions. Neurotherapeutics. 2017;14(3):546–553. doi: 10.1007/s13311-017-0521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feliu-Soler A., Montesinos F., Gutiérrez-Martínez O., Scott W., McCracken L.M., Luciano J.V. Current status of acceptance and commitment therapy for chronic pain: a narrative review. J. Pain Res. 2018;11:2145–2159. doi: 10.2147/JPR.S144631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk J.L., Rogge R.D. Testing the ruler with item response theory: increasing precision of measurement for relationship satisfaction with the couples satisfaction index. J. Fam. Psychol. 2007;21:572–583. doi: 10.1037/0893-3200.21.4.572. [DOI] [PubMed] [Google Scholar]
- Goodman C.R., Shippy R.A. Is it contagious? Affect similarity among spouses. Aging Ment. Health. 2002;6:266–274. doi: 10.1080/13607860220142431. [DOI] [PubMed] [Google Scholar]
- Grønkjær M., Osler M., Flensborg-Madsen T., Sørensen H.J., Mortensen E.L. Associations between education and age-related cognitive changes from early adulthood to late midlife. Psychol. Aging. 2019;34(2):177–186. doi: 10.1037/pag0000332. [DOI] [PubMed] [Google Scholar]
- Gupta S.K. Intention-to-treat concept: a review. Perspect.Clin.Res. 2011;2:109–112. doi: 10.4103/2229-3485.83221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hald G.M., Ciprić A., Øverup C.S., Štulhofer A., Lange T., Sander S., Kjeld S.G., Strizzi J.M. Randomized controlled trial study of the effects of an online divorce platform on anxiety, depression, and somatization. J. Fam. Psychol. 2020;34(6):740–751. doi: 10.1037/fam0000635. [DOI] [PubMed] [Google Scholar]
- Harris R.F. Embracing your demons: an overview of acceptance and commitment therapy. Psychother.Austr. 2006;12:70. [Google Scholar]
- Harris R. New Harbinger Publications; Oakland, CA: 2009. ACT Made Simple: An Easy-to-read Primer on Acceptance And Commitment Therapy. [Google Scholar]
- Harris R. New Harbinger Publications; Oakland, CA: 2009. ACT With Love: Stop Struggling, Reconcile Differences, And Strengthen Your Relationship With Acceptance And Commitment Therapy. [Google Scholar]
- Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav. Res. Ther. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hoffman D., Rask C.U., Hedman-Lagerlöf E., Ljótsson B., Frostholm L. Development and feasibility testing of internet-delivered acceptance and commitment therapy for severe health anxiety: pilot study. JMIR Ment.Health. 2018;5(2) doi: 10.2196/mental.9198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A.C., Jones R.L., Morris N. Development and validation of the couple communication satisfaction scale. Am. J. Fam. Ther. 2018;46(5):505–524. doi: 10.1080/01926187.2019.1566874. [DOI] [Google Scholar]
- Kenny D.A., Kashy D.A., Cook W.L. Guilford Press; 2006. Dyadic Data Analysis. [Google Scholar]
- Klimidis S., Minas I.H., Yamamoto K. Impact of illness scale: reliability, validity, and cross-cultural utility. Compr. Psychiatry. 2001;42(5):416–423. doi: 10.1053/comp.2001.26266. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr. Ann. 2002;32(9):509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton M.P., Brody E.M. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- Lehane C.M., Wittich W., Dammeyer J. Couples' experience of sensory loss: A research and rehabilitation imperative. Hear.J. 2016;69:34–36. doi: 10.1097/01.HJ.0000491116.66672.40. [DOI] [Google Scholar]
- Lehane C.M., Dammeyer J., Elsass P. Sensory loss and its consequences for couples' psychosocial and relational wellbeing: an integrative review. Aging Ment. Health. 2017;21(4):337–347. doi: 10.1080/13607863.2015.1132675. [DOI] [PubMed] [Google Scholar]
- Lehane C.M., Hofsöe S.M., Wittich W., Dammeyer J. Mental health and spouse support among older couples living with sensory loss. J.AgingHealth. 2018;30(8):1205–1223. doi: 10.1177/0898264317713135. [DOI] [PubMed] [Google Scholar]
- Lehane C.M., Nielsen T., Wittich W., Langer S., Dammeyer J. Couples coping with sensory loss: a dyadic study of the roles of self- and perceived partner acceptance. Br. J. Health Psychol. 2018;23(3):646–664. doi: 10.1111/bjhp.12309. [DOI] [PubMed] [Google Scholar]
- Molander P., Hesser H., Weineland S., Bergwall K., Buck S., Malmlöf J.J., Andersson G.… Internet-based acceptance and commitment therapy for psychological distress experienced by people with hearing problems: a pilot randomized controlled trial. Cogn. Behav. Ther. 2018;47(2):169–184. doi: 10.1080/16506073.2017.1365929. [DOI] [PubMed] [Google Scholar]
- Podina L.R., David D., Mogoaşe C. In: Cognitive Behavior Therapies: A Guidebook for Practitioners. Vernon A., Doyle K.A., editors. American Counseling Association; Alexandria, VA: 2018. Acceptance and commitment therapy; pp. 177–208. [Google Scholar]
- Rein D.B., Wittenborn J.S., Zhang X., Honeycutt A.A., Lesesne S.B., Saaddine J., Vision Health Cost-Effectiveness Study Group Forecasting age-related macular degeneration through the year 2050: the potential impact of new treatments. Arch. Ophthalmol. 2009;127(4):533–540. doi: 10.1001/archophthalmol.2009.58. [DOI] [PubMed] [Google Scholar]
- Roth T.N., Hanebuth D., Probst R. Prevalence of age-related hearing loss in Europe: a review. Eur. Arch. Oto-Rhino-Laryngol. 2011;268(8):1101–1107. doi: 10.1007/s00405-011-1597-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman M.E.P., Steen T.A., Park N., Peterson C. Positive psychology progress: empirical validation of interventions. Am. Psychol. 2005;60(5):410–421. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- Søgaard A.J., Selmer R., Bjertness E., et al. The Oslo Health Study: the impact of self-selection in a large, population-based survey. Int. J. Equity Health. 2004;3:3. doi: 10.1186/1475-9276-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teglbjærg J.H., Hovaldt H.B., Lehane C., Dammeyer J. Aetiologies of acquired deafblindness in a national sample. Br. J. Vis. Impair. 2018;36(2):175–189. doi: 10.1177/0264619618758352. [DOI] [Google Scholar]
- Thabane L., Mbuagbaw L., Zhang S., Samaan Z., Marcucci M., Ye C., Thabane M., Giangregorio L., Dennis B., Kosa D., Debono V.B., Dillenburg R., Fruci V., Bawor M., Lee J., Wells G., Goldsmith C.H. A tutorial on sensitivity analyses in clinical trials: the what, why, when and how. BMC Med. Res. Methodol. 2013;13(1) doi: 10.1186/1471-2288-13-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viljanen A., Törmäkangas T., Vestergaard S., Andersen-Ranberg K. Dual sensory loss and social participation in older Europeans. Eur. J. Ageing. 2013;11(2):155–167. doi: 10.1007/s10433-013-0291-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallhagen M.I., Strawbridge W.J., Cohen R.D., Kaplan G.A. An increasing prevalence of hearing impairment and associated risk factors over three decades of the Alameda County Study. Am. J. Public Health. 1997;87(3):440–442. doi: 10.2105/ajph.87.3.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellstead P. Information behaviour of Australian men experiencing stressful life events: the role of social networks and confidants. Inf. Res. 2011;16(2) 16-2. [Google Scholar]
- Yorgason J.B., Piercy F.P., Piercy S.K. Acquired hearing impairment in older couple relationships: an exploration of couple resilience processes. J. Aging Stud. 2007;21:215–228. doi: 10.1016/j.jaging.2006.10.002. [DOI] [Google Scholar]