Abstract
The use of levamisole as the most frequent adulterant of cocaine has merged in previously unknown toxicities, notably a disease entity called cocaine/levamisole-associated autoimmune syndrome (CLAAS). Clinically, CLAAS can manifest with diverse cutaneous and extracutaneous features sharing common laboratory findings (neutropenia, autoantibody patterns). We report the case of a cocaine-abusing female patient with relapsing episodes of painful ulcers, worsening and expanding over a three-year period. The case exhibited all features of a drug-induced, skin-limited, ANCA-associated vasculitis, evolving over time to PG-like findings. In both disease stages, the patient responded well to the cessation of cocaine exposure and systemic glucocorticosteroids. This case demonstrates the continuous nature of cutaneous CLAAS manifestations in a single patient. CLAAS has become a major public health issue in the at-risk group of cocaine users, and clinicians should be alert of this condition when treating cocaine users presenting with single or multiple skin ulcerations.
Keywords: cocaine, levamisole associated autoimmune syndrome, pyoderma gangrenosum
1. Background
Since its first report as an adulterant in 2003 [1], levamisole has become the most commonly used substance to “cut” cocaine [1,2]. Severe toxicities, mostly agranulocytosis, had previously led to the drug’s withdrawal from medical use in humans in the US [1]. The illegal use of levamisole in combination with cocaine has harbored additional, previously unknown health issues [3,4,5,6,7]. The most-discussed entity is the cocaine-/levamisole-associated autoimmune syndrome (CLAAS) [4,8,9]. In the skin, CLAAS manifests with retiform purpura [10,11,12,13] or pyoderma gangrenosum (PG)-like features [14,15,16,17,18,19,20,21]. Inner organs such as the kidney can also be affected [3,22,23]. Serological findings in CLAAS include neutropenia and increased titers of antineutrophil cytoplasmic antibodies (ANCA) with positive cytoplasmic (cANCA) and/or perinuclear (pANCA) staining patterns, and anti-neutrophil elastase (NE)-directed antibodies [5,24], and thus qualifies as a drug-induced, skin-limited, ANCA-associated vasculitis [25]. We report the case of a patient suffering from relapsing CLAAS with changing clinical and histological features over time.
2. Case Report
A 57-year-old woman presented at our dermatology outpatient clinic with disseminated painful ulcers. Following their first appearance three years earlier, the ulcers had “come and gone”, but then persisted and expanded over two months. Within this period, the patient also experienced relapsing fevers, night sweats and joint pain. She was reported to consume approximately 1 g of cocaine per day (mostly crack) for several years. Her personal history revealed a non-treated, chronic hepatitis C infection. Dermatological examination showed disseminated polycyclic ulcers covered by yellow exudate and surrounded by prominent red–violet borders (Figure 1a). Our differential diagnosis included granulomatosis with polyangiitis, cocaine-/levamisole-associated vasculitis, PG, ecthymas and superinfected, exogenically inflicted ulcers.
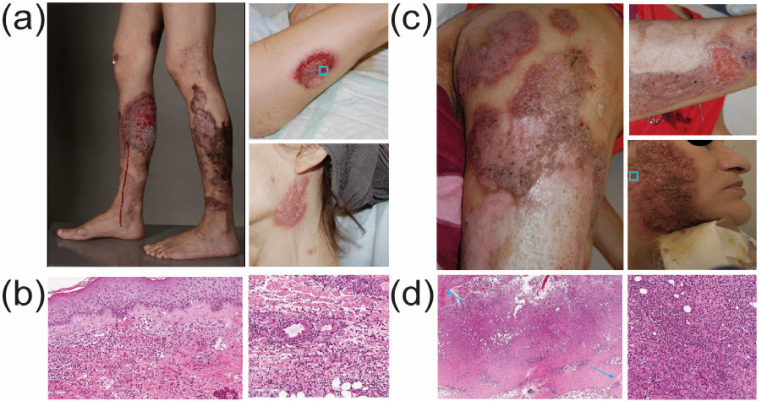
Figure 1.
Skin changes and histology of CLAAS over time. (a) Clinical presentation upon first admission. The patient had extensive polycyclic ulcerations on lower legs and forearms, partly covered by yellowish exsudate and with an undermined edge and surrounding erythematous–violaceous border. There was also cribriform scarring, as shown on the neck. (b) Hematoxylin and eosin (H&E) staining (indicated scale, 100 μm) of a lesional skin biopsy taken from a lesion border (as indicated in (a)) shows a leukocytoclastic hemorrhagic vasculitis. There is a massive, subepidermal neutrophilic infiltrate with some rare eosinophils, as well as extensive hemorrhage. (c) Clinical presentation after four years. Disseminated cribriform ulcerations and extensive scars on the upper leg (left), forearm and face. (d) H&E staining of a lesional skin biopsy taken from an ulcer (as indicated in (c)) shows prominent, focally granulomatous neutrophilc infilitrates and fistula in the dermis/hypodermis, which are indicative of PG.
Our diagnostic work-up included blood and urine analyses, wound swabs, a skin biopsy and chest X-ray. The differential blood count showed neutropenia and thrombopenia. Serum p-ANCA titers were increased, as were autoantibodies against NE. Dermatohistopathology (Figure 1b) revealed a leukocytoclastic, hemorrhagic vasculitis with a mostly neutrophilic infiltrate, a direct immunofluorescence was negative. The search for systemic vasculitis involvement was negative. Toxicological urine analyses came back positive for a cocaine metabolite (benzoylecgonine) but not levamisole. The patient tested negative for tuberculosis, HIV and hepatitis B and no relevant infectious agents were found in blood cultures, skin swabs and tissue cultures. We thus retained the diagnosis of a cocaine/levamisole-induced skin-limited ANCA-associated vasculitis in the spectrum of CLAAS.
Our patient agreed to enter a professional drug rehabilitation program (cessation of cocaine use being the mainstay of CLAAS treatment). Topically, we applied daily antiseptic kalium permanganate wound dressings and topical corticosteroids (TCS), namely clobetasol–propionate cream with gaze dressings. The ulcers healed within ca. two weeks and TCS were tapered. The patient was released from the hospital and relapsed on cocaine. She was admitted and treated a few months later for another CLAAS vasculitis episode and was treated with a similar regimen. After three years lost to follow-up, the patient was again admitted for painful ulcers and reduced overall condition. She had disseminated polycyclic ulcers with undermined, purple borders as well as multiple cribriform scars (Figure 1c). Histology revealed massive dermal neutrophilic infiltrates with fistulated areas (Figure 1d), consistent with chronic PG. Serological work-up revealed unchanged autoantibody patterns (increased p-ANCA-, MPO- and NE-antibodies). Toxicological urine analysis was positive for metabolites of heroin, cocaine and levamisole. These findings led us to the diagnosis of multiple PG as a manifestation of CLAAS. We administered oral prednisone (50 mg daily for 2 weeks) with a prescribed tapering over 6 weeks. As a topical treatment, we applied daily antiseptic wound dressings with octenidin solution for ca. 10 min without a subsequent dry dressing. The ulcers healed during the hospital stay within three weeks; the patient has not shown up for the scheduled follow-up control.
3. Discussion
In 2010 the first description of a levamisole-associated vasculitis was published [26]. CLAAS is characterized by a distinct serological profile of high titer p-ANCA and positive MPO antibodies in conjunction with purpuric skin lesions [10,23,27]. The distinction between idiopathic ANCA-associated vasculitis and CLAAS can be made via anti-neutrophil elastase antibodies [24]. Typical histological findings are thrombotic vasculopathy and small vessel vasculitis or a mixture of both [10], as we saw in the first dermatohistopathological assessment of our patient. The involvement of inner organs, particularly the kidney, has been described [22,23] but was not present in our case.
The abuse of levamisole-adulterated cocaine has also been linked to PG in a series of cases [16,28]. It was found that these PG patients exhibited the same serological findings as individuals with CLAAS [15]. The association with cocaine/levamisole exposure, the overlap in serological profile and the reoccurring histological findings have prompted the notion that LAC and levamisole-associated PG are clinical variants of an underlying spectrum of CLAAS [9].
The exact pathophysiology behind CLAAS remains elusive. In vitro studies have suggested a role of levamisole-induced NETosis [29]. Levamisole directly causes NETosis through binding to neutrophilic muscarinic type 3 receptors and the resulting NETs were shown to be enriched in neutrophil elastase [29,30]. It is, therefore, conceivable that overshooting NETosis in genetically susceptible individuals leads to autoantibody formation against certain NET associated proteins, such as MPO, PPR3 and NE [9]. It also remains to be elucidated whether and how levamisole/cocaine may impact the disease manifestation and course [16].
The cornerstones of CLAAS treatment are the cessation of levamisole exposure and immunosuppressive treatment [9]. Doses of up to 40 mg oral prednisone have been shown to lead to a quick and marked improvement in skin ulcerations in patients with a PG-like manifestation [15] within CLAAS [10]-. In line with these reports, and despite the impressive and extensive ulcers of our patient, the lesions healed within only weeks of high-potency topical clobetasol propinonate treatment, and, in the second episode, oral course of prednisone at 50 mg per day.
4. Conclusions
Our case shows the importance of considering CLAAS as a differential diagnosis for painful ulcers in the at-risk population of cocaine users. Our patient is the first reported case with cutaneous features of CLAAS, i.e., vasculitis and PG, changing over time. Future reports will help to expand our understanding of this dynamic and the means of dealing with it.
Author Contributions
Writing, original draft preparation, editing M.U.-M., J.-H.B.H., J.H. and M.-C.B.; Supervision J.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Larocque A., Hoffman R.S. Levamisole in cocaine: Unexpected news from an old acquaintance. Clin. Toxicol. 2012;50:231–241. doi: 10.3109/15563650.2012.665455. [DOI] [PubMed] [Google Scholar]
- 2.Kudlacek O., Hofmaier T., Luf A., Mayer F.P., Stockner T., Nagy C., Holy M., Freissmuth M., Shmid R., Sitte H.H. Cocaine adulteration. J. Chem. Neuroanat. 2017;83:75–81. doi: 10.1016/j.jchemneu.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collister D., Sathianathan C., Ryz K., Karpinski M., Bernstein K., Gibson I.W. ANCA associated vasculitis secondary to levamisole-adultered cocaine with associated membranous nephropathy: A case series. Am. J. Nephrol. 2017;45:209–216. doi: 10.1159/000456553. [DOI] [PubMed] [Google Scholar]
- 4.Garcia Perez M.R., Ortiz-Gonzalez V.L., Betancourt M., Mercado R. Cocaine-induced vasculitis: Is this a new trend? Open Access Rheumatol. Res. Rev. 2013;5:77–80. doi: 10.2147/OARRR.S51524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee K.C., Ladizinski B., Federman D.G. Complications associated with use of levamisole-contaminated cocaine: An emerging public health challenge. Mayo Clin. Proc. 2012;87:581–586. doi: 10.1016/j.mayocp.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vitt J.R., Brown E.G., Chow D.S., Josephson S.A. Confirmed case of levamisole-associated multifocal inflammatory leukoencephalopathy in a cocaine user. J. Neuroimmunol. 2017;305:128–130. doi: 10.1016/j.jneuroim.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 7.Vosoughi R., Schmidt B.J. Multifocal leukoencephalopathy in cocaine users: A report of two cases and review of the literature. BMC Neurol. 2015;15:208. doi: 10.1186/s12883-015-0467-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brunt T.M., Van den Berg J., Pennings E., Venhuis B. Adverse effects of levamisole in cocaine users: A review and risk assessment. Arch. Toxicol. 2017;91:2303–2313. doi: 10.1007/s00204-017-1947-4. [DOI] [PubMed] [Google Scholar]
- 9.Cascio M.J., Jen K.Y. Cocaine/levamisole-associated autoimmune syndrome: A disease of neutrophil-mediated autoimmunity. Curr. Opin. Hematol. 2018;25:29–36. doi: 10.1097/MOH.0000000000000393. [DOI] [PubMed] [Google Scholar]
- 10.Arora N.P. Cutaneous vasculopathy and neutropenia associated with levamisole-adulterated cocaine. Am. J. Med. Sci. 2013;345:45–51. doi: 10.1097/MAJ.0b013e31825b2b50. [DOI] [PubMed] [Google Scholar]
- 11.Arora N.P., Jain T., Bhanot R., Natesan S.K. Levamisole-induced leukocytoclastic vasculitis and neutropenia in a patient with cocaine use: An extensive case with necrosis of skin, soft tissue, and cartilage. Addict. Sci. Clin. Pract. 2012;7:19. doi: 10.1186/1940-0640-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El Khoury L., Zeineddine N., Felix R., Goldstein M. Cutaneous necrotizing vasculitis and leukopenia in a cocaine user: Is levamisole the culprit? Case Rep. Rheumatol. 2016;2016:2685267. doi: 10.1155/2016/2685267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agdamag A.C., Gevorgyan O., Co M.L., Hassan S. Multiple cutaneous and mucosal lesions in a patient with cocaine-levamisole–induced vasculopathy syndrome. Bayl. Univ. Med. Cent. Proc. 2019;32:93–95. doi: 10.1080/08998280.2018.1503478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jimenez-Gallo D., Albarran-Planelles C., Linares-Barrios M., Rodriguez-Hernandez C., Martinez-Rodriguez A., Garcia-Moreno E., Bravo-Monge R. Pyoderma gangrenosum and Wegener granulomatosis-like syndrome induced by cocaine. Clin. Exp. Dermatol. 2013;38:878–882. doi: 10.1111/ced.12207. [DOI] [PubMed] [Google Scholar]
- 15.Jeong H.S., Layher H., Cao L., Vandergriff T., Dominguez A.R. Pyoderma gangrenosum (PG) associated with levamisole-adulterated cocaine: Clinical, serologic, and histopathologic findings in a cohort of patients. J. Am. Acad. Dermatol. 2016;74:892–898. doi: 10.1016/j.jaad.2015.11.040. [DOI] [PubMed] [Google Scholar]
- 16.Baliu-Pique C., Mascaro J.M., Jr. Multifocal and refractory pyoderma gangrenosum: Possible role of cocaine abuse. Australas. J. Dermatol. 2017;58:e83–e86. doi: 10.1111/ajd.12498. [DOI] [PubMed] [Google Scholar]
- 17.Estebanez A., Silva E., Abdilla N. Ulcerative pyoderma gangrenosum associated with cocaine use. Med. Clin. 2019;154:373–374. doi: 10.1016/j.medcle.2019.03.043. [DOI] [PubMed] [Google Scholar]
- 18.Keith P.J., Joyce J.C., Wilson B.D. Pyoderma gangrenosum: A possible cutaneous complication of levamisole-tainted cocaine abuse. Int. J. Dermatol. 2015;54:1075–1077. doi: 10.1111/ijd.12212. [DOI] [PubMed] [Google Scholar]
- 19.Moreno-Artero E., Querol-Cisneros E., Rodriguez-Garijo N., Tomas-Velazquez A., Idoate M.A., Gil-Sanchez M.P., España A. Cocaine-induced pyoderma gangrenosum-like lesions. J. Dtsch. Dermatol. Ges. 2018;16:763–768. doi: 10.1111/ddg.13523. [DOI] [PubMed] [Google Scholar]
- 20.Ruiz-Villaverde R., Sanchez-Cano D. Multiple pyoderma gangrenosum ulcers associated with cocaine abuse. Sultan Qaboos Univ. Med. J. 2016;16:e527–e528. doi: 10.18295/squmj.2016.16.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang J.Y., French L.E., Shear N.H., Amiri A., Alavi A. Drug-induced pyoderma gangrenosum: A review. Am. J. Clin. Dermatol. 2018;19:67–77. doi: 10.1007/s40257-017-0308-7. [DOI] [PubMed] [Google Scholar]
- 22.Carlson A.Q., Tuot D.S., Jen K.Y., Butcher B., Graf J., Sam R., Imboden J.B. Pauci-immune glomerulonephritis in individuals with disease associated with levamisole-adulterated cocaine: A series of 4 cases. Medicine. 2014;93:290–297. doi: 10.1097/MD.0000000000000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGrath M.M., Isakova T., Rennke H.G., Mottola A.M., Laliberte K.A., Niles J.L. Contaminated cocaine and antineutrophil cytoplasmic antibody-associated disease. Clin. J. Am. Soc. Nephrol. 2011;6:2799–2805. doi: 10.2215/CJN.03440411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiesner O., Russell K.A., Lee A.S., Jenne D.E., Trimarchi M., Gregorini G., Specks U. Antineutrophil cytoplasmic antibodies reacting with human neutrophil elastase as a diagnostic marker for cocaine-induced midline destructive lesions but not autoimmune vasculitis. Arthritis Rheum. 2004;50:2954–2965. doi: 10.1002/art.20479. [DOI] [PubMed] [Google Scholar]
- 25.Sunderkötter C.H., Zelger B., Chen K.R., Requena L., Piette W., Carlson J.A., Dutz J., Lamprecht P., Mahr A., Aberer E., et al. Nomenclature of cutaneous vasculitis: Dermatologic addendum to the 2012 revised international Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheumatol. 2018;70:171–184. doi: 10.1002/art.40375. [DOI] [PubMed] [Google Scholar]
- 26.Bradford M., Rosenberg B., Moreno J., Dumyati G. Bilateral Necrosis of Earlobes and Cheeks: Another Complication of Cocaine Contaminated with Levamisole. Ann. Intern. Med. 2010;152:758–759. doi: 10.7326/0003-4819-152-11-201006010-00026. [DOI] [PubMed] [Google Scholar]
- 27.Marquez J., Aguirre L., Munoz C., Echeverri A., Restrepo M., Pinto L.F. Cocaine-Levamisole-Induced Vasculitis/Vasculopathy Syndrome. Curr. Rheumatol. Rep. 2017;19:36. doi: 10.1007/s11926-017-0653-9. [DOI] [PubMed] [Google Scholar]
- 28.Martínez-Gómez M., Ramírez-Ospina J.A., Ruiz-Restrepo J.D., Velásquez-Lopera M.M. Pyoderma gangrenosum associated to the use of cocaine/levamisole. Series of three cases and literature review. An. Bras. Dermatol. 2021;96:188–195. doi: 10.1016/j.abd.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lood C., Hughes G.C. Neutrophil Extracellular Traps as a Potential Source of Autoantigen in Cocaine-Associated Autoimmunity. Rheumatology. 2017;56:638–643. doi: 10.1093/rheumatology/kew256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carmona-Rivera C., Purmalek M.M., Moore E., Waldman M., Walter P.J., Garraffo H.M., Phillips K.A., Preston K.L., Graf J., Kaplan M.J., et al. A Role for Muscarinic Receptors in Neutrophil Extracellular Trap Formation and Levamisole-Induced Autoimmunity. JCI Insight. 2017;2:e89780. doi: 10.1172/jci.insight.89780. [DOI] [PMC free article] [PubMed] [Google Scholar]