Abstract
Introduction
We aimed to review the outcomes of endoscopic combined intrarenal surgery (ECIRS) as compared to conventional percutaneous nephrolithotomy (PCNL) for kidney stones.
Material and methods
We performed a systematic literature review using MEDLINE, EMBASE, and Cochrane Central Controlled Register of Trials. We included all studies comparing ECIRS and conventional PCNL. Surgical time, hemoglobin drop, and postoperative stay were pooled using the inverse variance of the mean difference (MD) with a random effect, 95% confidence intervals (CI), and p-values. Complications, stone-free rate, and retreatment were assessed using Cochran-Mantel-Haenszel method with random effect model and expressed as odds ratio (OR), 95% CI, and p-values.
Results
A total of 17 studies were included. Surgical time and mean postoperative length did not significantly differ between the groups (MD -8.39 minutes 95%CI -21.30, 4.53, p = 0.20; 5.09 days 95%CI -19.51, 29.69, p = 0.69). Mean hemoglobin drop was significantly lower in the ECIRS group (MD -0.56 g/dl 95%CI -1.08, -0.05, p = 0.03), while blood transfusion rate did not differ between the two groups (OR 0.88 95%CI 0.64, 1.23, p = 0.15). While the incidence of postoperative sepsis did not differ between the two groups (OR 0.52 95% CI 0.17, 1.59, p = 0.25), the incidence of postoperative fever was lower in the ECIRS group but the difference was not significant (OR 0.61 95%CI 0.35, 1.06, p = 0.08). The stone-free rate was significantly higher in the PCNL group (OR 2.52 95%CI 1.64, 3.90, p <0.0001) and the retreatment rate was lower in the ECIRS group (OR 0.34 95%CI 0.14, 0.87, p = 0.002).
Conclusions
ECIRS showed shorter operative time, lower complication rate, and retreatment compared to PCNL. Conventional PCNL showed a higher stone-free rate.
Keywords: percutaneous nephrolithotomy, retrograde intrarenal surgery, kidney stone, endoscopic combined intrarenal surgery
INTRODUCTION
Percutaneous nephrolithotomy (PCNL) is still the gold-standard treatment for large and/or complex renal stones as recommended by current international guidelines [1, 2]. Endoscopic combined intra renal surgery (ECIRS) is an established new way of performing PCNL. Originally described in the prone split-leg or reverse lithotomy position, it is most commonly performed in the Galdakao-modified supine Valdivia position; in recent times PCNL is also selectively done in prone position and combines percutaneous lithotrispy with retrograde intrarenal surgery (RIRS) [3–7]. The major advantage ECIRS offers is tailoring the procedure to the stone burden/location and anatomical complexity where two surgeons dynamically and synchronously maximize the antegrade and retrograde access with flexible and semirigid instruments [8]. Literature supports that this helps in overcoming limitations and complications of PCNL, especially in large stone volumes [9]. With endourological advancements, miniaturization and technological advancements, PCNL and RIRS have independently gained momentum as first-line minimally invasive interventions for urolithiasis depending on stone size. The working hypothesis is that combining these two in ECIRS offers the best possible surgical outcome for renal lithiasis.
The present study aims to systematically review studies comparing ECIRS and PCNL in terms of intra, peri, and postoperative outcomes of both ECIRS and PCNL. Secondary outcomes are to assess the difference in stone-free rate (SFR) and retreatment rate.
Evidence acquisition
Aim of the review
The present study aims to systematically review the safety and stone-free rate after ECIRS (PCNL with the use of contemporary flexible ureteroscopy and lithotripsy) as compared to conventional PCNL (24 Fr to 30 Fr tract without flexible ureteroscopy) for kidney stones. The main outcome is to evaluate for differences in surgical time, length of stay, and postoperative complications between the two procedures. The secondary outcome was to assess if there is any difference in the SFR and retreatment rate between the two procedures.
Literature search
This review was performed according to the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework. An extensive literature search was performed on 8th November 2021, using EMBASE, MEDLINE, and Cochrane Central Controlled Register of Trials (CENTRAL). Medical Subject Heading (MeSH) terms and keywords such as ‘kidney calculi’, ‘urolithiasis’, ‘Percutaneous Nephrolithotomy’, ‘PCNL’, ‘percutaneous lithotripsy’, ‘ureteroscopy’ or ‘endoscopy’, ‘ECIRS or Endoscopic Combined Intrarenal Surgery’ or ‘ureteroscopy’ or ‘no tube’ were used. No date limits were imposed. The search was restricted to English papers only. Animal and pediatric studies were also excluded. Appendix 1 shows the search strategy. Additional articles were sought from the reference lists of the included articles. The review protocol was submitted for registration in PROSPERO (registration #CRD42021291166).
Selection criteria
The PICOS (Patient Intervention Comparison Outcome Study type) model was used to frame and answer the clinical question. P: Adults with kidney stones; Intervention: ECIRS (PCNL with endovision puncture and/contemporary flexible ureteroscopy lithotripsy); Comparison: conventional PCNL (no flexile ureteroscopy and/or endovision puncture); Outcome: surgical time, length of postoperative stay, infection complications (fever defined as body temperature >38°C, and sepsis), bleeding complications (hemoglobin drop, and blood transfusion), retreatment rate, and stone-free rate; Study type: randomized, prospective non-randomized, and retrospective studies. Patients were assigned in two groups according to the type of surgery (ECIRS and conventional PCNL).
Study screening and selection
All retrieved records were screened by two independent authors through Covidence Systematic Review Management® (Veritas Health Innovation, Melbourne, Australia). Discrepancies were solved by a third author. Studies were included based on PICOS eligibility criteria. Retrospective, prospective nonrandomized, and randomized studies were accepted. Meeting abstracts were also included. Reviews, letters to the editor, case reports, and editorials were excluded. The full text of the screened papers was selected if found relevant to the purpose of this study. The search was further expanded by performing a manual search based on the references of the full-text relevant papers.
Statistical analysis
Surgical time, hemoglobin drop, and postoperative length of stay were pooled using the inverse variance of the mean difference (MD) with a random effect, 95% Confidence Intervals (CI), and p-values. Incidence of blood transfusion, fever, sepsis, retreatment rate, and the SFR were assessed using Cochran-Mantel-Haenszel Method with the random effect model and reported as Odd Ratio (OR), 95% CI, and p-values. Analyses were two-tailed and the significance was set at p <0.05 and a 95% CI. OR less than one indicates a lower risk in the ECIRS group. Study heterogeneity was assessed utilizing the I2 value. Substantial heterogeneity was defined as an I2 value >50%. Meta-analysis was performed using Review Manager (RevMan) 5.4 software by Cochrane Collaboration. The quality assessment of the included studies was performed using the Cochrane Risk of Bias tool, using RoB 2 for randomized studies and ROBINS-I for non-randomized ones [10, 11].
Evidence synthesis
The literature search retrieved 3321 papers. One paper was retrieved from other sources. Fourteen duplicates were excluded, leaving 3308 studies for screening. Another 3275 papers were excluded against the title and abstract screening because they were unrelated to the purpose of this study. The full texts of the remaining 33 studies were screened and 16 papers were further excluded for lack of specificity of data or duplicate studies. Finally, 17 studies were accepted and included for meta-analysis. Figure 1 shows the PRISMA flow diagram.
Figure 1.
PRISMA flow diagram of the study.
Study characteristics and quality assessment
Seventeen studies compared ECIRS and conventional PCNL [9, 12, 21–27, 13–20]. There were 16 retrospective studies [9, 12, 21–26, 13–20] and 1 randomized clinical trial [27].
Study characteristics are summarized in Table 1. There were 2054 patients included in 17 studies: 800 patients underwent ECIRS and 1254 underwent conventional PCNL. Figure 6 shows the details of quality assessment in the retrospective studies. Four studies showed a critical overall risk of bias, 6 studies a serious overall risk of bias, and the remaining a moderate risk overall of bias. The most common reason for the risk of bias was in the measurement of outcomes, followed by risk in patient selection and reported results. Figure 7 shows the details of quality assessment in the prospective randomized study that showed a low overall risk of bias.
Table 1.
Characteristics of studies comparing ECIRS vs conventional PCNL included in the review
| Author year of publication | Type of study | Type of paper | Patient positioning ECIRS | Patient positioning PCNL | Amplatz sheath size ECIRS | Amplatz sheath size PCNL | Endovision puncture ECIRS | Definition of stone-free | Mean age ECIRS, years (SD) | Mean age PCNL, years (SD) | Mean stone burden ECIRS | Mean stone burden PCNL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beck 2009 | Retrospective | Meeting abstract | GMSV | Supine | ≥20 Ch | ≥20 Ch | Yes | <1 mm | NA | NA | 17 cm3 | 16 cm³ |
| de la Rosa 2014 | Retrospective | Full text | Supine | Supine | ≥20 Ch | ≥20 Ch | No | < 5 mm | 52.6 (1.7) | 50.5 (1.3) | 39.9 mm | 39.8 mm |
| Gao 2019 | Retrospective | Full text | Prone | Prone | NA | <20 Ch | Yes | <4 mm | 52.3 (14.2) | 52.8 (13.1) | 26 mm | 24 mm |
| Hamamoto 2014 | Retrospective | Full text | Prone | Supine | <20 Ch | <20 Ch | No | <4 mm | 54.5 (1.5) | 48.9 (3.3) | 39.2 mm | 38.4 mm |
| Hong 2016 | Retrospective | Full text | GMSV | Prone | ≥20 Ch | ≥20 Ch | No | <3 mm | 49.6 (3.3) | 50.3 (1.2) | 33.4 mm | 32.5 mm |
| Isac 2013 | Retrospective | Full text | Prone | Prone | ≥20 Ch | <20 Ch | Yes | NA | 57 | 58 | 33 mm | 29 mm |
| Kavaliauskaite 2018 | Retrospective | Meeting abstract | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Kawahara 2012 | Retrospective | Full text | GMSV | Prone | ≥20 Ch | ≥20 Ch | Yes | No fragments | 57.2 (12.3) | 55.5 (11.4) | 59.1 mm | 57.6 mm |
| Kohjimoto 2011 | Retrospective | Meeting abstract | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Leng 2018 | Retrospective | Full text | Supine | Supine | <20 Ch | <20 Ch | No | <4 mm | 46.2 (12.7) | 45.8 (11.2) | 52 mm | 53 mm |
| Mami 2021 | Retrospective | Full text | Supine | Prone | NA | NA | No | <4 mm | 50.01 (9.26) | 45.4 (13.03) | 12.5 mm | 23 mm |
| Wen 2016 | Prospective randomized | Full text | GMSV | Prone | <20 Ch | <20 Ch | NA | <4 mm | 43.18 (14.11) | 45.76 (13.25) | 689 mm2 | 643.35 mm2 |
| Xu 2019 | Retrospective | Meeting abstract | NA | NA | <20 Ch | <20 Ch | NA | NA | 47.4 (10.9) | 52.2 (11.8) | 57.7 | 58.5 mm |
| Yong 2017 | Retrospective | Meeting abstract | NA | Supine or Prone | NA | NA | NA | <4 mm | NA | NA | NA | NA |
| Zelvys 2014 | Retrospective | Meeting abstract | Supine | Supine or Prone | NA | NA | No | NA | 67.65 (7.21) | 61.34 (11.6) | NA | NA |
| Zhang 2016 | Retrospective | Meeting abstract | NA | NA | NA | NA | NA | NA | 51.7 (9.2) | 52.3 (8.1) | NA | NA |
| Zhao 2021 | Retrospective | Full text | GMSV | Prone | <20 Ch | <20 Ch | Yes | <4 mm | 53.18 (12.66) | 53.1 (13.18) | 640.21 mm3 | 753.44 mm3 |
Ch – Charrier; PCNL – percutaneous nephrolithotomy; NA – data not available; SD – standard deviation; GMSV – Galdakao modified supine Valdivia; ECIRS – endoscopic combined intrarenal surgery
Figure 6.
Risk of bias in non-randomized controlled trials (ROBINS-I). A) Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies; B) Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Figure 7.
Risk of bias in randomized controlled trials (ROB-2). A) Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies; B) Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
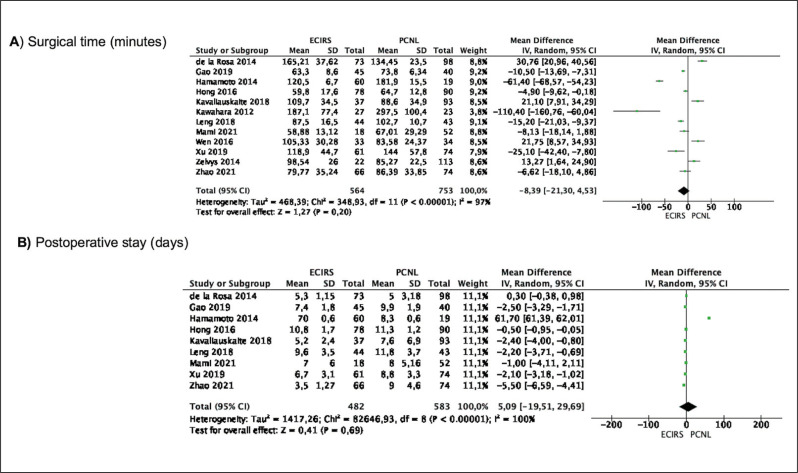
Meta-analyses of surgical time and length of stay
Meta-analysis from 12 studies (564 cases in ECIRS and 753 cases in conventional PCNL) showed that there was a trend for a shorter surgical time in the ECIRS group compared to conventional PCNL but the difference was not significant (MD -8.39 minutes 95% CI -21.30, 4.53, p = 0.20). Study heterogeneity was substantial (I2 97%) (Figure 2A).
Figure 2.
Meta-analysis of surgical time and length of stay in studies comparing ECIRS vs conventional PCNL.
ECIRS – endoscopic combined intrarenal surgery; PCNL – percutaneous nephrolithotomy
Meta-analysis of 9 studies (482 cases in ECIRS and 583 cases in conventional PCNL) showed that mean postoperative length of stay did not differ between the groups (MD 5.09 days 95% CI -19.51, 29.69, p = 0.69). Study heterogeneity was substantial (I2 100%) (Figure 2B).
Meta-analyses of bleeding
Meta-analysis from 4 studies (245 cases in ECIRS and 248 cases in conventional PCNL) showed that the mean hemoglobin drop was significantly lower in the ECIRS group compared with the conventional PCNL group (MD -0.56 g/dl 95% CI -1.08, -0.05, p = 0.03). Study heterogeneity was substantial (I2 99%) (Figure 3A).
Figure 3.
Meta-analysis of bleeding in studies comparing ECIRS vs conventional PCNL.
ECIRS – endoscopic combined intrarenal surgery; PCNL – percutaneous nephrolithotomy
Meta-analysis from 5 studies (232 cases in ECIRS and 242 cases in conventional PCNL) showed that blood transfusion rate did not differ between the two groups (OR 0.88 95% CI 0.64-1.23, p = 0.15). There was no significant heterogeneity among the studies (I2 0%) (Figure 3B).
Meta-analyses of infection complications
Meta-analysis from 7 studies (339 cases in ECIRS and 396 cases in conventional PCNL) showed that there was a trend for a lower incidence of postoperative fever in the ECIRS group but the difference did not reach significance (OR 0.61 95% CI 0.35, 1.06, p = 0.08) (Figure 4A). There was no significant heterogeneity among the studies (I2 0%).
Figure 4.
Meta-analysis of infection complications in studies comparing ECIRS vs conventional PCNL.
ECIRS – endoscopic combined intrarenal surgery; PCNL – percutaneous nephrolithotomy
Meta-analysis from 4 studies (250 cases in ECIRS and 263 cases in conventional PCNL) showed that the incidence of postoperative sepsis did not differ between the two groups (OR 0.52 95% CI 0.17, 1.59, p = 0.25) (Figure 4B). There was no heterogeneity among the studies (I2 0%).
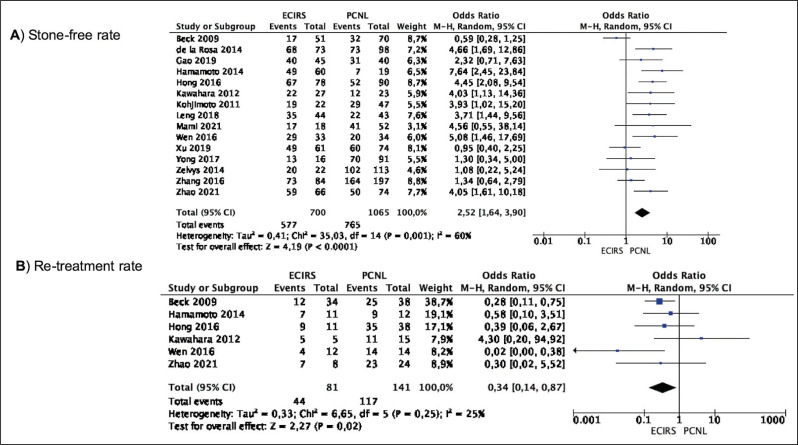
Meta-analyses of stone-free rate and retreatment rate
Meta-analysis from 15 studies (700 cases in ECIRS and 1065 cases in conventional PCNL) showed that the SFR was significantly higher in the conventional PCNL group compared to the ECIRS group (OR 2.52 95% CI 1.64, 3.90, p <0.0001) (Figure 5A). Study heterogeneity was substantial (I2 60%).
Figure 5.
Meta-analysis of stone-free rate and retreatment rate in studies comparing ECIRS vs conventional PCNL.
ECIRS – endoscopic combined intrarenal surgery; PCNL – percutaneous nephrolithotomy
Meta-analysis from 6 studies (81 cases in ECIRS and 141 cases in conventional PCNL) showed that the retreatment rate among patients who were not stone-free at the first follow-up visit was significantly lower in the ECIRS groups compared to the conventional PCNL group (OR 0.34 95% CI 0.14, 0.87, p = 0.002) (Figure 5B). Study heterogeneity was moderate (I2 25%).
DISCUSSION
Evolution in endoscopic armamentarium has introduced several energy devices, higher power lasers for lithotripsy, use of antegrade flexible nephroscopy, which are all aimed at maximizing PCNL outcomes with minimal morbidity. Simultaneously, the growing popularity of supine PCNL from its introduction in 1987 by Valdivia et al. [28] has influenced urologists to adopt ECIRS as a safe and efficacious alternative option, especially in proximal stones, impacted pelvic stones, complex anatomy, forgotten encrusted stents, and large stone volumes [29]. In our meta-analysis, only 1 study by Isac et al. reported patient outcomes in both ECIRS and PCNL cohorts in prone position [16]. Of the 17 studies included, the majority of the ECIRS patients had their procedure in the Galdakao-modified supine Valdivia position or supine position while PCNL was done equally in the prone and supine position. There was a homogeneous distribution of patients in both cohorts concerning age, stone burden, and tract sizes. Minimally invasive PCNL (mini-PCNL) avoids the morbidity of conventional PCNL wherein a tract size of 16 Fr to 20 Fr is used variably [30]. In a recent meta-analysis by Sharma et al., mini-PCNL had similar efficacy with a superior safety profile and lower all-cause complication rate compared to conventional PCNL, yet the need for auxiliary procedures (RR 0.77 [0.58, 1.03], p = 0.08) remained the same [31]. Of the studies that reported tract sizes in our review, interestingly, all studies after 2014 had only mini-PCNL with a tract size <20 Fr in both cohorts reflecting a predicament towards miniaturized access even though both cohorts had many patients with partial or complete staghorn stones with a large stone volume.
We found that the PCNL group had a higher SFR but we were unable to have clear definitions of SFR or methodology used to determine the same. From the available reported data of the included studies, the majority used a <4 mm size as a cut-off for the residual fragments based on postoperative imaging for which there was no standardization in imaging modality or time for evaluation. This could account for the higher SFR in the conventional PCNL group. This problem is not unique to our review as has been demonstrated by Ermis et al. who stated that limited data in staghorn stones show residual fragment range from 47% to 87% [32]. Therefore, there was confusion about the overall SFR which varied between 79.0% and 90.5% depending on the definition and possible adjuvant treatments carried out [32].
There is also no consensus on the best imaging modality or their timing in the evaluation of possible residual fragments. In the ECIRS cohort, however, SFR was determined in most series as on table direct inspection of calyces which has been proposed as an advantage of ECIRS by Scoffone et al. [4]. The retreatment rate among patients who were not stone-free at the first follow-up visit was significantly lower in the ECIRS groups compared to the conventional PCNL group, which could indicate that by careful inspection of calyces significant residual fragments are not left behind. Further, flexible ureteroscopy may help mitigate the possibility of residual fragments in inaccessible calyces in conventional PCNL and hence the need for ancillary intervention and re-imaging. This is akin to using flexible nephroscopy in an antegrade fashion post PCNL which has shown to improve SFR after PCNL, significantly for staghorn calculi as demonstrated by Masood et al. [30]. However, the authors had to use a minimum nephrostomy sheath of 24 Fr to insert the nephroscope. This may have some limitations due to angulation issues to reach different calyces but this can be overcome as the flexible ureteroscope can easily inspect all calyces. This was reiterated in a study by Kuroda et al. wherein the stone surface area and the number of involved calyces were independent predictors of the successful status after ECIRS [33]. This strengthens the feeling that intraoperative assessment of all calyces by flexible ureteroscopy could help improve stone clearance.
Whilst post-PCNL calyceal inspection by flexible ureteroscopy is a bonus, the singular advantage of using this in ECIRS is the ability to allow endoscopic-guided puncture which permits precise access to a targeted calyx under vision [3, 4]. Of the 16 studies in our meta-analysis, only 5 specifically mentioned this utility [12, 14, 16, 18, 26]. A proper puncture and tract creation is the Achilles heel in percutaneous access to prevent complications such as pelvicalyceal system perforation, bleeding, fluid extravasation, and infectious complications [34]. Either this utility is underreported or underutilized or maybe they are not particularly useful in well-trained and experienced PCNL surgeons but this is yet to be determined.
Amongst the included studies that reported the use of single vs. multiple tracts, 8 ECIRS studies reported using only one tract and only one series had some patients needing multiple tracts. Five PCNL series were reported using multiple tracts and 4 PCNL series used single tracts where 3 of these 4 had tract size >20 Fr. Larger diameter tract and multiplicity are well-known risk factors for complications [34]. On reviewing the infectious complications available from 7 studies, there was a trend for a lower incidence of postoperative fever in the ECIRS group but the difference did not reach significance. As no information was available on the number of cases with a preoperative positive culture in either group, this finding might be partially explained by the higher number of tracts in our PCNL studies as was also demonstrated by a recent meta-analysis which showed that preoperative urine culture, stone culture, number of access points, and need for blood transfusion were found to be significant factors for postoperative infection events [35]. This indicates that the presence of pathogens in the urine/stone preoperatively as well as the amount of trauma the kidney sustains during the procedure caused by the number of tracts are major predictors of postoperative infections. However, our meta-analysis revealed that the incidence of postoperative sepsis did not differ between the two groups. This could correlate with either the presence of a ureteral access sheath that helps to lower the intrarenal pressure together or an adequate Amplatz/Nephroscope sheath ratio which allows for proper irrigation outflow from the pelvicalyceal system [36]. Indeed, intrarenal pressure is a well-known and recognized key contributor to post-operative fever and sepsis in endoscopic kidney stone surgery and the use of ureteral access sheath has been demonstrated to optimize fluid irrigation during intrarenal surgery which can be increased by 35 to 80% keeping the same intrarenal pressure [37, 38]. Therefore, the use of ureteral access sheath in ECIRS not only helps in fragment extraction by the ‘pass the ball technique’ but it may have also contributed to the lower incidence of fever and sepsis in ECIRS studies [4]. While overall transfusion rates remained the same in both cohorts the mean hemoglobin drop was significantly lower in the ECIRS group compared with the conventional PCNL group. This could be partially explained by the endovision puncture that may allow for a more accurate and easier puncture.
Minimizing complications and maximizing efficacy is the hallmark of a well-done endourological intervention. Data from our ECIRS studies provide indirect evidence that the procedure may help reduce the number of percutaneous tracts and that a single <20 Fr miniaturized ECIRS access is safe and good enough to achieve a high SFR even in large volume/complete and partial staghorn stones [3, 5, 9]. Achieving reasonable SFR without significant complications with minimal bleeding from a single mini PCNL tract in the ECIRS cohort reinstates confidence that miniaturized single access with adequate drainage of the pelvicalyceal system is indeed a safe procedure. However, if urologists adopted and used ECIRS, it would allow for more tailored access to decide on the need for size and number of access required, based on a dynamic assessment of the pelvicalyceal system even in large volume stones [3, 33], avoiding multiple punctures while maintaining high SFR [3, 29].
Lastly, any procedure while being efficacious must also optimize operative theater utilization. In our meta-analysis of 12 studies, we found that, while not significant, there was a trend for a shorter surgical time in the ECIRS group. Inference can be made that in ECIRS, by optimally using single percutaneous access, two surgeons synchronously working in tandem by antegrade and retrograde approach complement each other, and hence can reduce operative time without compromising procedural safety and efficacy. There has always been a critique that ECIRS requires more resource allocation and hence added cost (2 surgeons, 2 energy devices, 2 sets of equipment). In our meta-analysis, we did not have any data on cost comparisons between the two groups. However, if resources are available, institutes could purpose this procedure to achieve a single-stage minimally invasive approach (single, miniaturized percutaneous tract with minimal infectious complication) even for partial and staghorn stones.
Our study is the first of its kind to analyze the intervention outcomes of patients undergoing ECIRS vis a vis PCNL but it has some limitations. Firstly, the study heterogeneity underpowered some of the results, yet identifies strong indicators and specific trends in both ECIRS and PCNL intervention outcomes. Our analysis reveals how a lack of a standardized reporting of intraoperative outcomes in the ECIRS cohort further limits the ability to gather specific information on pelvicalyceal system injuries, preference of energy devices used, the technique of tract creation, and importantly the different ways in which the retrograde access was utilized to complement the antegrade access which is the hallmark of ECIRS. Thereby, this limits our ability to draw definitive conclusions on the full potential of ECIRS. This alongside limited information from abstract papers weakens our ability to make categorical statements in favor of either surgical technique. Nevertheless, our results allow for the clinical scope to conduct a future randomized trial with a curated checklist to report ECIRS specific outcomes which describe and incorporate the key steps of both antegrade and retrograde access during the procedure.
CONCLUSIONS
Analyzing the existing comparative studies inferences strongly indicate that most urologists use ECIRS to minimize the number of percutaneous access tracts and with added flexible ureteroscopy even large stones can be tackled safely with a single mini-PCNL tract, as it aids in the post-procedure calyceal inspection as a useful adjunct. The utility of ECIRS over PCNL for endoscopic guided punctures remains uncertain. As complication rates did not differ and SFR was higher in the PCNL group, it also remains to be seen if ECIRS can supersede PCNL as the better choice for all renal stones. A prospective comparison of ECIRS and PCNL with standardized reporting in how added flexible ureteroscopy was utilized and helped overcome PCNL challenges may be one good way of analyzing the real potential advantages of ECIRS.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Türk C, Petřík A, Sarica K, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol. 2016;69:475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 2.Assimos D, Krambeck A, Miller NL, et al. Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART I. J Urol. 2016;196:1153–1160. doi: 10.1016/j.juro.2016.05.090. [DOI] [PubMed] [Google Scholar]
- 3.Cracco CM, Scoffone CM. ECIRS (Endoscopic Combined Intrarenal Surgery) in the Galdakao-modified supine Valdivia position: a new life for percutaneous surgery? World J Urol. 2011;29:821–827. doi: 10.1007/s00345-011-0790-0. [DOI] [PubMed] [Google Scholar]
- 4.Scoffone CM, Cracco CM, Cossu M, Grande S, Poggio M, Scarpa RM. Endoscopic combined intrarenal surgery in Galdakao-modified supine Valdivia position: a new standard for percutaneous nephrolithotomy? Eur Urol. 2008;54:1393–1403. doi: 10.1016/j.eururo.2008.07.073. [DOI] [PubMed] [Google Scholar]
- 5.Hamamoto S, Yasui T, Okada A, et al. Efficacy of endoscopic combined intrarenal surgery in the prone split-leg position for staghorn calculi. J Endourol. 2015;29:19–24. doi: 10.1089/end.2014.0372. [DOI] [PubMed] [Google Scholar]
- 6.Grasso M, Nord R, Bagley DH. Prone split leg and flank roll positioning: simultaneous antegrade and retrograde access to the upper urinary tract. J Endourol. 1993;7:307–310. doi: 10.1089/end.1993.7.307. [DOI] [PubMed] [Google Scholar]
- 7.Lehman T, Bagley DH. Reverse lithotomy: modified prone position for simultaneous nephroscopic and ureteroscopic procedures in women. Urology. 1988;32:529–531. doi: 10.1016/s0090-4295(98)90035-8. [DOI] [PubMed] [Google Scholar]
- 8.Lim EJ, Osther PJ, Valdivia Uría JG, et al. Personalized stone approach: can endoscopic combined intrarenal surgery pave the way to tailored management of urolithiasis? Minerva Urol Nephrol. 2021;73:428–430. doi: 10.23736/S2724-6051.21.04443-8. [DOI] [PubMed] [Google Scholar]
- 9.Hamamoto S, Yasui T, Okada A, et al. Endoscopic combined intrarenal surgery for large calculi: simultaneous use of flexible ureteroscopy and mini-percutaneous nephrolithotomy overcomes the disadvantageous of percutaneous nephrolithotomy monotherapy. J Endourol. 2014;28:28–33. doi: 10.1089/end.2013.0361. [DOI] [PubMed] [Google Scholar]
- 10.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beck S, Jain N, Kaplan A, Box G Clayman R, Mcdougall E. Endoscopic guided percutaneous access during percutaneous nephrolithotomy: Is it of any clinical advantage? J Endourol. 2009;23:A154–A155. [Google Scholar]
- 13.Nuño de la Rosa I, Palmero JL, Miralles J, Pastor JC, Benedicto A. A comparative study of percutaneous nephrolithotomy in supine position and endoscopic combined intrarenal surgery with flexible instrument. Actas Urol Esp. 2014;38:14–20. doi: 10.1016/j.acuro.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Gao H, Zhang H, Wang Y, Li K, Du W, Wang X, Wang J. Treatment of Complex Renal Calculi by Digital Flexible Ureterorenoscopy Combined with Single-Tract Super-Mini Percutaneous Nephrolithotomy in Prone Position: A Retrospective Cohort Study. Med Sci Monit. 2019;25:5878–5885. doi: 10.12659/MSM.915034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong X, Wang X, Yang B, et al. Comparison of efficacy and safety between flexible ureteroscopy-assisted percutaneous nephrolithotomy and percutaneous nephrolithotomy monotherapy for the treatment of complicated renal calculi. Int J Clin Exp Med. 2016;9:18537–18542. [Google Scholar]
- 16.Isac W, Rizkala E, Liu X, Noble M, Monga M. Endoscopic-guided versus fluoroscopic-guided renal access for percutaneous nephrolithotomy: a comparative analysis. Urology. 2013;81:251–256. doi: 10.1016/j.urology.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Kavaliauskaite R, Želvys A. 65 - Endoscopic combined intrarenal surgery value in multiple renal stones treatment. Eur Urol Suppl. 2018;17:e2232. [Google Scholar]
- 18.Kawahara T, Ito H, Terao H, Kato Y, Uemura H, Kubota Y, Matsuzaki J. Effectiveness of ureteroscopy-assisted retrograde nephrostomy (UARN) for percutaneous nephrolithotomy (PCNL) PLoS One. 2012;7:e52149. doi: 10.1371/journal.pone.0052149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yasuo K, Sasaki, Kusumoto Y, Ura H, et al. Simultaneous combined percutaneous and retrograde approach versus percutaneous approach for complex renal calculi. J Endourol. 2011;25(S1):A292–A293. [Google Scholar]
- 20.Leng S, Xie D, Zhong Y, Huang M. Combined Single-Tract of Minimally Percutaneous Nephrolithotomy and Flexible Ureteroscopy for Staghorn Calculi in Oblique Supine Lithotomy Position. Surg Innov. 2018;25:22–27. doi: 10.1177/1553350617741023. [DOI] [PubMed] [Google Scholar]
- 21.Mami D, Alchinbayev M, Kazachenko A. Comparison of minimally invasive treatment methods for urinary stones: A retrospective analysis. Electron J Gen Med. 2021;18:em321. [Google Scholar]
- 22.Xu K, Li Z. Comparison of Multi-tract minimally invasive percutaneous nephrolithotomy and Endoscopic Combined Intrarenal Surgery for Staghorn Renal Calculi: A single institution experience. J Endourol. 2019;33(S1):A185. [Google Scholar]
- 23.Yong D, Koh S, Tan Y. Supine percutaneous nephrolithotomy is safe and achieves higher stone free rates when combined with retrograde intrarenal surgery (endoscopic combined intra renal surgery) J Endourol. 2017;31(S2):A42–A43. [Google Scholar]
- 24.Zelvys A, Cekauskas A, Jankevicius F. B71 - Role of combined intrarenal surgery (ECIRS) in management of large/complex kidney stones. Eur Urol Suppl. 2014;13:e1192. [Google Scholar]
- 25.Zhang W, Lu P. Super-mini percutaneous nephrolithotomy combined with flexible ureteroscopy versus the Chinese minimally invasive percutaneous nephrolithotomy: An efficacy analysis in patients with renal stones 2.5-4.0 cm. J Endourol. 2016;30(S2):A207–A208. [Google Scholar]
- 26.Zhao F, Li J, Tang L, Li C. A comparative study of endoscopic combined intrarenal surgery (ECIRS) in the galdakao-modified supine valdivia (GMSV) position and minimally invasive percutaneous nephrolithotomy for complex nephrolithiasis: a retrospective single-center study. Urolithiasis. 2021;49:161–166. doi: 10.1007/s00240-020-01207-5. [DOI] [PubMed] [Google Scholar]
- 27.Wen J, Xu G, Du C, Wang B. Minimally invasive percutaneous nephrolithotomy versus endoscopic combined intrarenal surgery with flexible ureteroscope for partial staghorn calculi: A randomised controlled trial. Int J Surg. 2016;28:22–27. doi: 10.1016/j.ijsu.2016.02.056. [DOI] [PubMed] [Google Scholar]
- 28.Valdivia Uría JG, Lachares Santamaría E, Villarroya Rodríguez S, Taberner Llop J, Abril Baquero G, Aranda Lassa JM. Percutaneous nephrolithectomy: simplified technic (preliminary report) Arch Esp Urol. 1987;40:177–180. [PubMed] [Google Scholar]
- 29.Cracco CM, Scoffone CM. Endoscopic combined intrarenal surgery (ECIRS) – Tips and tricks to improve outcomes: A systematic review. Turkish J Urol. 2020;46:S46–S57. doi: 10.5152/tud.2020.20282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Masood Y, Iqbal N, Farooq RM, Iqbal S, Khan F. Intraoperative flexible nephroscopy during percutaneous nephrolithotomy: An 8 years’ experience. Pak J Med Sci. 2021;37:716–720. doi: 10.12669/pjms.37.3.3565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sharma G, Sharma A, Devana SK, Singh SK. Mini Versus Standard Percutaneous Nephrolithotomy for the Management of Renal Stone Disease: Systematic Review and Meta-analysis of Randomized Controlled Trials. Eur Urol Focus. doi: 10.1016/j.euf.2021.07.014. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 32.Ermis O, Somani B, Reeves T, et al. Definition, treatment and outcome of residual fragments in staghorn stones. Asian J Urol. 2020;7:116–121. doi: 10.1016/j.ajur.2019.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuroda S, Ito H, Sakamaki K, et al. Development and Internal Validation of a Classification System for Predicting Success Rates After Endoscopic Combined Intrarenal Surgery in the Modified Valdivia Position for Large Renal Stones. Urology. 2015;86:697–702. doi: 10.1016/j.urology.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 34.de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, Tefekli A, CROES PCNL Study Group The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25:11–17. doi: 10.1089/end.2010.0424. [DOI] [PubMed] [Google Scholar]
- 35.Lai WS, Assimos D. Factors Associated With Postoperative Infection After Percutaneous Nephrolithotomy. Rev Urol. 2018;20:7–11. doi: 10.3909/riu0778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ganpule AP, Bhattu AS, Desai M. PCNL in the twenty-first century: role of Microperc, Miniperc, and Ultraminiperc. World J Urol. 2015;33:235–240. doi: 10.1007/s00345-014-1415-1. [DOI] [PubMed] [Google Scholar]
- 37.Traxer O, Wendt-Nordahl G, Sodha H, et al. Differences in renal stone treatment and outcomes for patients treated either with or without the support of a ureteral access sheath: The Clinical Research Office of the Endourological Society Ureteroscopy Global Study. World J Urol. 2015;33:2137–2144. doi: 10.1007/s00345-015-1582-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lopes AC Neto, Dall'Aqua V, Carrera RV, Molina WR, Glina S. Intra-renal pressure and temperature during ureteroscopy: Does it matter? Int Braz J Urol. 2021;47:436–442. doi: 10.1590/S1677-5538.IBJU.2020.0428. [DOI] [PMC free article] [PubMed] [Google Scholar]