Abstract
Introduction
Renal colic due to ureteral stones represents the primary acute condition in urology. Although guideline recommendations are available the institution, urologist, and patient preferences in diagnosis and treatment may differ. We aimed to evaluate the adherence of different European countries to the European Association of Urology (EAU) guidelines of urolithiasis and demonstrate trends in diagnostic and treatment approaches.
Material and methods
We used a survey including 33 questions clustered in four sections. The survey was circulated to the representatives of the main urological centers in Europe using the European Section of Uro-technology (ESUT), the European Section of Urolithiasis (EULIS), the Young Academic Urologists (YAU), and the European Urology Residents Education Programme (EUREP) mailing lists. The first section included participant and institution demographics, the second assessed the common diagnostic and treatment pathways, the third discussed the advantages and disadvantages of treatment strategies and the fourth investigated treatment preferences in different clinical scenarios. A descriptive analysis was performed.
Results
Of all participants, 84.21% stated that their departments follow specific guidelines, with no significant differences between institutions (p = 0.18). Preferred treatment practice difference in the case scenarios was significantly influenced by the Department bed capacities (p = 0.01), and complications varied between institutions (p = 0.02). Interestingly, 37–45% of participants were unaware of the different treatment costs.
Conclusions
Although urologists generally decide according to local or international guidelines when approaching renal colic patients, there are deviations in clinical practice due to ‘doctor preference’ and ‘bed availability’. Many urologists are unaware of treatment costs.
Keywords: renal colic, urolithiasis, ureteroscopy, extracorporeal shock wave lithotripsy, care survey, health
INTRODUCTION
Urolithiasis is a clinical condition showing increasing trends [1, 2]. Acute renal colic is an emergency requiring immediate pain management. Patients admitted to the hospital with an acute, noninfected episode of urolithiasis may undergo medical expulsive therapy (MET), ureteral stent placement, or upfront ureteroscopy (URS). The implementation of these therapeutic approaches is likely to be dictated by their availability [3–6].
Appropriate treatment and follow-up should be tailored, considering stone stratification, patient preference, surgeon experience and availability of minimally invasive treatment options. Additional factors influencing treatment decisions include Institution or Department treatment policies, bed availability, surgeon preference, insurance and financial issues, and different functions of European Health Systems. New technologies offer various diagnostics and therapies but display a financial burden on healthcare systems. Clinical practice guidelines are essential to implement evidence-based medicine and assure a standard of care considering limited resources. The European Association of Urology (EAU) guidelines provide urologists a tool for optimizing patient care and decision-making. Other urological societies have also provided guidelines to help urologists make therapeutic choices [1, 7]. However, these recommendations may be heterogeneous due to various development methods [8]. Surveys from different European countries have demonstrated significant differences regarding diagnostic and treatment strategies. Urologists working in university hospitals are more inclined to adopt guidelines compared to those who practice in non-academic centers [9, 10, 11]. The aim of this study is to control the adherence of European countries to the EAU guidelines of urolithiasis and demonstrate different trends in diagnostic and treatment approach in a European level.
MATERIAL AND METHODS
A questionnaire was prepared after the available evidence on renal colic was reviewed (TT, SG). A larger panel of experts (TT, SG, BKS, ASG, KS, and UN) convened and discussed essential aspects of renal colic based on available evidence and personal experience and revised the questionnaire which included 33 questions clustered in four main sections (supplementary material). The first section included participant and institution demographics. The second assessed common diagnostic and treatment pathways applied in renal colic patients. The third discussed the advantages and disadvantages of different treatment strategies. Finally, the fourth section aimed to investigate the participants’ treatment preference in different clinical scenarios. The survey was circulated primarily to urinary stone disease experts of the European Section of Uro-technology (ESUT) and the European Section of Urolithiasis (EULIS) working groups. It was then shared using the Survey Monkey platform (Palo Alto, CA, USA) to all representatives of the main European urological centers using the ESUT, the EULIS, the Young Academic Urologists (YAU), and the European Urology Residents Education Program (EUREP) mailing lists. An invitation e-mail was sent on September 09, 2020, and responses were recorded until December 08, 2020. Care was taken to include only one urologist from each institution. The authors collected the results on a spreadsheet and analyzed them using the Windows Excel software. Only complete questionnaires were included in the analysis.
Statistical analysis
Continuous variables were presented as the mean ± standard deviation (SD) and categorical variables were presented as percentages. In the case of small proportions, the actual number was also presented. Descriptive information and percentages were based on available data. Statistical significance between continuous variables was determined using the Student’s t test. The Mann–Whitney test and Kruskal-Wallis test were used for non-parametric data. Pearson’s Chi-square analysis was performed to test for differences in proportions of categorical variables between two or more groups. All statistical analyses were performed using IBM SPSS 23.0. A p value < 0.05 was considered statistically significant.
RESULTS
Demographics
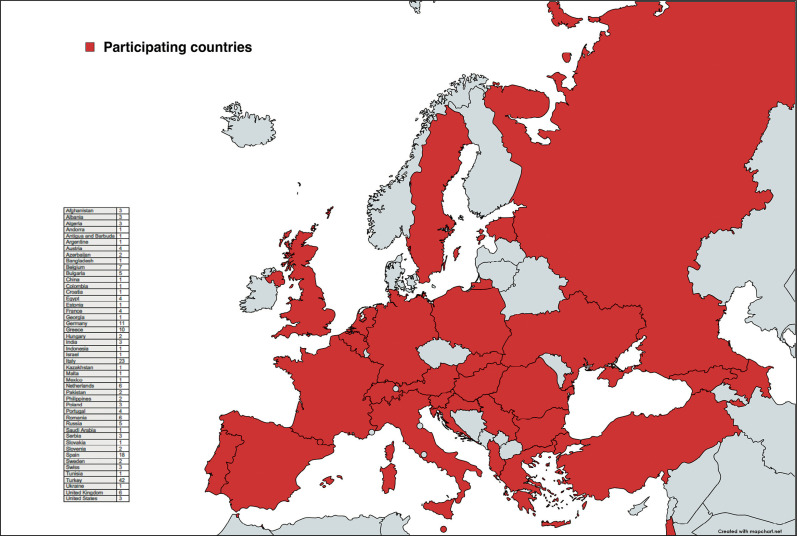
A total of 209 recipients from 47 countries completed the survey (Figure 1, Table 1).
Figure 1.
Participants.
Table 1.
Demographic data of the survey participants
| N | % | |
|---|---|---|
| Gender Male Female |
180 29 |
86.12% 13.88% |
| Ιnstitution University Hospital Government Based Research and Training Hospital Private Hospital Governmental Hospital (State Hospital) Military Hospital Other |
136 23 45 36 5 1 |
65.07% 11.00% 21.53% 17.22% 2.39% 0.48% |
| Department area of interest (more than one option is possible) General Urology Endo-urology Oncology Pediatric Urology Laparascopic/Robotics Female/Incontinence Reconstructive Urology Andrology/Men’s’ Health |
120 157 103 22 87 27 31 39 |
57.42% 75.12% 49.28% 10.53% 41.63% 12.92% 14.83% 18.66% |
N – number of survey participants; % – percentage of participants
Different diagnostic approaches for renal colic patients
Regarding use of specific guidelines in colic patient diagnosis and treatment, with more than one option being allowed, 84.21% responded ‘Yes, the EAU guidelines’, 22.01% ‘According to surgeon preference’, 18.18% ‘Yes, national guidelines’, and 6.70% followed no guidelines at all. The subgroup analysis according to different institutions, showed no significant difference (p = 0.26, Table 2). Regarding preferred imaging pathway, 30.14% chose kidney/bladder ultrasound + non-contrast computer tomography (NCCT), 29.67% only NCCT, 15.31% X ray-kidney ureter bladder (KUB) + kidney/bladder ultrasound and 11.48% X ray-KUB + kidney/bladder ultrasound + NCCT. Only 6.70% and 3.35% chose the option of kidney/bladder ultrasound and x ray-KUB only respectively (Table 3).
Table 2.
Responses according to different types of institutions
| University Hospital n = 130 (%) | Governmental (State) Hospital n = 30 (%) | Government Based Research and Training Hospitaln = 21 (%) | Private Hospital n = 23 (%) | Military Hospital (%)n = 5 | p | |
|---|---|---|---|---|---|---|
| Age (mean ±SD) | 38.4 ±9.2 | 40.7 ±11.5 | 40.1 ±8.8 | 43.68 ±10.3 | 44.4 ±16.6 | 0.18+ |
| Clinical practice according to: EAU guidelines National guidelines Surgeon preference Institution/department regulations |
78 (60) 22 (16.9) 25 (19.2) 5 (3.8) |
16 (53.3) 2 (6.7) 7 (23.3) 5 (16.7) |
12 (57.1) 4 (19) 5 (23.8) 0 |
11 (47.8) 5 (21.7) 4 (13) 3 (17.4) |
4 (80) 1 (20) |
0.26* |
| Main complications of active renal colic treatment Sepsis Acute Kidney Injury Urinoma Ureteral injury / stenosis |
91 (70) 31 (23.8) 1 (0.8) 7 (5.4) |
16 (53.3) 9 (30) 0 5 (16.7) |
10 (47.6) 8 (38.1) 0 3 (14.3) |
9 (39.1) 10 (43.5) 3 (13) 1 (4.3) |
3 (60) 1 (20) 0 1 (20) |
0.02* |
| General questions | ||||||
| What type of SWL service does your department offer? | 0.38* | |||||
| MET as a standard treatment | 0.2* | |||||
| Type of anesthesia for DJ stent insertion | 0.28* | |||||
| Duration of DJ stent placement after URS | 0.14* | |||||
| Main benefits of a primary URS stone treatment, | 0.52* | |||||
EAU – European Association of Urology; SWL – shock wave lithotripsy; MET – medical expulsive therapy; DJ – double J stent; URS – ureteroscopy;
Kruskal Wallis;
Pearson Chi-square test
Table 3.
Summary of survey results
| Department bed capacity <20 beds 20–40 beds >40 beds |
47 111 51 |
22.49% 53.11% 24.40% |
| Offered types of stone treatment SWL sURS fURS PCNL |
136 189 173 171 |
65.07% 90.43% 82.78% 81.82% |
| Type of SWL service We have a fixed-site SWL machine We have access to a mobile SWL machine We refer patients to another hospital for SWL We do not offer SWL |
128 13 23 45 |
61.24% 6.22% 11.00% 21.53% |
| SWL performed by… Trained Urologist Resident Technician |
124 69 81 |
59.33% 33.01% 38.76% |
| In the primary setting renal colic patients are treated by… GP Private urologist Hospital urologist |
68 23 118 |
32.54% 11.00% 56.46% |
| Number of renal colic patients treated per day <5 5–10 10–20 >20 |
89 94 18 8 |
42.58% 44.98% 8.61% 3.83% |
| Urolithiasis patients treated per week 0–5 5–10 10–15 15–20 >20 |
31 58 52 28 40 |
14.83% 27.75% 24.88% 13.40% 19.14% |
| Diagnostic imaging strategy for renal colic in the acute setting Xray – KUB Kidney / Bladder Ultrasound Kidney / Bladder Ultrasound + NCCT Xray – KUB + Kidney / Bladder Ultrasound NCCT Xray-KUB + NCCT Xray-KUB + Kidney / Bladder Ultrasound + NCCT |
7 14 63 32 62 7 24 |
3.35% 6.70% 30.14% 15.31% 29.67% 3.35% 11.48% |
| Specific guidelines applied in colic patient diagnosis and treatment (more than one option is possible) Yes, EAU guidelines Yes, National guidelines According to surgeon preference No, we follow our institution / department regulations |
176 38 46 14 |
84.21% 18.18% 22.01% 6.70% |
| Use of MET Yes, always No, we never use it Doctor preference |
115 12 82 |
55.02% 5.74% 39.23% |
| Admission of renal colic patients Yes always, except when patients refuse it Yes, if there are free beds Patient preference Urologist preference No, only when there is an absolute indication (resistant pain, sepsis, renal insufficiency) |
34 11 3 25 136 |
16.27% 5.26% 1.44% 11.96% 65.07% |
| Reasons for renal colic patient admission (more than one option is possible) We always have beds for them It is a standard treatment, according to my Institution/ department regulations Our goal is to manage the colic and if stone diagnosed to treat it at the same time Financial reasons / Insurance issues They cannot be treated elsewhere |
10 19 18 4 5 |
22.22% 42.22% 40.00% 8.89% 11.11% |
| Most common treatment strategy in case of patient admission Conservative treatment until patient symptom-free, if no relief offer minimally invasive management Conservative treatment until a spontaneous stone passage 1–2 days conservative treatment, if no spontaneous stone passage then offer minimally invasive management Direct minimally invasive management (emergency URS or SWL) According to doctor preference According to patient preference |
73 3 56 17 17 5 |
42.69% 1.75% 32.75% 9.94% 9.94% 2.92% |
| Common minimally invasive management strategy of renal colic for a ureteral stone Primary SWL Insertion of DJ stent with the intention to push stone in the kidney and planning of secondary treatment with SWL Insertion of DJ stent and planning of secondary treatment with sURS or fURS Primary sURS under general anesthesia. If failure DJ insertion and planning of secondary treatment Surgeon preference Patient preference |
21 7 65 57 19 2 |
12.28% 4.09% 38.01% 33.33% 11.11% 1.17% |
| Encountered complications in active renal colic treatment Sepsis Acute Kidney Injury Urinoma Ureteral injury / stenosis |
129 59 4 17 |
61.72% 28.23% 1.91% 8.13% |
| Type of applied anesthesia for DJ stent insertion General anesthesia Sedation Regional/Spinal anesthesia Local anesthesia By men always general anesthesia, by women local anesthesia Patient preference Doctor preference |
89 69 51 31 12 8 9 |
52.05% 40.35% 29.82% 18.13% 7.02% 4.68% 5.26% |
| Reasons for avoiding admission of renal colic patients Not enough beds Admission is not a standard treatment, according to my Institution / department regulations The goal is for the stone to be treated in a second session/admission Financial reasons |
62 90 35 13 |
36.26% 52.63% 20.47% 7.60% |
| Follow up of patients during the whole treatment Yes, always Yes, but only if we can offer the treatment needed (SWL, fURS, PCNL) otherwise patients are admitted elsewhere No, we just treat the acute problem Surgeon preference Patient preference |
125 24 10 5 7 |
73.10% 14.04% 5.85% 2.92% 4.09% |
| Length of DJ stent placement after URS <1 week 1–2 weeks 2–4 weeks >4weeks If patient pre-stented and/or uncomplicated URS, one day If patient pre-stented and/or uncomplicated URS, no stent Surgeon preference |
23 75 65 16 18 33 11 |
13.45% 43.86% 38.01% 9.36% 10.53% 19.30% 6.43% |
| Benefits of a primary URS in stone treatment Colic and stone are treated in one session Need to decrease future general anesthesia Less patient discomfort/stress Less administrative/secretary work (planning of appointments etc.) No benefits No opinion Financial benefits /insurance issues (please explain) |
149 43 86 36 5 6 5 |
87.13% 25.15% 50.29% 21.05% 2.92% 3.51% 2.92% |
| Drawbacks of a primary URS stone treatment Needs more surgeon experience Very often unsuccessful, patients undergo a second treatment anyway High complication rates An emergency operation plan often not accomplished No drawbacks No opinion Financial drawbacks / insurance issues (explain) |
73 28 27 58 28 7 5 |
42.69% 16.37% 15.79% 33.92% 16.37% 4.09% 2.92% |
GP – general practitioner; SWL – shock wave lithotripsy; URS – ureteroscopy; sURS – semi-rigid ureterocopy; fURS – flexible ureteroscopy; PCNL – percutaneous nephrolithotripsy; KUB – kidney ureter bladder; NCCT – non-contrast computer tomography; MET – medical expulsive therapy; DJ– double-J stent
Different treatment strategies followed
Among responders, 55.02% always use MET in primary treatment, 39.23% of institutions depend on doctor preference and 5.74% of responders avoid using it. Regarding patient admission, 65.07% only admit patients in case of an absolute indication (resistant pain, sepsis, renal insufficiency), 16.27% always admit patients except when they refuse, 11.96% depend on doctor preference, and 5.26% and 1.44% depend on bed availability, and patient preference (Table 3).
Regarding primary double-J (DJ) stent insertion (with more than one possible option), 52.05% of responders place it under general anesthesia, 40.35% under sedation, 29.82% under regional/spinal, and 18.13% under local anesthesia. Regarding stent placement after URS (with more than one possible answer), 43.86%, 38.01%, 13.45% and 9.36% leave a DJ stent in place for 1–2, 2–4, <1, and >4 weeks respectively. In case of pre-stented patients and an uncomplicated URS 10.53% leave the stent in place only for one day, and 19.30% do not place a stent at all. Finally, only in 6.43% of the cases the chosen strategy depends on the surgeon preference (Table 3).
Advantages and disadvantages of different treatment choices
Among responders, 61.72%, 28.23%, 8.13%, and 1.91% highlighted urosepsis, acute kidney injury, ureteral injury with consecutive stenosis, and urinoma respectively as the most common complication of active stone treatment. Responses differed significantly between institutions (p = 0.02, Table 2) with sepsis (70%) being common in the university hospital group, acute kidney injury, and urinoma in the private hospital group (43.5% and 13%, respectively), and ureteral injury/stenosis in the military hospital (20%).
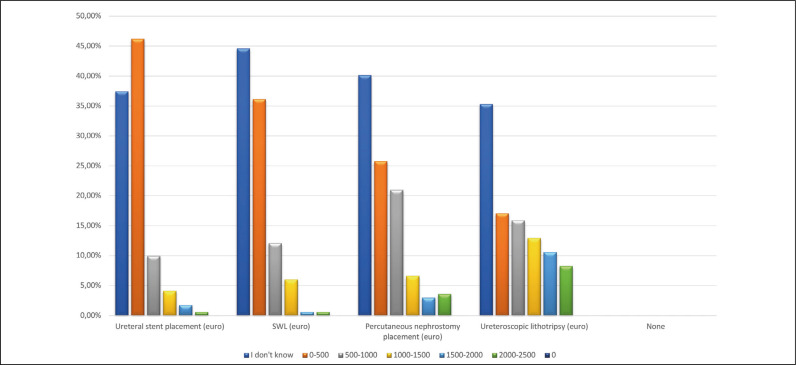
Participants highlighted the simultaneous treatment of renal colic and the ureteral stone (87.13%), the reduced patient stress and discomfort (50.29%), the minimized need for a second general anesthesia (25.15%), and the reduced secretary/administrative work (21.05%) as the main benefits of primary URS. Nevertheless, 42.69% suggest that a primary URS demands surgeon experience and 33.92% think that an emergency operation plan can rarely be accomplished. Furthermore, 16.37% highlight the common need of a second operative treatment due to an unsuccessful primary URS, and 15.79% due to its high complication rates (Table 3). Interestingly, 37–45% of participants were unaware of the different treatment costs in their department (Figure 2).
Figure 2.
The average cost of the intervention per patient.
SWL – shock wave lithotripsy
Clinical scenarios (Table 4)
Table 4.
Treatment preference according to different clinical scenarios
| n | % | P type of SWL service | P bed capacity <20, 20–40, >40 | P institution | |
|---|---|---|---|---|---|
| Renal colic for 1–2 days, distal ureter stone with diameter <4 mm. No absolute indications for acute treatment | |||||
| Conservative outpatient treatment, no follow-up | 14 | 8.24 | 0.94 | 0.03 | 0.38 |
| Conservative outpatient treatment, follow-up until active treatment/ stone passage | 135 | 79.41 | |||
| Admission, conservative treatment for 1–2 days, MIM if symptoms persist. If symptoms subside then no management | 18 | 10.59 | |||
| Admission and MIM on the same day | 1 | 0.59 | |||
| Planning of patient admission and MIM on the following week | 2 | 1.18 | |||
| Renal colic for 1-week, distal ureter stone with diameter >4 mm. No absolute indications for acute treatment | |||||
| Conservative outpatient treatment, no follow-up | 11 | 6.47 | 0.19 | 0.01 | 0.39 |
| Conservative outpatient treatment, follow-up until active treatment/ stone passage | 72 | 42.35 | |||
| Planning of patient admission and MIM on the following week | 42 | 24.71 | |||
| Admission, conservative treatment for 24hrs, MIM if symptoms persist. If symptoms subside then no management | 27 | 15.88 | |||
| Admission and MIM on the same day | 18 | 10.59 | |||
| Renal colic for 1-day, proximal ureter stone with diameter <4 mm. No absolute indications for acute treatment | |||||
| Conservative outpatient treatment, no follow-up | 16 | 9.47 | 0.83 | 0.08 | 0.41 |
| Conservative outpatient treatment, follow-up until active treatment/ stone passage | 130 | 76.92 | |||
| Planning of admission and MIM on the following week | 5 | 2.96 | |||
| Admission, conservative treatment for 24hrsMIM if symptoms persist. If symptoms subside then no management | 18 | 10.65 | |||
| Admission and MIM on the same day | 0 | 0.00 | |||
| Renal colic since 1-day, proximal ureter stone with diameter >4 mm. No absolute indications for acute treatment | |||||
| Conservative outpatient treatment, no follow-up | 8 | 4.73 | 0.37 | <0.001 | 0.81 |
| Conservative outpatient treatment, follow-up until treatment/ stone passage | 74 | 43,79 | |||
| Planning of patient admission and MIM on the following week | 42 | 24,85 | |||
| Admission, conservative treatment for 24hrs, MIM if symptoms persist. If symptoms subside then no management | 31 | 18,34 | |||
| Admission and MIM on the same day | 14 | 8,28 | |||
| Renal colic since 1-day, ureter stone with diameter <4 mm. Additional ipsilateral kidney stone/s. Kidney obstruction. No absolute indications for acute treatment | |||||
| Conservative outpatient treatment, no follow-up | 11 | 6.43 | 0.69 | 0.05 | 0.43 |
| Conservative outpatient treatment, follow-up until active treatment/ stone passage | 54 | 31.58 | |||
| Planning of patient admission and MIM on the following week (preferably also treating the kidney stone) | 32 | 18.71 | |||
| Admission, conservative treatment for 24hrs, then MIM if symptoms persist (preferably also treating the kidney stone). If symptoms subside then no management | 12 | 7.02 | |||
| Stent insertion on the same day then second treatment according to stone size and location | 43 | 25.15 | |||
| Admission and MIM on the same day according to stone size and location (preferably also treating the kidney stone) | 15 | 8.77 | |||
MIM – minimally invasive management
Distal stones
In the case of renal colic for 1–2 days due to a stone with diameter <4 mm and no absolute treatment indication, 79.41% would choose a conservative outpatient treatment and follow-up until treatment or spontaneous stone passage. Conservative treatment was preferred in 76.5%, 73.8%, and 57.4% in Departments with >40, 20–40, and <20 beds respectively (p = 0.03; Table 4). In the case of renal colic for one week due to a stone with >4 mm and no absolute treatment indication, 42.35% would choose a conservative outpatient treatment and patient follow-up until treatment/ stone passage. In 24.71%, responders initially avoid, but would plan a patient admission and minimally invasive management in the following week (Table 4). Respondents chose conservative treatment options at a rate of 33.3%, 43.1%, and 36.1% in Departments with >40, 20–40, and <20 beds respectively (p = 0.01, Table 4).
Proximal stones
In the case of renal colic for 1–2 days due to a stone with diameter <4 mm and no absolute treatment indication, 76.92% would choose a conservative outpatient treatment and patient follow-up until treatment/ stone passage. Conservative treatment was preferred in 39.2%, 30.6%, and 22.4% in Departments with >40, 20–40, and <20 beds respectively (p = 0.08, Table 4). In the case of a renal colic for 1 day due to a stone with diameter >4mm and no absolute treatment indication, 43.79% would still prefer a conservative outpatient treatment and patient follow-up until treatment/ stone passage. In 24.85%, responders would initially avoid, but plan a patient admission and minimally invasive management in the following week, while in 18.34% the patients are admitted and follow a conservative treatment for 24 hours to undergo a minimally invasive treatment in case of conservative treatment failure. Conservative treatment was chosen at a rate of 35.3%, 42.3%, and 36.2% in Departments with >40, 20–40, and <20 beds respectively (p <0.001, Table 4).
Ureteral and ipsilateral kidney stones
In case of renal colic for 1 day due to a ureteral stone of diameter <4 mm, kidney obstruction, ipsilateral stone/s, and no absolute treatment indication, 31.58% would still prefer a conservative outpatient treatment and patient follow-up until treatment/ stone passage. Another 25.15% would perform a DJ stent insertion on the same day and plan a second treatment according to stone size and location. Another 18.71% would avoid stent placement or primary treatment but plan a primary minimally invasive treatment during the following week, while 8.77% would proceed to a minimally invasive treatment at the same day. In case of minimally invasive treatment, 38.01% of respondents prefer insertion of DJ stent and planning of secondary treatment with semi-rigid ureteroscopy (sURS) or flexible ureteroscopy (fURS), 33.33% prefer primary sURS under general anesthesia, 12.28% primary shockwave lithotripsy (SWL) and 4.09% DJ stent placement with the intention to push the stone in the kidney (Table 4).
DISCUSSION
The increasing incidence of kidney stone disease, along with the need for instant pain relief and technology developments necessitate the use of diagnostic and therapeutic algorithms for optimizing patient care. The role of the EAU Urolithiasis Guideline Panel is to provide such a tool on an annual basis [12]. Nonetheless, there are different approaches in diagnosis, follow-up, and treatment decisions in the everyday clinical practice [8–11]. The survey demonstrated that more than 80% of urologists depend on local or international guidelines when approaching renal colic patients. However, despite their close adherence to the EAU guidelines, participant responses in different case scenarios became heterogeneous due to ‘doctor preference’ and ‘bed availability’ parameters. Preferred treatment practices in different case scenarios were also significantly affected by the number of hospital beds.
According to more than 70% of responders, NCCT was the imaging of choice, with or without combination with x-ray or ultrasound. This finding is in line with the EAU Guidelines recommendations [1] and reflects the wide acceptance of this imaging tool despite its higher costs and, in many cases, higher radiation exposure. Furthermore, most responders that do not initially use NCCT, usually recommend it when planning any type of active treatment. This delay of NCCT has been demonstrated in different emergency departments and observational studies and is due to radiation exposure and cost concerns [13].
Around 65% of the survey participants admit renal colic patients only in case of absolute indications (resistant pain, sepsis, renal insufficiency) and only 16% admit all patients. This result reflects the common knowledge that spontaneous stone passage occurs in 60–90% [14, 15, 16]. Additionally, approximately 93% of responders use MET as it is believed that it facilitates spontaneous stone passage. The main complications faced differ between institutions, with sepsis being higher in the university hospital group (70%), while acute kidney injury and urinoma (43.5% and 13%, respectively) being prominent in non-university institutions (p = 0.02). Further studies are needed to confirm this information with real-life data. Additionally, there is limited information on hospital admission and active treatment rates with reported admission rates ranging from 2% to 13% [17, 18], but it has been shown that the index admission/intervention rate can be seven times different [19]. Among responders, only 10% suggested a direct, minimally invasive treatment (emergency URS or SWL), while most believe that the main benefits of primary URS stone treatment are the treatment of both colic and stone in one session and the decreased patient discomfort/stress. Innes et al. reported that an early interventional approach was associated with higher revisit, hospitalization, and intervention rate [19].
Regarding the first choice of preferred minimally invasive treatment, 70% of responders chose URS either in the primary setting or after inserting a DJ stent, and only 12% offer an SWL in the acute setting, although the survey was conducted amid the COVID-19 pandemic. This challenges the suggestion that SWL requires fewer healthcare resources than URS over a 3-month period in the acute ureteral stone management, which also conserves personal protection equipment and reduces the risk of infectious transmission [20]. Interestingly, perhaps due to this current risk of COVID-19 transmission, almost 50% of the participants do not prefer general anesthesia when placing a ureteral stent. Additionally, the majority leave a DJ stent after URS even if patients are pre-stented and/or the intervention is uncomplicated, and around 80% always leave DJ stent for 1–4 weeks despite suggestions for a stent-less procedure [21–24]. Finally, for ureteral stones with a diameter of <4 mm irrespective of stone location, conservative outpatient treatment and patient follow-up until treatment/stone passage is the first choice, while for stones with diameter >4 mm patient admission and primary intervention rates increase. In case of renal colic due to a ureteral stone and the additional ipsilateral kidney stone, the preference of urologists varies, with conservative outpatient follow-up, patient admission and minimally invasive management of both stones, and stent insertion with second treatment according to stone size and location being possible treatment options.
Knowledge of different treatment costs is essential in the decision-making process [25]. Responses showed variation of costs between countries and departments. Interestingly, it could be demonstrated that most of the urologists are unaware about the exact costs of different treatment modalities. This fact could also reflect the preference of participants in URS despite its higher costs. In endourology, where the industry is involved, increasing the awareness of urologists in cost analysis of treatments would also affect treatment decisions. While our study yielded valuable results, limitations inherent in survey-based studies apply not being representative of the ‘whole’ population, such as being answered only by those interested in the subject, guided by countries with a high number of responses. However, the authors believe that it helps the urological community to draw real-world patterns of adherence to the EAU guidelines.
CONCLUSIONS
Although urologists try to make decisions according to local or international guidelines when approaching renal colic patients, there are deviations in clinical practice due to ‘doctor preference’ and ‘bed availability’. Imaging with non-contrast enhanced computed tomography (NCCT) plays the major role in patient diagnosis and treatment planning. Urologists, usually, only admit patients when they suffer from complications or by uncontrollable pain, and only one third of them follow a direct minimally invasive treatment (URS or SWL). In the case of emergency treatment, URS either in the primary setting or after inserting a DJ stent is usually the first choice. SWL is less preferred than expected although it is less costly, bares minimal infection risks and could be offered in times of pandemic conditions. It seems that most urologists are unaware about treatment costs.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
All authors have made substantial contributions to the material submitted for publication; all have read and approved the final manuscript.
References
- 1.Türk C, Petřík A, Sarica K, et al. EAU Guidelines on Diagnosis and Conservative Management of Urolithiasis. Eur Urol. 2016;69:468–474. doi: 10.1016/j.eururo.2015.07.040. [DOI] [PubMed] [Google Scholar]
- 2.Pearle MS, Goldfarb DS, Assimos DG, et al. Medical management of kidney stones: AUA guideline. J Urol. 2014;192:316–324. doi: 10.1016/j.juro.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Arcaniolo D, De Sio M, Rassweiler J, et al. Emergent versus delayed lithotripsy for obstructing ureteral stones: a cumulative analysis of comparative studies. Urolithiasis. 2017;45:563–572. doi: 10.1007/s00240-017-0960-7. [DOI] [PubMed] [Google Scholar]
- 4.Hollingsworth JM, Norton EC, Kaufman SR, Smith RM, Wolf JS, Jr, Hollenbeck BK. Medical expulsive therapy versus early endoscopic stone removal for acute renal colic: an instrumental variable analysis. J Urol. 2013;190:882–887. doi: 10.1016/j.juro.2013.03.040. [DOI] [PubMed] [Google Scholar]
- 5.McKay A, Somani BK, Pietropaolo A, et al. Comparison of Primary and Delayed Ureteroscopy for Ureteric Stones: A Prospective Non-Randomized Comparative Study. Urol Int. 2021;105(1-2):90–94. doi: 10.1159/000510213. [DOI] [PubMed] [Google Scholar]
- 6.Kirshenbaum EJ, Doshi C, Dornbier R, et al. Socioeconomic Disparities in the Acute Management of Stone Disease in the United States. J Endourol. 2019;33:167–172. doi: 10.1089/end.2018.0760. [DOI] [PubMed] [Google Scholar]
- 7.Türk C, Petřík A, Sarica K, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol. 2016;69:475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 8.Pradère B, Doizi S, Proietti S, Brachlow J, Traxer O. Evaluation of Guidelines for Surgical Management of Urolithiasis. J Urol. 2018;199:1267–1271. doi: 10.1016/j.juro.2017.11.111. [DOI] [PubMed] [Google Scholar]
- 9.Betschart P, Zumstein V, Jichlinski P, et al. Spoilt for Choice: A Survey of Current Practices of Surgical Urinary Stone Treatment and Adherence to Evidence-Based Guidelines among Swiss Urologists. Urol Int. 2019;103:357–363. doi: 10.1159/000502806. [DOI] [PubMed] [Google Scholar]
- 10.Cacciamani G, Artibani W, Briganti A, N'Dow J. Adherence to the European Association of Urology Guidelines: A National Survey among Italian Urologists. Urol Int. 2018;100:139–145. doi: 10.1159/000486344. [DOI] [PubMed] [Google Scholar]
- 11.Eismann L, Kretschmer A, Bader MJ, Kess S, Stief CG, Strittmatter F. Adherence to guidelines in the management of urolithiasis: are there differences among distinct patient care settings? World J Urol. 2021;39:3079–3087. doi: 10.1007/s00345-020-03562-9. [DOI] [PubMed] [Google Scholar]
- 12.Tzelves L, Türk C, Skolarikos A. European Association of Urology Urolithiasis Guidelines: Where Are We Going? Eur Urol Focus. 2021;7:34–38. doi: 10.1016/j.euf.2020.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Schoenfeld EM, Shieh MS, Pekow PS, et al. Association of Patient and Visit Characteristics With Rate and Timing of Urologic Procedures for Patients Discharged From the Emergency Department With Renal Colic. JAMA Netw Open. 2019;2:e1916454. doi: 10.1001/jamanetworkopen.2019.16454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morse RM, Resnick MI. Ureteral calculi: natural history and treatment in an era of advanced technology. J Urol. 1991;145:263–265. doi: 10.1016/s0022-5347(17)38310-6. [DOI] [PubMed] [Google Scholar]
- 15.Miller OF, Kane CJ. Time to stone passage for observed ureteral calculi: a guide for patient education. J Urol. 1999;162(3 Pt 1):688–600. doi: 10.1097/00005392-199909010-00014. [DOI] [PubMed] [Google Scholar]
- 16.Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004;350:684–693. doi: 10.1056/NEJMcp030813. [DOI] [PubMed] [Google Scholar]
- 17.Sfoungaristos S, Kavouras A, Kanatas P, Duvdevani M, Perimenis P. Early hospital admission and treatment onset may positively affect spontaneous passage of ureteral stones in patients with renal colic. Urology. 2014;84:16–21. doi: 10.1016/j.urology.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Hyams ES, Korley FK, Pham JC, Matlaga BR. Trends in imaging use during the emergency department evaluation of flank pain. J Urol. 2011;186:2270–2274. doi: 10.1016/j.juro.2011.07.079. [DOI] [PubMed] [Google Scholar]
- 19.Innes G, McRae A, Grafstein E, et al. Variability of renal colic management and outcomes in two Canadian cities. CJEM. 2018;20:702–712. doi: 10.1017/cem.2018.31. [DOI] [PubMed] [Google Scholar]
- 20.Farag M, Jack GS, Wong L-M, Bolton DM, Lenaghan D. What is the best way to manage ureteric calculi in the time of COVID-19? A comparison of extracorporeal shockwave lithotripsy (SWL) and ureteroscopy (URS) in an Australian health-care setting. BJUI Compass. 2020;2:92–96. doi: 10.1002/bco2.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guven S, Yigit P, Tuncel A, et al. Retrograde intrarenal surgery of renal stones: a critical multi-aspect evaluation of the outcomes by the Turkish Academy of Urology Prospective Study Group (ACUP Study) World J Urol. 2021;39:549–554. doi: 10.1007/s00345-020-03210-2. [DOI] [PubMed] [Google Scholar]
- 22.Hollenbeck BK, Schuster TG, Seifman BD, Faerber GJ, Wolf JS., Jr Identifying patients who are suitable for stentless ureteroscopy following treatment of urolithiasis. J Urol. 2003;170:103–106. doi: 10.1097/01.ju.0000069546.53896.6a. [DOI] [PubMed] [Google Scholar]
- 23.New F, Somani BK. A Complete World Literature Review of Quality of Life (QOL) in Patients with Kidney Stone Disease (KSD) Curr Urol Rep. 2016;17:88. doi: 10.1007/s11934-016-0647-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehmi A, Jones P, Somani BK. Current Status and Role of Patient-reported Outcome Measures (PROMs) in Endourology. Urology. 2021;148:26–31. doi: 10.1016/j.urology.2020.09.022. [DOI] [PubMed] [Google Scholar]
- 25.Geraghty RM, Jones P, Herrmann TRW, Aboumarzouk O, Somani BK. Ureteroscopy is more cost effective than shock wave lithotripsy for stone treatment: systematic review and meta-analysis. World J Urol. 2018;36:1783–1793. doi: 10.1007/s00345-018-2320-9. [DOI] [PMC free article] [PubMed] [Google Scholar]