Abstract
Background:
Chronic ankle instability (CAI) is commonly encountered in soccer players. The feelings of instability and anxiety caused by CAI can lead to poor performance, such as difficulty in sharp change of direction during soccer play. The single-leg drop landing (SLDL) task is often used to evaluate dynamic postural stability.
Purpose/Hypothesis:
The purpose of this study was to clarify whether dynamic stability measured during SLDL is altered in male collegiate soccer players with CAI. The hypothesis was that athletes with CAI would show poor dynamic postural stability.
Study Design:
Controlled laboratory study.
Methods:
A total of 103 male collegiate soccer players were recruited, and their limbs were classified based on the new international CAI criteria. All players performed three 5-second SLDL trials on a force plate. The main outcome measures included time to stabilization of the horizontal ground-reaction force (GRF); peak GRF in the vertical, horizontal, and sagittal directions; and trajectory length of the center of pressure during SLDL.
Results:
Data from 59 CAI limbs and 147 non-CAI limbs were collected in this study. Time to stabilization of horizontal GRF was significantly longer in the CAI limbs (P < .001), and the peak GRFs in all directions were significantly lower in the CAI limbs (vertical, P < .001; horizontal, P < .001; sagittal, P = .001). Additionally, the trajectory length of the center of pressure was significantly greater in the CAI limbs (P = .004).
Conclusion:
Soccer players with CAI had decreased dynamic postural stability that led them to land softly when performing the SLDL task. Measurement of dynamic postural stability may be useful in the evaluation of CAI.
Clinical Relevance:
Our findings may be useful for strategies of daily training or as an evaluation tool.
Keywords: chronic ankle instability, dynamic postural stability, single-leg drop landing, soccer, force plate
Ankle sprains are observed frequently in competitive athletes, 11,18 and approximately 20% to 30% of players with acute ankle sprains develop mechanical and/or functional ankle instabilities, resulting in residual symptoms commonly referred to as chronic ankle instability (CAI). 5,29 CAI is characterized by recurrent ankle sprains, giving way sensations, and a sense of instability at the ankle joint, irrespective of whether CAI is combined with mechanical laxity. 8,16,26 In addition, CAI has been associated with a decreased level of participation in sports and the development of ankle osteoarthritis. 1,19 However, definitions of CAI have varied among studies, making direct comparison of results difficult. In 2013, the International Ankle Consortium reached a consensus on the criteria for participant selection in research focused on CAI. 16 However, only a limited number of CAI studies have been conducted based on these new criteria.
Single-leg drop landing (SLDL), which imposes large and rapid impulse loads to the ankle complex, is a commonly reported dynamic maneuver that simulates the mechanism of a lateral ankle sprain. 3,10,28 SLDL is considered to be an effective method of evaluating postural stability for soccer players with CAI because landing is the most common mechanism of soccer-related, noncontact ankle sprains. 31 There have been 3 reports 21,25,32 on postural dynamic stability during SLDL in athletes diagnosed with CAI based on the new criteria. 23 The 3 studies reported conflicting findings with regard to postural dynamic stability in athletes who have CAI, indicating the need for further research.
The aim of the current study was to evaluate dynamic postural stability during SLDL in male collegiate soccer players diagnosed with CAI based on the new criteria. Our hypothesis was that male collegiate soccer players with CAI would show poor dynamic postural stability during SLDL.
Methods
This study was part of a sports injury prevention project titled “The Prospective Study of Predictors of Sports Injuries: UTokyo Sports Science Initiative.” 27 The SLDL assessment was performed as a preseason medical assessment before the onset of the season for each player. The study protocol was approved by the ethics committee of our institution, written consent was obtained from all participants, and the study was performed in accordance with the Declaration of Helsinki.
Participants and CAI Criteria
A total of 103 male soccer players from 2 regional first-division collegiate soccer teams were enrolled in this study. None of the players had acute injuries when the study was performed, and none reported any musculoskeletal injuries of the lower limb in the 3 months before the study.
Soccer players with CAI had to meet the following new CAI criteria 16 : (1) history of at least 1 significant ankle sprain, (2) self-reported sensations of giving way during activities, (3) a Cumberland Ankle Instability Tool (CAIT) score <25, and (4) no signs or symptoms of an acute injury. CAIT 17 is a reliable and valid 9-item questionnaire used to identify patients with CAI. The validity and reliability of the Japanese version of CAIT have been verified. 20 The total score of the 9 items ranges from 0 (severe instability) to 30 (normal stability). The cutoff CAIT score used to determine CAI was set to values <25 according to previous reports. 16,28 The presence of CAI was evaluated separately in both limbs. Additionally, we divided non-CAI limbs into 2 groups; one group contained “coper” limbs, which had sustained previous ankle sprain and had a CAIT score >25, and the other group contained control limbs without previous ankle sprain.
SLDL Procedures
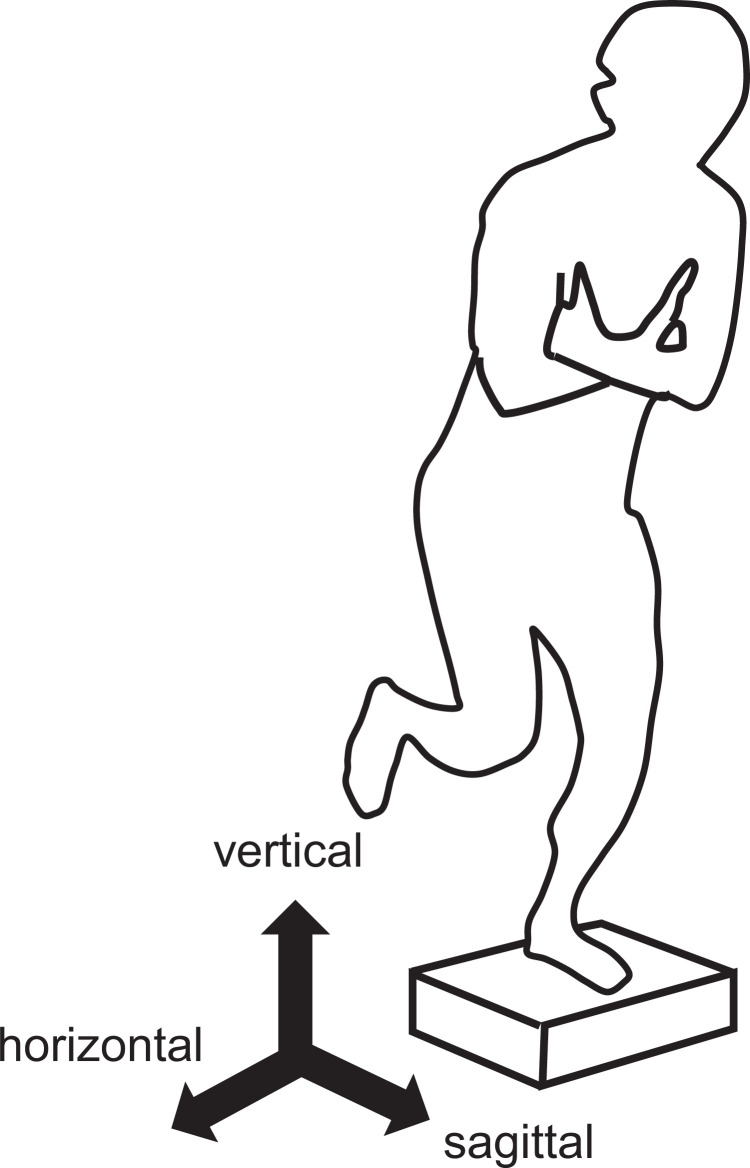
The SLDL task was used to measure dynamic postural stability between limbs or players with CAI and those without CAI. The SLDL protocol was based on previous reports. 13,15 We asked each participant to perform 1 session that comprised 3 valid trials for both legs. A trial was considered invalid if a participant shifted his standing leg or touched the floor with the contralateral leg. The SLDL was executed from a box with a height of 30 cm, which was placed at a distance of 1 cm posterior to the force plate (Figure 1). The height difference on the drop landing between the box and the force plate was 20 cm because the thickness of the force plate was approximately 10 cm. Participants stood on the testing leg, crossed their arms on their chest, took off, landed on the same leg on the center of the force plate, stabilized as quickly as possible, and balanced for 5 seconds by maintaining a posture that was as motionless as possible. Other than to “hop off the box,” no instructions (eg, for the jump height) were given.
Figure 1.
Single-leg drop landing test. (A) The start position on the 30-cm box. (B) The single-leg landing on the force plate.
Assessment of Dynamic Postural Stability During the SLDL Task
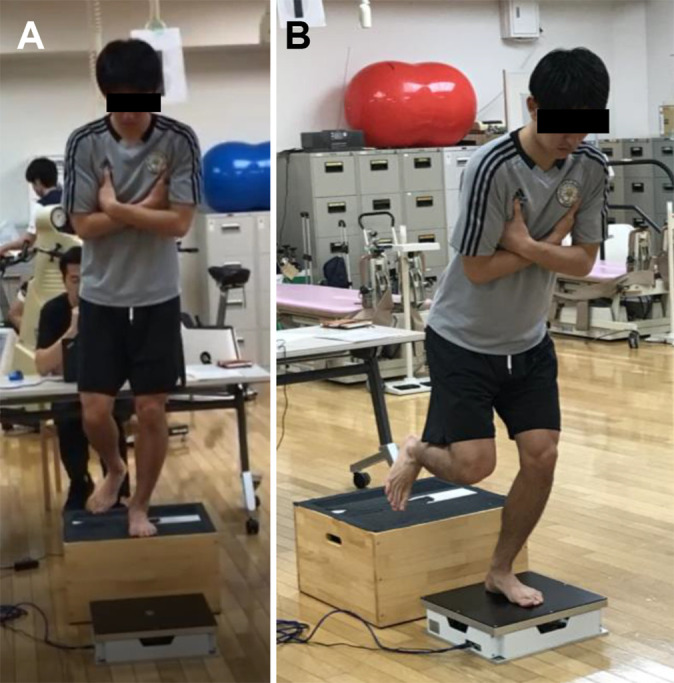
Measurements of the ground-reaction force (GRF) were conducted using a force plate (Type 9281B; Kistler), and analytic software (Version 1.2; Technology Service) was used to record the measurement data at 1000 Hz and calculate the center of pressure (COP) trajectory length. Data were filtered using a Butterworth low-pass filter (zero time shift; cutoff, 70 Hz). Based on the data of the measured GRF, the distance the COP moved during the 5-second period immediately after landing was calculated to determine the total COP trajectory length. We then calculated the ratio of the total COP trajectory length at every 1-second interval; the peak values of the vertical, horizontal, and sagittal components of the GRF; and the time to reach the peak values. Orientation of the axes was defined as vertical pointing upward, frontal pointing mediolateral, and sagittal pointing forward (Figure 2). The COP trajectory length and GRF were normalized to leg length and body weight, respectively. The COP trajectory length up to 20 milliseconds was excluded because the exact COP could not be calculated owing to the extremely small vertical GRF values immediately after landing. Additionally, we measured the time to stabilization after landing (TTS). The TTS of horizontal GRF was defined as the time required for the unbounded third-order polynomial to reach a value below the reference value. All postural stability parameters were calculated as the average of 3 valid trials.
Figure 2.
Definition of the ground-reaction forces (GRFs). The vertical GRF was defined as a vector perpendicular to the force plate in the total GRF. The horizontal GRF was defined as a mediolateral vector in the GRF, and the sagittal GRF was defined as an anteroposterior vector in the GRF.
Statistical Analysis
All statistical analyses were performed using SPSS (Version 25.0; IBM Corp). An independent t test was used in the comparison analysis between the CAI and non-CAI limbs. Analysis of variance was used to compare group means for each dependent variable (CAI, coper, and control), and Bonferroni post hoc examination was used to ascertain the location of significant findings. All significance tests were 2-tailed, and a significance level of P < .05 was used for all tests.
A post hoc power analysis using TTS for horizontal GRF; trajectory length of COP; and vertical, horizontal, and sagittal peak GRF showed that this study yielded a power of 0.99, 0.65, 0.99, 0.99, and 0.95, respectively, (1 – β) with a 2-sided significance level set at .05. Additionally, the effect size (Cohen d) was calculated.
Results
The characteristics of the players are provided in Table 1. The limbs of players were classified into 59 limbs with CAI (previous ankle sprain with CAIT score <25) and 147 non-CAI limbs (previous ankle sprain with CAIT score ≥25 [coper limbs] or no prior history of ankle sprain [control limbs]). A total of 19 players had bilateral CAI. The 59 limbs with CAI consisted of 31 dominant limbs and 28 nondominant limbs. The 147 non-CAI limbs consisted of 82 control limbs and 65 coper limbs.
Table 1.
Participant Characteristics (N = 103 Players) a
| Variable | Value |
|---|---|
| Age, y | 20.2 ± 1.0 |
| Weight, kg | 68.2 ± 6.0 |
| Height, cm | 173.7 ± 5.7 |
| Body mass index | 22.4 ± 1.7 |
| Dominant side, right:left | 95:8 |
a Data are presented as mean ± SD or No. of participants.
Table 2 provides the results for group comparisons of outcomes between the CAI and non-CAI limbs. The TTS of horizontal GRF was significantly longer in the CAI limbs compared with the non-CAI limbs (P < .001). Vertical, horizontal, and sagittal peak GRFs were all significantly lower in the CAI limbs compared with the non-CAI limbs (P ≤ .001 for all). The times to peak vertical and sagittal GRFs were longer in the CAI limbs (P = .024 and .032, respectively). The total trajectory length of the COP in the range of 20 milliseconds to 5 seconds was significantly greater in CAI limbs (P = .004). Furthermore, the trajectory length of the COP in the range of 20 milliseconds to 1 second was significantly greater in CAI limbs (P = .004).
Table 2.
Comparison of Single-Leg Drop Landing Results Between the CAI and Non-CAI Limbs a
| CAI Limbs (n = 59) |
Non-CAI Limbs (n = 147) |
P | ES | |
|---|---|---|---|---|
| TTS of horizontal GRF, s | 0.17 ± 0.13 | 0.08 ± 0.11 | <.001 b | 0.827 |
| Trajectory length of COP (m) | ||||
| 20 ms to 5 s | 3.57 ± 4.97 | 2.24 ± 1.34 | .004 b | 0.467 |
| 20 ms to 1 s | 2.71 ± 5.00 | 1.38 ± 1.32 | .004 b | 0.472 |
| 1-2 s | 0.30 ± 0.07 | 0.28 ± 0.07 | .252 | 0.175 |
| 2-3 s | 0.21 ± 0.05 | 0.21 ± 0.05 | .351 | 0.163 |
| 3-4 s | 0.18 ± 0.05 | 0.19 ± 0.04 | .561 | 0.107 |
| 4-5 s | 0.17 ± 0.05 | 0.17 ± 0.04 | .718 | 0.041 |
| Vertical peak GRF, N/kg | 39.37 ± 8.49 | 47.07 ± 13.37 | <.001 b | 0.629 |
| Time to peak vertical GRF, s | 0.06 ± 0.02 | 0.05 ± 0.02 | .024 b | 0.362 |
| Horizontal peak GRF, N/kg | 4.02 ± 1.34 | 6.52 ± 3.58 | <.001 b | 0.799 |
| Time to peak horizontal GRF, s | 0.06 ± 0.02 | 0.06 ± 0.02 | .279 | 0.173 |
| Sagittal peak GRF, N/kg | 5.66 ± 2.39 | 6.96 ± 2.32 | .001 b | 0.556 |
| Time to peak sagittal GRF, s | 0.07 ± 0.03 | 0.06 ± 0.02 | .032 b | 0.345 |
a Data are presented as mean ± SD. CAI, chronic ankle instability; COP, center of pressure; ES, effect size (Cohen d); GRF, ground-reaction force; TTS, time to stabilization after landing.
b Significant difference between groups (P < .05).
Table 3 shows the results for group comparisons of outcomes between the CAI limbs, coper limbs, and control limbs. The results of comparison between the CAI limbs and the coper limbs were similar to the results of comparison between the CAI limbs and the non-CAI limbs. No difference was found between the coper limbs and the control limbs.
Table 3.
Comparison of Single-Leg Drop Landing Results Between the CAI, Coper, and Control Limbs a
| CAI Limbs (n = 59) |
Coper Limbs (n = 65) |
Control Limbs (n = 82) |
P | |
|---|---|---|---|---|
| TTS of horizontal GRF, s | 0.17 ± 0.13 b,c | 0.08 ± 0.10 b | 0.07 ± 0.11 c | <.001 d |
| Trajectory length of COP (m) | ||||
| 20 ms to 5 s | 3.57 ± 4.97 | 2.39 ± 1.74 | 2.11 ± 0.85 | .063 |
| 20 ms to 1 s | 2.71 ± 5.00 | 1.52 ± 1.73 | 1.27 ± 0.83 | .073 |
| 1-2 s | 0.30 ± 0.07 | 0.29 ± 0.06 | 0.28 ± 0.07 | .360 |
| 2-3 s | 0.21 ± 0.05 | 0.22 ± 0.05 | 0.21 ± 0.05 | .151 |
| 3-4 s | 0.18 ± 0.05 | 0.19 ± 0.04 | 0.19 ± 0.04 | .782 |
| 4-5 s | 0.17 ± 0.05 | 0.18 ± 0.04 | 0.17 ± 0.03 | .300 |
| Vertical peak GRF, N/kg | 39.37 ± 8.49 b,c | 47.55 ± 13.93 b | 46.48 ± 13.03 c | <.001 d |
| Horizontal peak GRF, N/kg | 4.02 ± 1.34 b,c | 6.94 ± 3.89 b | 6.13 ± 3.27 c | <.001 d |
| Sagittal peak GRF, N/kg | 5.66 ± 2.39 b,c | 7.08 ± 2.69 b | 6.78 ± 1.98 c | .005 d |
a Data are presented as mean ± SD. CAI, chronic ankle instability; COP, center of pressure; GRF, ground-reaction force; TTS, time to stabilization after landing.
b Significant difference between CAI and coper limbs (P < .05).
c Significant difference between CAI and control limbs (P < .05).
d Significant difference among three groups (P < .05).
Discussion
The results of this study indicated that dynamic postural stability, as represented by the TTS of horizontal GRF and the trajectory length of the COP during SLDL, was decreased in CAI limbs compared with non-CAI limbs. Additionally, the peak GRFs in all 3 directions (vertical, horizontal, and sagittal) during SLDL were significantly lower in CAI limbs compared with non-CAI limbs. These findings indicate that players with CAI had decreased dynamic postural stability that led them to land softly when performing the SLDL task.
Consistent with our findings, mediolateral (horizontal) stability deficits have been reported in individuals with CAI or chronic functional ankle instability during diagonal jumps or forward jumps, with mediolateral (horizontal) stability deemed important for determining CAI during jumps. 6,21,32 Because players with CAI could have mechanical dysfunction, proprioceptive deficit, and/or neural inhibitions due to repetitive ligamentous injury, 25 they may require a longer time to regain a stabilized single-leg landing. Conversely, Shiravi et al 25 reported that the mediolateral (horizontal) dynamic stability index was similar between patients with CAI and healthy controls during lateral jumps. However, participants in that study were athletes of several types of sports, and the jumping task did not involve a drop jump.
Dynamic stability, as indicated by the trajectory length of the COP, also decreased in CAI limbs in our study. In terms of the relationship between CAI and COP, Pope et al 24 suggested that the CAI group yielded greater anterior and lateral displacements. McKeon and Hertel 22 also evaluated single-limb stance postural stability in patients with CAI by measuring time-to-boundary (analyzing the spatiotemporal relationship of the COP to the boundary of stability) deficits in the anteroposterior and mediolateral components of COP. Significant deficits in time to boundary were identified during eye-closure balance trials in the CAI group compared with controls. These findings agreed with our data. However, these 2 studies were based on static balance evaluations; thus, our findings are relevant for evaluating dynamic stability in CAI.
Peak GRFs in all 3 directions (vertical, horizontal, and sagittal) were significantly lower in CAI limbs than non-CAI limbs. Fransz et al 14 showed that a larger peak vertical GRF was associated with a lower risk of severe ankle sprain and likely indicated that an optimized jump-landing rapidly coped with the perturbation or impact, thus reducing injury risk, which is in agreement with our results. Conversely, some studies have reported that higher vertical GRFs were generated in participants with CAI during drop jumps, 4,7,10 unlike the results of the current study. A possible explanation of these differences could be that participants were different among these studies. Some studies included not specific sports athletes, whereas some studies enrolled high-level sports athletes, as did our study. Therefore, coping methods accommodating these forces in drop jump tasks may be different. Vertical peak GRFs in CAI limbs and non-CAI limbs should be investigated using a larger sample size, including various levels of sports and various kinds of sports.
Wikstrom et al 30 reported that participants with CAI had lower variability in horizontal GRF (mediolateral stability index) than did non-CAI copers. Additionally, high variability in horizontal GRF was a possible mechanism controlling mediolateral dynamic stability, thus agreeing with our results. Conversely, 3 studies 3,10,32 reported no differences in horizontal GRFs between participants with and without CAI during drop landings. However, the participants in these studies were not athletes who belonged to one specific sport.
Several studies have reported no differences in sagittal GRFs between participants with and without CAI during drop landings. 3,9,10,32 No consensus exists for sagittal GRF in CAI, similar to other GRF directions. We showed that GRFs in all 3 directions were significantly lower in CAI limbs, suggesting that players with CAI could execute soft and gentle landings in the SLDL. It was assumed that players with CAI may not jump higher and land harder due to CAI concerns. However, it is impossible to precisely determine how jump-landing strategies differ among players and limbs based on GRF. In future work, combining kinetics with kinematics and electromyography may be insightful.
For coper and control limbs in the non-CAI group, no differences in measurement items were observed between groups. A history of previous ankle sprain is a factor in CAI; however, subjective evaluation tools such as CAIT score or giving way sensation are more relevant for precise CAI selection. Consequently, we included both coper and control limbs in the non-CAI limb group.
Limitations
This study had several limitations. First, we did not evaluate ankle laxity using an arthrometer or radiographic imaging. However, instability feelings can occur in the absence of laxity. Second, we did not include previous injuries to the lower extremity and trunk. 12 Third, we did not include lower limb and trunk kinematics in the SLDL task, and differences in kinematics could influence the TTS and GRF in SLDL. However, several studies have reported no significant differences in kinematics between participants with CAI and controls during anterior unilateral stop jumps or single-leg jumps. 2,8,10,32 Therefore, we investigated kinematics in drop vertical jumps in participants with CAI. Fourth, muscle strength in lower extremities was not assessed.
Conclusion
The TTS of horizontal GRF and the trajectory length of COP decreased in the CAI limb compared with the non-CAI limb. The peak GRFs in all 3 directions were significantly lower, and the time to peak GRF occurred much later in the CAI limb compared with the non-CAI limb in SLDL. These findings indicated that soccer players with CAI had decreased dynamic postural stability that led them to land softly when performing the SLDL task. This measurement could be useful in an evaluation of CAI.
Acknowledgment
The authors gratefully acknowledge the cooperation of physicians, physical therapists, and athletic trainers as volunteer staff in our study.
Footnotes
Final revision submitted March 13, 2022; accepted March 31, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding was provided in the form of scholarships from the East Japan Railway Company and Shimamura-Syoukai, as well as grants from the Nakatomi Foundation; the Japanese Orthopaedic Society of Knee, Arthroscopy and Sports Medicine; the Japanese Sports Medicine Foundation; the Japan Sport Council; the Watanabe Memorial Foundation for the Advancement of Technology; and the Japan Orthopaedics Traumatology Foundation. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Graduate School of Medicine and Faculty of Medicine, University of Tokyo (study No. 11907-2).
References
- 1. Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brown C, Bowser B, Simpson KJ. Movement variability during single leg jump landings in individuals with and without chronic ankle instability. Clin Biomech (Bristol, Avon). 2012;27(1):52–63. [DOI] [PubMed] [Google Scholar]
- 3. Brown C, Padua D, Marshall SW, Guskiewicz K. Individuals with mechanical ankle instability exhibit different motion patterns than those with functional ankle instability and ankle sprain copers. Clin Biomech (Bristol, Avon). 2008;23(6):822–831. [DOI] [PubMed] [Google Scholar]
- 4. Caulfield B, Garrett M. Changes in ground reaction force during jump landing in subjects with functional instability of the ankle joint. Clin Biomech (Bristol, Avon). 2004;19(6):617–621. [DOI] [PubMed] [Google Scholar]
- 5. Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis. 2011;69(1):17–26. [PubMed] [Google Scholar]
- 6. de Noronha M, Refshauge KM, Crosbie J, Kilbreath SL. Relationship between functional ankle instability and postural control. J Orthop Sports Phys Ther. 2008;38(12):782–789. [DOI] [PubMed] [Google Scholar]
- 7. De Ridder R, Willems T, Vanrenterghem J, Robinsonet MA, Palmans T, Roosen P. Multi-segment foot landing kinematics in subjects with chronic ankle instability. Clin Biomech (Bristol, Avon). 2015;30(6):585–592. [DOI] [PubMed] [Google Scholar]
- 8. De Ridder R, Willems T, Vanrenterghem J, Robinson MA, Roosen P. Lower limb landing biomechanics in subjects with chronic ankle instability. Med Sci Sports Exerc. 2015;47(6):1225–1231. [DOI] [PubMed] [Google Scholar]
- 9. Delahunt E, Monaghan K, Caulfield B. Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. J Orthop Res. 2006;24(10):1991–2000. [DOI] [PubMed] [Google Scholar]
- 10. Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Deahunt E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am J Sports Med. 2016;44(4):995–1003. [DOI] [PubMed] [Google Scholar]
- 11. Doherty C, Delahunt E, Caulfield B, Hertel JR, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sport Med. 2014;44(1):123–140. [DOI] [PubMed] [Google Scholar]
- 12. Finch CF, Cook J. Categorising sports injuries in epidemiological studies: the subsequent injury categorisation (SIC) model to address multiple, recurrent and exacerbation of injuries. Br J Sports Med. 2014;48(17):1276–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fransz DP, Huurnink A, de Boode VA, Kingma I, van Dieën JH. Time to stabilization in single leg drop jump landings: an examination of calculation methods and assessment of differences in sample rate, filter settings and trial length on outcome values. Gait Posture. 2015;41(1):63–69. [DOI] [PubMed] [Google Scholar]
- 14. Fransz DP, Huurnink A, Kingma I, et al. Performance on a single-legged drop-jump landing test is related to increased risk of lateral ankle sprains among male elite soccer players: a 3-year prospective cohort study. Am J Sports Med. 2018;46(14):3454–3462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fransz DP, Huurnink A, Kingma I, van Dieën JH. How does postural stability following a single leg drop jump landing task relate to postural stability during a single leg stance balance task? J Biomech. 2014;47(12):3248–3253. [DOI] [PubMed] [Google Scholar]
- 16. Gribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. Br J Sports Med. 2014;48(13):1014–1018. [DOI] [PubMed] [Google Scholar]
- 17. Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. [DOI] [PubMed] [Google Scholar]
- 18. Kaminski TW, Hertel J, Amendola N; et al. National Athletic Trainers’ Association. National Athletic Trainers’ Association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48(4):528–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12(3):129–135. [DOI] [PubMed] [Google Scholar]
- 20. Kunugi S, Masunari A, Noh B, Mori T, Yoshida N, Miyakawa S. Cross-cultural adaptation, reliability, and validity of the Japanese version of the Cumberland ankle instability tool. Disabil Rehabil. 2017;39(1):50–58. [DOI] [PubMed] [Google Scholar]
- 21. Kunugi S, Masunari A, Yoshida N, Miyakawa S. Association between Cumberland ankle instability tool score and postural stability in collegiate soccer players with and without functional ankle instability. Phys Ther Sport. 2018;32:29–33. [DOI] [PubMed] [Google Scholar]
- 22. McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Park YH, Park SH, Kim SH, Choi GW, Kim HJ. Relationship between isokinetic muscle strength and functional tests in chronic ankle instability. J Foot Ankle Surg. 2019;58(6):1187–1191. [DOI] [PubMed] [Google Scholar]
- 24. Pope M, Chinn L, Mullineaux D, McKeon PO, Drewew L, Hertel J. Spatial postural control alterations with chronic ankle instability. Gait Posture. 2011;34(2):154–158. [DOI] [PubMed] [Google Scholar]
- 25. Shiravi Z, Shadmehr A, Moghadam ST, Moghadam BA. Comparison of dynamic postural stability scores between athletes with and without chronic ankle instability during lateral jump landing. Muscles Ligaments Tendons J. 2017;7(1):119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Simpson JD, Stewart EM, Macias DM, Chander H, Knight AC. Individuals with chronic ankle instability exhibit dynamic postural stability deficits and altered unilateral landing biomechanics: a systematic review. Phys Ther Sport. 2019;37:210–219. [DOI] [PubMed] [Google Scholar]
- 27. Taketomi S, Kawaguchi K, Mizutani Y, et al. Anthropometric and musculoskeletal gender differences in young soccer players. J Sports Med Phys Fitness. 2021;61(9):1212–1218. [DOI] [PubMed] [Google Scholar]
- 28. Terada M, Gribble PA. Jump landing biomechanics during a laboratory recorded recurrent ankle sprain. Foot Ankle Int. 2015;36(7):842–848. [DOI] [PubMed] [Google Scholar]
- 29. van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Sports Med. 2008;121(4):324–331.e326. [DOI] [PubMed] [Google Scholar]
- 30. Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Naugle KE, Borsa PA. Dynamic postural control but not mechanical stability differs among those with and without chronic ankle instability. Scand J Med Sci Sports. 2010;20(1):e137–e144. [DOI] [PubMed] [Google Scholar]
- 31. Woods C, Hawkins R, Hulse M, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football. An analysis of ankle sprains. Br J Sports Med. 2003;37(3):233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wright CJ, Arnold BL, Ross SE. Altered kinematics and time to stabilization during drop-jump landings in individuals with or without functional ankle instability. J Athl Train. 2016;51(1):5–15. [DOI] [PMC free article] [PubMed] [Google Scholar]