Summary
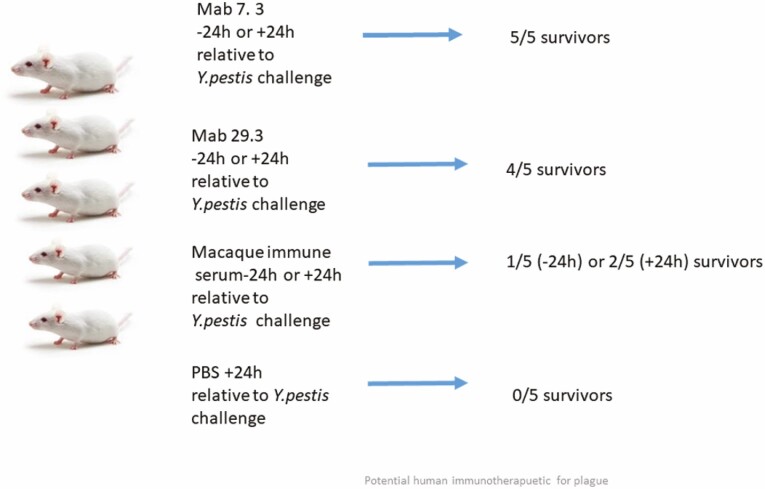
Two monoclonal antibodies directed to the V antigen of Yersinia pestis have been tested for protective efficacy in a murine model of bubonic plague. Mice were infected with a current clinical isolate from Madagascar, designated Y. pestis 10–21/S. Mab7.3, delivered to mice intra-periteoneally at either 24 h prior to, or 24 h post-infection, was fully protective, building on many studies which have demonstrated the protective efficacy of this Mab against a number of different clinical isolates of Y. pestis. Mab 29.3, delivered intra-peritoneally at either −24 h or +24 h, protected 4/5 mice in either condition; this has demonstrated the protective efficacy of this Mab in vivo for the first time. These results add to the cumulative data about Mab7.3, which is currently being humanized and highlight its potential as a human immunotherapeutic for plague, which is an enduring endemic disease in Madagascar and other regions of Africa, Asia, and South America.
Keywords: Plague, immunotherapeutic, passive therapy, protection, clinical isolate
Graphical Abstract
Introduction
Although an ancient disease, plague is still an unwelcome presence in certain regions of the world, where it exists in enzootic reservoirs and erupts form time to time. According to the World Health Organization (WHO), 3248 cases of human plague have been reported between 2010 and 2015 by 11 countries from Africa, the Americas and Asia [1]. During this period, Madagascar accounted for 74% of all cases reported worldwide with an 18% case fatality rate, making this island the most affected country in the world [1]. Despite good public health measures, human plague cases occur on a seasonal basis in the central highlands (September–April), the most active plague foci in Madagascar, with a particularly serious outbreak occurring during the 2017/18 season with 2417 cases and 209 deaths [2].
Plague pathogenesis, caused by the bacterium Yersinia pestis, relies on two major virulence mechanisms: the expression, triggered by the human host’s body temperature of a protective proteinaceous capsule around the bacteria, which render them resistant to phagocytosis and cell-mediated killing [3]; and a type III secretion system (TTSS) which injects cytotoxic factors into host cells to promote bacterial colonization of tissues and organs [4]. Central to these mechanisms are the F1 protein in the capsule and the V antigen which orchestrates the TTSS [3, 4]. F1 and V also provide targets for vaccine and therapeutic approaches [5].
Characterization of anti-V monoclonal antibodies
Here, we focus on the protective potential of two monoclonal antibodies (Mabs) directed against the V antigen. Both Mabs have previously been shown to have at least in vitro binding or neutralization activity, protecting cultured cells against the cytotoxic effect of Yersinia pseudotuberculosis expressing the Y. pestis V antigen [6].
The first Mab is 7.3, an IgG1, which has been extensively studied by ourselves and others to be protective in both bubonic and pneumonic murine models of plague, when given at a range of time-points pre- or post-infection [7–10].
Mab 7.3 has prophylactic and therapeutic potential against Y. pestis causing the bubonic and pneumonic forms of plague. In addition, it is known that Mab7.3 binds to a region spanning amino acids 135–275 [9, 11] in the centre of the V antigen conformational structure [12], and this region is strongly influenced by the residue N255 [13]. Mab 7.3 has a fast association with the V antigen, high binding affinity for its target and long half-life (t1/2) of the antigen-antibody complex (Kd of Fab for V antigen is 80±7pM with t1/2 533±42 min) [14]. However when scaled against a number of other anti-V Mab’s, this binding affinity was not exceptional and so it seems that it is the location of Mab7.3’s binding to the V antigen which is particularly significant in determining its protective effect [10].
It has been hypothesized that the conformational epitope in the V antigen may be accessible to Mab7.3 [15] in the homopentamer formed by the V antigen on the tip of the TTSS needle [4], thus preventing Yop translocation, or disrupting the cooperative activity of Yops B and D to achieve pore formation in host cells, a pre-requisite for translocation [15]. This conclusion is reinforced by the observation that the Fc portion of Mab7.3 is not required for its neutralizing activity [14, 15], suggesting that its neutralizing effect is due to the direct binding of the variable portions of Mab7.3 to the V antigen. Interestingly, Mab7.3 was originally derived by immunization of mice with an SDS-denatured rV antigen; although one of a panel of 7 Mabs generated in the same way with denatured V antigen and all recognizing the region of V spanning amino acids 135–326, Mab7.3 was the only protective Mab [7].
The second Mab is 29.3, which is also an IgG1 and directed to the V antigen. Much less is known about this Mab, although evidence suggests that it binds to V at a locus near the epitope for Mab7.3 [14]. Also, although its in vitro binding to the V antigen is slower, of lower affinity and with shorter half-life (Kd of 399 ±27pM with t 1/2 of 247 ± 11 min) than that of Mab7.3, the variable regions, and not the Fc portion of this Mab have significant affinity for the V antigen [14] and it also has significant neutralizing activity in vitro for the cytotoxic effect of Y. pestis [15].
Prior to their use in this passive transfer study, the hybridoma supernates of each Mab were purified on a HiTrap Protein L column (Cytiva) to eliminate contamination from bovine immunoglobulin present in hybridoma growth media, and to achieve purified Mab’s at concentrations of 1 mg/ml (Mab7.3) and 1.7 mg/ml (Mab 29.3) respectively.
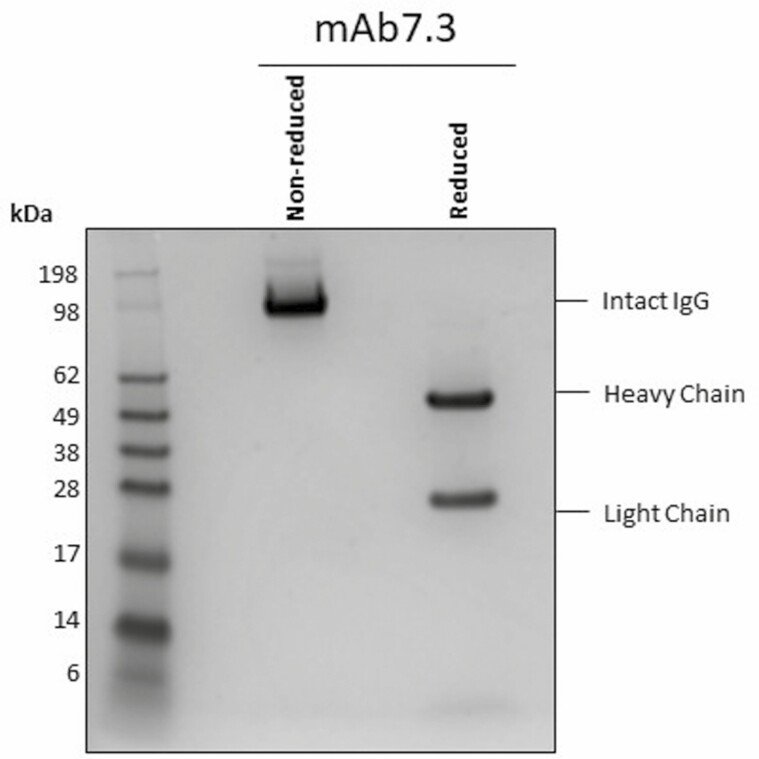
The Mab’s were evaluated by SDS-Page and a representative gel is shown for Mab7.3 (Fig. 1).
Figure 1.
SDS-Page for Mab 7.3. For the nonreduced sample, Mab7.3 was diluted to 5 µg in a final volume of 15 µl using NuPage LPS 4× sample buffer (Novex, NP007) in accordance with the manufacturer’s instructions. The reduced sample was prepared similarly, but with the addition instead of NuPage 10× sample reducing agent (Novex, NP004) and heating of the sample (95°C for 15 min). SDS-PAGE was performed after loading 10 µl of antibody samples and 5 µl of SeeBlue Plus2 marker (Invitrogen, LC5925) into a NuPAGE 4–12% gradient Bis-Tris gel. Electrophoresis conditions were 200 V for 20 min. The gel was stained with SimplyBlue Safe Stain (Invitrogen, LC6065) for 1 h and destained in distilled water overnight.
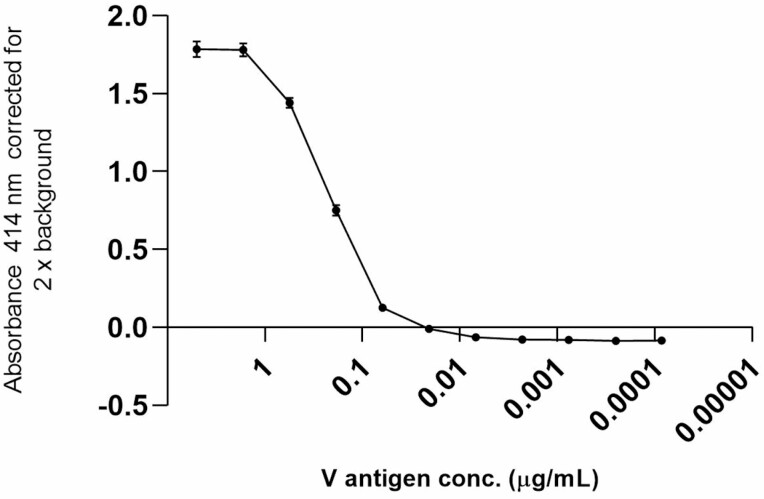
The limit of detection of V antigen by Mab 7.3 determined by titrating dilutions of the V antigen against a fixed concentration of Mab was 20 ng.ml-1 (Fig. 2).
Figure 2.
Limit of detection of V antigen by Mab 7.3. V antigen was coated to a microtitre plate in the dilution range 5 µg/ml to 85 pg/ml in triplicate (0.1 ml/well) and then probed with a fixed concentration (800 ng/ml) of biotinylated Mab 7.3. After washing in PBS/Tween 20 and blocking with 2% milk powder in PBS (Blotto), binding was detected with streptavidin peroxidase (Pierce High Sensitivity Streptavidin-HRP, 21132) at 1:10,000 in Blotto and developed with 2,2’-Azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) diammonium salt (ABTS; SeraCare, 5120-0041) and the signal was read at OD414. The LOD was 20 ng/ml.
To determine more about the prophylactic and therapeutic potential of these anti-V Mabs and building on the recent data in Amemiya et al. 2020 [10], we have now tested the ability of both Mab7.3 and Mab29.3 to protect a different strain of outbred mice from a current clinical isolate of Y. pestis from Madagascar.
OF1 female outbred mice (6–8 weeks of age) were used for this study. They were bred at the Institut Pasteur de Madagascar animal facility. Mice were randomized for allocation to treatment group with food and water ad libitum and acclimatized to the facility for 5 days prior to any procedures. Mice were dosed with Mab at either 24 h prior to, or 24 h post-infection with a clinical isolate of Y. pestis, which had been isolated in 2021 from the bubo of a confirmed plague case (F1+, qPCR+, culture+) in an 18-year-old male survivor, from Ankazobe District, one of the active plague foci in the Central Highlands of Madagascar. The Y. pestis 10/21-S strain has been genotyped and is of biovar Orientalis. Before use, the 10/21-S Y. pestis isolate was cultured for 2 days in Brain- Heart Infusion (BHI) broths (Oxoid Ltd., Basingstoke, England) to provide an inoculum and on Cefsulodin-Ingrasan-Novobiocin (CIN) agar plates to enumerate viable bacterial colonies. Following culture of Y.pestis 10/21-S in BHI at 37°C for >24 h, F1 and V expression were detected by immunoassay, whilst DNA from a 26°C-cultured extract of Y. pestis 10/21-S was positive for V antigen by qPCR. An in vivo pre-screen in naive OF1 mice had determined the median lethal dose (MLD) of the 10/21-S strain to be 65cfu (data not shown).
For the efficacy study, an estimated 30 cfu of the Y.pestis 10/21-S, determined by measuring the OD600 of the bacterial suspension, was inoculated sub-cutaneously (s.c.) in 0.1 ml at the back of the neck to all groups of mice. Mice were divided into seven groups, each comprising five mice and were dosed as follows:
Groups 1 and 2 were dosed with 50 µg Mab 7.3 at 24 h prior to (−24 h), or at 24 h post-infection (+24 h) respectively, with Y. pestis. Mab7.3 was diluted in PBS and delivered in 0.1 ml by the intra-peritoneal (i.p.) route. Groups 3 and 4 were dosed with 50 µg Mab 29.3 in 0.1 ml i.p. at −24 h or +24 h, respectively. Groups 5 and 6 were dosed with a 1:10 dilution in PBS of a pooled macaque immune serum, delivered in 0.1 ml i.p, as a positive control, at −24 h or +24 h, respectively. Group 7 mice served as negative controls and were dosed with 0.1 ml PBS by the i.p. route, at +24 h. The Y. pestis inoculum was enumerated retrospectively, from duplicate cultures on CIN-agar and determined to be 95 cfu/0.1 ml. Mice were observed for 14 days post-infection (p.i.) and were culled if they reached the humane end point beforehand. Survival curves are shown in Fig. 3.
Figure 3.
Survival of mice dosed with Mab 7.3. or Mab 29.3 or macaque immune serum pre- or post-infection with 95 cfu Y. pestis 10/21-S.
All of the negative control mice had succumbed to the bacterial infection by day 11. Mice receiving the pooled immune macaque serum at −24 h or +24 h had survival rates of 1/5 and 2/5, respectively, by day 14. In contrast, 4/5 mice receiving Mab 29.3 at either −24 h or +24 h, survived until the end of the observation period (day 14). However 5/5 mice administered Mab 7.3 at either −24 h or +24 h, survived to day 14 (Fig. 3; Table 2). Statistical analysis of the survival curves showed that Mabs 7.3 and 29.3 conferred significant survival benefit, compared with the negative control group (P = 0.0002, P = 0.007, respectively by Log-rank Mantel-Cox test). There were no significant differences in the survival curves resulting from Mab7.3 versus Mab29.3, when either Mab was given at −24 h or +24 h. There were no significant differences in the survival curves resulting from pre- or post-infection delivery of the macaque serum, but the macaque serum did not provide any survival benefit over untreated mice (P = 0.06); Mab 7.3 given at +24 h conferred significant benefit over the macaque serum at +24 h (P = 0.05).
Table 2.
The reported protective efficacy of Mab7.3 in murine bubonic and pneumonic plague models
| Mab 7.3 dosage | Pre-infection delivery; mouse strain | Post-infection delivery; mouse strain | Pneumonic /bubonic; median lethal dose/LD50; Y.p. strain | Survival | Reference |
|---|---|---|---|---|---|
| 350 µg | −24 h; Balb/c | Bubonic; 12 MLD; GB | 6/6 | [7] | |
| 35 µg | −24 h; Balb/c | Bubonic; 9.6MLD; GB | 5/6 | [8] | |
| 35 µg | −24 h; Balb/c | Bubonic; 96MLD; GB | 3/6 | [8] | |
| 35 µg | −4 h; Balb/c | Bubonic; 46MLD; GB | 7/10 | [8] | |
| 35 µg | −4 h; Balb/c | Pneumonic; 88MLD; GB | 10/10 | [8] | |
| 35 µg | −24 h; Balb/c | Pneumonic; 88MLD; GB | 8/10 | [8] | |
| 35 µg | +24 h;Balb/c | Bubonic; 46MLD; GB | 7/10 | [8] | |
| 35 µg | +48 h;Balb/c | Bubonic; 46MLD; GB | 3/10 | [8] | |
| 35 µg | +96 h;Balb/c | Bubonic; 46MLD; GB | 0/10 | [8] | |
| 30 µg | +24 h;C57Bl6 | Pneumonic (Intranasal); 12LD50;CO92 | 10/10 | [9] | |
| 3 µg | +24 h;C57Bl6 | Pneumonic (Intranasal); 12LD50;CO92 | 0/10 | [9] | |
| 50 µg | −24 h; Balb/c | Bubonic; 21LD50;CO92 | 8/8 | [10] | |
| 100 µg | −24 h; Swiss-Webster | Bubonic; 38LD50;CO92 | 6/6 | [10] | |
| 50 µg | −24 h OF1 | Bubonic; 1.5MLD; 10/21-S | 5/5 | This paper | |
| 50 µg | +24 h OF1 | Bubonic; 1.5MLD; 10/21-S | 5/5 | This paper |
Analysis of blood and tissues from surviving mice
Analysis of spleens and blood collected at the end of the observation period showed no recovery of Y. pestis from mice treated with Mab7.3 at −24 h and from only 1/5 mice treated with Mab 7.3 at +24 h (Table 1). Remarkably, 4/5 mice pretreated with Mab 7.3 had developed IgG to F1 antigen, suggesting that they had been exposed to F1-expressing, replicating bacteria. In contrast, 0/5 mice post-treated with Mab7.3 had developed IgG to F1, suggesting that p.i. dosing with Mab 7.3 had prevented bacterial replication to the extent that F1 expression did not occur in vivo to a level to induce an antibody response.
Table 1.
Summary of results
| Group and time of dosing relative to Y. pestis infection | N mice | N surviving mice (D14) | N surviving mice with Y. pestis1 | N positive anti-F1 IgG serology2 | |
|---|---|---|---|---|---|
| Mab 7.3 | −24 h | 5 | 5 | 0 | 4 |
| Mab 7.3 | +24 h | 5 | 5 | 1 | 0 |
| Mab 29.3 | −24 h | 5 | 4 | 1 | 2 |
| Mab 29.3 | +24 h | 5 | 4 | 0 | 2 |
| Macaque serum | −24 h | 5 | 1 | 1 | 5 |
| Macaque serum | +24 h | 5 | 2 | 0 | 0 |
| PBS | +24 h | 5 | 0 | 0 | 3 |
1Identified by culture of spleens and blood on CIN media and on BHI broth [22]. API20E biochemical strips were used to identify Y. pestis.
2Whole blood and sera were assayed for IgG to F1 antigen as previously described [23]. The threshold of positivity was set at an OD of 0.150 when using serum and at OD 0.050 when using whole blood.
The effect of pre- or post-dosing with Mab 29.3 on these parameters was less polarized: in each group, 2/5 mice were positive for IgG to F1 antigen and 1/4 mice surviving at day 14 p.i. was positive for Y. pestis in the pre-treatment group and 0/4 in the post-treatment group.
Pre-treatment with macaque immune serum resulted in 1 survivor at day 14 p.i.; this mouse was positive for plague and all the mice in this group had developed IgG to F1. The 2 surviving mice in the post-treatment with macaque immune serum group were negative for Y. pestis and negative for IgG to F1. There were no survivors in the negative control group; all were positive for Y. pestis and 3/5 had developed IgG to F1.
Discussion
Immunotherapy with Mab’s is being widely used in clinical medicine [16, 17], particularly for conditions such as rheumatoid arthritis and cancer [18] and more recently has been adopted as an adjunct to treating infectious disease in, for example, the successful use of the anti-IL6R therapy Tocilizumab in Covid-19 infection [19]. Here, we have explored Mabs to plague as potential immunotherapeutics.
This small study adds to the burden of proof of the efficacy of the anti-V Mab 7.3 as a potential therapeutic for plague. This Mab has now been independently tested in a number of laboratories and found to be consistently efficacious in murine studies (summarized in Table 2) in protecting against a number of clinical isolates of Y. Pestis, e.g. the GB isolate from a fatal laboratory accident in the UK in the 1960’s [cited in 20], the CO92 isolate from the USA [21], and now the 10/21-S isolate from Madagascar. Additionally, Mab 7.3 has been fully characterized in terms of its amino acid sequence (unpublished data), it is likely binding site for the V protein, its ability to neutralize the cytotoxic effect of the V antigen expressed in vitro and its protective effects in vivo in models of both pneumonic and bubonic plague. This Mab is currently being humanized for eventual clinical use.
Here, we have shown for the first time that Mab 29.3 can also protect mice in vivo against injected infection with the 10/21-S isolate of Y. pestis, adding to the previously published in vitro neutralization data for this Mab. Although not as solidly protective as Mab7.3, the level of protection observed (80%) for Mab 29.3 remains high, particularly since Mab therapy for the serious infection of plague, would likely be part of a layered approach in which the post-exposure therapy of individuals might also include vaccination and/or antibiotic therapy. Additionally, here we have tested only the 50 µg dose level of Mab29.3; by increasing the dose administered it may well be possible to improve efficacy.
A single bolus of passively transferred antibody (monoclonal or polyclonal) will have a limited half-life in vivo which, exacerbated by lesser neutralizing activity, is why we have seen breakthrough in this study in the protective effect conferred by the immune macaque serum used for reference here. In vitro data gained recently indicate that this pooled, polyclonal macaque reference serum [6] has become poorly neutralizing for the V antigen over some years of storage (unpublished data).
The F1 and V antigens are only produced by Y. pestis when the bacteria enter the host and expression is triggered at 37°C. F1 secreted by the bacteria forms a dense proteinaceous capsule around the bacteria, while the V antigen is intracellular and is secreted through the bacterial injectisome into host cells. It is not certain how long this process takes in vivo, perhaps 24 h or more and the level of expression will be challenge dose-related. Since none of the mice given Mab7.3 at 24 h p.i. had developed an anti-F1 response, this suggests that delivery of the Mab at this time may have effectively limited host cell invasion and replication of the bacterial challenge so that F1 was not expressed in vivo, at least not to a sufficient level to induce an IgG response. In contrast, 4/5 of the mice dosed with Mab 7.3 at −24 h had developed an anti-F1 titre, suggesting that although all of these mice survived, delivery of the Mab this much in advance did not limit bacterial replication such that the mice were exposed to F1-expressing bacteria.
The data reported here for Mab7.3 and 29.3 reinforce the importance of antibody responses to V as a key protective mechanism in plague. As well as their obvious immunotherapeutic potential, these Mabs also constitute a reference reagent to underpin the development and evaluation of existing and new vaccines against new isolates of Y. pestis.
Clearly, more work will need to be done in non-human primates and clinical safety trials, to determine a translational dosing regimen in man for Mab 7.3, but the accumulated murine data to date provides a sound basis for this.
Acknowledgements
The contribution of technical staff at the Institut Pasteur de Madagascar to this work is acknowledged with thanks. The Editor-in-Chief, Tim Elliott, and handling editor, Stefan Barth, would like to thank the following reviewers, Jennifer Maynard and Matthias Peipp, for their contribution to the publication of this article.
Glossary
Abbreviations
- CFU
Colony forming units
- F1
Fraction1 antigen
- Kd
Dissociation constant
- LOD
Limit of detection
- LD50
50% lethal dose
- Mab
Monoclonal antibody
- MLD
Median lethal dose
- OF1
Oncins France1 mouse
- qPCR
Quantitative PCR
- rV
Recombinant V antigen
- SDS
Sodium dodecyl sulphate
- T1/2
Half-life
- TTSS
Type three secretion system
- V
Virulence antigen
Content includes material subject to © Crown copyright (2021), Dstl. This material is licensed under the terms of the Open Government Licence except where otherwise stated. To view this licence, visit http://www.nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: psi@nationalarchives.gov.uk
Funding
This work was commissioned in part by Innovate UK and the UK Department of Health and Social Care (Project title “Serological Vaccine Standards for Emerging Diseases; File Ref. 971613). The views expressed in this publication are those of the author(s) and not necessarily those of Innovate UK, the Department of Health and Social Care, ‘arms’ length bodies or other government departments.
Author contributions
Conceptualization (E.D.W.); Funding acquisition (N.A., S.K.); Investigation (K.M.M., V.A., L.N.R.); Methodology (N.J.W., S.G.L.); Project administration (M.R.); Writing (V.A., K.M.M.); Review and editing (E.D.W.); Resources (M.R., S.G.L., E.D.W.).
Data availability
The data underlying this article are available in the article and in its online supplementary material.
Conflict of interest
None of the authors declares a conflict of interest.
References
- 1. World Health Organization. Plague around the world, 2010–2015. Wkly Epidemiol Rec 2016;91(8):89–93. http://www.who.int/wer26922822 [Google Scholar]
- 2. Plague outbreak in Madagascar; external situation report 14, 4 Dec 2017, WHO; afro.who.int/health-topics/plague/plague-outbreak-situation-reports. [Google Scholar]
- 3. Williams RC Jr, Gewurz H, Quie PG. Effects of fraction I from Yersinia pestis on phagocytosis in vitro. J Infect Dis 1972;126(3):235–41. doi: 10.1093/infdis/125.3.235 [DOI] [PubMed] [Google Scholar]
- 4. Mueller CA, Broz P, Müller SAet al. The V-antigen of Yersinia forms a distinct structure at the tip of injectisome needles. Science 2005;310(5748):674–6. doi: 10.1126/Science.1118476 [DOI] [PubMed] [Google Scholar]
- 5. Sun W, Singh AK. Plague vaccine: recent progress and prospects. npj Vaccines 2019;4(1):11. doi: 10.1038/s41541-019-0105-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Williamson ED, Flick-Smith HC, Waters Eet al. Immunogenicity of the rF1+rV vaccine for plague with identification of potential immune correlates. Microb Pathogen 2007;42:12–22. doi: 10.1016/j.micpath.2006.09.003 [DOI] [PubMed] [Google Scholar]
- 7. Hill J, Leary SE, Griffin KFet al. Regions of Yersinia pestis V antigen that contribute to protection against plague identified by passive and active immunization. Infect Immun 1997;65(11):4476–82. doi: 10.1128/iai.65.11.4476-4482.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hill J, Copse C, Leary Set al. Synergistic protection of mice against plague with monoclonal antibodies specific for the F1 and V antigens of Yersinia pestis. Infect Immun 2003;71(4):2234–8. doi: 10.1128/IAI.71.4.2234-2238.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin JS, Park S, Adamovicz JJet al. TNFa and IFNg contribute to F1/LcrV-targeted immune defense in mouse models of fully virulent pneumonic plague. Vaccine 2011;29(2):357–62. doi: 10.1016/j.vaccine.2010.08.099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Amemiya K, Dankmeyer JL, Keasey SLet al. Binding sites of anti-Lcr V monoclonal antibodies are more critical than the avidities and affinities for passive protection against Yersinia pestis infection in a bubonic plague model. Antibodies (Basel) 2003;71(4):2234–8. doi. 10.1128/IAI.71.4.2234-2238.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vernazza C, Lingard B, Flick-Smith HCet al. Small protective fragments of the Yersinia pestis V antigen. Vaccine 2009;279(21):2775–80. doi. 10.1016/j.vaccine.2009.03.011 [DOI] [PubMed] [Google Scholar]
- 12. Derewenda U, Mateja A, Devedjiev Yet al. The structure of Yersinia pestis V-antigen, an essential virulence factor and mediator of immunity against plague. Structure 2004;12(2):301–6. doi: 10.1016/j.str.2004.01.010 [DOI] [PubMed] [Google Scholar]
- 13. Hill J, Leary S, Smither Set al. N255 is a key residue for recognition by a monoclonal antibody which protects against Yersinia pestis infection. Vaccine 2009;27(50):7073–9. doi:10.1016.j.vaccine.2009.09.061 [DOI] [PubMed] [Google Scholar]
- 14. Read T, Olkhov R, Williamson ED, Shaw AM. Kinetic epitope mapping of monoclonal antibodies raised against the Yersinia pestis virulence factor LcrV. Biosensors and Bioelectronics 2015;65:47–53. doi: 10.1016/j.bios.2014.09.90 [DOI] [PubMed] [Google Scholar]
- 15. Ivanov MI, Hill J, Bliska JB. Direct neutralisation of type III effector translocation by the variable region of a Mab to Y. pestis LCRV. Clin Vacc Immunol 2015;21(5):667–73. doi: 10.1128/cvi.00013-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wraith David C. The future of immunotherapy: a 20-year perspective. Front Immunol 2017;8:Article 1668. doi: 10.3389/fimmu.2017.01668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Floudas CS, Brar G, Greten TF. Immunotherapy: current status and future perspectives. Dig Dis Sci 2019;64(4):1030–40. doi: 10.1007/s11620-019-05516-7 [DOI] [PubMed] [Google Scholar]
- 18. Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol 2020;20(11):651–68. doi.10.1038.s41577-020-0306-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rosas IO, Bräu N, Waters Met al. Tocilizumab in hospitalized patients with severe Covid-19 pneumonia. N. Engl J Med 2021;384(16):1503–16. doi. 10.1056/NEjMoa2028700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Russell P, Eley SM, Hibbs SEet al. A comparison of Plague vaccine, USP and EV76 vaccine induced protection against Yersinia pestis in a murine model. Vaccine 1995;13(16):1551–6. doi: 10.1016/0264.410x(95)00090-n [DOI] [PubMed] [Google Scholar]
- 21. Doll JM, Zeitz PS, Ettestad P, et al. Cat-transmitted fatal pneumonic plague in a person who traveled from Colorado to Arizona. Am J Trop Med Hyg 1994;51(1):109–14. doi:10.4269.ajtmh.1994.51.109 [DOI] [PubMed] [Google Scholar]
- 22. Rasoamanana B, Rahalison L, Raharimanana Cet al. Comparison of Yersinia CIN agar and mouse inoculation assay for the diagnosis of plague. Trans R Soc Trop Med Hyg 1996;90:651. doi: 10.1016/S0035-9203(96)9042-4 [DOI] [PubMed] [Google Scholar]
- 23. Dromigny JA, Ralafiarisoa L, Raharimanana C, Randriananja N, Chanteau S. La sérologie anti-F1 chez la souris OF1, test complémentaire pour le diagnostic de la peste humaine. Arch Inst Pasteur Madagascar 1998;64(1–2):18–20. ISSN: 0020-2495. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.