Abstract
Background
This study used CBCT images to evaluate the suitability of maxillary first and second molar sites to receive immediate implants. Buccopalatal and mesiodistal widths of maxillary molar inter-radicular septum were evaluated at three different levels (crestal, middle, and apical), in addition to assessments of the root apex and furcation proximities to the sinus floor and comparisons of these measurements between the first and second upper molar sites before extraction.
Methods
A total of 427 dental sites from 223 patients were used to measure the buccopalatal and mesiodistal widths of inter-septal/furcal (IRS) bone of maxillary first and second molars and vertical distances from the furcation and from all the root apices to the sinus floor (SF).
Results
Mean coronal-most buccopalatal/mesiodistal IRS widths were 7.33/6.52 mm for the first and 6.86/5.85 mm for the second molars (P=0.008). Corresponding mean FSD (furcation-sinus floor) values were 9.69 mm (range: 2.02-24.68 mm) and 8.84 mm (range: 1.48-25.09 mm). Mean distances from all the root apices to SF were <3 mm. The palatal roots of the first molars had higher sinus intrusion rates (28.85%) than their buccal counterparts, while for the second molars, the mesiobuccal roots showed the highest sinus intrusion (37.65%).
Conclusion
In the current patient sample, 61.7% of the first and 34% of the second molars had a sufficiently broad IRS to encase a 5-mm-diameter IMI (immediate molar implant) completely. The mean FSD of 9 mm for both molars indicated that some sinus floor elevation would likely be needed unless short implants were used.
Keywords: Cone-beam computed tomography, immediate implant, inter-radicular septum, maxillary molar
Introduction
Cone-beam computed tomographic (CBCT) scans are now universally considered the gold standard for implant site assessment and treatment planning. 1 These three-dimensional cross-sectional images help the surgeon optimize implant positioning and avoid complications. 2 The placement of dental implants at the time of tooth extraction (immediate implantation) was introduced in 1989 by Lazzara 3 and is now widely used. The advantages of this approach include a reduction in the number of surgical interventions and overall treatment times.
When screening for immediate molar implant (IMI) treatment in the maxilla, some important pre-extraction radiographic parameters that need consideration include the dimensions of inter-radicular septal bone (IRS), the distance (bone height) between the molar furcation and sinus floor (SF), the distance from SF to each root apex, and any root intrusion into the sinus.
Within a few months following tooth extraction, substantial losses in vertical and buccopalatal alveolar ridge widths are expected to occur at maxillary molar sites. 4 Furthermore, when more than one molar is lost in a maxillary sextant, sub-antral bone height losses of another 2 to 5.27 mm can occur. 5 Any associated post-extraction sinus pneumatization might further limit the bone available for future placement of implants to replace lost molars with often greater pneumatization at maxillary second versus first molar sites and where two or more adjacent posterior teeth have been removed. 6 Once all these changes have occurred, traditional delayed dental implant placement often becomes challenging, invasive, and costly. As a result, keen interest has developed in employing immediate maxillary molar implant treatment if certain prerequisites can be met. Systematic literature reviews with meta-analyses have suggested that IMIs have similar outcomes for implants placed in healed extraction sites. 7,8 To date, however, the use of maxillary immediate molar implants has not been widely prescribed because of technical difficulties. 9
The key to success with maxillary IMI treatment is careful site selection. A pre-treatment (i.e., before extraction) CBCT radiographic assessment is essential to estimate the remaining dimensions of the inter-radicular septal bone (IRS) associated with the molar furcation. Smith and Tarnow categorized molar socket IRSs into three types depending on their usefulness in stabilizing an implant of sufficient diameter to support a molar crown. 10 Type A extraction sites have adequate IRS volume to completely contain the coronal perimeter of an appropriately sized implant (i.e., ≥5 mm in diameter) and are the most favorable sites for maxillary IMIs. In contrast, Type B sites are those that can stabilize the implant but not contain it completely. Finally, the IRS at Type C sites will have an insufficient volume to allow osteotomy localization within it. As a result, achieving stability of an IMI intended for a Type C socket will require either an even wider diameter implant to make some contact with the socket walls or placement of a longer implant into the palatal root socket if adequate bone remains apically to stabilize it. 11 The mean available heights from furcation to sinus floor have been reported to be 7.43 mm for maxillary first and 7.07 mm for maxillary second molars. In contrast, an inter-radicular septum (IRS) is present in 74% of maxillary first and 44% of maxillary second molars. 12
Smith & Tarnow classification can be roughly utilized as a useful clinical guide for placing appropriate sizes of dental implants into the IRS. However, there appears to be no published numerical data to help clinicians define IRS dimensions before extraction for the three socket types established by Smith and Tarnow and how these dimensions might vary between first molar (MFM) and second maxillary molar (MSM) sites. Previous studies using coronal and sagittal CBCT images have reported average distances from root apices to the sinus floor, 13-16 and between molar furcation and sinus floor. 17 However, none have addressed any dimensional differences in these parameters between first and second molars. Accordingly, the present study used CBCT data to assess the buccopalatal and mesiodistal widths of maxillary molar IRS at three different levels (crestal, middle, and apical) as well as assessments of both root apex and furcation proximities to the sinus floor (SF) and comparisons of these measurements between first and second molar sites before extraction.
Methods
The CBCT images used for this retrospective study were obtained from the files of 223 patients seeking dental treatment in two different maxillofacial radiology centers in Lahijan, Iran, and Toronto, Canada, between 2016 and 2019. All the patients signed a consent form permitting that their CBCT images could be used for the measurements necessary for this research project. In total, 427 dental sites were eligible based on the fact that maxillary permanent first and/or second molars were present. Criteria for inclusion in the study were as follows:
Age >18 years
The presence of at least two occluding maxillary posterior teeth (premolar and/or molar) at least one of which was a fully erupted molar with fully formed root apices
No radiographic/clinical evidence of sinus pathology
No radiographic evidence of periodontal disease (bone loss), infection, severe root resorption, or periapical pathology
No history of previous surgical interventions of the selected teeth
Absence of metal restorations in the molar teeth that could create artifacts affecting the desired CBCT measurements
No current drug or alcohol abuse issues, history of chemotherapy, or relevant radiotherapy
No history of medications affecting the skeletal system
All the scans were taken using the same CBCT machine (Sirona Dental Systems, Bensheim, Germany) set at 98 kVp and 12 mA and assessed using Galileos viewer 1.9 software program (Sirona Dental Systems, Bensheim, Germany). To assess examiner reliability, all the images were measured twice within a 4-week interval. All the images were examined using a strict protocol after first rotating them such that their long axes were perpendicular to the occlusal plane. The axial CBCT view of the central fossa of each molar assisted in selecting the desired coronal and sagittal slices.
The following measurements were obtained from the CBCT images of each tooth:
Using axial images, IRS widths were recorded both mesiodistally and buccopalatally at three levels, i.e., crestal widths at 0.5 mm apical to the furcation, apical widths recorded at 0.5 mm coronal to a line connecting the apices of the two shortest roots, and middle level measurements taken at the mid-point between the other two measurement levels (Figure 1).
Figure 1.

(a) A crestal measurement was recorded 0.5 mm apical to the molar furcation. (b) An apical measurement was recorded 0.5 mm coronal to the line connecting the apices of the two shortest roots. (c) A middle measurement was recorded midway between the crestal and apical levels; (d), (e), and (f) show the axial views of the same points corresponding to a, b, and c, respectively (MB: mesiobuccal, DB: distobuccal, P: palatal).
To allow impartial measurements at each of the three levels of data collection, reference lines were placed, as shown in Figure 2. To do this, the most mesial points of the mesiobuccal and palatal roots of the tooth were determined and connected by a straight line, and its halfway point was denoted as point mid-mesial (MM). Similarly, a straight line connecting the most distal points of the mesiodistal and palatal roots was used to establish a point called mid-distal (MD), and another connecting the most buccal aspects of the two buccal roots was used to establish the point designated mid-buccal (MB). After that, the distance between points MM and MD was recorded as the mesiodistal width of the IRS (MDW). Similarly, the buccopalatal IRS width (BPW) was recorded as the measurement from MB to the most buccal point of the palatal root.
Figure 2.

Buccopalatal width (BPW) and mesiodistal width (MDW) measurements were recorded at each of the crestal, middle, and apical levels of each molar IRS.
The distance (FSD) from the sinus floor (SF) to the molar furcation in the mid-most CBCT slice was recorded as described by Choi et al (Figure 3). 17
Figure 3.

A measurement of the distance (FSD) from the furcation to the sinus floor (SF) was made in the middle-most coronal CBCT slice.
The shortest distance to SF from each root apex was recorded in the coronal slice (Figure 4).
Figure 4.
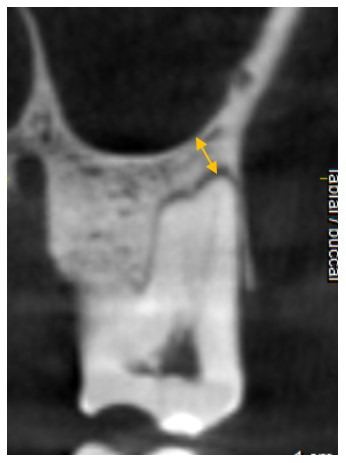
This figure shows an example of the measurement recorded for the distance of the mesiobuccal root apex to SF. In all the images, the closest point to SF was selected.
The abbreviations for the parameters measured are as follows:
FSD = furcation to sinus floor distance
CBPD = crestal buccopalatal septum diameter
MBPD = middle buccopalatal septum diameter
ABPD = apical buccopalatal septum diameter
CMDD = crestal mesiodistal septum diameter
MMDD = middle mesiodistal septum diameter
AMDD = apical mesiodistal septum diameter
MBRS = mesiobuccal root apex-to-sinus distance
DBRS = distobuccal root apex-to-sinus distance
PRS = palatal root apex-to-sinus distance
Continuous variables of the first and second molars were compared with Student’s t-test. Pearson’s correlation analysis was used to assess any collinearity in the listed measures for each molar. Examiner reliability was assessed by the intraclass correlation coefficient. Linear mixed model analysis was employed to assess any differences in measures of MBRS, DBRS, and PRS to accommodate for the collinearity of these measurements from the same molar. Examiner reliability was evaluated at a statistical significance of P<0.05. Version 9.4 of Windows’ SAS was employed for all the analyses.
Results
The intraclass correlation coefficient was 0.91. Table 1 summarizes continuous variables for the different CBCT measurements taken at maxillary first and second molars, as means, standard deviations, medians and/or ranges.
Table 1. The CBCT measurements taken at maxillary first and second molars are summarized as means, standard deviations, medians, and/or ranges .
| First Maxillary Molars | Second Maxillary Molars | |||||||
| N | Mean (+SD) | Min | Max | N | Mean (+SD) | Min | Max | |
| FSD | 201 | 9.69 (4.29) | 2.02 | 24.68 | 201 | 8.84 (3.54) | 1.48 | 25.09 |
| CBPD | 203 | 7.33 (1.22)a | 1.54 | 10.83 | 200 | 6.86 (1.63)b | 1.3 | 12.78 |
| MBPD | 203 | 8.39 (1.24)a | 2.61 | 11.03 | 201 | 7.69 (1.78)b | 2.58 | 13.23 |
| ABPD | 203 | 9.24 (1.62)a | 3.20 | 12.61 | 201 | 7.54 (2.19)b | 1.66 | 11.84 |
| CMDD | 203 | 6.52 (1.2)a | 2.18 | 8.89 | 200 | 5.85 (1.36)b | 1.79 | 8.94 |
| MMDD | 203 | 6.17 (1.11)a | 2.65 | 8.63 | 201 | 5.34 (1.38)b | 1.95 | 8.38 |
| AMDD | 203 | 5.22 (1.4)a | 2.18 | 8.41 | 201 | 3.97 (1.55)b | 1.34 | 7.79 |
| MBRS | 203 | 3.06 (4.44)aA | -5.59 | 17.3 | 199 | 1.34 (3.52)bA | -5.56 | 16.02 |
| DBRS | 200 | 2.78 (4.14) | -4.20 | 16.11 | 201 | 2.68 (3.43)B | -3.90 | 14.41 |
| PRS | 201 | 2.54 (4.58)B | -5.68 | 17.42 | 201 | 2.96 (3.57)B | -4.57 | 14.58 |
Different capital letters indicate significant differences in vertical lines, and different lowercase letters indicate significant differences in the horizontal lines.
furcation to sinus floor distance (FSD), crestal buccopalatal septum diameter (CBPD), middle buccopalatal septum diameter (MBPD), apical buccopalatal septum diameter (ABPD), crestal mesiodistal septum diameter (CMDD), middle mesiodistal septum diameter (MMDD), apical mesiodistal septum diameter (AMDD), mesiobuccal root apex-to-sinus distance (MBRS), distobuccal root apex-to-sinus distance (DBRS), palatal root apex-to-sinus distance (PRS)
Estimation of the inter-radicular septum (IRS) diameters
The mean crestal (CBPD), middle (MBPD), and apical (ABPD) buccopalatal IRS widths for maxillary first molars were 7.33, 8.39, and 9.24 mm, respectively, compared to those for second maxillary molars, i.e., 6.86, 7.69, and 7.54 mm. These mean values were significantly different (P=0.008, P=0.003, and P<0.0001, respectively) between the first and second molar sites. Regarding mesiodistal widths of IRS, the mean crestal (CMDD), middle (MMDD), and apical (AMDD) values for maxillary first molars were 6.52, 6.17, and 5.22 mm, respectively, compared to the corresponding values for second molars (5.85, 5.34, and 3.97 mm); and, once again all these parameters were significantly different between the two molar sites (P=0.014, P<0.0001, and P<0.0001, respectively). It was of interest for us to estimate the percentage of molar IRS values that could be classified as Types A, B, and C. In their original classification, Smith and Tarnow 10 did not provide actual measurements for each IRS type. Rather, they based the differences on whether or not the crestal aspect of a 5-mm-diameter implant could be inserted to be completely encased in bone or not. Therefore, in the present investigation, we arbitrarily assigned dimensions for each IRS type as follows: Type A to have >6 mm of bone both M-D and B-P; Type B to have between 3 mm and 6 mm of M-D or B-P and Type C to have <3 mm of IRS bone M-D or B-P. This allowed us to estimate the percentages shown in Table 2.
Table 2. Percentage of Types A, B, and C forfirst and second molars .
| First Maxillary Molars | Second Maxillary Molars | |
| Type | % | % |
| Type A | 61.7 | 34.03 |
| Type B | 33.45 | 59.41 |
| Type C | 4.85 | 6.56 |
Furcation to sinus floor distances (FSD)
The mean FSD distance for maxillary first molars was 9.69 mm, with a range of 2.02-24.68 mm. The corresponding mean value for second molars was 8.84 mm (range: 1.48-25.09 mm). These distances were not significantly different (P=0.539). These FSD distances were categorized into <5, 5-9, and >9 mm (Table 3). Based on these measurements, and assuming that 5 mm of FSD is sufficient to place an implant without the need for direct sinus floor elevation, fewer second molar sites would require this more invasive treatment.
Table 3. Categorization of FSD measurements for both molar locations .
| First Maxillary Molar | Second Maxillary Molar | |
| FSD | % | % |
| <5mm | 17.58 | 9.16 |
| 5-9mm | 21.23 | 49.17 |
| >9mm | 61.19 | 41.67 |
Furcation to sinus distance (FSD)
The distance from the root apex to the sinus floor
Mean distances from the mesiobuccal (MBRS), distobuccal (DBRS), and palatal (PRS) root apex to SF were 3.06, 2.78, and 2.54 mm for first molars and 1.34, 2.78, and 2.54 mm for second molars. Only the MBRS distances were significantly different (P=0.035) between the two molar sites.
Root intrusion
Regarding root intrusion into the sinus, 38.94% of first and 45.45% of second molars had one or more roots showing intrusion into the sinus (Table 4). The palatal roots of maxillary first molars showed higher intrusion rates (28.85%) than the two buccal roots, while with second molars, the mesiobuccal roots were more likely to intrude into the sinus (37.65%) (Table 5).
Table 4. Descriptive statistics of root intrusion for first and second maxillary molars mesiobuccal root apex-to-sinus (MBR), distobuccal root apex-to-sinus (DBR), palatal root apex-to-sinus (PR) distances .
| With Intrusion | Without Intrusion | ||||||||
| Tooth | Percentage | Min | Max | Mean (±SD) | Percentage | Min | Max | Mean (±SD) | |
| First Maxillary Molars | MBR | 20.18 | –5.59 | –0.31 | –1.81(1.37) | 79.82 | 0.21 | 17.3 | 5.15(3.93) |
| DBR | 24.51 | 4.20 | –0.11 | –1.87(1.48) | 75.49 | 0.23 | 16.11 | 4.89 (3.85) | |
| PR | 28.85 | –5.68 | –0.14 | –1.61(1.4) | 71.15 | 0.18 | 17.42 | 5.37(3.81) | |
| Second Maxillary Molars | MBR | 37.65 | –5.56 | –0.19 | –1.61(1.09) | 63.35 | 0.11 | 16.02 | 3.13(3.26) |
| DBR | 20.48 | –3.90 | –0.22 | –1.84(1.21) | 79.52 | 0.05 | 14.41 | 3.85(2.91) | |
| PR | 22.89 | –4.57 | –0.14 | –1.37(1.17) | 77.11 | 0.04 | 14.58 | 4.02(3.13) | |
Table 5. Percentages of first and second maxillary molars with no or one, two, and three root apex intrusions .
| First Maxillary Molar | Second Maxillary Molar | |||
|
Number of
Intruded roots |
Percentage |
Cumulative
Percentage |
Percentage |
Cumulative
Percentage |
| 1 | 18.58 | 18.58 | 27.27 | 27.27 |
| 2 | 9.73 | 28.32 | 11.36 | 38.64 |
| 3 | 10.62 | 38.94 | 6.82 | 45.45 |
| No intrusion | 61.06 | 100.00 | 54.55 | 100.00 |
Discussion
There are some key clinical factors affecting outcomes following immediate molar implant (IMI) placement. 18 One of them is socket anatomy, which will dictate whether an IMI can be properly stabilized. 19,20 Optimal, prosthetically driven IMI positioning is often best achieved if the implant osteotomy is prepared into the inter-septal/furcal bone (IRS). The results of the present study determined the mean coronal-most, buccopalatal, and mesiodistal IRS widths at 7.33 and 6.52 mm for maxillary first molars and 6.86 and 5.85 mm for second molars, respectively. In addition, buccopalatal widths of IRS increased towards the apical level while mesiodistal IRS widths decreased apically (see Table 1).
In their classification of maxillary molar socket anatomies, Smith and Tarnow 10 designated Type A sockets to be those into which an implant of at least 5-mm diameter can be placed into the remaining IRS such that its entire coronal portion, when seated, is fully surrounded by bone. Combining the assumption of Smith and Tarnow with our new data, we suggest that Type A sockets are those with IRS widths >6 mm.
Assuming that >6 mm of IRS width buccopalatally and/or mesiodistally would be required to house a 5-mm-diameter implant, we estimated that in our sample of patients, 61.7% of maxillary first molars and 34.34% of second molars were qualified as Type A. For Type B sockets, i.e., those classified by Smith and Tarnow as having sufficient IRS bone to stabilize an IMI but insufficient to encase its coronal portion fully, we assigned the measurement range between 3 and 6 mm. Based on these values, it was estimated that 33.45% of first and 59.41% of second molar sites were Type B in our sample. Only 4.85% of first and 6.56% of second molar sockets in our sample were Type C, which we considered to be those <3 mm in width.
In their latest report, Smith et al 20 reported retrospective outcomes for 300 IMIs placed in either jaw (specific numbers per jaw not given) from 2006 to 2017, including a technique development phase. Flap-less surgery during extraction and no peri-implant gap grafting or barrier membranes were used. Only twenty Type A sockets were identified, suggesting that more mandibular than maxillary sites and/or more second (see there Figures 7 to 13) than first molar sites were treated. The majority were Type B (185) or Type C (95) sockets, and while failure was <3%, all failures were in Type B sockets. The authors did not speculate on why Type B sockets were the most challenging. Implants from five different manufacturers were used with lengths and diameters ranging from 8.5 to 13 mm and 4 to 9 mm, respectively. Only eighteen of the 300 implants were 4 mm in diameter, with 106 being ≥6 mm in diameter and the remainder between 4.6 and 5.8 mm in diameter. They reported that with Type C and some Type B sockets, insufficient IRS meant that a crucial factor for success was the need for intact, thick outer bony socket walls and use of implants of wide enough diameter to contact these walls; interestingly, only one of the 106 implants measuring ≥6 mm in diameter failed.
The mean FSD height, i.e., bone height between the molar furcation and sinus floor, of IRS in the present sample was 9.69 mm for first and 8.84 mm for second molar sockets. However, others have reported that provided that FSD is ≥5 mm at a healed molar extraction socket that an implant can be placed without the need for direct sinus floor elevation techniques. 21 If one assumes that an FSD of ≥5 mm is also suitable for placing an IMI, then 82.42% of the first molar and 90.84% of the second molar sockets in the present sample could be considered favorable.
If the clinician concludes that there is insufficient IRS bone volume to secure an IMI (Types B or C), one option might be to place the implant into the tooth’s palatal root socket using the bone available apically to gain primary stability. 22 However, mean distances from the palatal root apices to the sinus floor in the present sample were <3 mm. In addition, palatal root intrusion into the sinus needs consideration since 28.85% of first molar palatal root apices showed such intrusion adding additional difficulty and risk. Less palatal root intrusion into the sinus (22.89%) was found at second molar sites, suggesting that implant placement into the palatal root here might be an option.
Conclusions
Valuable pre-extraction information can be obtained from CBCT scans of maxillary molars being considered for immediate replacement with dental implants (IMIs). If sufficient inter-septal/furcal bone (IRS) remains, the ideal osteotomy location for an IMI is considered to be in the IRS. In the sample of patients considered in the present study, 61.7% of maxillary first molars, but only 34% of second molars, would have been potential candidates for this treatment approach. In addition, the mean bone heights from the furcation to the sinus floor (FSD) in the present sample for both molar sites was approaching 9 mm, indicating that unless a short implant 23 was to be used, some sinus floor elevation, possibly using trans-crestal techniques, would be necessary at most sites.
Authors’ contributions
Conceptualization, MK and DD; methodology, MK and DD; investigation, MED; resources, AR; writing the original draft, MK and DD; formal analysis, EA; writing the review and editing, MK and DD; supervision, DD.
Avalibility of data
The data from the reported study are available upon request from the corresponding author.
Ethics approval
The protocol of the present study was approved by the Ethics Committee of Guilan University of Medical Sciences under the code IR.GUMS.REC.1396.324. Written informed consent was obtained from all the patients for using their scans in this study.
Competing interests
The authors declare that they have no competing interests regarding authorship and/or publications of this paper.
Acknowledgments
None.
Funding Statement
Funding: This study was not financially supported by any entity.
References
- 1.Wanschitz F, Birkfellner W, Watzinger F, Schopper C, Patruta S, Kainberger F. et al. Evaluation of accuracy of computer-aided intraoperative positioning of endosseous oral implants in the edentulous mandible. Clin Oral Implants Res. 2002;13(1):59–64. doi: 10.1034/j.1600-0501.2002.130107.x. [DOI] [PubMed] [Google Scholar]
- 2.Reddy MS, Mayfield-donahoo T, Vanderven FJJ, Jeffcoat MK. A comparison of the diagnostic advantages of panoramic radiography and computed tomography scanning for placement of root form dental implants. Clin Oral Implants Res. 1994;5(4):229–238. doi: 10.1034/j.1600-0501.1994.050406.x. [DOI] [PubMed] [Google Scholar]
- 3. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent 1989;9(5):332-343. https://pubmed.ncbi.nlm.nih.gov/2640210/. Accessed March 16, 2021. [PubMed]
- 4.Tan WL, Wong TLT, Wong MCM, Lang NP. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012;23(Suppl 5):1–21. doi: 10.1111/j.1600-0501.2011.02375.x. [DOI] [PubMed] [Google Scholar]
- 5.Harorh A, Bocutoglu O. The comparison of vertical height and width of maxillary sinus by means of Waters’ view radiograms taken from dentate and edentulous cases. Ann Dent. 1995;54(1-2):47–49. [PubMed] [Google Scholar]
- 6.Sharan A, Madjar D. Maxillary sinus pneumatization following extractions: a radiographic study. Int J Oral Maxillofac Implants. 2008;23(1):48–56. [PubMed] [Google Scholar]
- 7.Ketabi M, Deporter D, Atenafu EG. A Systematic Review of Outcomes Following Immediate Molar Implant Placement Based on Recently Published Studies. Clin Implant Dent Relat Res. 2016;18(6):1084–1094. doi: 10.1111/cid.12390. [DOI] [PubMed] [Google Scholar]
- 8.Atieh MA, Payne AGT, Duncan WJ, Cullinan MP. Immediate restoration/loading of immediately placed single implants: Is it an effective bimodal approach? Clin Oral Implants Res. 2009;20(7):645–659. doi: 10.1111/j.1600-0501.2009.01725.x. [DOI] [PubMed] [Google Scholar]
- 9. Dawson A, Chen S. The SAC Classification in Implant Dentistry Quintessence Publishing; 2009.
- 10.Smith RB, Tarnow DP. Classification of Molar Extraction Sites for Immediate Dental Implant Placement: Technical Note. Int J Oral Maxillofac Implants. 2013;28(3):911–916. doi: 10.11607/jomi.2627. [DOI] [PubMed] [Google Scholar]
- 11.Wychowański P, Woliński J, Kacprzak M, Tomkiewicz W, Bartłomiej I, Szubińska-Lelonkiewicz D. et al. Immediate Palatal Molar Implants: A Simple, Safe, Minimally Invasive Technique. Int J Periodontics Restorative Dent. 2017;37(6):e297–e301. doi: 10.11607/prd.3025. [DOI] [PubMed] [Google Scholar]
- 12.Agostinelli C, Agostinelli A, Berardini M, Trisi P. Radiological evaluation of the dimensions of lower molar alveoli. Implant Dent. 2018;27(3):271–275. doi: 10.1097/ID.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 13.Tian XM, Qian L, Xin XZ, Wei B, Gong Y. An analysis of the proximity of maxillary posterior teeth to the maxillary sinus using cone-beam computed tomography. J Endod. 2016;42(3):371–377. doi: 10.1016/j.joen.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 14.Matsuda H, Borzabadi-Farahani A, Le BT. Three-dimensional alveolar bone anatomy of the maxillary first molars: A cone-beam computed tomography study with implications for immediate implant placement. Implant Dent. 2016;25(3):367–372. doi: 10.1097/ID.0000000000000430. [DOI] [PubMed] [Google Scholar]
- 15.Demircan S, Çankaya AB. Is immediate implant placement possible in the maxillary molar area? An anatomical study. Quintessence Int. 2016;47(10):853–859. doi: 10.3290/j.qi.a36886. [DOI] [PubMed] [Google Scholar]
- 16.Jung YH, Cho BH. Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography. Imaging Sci Dent. 2012;42(4):219–224. doi: 10.5624/isd.2012.42.4.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choi YJ, Kim YH, Han SS, Jung UW Jung UW, Lee C, Lee A. et al. Alveolar bone height according to the anatomical relationship between the maxillary molar and sinus. J Periodontal Implant Sci. 2020;50(1):38–47. doi: 10.5051/jpis.2020.50.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deporter D, Ketabi M. Guidelines for Optimizing Outcomes with Immediate Molar Implant Placement. J Adv Periodontol Implant Dent. 2017;9(2):37–44. doi: 10.15171/JPID.2017.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Block MS. Placement of implants into fresh molar sites: Results of 35 cases. J Oral Maxillofac Surg. 2011;69(1):170–174. doi: 10.1016/j.joms.2010.07.040. [DOI] [PubMed] [Google Scholar]
- 20.Smith RB, Tarnow DP, Sarnachiaro G. Immediate Placement of Dental Implants in Molar Extraction Sockets: An 11-Year Retrospective Analysis. Compend Contin Educ Dent. 2019;40(3):166–170. [PubMed] [Google Scholar]
- 21.Zill A, Precht C, Beck-Broichsitter B, Sehner S, Smeets R, Heiland M. et al. Implants inserted with graftless osteotome sinus floor elevation - A 5-year post-loading retrospective study. Eur J Oral Implantol. 2016;9(3):277–289. [PubMed] [Google Scholar]
- 22.Peñarrocha-Oltra D, Demarchi CL, Maestre-Ferrín L, Peñarrocha-Diago M, Peñarrocha-Diago M. Comparison of immediate and delayed implants in the maxillary molar region: A retrospective study of 123 implants. Int J Oral Maxillofac Implant. 2012;27(3):604–610. [PubMed] [Google Scholar]
- 23.Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res. 2006;17(Suppl 2):35–51. doi: 10.1111/j.1600-0501.2006.01349.x. [DOI] [PubMed] [Google Scholar]


