Abstract
The early months of the COVID-19 pandemic saw significant increases in symptoms of anxiety and depression, particularly among college students. However, research has not examined how internalizing symptoms in this population have changed as the pandemic has continued into its second year. Further, there has yet to be an examination of potential changes in transdiagnostic vulnerability factors. Therefore, the purpose of the current repeated cross-sectional study was to examine differences by term in undergraduates’ symptoms of depression, anxiety, worry, social anxiety, and anxiety sensitivity in the Spring 2020 (n = 251), Fall 2020 (n = 427), and Spring 2021 (n = 256) semesters. Results indicated that there were significant increases in depression, anxiety, worry, and anxiety sensitivity from Spring 2020 to Fall 2020 that were maintained through the Spring 2021 semester, and levels of social anxiety were significantly higher in Spring 2021 compared to Spring 2020. These findings suggest that the mental health impacts of the COVID-19 pandemic on college students have continued beyond the initial months, and colleges and universities will need to develop comprehensive plans to adequately address college students’ mental health needs.
Keywords: Anxiety, Anxiety sensitivity, College students, COVID-19, Depression
In early 2020, a novel coronavirus, SARS-CoV-2, quickly spread from an isolated outbreak in China to a global pandemic creating massive disruptions in everyday life. These sudden, drastic changes resulted in a host of significant and interrelated stressors, including fear and uncertainty about the virus, loss of loved ones, social isolation, economic uncertainty, and increased caregiving demands. Not surprisingly, given the link between stress and psychopathology, studies conducted in the first several months of the pandemic showed an exponential increase in stress and psychological distress as well as symptoms of depression, anxiety, and posttraumatic stress disorder (PTSD; Czeisler et al., 2020; Xiong et al., 2020). For example, in late April 2020 adults in the United States (U.S.) were three times more likely than in 2018 to meet criteria for moderate or serious mental distress (70.4% vs. 22.0%; Twenge & Joiner, 2020). These and other similarly startling statistics led the American Psychological Association (2020) to warn of an impending mental health crisis in the U.S. with the potential for significant long-term effects.
Although the negative impacts of the pandemic have touched everyone, college students have been disproportionately affected. Not only did they experience educational disruptions (e.g., rapid transition to online learning, challenges with access to technology), but also social network disruptions, housing disruptions when campuses shut down, and financial strains due to job loss or reduced work hours because of stay-at-home orders. These stressors occurred (and continue to occur) against a backdrop of significant pre-existing vulnerability to psychopathology in this age group. The average age of onset for many psychological disorders occurs within this developmental period (American Psychiatric Association, 2013). Moreover, even prior to the pandemic, rates of psychopathology, particularly anxiety, depression, and substance use, had been increasing among college students (Holm-Hadulla & Koutsoukou-Argyraki, 2015; Lipson et al., 2019).
Thus, college students are likely a particularly vulnerable population for experiencing pandemic-related increases in psychopathology. Indeed, work conducted during the early months of the pandemic indicated that, compared to older adults, younger adults experienced worse mental health outcomes, including increased rates of anxiety, depression, trauma and stressor-related disorders, substance use, and suicidal ideation (Czeisler et al., 2020; Twenge & Joiner, 2020; Zhou et al., 2020). Among college students, specifically, there are similar trends (Fu et al., 2021; Rodriguez-Hidalgo et al., 2020). As one illustrative example, Liu et al. (2020) found rates of depression were nearly seven times higher, rates of anxiety twice as high, and rates of PTSD symptoms were as high or higher compared to studies of college students conducted prior to the pandemic.
Further, an emerging body of work suggests that anxiety sensitivity, a well-established risk factor for internalizing psychopathology indexing a fear of arousal-related sensations (Reiss et al., 1986; Schmidt et al., 2006), may be particularly relevant to understanding the COVID-19 pandemic’s effects on mental health. Indeed, work conducted early in the pandemic found that greater anxiety sensitivity was associated with greater anxiety, depression, suicidal ideation, and COVID-19-related distress, disability, and safety behaviors (e.g., stockpiling, cleaning; Allan et al., 2021; Rogers et al., 2021; Saulnier et al., 2021; Schmidt et al., 2021; Warren et al., 2021). Anxiety sensitivity also moderates the relationship between COVID-19-related stress and anxiety and functional impairment (Manning et al., 2021). Moreover, prospective work has found significant associations between anxiety sensitivity and greater depression and COVID-19-related fear and worry one month later (Paluszek et al., 2021; Schmidt et al., 2021). While anxiety sensitivity is conceptualized as a trait-like characteristic and has demonstrated stability over two years (Hovenkamp-Hermelink et al., 2019), the prolonged stress associated with the unprecedented nature and duration of the pandemic may have increased anxiety sensitivity levels. Thus, additional work to further examine the long-term impacts of the pandemic is warranted.
Unfortunately, in addition to the enormous impacts on daily life, the pandemic also has been unprecedented in its duration. However, most studies examining the pandemic’s impact on college student mental health were conducted during the early stages of the pandemic (i.e., March-June 2020), and data on the long-term impacts of the pandemic are just beginning to emerge. These newer data suggest that after initial increases in March 2020, psychological distress had largely decreased by July 2020 in both the U.S. and England (Daly & Robinson, 2021; Fancourt et al., 2021; Pierce et al., 2021), and most individuals had returned to their pre-pandemic levels of mental health by October 2020 (Pierce et al., 2021). On the other hand, Tanaka and Okamoto (2021) found that suicide rates in Japan decreased from February to June 2020 and increased from July to October 2020 during their second wave of the pandemic. To our knowledge, no published studies have examined symptom change beyond October 2020. Additionally, most studies have focused on broad symptom categories (e.g., anxiety) or general psychological distress. As a result, little is known about the pattern of changes in symptoms of specific disorders over the course of the pandemic so far. Moreover, given the importance of anxiety sensitivity in understanding mental health outcomes during the COVID-19 pandemic, it will be important to determine whether there have been significant changes in anxiety sensitivity as well.
Therefore, the purpose of the current study was to examine changes in internalizing symptoms and anxiety sensitivity among college students over the course of the COVID-19 pandemic’s first year. Specifically, we examined differences in symptoms of depression, anxiety, worry, social anxiety, and anxiety sensitivity between the Spring 2020, Fall 2020, and Spring 2021 semesters. Based on research showing that greater COVID-19 related stress is associated with greater symptoms of anxiety and depressive disorders (Gallagher et al., 2020), it was expected that symptoms of anxiety and depression and levels of anxiety sensitivity would be higher in the Fall 2020 semester compared to the Spring 2020 semester. Specific hypotheses were not generated for the Spring 2021 semester. Although the development of effective vaccines for COVID-19 could have resulted in a decrease in symptoms, the vaccine was not widely available until the end of the spring semester and pandemic fatigue could have instead resulted in further increases in symptomatology.
Method
Participants
The sample consisted of 934 undergraduates (Mage = 20.38, SD = 3.59); 72.4% identified as female, 26.0% as male, 0.9% as non-binary, 0.5% as transgender, and 0.2% did not specify. In terms of racial and ethnic background, 7.5% reported Hispanic ethnicity, 69.3% identified as White, 14.7% as Black or African American, 7.2% as multiracial, 5.9% as Asian, 0.2% as American Indian or Alaska Native, 0.1% as Native Hawaiian or Pacific Islander, 2.2% as Other, and 0.4% did not specify. We divided participants into three groups based on when the survey was completed: (1) March–May 2020 (Spring 2020; n = 251; modal completion date = April 17, 2020), (2) September-December 2020 (Fall 2020; n = 427; modal completion date = November 16, 2020), and (3) January-April 2021 (Spring 2021; n = 256; modal completion date = April 19, 2021). A breakdown of demographic information by group is presented in Table 1. The groups did not significantly differ in terms of age, gender identity, race, or ethnicity.
Table 1.
Sample Demographic Information by Semester
|
Spring 2020 n = 251 |
Fall 2020 n = 427 |
Spring 2021 n = 256 |
|
|---|---|---|---|
| Age [M (SD)] | 20.52 (3.63) | 20.49 (4.05) | 20.08 (2.62) |
| Gender [% (n)] | |||
| Female | 73.3 (184) | 69.1 (295) | 77.0 (197) |
| Male | 25.1 (63) | 29.0 (124) | 21.9 (56) |
| Non-Binary | 0.8 (2) | 0.9 (4) | 0.8 (2) |
| Transgender | 0.4 (1) | 0.7 (3) | 0.4 (1) |
| Other | 0.4 (1) | 0.2 (1) | 0.0 (0) |
| Race [% (n)] | |||
| White | 66.5 (167) | 71.2 (304) | 68.8 (176) |
| Black/African American | 19.1 (48) | 13.3 (57) | 12.5 (32) |
| Asian | 5.2 (13) | 4.7 (20) | 8.6 (22) |
| Multi-racial | 4.0 (10) | 8.0 (34) | 9.0 (23) |
| American Indian or Alaska Native | 0.0 (0) | 0.5 (2) | 0.0 (0) |
| Native Hawaiian or Pacific Islander | 0.0 (0) | 0.2 (1) | 0.0 (0) |
| Other | 5.2 (13) | 2.1 (9) | 1.2 (3) |
| Ethnicity [% Hispanic (n)] | 7.2 (18) | 6.3 (27) | 9.8 (25) |
The groups did not significantly differ on any demographic variables
Measures
Demographic Questionnaire
Participants provided general demographic information (i.e., age, gender identity, race, and ethnicity).
Overall Anxiety Severity and Impairment Scale (OASIS)
The OASIS is a five-item self-report measure that assesses the frequency and severity of anxiety symptoms as well as functional impairment related to anxiety (Norman et al., 2006). Items are rated on a 0 (none) to 4 (constant or extreme) Likert-type scale. Items are summed to create a total score with higher scores indicating greater anxiety. The OASIS demonstrates excellent test–retest reliability, convergent and discriminant validity, and the ability to discriminate between individuals with and without anxiety disorders (Bragdon et al., 2016; Campbell-Sills et al., 2009; Norman et al., 2006). It also has been found to reliably detect clinical symptom change among individuals seeking treatment for anxiety disorders (Moore et al., 2015). Internal consistency for the OASIS in the current sample was excellent (α = .91).
Overall Depression Severity and Impairment Scale (ODSIS)
The ODSIS is a five-item self-report measure that assesses the frequency and intensity of depressive symptoms as well as functional impairment related to depression (Bentley et al., 2014). Items are rated on a 0 (none) to 4 (constant or extreme) Likert-type scale. Items are summed to create a total score with higher scores indicating greater depression. Research indicates that the ODSIS possesses good internal consistency, convergent and discriminant validity, and the ability to reliably discriminate between individuals with and without a mood disorder (Bentley et al., 2014; Ito et al., 2015). Internal consistency for the ODSIS in the current sample was excellent (α = .96).
Ultra-Brief Penn State Worry Questionnaire (PSWQ-3)
The PSWQ-3 (Berle et al., 2011) is a three-item self-report measure that assesses three key aspects of pathological worry: high frequency, uncontrollability, and worry across multiple domains. The PSWQ-3 is a shortened version of the Penn State Worry Questionnaire (PSWQ), a 16-item measure considered to be the gold standard assessment tool for worry (Meyer et al., 1990). Items are rated on a 1 (not at all typical of me) to 5 (very typical of me) scale. Items are summed to create a total score with higher scores indicating greater worry. The psychometric properties of the PSWQ-3 are comparable to the longer PSWQ (Berle et al., 2011; Kertz et al., 2014). The PSWQ-3 demonstrated excellent internal consistency in the current sample (α = .91).
Short Form Social Interaction Anxiety Scale (SIAS-6) and Social Phobia Scale (SPS-6)
The SIAS-6 and the SPS-6 are six-item self-report measures designed to assess two aspects of social anxiety: social scrutiny fears and anxiety regarding social interactions (Peters et al., 2012). The SIAS-6 and the SPS-6 are shortened versions of the 20-item SIAS and the 20-item SPS, respectively (Mattick & Clarke, 1998). Items for both measures are rated on a 5-point scale ranging from 0 (not at all characteristic of me) to 4 (extremely characteristic of me). Items are summed to create a total score with higher scores indicating greater social anxiety. Research indicates that scores on the briefer versions correlate with those of the longer, original versions and possess good convergent and discriminant validity (Carleton et al., 2014; Le Blanc et al., 2014; Peters et al., 2012). Scores on the SIAS-6 and SPS 6 can also discriminate between those with and without a diagnosis of social anxiety disorder and are sensitive to treatment-related symptom change (Peters et al., 2012). Internal consistency in the current sample was good for both scales (SIAS-6 = .89, SPS-6 = .87).
Short Scale Anxiety Sensitivity Index (SSASI)
The SSASI is a five-item self-report measure that assesses the degree to which individuals fear the negative consequences associated with anxiety symptoms (Zvolensky et al., 2018). It is a shortened version of the Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007). Similar to the ASI-3, items are rated on a 0 (very little) to 4 (very much) scale. Items are summed to create a total score with higher scores indicating greater anxiety sensitivity. Results from the initial validation study indicate that scores on the SSASI strongly correlate with scores on the ASI-3, and that the SSASI possesses good internal consistency and excellent convergent and discriminant validity (Zvolensky et al., 2018). The SSASI demonstrated good internal consistency in the current sample (α = .85).
Procedure
Data were collected between March 2020 and April 2021 as part of a larger survey on college student health. Undergraduate students at a large public university who were over the age of 18 were invited to participate in the study. Interested students signed up for the study using Sona Systems research participant pool management software, which provided students with a link to complete study measures online and ensured that students did not complete the study multiple times. We collected and managed study data using REDCap (Research Electronic Data Capture; Harris et al., 2009). To ensure anonymity, we did not collect information regarding participants’ IP addresses. Participants were granted course credit for their participation. The Institutional Review Board approved all study materials and procedures prior to data collection (IRB # 19.1013).
Data Analytic Plan
There were a total of 1502 survey responses. To ensure data quality, data were examined for correct responses to three quality control questions that were randomly distributed throughout the survey (e.g., “Choose option A for this question”) and an affirmative answer to the question “Have you carefully and accurately answered all the questions” at the end of the survey. As a result, data from 568 participants were removed (n = 96 did not answer quality control questions correctly, n = 472 had missing data for quality control questions and nearly all other survey questions). Data analyses were completed on the remaining 934 participants using SPSS version 27.
A multivariate analysis of variance (MANOVA) was conducted to evaluate differences between participants in Spring 2020, Fall 2020, and Spring 2021 in depression, anxiety, worry, and social anxiety. A univariate analysis of variance (ANOVA) was conducted to evaluate group differences in anxiety sensitivity. For significant univariate differences, post hoc pairwise comparisons were conducted to examine the specificity of group differences. Partial eta squared (ηp2) served as an index of effect size of mean differences (small = .01, medium = .09, large = .25; Richardson, 2011).
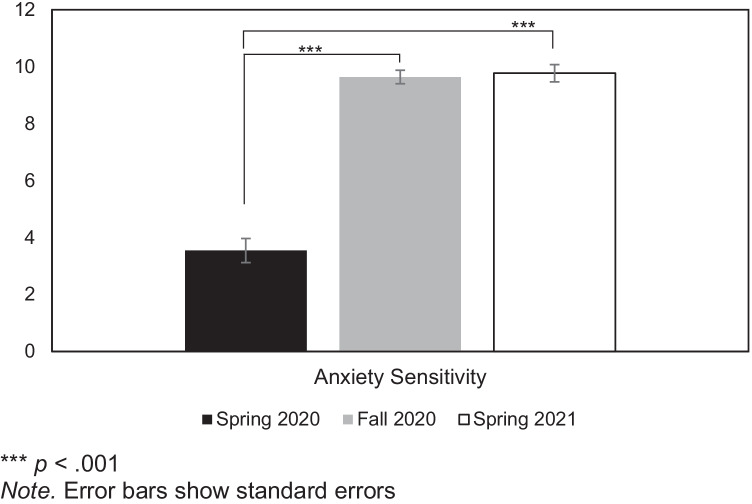
Results
Significant group differences emerged for internalizing symptoms [F (10,1800) = 3.94, p < .001, ηp2 = .02]. There were significant univariate differences for depression [F (2,903) = 5.02, p = .007, ηp2 = .011], anxiety [F (2,903) = 13.71, p < .001, ηp2 = .029], and worry [F (2,903) = 8.95, p < .001, ηp2 = .019]. Follow up post hoc comparisons used a Bonferroni correction to decrease the chance of Type I error. Based on this correction, the significance level was adjusted to .0125 (i.e., .05/4). Students in the Fall 2020 and Spring 2021 semesters reported significantly higher levels of depression, anxiety, and worry compared to students in Spring 2020 (see Table 2), while scores in Fall 2020 and Spring 2021 were not significantly different from one another. There were also significant univariate differences for social anxiety [F (2,903) = 4.44, p = .012, ηp2 = .01]. Students in Spring 2021 reported significantly higher levels of social interaction anxiety compared to students in Spring 2020; however, scores did not differ significantly between Fall 2020 and Spring 2020 or Spring 2021. There were no significant univariate differences for social phobia [F (2,903) = 2.44, p = .088, ηp2 = .005]. Results of the ANOVA for anxiety sensitivity also showed significant group differences [F(2,803) = 88.71, p < .001, ηp2 = .18]. Students in Fall 2020 and Spring 2021 reported significantly higher levels of anxiety sensitivity compared to students in Spring 2020 (see Fig. 1). No significant differences in anxiety sensitivity between Fall 2020 and Spring 2021 were found.
Table 2.
Group Differences in Internalizing Symptoms by Semester
|
Spring 2020 (1) M (SD) |
Fall 2020 (2) M (SD) |
Spring 2021 (3) M (SD) |
Group Differences | |
|---|---|---|---|---|
| Depression | 3.96 (4.69) | 5.14 (5.27) | 5.19 (5.01) | 2,3 > 1 |
| Anxiety | 5.37 (4.61) | 7.12 (4.76) | 7.26 (4.35) | 2,3 > 1 |
| Worry | 7.58 (3.74) | 8.76 (3.86) | 8.84 (3.82) | 2,3 > 1 |
| Social Phobia | 6.76 (6.04) | 7.47 (6.06) | 7.92 (5.56) | - |
| Social Anxiety | 8.75 (6.54) | 9.34 (6.28) | 10.41 (6.18) | 3 > 1 |
Depression: Overall Depression Severity and Impairment Scale (Bentley et al., 2014); Anxiety: Overall Anxiety Severity and Impairment Scale (Norman et al., 2006); Worry: Ultra-Brief Penn State Worry Questionnaire (Berle et al., 2011); Social Phobia: Short Form Social Phobia Scale (Peters et al., 2012); Social Anxiety: Short Form Social Interaction Anxiety Scale (Peters et al., 2012)
Fig. 1.
Estimated Marginal Means for Anxiety Sensitivity by Semester
Discussion
Given the prolonged and unprecedented nature of the COVID-19 pandemic, the current study was designed to examine changes in depression, anxiety, worry, social anxiety, and anxiety sensitivity among college students over a longer period of time than previous work using data from three independent samples. Results indicated that there were higher levels depression, anxiety, worry, and anxiety sensitivity among students sampled in the Fall 2020 and Spring 2021 semesters as compared to those sampled during Spring 2020. Although the effect sizes were small, the number of students who were above the clinical cut-offs for anxiety and depression were approximately 1.5 times higher in Fall 2020 (anxiety = 41.3%, depression = 27.5%) and Spring 2021 (anxiety = 41.3%, depression = 27.5%) compared to Spring 2020 (anxiety = 26.1%, depression = 18.8%). Although there were no significant changes in social scrutiny fears, anxiety regarding social interaction was significantly higher in Spring 2021 compared to Spring 2020. In Spring 2021, 64.9% of participants were above the clinical cutoff for anxiety regarding social interaction compared to 52.6% in Spring 2020. These rates are much higher than what has been found in other young adult samples (e.g., 40%; Jefferies & Ungar, 2020) suggesting that many students have been coping with clinically significant levels of social anxiety throughout the COVID-19 pandemic. Such high prevalence rates may also explain the small effect sizes.
These findings suggest that increases in anxiety and depression that were seen in the first few months of the pandemic (Fu et al., 2021; Liu et al., 2020; Rodriguez-Hidalgo et al., 2020) have been maintained over the course of the pandemic’s first year. Highly effective COVID-19 vaccines and the possibility of easing state and county restrictions do not appear to have improved mental health as symptom elevations remained relatively stable. For example, relaxing of public health measures (e.g., business capacity, restaurant and bar curfews, outdoor masking) was underway during mid-April 2021 when the majority of students were completing the measures for the Spring 2021 data collection. In fact, the findings for social interaction anxiety would suggest that, after a significant period of social isolation and physical distancing, college students may be even more anxious about interacting with others. Such a perspective is supported by research demonstrating that social isolation is associated with higher levels of social anxiety among college students (Chow et al., 2017). Thus, it may be helpful for schools to provide supportive opportunities for social interactions, perhaps by scaling back large, campus-wide events and providing smaller, more structured events focused on building community as a way to ease students back into social activities.
Moreover, anxiety sensitivity levels, which tend to be fairly stable, also have increased over the course of the pandemic. The medium to large effect size of this finding indicates that these changes are robust and clinically significant. In fact, mean anxiety sensitivity scores in Fall 2020 (M = 9.64) and Spring 2021 (M = 9.77) were higher than the mean of a treatment-seeking sample used in the original validation study (M = 8.14; Zvolensky et al., 2018). Therefore, it appears that college students, an already vulnerable population, are experiencing further increases in risk for psychopathology. Although this study cannot determine causality, given the typical stability of anxiety sensitivity, it is likely that these significant changes are a result of the pandemic.
These findings point to a number of possible solutions to mitigate pandemic-related effects on students’ mental health. Institutions of higher learning might consider conducting universal mental health screenings in order to identify students most in need of services. Further, given the importance of anxiety sensitivity in COVID-related mental health outcomes as well as the current findings demonstrating significant increases in anxiety sensitivity, interventions targeting anxiety sensitivity may be particularly useful. For example, brief (30–45 min) one-session online interventions targeting anxiety sensitivity have been developed (Schmidt et al., 2007, 2014, 2017) that result in long-lasting reductions in anxiety sensitivity as well as anxiety and depression symptoms (Norr et al., 2017). Thus, they may be an effective way to quickly reach large numbers of students in order to prevent a pandemic-related mental health crisis.
However, several limitations to the current study warrant consideration. First, though the current study collected data at various timepoints, it was not a true longitudinal study that followed individuals over time. Therefore, we can only look at group rather than individual differences. Future work on the effects of the pandemic on college student mental health will benefit from utilizing true longitudinal designs in order to address this issue and enable us to look at causality and potential mediators of outcomes. In particular, future studies may build on the present work and examine anxiety sensitivity as a mediator of the changes in anxiety and depression symptoms during the COVID-19 pandemic. Second, the current study relied solely on self-report measures, which increases the possibility for shared method variance and reporting errors. Future studies could, therefore, incorporate a multimethod assessment approach, such as biological challenge paradigms (e.g., carbon dioxide-enriched air inhalation) or social interaction tasks. Finally, the current sample was primarily female and white, potentially limiting the generalizability of these results. Future studies would benefit from using more demographically diverse samples that would allow for an investigation of potential differential effects.
Despite these limitations, the current study suggests that the mental health of college students has suffered during the pandemic, particularly in terms of depression, anxiety, worry, and anxiety regarding social interactions. Moreover, there were significant increases in anxiety sensitivity, a well-established risk factor for psychopathology. Although additional research is needed, given that the pandemic continues, these findings suggest that colleges and universities will need to develop comprehensive plans to adequately address college students’ mental health needs during the current pandemic as well as in future, large-scale stressors.
Funding
There is no funding associated with this study.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Conflict of Interest
Alison C. McLeish, Kandi L. Walker, and Joy L. Hart declare that there is no conflict of interest.
Experiment Participants
The questionnaire and methodology for this study was approved by the Human Research Ethics committee of the University of Louisville (Ethics approval number: 19.1013).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Allan NP, Volarov M, Koscinski B, Pizzonia KL, Potter K, Accorso C, Saulnier KG, Ashrafioun L, Stecker T, Suhr J, Allan DM. Lonely, anxious, and uncertain: Critical risk factors for suicidal desire during the COVID-19 pandemic. Psychiatry Research. 2021;304:114144. doi: 10.1016/j.psychres.2021.114144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596
- American Psychological Association. (2020). Stress in America 2020: a national mental health crisis.https://www.apa.org/news/press/releases/stress/2020/report-october
- Bentley KH, Gallagher MW, Carl JR, Barlow DH. Development and validation of the Overall Depression Severity and Impairment Scale. Psychological Assessment. 2014;26:815–830. doi: 10.1037/a0036216. [DOI] [PubMed] [Google Scholar]
- Berle D, Starcevic V, Moses K, Hannan A, Millcevic D, Sammut P. Preliminary validation of an ultra-brief version of the Penn State Worry Questionnaire. Clinical Psychology and Psychotherapy. 2011;18:339–346. doi: 10.1002/cpp.724. [DOI] [PubMed] [Google Scholar]
- Bragdon LB, Diefenbach GJ, Hannan S, Tolin DF. Psychometric properties of the Overall Anxiety Severity and Impairment Scale (OASIS) among psychiatric outpatients. Journal of Affective Disorders. 2016;201:112–115. doi: 10.1016/j.jad.2016.05.005. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Norman SB, Craske MG, Greer S, Lang AJ, Chavira DA, Bystritsky A, Sherbourne C, Roy-Byrne P, Stein MB. Validation of a brief measure of anxiety-related severity and impairment: the Overall Anxiety Severity and Impairment Scale (OASIS) Journal of Affective Disorders. 2009;112:92–101. doi: 10.1016/j.jad.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton RN, Thibodeau MA, Weeks JW, Teale Sapach MJN, McEvoy PM, Horswill SG, Heimberg RG. Comparing short forms of the Social Interaction Anxiety Scale and the Social Phobia Scale. Psychological Assessment. 2014;26(4):116–1126. doi: 10.1037/a0037063. [DOI] [PubMed] [Google Scholar]
- Chow, P. I., Fua, K., Huang, Y., Bonelli, W., Xiong, H., Barnes, L. E., & Teachman, B. A. (2017). Using mobile sensing to test clinical models of depression, social anxiety, state affect, and social isolation among college students. Journal of Medical Internet Research, 19(3), e62. 10.2196/jmir.6820 [DOI] [PMC free article] [PubMed]
- Czeisler, M. E., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., Weaver, M. D., Robbins, R., Facer-Childs, E. R., Barger, L. K., Czeisler, C. A., Howard, M. E., & Rajaratnam, S. M. W. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic- United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69, 1049–1057. 10.15585/mmwr.mm6932a1 external icon [DOI] [PMC free article] [PubMed]
- Daly M, Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. Journal of Psychiatric Research. 2021;136:603–609. doi: 10.1016/j.jpsychires.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu W, Yan S, Zong Q, Anderson-Luxford D, Song X, Lv Z, Lv C. Mental health of college students during the COVID-19 epidemic in China. Journal of Affective Disorders. 2021;280:7–10. doi: 10.1016/j.jad.2020.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher MW, Zvolensky MJ, Long LJ, Rogers AH, Garey L. The impacts of Covid-19 experiences and associated stress on anxiety, depression, and functional impairment in American Adults. Cognitive Therapy and Research. 2020;44:1043–1051. doi: 10.1007/s10608-020-10143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm-Hadulla RM, Koutsoukou-Argyraki A. Mental health of students in a globalized world: Prevalence of complaints and disorders, methods and effectivity of counseling, structure of mental health services for students. Mental Health & Prevention. 2015;3(1–2):1–4. doi: 10.1016/j.mhp.2015.04.003. [DOI] [Google Scholar]
- Hovenkamp-Hermelink JHM, van der Veen DC, Oude Voshaar RC, Batelaan NM, Penninx BWJH, Jeronimus BF, Schoevers RA, Riese H. Anxiety sensitivity, its stability and longitudinal associations with severity of anxiety symptoms. Scientific Reports. 2019;9:4314. doi: 10.1038/s41598-019-39931-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito M, Bentley KH, Oe Y, Nakajima S, Fujisato H, Miyamae M, Kanie A, Horikoshi M, Barlow DH. Assessing depression related severity and functional impairment: the Overall Depression Severity and Impairment Scale (ODSIS) PLoS One. 2015;10(4):e0122969. doi: 10.1371/journal.pone.0122969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferies P, Ungar M. Social anxiety in young people: a prevalence study in seven countries. PLoS One. 2020;15(9):e0239133. doi: 10.1371/journal.pone.0239133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertz SJ, Lee J, Björgvinsson T. Psychometric properties of abbreviated and ultra-brief versions of the Penn State Worry Questionnaire. Psychological Assessment. 2014;26(4):1146–1154. doi: 10.1037/a0037251. [DOI] [PubMed] [Google Scholar]
- Le Blanc AL, Bruce LC, Heimberg RG, Hope DA, Blancom C, Schneier FR, Liebowitz MR. Evaluation of the psychometric properties of two short forms of the Social Interaction Anxiety Scale and the Social Phobia Scale. Assessment. 2014;21(3):312–323. doi: 10.1177/1073191114521279. [DOI] [PubMed] [Google Scholar]
- Lipson SK, Lattie EG, Eisenberg D. Increased rates of mental health service utilization by U.S. college students: 10-year population-level trends (2007–2017) Psychiatric Services. 2019;70:60–63. doi: 10.1176/appi.ps.201800332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S., & Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290, 113172. 10.1016/j.psychres.2020.113172 [DOI] [PMC free article] [PubMed]
- Manning K, Eades ND, Kauffman BY, Long LJ, Richardson AL, Garey L, Zvolensky MJ, Gallagher MW. Anxiety sensitivity moderates the impact of COVID-19 perceived stress on anxiety and functional impairment. Cognitive Therapy and Research. 2021;45:689–696. doi: 10.1007/s10608-021-10207-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/S0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Moore SA, Welch SS, Michonski J, Poquiz J, Osborne TL, Sayrs J, Spanos A. Psychometric evaluation of the Overall Anxiety Severity and Impairment Scale (OASIS) in individuals seeking outpatient specialty treatment for anxiety-related disorders. Journal of Affective Disorders. 2015;175:463–470. doi: 10.1016/j.jad.2015.01.041. [DOI] [PubMed] [Google Scholar]
- Norman SB, Cissell SH, Means-Christensen AJ, Stein MB. Development and validation of an Overall Anxiety Severity and Impairment Scale (OASIS) Depression and Anxiety. 2006;23:245–249. doi: 10.1002/da.20182. [DOI] [PubMed] [Google Scholar]
- Norr AM, Gibby BA, Schmidt NB. Is computerized psychoeducation sufficient to reduce anxiety sensitivity in an at-risk sample?: A randomized trial. Journal of Affective Disorders. 2017;212:48–55. doi: 10.1016/j.jad.2017.01.032. [DOI] [PubMed] [Google Scholar]
- Paluszek MM, Asmundson AJN, Landry CA, McKay D, Taylor S, Asmundson GJG. Effects of anxiety sensitivity, disgust, and intolerance of uncertainty on the COVID stress syndrome: a longitudinal assessment of transdiagnostic constructs and the behavioural immune system. Cognitive Behaviour Therapy. 2021;50(3):191–203. doi: 10.1080/16506073.2021.1877339. [DOI] [PubMed] [Google Scholar]
- Peters L, Sunderland M, Andrews G, Rapee RM, Mattick RP. Development of a short form Social Interaction Anxiety (SIAS) and Social Phobia Scale (SPS) using nonparametric item response theory: the SIAS-6 and the SPS-6. Psychological Assessment. 2012;24(1):66–76. doi: 10.1037/a0024544. [DOI] [PubMed] [Google Scholar]
- Pierce M, McManus S, Hope H, Hotopf M, Ford T, Hatch SL, John A, Kontopantelis E, Webb RT, Wessely S, Abel KM. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. The Lancet. 2021;8(7):610–619. doi: 10.1016/S2215-0366(21)00151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency, and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24(1):1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Richardson JTE. Eta squared and partial eta squared as measures of effect size in educational research. Educational Research Review. 2011;6(2):135–147. doi: 10.1016/j.edurev.2010.12.001. [DOI] [Google Scholar]
- Rodriguez-Hidalgo, A. J., Pantaleon, Y., Dios, I., & Falla, D. (2020). Fear of COVID-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Frontiers in Psychology, 11, 591797. 10.3389/fpsyg.2020.591797 [DOI] [PMC free article] [PubMed]
- Rogers AH, Bogiaizian D, Salazar PL, Solari A, Garey L, Fogle BM, Schmidt NB, Zvolensky MJ. COVID-19 and anxiety sensitivity across two studies in Argentina: Associations with COVID-19 worry, symptom severity, anxiety, and functional impairment. Cognitive Therapy and Research. 2021;45:697–707. doi: 10.1007/s10608-020-10194-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saulnier KG, Koscinski B, Volarov M, Accorso C, Austin MJ, Suhr JA, Allan D, Allan N. Anxiety sensitivity and intolerance of uncertainty are unique and interactive risk factors for COVID-19 safety behaviors and worries. Cognitive Behaviour Therapy. 2021 doi: 10.1080/16506073.2021.1976819. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, Allan NP. Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. Journal of Consulting and Clinical Psychology. 2014;82(6):1023–1033. doi: 10.1037/a0036651. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey JA. Anxiety Sensitivity Amelioration Training (ASAT): a longitudinal primary prevention program targeting cognitive vulnerability. Journal of Anxiety Disorders. 2007;21(3):302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Morabito DM, Mathes BM, Martin A. Anxiety sensitivity prospectively predicts pandemic-related distress. Journal of Affective Disorders. 2021;292:660–666. doi: 10.1016/j.jad.2021.05.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Norr AM, Allan NP, Raines AM, Capron DW. A randomized clinical trial targeting anxiety sensitivity for patients with suicidal ideation. Journal of Consulting and Clinical Psychology. 2017;85(6):596–610. doi: 10.1037/ccp0000195. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. Journal of Psychiatric Research. 2006;40(8):691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Tanaka, T., & Okamoto, S. (2021). Increase in suicide following an initial decline during the COVIVD-19 pandemic in Japan. Nature Human Behaviour, 5, 229–238. 10.1038/s41562-020-01042-z [DOI] [PubMed]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Abramowitz JS, Holaway RM, Sandin B, Stewart SH, Coles M, Eng W, Daly ES, Arrindell WA, Bouvard M, Cardenas SJ. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Joiner TE. Mental distress among U.S. adults during the COVID-19 pandemic. Journal of Clinical Psychology. 2020;76:2170–2182. doi: 10.1002/jclp.23064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren, A. M., Zolfaghari, K., Fresnedo, M., Bennett, M., Pogue, J., Waddimba, A., Zvolensky, M. J., Carlbring, P., & Powers, M. B. (2021). Anxiety sensitivity, COVID-19 fear, and mental health: Results from a United States population sample. Cognitive Behaviour Therapy, 50(3), 204–216. 10.1080/16506073.2021.1874505 [DOI] [PubMed]
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y, MacGeorge EL, Myrick JG. Mental health and its predictors during the early months of the COVID-19 pandemic experience in the United States. International Journal of Environmental Research and Public Health. 2020;17(17):6315. doi: 10.3390/ijerph17176315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Garey L, Fergus TA, Gallagher MW, Viana AG, Shepherd JM, Mayorga NA, Kelley LP, Griggs JO, Schmidt NB. Refinement of anxiety sensitivity measurement: the Short Scale Anxiety Sensitivity Index. Psychiatry Research. 2018;269:549–557. doi: 10.1016/j.psychres.2018.08.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.