Abstract
Objectives
Consumption of the drug khat is high across East Africa and the South-Western Arabian Peninsula despite evidence for its adverse psychiatric effects. This systematic review aims to explore cross-sectional research in the field to determine the strength of the association between khat use and psychiatric symptoms
Methods
Six databases were searched in October 2021—Ovid Medline, Embase, APA PsycINFO, CINAHL, Scopus and Proquest—using the following search terms: “khat” OR “qat” OR “qaad” OR “catha” OR “miraa” OR “mairungi” AND “depression” OR “anxiety” OR “mania” OR “psych*” OR “schiz*” OR “mental” OR “hallucinations” OR “delusions” OR “bipolar”. Eligible studies were cross-sectional studies of any population or setting comparing the prevalence of psychiatric symptoms in long term or dependent khat users with non-users. The quality of each study was appraised by the Newcastle-Ottawa scale. A meta-analysis was planned using a random effects model to produce an OR with 95% CIs—using the Mantel-Haenszel method—alongside an I2 statistic to represent heterogeneity. The quality of this meta-analysis was appraised using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) scoring system.
Results
35 studies were eligible for inclusion (total participants=31 893), spanning 5 countries (Ethiopia, Somalia, Kenya, Saudi Arabia, UK). Meta-analysis suggests that khat use is associated with an 122% increased prevalence of psychiatric symptoms (OR 2.22, 95% CIs 1.76 to 2.79, p<0.00001, GRADE score: ‘very low’).
Conclusions
The high heterogeneity of the meta-analysis is likely due to the wide variation between the studies within the evidence base. To perform a more accurate systematic review, further primary studies are needed with standardised measurements of variables, particularly khat consumption.
PROSPERO registration number
CRD42020224510.
Keywords: psychiatry, mental health, substance misuse, public health, adult psychiatry
Strengths and limitations of this study.
Follows all guidelines listed in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 Checklist for systematic reviews.
Searches published and unpublished literature using search terms that include all commonly-used variations of ‘khat’ from around the world.
Includes both dependent and non-dependent khat use due to poor definitions of khat usage in primary research studies.
Includes both psychiatric symptoms and psychiatric disorders.
Introduction
The stimulant drug khat consists of the buds and leaves of the plant Catha edulis, an evergreen shrub highly prevalent in East Africa and the South-Western Arabian Peninsula.1 2 Ethiopia is the world’s largest exporter of khat, however, its consumption is highest in Yemen where up to 90% of adult males and 50% of adult females chew khat for 3–4 hours per day.3–5 Within its local regions, khat chewing has been a cultural tradition for many generations and is thought to increase sociability, concentration, energy and spirituality.2 6 7
Psychiatric symptoms have been recognised as a consequence of khat use for several decades.8 9 Milder psychological consequences related to its use include anxiety, restlessness, insomnia and dysphoric mood, all of which can reduce quality of life.2 8–11 More severe psychological harms associated with its use include psychosis and depression, which in some cases have resulted in acts of suicide and homocide.8–11 Users most at risk of these sequelae are those abusing larger amounts of khat—some studies have provided evidence for a dose-dependent relationship—and those with pre-existing psychiatric disorders.8–10
The evidence base exploring the association between khat use and psychiatric symptoms—which consists mostly of cross-sectional studies—is currently small and insufficient.12 Studies often vary in terms of populations and regions studied, measurement of khat use, symptoms explored and quality of methodology. Hence, results can be inconsistent, making it difficult for academics, policy-makers and the public to understand the psychiatric risks of khat consumption. This systematic review aims to investigate the strength of the association between khat use and psychiatric symptoms by collating the evidence we have so far, in order to guide further research in the field and to evaluate the need for any potential interventions for khat users, for example, increased education about potential psychiatric side effects.
Methods
The protocol for this systematic review can be found on Prospero, with registration number CRD42020224510.13 Originally, this systematic review had two objectives: to investigate the strength of the association between khat use and psychiatric symptoms, and secondly to investigate the role of trauma within this relationship. Due to the vast amount of literature in the field, the second objective was removed from the protocol to ensure that the findings would be suitable for one single review. It is recommended that a follow-up review should be conducted exploring the role of trauma.
This review followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines at all times.14
Patient and public involvement
No members of the public or patients were involved in the design of this systematic review.
Literature search
A literature search was carried out independently by authors BE and NA in October 2021 using the following search terms:
“khat” OR “qat” OR “qaad” OR “catha” OR “miraa” OR “mairungi”
AND
“depression” OR “anxiety” OR “mania” OR “psych*” OR “schiz*” OR “mental” OR “hallucinations” OR “delusions” OR “bipolar”
These search terms encompassed all previously reported psychiatric symptoms associated with khat, and included all predominant cultural variations of the term ‘khat’ as identified by the Medical Subject Headings Thesaurus.15 Advice was provided by the library team at the University of Birmingham. Note that studies surrounding suicidality were excluded, as suicidality is often but not always associated with psychiatric dysfunction.16 Disagreements between the authors were discussed in person. Removal of duplicates was automated for the databases Ovid MEDLINE, Embase and APA PsycINFO, and was performed manually for the remaining databases.
Six electronic databases were searched. Five of these were databases of published literature: Ovid MEDLINE, Embase, APA PsycINFO, CINAHL and Scopus. Additionally, Proquest was searched to obtain any relevant grey or unpublished literature. The full search strategy for each database can be found in online supplemental material 1.
bmjopen-2022-061865supp001.pdf (43.8KB, pdf)
Study eligibility
The literature search used the following inclusion criteria:
Population: adults (aged 18+).
Exposure: long-term or dependent khat use.
Comparator: no khat use or non-dependent khat use*.
Outcome: prevalence of psychiatric symptoms in khat users and prevalence of psychiatric symptoms in non-users.
Study design: cross-sectional studies; note that mixed-method studies are considered eligible but only the cross-sectional data will be considered for the review.
Language: all.
Publication type: must be a complete study but no restriction on publication status.
Setting: all.
Date of publication: all.
Each potentially eligible study was compared with a checklist of the above criteria to determine whether or not it should be included within the review.
*Note that non-dependent khat use was only considered a suitable comparator for studies where the exposure group were dependent khat-users, where both dependence and non-dependence were validated by a recognised tool such as the Severity of Dependence Scale.
The literature search used the following exclusion criteria:
Population: children, animals.
Exposure: substance abuse other than khat.
Comparator: ‘substance users’ where khat use is not specifically described.
Outcome: neurobehavioural processes, withdrawal symptoms, suicide, substance use disorders.
Study design: any study design other than cross-sectional, for example, case control, randomised controlled trial, case report, review.
Language: no exclusion criteria.
Publication type: unfinished studies including abstract only, conference abstracts, letters, retracted articles, book chapters.
Setting: no exclusion criteria.
Data collection and quality assessment
A summary of findings table—see online supplemental material 2—was created to present the following study features: population, sample, criteria for ‘khat user’, psychiatric measure, effect estimate. In addition, the quality of each primary study (e.g., risk of bias due to inadequate reporting methods or missing data) was assessed using the Newcastle-Ottawa Scale (see online supplemental material 3).17 18 Data were collected manually by both authors independently, with any disagreements between the independent assessments resolved by discussion.
bmjopen-2022-061865supp002.pdf (90.9KB, pdf)
bmjopen-2022-061865supp003.pdf (85.5KB, pdf)
Synthesis of findings
The prevalence of khat-users and non-users with psychiatric symptoms from each study was entered into a meta-analysis using the software Revman, provided by the Cochrane organisation. After inputting all dichotomous values, this software created a forest plot of ORs, each with 95% CIs, using the Mantel-Haenszel method.19 A random effects model was used as this assumes that the outcome is normally distributed, hence attributing the differences between studies to both chance and genuine variation.19 An I2 statistic was given to indicate variability between studies, as this is again recommended by the Cochrane organisation.20
A subgroup analysis was also included, grouping studies investigating similar symptoms. An OR and I2 statistic was provided for each subgroup, as well as a χ2 test and p value for overall subgroup differences.
A sensitivity analysis was conducted to look for any studies that are prominent outliers. Each study was removed from the meta-analysis one at a time, and the OR, 95% CIs, I2 value and p value reported within a table.
The quality of the meta-analysis was evaluated using the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) framework.21
Results
Included and excluded studies
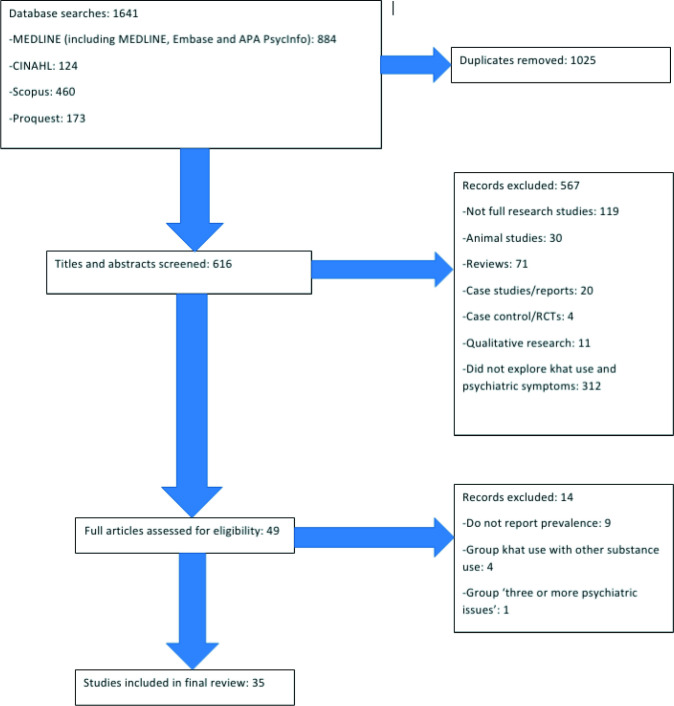
The PRISMA flow chart in figure 1 shows the number of studies included and excluded at each stage of the literature search.14 When searching the relevant databases, 1641 results were found that included the relevant terms within their title or abstract. After removing duplicates, this number was reduced to 616.
Figure 1.
PRISMA flow chart of included and excluded studies. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Each title and abstract were screened, and 567 results were removed for the following reasons:
One hundred and nineteen were not research studies, for example, these included conference abstracts, letters, and newspaper/magazine articles.
Thirty were animal studies.
Seventy-one were reviews, including systematic reviews and meta-analyses.
Twenty were case studies or case reports.
Four were case–control studies or randomised controlled trials.
Eleven were qualitative studies.
A total of 312 did not explore the relationship between khat use and psychiatric symptoms.
Forty-nine studies were read in full in order to determine their eligibility. Of these, 14 were excluded for the following reasons:
Nine explored both khat use and psychiatric symptoms but not their prevalence.22–30
Four did not report khat-use alone, and instead reported substance use or equivalent.31–34
One only reported the prevalence of khat use alongside ‘three or more psychiatric issues’.10
Thirty-five studies were included in the final review.7 35–68
Summary of included studies
The summary of findings table—online supplemental material 2—contains the effect estimates of each individual study, alongside each study’s characteristics (ie, target population, sample and methods of measuring khat use and psychiatric symptoms).
A subsequent table—online supplemental material 3—provides information regarding the quality of each primary study, assessed using the Newcastle-Ottawa Scale.17 18 According to Mekuriaw et al, a score of 5/10 indicates a medium-quality study while a score of 6/10 indicates a high-quality study.69 In this systematic review, the average quality score was 6.8, with a range of 4–8. No issues due to missing data arose.
Symptoms explored within included studies
The included studies explored a range of symptoms in association with khat usage. These have been grouped into the following subgroups:
Twelve studies explored symptoms of ‘depression’; this subgroup includes ‘depressive symptoms’, ‘feeling depressed’, diagnoses of depression, and the presence of ‘depressive episodes’ within the last month.
Six studies explored symptoms of‘ anxiety’; this subgroup includes ‘feeling anxious’, ‘obsession–compulsion’, ‘phobic anxiety’ and diagnoses of anxiety disorders.
Sixteen studies explored symptoms of ‘psychological distress’; this subgroup includes ‘psychological stress’, ‘psychological distress’, ‘mental distress’ and ‘stress’.
Six studies explored symptoms of psychotic disorders; this subgroup includes ‘psychotic symptoms’, ‘psychosis’, ‘paranoid ideation’, ‘psychoticism’ and diagnoses of ‘schizophrenia’.
One study explored psychopathy.
Five studies explored unspecified psychiatric symptoms and disorders; this subgroup includes 'common mental disorders’, ‘psychiatric dysfunction’, ‘mental illness’ and ‘mental problems that prevent employment or household tasks’.
No studies explored bipolar disorder or mania.
Meta-analysis
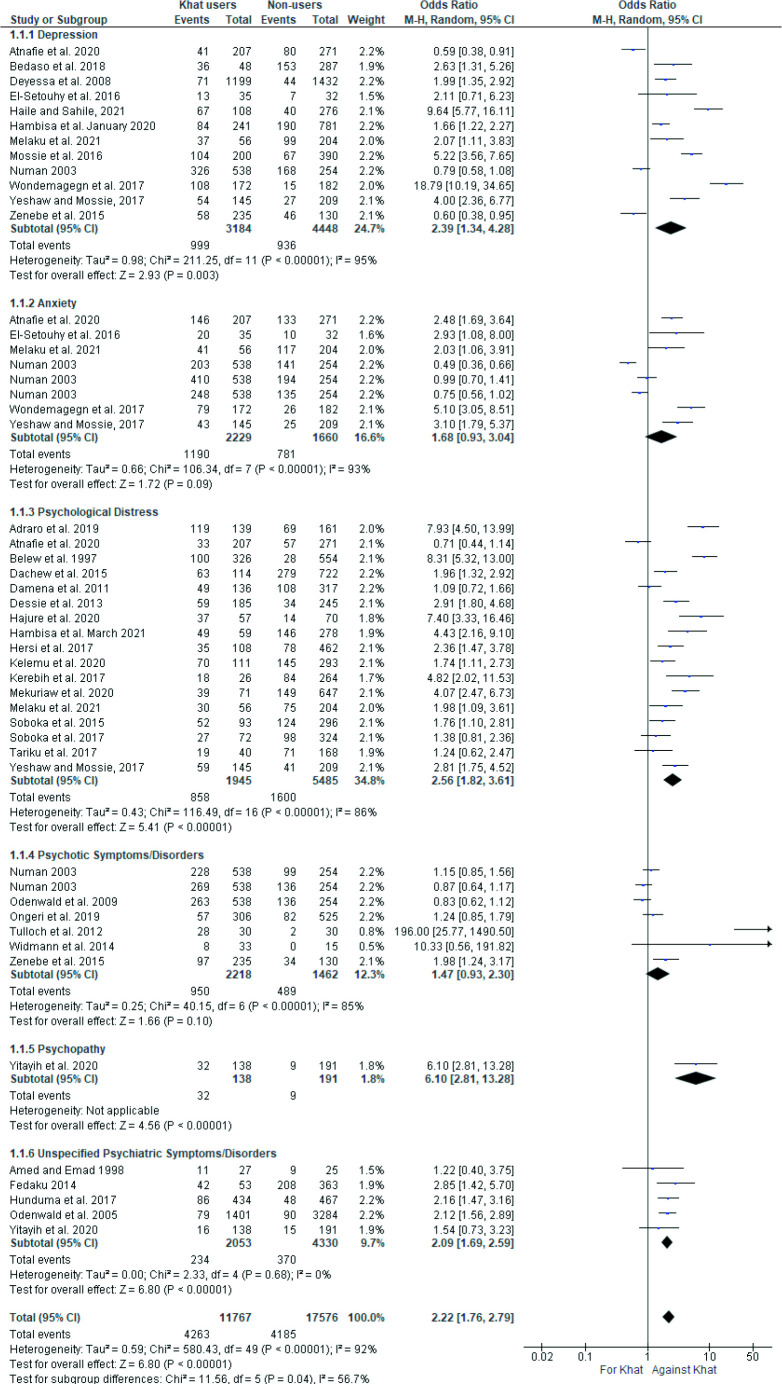
The meta-analysis of the 35 included studies can be seen in figure 2. This meta-analysis suggests that khat use is associated with an 122% increased prevalence of psychiatric symptoms (OR 2.22, 95% CIs 1.76 to 2.79, p<0.00001). All but one of the 35 studies were scored as at least medium or high-quality when assessed using the Newcastle-Ottawa Scale; the remaining study scored 4/10—where 5/10 is medium quality—and had a very small weighting within the meta-analysis of 1.5%. The heterogeneity of this meta-analysis is 92%, which is classified as high.20 21
Figure 2.
Meta-analysis of included studies. M-H, Mantel-Haenszel.
Subgroup analysis
The accompanying subgroup analysis—grouping studies investigating similar symptoms—shows that there is a statistically significant subgroup effect of p=0.04; usually, a p value of less than 0.1 is regarded as a statistically significant subgroup effect.70 This means that khat use has a varying association with the symptoms investigated.
The largest association found is between khat use and symptoms of psychological distress (OR 2.56, 95% CIs 1.82 to 3.61, p<0.00001). A higher OR can be found in the psychopathology category (OR 6.10, 95% CIs 2.81 to 13.28), but as this is only composed of one single study this has not been considered as a subgroup.
The two subgroups of symptoms with the lowest ORs are anxiety (OR 1.68, 95% CIs 0.93 to 3.04) and psychotic symptoms/disorders (OR 1.47, 95% CIs 0.93 to 2.30). As the CIs cross the null value in both of these subgroups, this meta-analysis suggests that neither anxiety nor psychotic symptoms are associated with khat use.
Every subgroup has at least five studies to support it, a reasonable amount of supporting evidence. Most of these subgroups have a high level of heterogeneity, apart from the subgroup of unspecified psychiatric symptoms/disorders, which has a heterogeneity of 0%. Note that while psychopathology has been listed as a separate symptom, it is not to be considered as a subgroup as only one study investigated this.
Sensitivity analysis
A sensitivity analysis of the meta-analysis data was conducted and can be seen in online supplemental material 4. Each study was removed in turn and the OR, confidence intervals, I2 value and p value recorded. Removing the depression data from Wondemagegn et al55 caused the largest change in OR, from 2.22 to 2.11. The I2 value for heterogeneity remained at 91% or 92% regardless of which study was removed, and the p value was always <0.00001.
bmjopen-2022-061865supp004.pdf (49.2KB, pdf)
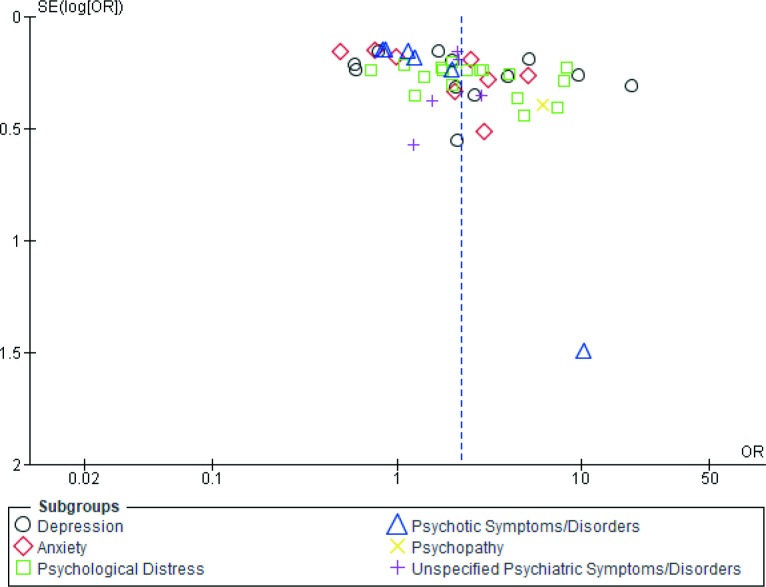
GRADE analysis
The meta-analysis shown in figure 2 received a GRADE score of ‘very low’.21 As per guidance in the GRADE handbook, the score automatically started as ‘low’, because the meta-analysis focuses on observational studies.21 The score was then downgraded for the following two reasons: ‘inconsistency of results’ demonstrated by the high I2 statistic, and ‘indirectness of evidence’ due to the differences between studies including populations investigated and methods of measuring khat use.21 The score was not downgraded for publication bias, as despite occasional outliers, overall the funnel plot for the included studies was fairly symmetrical (see figure 3).
Figure 3.
Funnel plot of included studies.
Discussion
Our findings suggest that khat use is associated with a 122% increased prevalence in overall psychiatric symptoms (OR 2.22, 95% CIs 1.76 to 2.79, p<0.00001). Subgroup analyses suggest thats suggests that the strongest relationship is between khat use and psychological distress (OR 2.56, 95% CIs 1.82 to 3.61, p<0.00001). Subgroup analyses also found that the associations between khat use and anxiety, and khat use and psychotic symptoms/disorders is statistically insignificant (OR 1.68, 95% CIs 0.93 to 3.04 and OR=1.47, 95% CIs 0.93 to 2.30, respectively).
The overall prevalence of psychiatric symptoms and disorders within this systematic review is 29%. Most of the included studies were conducted in Africa, which the WHO estimates has a 5.5% prevalence of common mental disorders.71 The prevalence of symptoms is higher in this review than expected, as many of the studies focus on populations with an increased risk of mental illness, for example, students, migrants, combatants, refugees, prisoners and psychiatric outpatients.72–76
This review has a strong, high-quality methodology, following all of the PRISMA guidelines for systematic reviews.14 However, it can be argued that the evidence base surrounding khat use and psychiatric symptoms is too small to merit the pooling of data. This is reflected in the high heterogeneity of the meta-analysis conducted (I2=92%), which suggests that the studies analysed may be too different to meaningfully compare20; these differences are likely to include the wide variety of populations and regions studies, the differences in khat consumption measurement, and the differences in psychiatric symptom explored. It is also reflected in the low GRADE score of the meta-analysis, however, this scoring system favours experimental rather than observational data, which would be both pragmatically and ethically inappropriate when investigating substance use.77
Despite these concerns, this review is important as it is currently the largest systematic review of khat usage and psychiatric symptoms. A 122% increase in psychiatric symptoms is easy for laypersons to understand, eliminating their need to evaluate various studies of varying quality against each other. Furthermore, the issues highlighted by this review are important for guiding further research. While the results provided by this review are unlikely to be entirely accurate, they can provide a valid estimate until the evidence base expands enough to provide a systematic review with much lower heterogeneity.
One issue in particular is the variation in measuring khat consumption between studies. This review is limited as it has included both non-dependent and dependent khat use, which are likely to have varying association with psychiatric symptoms. Many studies simply described khat users as those who had chewed within the previous week or previous month, hence it was often difficult to distinguish between current users, long-term users and dependent users. This likely contributes to the high heterogeneity of the meta-analysis of this review, and should be considered in future primary and secondary research within this field.
Another limitation of this review is that it includes both psychiatric symptoms and psychiatric disorders under the term ‘psychiatric symptoms’. Out of the 35 included studies, 28 measured psychiatric symptoms using screening tools, 5 measured psychiatric disorders using diagnostic tools and 2 used a mixture of both screening and diagnostic tools. This may also have contributed to the high heterogeneity of the meta-analysis.
One final limitation of this review is that it cannot demonstrate causation between the two variables. It would be useful for future research to include cohort studies. Many researchers hypothesise that khat use is the cause of psychiatric symptoms, with its active ingredients distorting the brain’s cytoarchitecture and, therefore, increasing one’s vulnerability to mental illness.78–80 Contrastingly, other researchers suggest that those with mental illness are more likely to chew khat as an attempt to self-medicate their symptoms.81 Long-term cohort studies would be able to assess which variable predisposes the other, monitor psychiatric symptoms that take time to manifest, and investigate how the prevalence of psychiatric symptoms changes as the duration of khat use increases.
Conclusions
This review combines 35 cross-sectional studies in the field of khat use, and using meta-analysis suggests that khat use is associated with a 122% increase in the prevalence of psychiatric symptoms, particularly psychiatric distress. The high heterogeneity of the meta-analysis is likely due to the wide variation between the studies within the evidence base. To perform a more accurate systematic review, further primary studies are needed with standardised measurements of variables, particularly khat consumption. Furthermore, the evidence base is unclear about causality within this relationship, another important focus for future research.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Dr Keith Brain (University of Birmingham) who originally suggested the topic idea, and Dr Jesse Young (University of Melbourne) for his feedback and enthusiasm towards the project. The authors would also like to thank the library team at the University of Birmingham for their help with the literature search. Finally, the authors would like to thank the Leslie James Topham fund (University of Birmingham Medical School) for providing funding towards living costs while this research was conducted.
Footnotes
Contributors: BE planned the review and created the protocol. BE and NA completed the independent literature searches and created the summary of findings table. BE completed the meta-analyses including the sensitivity analysis. BE and NA independently assessed the quality of the included studies using the Newcastle-Ottawa Scale, and BE completed the GRADE scoring. BE wrote the systematic review and acts as the guarantor for this paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval was not necessary as only secondary data were used.
References
- 1.European Monitoring Centre for Drugs and Drug Addiction . Khat drug profile (date unknown). Available: https://www.emcdda.europa.eu/publications/drug-profiles/khat/de [Accessed 01 Dec 2020].
- 2.Wabe NT. Chemistry, pharmacology, and toxicology of khat (Catha edulis Forsk): a review. Addict Health 2011;3:137–49. [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation . Khat chewing in Yemen: turning over a new leaf, 2008. Available: https://www.who.int/bulletin/volumes/86/10/08-011008/en/ [Accessed 01 Dec 2020]. [DOI] [PMC free article] [PubMed]
- 4.Al-Juhaishi T, Al-Kindi S, Gehani A. Khat: a widely used drug of abuse in the horn of Africa and the Arabian Peninsula: review of literature. Qatar Med J 2012;2012:1–6. 10.5339/qmj.2012.2.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cochrane L, O'Regan D. Legal harvest and illegal trade: trends, challenges, and options in khat production in Ethiopia. Int J Drug Policy 2016;30:27–34. 10.1016/j.drugpo.2016.02.009 [DOI] [PubMed] [Google Scholar]
- 6.Douglas H, Boyle M, Lintzeris N. The health impacts of khat: a qualitative study among Somali-Australians. Med J Aust 2011;195:666–9. 10.5694/mja11.10166 [DOI] [PubMed] [Google Scholar]
- 7.Widmann M, Warsame AH, Mikulica J, et al. Khat Use, PTSD and Psychotic Symptoms among Somali Refugees in Nairobi - A Pilot Study. Front Public Health 2014;2:71. 10.3389/fpubh.2014.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cox G, Rampes H. Adverse effects of khat: a review. Adv. psychiatr. treat 2003;9:456–63. 10.1192/apt.9.6.456 [DOI] [Google Scholar]
- 9.Hassan NAGM, Gunaid AA, Murray-Lyon IM. Khat (Catha edulis): health aspects of khat chewing. East Mediterr Health J 2007;13:706–18. [PubMed] [Google Scholar]
- 10.Young JT, Butt J, Hersi A, et al. Khat dependence, use patterns, and health consequences in Australia: an exploratory study. J Stud Alcohol Drugs 2016;77:343–8. 10.15288/jsad.2016.77.343 [DOI] [PubMed] [Google Scholar]
- 11.Omar YS, Jenkins A, Altena MvanR, et al. Khat use: what is the problem and what can be done? Biomed Res Int 2015;2015:1–7. 10.1155/2015/472302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson DM, Carrier NCM. Khat: social harms and legislation, 2011. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/116260/occ95.pdf
- 13.Edwards B, Atkins N. Exploring the association between khat use and psychiatric symptoms: a systematic review, 2021. Available: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=224510 [DOI] [PMC free article] [PubMed]
- 14.PRISMA . PRISMA checklist, 2021. Available: http://www.prisma-statement.org/PRISMAStatement/Checklist [Accessed 3 May 2021].
- 15.Medical Subject Headings . Us national library of medicine (2021), 2021. Available: https://meshb.nlm.nih.gov/search [Accessed 19 September].
- 16.Sanati A. Does suicide always indicate a mental illness? London J Prim Care 2009;2:93–4. 10.1080/17571472.2009.11493259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Ottawa Hospital . Newcastle-Ottawa quality assessment scale, 2021. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Accessed 19 Sep 2021].
- 18.Modesti PA, Reboldi G, Cappuccio FP, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One 2016;11:e0147601. 10.1371/journal.pone.0147601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deeks JJ, Higgins JPT, Altman DG. Chapter 10: analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, et al., eds. Cochrane Handbook for systematic reviews of interventions. version 6.2. Cochrane, 2021. www.training.cochrane.org/handbook [Google Scholar]
- 20.Sambunjak D, Cumpston M, Watts C. Module 6: analysing the data. in: cochrane interactive learning: conducting an intervention review. Cochrane, 2017. Available: https://training.cochrane.org/interactivelearning/module-6-analysing-data [Accessed 05 Nov 2021].
- 21.Schünemann H, Brozek J, Guyaa G. The grade Handbook, 2013. Available: https://gdt.gradepro.org/app/handbook/handbook.html#h.svwngs6pm0f2 [Accessed 2 May 2021].
- 22.Nakajima M, Hoffman R, al'Absi M. Level of khat dependence, use patterns, and psychosocial correlates in Yemen: a cross-sectional investigation. East Mediterr Health J 2017;23:161–7. 10.26719/2017.23.3.161 [DOI] [PubMed] [Google Scholar]
- 23.al'Absi M, Khalil NS, Al Habori M, et al. Effects of chronic khat use on cardiovascular, adrenocortical, and psychological responses to stress in men and women. Am J Addict 2013;22:99–107. 10.1111/j.1521-0391.2013.00302.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boka A, Alemu M, Fantu A. Magnitude of substance induced psychosis among adolescents in amanuel mental specialised Hospital Addis Ababa, Ethiopia. J Drug Alcohol Res 2021;10:236126 https://www.ashdin.com/articles/magnitude-of-substance-induced-psychosis-among-adolescents-in-amanuel-mental-specialized-hospital-addis-ababa-ethiopia-81031.html [Google Scholar]
- 25.Hassen MT, Soboka M, Widmann M, et al. Khat use patterns, associated features, and psychological problems in a Khat-Treatment-Seeking student sample of Jimma University, southwestern Ethiopia. Front Public Health 2021;9:645980. 10.3389/fpubh.2021.645980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al Bahhawi T, Albasheer OB, Makeen AM, et al. Depression, anxiety, and stress and their association with khat use: a cross-sectional study among Jazan university students, Saudi Arabia. Neurospcyhiatr Dis Treat 2018;14:2755–61. 10.2147/NDT.S182744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakajima M, Jebena MG, Taha M, et al. Correlates of khat use during pregnancy: a cross-sectional study. Addict Behav 2017;73:178–84. 10.1016/j.addbeh.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 28.Mains D, Hadley C, Tessema F. Chewing over the future: khat consumption, anxiety, depression, and time among young men in Jimma, Ethiopia. Cult Med Psychiatry 2013;37:111–30. 10.1007/s11013-012-9292-9 [DOI] [PubMed] [Google Scholar]
- 29.Bhui K, Warfa N. Trauma, khat and common psychotic symptoms among Somali immigrants: a quantitative study. J Ethnopharmacol 2010;132:549–53. 10.1016/j.jep.2010.07.027 [DOI] [PubMed] [Google Scholar]
- 30.Woods D. Mental health and wellbeing of Somalis in the United Kingdom, 2004. Available: https://www.semanticscholar.org/paper/Mental-health-and-well-being-of-Somalis-in-the-Woods/2c4a853a72d029c785575880fcf8a0870d7d0b7c
- 31.Dawud B, Yeshigeta E, Negash A. Substance use disorders and associated factors among adult psychiatric patients in Jimma town, Southwest Ethiopia, 2017, community-based cross-sectional study. Clin Med Insights Psychiatry 2017;12. [Google Scholar]
- 32.Alebachew W, Semahegn A, Ali T, et al. Prevalence, associated factors and consequences of substance use among health and medical science students of Haramaya University, eastern Ethiopia, 2018: a cross-sectional study. BMC Psychiatry 2019;19:343. 10.1186/s12888-019-2340-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yitayih Y, Abera M, Tesfaye E, et al. Substance use disorder and associated factors among prisoners in a correctional institution in Jimma, Southwest Ethiopia: a cross-sectional study. BMC Psychiatry 2018;18:314. 10.1186/s12888-018-1901-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kroll J, Yusuf AI, Fujiwara K. Psychoses, PTSD, and depression in Somali refugees in Minnesota. Soc Psychiatry Psychiatr Epidemiol 2011;46:481–93. 10.1007/s00127-010-0216-0 [DOI] [PubMed] [Google Scholar]
- 35.Ahmed AG, Salib E, Emad S. The khat users: a study of khat chewing in Liverpool's Somali men. Med Sci Law 1998;38:165–9. 10.1177/002580249803800215 [DOI] [PubMed] [Google Scholar]
- 36.Belew M, Kebede D, Kassaye M, et al. The magnitude of khat use and its association with health, nutrition and socio-economic status. Ethiop Med J 2000;38:11–26. [PubMed] [Google Scholar]
- 37.Numan N. Exploration of adverse psychological symptoms in Yemeni khat users by the symptoms Checklist-90 (SCL-90). Addiction 2004;99:61–5. 10.1111/j.1360-0443.2004.00570.x [DOI] [PubMed] [Google Scholar]
- 38.Odenwald M, Neuner F, Schauer M, et al. Khat use as risk factor for psychotic disorders: a cross-sectional and case-control study in Somalia. BMC Med 2005;3:5. 10.1186/1741-7015-3-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deyessa N, Berhane Y, Alem A, et al. Depression among women in rural Ethiopia as related to socioeconomic factors: a community-based study on women in reproductive age groups. Scand J Public Health 2008;36:589–97. 10.1177/1403494808086976 [DOI] [PubMed] [Google Scholar]
- 40.Odenwald M, Hinkel H, Schauer E, et al. Use of khat and posttraumatic stress disorder as risk factors for psychotic symptoms: a study of Somali combatants. Soc Sci Med 2009;69:1040–8. 10.1016/j.socscimed.2009.07.020 [DOI] [PubMed] [Google Scholar]
- 41.Damena T, Mossie A, Tesfaye M. Khat chewing and mental distress: a community based study, in jimma City, southwestern Ethiopia. Ethiop J Health Sci 2011;21:37–45. 10.4314/ejhs.v21i1.69042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tulloch AD, Frayn E, Craig TKJ, et al. Khat use among Somali mental health service users in South London. Soc Psychiatry Psychiatr Epidemiol 2012;47:1649–56. 10.1007/s00127-011-0471-8 [DOI] [PubMed] [Google Scholar]
- 43.Dessie Y, Ebrahim J, Awoke T. Mental distress among university students in Ethiopia: a cross sectional survey. Pan Afr Med J 2013;15:95. 10.11604/pamj.2013.15.95.2173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fekadu W, Haregwoin M, Kibrom H. Magnitude of mental illness and associated factors among Holy water users at Entoto ST Mary church, Addis Ababa, Ethiopia, 2014. J Psychiatry 2014;18:285. [Google Scholar]
- 45.Dachew B, Bifftu B, Tadesse B. Khat use and its determinants among university students in Northwest Ethiopia: a multivariable analysis. Int J Med Sci Public Health 2014;4:1. [Google Scholar]
- 46.Soboka M, Tesfaye M, Feyissa GT, et al. Khat use in people living with HIV: a facility-based cross-sectional survey from South West Ethiopia. BMC Psychiatry 2015;15:69. 10.1186/s12888-015-0446-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zenebe Y, Feyissa GT, Krahl W. Khat use in persons with mental illness in Southwest Ethiopia: a cross-sectional study. J Addict Res Ther 2015;6:3. [Google Scholar]
- 48.El-Setouhy M, Alsanosy RM, Alsharqi A. Khat dependency and psychophysical symptoms among chewers in Jazan region, Kingdom of Saudi Arabia. BioMed Res Int 2016;1:2642506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hersi L, Tesfay K, Gesesew H, et al. Mental distress and associated factors among undergraduate students at the University of Hargeisa, Somaliland: a cross-sectional study. Int J Ment Health Syst 2017;11:39. 10.1186/s13033-017-0146-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hunduma G, Girma M, Digaffe T, et al. Prevalence and determinants of common mental illness among adult residents of Harari regional state, eastern Ethiopia. Pan Afr Med J 2017;28:262. 10.11604/pamj.2017.28.262.12508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kerebih H, Ajaeb M, Hailesilassie H. Common mental disorders among medical students in Jimma University, Southwest Ethiopia. Afr Health Sci 2017;17:844–51. 10.4314/ahs.v17i3.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mossie A, Kindu D, Negash A. Prevalence and severity of depression and its association with substance use in Jimma town, Southwest Ethiopia. Depress Res Treat 2016;2016:3460462. 10.1155/2016/3460462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Soboka M, Gudina EK, Tesfaye M. Psychological morbidity and substance use among patients with hypertension: a hospital-based cross-sectional survey from South West Ethiopia. Int J Ment Health Syst 2017;11:5. 10.1186/s13033-016-0108-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tariku GH, Zerihun AA, Bisrat ZS, et al. Mental distress and its associated factors among students of Mizan AMAN health science College, Ethiopia. J. of Medical Sciences 2017;17:61–7. 10.3923/jms.2017.61.67 [DOI] [Google Scholar]
- 55.Wondemagegn AT, Cheme MC, Kibret KT. Perceived psychological, economic, and social impact of khat chewing among adolescents and adults in Nekemte town, East Welega zone, West Ethiopia. Biomed Res Int 2017;2017:7427892. 10.1155/2017/7427892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yeshaw Y, Mossie A. Depression, anxiety, stress, and their associated factors among Jimma university staff, Jimma, Southwest Ethiopia, 2016: a cross-sectional study. Neuropsychiatr Dis Treat 2017;13:2803–12. 10.2147/NDT.S150444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bedaso A, Kediro G, Yeneabat T. Factors associated with depression among prisoners in southern Ethiopia: a cross-sectional study. BMC Res Notes 2018;11:637. 10.1186/s13104-018-3745-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Adraro W, Kerebih H, Tesema W, et al. Nearly three in every five prisoners experience common mental disorders (CMDs) in Jimma correctional institution; south-west Ethiopia. BMC Public Health 2019;19:1559. 10.1186/s12889-019-7879-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ongeri L, Kirui F, Muniu E, et al. Khat use and psychotic symptoms in a rural khat growing population in Kenya: a household survey. BMC Psychiatry 2019;19:137. 10.1186/s12888-019-2118-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Atnafie SA, Muluneh NY, Getahun KA, et al. Depression, anxiety, stress, and associated factors among khat chewers in Amhara region, Northwest Ethiopia. Depress Res Treat 2020;2020:1–12. 10.1155/2020/7934892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hajure M, Dibaba B, Shemsu S. Psychological distress among health care workers in health facilities of Mettu town during COVID-19 outbreak, Southwest Ethiopia, 2020. Front Psychiatry 2021;10:740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hambisa M, Derese A, Abdeta T. Depressive symptoms among Haramaya university students in Ethiopia: a cross-sectional study. Depress Res Treat 2020;1:5027918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kelemu R, Kahsay A, Ahmed K. Prevalence of mental distress and associated factors among Samara university students, northeast Ethiopia. Depress Res Treat 2020;1:7836296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mekuriaw B, Belayneh Z, Yitayih Y. Magnitude of khat use and associated factors among women attending antenatal care in Gedeo zone health centers, southern Ethiopia: a facility based cross sectional study. BMC Public Health 2020;20:110. 10.1186/s12889-019-8026-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yitayih Y, Soboka M, Tesfaye E, et al. A cross-sectional study of psychopathy and khat abuse among prisoners in the correctional institution in Jimma, Ethiopia. PLoS One 2020;15:e0227405. 10.1371/journal.pone.0227405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Haile K, Sahile AT. Depressive symptoms in primary health care Attendees in Sebeta town, Ethiopia: prevalence, associated factors, and detection by health workers. Sci Prog 2021;104:1–15. 10.1177/00368504211034304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hambisa S, Siraj J, Mesafint G, et al. Assessment of psychological distress and associated factors among hospitalized patients during the COVID-19 pandemic at selected hospitals in Southwest Ethiopia. Neuropsychiatr Dis Treat 2021;17:885–92. 10.2147/NDT.S297460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Melaku L, Mossie A, Negash A. Stress among medical students and its association with substance use and academic performance. J Biomed Educ 2015;1:149509. [Google Scholar]
- 69.Mekuriaw B, Zegeye A, Molla A, et al. Prevalence of common mental disorder and its association with khat chewing among Ethiopian college students: a systematic review and meta-analysis. Psychiatry J 2020;2020:1462141. 10.1155/2020/1462141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Richardson M, Garner P, Donegan S. Interpretation of subgroup analyses in systematic reviews: a tutorial. Clinical Epidemiology and Global Health 2019;7:192–8. 10.1016/j.cegh.2018.05.005 [DOI] [Google Scholar]
- 71.World Health Organisation . Depression and other common mental disorders; global health estimates, 2017. Available: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf [Accessed 05 Nov 2021].
- 72.Bantjes J, Lochner C, Saal W, et al. Prevalence and sociodemographic correlates of common mental disorders among first-year university students in post-apartheid South Africa: implications for a public mental health approach to student wellness. BMC Public Health 2019;19:922. 10.1186/s12889-019-7218-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mental Health Foundation . Mental health statistics: refugees and asylum seekers (NO date). Available: https://www.mentalhealth.org.uk/statistics/mental-health-statistics-refugees-and-asylum-seekers [Accessed 05 Nov 2021].
- 74.Public Health England . Mental health: migrant health guide, 2017. Available: https://www.gov.uk/guidance/mental-health-migrant-health-guide [Accessed 05 Nov 2021].
- 75.Murthy RS, Lakshminarayana R. Mental health consequences of war: a brief review of research findings. World Psychiatry 2006;5:25–30. [PMC free article] [PubMed] [Google Scholar]
- 76.Durcan G, Zwemstra JC. Mental health in prison (NO date). Available: https://www.euro.who.int/__data/assets/pdf_file/0017/249200/Prisons-and-Health,-11-Mental-health-in-prison.pdf [Accessed 05 Nov 2021].
- 77.Price PC, Jhangiani R, Chiang IA. Chapter 6: Nonexperimental research. In: Price PC, Jhangiani R, Chiang IA, et al., eds. Research methods in psychology. 3rd ed, 2017. https://opentext.wsu.edu/carriecuttler/ [Google Scholar]
- 78.Echoru I, Bukenya EEM, Masilili G, et al. Khat distorts the prefrontal cortex histology and function of adult Wistar rats. Anat J Afr 2018;7:1121–31. 10.4314/aja.v7i1.169485 [DOI] [Google Scholar]
- 79.Fluyau D, Mitra P, Lorthe K. Antipsychotics for amphetamine psychosis. A systematic review. Front Psychiatry 2019;10:740. 10.3389/fpsyt.2019.00740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mullen J, Richards J, Crawford A. “Amphetamine related psychiatric disorders”, In: Statpearls. Florida, USA: Statpearls Publishing, 2021. [PubMed] [Google Scholar]
- 81.Odenwald M, al'Absi M, al’Absi M. Khat use and related addiction, mental health and physical disorders: the need to address a growing risk. East Mediterr Health J 2017;23:236–44. 10.26719/2017.23.3.236 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-061865supp001.pdf (43.8KB, pdf)
bmjopen-2022-061865supp002.pdf (90.9KB, pdf)
bmjopen-2022-061865supp003.pdf (85.5KB, pdf)
bmjopen-2022-061865supp004.pdf (49.2KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study.