Abstract
Background:
Among people without psychiatric disorders who smoke, very low nicotine content (VLNC) cigarette use reduces cigarette reinforcement. Whether this is true of people with serious mental illness (SMI) who smoke is unknown. Using a hypothetical purchase task, we compared the effects of 6-week use of VLNC versus normal nicotine content (NNC) cigarettes on study cigarette and usual brand (UB) cigarette reinforcement among people with SMI who smoke.
Methods:
After a baseline period of UB cigarette use, participants with SMI (n = 58) were randomized to use NNC cigarettes (15.8 mg nicotine/g tobacco) or VLNC cigarettes (0.4 mg/g) for 6 weeks. At Week 6, they completed the CPT for both their assigned study cigarette and UB. The groups were compared on demand intensity (number of cigarettes purchased at no cost) and elasticity (rate of decline in demand as price increases) using extra sum-of-squares F-tests. The effects of treatment on demand indices while controlling for covariates were assessed using hierarchical regression.
Results:
At Week 6, intensity of demand for study cigarettes was lower and elasticity was higher for the VLNC group relative to the NNC group (p < 0.0001). Furthermore, intensity of demand for UB cigarettes was lower for participants in the VLNC group relative to participants in the NNC group (p < 0.01). When controlling for baseline cigarettes per day, intensity remained significantly different for study cigarettes and usual brand cigarettes at Week 6.
Conclusion:
A nicotine reduction policy may reduce cigarette reinforcement in this vulnerable population.
Keywords: Serious mental illness, Reinforcement, Demand, Low-nicotine
1. Introduction
Rates of combustible tobacco use among individuals with serious mental illness (SMI), i.e., people with schizophrenia or bipolar disorder, have remained consistently high over the last 20 years (Prochaska et al., 2017). Their smoking rates are 2–4 times higher than rates in the general population at 14% (Centers for Disease Control and Prevention, 2019; Lasser et al., 2000; McClave et al., 2010; Smith et al., 2014). High rates of smoking have been linked to higher mortality risk of cardiovascular disease, tobacco-related cancer and respiratory illness in people with SMI (Callaghan et al., 2014; Saha et al., 2007).
Several theories have been offered for why the high rates of smoking in individuals with SMI persist. Structural, neurobiological, and psychosocial factors may increase smoking initiation, drive progression to dependence, and reduce cessation success among individuals with SMI (Tidey & Miller, 2015). People with SMI have higher levels of cigarette dependence, cigarette craving, withdrawal symptoms, and smoking motives, and relapse to smoking sooner, than those without SMI (DeAtley et al., 2020; Tidey et al., 2014). Reducing cigarette reinforcement may help people with SMI reduce and quit smoking. One theoretical framework for understanding smoking is behavioral economics, which focuses on the reinforcing efficacy of drugs: that is, the extent to which drugs can maintain behavior through either positive or negative reinforcement processes. Tidey (2016) identified two major behavioral mechanisms that may underlie smoking persistence among individuals with SMI: 1) overvaluation of reinforcement from cigarettes and 2) undervaluation of smoking costs (health consequences and benefits of abstinence). Tidey (2016) further proposed that interventions that reduce cigarette reinforcement, combined with interventions that increase the opportunity cost of smoking (such as contingency management), may reduce smoking and related health harms in this population.
One regulatory approach that could be used to reduce the reinforcing efficacy of cigarettes is a federally-mandated reduced-nicotine standard for cigarettes. Authority to regulate the nicotine content in commercially sold cigarettes was granted to the Food and Drug Administration (FDA) in 2009 (The U.S. Food and Drug Administration, 2020) A large body of data has shown that switching people who smoke to very low nicotine content (VLNC) cigarettes reduces cigarettes smoked per day and toxicant exposure without leading to compensatory smoking or intolerable symptoms of withdrawal (Benowitz et al., 2007, 2012; Donny et al., 2015; Hatsukami et al., 2010). Recent trials have extended these findings to people with psychiatric disorders (SMI, depression, anxiety, opioid use disorder) who smoke and have documented positive impacts of VLNC use on cigarette use over 6–20 weeks, without observing compensatory smoking or increases in psychiatric symptoms (Higgins et al., 2020; Tidey et al., 2017, 2019). One 6-week trial found that participants with SMI randomized to the VLNC condition smoked fewer cigarettes per day (CPD) and had lower breath carbon monoxide levels and craving scores than those randomized to normal nicotine content (NNC) cigarettes, without experiencing increases in psychiatric symptoms (Tidey et al., 2019). The current study reports secondary outcomes from data collected in this trial. Similarly, individuals with elevated depressive symptoms at baseline who were randomized to VLNC cigarettes for 6 weeks decreased total cigarettes smoked per day and nicotine dependence severity, while experiencing decreases in depressive symptoms(Tidey et al., 2017). A large randomized trial in three vulnerable populations, including people with depression and anxiety disorders, also found that participants randomized to VLNC cigarettes for 12 weeks reduced their cigarette use and nicotine dependence severity, with minimal or no effects on psychiatric symptoms (Higgins et al., 2020).
An important assessment tool for cigarette reinforcement investigated across these trials is the cigarette purchase task (CPT), which provides information about how reducing the nicotine content of cigarettes affects sensitivity to cigarette cost. The CPT, developed by MacKillop et al., (MacKillop et al., 2008) is a hypothetical task in which participants are asked to estimate the number of cigarettes they would smoke across an increasing range of prices. From these data, a demand curve is produced for each participant that characterizes changes in cigarette consumption as a function of price. Demand indices can be generated that indicate intensity of demand (i.e., number of cigarettes they would smoke if the cigarettes were free), and elasticity of demand (i.e., the rate of change in consumption as price increases) as measures of reinforcement value (MacKillop et al., 2008). This task was previously used in randomized controlled trials of VLNC cigarettes in people sampled from the general population and those from three vulnerable populations. Results indicate that VLNC cigarette use consistently decreases demand for both study cigarettes and usual brand (UB) cigarettes (Higgins et al., 2020; Smith et al., 2017). In a 10-site double blind randomized controlled trial that compared the effects of UB, NNC study cigarettes and reduced-nicotine study cigarettes over a 6-week period, (Donny et al., 2015) participants who had been randomized to use cigarettes with ≤ 2.4 mg nicotine/g tobacco during the intervention reported lower intensity of demand and lower daily expenditure for study cigarettes than those who had been randomized to use UB or NNC cigarettes (Smith et al., 2017). Moreover, those who had used VLNC cigarettes also reported lower intensity of demand and expenditures for their UB cigarettes than those who had used UB or NNC cigarettes during the trial (Smith et al., 2017). However, to date, effects of extended use of VLNC cigarettes on cigarette demand have not been reported for a sample of people with SMI who smoke.
The aim of this secondary analysis was to use the CPT to investigate how 6-week use of VLNC cigarettes impacts cigarette reinforcement among people with SMI who smoke. We hypothesized that 1) compared to participants randomized to NNC cigarettes, participants randomized to VLNC cigarettes would have lower reinforcement from study cigarettes at Week 6, and that 2) those in the VLNC group would also report lower demand for their UB cigarettes at Week 6 relative to the NNC group.
2. Methods
This secondary analysis consists of a comparison of CPT data collected during a randomized controlled trial that compared the effects of using NNC or VLNC cigarettes for 6 weeks on smoking and related subjective and physiological measures among smokers with SMI (Tidey et al., 2019).
2.1. Inclusion criteria
All participants met DSM-IV criteria for lifetime schizophrenia, schizoaffective disorder or bipolar disorder based on the Structured Clinical Interview for DSM-IV Axis-I Disorders (SCID) (First et al., 1994). All participants were at least 18 years of age, smoked at least 10 CPD and provided an exhaled breath CO sample of at least 8 ppm or a urinary cotinine level of at least 100 ng/ml. Women could not be pregnant or breastfeeding, and participants had to provide a negative drug toxicology screen for illicit drugs other than cannabis at enrollment and a negative breath alcohol level at each session. Participants were excluded if they were medically unstable, reported changes in psychiatric symptoms or medications in the last 4 weeks, displayed severe disorientation or uncooperativeness during screening, reported past month suicidal ideation or past year suicide attempt, had tried to quit smoking within the past 30 days, intended to quit smoking within the next 30 days, had used tobacco products other than combustible cigarettes for more than 9 of the last 30 days, or if they reported binge drinking on more than 9 of the last 30 days. For a full description of study details, see (Tidey et al., 2019).
2.2. Intervention design
Prior to randomization, participants had a two-week baseline period in which they smoked their usual brand cigarette. Then, participants were randomized to one of two study conditions: Spectrum NNC cigarettes (15.8 mg nicotine/g tobacco) or VLNC cigarettes (0.4 mg/g). Based on their preference, participants received either menthol or non-menthol study cigarettes. At each weekly visit during the 6-week intervention period, participants were provided with a 14-day supply of research cigarettes to allow for potential compensatory increases in smoking relative to baseline. Participants asked to switch entirely to the research cigarettes and to refrain from using usual brand cigarettes. Participants, staff and investigators were blind to cigarette group assignment (Tidey et al., 2019).
After the second baseline visit, participants visited the lab once every week over the 6-week intervention period and completed a battery of biopsychosocial, physiological and psychiatric measures at each visit (Tidey et al., 2019). At each intervention visit, participants were given brief study cigarette compliance counseling, consistent with other randomized controlled trials (Donny et al., 2015; Hatsukami et al., 2018). To increase study cigarette adherence, participants were eligible for a $200 lottery-based incentive payment if they attended study sessions as scheduled, provided urine samples that met a nicotine reduction criterion (VLNC condition only), and if their self-reported study cigarette compliance was consistent with their biologically-verified compliance status (VLNC condition only). This incentive system used a semi-bogus pipeline in which urine samples from all participants were collected weekly, but tested only monthly, and only samples from participants in the VLNC condition were tested. Because it was not possible to biochemically verify study cigarette compliance in the NNC condition, participants in that condition were yoked with a participant in the VLNC condition so that compensation would be equal across groups. Samples were tested by Biomarkers Core staff at another site. Study staff who interacted with participants were informed who had won the lottery but were not given any other information (Tidey et al., 2019).
2.3. Measures
2.3.1. Cigarettes per day
We used self-reported baseline CPD as a measure of smoking heaviness to validate the use of this task among this sample.
2.3.2. Cigarette purchase task - baseline
At Week 2 (baseline period), participants in both studies were asked to complete the CPT for their usual brand.
In this task, participants were told to imagine they had the same income/savings that they had right now and that they had no access to any cigarettes or nicotine products other than those offered in the task and could not stockpile cigarettes for a later day. Under these conditions, participants were asked how many usual brand cigarettes they would smoke without any restrictions for the next 24 h. The price per cigarette started at $0.00 and increased to the following amounts: $0.02, $0.05 and from $0.10–1.00 in $0.10 increments. At $1.00 the response options increased by $1.00 increments up to $5.00. At each price, participants were also given the corresponding price per pack at each respective price per cigarette (Smith et al., 2017).
2.3.3. Cigarette purchase task – Week 6
At Week 6, participants were asked to complete the CPT for their assigned study cigarette and for their usual brand cigarette. The version of the CPT for study cigarettes was identical to the usual brand version administered at baseline, apart from the product specification in the instructions.
2.4. Behavioral economic analysis
2.4.1. Cigarette purchase task demand indicies
Changes in cigarette demand were determined by plotting data from the CPT and calculating the slope of the demand curve across a range of prices. Specific indices that were empirically derived using an observed values approach include: Intensity (the number of cigarettes participants would consume if they were free), Omax (the maximum expenditure on cigarettes), Pmax (the price at which Omax is reached), Breakpoint (the price at which consumption drops to zero) and α, which is a rate parameter and measure of demand elasticity, and is derived from the equation:
Q is consumption of cigarettes; Q0 is maximum consumption at $0.00 (fitted intensity parameter); k is set to a constant of 3; and C is price. There is an inverse relationship between alpha and reinforcing efficacy, meaning that higher alpha values indicate lower reinforcing efficacy. Demand can either be inelastic or elastic. If a commodity has high reinforcing efficacy, then demand is inelastic, meaning that it is relatively insensitive to change in price. If a commodity has low reinforcing efficacy, demand is elastic, and consumption of a commodity is sensitive to change in price.
Purchase task raw data were first examined for nonsystematic patterns using an approach developed by Stein et al. (Stein et al., 2015). Briefly, three criteria were used to identify and exclude nonsystematic data (trend, bounce and reversals from zero). For non-systematic trend data, an algorithm was used to identify invariant or ascending demand curves. Similarly, for bounce data, an algorithm was used to identify variable price-to-price data that exceeded 25% of the initial consumption at the lowest price. Lastly, we excluded data that violated a reversal from zero (i.e., consumption increasing after having reached zero), reflecting inconsistent purchasing. At baseline, after accounting for nonsystematic patterns, the final sample was n = 49 (21 in the NNC condition and 28 in the VLNC condition). Usual brand CPT data were removed from seven participants due to trend criteria and data from three participants were removed due to bounce criteria. Reasons for removal were not mutually exclusive, meaning that a participant could have data that failed to meet more than one criterion. At Week 6, usual brand CPT data from two participants were removed due to trend criteria, data from one participant were removed due to bounce criteria, and 10 participants had missing data. This resulted in a final analyzed sample of 45 participants (21 in the NNC and 24 in the VLNC condition). At Week 6 for study cigarettes, data were removed from nine participants due to trend criteria and data from four participants were removed due to bounce criteria. 10 participants had missing data, resulting in a final analyzed sample of 37 participants (19 in the NNC and 18 in the VLNC condition).
Indices were checked for outliers using the z-score method, and outliers were recoded to 3 standard deviations above the mean. This affected 2 intensity values and one Omax value at baseline. In addition, at Week 6, one intensity value and two Omax values were adjusted for usual brand cigarette data and one intensity value and one Omax value were adjusted for study cigarette data. Among participants who did not reach breakpoint (i.e., did not reduce their response output to zero), breakpoint values were recoded to one unit higher than the highest price in the CPT, $6.00. Predicted and observed points on the curve were fitted using non-linear least squares regression which calculates the vertical distances of the points (actual and derived) from the curve (Motulsky, 2014). For the t-tests and hierarchical regressions, data was log-transformed or cube-root transformed if necessary to meet normality assumptions (Koffarnus et al., 2015).
At Week 6, usual brand CPT data from one participant and study cigarette CPT data from five participants were excluded from the exponentiated demand equation analysis due to null demand. Data for these participants were not used for the exponentiated demand curve because the curve cannot be fitted to values of zero. A more detailed description of analyses of these data can be found in the null demand section, below.
2.4.2. Correlations and associations
We examined correlations between demand indices for usual brand cigarettes at baseline and participant gender, age, and CPD, to characterize demand differences due to gender and age, and to determine the validity of the demand indices by indexing their concurrent associations with self-reported smoking rate. Correlation analyses were limited to intensity, alpha and Omax as these are the indices with the strongest associations reported for substance use outcomes (Strickland et al. 2020; Zvorsky et al., 2019). In addition, to explore the association between demand indices and menthol, t-tests were run for each demand indice by menthol-preference status.
2.4.3. Fitting exponential demand across condition
The demand curves for both usual brand and study cigarettes were fitted to an exponentiated demand equation derived by Koffarnus et al. (2015) The group-fitted intensity (Q0) and group curve elasticity (alpha) values for each condition were compared at each time point using an F-test using GraphPad Prism Version 9 software (GraphPad Prism, 2020). This approach allows us to test whether a model in which alpha and Q0 for both study cigarettes and usual brand cigarettes at Week 6 are shared parameters is a better fit than two separate models when accounting for increases in degrees of freedom. Participants with null demand cannot be included in such analyses; see the null demand section below for further information.
2.4.4. Condition effects on Intensity, break point, Omax, Pmax and alpha
To determine the effects of cigarette condition on demand indices derived from the raw data, differences across VLNC and NNC cigarette groups in each index were examined using hierarchical regressions in STATA (StataCorp, 2017). We tested models for study cigarettes (VLNCs vs. NNCs) and demand for study cigarettes and usual brand cigarettes at Week 6 to determine the effects of treatment group on dimensions of reinforcing efficacy. Blocks in the hierarchical regression were grouped as: cigarette condition at baseline in block 1, and heaviness of smoking as measured by CPD in block 2. Entering CPD in block 2 enabled us to examine the unique contributing effect of CPD in this heavy-smoking sample. Given that lack of demand is an important observation when measuring reinforcing efficacy, we included participants’ null demand data for these empirical comparisons. Removing participants who reported null demand could artificially inflate demand indices such as intensity. Since we did not observe significant correlations with sex or age for the primary demand indices at baseline, we did not include these covariates in hierarchical regressions.
2.4.5. Null demand analysis
Six participants reported that they would not purchase any cigarettes at Week 6 (N = 1 for usual brand cigarettes and N = 5 for study cigarettes). Data for these participants were not used for the exponentiated demand curve because the curve cannot be fitted to values of zero. Given the importance of exposure to VLNCs on addiction potential and the interpretation of null demand as a potential intention to quit, we expressed null demand data as the count of participants who expressed null demand at price zero across nicotine dose.
3. Results
At baseline, participants in the final sample (n = 49), were 37% female and 63% male, and an average of 42.8 years old (SD = 9.9). Over half of participants identified as White 55%, 20% identified as Black and 25% identified as some other race. Participants reported smoking an average of 18.9 (SD = 7.8) CPD and 71% were menthol smokers. The VLNC and NNC groups did not differ on any demographic or smoking history measure.
3.1. Correlations
Bivariate correlations between sex, age, and CPD with usual brand demand indices intensity, alpha, and Omax are shown in Table 1. Baseline CPD was positively associated with intensity and negatively associated with alpha (Table 1). Omax was negatively correlated with age and positively correlated with intensity. There were no significant effects of menthol-status on demand indicies.
Table 1.
Correlations Between Baseline Variables and Usual Brand Demand Indices Derived from the CPT (N = 49).
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Sex | 1 | |||||
| 2. Age | −0.05 | 1 | ||||
| 3. Baseline Cigarettes per Day | −0.28 | 0.22 | 1 | |||
| 4. Intensity | −0.11 | −0.06 | 0.54 * | 1 | ||
| 5. Omax | −0.12 | −0.31 * | 0.27 | 0.36 * | 1 | |
| 6. Alpha | −0.04 | 0.26 | −0.34 * | −0.36 * | −0.48 * | 1 |
denotes significance level of<0.05.
CPT, Cigarette Purchase Task.
3.2. Comparison of demand indices across conditions
As expected, the VLNC and NNC groups did not differ on demand indices for UB cigarettes at baseline (not shown). Figure 1 (top) shows the global fit curves using the derived values of alpha (elasticity) and Q0 (intensity) for study cigarettes at Week 6, and Figure 1 (bottom) shows the global fit curves for UB cigarettes at Week 6. Effects of treatment group on Q0, Omax and alpha values for UB and study cigarettes at Week 6 are shown in Figure 2. Extra sum of squares F-tests showed that alpha was higher and intensity of demand for study cigarettes was lower in the VLNC group than in the NNC group at Week 6, indicating greater sensitivity to cost (F (2, 625) = 19.99, p < 0.0001). In addition, participants in the VLNC group demonstrated reduced intensity of demand for their UB cigarettes relative to participants in the NNC group at Week 6 (F (1, 761) = 10.31, p < 0.01), indicating that those who had switched to VLNC cigarettes during the 6-week intervention had reduced magnitude of UB demand relative to those who had used NNC cigarettes.
Fig. 1.

Fitted Demand Curves for Cigarettes by Cigarette Condition.
Fig. 2.
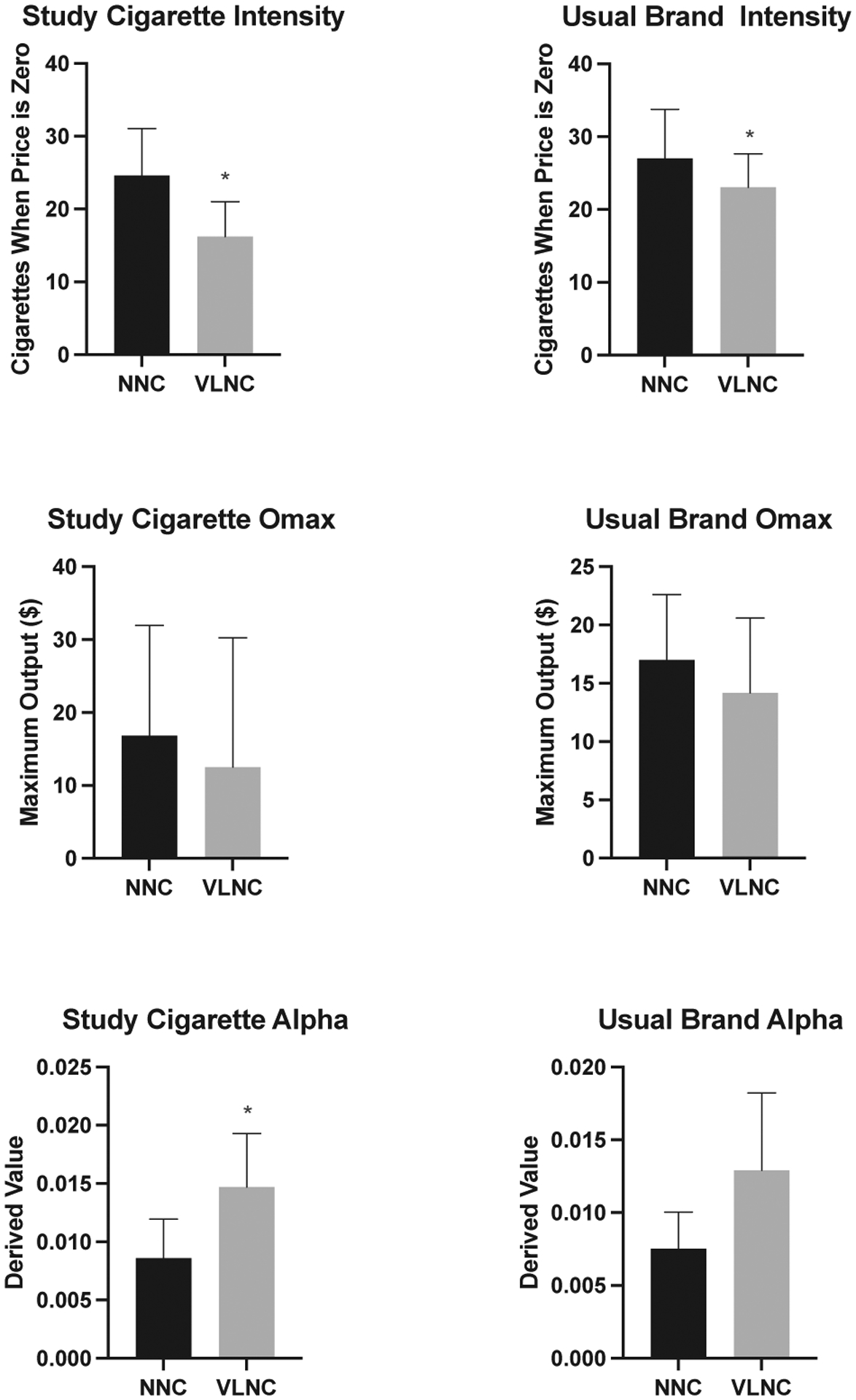
Demand Indicies at Week 6 by Treatment Group.
*Asterisks denote a significant difference between f NNC and VLNC cigarettes
Results of the hierarchical regressions are shown in Table 2. Effects of treatment group on intensity and elasticity of demand for study cigarettes were significant prior to controlling for baseline CPD (p = 0.015, p = 0.017, respectively). After controlling for baseline CPD, the effect of treatment group on intensity of demand for study cigarettes remained significant (p = 0.015), but the effect of treatment group on elasticity of demand for study cigarettes was no longer significant. The effect of treatment group on intensity of demand for usual brand cigarettes was significant after controlling for baseline CPD (p = 0.00). The effect of treatment group on elasticity of demand for UB cigarettes approached significance (p = 0.059), although not after controlling for baseline CPD (Table 2).
Table 2.
Hierarchical Regression Results by Demand Index for Usual Brand and Study Cigarette Purchase Task Data.
| Block 1 | Block 2 | ||||||
|---|---|---|---|---|---|---|---|
| Demand Index at Week 6 | Predictor | Beta | 95% CI | P-Value | Beta | 95% CI | P-Value |
| Study Cigarette Intensity | Treatment Group | −8.38 | −16.04 – −0.71 | 0.03 | −9.10 | −16.33 – −1.8 | 0.02 * |
| Baseline CPD | 0.56 | 0.11 – 0.98 | 0.02 * | ||||
| Study Cigarette Omax | Treatment Group | −4.3 | −15.3 – 6.67 | 0.43 | −4.5 | −15.67 – 6.6 | 0.41 |
| Baseline CPD | 0.20 | −0.53 – 0.91 | 0.60 | ||||
| Study Cigarette Pmax | Treatment Group | 0.002 | −0.32 – − 0.32 | 0.99 | 0.01 | −0.31 – 0.34 | 0.93 |
| Baseline CPD | −0.01 | −0.03 – 0.01 | 0.34 | ||||
| Study Cigarette Breakpoint | Treatment Group | −0.53 | −2.1 – 1.03 | 0.49 | −0.46 | −2.03 – 1.10 | 0.55 |
| Baseline CPD | −0.06 | −0.16 – 0.04 | 0.25 | ||||
| Study Cigarette Alpha | Treatment Group | 0.05 | 0.01 – 0.09 | 0.02 | 0.05 | 0.011 – 0.09 | 0.02 * |
| Baseline CPD | −0.001 | −0.003 – 0.002 | 0.54 | ||||
| Usual Brand Intensity | Treatment Group | −1.91 | −10.10 – 6.28 | 0.64 | −5.13 | −11.89 – 1.6 | 0.13 |
| Baseline CPD | 1.03 | 0.60 – 1.45 | 0.00 * | ||||
| Usual Brand Omax | Treatment Group | −0.15 | −0.36 – 0.07 | 0.18 | −0.16 | −0.38 – 0.05 | 0.13 |
| Baseline CPD | 0.007 | −0.01 – 0.02 | 0.32 | ||||
| Usual Brand Pmax | Treatment Group | −0.12 | −0.43 – 0.18 | 0.42 | −0.10 | −0.41 – 0.21 | 0.52 |
| Baseline CPD | −0.01 | −0.03 – 0.01 | 0.43 | ||||
| Usual Brand Breakpoint | Treatment Group | −0.63 | −2.1 – 0.82 | 0.38 | −0.46 | −1.9 – 0.10 | 0.53 |
| Baseline CPD | −0.06 | −0.15 – 0.03 | 0.23 | ||||
| Usual Brand Alpha | Treatment Group | 0.03 | −0.004 – 0.07 | 0.08 | 0.04 | −0.002 – 0.07 | 0.06 |
| Baseline CPD | −0.001 | −0.003 – 0.001 | 0.40 | ||||
denotes significance level of<0.05
3.3. Null demand analysis
Among participants at Week 6, five participants expressed zero demand for study cigarettes and one participant expressed zero demand for their usual brand cigarettes. Of the five that expressed null demand for their study cigarettes at Week 6, one participant was in the NNC condition and four were in the VLNC condition. A nonparametric Wilcox signed-rank U test indicated that, after recoding VLNC cigarettes and NNC cigarettes to one for null demand and zero for demand, the difference between treatment groups approached significance, p = 0.08.
4. Discussion
High smoking rates and poor tobacco-related health outcomes among individuals with SMI highlight the need to generate innovative solutions for this vulnerable population given that current tobacco control efforts have not achieved adequate success. A reduced-nicotine standard is one potentially effective approach. Building on the main outcomes from this study, in which participants with SMI who were randomized to switch to VLNC cigarettes had lower smoking rates, dependence, and cigarette craving at Week 6 than those randomized to NNC cigarettes, (Tidey et al., 2019) the current findings indicate that a nicotine reduction policy may reduce the reinforcing value of cigarettes among individuals with SMI. Specifically, VLNC use led to significantly lower demand intensity for both study and UB cigarettes, and sensitivity to price for study cigarettes was higher among individuals in the VLNC condition relative to the NNC condition. These findings replicate other findings that demonstrate the reduced reinforcing efficacy of VLNC cigarettes among other populations of adults, (Higgins et al., 2020; Smith et al., 2017) and extend these findings to individuals with SMI, a vulnerable population.
Importantly, our data suggest that not only would individuals with SMI attain less reinforcement from VLNC cigarettes, but they may also be less inclined to seek out their UB cigarettes, as shown by reduced intensity of demand for UB cigarettes in the VLNC group after 6 weeks of exposure relative to the NNC group. A larger trial of non-psychiatric adults likewise found that 6 weeks of VLNC cigarette use reduced reinforcement from UB cigarettes (Smith et al., 2017). One explanation for why use of VLNC cigarettes may reduce the reinforcing efficacy of UB cigarettes may lie in the fact that reinforcement from smoking is derived from both the pharmacological effects of nicotine and the conditioned reinforcing effects of smoking-associated sensorimotor stimuli from repeated pairings with nicotine delivery (Rose, 2006). VLNC cigarettes deliver only trace amounts of nicotine and may attenuate the conditioned reinforcing effects of smoking stimuli, as they are no longer paired with the primary reinforcer, nicotine. It is possible that some of the extinction effects of exposure to VLNC cigarettes may generalize to UB cigarettes as well, such that demand for them is reduced (Donny et al., 2007) For example, lower levels of cigarette satisfaction and reward are reported with VLNCs (Tidey et al., 2019) and may result in reduced reinforcement. Another potential explanation is that extended use of VLNC cigarettes may lead to reduced nicotine withdrawal severity, leading to lower demand for usual brand cigarettes. However, the report of primary outcomes from this study found no effects of cigarette condition on withdrawal symptoms at Week 6, (Tidey et al., 2019) similar to other reports (Donny et al., 2015).
Despite our sample being predominately menthol smokers, no effects of menthol status were observed on demand indices. Evidence suggests that menthol interacts with nicotine content to enhance subjective response and menthol flavoring my have rewarding effects on its own. However, Denlinger-Apte found that people using menthol cigarettes still respond to VLNCs cigarettes, albeit with slightly smaller reductions in smoking and toxicant exposure relative to non-menthol cigarette users (Denlinger-Apte et al., 2019).
Limitations to this analysis include its small sample size relative to CPT analyses conducted in smokers without SMI, and the relatively limited VLNC intervention period (6 weeks). The extent to which our results may change after a longer exposure period to VLNCs is not known. Our sample had slightly more males than females, which may bias our results as men have been found to be slightly more sensitive to price than females, however, gender generally does not appear to impact intensity of demand (Liao et al., 2013). Although income has been found to be an important moderator of nicotine dependence among adults, (Hobkirk et al., 2018) the measures of SES collected were inadequate for assessing the potential moderating effect of SES in this study. In addition, VLNC cigarettes were provided free of charge, therefore we cannot draw any conclusions about the impact of nicotine reduction on cigarette reinforcement within the context of normally priced cigarettes or other nicotine products available on the market. Trials are underway among adults with affective disorders, substance use disorders, and socioeconomic disadvantages exposed to VLNCs with and without e-cigarettes for 20 weeks, which may shed light on whether the availability of an alternative nicotine-containing product may further reduce the effects of VLNC use on cigarette reinforcement.
5. Conclusion
This study complements other studies that have demonstrated that VLNC cigarettes reduce cigarette reinforcement among smokers in the general population and vulnerable populations such as pregnant women, opioid users, and individuals with affective disorders. Overall, our findings provide important information to scientists and regulators by demonstrating that the benefits of a nicotine reduction policy for individuals with SMI may be similar to those in people without SMI who smoke. Reducing the reinforcing effects of cigarettes may also increase the efficacy of pharmacological and behavioral smoking cessation treatment approaches, including nicotine replacement therapy and contingency management interventions. It is important to continue to explore the potential effects of this policy for vulnerable populations and subpopulations to maximize the policy’s effectiveness.
Abbreviations:
- SMI
serious mental illness
- UB
usual brand
- VLNC
very low nicotine content
- NNC
normal nicotine content
- CPT
cigarette purchase task
Footnotes
CRediT authorship contribution statement
Teresa E. DeAtley: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Software, Visualization, Writing – original draft. Rachel Cassidy: Conceptualization, Data curation, Formal analysis, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft. Morgan L. Snell: Data curation, Formal analysis, Software, Writing – review & editing. Suzanne M. Colby: Funding acquisition, Investigation, Writing – review & editing. Jennifer W. Tidey: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Visualization, Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Benowitz NL, Dains KM, Hall SM, Stewart S, Wilson M, Dempsey D, et al. (2012). Smoking behavior and exposure to tobacco toxicants during 6 months of smoking progressively reduced nicotine content cigarettes. Cancer Epidemiology, Biomarkers and Prevention. 10.1158/1055-9965.EPI-11-0644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL, Hall SM, Stewart S, Wilson M, Dempsey D, & Jacob P (2007). Nicotine and carcinogen exposure with smoking of progressively reduced nicotine content cigarette. Cancer Epidemiology, Biomarkers and Prevention, 16, 2479. 10.1158/1055-9965.EPI-07-0393 [DOI] [PubMed] [Google Scholar]
- Callaghan RC, Veldhuizen S, Jeysingh T, Orlan C, Graham C, Kakouris G, et al. (2014). Patterns of tobacco-related mortality among individuals diagnosed with schizophrenia, bipolar disorder, or depression. Journal of Psychiatric Research, 48, 102–110. 10.1016/j.jpsychires.2013.09.014 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Current Cigarette Smoking Among Adults in the United States. 2019. Available from: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm.
- DeAtley T, Denlinger-Apte RL, Cioe PA, Colby SM, Cassidy RN, Clark MA, et al. (2020). Biopsychosocial mechanisms associated with tobacco use in smokers with and without serious mental illness. Preventive Medicine, 140, Article 106190. 10.1016/j.ypmed.2020.106190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denlinger-Apte RL, Kotlyar M, Koopmeiners JS, Tidey JW, Luo X, Benowitz NL, et al. (2019). Effects of very low nicotine content cigarettes on smoking behavior and biomarkers of exposure in menthol and non-menthol smokers. Nicotine & Tobacco Research, 21(Suppl 1), S63–S72. 10.1093/ntr/ntz160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donny EC, Denlinger RL, Tidey JW, Koopmeiners JS, Benowitz NL, Vandrey RG, et al. (2015). Randomized trial of reduced-nicotine standards for cigarettes. NEJM., 373, 1340–1349. 10.1056/NEJMsa1502403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donny EC, Houtsmuller E, & Stitzer ML (2007). Smoking in the absence of nicotine: Behavioral, subjective and physiological effects over 11 days. Journal of Addiction, 102, 324–334. 10.1111/j.1360-0443.2006.01670.x [DOI] [PubMed] [Google Scholar]
- First MBSR, Gibbon M, & Williams JB (1994). Structured Clinical Interview for DSM-IV Axis-I Disorders—Patient Edition (SCID -I / P, Version 2.0). New York, NY: Biometric Research Department. [Google Scholar]
- GraphPad Prism Version 9.0. GraphPad Software. San Diego California USA: 2020; Available from: www.graphpad.com. [Google Scholar]
- Hatsukami DK, Kotlyar M, Hertsgaard LA, Zhang Y, Carmella SG, Jensen JA, et al. (2010). Reduced nicotine content cigarettes: Effects on toxicant exposure, dependence and cessation. Journal of Addiction, 105, 343–355. 10.1111/j.1360-0443.2009.02780.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami DK, Luo X, Jensen JA, et al. (2018). Effect of immediate vs gradual reduction in nicotine content of cigarettes on biomarkers of smoke exposure: A randomized clinical trial. JAMA, 320, 880–891. 10.1001/jama.2018.11473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Tidey JW, Sigmon SC, Heil SH, Gaalema DE, Lee D, et al. (2020). Changes in Cigarette Consumption With Reduced Nicotine Content Cigarettes Among Smokers With Psychiatric Conditions or Socioeconomic Disadvantage: 3 Randomized Clinical Trials. JAMA Network Open, 3. 10.1001/jamanetworkopen.2020.19311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobkirk AL, Krebs NM, & Muscat JE (2018). Income as a moderator of psychological stress and nicotine dependence among adult smokers. Addictive Behaviors, 84, 215–223. 10.1016/j.addbeh.2018.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Franck CT, Stein JS, & Bickel WK (2015). A modified exponential behavioral economic demand model to better describe consumption data. Experimental and Clinical Psychopharmacology, 23, 504–512. 10.1037/pha0000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasser K, Boyd J, Woolhandler S, Himmelstein DU, McCormick D, & Bor DH (2000). Smoking and mental illness: A population-based prevalence study. The Journal of the American Medical Association, 284, 2606–2610. 10.1001/jama.284.20.2606 [DOI] [PubMed] [Google Scholar]
- Liao W, Luo X, Le CT, Chu H, Epstein LH, Yu J, et al. (2013). Analysis of cigarette purchase task instrument data with a left-censored mixed effects model. Experimental and Clinical Psychopharmacology, 21(2), 124–132. 10.1037/a0031610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Ray LA, Eisenberg DTA, Lisman SA, Lum JK, et al. (2008). Further validation of a cigarette purchase task for assessing the relative reinforcing efficacy of nicotine in college smokers. Experimental and Clinical Psychopharmacology, 16, 57–65. 10.1037/1064-1297.16.1.57 [DOI] [PubMed] [Google Scholar]
- McClave AK, McKnight-Eily LR, Davis SP, & Dube SR (2010). Smoking characteristics of adults with selected lifetime mental illnesses: Results from the 2007 National Health Interview Survey. American Journal of Public Health, 100, 2464–2472. 10.2105/AJPH.2009.188136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motulsky H (2014). Intuitive biostatistics: A nonmathematical guide to statistical thinking. USA: Oxford University Press. [Google Scholar]
- Prochaska JJ, Das S, & Young-Wolff KC (2017). Smoking, mental illness, and public health. Annual Review of Public Health, 38, 165–185. 10.1146/annurev-publhealth-031816-044618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose JE (2006). Nicotine and nonnicotine factors in cigarette addiction. Psychopharmacology (Berl), 184, 274–285. 10.1007/s00213-005-0250-x [DOI] [PubMed] [Google Scholar]
- Saha S, Chant D, & McGrath J (2007). A systematic review of mortality in schizophrenia: Is the differential mortality gap worsening over time? Archives of General Psychiatry, 64, 1123–1131. 10.1001/archpsyc.64.10.1123 [DOI] [PubMed] [Google Scholar]
- Smith TT, Cassidy RN, Tidey JW, Luo X, Le CT, Hatsukami DK, et al. (2017). Impact of smoking reduced nicotine content cigarettes on sensitivity to cigarette price: Further results from a multi-site clinical trial. Journal of Addiction, 112, 349–359. 10.1111/add.13636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PH, Mazure CM, & McKee SA (2014). Smoking and mental illness in the US population. Tobacco Control., 23, e147. 10.1136/tobaccocontrol-2013-051466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. Available from: https://www.stata.com/. [Google Scholar]
- Stein JS, Koffarnus MN, Snider SE, Quisenberry AJ, & Bickel WK (2015). Identification and management of nonsystematic purchase task data: Toward best practice. Experimental and Clinical Psychopharmacology, 23, 377–386. 10.1037/pha0000020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland JC, Campbell EM, Lile JA, & Stoops WW (2020). Utilizing the commodity purchase task to evaluate behavioral economic demand for illicit substances: A review and meta-analysis. Journal of Addiction, 115, 393–406. 10.1111/add.14792 [DOI] [PubMed] [Google Scholar]
- The U.S. Food and Drug Administration. Family Smoking Prevention and Tobacco Control Act. 2020. Accessed 2021, Available from: https://www.fda.gov/tobacco-products/rules-regulations-and-guidance/family-smoking-prevention-and-tobacco-control-act-overview.
- Tidey JW (2016). A behavioral economic perspective on smoking persistence in serious mental illness. Preventive Medicine, 92, 31–35. 10.1016/j.ypmed.2016.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tidey JW, Colby SM, Denlinger-Apte RL, Goodwin C, Cioe PA, Cassidy RN, et al. (2019). Effects of 6-week use of very low nicotine content cigarettes in smokers with serious mental illness. Nicotine & Tobacco Research, 21, S38–S45. 10.1093/ntr/ntz133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tidey JW, Colby SM, & Xavier EM (2014). Effects of smoking abstinence on cigarette craving, nicotine withdrawal, and nicotine reinforcement in smokers with and without schizophrenia. Nicotine & Tobacco Research, 16(3), 326–334. 10.1093/ntr/ntt152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tidey JW, & Miller ME (2015). British Medical Journal (Clinical Research ed), 351, h4065. 10.1136/bmj.h4065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tidey JW, Pacek LR, Koopmeiners JS, Vandrey R, Nardone N, Drobes DJ, et al. (2017). Effects of 6-week use of reduced-nicotine content cigarettes in smokers with and without elevated depressive symptoms. Nicotine & Tobacco Research, 19, 59–67. 10.1093/ntr/ntw199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvorsky I, Nighbor TD, Kurti AN, DeSarno M, Naudé G, Reed DD, et al. (2019). Sensitivity of hypothetical purchase task indices when studying substance use: A systematic literature review. Preventive Medicine, 128, Article 105789. 10.1016/j.ypmed.2019.105789 [DOI] [PMC free article] [PubMed] [Google Scholar]


