Abstract
Mindfulness-based cognitive therapy (MBCT) is a promising intervention for reducing depressive symptoms in individuals with comorbid chronic disease, but the program’s attendance demands make it inaccessible to many who might benefit. We tested the feasibility, acceptability, safety, and preliminary efficacy of an abbreviated, telephone-delivered adaptation of the in-person mindfulness-based cognitive therapy (MBCT-T) program in a sample of patients with depressive symptoms and hypertension.
Participants (n = 14; 78.6% female, mean age = 60.6) with mild to moderate depressive symptoms and hypertension participated in the 8-week MBCT-T program. Feasibility was indexed via session attendance and home-based practice completion. Acceptability was indexed via self-reported satisfaction scores. Safety was assessed via reports of symptomatic decline or need for additional mental health treatment. Depressive symptoms (Quick Inventory of Depressive Symptomatology–Self-Report [QIDS-SR]) and anxiety (Hospital Anxiety and Depression Scale—Anxiety subscale; HADS-A) were assessed at baseline and immediately following the intervention.
Sixty-four percent of participants (n = 9) attended ≥4 intervention sessions. Seventy-one percent (n = 6) of participants reported completing all assigned formal home practice and 89.2% (n = 8) reported completing all assigned informal practice. Participants were either very satisfied (75%; n = 6) or mostly satisfied (25%; n = 2) with the intervention. There were no adverse events or additional need for mental health treatment. Depressive symptom scores were 4.09 points lower postintervention (p = .004). Anxiety scores were 3.18 points lower postintervention (p = .039).
Results support the feasibility, acceptability, safety, and preliminary efficacy of an abbreviated, telephone-delivered version of MBCT for reducing depressive and anxiety symptoms in individuals with co-occurring chronic disease.
Keywords: mindfulness-based cognitive therapy, telephone-delivered, depression, pilot trial, hypertension
Elevated depressive symptoms in the moderate to severe range are experienced by nearly 10% of the U.S. population and frequently lead to a major depressive disorder (MDD; Pratt & Brody, 2014). Depressive symptoms also commonly co-occur in patients with chronic diseases and are associated with poorer disease outcomes and increased risk for mortality compared to those without depressive symptoms (Iosifescu et al., 2004; Katon, 2011). Substantial evidence indicates that mindfulness-based cognitive therapy (MBCT), which combines mindfulness training with cognitive therapy, is an efficacious intervention for reducing residual depressive symptoms in patients with a history of recurrent MDD (Shallcross et al., 2015; Teasdale et al., 2000). Several recent studies have also demonstrated that MBCT reduces depressive symptoms in people with comorbid chronic diseases, including cardiovascular disease (Abbott et al., 2014), diabetes (Tovote et al., 2014), fibromyalgia (Parra-Delgado & Latorre-Postigo, 2013), and cancer (Foley et al., 2010).
Relevant to the present study, up to 38% of patients with hypertension, the most common diagnosis in primary care practices and a primary risk factor for cardiovascular disease (Centers for Disease Control and Prevention, 2011; Hsiao et al., 2010), have comorbid depressive disorders (Amaral et al., 2007). The relationship between hypertension and depression is likely bidirectional (Lippi et al., 2009), explained by shared biological (e.g., autonomic nervous system functioning) and behavioral pathways (e.g., smoking, inactivity; Lippi et al., 2009; Meng et al., 2012). Despite bidirectional evidence, depression has been shown to be independently associated with poor blood pressure control and an up to a 14-fold increase in mortality in patients with hypertension (Patten et al., 2009; Rubio-Guerra et al., 2013).
Although depression is common and eminently treatable, 50% of patients with depression remain undiagnosed or inadequately treated in primary care settings (Thornicroft et al., 2017). This is especially problematic because depression is most commonly diagnosed and treated by primary care practitioners. Psychotropic medications are the most common treatment for depression but are associated with poor adherence (Sansone & Sansone, 2012), side effects (Ferguson, 2001), and unpredictable responsiveness (Fournier et al., 2010). Further, many patients prefer nonpharmacological approaches (Prins et al., 2008).
Psychological interventions like MBCT are a viable complementary or alternative treatment option for depression—however, MBCT remains inaccessible to many individuals who might benefit from it (Creswell, 2017). The standardized MBCT protocol is delivered in eight weekly 2.5-hour, in-person group sessions. This format presents feasibility challenges as the time commitment and practical effort involved in attending sessions may prevent people from receiving benefit from MBCT. This may be especially true for individuals with busy or stressful lives and those suffering from acute or chronic health problems that may preclude traveling to sessions and where physical symptoms may already interfere with daily functioning (Spruill et al., 2018). Also, there is a dearth of qualified MBCT facilitators. The Access MBCT website, the primary resource for finding referrals for qualified MBCT facilitators, lists only 20 individuals in the United States who have completed the training required to be a certified MBCT facilitator. Further, all facilitators reside in major metropolitan cities, thus limiting access to MBCT for populations in rural areas (Access MBCT, n.d.).
A web-based version of the in-person MBCT protocol known as Mindful Mood Balance (MMB) has recently been developed as a self-paced, nonsynchronous program that facilitates access to the same in-person MBCT content and includes individual-based phone and text coaching. MMB demonstrates potential for improving the reach of MBCT and reducing depressive symptoms and depression relapse but is associated with lower engagement compared to the in-person protocol (Dimidjian et al., 2014; Felder et al., 2017; Segal & Dimidjian et al., 2020). Also, the long-term potential for extending the reach of MBCT with the MMB program is unclear in terms of scalability, cost-effectiveness, and potential need to modernize the aesthetics of the interface over time.
A group-based telephone-delivered approach that retains human-centered interaction in “real time” may extend the reach of MBCT without compromising clinical engagement. Also, telephone-delivered interventions have no requirement for meeting high expectations for state-of-the-art interfaces that can be costly. A telephone-based platform also does not require access to high-speed Internet, thus minimizing risk for technical difficulties while maximizing reach for people with suboptimal web access (Mohr et al., 2008). A handful of studies have examined telephone-delivered versions of other mindfulness-based interventions, including mindfulness-based stress reduction (e.g., Salmoirago-Blotcher et al., 2013) and a mindfulness-based intervention for epilepsy patients with depression that targets primarily cognitive and behavioral skills (Thompson et al., 2010).
Given the prevalence of depression and strong evidence for the prevention and treatment of depression with MBCT, extending the reach and scalability of MBCT without compromising clinical engagement is a priority in the field of digital mental health. One of the ways to do this is to incorporate, in a remote-delivered platform, the approaches currently utilized during in-person clinical delivery, such as experiential learning, personal home-based practice, and using the facilitator-led inquiry and group-based discussions to normalize challenges and insights (Segal et al., 2019). With these considerations in mind, we adapted MBCT for delivery in shorter sessions (1 hour) by telephone (MBCT-T), while retaining real-time interaction to preserve the inquiry process and group-based discussions (Spruill et al., 2018). The primary aim of this study was to examine the feasibility, acceptability, safety, and preliminary efficacy of MBCT-T for reducing depressive symptoms in patients with depression and co-occurring chronic illness. A diagnosis of hypertension was used as a model comorbid and chronic condition. In secondary analyses, we examined the effects of MBCT-T on anxiety symptoms given high comorbidity with depression and increasing evidence for the effects of MBCT on anxiety (Evans et al., 2008; Hirschfeld, 2001).
Method
Participants
This trial was conducted at a large academic medical center in the Northeastern region of the United States. Participants (n = 14) were recruited from April through October 2017. Inclusion criteria were (a) age 21 or older, (b) able to speak and read English, (c) score on the Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001) consistent with mild to moderate depressive symptoms (5–14) at screening, (d) diagnosis of hypertension based on the 10th edition of International Classification of Diseases (ICD-10) criteria, and (e) no change to type or dose of antidepressant medications for at least 6 weeks prior to screening. Inclusion and exclusion criteria were developed to be consistent with other MBCT trials, which have primarily focused on depression relapse prevention in samples in remission from MDD. Thus, exclusion criteria were (a) moderately severe or severe depressive symptoms (PHQ-9 ≥ 15); (b) current substance abuse, current eating disorders, current obsessive–compulsive disorder, current anxiety disorder; (c) significant cognitive impairment; (d) active suicidal ideation or self-harm within the past 90 days; (e) history of or current diagnosis of psychosis; (f) a history of more than eight sessions of cognitive-behavioral therapy; and (g) a history of previous training in mindfulness or undergoing counseling more than once a month.
Power analyses using G-power (Faul et al., 2007) indicated that, based on large effect sizes for pre–post changes in depressive symptoms observed in prior MBCT trials, our design had 80% power to detect a large effect (Cohen’s d = 1.0) on changes in depressive symptoms, assuming a 20% attrition rate.
Procedures
All study protocols were approved by the Institutional Review Board at NYU Langone Health and procedures were carried out in accordance with the approved guidelines. Informed consent was obtained in person from all participants after meeting prescreening eligibility criteria. Prospective participants were initially identified using electronic health records based on parameters requiring an ICD-10 diagnosis of hypertension and an office visit to one of the study institution’s ambulatory care clinics in the last 6 months. Participants identified based on these criteria were sent an automated message to their MyChart account or personal e-mail with an invitation to click a link to learn more about a study on “improving mood and psychological well-being for individuals with elevated psychological distress and high blood pressure.” Participants who indicated they were interested in the study were then prescreened over the phone to determine their initial eligibility. Preliminarily eligible participants were invited to complete an in-person assessment to determine appropriateness for the group-based MBCT intervention. Eligible participants then completed a baseline assessment and a battery of online questionnaires. Finally, eligible participants completed an orientation session with the intervention facilitator where details about the treatment program and expectations for participation were explained. Participants were paid $10 for completing the initial in-person visit and $20 for the postintervention follow-up assessment, which was conducted online.
Intervention
The original, in-person MBCT treatment protocol (Segal et al., 2001) was adapted to be delivered over the telephone in an abbreviated format of 1-hour sessions over 8 weeks, instead of 2.5-hour sessions over 8 weeks. The adaptation process was led by authors A. J.S., P.D.V., and T.M.S. Full details of the adapted treatment protocol are discussed elsewhere (Spruill et al., 2018).
All MBCT-T sessions were facilitated by P.D.V., a licensed clinical psychologist and certified MBCT facilitator. The facilitator conducted a total of two MBCT-T groups; each group comprised eight participants. Prior to the start of each group, participants received a workbook containing session content, home practice logs, and audio guides to support assigned home practice. Similar to the original protocol, sessions were delivered to eight participants in a group-based format. Each weekly session was delivered using Webex, a web-based conference-call platform that incorporates administrative and technical safeguards that meet Health Insurance Portability and Accountability Act (HIPAA) requirements. Participants were provided a phone number and instructions for calling into each weekly session. The format for each weekly session included a brief check-in, teaching on the week’s topic, guided practice, inquiry, and home practice assignment. Mindfulness training includes formal (e.g., body scan, mindfulness of breath) and informal (e.g., mindfulness of daily activities) practices, and cognitive approaches, including thought monitoring, cognitive defusion, and skillful action. The final two sessions focus on developing individualized plans for sustainable daily mindfulness practice. Session topics and content areas are described in Table 1. Participants who missed sessions were provided makeup sessions with the facilitator. The time assigned for home practice between weekly sessions was approximately 15–20 minutes per day, abbreviated from approximately 50 minutes per day in MBCT. Home practice involved both formal (e.g., guided body scan, sitting meditations) and informal (e.g., mindfulness of a routine activity) practices. Formal practices were facilitated using guided audio recordings recorded by the expert facilitator.
Table 1.
MBCT-T Session Content
| Session | Topics |
|---|---|
| Orientation |
|
| 1. Awareness and Automatic Pilot |
|
| 2. Living in Our Heads |
|
| 3. Gathering the Scattered Mind |
|
| 4. Thoughts Are Not Facts |
|
| 5. Allowing and Letting Be (Part I) |
|
| 6. Allowing and Letting Be (Part II) |
|
| 7. Taking Care of Myself |
|
| 8. Maintenance |
|
Note. MBCT-T = Mindfulness-Based Cognitive Therapy—Telephone.
A rater with training in and familiarity with both the MBCT and MBCT-T protocols rated audio recordings of all 16 sessions from the two groups using an adherence scale adapted from the MBCT Adherence Scale (Segal et al., 2002), the Mindfulness-Based Interventions: Teaching Assessment Criteria (MBI:TAC; Crane et al., 2013), and the Mindfulness-Based Relapse Prevention Adherence and Competence Scale (Chawla et al., 2010). The adapted scale for MBCT-T adherence assesses both structural course components (e.g., homework review, guided exercises for each session, homework setting) and teachings imparted primarily through the inquiry process (e.g., recognizing aversion, behavioral strategies for mood regulation). Scores were calculated based on a rating of 0 (no evidence for item) to 3 (definite evidence) and were rated for each session and then averaged across the 8 weeks. The independent rater observed definite evidence (M = 3.0) for all of the course components and for each of the training goals, with the exception of moderate evidence for two teachings in Sessions 3 and 4 (M = 2.8). This yielded an overall score of 2.9, which represents strong fidelity to the protocol.
Measures
Feasibility
Feasibility was assessed by indexing session attendance (i.e., the total number of weekly sessions attended); home practice completion (i.e., number of days that all assigned home practice was completed); and study recruitment, enrollment, and attrition rates. Home practice was assessed using daily practice diaries over the 8-week intervention period. Participants returned home practice logs at the end of each week through an online form and were also given the option to scan and e-mail their logs to the study team. Study recruitment rate was operationalized as the percentage of participants enrolled from the initial pool of interested participants. Study enrollment rate was calculated based on the proportion of people who signed consent from the pool of eligible participants. Attrition rate was operationalized as the percentage of enrolled participants who failed to complete the primary outcome assessment.
Acceptability and Safety
Acceptability was assessed via self-reported satisfaction scores measured using two items. Item 1 asked participants to rate their overall satisfaction with the intervention using a 4-point Likert scale ranging from 1 (quite dissatisfied) to 4 (very satisfied). Item 2 asked participants to rate how helpful they believed the intervention was for them on a scale from 1 (not at all helpful) to 10 (very helpful). Participant safety was measured using reports from the facilitator or participants about symptomatic decline or need for additional depressive symptom management outside of the MBCT-T intervention.
Depressive Symptoms
Depression screening was conducted with the widely used PHQ-9 (Kroenke et al., 2001), which measures the frequency of depressive symptoms experienced over the past 14 days. The nine items are scored on a 4-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day). The total score ranges from 0 to 27. A score of 5–9 represents mild depressive symptoms, a score of 10–14 represents moderate depression, and a score of 15 or greater indicates moderately severe to severe depression. The PHQ-9 demonstrated acceptable internal consistency in our sample (α = .83).
Depressive symptoms as an outcome were assessed using the Quick Inventory of Depressive Symptomatology–Self-Report (QIDS-SR16; Rush et al., 2003), as this measure is highly sensitive to changes in depressive symptoms in response to treatment. Each item is scored on a scale from 0 to 3 points and references symptom domains during the prior 7 days. Total scores range from 0 to 27. Score cutoffs are 0–5 for no depression, 6–10 for mild depression, 11–15 for moderate depression, 16–20 for severe depression, and 21–27 for very severe depression. Internal consistency for pre- and postassessments was α > .62. The QIDS-SR16 has sound psychometric properties, including strong internal consistency and concurrent validity (Rush et al., 2003).
Anxiety
The Hospital Anxiety and Depression Scale—Anxiety subscale (HADS-A; Zigmond & Snaith, 1983) is validated and widely used to assess symptoms of generalized anxiety disorder during the prior 7 days in medical outpatients. The seven items are scored on a 4-point Likert scale ranging from 0 to 3. Scores between 8–10 indicate mild symptoms, 11–14 indicate moderate symptoms, and 15–21 indicate severe symptoms. Internal consistency for pre- and postassessments was α > .81.
Data Analysis
Prior to analyses, all variables were examined for extreme outliers and fit between their distributions and the assumptions of multivariate analysis. Descriptive statistics were computed for demographic and baseline characteristics. Means and standard deviations were used to characterize continuous variables and frequencies, and percentages were used for categorical variables. Paired t-tests were performed in order to determine whether MBCT-T was associated with a pre–post change in QIDS-SR16 and HADS-A scores. Cohen’s d was calculated as a measure of the effect size for t-tests. Analyses were conducted using R version 3.5 (R Core Team, 2018).
Results
Participants
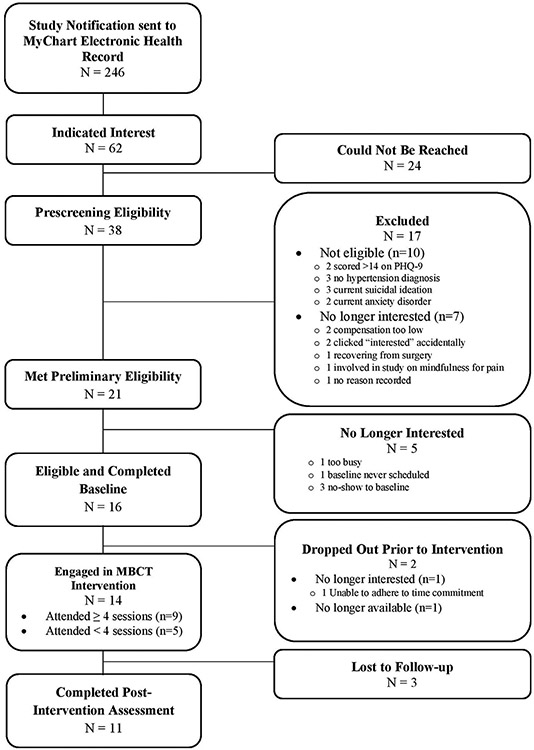
Fig. 1 presents the CONSORT diagram summarizing overall enrollment and attrition. A total of 62 potential participants indicated that they were interested in the study. A total of 38 participants were screened over the telephone. Sixteen people met preliminary eligibility criteria and completed baseline visits. Of the ineligible people, 20% had PHQ-9 scores >14, 30% did not have a hypertension diagnosis, 30% were currently experiencing suicidal ideation, and the remaining 20% had a current anxiety disorder. Following the baseline assessment, one participant was no longer interested in the study and one individual was unable to participate due to a scheduling conflict. The final enrolled sample size was 14. Of these, 11 participants (79%) completed assessments at both time points.
Fig. 1.
CONSORT diagram. Note. PHQ-9 = Patient Health Questionnaire; MBCT = Mindfulness-Based Cognitive Therapy.
Demographic characteristics of the final enrolled sample (n = 14) are described in Table 2. The mean age was 60.6 years (SD = 10.2), and the sample was comprised primarily of females (78.6%). The racial and ethnic breakdown of the sample was 35.7% non-Hispanic Black, 57.1% non-Hispanic White, 7.1% multiple races, and 14.3% multiple ethnicities. Approximately 43.0% of the sample reported a family income ≤$60,000.
Table 2.
Sociodemographic Data for All Study Participants (n = 14) Note. SD = standard deviation
| Age, mean (SD) | 60.6 (10.2) |
| Education, frequency (%) | |
| High school graduate | 1 (7.14%) |
| Partial college or specialized training | 2 (14.29%) |
| Standard college or university graduation | 3 (21.43%) |
| Graduate professional training | 8 (57.14%) |
| Income, frequency (%) | |
| $19,000 or below | 1 (7.14%) |
| $20,000–39,999 | 3 (21.43%) |
| $40,000–59,999 | 2 (14.29%) |
| $60,000–79,999 | 2 (14.29%) |
| $80,000–99,999 | 2 (14.29%) |
| $100,000 or above | 3 (21.43%) |
| Don’t know | 1 (7.14%) |
| Sex, frequency (%) | |
| Male | 3 (21.43%) |
| Female | 11 (78.57%) |
| Race, frequency (%) | |
| Black | 5 (35.71%) |
| White | 8 (57.14%) |
| Multiple races | 1 (7.14%) |
| Ethnicity, frequency (%) | |
| Not Hispanic/Latino | 11 (78.57%) |
| Multiple ethnicities | 2 (14.29%) |
| Decline to answer | 1 (7.14%) |
Feasibility
Participants attended an average of 66.0% of the sessions (mean number of sessions = 5.28). Most participants (n = 9; 64.0%) attended ≥4 of the 8 intervention sessions, the threshold for minimum effective treatment dose and “treatment completion,” as defined in prior MBCT studies (Teasdale et al., 2000). The mean number of sessions attended by the 9 treatment completers (≥4 sessions) was 7.4 sessions. Among participants who completed ≤4 sessions (36%), 1 participant attended 3 sessions and 4 participants attended 1 session. Of the 3 participants who were lost to follow-up, 2 were treatment noncompleters (attended 1 session) and 1 was a treatment completer (attended 4 sessions). Among treatment completers, 71.2% (n = 6) reported completing all assigned formal home practice and 89.2% (n = 8) reported completing all assigned informal home practice. Study recruitment rate was 22.0%. Study enrollment rate was 76.0%. Study attrition rate was 21.0%.
Acceptability and Safety
In response to the question about overall satisfaction with the intervention, all eight participants who completed the satisfaction questionnaire and who attended enough sessions to rate their satisfaction indicated that they were very (n = 6) or mostly (n = 2) satisfied with the training. Three participants indicated that they had not attended enough sessions to weigh in. Participants also reported high scores in response to the question about how helpful the intervention was (M = 7.89, SD = 3.10, range 1–10).
No adverse events were reported over the course of this trial. Neither the facilitator nor participants reported any symptomatic deterioration or need for additional safety or symptom management for any of the participants. No differences were observed in any of the feasibility and acceptability outcomes between the two separate MBCT-T groups.
Depressive and Anxiety Symptoms
Pre–post intervention changes in depressive and anxiety symptoms are presented in Table 3. Significant changes in scores on the QIDS were observed following MBCT-T: Mchange = 4.09, SD = 3.7, t(10) = 3.667, p = .004, d = 1.1. Significant changes were also observed in HADS-A scores: Mchange = 3.18, SD = 4.4, t(10) = 2.374, p = .039, d = 0.72. Improvements in depressive and anxiety symptoms did not differ between the two separate MBCT-T groups.
Table 3.
Pre–Post Intervention Changes in Depressive and Anxiety Symptoms (n = 11)
| Preintervention |
Postintervention |
Pre-post change |
|||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | t | P value | d | |
| Depressive symptoms (QIDS) | 11.73 | 3.93 | 7.64 | 3.78 | 3.667 | 0.004 | 1.1 |
| Hospital Anxiety and Depression Scale—Anxiety (HADS-A) | 10.64 | 4.03 | 7.46 | 3.98 | 2.374 | 0.039 | 0.72 |
Note. M = mean; SD = standard deviation; QIDS = Quick Inventory of Depressive Symptomatology.
Discussion
Results from this open trial offer support that an abbreviated and telephone-delivered version of MBCT (MBCT-T) is feasible, acceptable, safe, and potentially efficacious for reducing depressive and anxiety symptoms in a sample with the common comorbidity of moderately elevated depressive symptoms and hypertension. Results support that MBCT-T may be a viable intervention in primary care settings where depression is most commonly diagnosed and treated, but where few behavioral interventions are readily prescribed and accessible. Sixty-four percent of participants completed the MBCT-T intervention, defined as attending at least four of eight sessions. Formal home-based practice completion among treatment completers was over 70% and over 89% for informal practice. Overall study attrition rate was 21%. Satisfaction was high and no adverse events were reported. Significant reductions in depressive and anxiety symptoms were observed following MBCT-T.
The treatment completion rate of 64.0% in this study is higher than the average treatment completion rate of 57.4% across three trials of the MMB program, the web-based version of MBCT (Dimidjian et al., 2014; Felder et al., 2017; Segal & Dimidjian et al., 2020). One of the reasons for the superior attendance rates in the MBCT-T intervention may be due to the retention of the group-based format and live interaction with a facilitator. Mindfulness-based studies comparing in-person to self-administered or asynchronous interaction with a therapist have shown lower participation in treatment arms with minimal or no human interaction (Compen et al., 2018).
The treatment completion rate for our telephone-delivered version of MBCT is lower than in-person MBCT trials, which have completion rates as high as 85–90% in seminal studies (Kuyken et al., 2008; Williams et al., 2014). However, the majority of trials testing in-person MBCT have been conducted in the United Kingdom, where MBCT is integrated into the National Institute for Health and Care Excellence (NICE) guidelines. Thus, higher attendance may be expected given greater potential perceived efficacy and familiarity with MBCT in the United Kingdom. Differences in completion rate between in-person and telephone delivery may also reflect varying levels of engagement with in-person versus telephone delivery, with in-person providing more opportunity for connectivity with other participants and the facilitator, and also potentially greater levels of accountability.
Relatedly, participants in U.K. trials have been recruited primarily from practice-based settings and are predominately White and socioeconomically homogeneous. The MBCT-T intervention has higher feasibility (i.e., higher treatment completion rate) than at least one trial in the United States that had a 47.8% completion rate and that tested in-person MBCT in a community-based and racially, ethnically, and socioeconomically diverse sample (Shallcross et al., 2015). This supports the possibility that the telephone-delivered MBCT may be more feasible and acceptable for community-based participants with low socioeconomic resources in the United States and who have time and/or transportation challenges around attending in-person sessions.
Assigned home practice required roughly half of the time compared to the in-person MBCT protocol. Home practice completion rates between 70 and 90% for formal and informal practice were significantly higher in this study compared to online or in-person trials. Estimated pooled homework completion across >1,400 studies is 64% (Parsons et al., 2017). This points to the possibility that setting a lower threshold and expectation for practice may lead participants to evaluate this as an achievable goal, thus facilitating self-efficacy, confidence, and mastery of integrating the practices into their busy lives outside of the intervention.
The study recruitment rate of 22% (i.e., randomization of 14 eligible participants from an initial pool of 64 interested) is comparable to other studies testing similar remote-delivered interventions (Brenes et al., 2012, 2015; Carmody et al., 2013), including MMB trials (Dimidjian et al., 2014; Felder et al., 2017; Segal & Dimidjian et al., 2020). The enrollment rate of individuals who were eligible and signed consent was 76%, a respectable yield that suggests high interest in participation among individuals most suited for the treatment. Overall study attrition was 21% and compares favorably to attrition rates across other telephone-administered psychotherapy trials (Carmody et al., 2013; Ransom et al., 2008) and the online MMB program (Felder et al., 2017).
Finally, effect sizes for postintervention reductions in depressive and anxiety symptoms immediately following MBCT-T are comparable to in-person MBCT trials with a similar study design (Vøllestad et al., 2012). Thus, this study demonstrates that a remote-delivered MBCT protocol that requires less than half of the time (1hr/week, instead of 2.5 hrs/week) across eight weekly sessions reduces depressive symptoms on par with the longer, in-person version. This is significant because despite the clear benefits of the in-person MBCT intervention, particularly for relapse prevention, MBCT requires a burdensome time commitment that prevents many people who seek depression treatment from engaging with it.
Given comparable effect sizes to the in-person MBCT protocol, results from this study raise important questions about the necessary dose of MBCT and potentially other standardized mindfulness-based interventions that similarly require 2–2.5 hours/week for 8 weeks. Our findings converge with mindfulness-based stress reduction studies that demonstrate non-significant relationships between effect size and number of in-class hours (Carmody & Baer, 2009). Collectively, these results support that abbreviated formats that include fewer class hours are worthwhile for people who seek treatment for depression and for whom attending longer and in-person treatments is a barrier to their ability or willingness to participate.
In addition to an abbreviated format, the telephone-delivered option for MBCT addresses an important gap in access to treatment because MBCT is not yet widely available or accessible. Suboptimal access is due primarily to the scarcity of certified MBCT facilitators and the limited reach of MBCT that does not appear to extend beyond populations residing in metropolitan cities (Access MBCT, n.d.). Improving access to MBCT with remote delivery can extend the reach of this treatment to the nearly 20% of the U.S. population living in rural areas.
Strengths, Limitations, and Future Directions
The present study had a number of strengths. First, as the initial trial of an abbreviated and telephone-delivered version of MBCT, results have implications for improving the scalability and reach of MBCT. Second, this study serves as a proof-of-concept model for the treatment of depression with MBCT among people with chronic disease, for whom in-person depression treatment is a significant barrier. Third, this study included a more socioeconomically, racially, and ethnically diverse sample than prior MBCT trials, characterized by predominately homogeneous samples, with over 80% representation from Whites (Waldron et al., 2018). This is an important strength given disparities in mental health outcomes (Safran et al., 2009) and underrepresentation of people of color in depression treatment studies (Miranda et al., 2005). Finally, the study was methodologically rigorous in terms of intervention delivery by a certified MBCT facilitator with high treatment fidelity.
In light of these strengths, the current study must be interpreted in the context of several methodological limitations. First, the absence of a control group renders it impossible to know whether improvements in depressive and anxiety symptoms were not merely due to passage of time (e.g., natural regression to lower levels of depression and anxiety). Second, while nearly all of the reliabilities of assessments were considered acceptable (>.7), the reliability of the QIDS at postintervention was .62. Although we confirmed that our results were unchanged when dropping the item that reduced reliability below .70 (Item 11, perception of self: The degree to which I think about my defects), suboptimal reliabilities can threaten the validity of results. Third, as a feasibility study, our sample size was small and results require replication in larger samples. Relatedly, although results support promising preliminary efficacy for reductions in depressive and anxiety symptoms, and our effect sizes can still be interpreted and compared to other trials, our power was slightly lower than anticipated given that our attrition was 21% rather than 20%. Thus, conclusions must be considered in this context. Fourth, formal assessments of safety (e.g., depressive symptom deterioration and suicidal ideation) were measured before and after the MBCT-T training but were not assessed during the course of the training. Although participants were encouraged to notify the study team and/or facilitator of any need for additional psychological support, future studies, especially those with higher risk samples (e.g., patients with a history of recurrent MDD), should conduct weekly safety assessments. Finally, this study did not include a longer-term follow-up, which limits conclusions that can be drawn about the sustainability of benefits of MBCT-T for depression.
Future directions should include randomized controlled trials (RCTs) with longitudinal assessments to confirm that symptomatic improvement is due to MBCT-T, rather than the passage of time, and that effects are sustained over a longer-term follow-up period. Given the high comorbidity and bidirectional relationships between depression and hypertension, studies are needed to examine the effects of MBCT-T on blood pressure outcomes. While we anticipate findings from this study will generalize to people without hypertension, replication is needed in people with other chronic conditions that are comorbid with depression. Also needed are studies that develop and test other popular remote-delivered platforms, such as video delivery that may maximize patient engagement above and beyond a telephone-delivered platform. Efficacy studies would be useful to compare various remote-delivered platforms to one another and to in-person MBCT. Such studies should include depression relapse prevention as an outcome given that MBCT is one of the few psychological interventions for prophylactic treatment of depression, the efficacy for which is on par with that of maintenance antidepressant medication for people with recurrent MDD (Kuyken et al., 2008). If evidence for MBCT-T is found after rigorous controlled studies, evaluating the cost-effectiveness of this approach would add to our understanding of the scalability of this delivery method. This is especially important given that the abbreviated MBCT-T protocol is likely to be even less costly than in-person MBCT that, compared to treatment as usual, is a more cost-effective treatment for relapse prevention (Kuyken et al., 2008).
In sum, while future RCTs are needed to confirm the beneficial effects of MBCT-T for depressive symptom reduction and relapse prevention, results support the feasibility, acceptability, and preliminary efficacy of MBCT-T for reducing depressive symptoms in patients with hypertension. Findings support improved reach of MBCT for patients with elevated depressive symptoms and co-occurring chronic illness for whom accessing in-person treatments is either not feasible or overly burdensome. Telephone-delivered MBCT retains critical aspects of in-person MBCT (e.g., experiential practice, facilitator-led group discussion) but removes the need for brick-and-mortar establishments to hold in-person groups, improves ease of access for people with chronic illness or who may benefit from it in the comfort of their own homes, extends the geographic reach for people who do not reside in cities with qualified facilitators, and has potential cost and scalability advantages over in-person MBCT. In accordance with recommendations to ensure the “sustained relevance of MBCT” at the level of population health (Segal et al., 2019), these aspects support that telephone-delivered MBCT may be a compelling approach to improve the implementation and reach of MBCT.
Acknowledgments
This research was approved by the Institutional Review Board at NYU Langone Health. Informed consent was obtained from all individual participants. This study was supported by a National Center for Complementary and Integrative Health grant, K23AT009208, awarded to Amanda J. Shallcross.
Footnotes
The authors declare that they have no conflict of interest.
Contributor Information
Amanda J. Shallcross, New York University, School of Medicine
Zoe T. Duberstein, New York University, School of Medicine
Sarah H. Sperber, New York University, School of Medicine
Pallavi D. Visvanathan, Manhattan Center for Mindfulness-Based Cognitive Therapy
Samina Lutfeali, New York University, School of Medicine.
Nathaniel Lu, New York University, School of Medicine.
James Carmody, University of Massachusetts Medical School.
Tanya M. Spruill, New York University
References
- Abbott RA, Whear R, Rodgers LR, Bethel A, Coon JT, Kuyken W, Stein K, & Dickens C (2014). Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. Journal of Psychosomatic Research, 76(5), 341–351. [DOI] [PubMed] [Google Scholar]
- Access MBCT (n.d.). Find an MBCT therapist. (n.d.). Retrieved April 20, 2020, from https://www.accessmbct.com/find-a-mbct-therapist.html/.
- Amaral GFD, Jardim PCBV, Brasil MAA, Souza ALL, Freitas HF, Taniguchi LM, Melo AFBD, & Ribeiro CN (2007). Prevalence of major depressive disorders in a reference center for the treatment of hypertension. Revista de Psiquiatria do Rio Grande do Sul, 29(2), 161–168. [Google Scholar]
- Brenes GA, Danhauer SC, Lyles MF, Hogan PE, & Miller ME (2015). Telephone-delivered cognitive behavioral therapy and telephone-delivered nondirective supportive therapy for rural older adults with generalized anxiety disorder: A randomized clinical trial. JAMA Psychiatry, 72(10), 1012–1020. 10.1001/jamapsychiatry.2015.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes GA, Miller ME, Williamson JD, McCall WV, Knudson M, & Stanley MA (2012). A randomized controlled trial of telephone-delivered cognitive-behavioral therapy for late-life anxiety disorders. American Journal of Geriatric Psychiatry, 20 (8), 707–716. 10.1097/JGP.0b013e31822ccd3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody TP, Duncan CL, Huggins J, Solkowitz SN, Lee SK, Reyes N, Mozgai S, & Simon JA (2009). Telephone-delivered cognitive–behavioral therapy for pain management among older military veterans: A randomized trial. Psychological Services, 10(3), 265. [DOI] [PubMed] [Google Scholar]
- Carmody TP, Duncan CL, Huggins J, Solkowitz SN, Lee SK, Reyes N, Mozgai S, & Simon JA (2013). Telephone-delivered cognitive-behavioral therapy for pain management among older military veterans: A randomized trial. Psychological Services, 10(3), 265–275. 10.1037/a0030944. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2011). Vital signs: Prevalence, treatment, and control of hypertension—United States, 1999–2002 and 2005–2008. Morbidity and Mortality Weekly Report https://www.ncbi.nlm.nih.gov/pubmed/21293325. [PubMed] [Google Scholar]
- Chawla N, Collins S, Bowen S, Hsu S, Grow J, Douglass A, & Marlatt GA (2010). The mindfulness-based relapse prevention adherence and competence scale: Development, interrater reliability, and validity. Psychotherapy Research. 10.1080/10503300903544257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compen F, Bisseling E, Schellekens M, Donders R, Carlson L, van der Lee M, & Speckens A (2018). Face-to-face and Internet-based mindfulness-based cognitive therapy compared with treatment as usual in reducing psychological distress in patients with cancer: A multicenter randomized controlled trial. Journal of Clinical Oncology. 10.1200/JCO.2017.76.5669. [DOI] [PubMed] [Google Scholar]
- Crane RS, Eames C, Kuyken W, Hastings RP, Williams JMG, Bartley T, Evans A, Silverton S, Soulsby JG, & Surawy C (2013). Development and validation of the mindfulness-based interventions–teaching assessment criteria (MBI: TAC). Assessment, 20(6), 681–688. [DOI] [PubMed] [Google Scholar]
- Creswell JD (2017). Mindfulness interventions. Annual Review of Psychology. 10.1146/annurev-psych-042716-051139. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Beck A, Felder JN, Boggs JM, Gallop R, & Segal ZV (2014). Web-based mindfulness-based cognitive therapy for reducing residual depressive symptoms: An open trial and quasi-experimental comparison to propensity score matched controls. Behaviour Research and Therapy. 10.1016/j.brat.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S, Ferrando S, Findler M, Stowell C, Smart C, & Haglin D (2008). Mindfulness-based cognitive therapy for generalized anxiety disorder. Journal of Anxiety Disorders. 10.1016/j.janxdis.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Felder JN, Segal Z, Beck A, Sherwood NE, Goodman SH, Boggs J, Lemon E, & Dimidjian S (2017). An open trial of web-based mindfulness-based cognitive therapy for perinatal women at risk for depressive relapse. Cognitive and Behavioral Practice, 24(1), 26–37. [Google Scholar]
- Ferguson JM (2001). SSRI antidepressant medications: Adverse effects and tolerability. Primary Care Companion to the Journal of Clinical Psychiatry, 3(1), 22–27. 10.4088/pcc.v03n0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley E, Baillie A, Huxter M, Price M, & Sinclair E (2010). Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 10.1037/a0017566. [DOI] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, & Fawcett J (2010). Antidepressant drug effects and depression severity: A patient-level meta-analysis. JAMA, 303(1), 47–53. 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfeld RMA (2001). The comorbidity of major depression and anxiety disorders: Recognition and management in primary care. Primary Care Companion to the Journal of Clinical Psychiatry. 10.4088/pcc.v03n0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao CJ, Cherry DK, & Beatty PC (2010). National ambulatory medical care survey: 2007 summary. National Health Statistics Reports, 27. [PubMed] [Google Scholar]
- Iosifescu DV, Nierenberg AA, Alpert JE, Papakostas GI, Perlis RH, Sonawalla S, & Fava M (2004). Comorbid medical illness and relapse of major depressive disorder in the continuation phase of treatment. Psychosomatics. 10.1176/appi.psy.45.5.419. [DOI] [PubMed] [Google Scholar]
- Katon WJ (2011). Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues in Clinical Neuroscience. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181964/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, Barrett B, Byng R, Evans A, Mullan E, & Teasdale JD (2008). Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of Consulting and Clinical Psychology, 76(6), 966. [DOI] [PubMed] [Google Scholar]
- Lippi G, Montagnana M, Favaloro EJ, & Franchini M (2009). Mental depression and cardiovascular disease: A multifaceted, bidirectional association. Seminars in Thrombosis and Hemostasis. 10.1055/s-0029-1222611. [DOI] [PubMed] [Google Scholar]
- Meng L, Chen D, Yang Y, Zheng Y, & Hui R (2012). Depression increases the risk of hypertension incidence: A meta-analysis of prospective cohort studies. Journal of Hypertension, 30(5), 842–851. 10.1097/HJH.0b013e32835080b7. [DOI] [PubMed] [Google Scholar]
- Miranda J, Bernal G, Lau A, Kohn L, Hwang W-C, & LaFromboise T (2005). State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology. 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Vella L, Hart S, Heckman T, & Simon G (2008). The effect of telephone-administered psychotherapy on symptoms of depression and attrition: A meta-analysis. Clinical Psychology: Science and Practice. 10.1111/j.1468-2850.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra-Delgado M, & Latorre-Postigo JM (2013). Effectiveness of mindfulness-based cognitive therapy in the treatment of fibromyalgia: A randomised trial. Cognitive Therapy and Research. 10.1007/s10608-013-9538-z. [DOI] [Google Scholar]
- Parsons CE, Crane C, Parsons LJ, Fjorback LO, & Kuyken W (2017). Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behaviour Research and Therapy, 95(Suppl. C), 29–41. 10.1016/j.brat.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten SB, Williams JV, Lavorato DH, Campbell NR, Eliasziw M, & Campbell TS (2009). Major depression as a risk factor for high blood pressure: Epidemiologic evidence from a national longitudinal study. Psychosomatic Medicine, 71 (3), 273–279. 10.1097/PSY.0b013e3181988e5f. [DOI] [PubMed] [Google Scholar]
- Pratt LA, & Brody DJ (2014). Depression in the U.S. household population, 2009–2012. NCHS Data Brief https://www.ncbi.nlm.nih.gov/pubmed/25470183. [PubMed] [Google Scholar]
- Prins MA, Verhaak PFM, Bensing JM, & van der Meer K (2008). Health beliefs and perceived need for mental health care of anxiety and depression: The patients’ perspective explored. Clinical Psychology Review. 10.1016/j.cpr.2008.02.009. [DOI] [PubMed] [Google Scholar]
- R Core Team (2018). R: A language and environment for statistical computing. Software. Doi: ISBN 3-900051-07-0. [Google Scholar]
- Ransom D, Heckman TG, Anderson T, Garske J, Holroyd K, & Basta T (2008). Telephone-delivered, interpersonal psychotherapy for HIV-infected rural persons with depression: A pilot trial. Psychiatric Services, 59(8), 871–877. 10.1176/ps.2008.59.8.871. [DOI] [PubMed] [Google Scholar]
- Rubio-Guerra AF, Rodriguez-Lopez L, Vargas-Ayala G, Huerta-Ramirez S, Serna DC, & Lozano-Nuevo JJ (2013). Depression increases the risk for uncontrolled hypertension. Experimental and Clinical Cardiology, 18(1), 10–12 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3716493/. [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, & Thase ME (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS- C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54 (5), 573–583. [DOI] [PubMed] [Google Scholar]
- Safran MA, Mays RA Jr., Huang LN, McCuan R, Pham PK, Fisher SK, McDuffie KY, & Trachtenberg A (2009). Mental health disparities. American Journal of Public Health, 99 (11), 1962–1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmoirago-Blotcher E, Crawford SL, Carmody J, Rosenthal L, Yeh G, Stanley M, Rose K, Browning C, & Ockene IS (2013). Phone-delivered mindfulness training for patients with implantable cardioverter defibrillators: results of a pilot randomized controlled trial. Annals of Behavioral Medicine, 46 (2), 243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone RA, & Sansone LA (2012). Antidepressant adherence: Are patients taking their medications? Innovations in Clinical Neuroscience, 9(5–6), 41–46 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3398686/. [PMC free article] [PubMed] [Google Scholar]
- Segal Z, Dimidjian S, Vanderkruik R, & Levy J (2019). A maturing mindfulness-based cognitive therapy reflects on two critical issues. Current Opinion in Psychology. 10.1016/j.copsyc.2019.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Dimidjian S, Beck A, Boggs JM, Vanderkruik R, Metcalf CA, Gallop R, Felder JN, & Levy J (2020). Outcomes of online mindfulness-based cognitive therapy for patients with residual depressive symptoms: a randomized clinical trial. JAMA Psychiatry, 77(6), 563–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Teasdale JD, Williams JM, & Gemar MC (2002). The Mindfulness-Based Cognitive Therapy Adherence Scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology and Psychotherapy, 9(2), 131–138. 10.1002/cpp.320. [DOI] [Google Scholar]
- Segal ZV, Williams MG, & Teasdale JD (2001). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Guilford Press. [Google Scholar]
- Shallcross AJ, Gross JJ, Visvanathan PD, Kumar N, Palfrey A, Ford BQ, Dimidjian S, Shirk S, Holm-Denoma J, Goode KM, Cox E, & Mauss IB (2015). Relapse prevention in major depressive disorder: Mindfulness-based cognitive therapy versus an active control condition. Journal of Consulting and Clinical Psychology, 83(5). 10.1037/ccp0000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruill TM, Reynolds HR, Dickson VV, Shallcross AJ, Visvanathan PD, Park C, Kalinowski J, Zhong H, Berger JS, Hochman JS, Fishman GI, & Ogedegbe G (2018). Telephone-based mindfulness training to reduce stress in women with myocardial infarction: Rationale and design of a multicenter randomized controlled trial. American Heart Journal, 202, 61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale JD, Williams JMG, Ridgeway VA, Soulsby JM, & Lau MA (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623. 10.1037//0022-006X.68.4.615. [DOI] [PubMed] [Google Scholar]
- Thompson NJ, Walker ER, Obolensky N, Winning A, Barmon C, Diiorio C, & Compton MT (2010). Distance delivery of mindfulness-based cognitive therapy for depression: Project UPLIFT. Epilepsy and Behavior, 19(3), 247–254. 10.1016/j.yebeh.2010.07.031. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Andrade L, Borges G, Bruffaerts R, Bunting B, Almeida JMCD, Florescu S, Girolamo GD, Gureje O, Haro JM, He Y, Hinkov H, Karam E, Kawakami N, Lee S, Navarro-Mateu F, Piazza M, Posada-Villa J, Galvis YTD, & Kessler RC (2017). Undertreatment of people with major depressive disorder in 21 countries. The British Journal of Psychiatry, 210 (2), 119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tovote KA, Fleer J, Snippe E, Peeters AC, Emmelkamp PM, Sanderman R, Links TP, & Schroevers MJ (2014). Individual mindfulness-based cognitive therapy and cognitive behavior therapy for treating depressive symptoms in patients with diabetes: results of a randomized controlled trial. Diabetes Care, 37(9), 2427–2434. [DOI] [PubMed] [Google Scholar]
- Vøllestad J, Nielsen MB, & Nielsen GH (2012). Mindfulness- and acceptance-based interventions for anxiety disorders: A systematic review and meta-analysis. British Journal of Clinical Psychology. 10.1111/j.2044-8260.2011.02024.x. [DOI] [PubMed] [Google Scholar]
- Waldron EM, Hong S, Moskowitz JT, & Burnett-Zeigler I (2018). A systematic review of the demographic characteristics of participants in US-based randomized controlled trials of mindfulness-based interventions. Mindfulness. 10.1007/s12671-018-0920-5. [DOI] [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJ, Hackmann A, Krusche A, Muse K, Rohr IRV, Shah D, Crane RS, Eames C, Jones M, Radford S, Silverton S, Sun Y, Weatherley-Jones E, Whitaker CJ, Russell D, & Russell IT (2014). Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. Journal of Consulting and Clinical Psychology, 82(2), 275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]