Abstract
Background:
Although implementation of patient navigation programs in clinical practice is widespread, heterogeneity exists in the design and delivery of these services. Greater clarity is required on competencies of personnel, delineation of their roles in multidisciplinary cancer care teams, navigation service components that positively impact patient outcomes, and associated metrics.
Methods:
A national, double-blind, online survey was implemented between January 24, 2019, and April 25, 2019, to investigate care coordination for advanced (stage III/IV) non–small cell lung cancer (NSCLC). Respondents included multidisciplinary team (MDT) members, such as oncologists, pathologists, oncology nurses, advanced practice nurses, and patient navigators, from US cancer programs. Customized questions covered NSCLC screening, diagnosis, treatment, and care coordination, with a focus on oncology nurses, advanced practice nurses, and patient navigation. Descriptive statistics were computed. Subanalyses examined relationships between care delivery and outcomes such as shared decision-making (SDM) through statistical testing.
Results:
Across programs, there was a lack of patient (nurse or lay) navigators (22.3%, 101/452) to assist patients with NSCLC. Most respondents (90.1%, 100/111) worked in programs with no formal health literacy assessments. Significantly higher mean SDM scores (p < .05) were observed in programs with patient navigators compared with programs without these specialists.
Conclusion:
Patient navigation is pivotal to enhancing the patient experience along the lung cancer care continuum and should be strategically integrated within lung cancer MDTs. These findings, along with survey inputs from other MDT disciplines, can help support process improvement plans for patient-centered advanced NSCLC care delivery.
Cancer of the lung and bronchus remained the leading cause of cancerspecific mortality and was the second leading cause of newly diagnosed cancer cases in the United States in 2019 (Siegel et al., 2019). Non–small cell lung cancer (NSCLC) accounts for the majority (80%–85%) of histological confirmed cases (Howlader et al., 2019). Among these cases, diagnostic evaluation, based on histological subtypes and biomarkers, contributes to complexities in treatment-related planning and decision-making for locally advanced or metastatic disease (Bubendorf et al., 2017).
Patient-centered cancer care delivery requires multidisciplinary and coordinated efforts. Patient navigation—a patient-centered health-care service delivery model (Freeman & Rodriguez, 2011)—is defined in the cancer care setting as ‘‘individualized assistance offered to patients, families, and caregivers to help overcome health-care system barriers and facilitate timely access to quality health and psychosocial care from prediagnosis through all phases of the cancer experience” (Oncology Nursing Society et al., 2010). Both oncology nursing and patient navigation serve critical functions in cancer care planning, coordination, and delivery within multidisciplinary teams (MDTs). This includes the provision of appropriate and timely resources to patients and their caregivers, facilitation of shared decision-making (SDM), and effective implementation of treatment decisions, including assistance in the management of symptoms and adverse events, to improve patient outcomes (Oncology Nursing Society, 2016, 2017, 2019). Across cancer types, including breast, lung, and colorectal, there is added value in integrating patient navigation services as a care coordination intervention in the cancer care continuum (Gorin et al., 2017). The contributions of these professionals are manifold, and their involvement can enhance patient experience through the provision of appropriate and timely resources to overcome barriers to health system access and use (Institute of Medicine, 2013), including improvements in the timeliness of diagnosis and treatment initiation (Alsamarai et al., 2013; Hunnibell et al., 2012). One avenue is the promotion of lung cancer screening, especially among high-risk patients; assistance with procedures; and appropriate management and follow-up of lung nodules (Hunnibell et al., 2013). Through their roles, these professionals can ensure physician adherence to treatment guidelines and streamlined patient care on lung cancer tumor boards (Peckham & Mott-Coles, 2018) and support the implementation of treatment decisions to improve patient outcomes (Specchia et al., 2020). Furthermore, their engagement with patients in SDM may contribute to improved patient satisfaction (Kehl et al., 2015; Wells et al., 2018), higher perceived quality of care (Kehl et al., 2015), and improved health outcomes (Reuland et al., 2017). In addition, nurses and navigators play a vital role in communicating the importance of treatment completion and providing supportive care (Martelli-Reid et al., 2008).
Since the inception of the first patient navigation program in the US three decades ago, the implementation of such programs in clinical practice has become more widespread (Freeman, 2012). However, with this rapid expansion, heterogeneity in the design and delivery of such services has become more evident (Desveaux et al., 2019; Freund, 2017; Gorin et al., 2017). Consequently, greater clarity is required on the qualifications and competencies of personnel, delineation of their roles and functions in multidisciplinary cancer care teams, and evidence-based interventions or service components that positively impact patient outcomes (Desveaux et al., 2019; Fiscella et al., 2011; Freund, 2017; Gorin et al., 2017).
Considering these contextual factors, the Association of Community Cancer Centers (ACCC) and partner organizations sought to gain a comprehensive understanding of current practices and barriers to ideal, patient-centered NSCLC care delivery along the cancer care continuum encompassing disciplines such as medical oncology, oncology nursing, pathology, pulmonary medicine, radiation oncology, and thoracic surgery. In 2019, a multiphase initiative—Fostering Excellence in Care and Outcomes in Patients with Stage III and IV NSCLC—was implemented to identify practice-related barriers to ideal care delivery and to provide evidence-based guidance for achieving care excellence across a variety of cancer care settings. The first phase of this initiative, reported herein, included the implementation of a National Quality Survey.
The overall purpose of the survey was to understand how patients with advanced NSCLC are diagnosed and managed across US community-based cancer programs by the different disciplines that constitute lung cancer MDTs. This article focuses on the roles of oncology nurses, advanced practice nurses, and patient navigation in NSCLC care delivery, including care coordination within oncology MDTs.
METHODS
Survey Design
Under the leadership of the steering committee comprising multidisciplinary experts, a comprehensive, double-blind, online survey was developed and implemented by the ACCC and partner organizations. The survey was customized for each oncology MDT specialty, with questions encompassing screening, diagnosis, treatment, and care coordination for advanced NSCLC. Detailed methods, including the survey instrument, are reported elsewhere (Salgia et al., 2021).
Sample and Setting
Oncology MDT members, such as medical oncologists, thoracic surgeons, radiation oncologists, pulmonologists, pathologists, oncology nurses, nurse navigators, advanced practice nurses, lay navigators, pharmacists, and cancer program administrators, from a diverse group of US cancer programs participated in the survey between January 24, 2019, and April 25, 2019.
Variables
Variables specific to screening, diagnosis, treatment, and care coordination for advanced NSCLC were included. Demographic variables included profession or specialty of the survey respondent, type of affiliated cancer program, and geographical area classification (i.e., rural, urban, or suburban) of the primary cancer program.
Procedure
In addition to overall survey findings, subanalyses were performed to examine care delivery practices relevant to oncology nurses, advanced practice nurses, and patient navigation. The research questions for these subanalyses were as follows: (1) To what extent does the presence of a patient navigator (i.e., nurse or lay person) in a cancer program differ by geographical area classification and by cancer program type? (2) To what extent is the use of formal health literacy assessments associated with the presence of patient navigators in cancer programs? (3) To what extent are differences in SDM influenced by the presence of patient navigators in cancer programs? and (4) To what extent are there relationships between time to receipt of the first treatment modality and difficulty in obtaining prior authorization from health insurance companies for biomarker testing and treatment? Research question 4 was related to the provision of patient navigation to encourage timely completion of these services.
Data Analysis
Sample sizes varied by survey question owing to missing data and/or skip logic; that is, only a subset of respondents was required to answer certain survey questions. Response scales of several continuous variables, such as elements of SDM and difficulty in obtaining prior authorization, were reverse scored to allow for ease of interpretation—for example, higher scores were indicative of greater occurrence of SDM or more difficulty in obtaining prior authorization.
Descriptive statistics were computed for survey questions relevant to patient navigation. Continuous data were presented as mean ± standard deviation (SD) with minimum and maximum values; categorical data were presented as frequency (percentage). Pearson's chi-square cross tabulations were used to examine associations between the presence of nursing and navigation services in cancer programs and factors such as geographical area classification, cancer program type, and use of formal health literacy assessments. Independent samples t-test and Mann-Whitney U test were used to examine differences in SDM by the presence of patient navigators in cancer programs. Pearson's linear correlation and Spearman's rank-order correlation tests were used to assess the strength and direction of the association between time to receipt of the first treatment modality and difficulty in obtaining prior authorization from health insurance companies for biomarker testing and treatment. Parametric analyses for continuous variables with non-normal (left skewed) distributions, such as elements of SDM and difficulty in obtaining prior authorization, were supplemented with nonparametric equivalents to determine statistical significance, which was assessed at an alpha level of .05. All analyses were conducted using IBM® SPSS® Statistics for Windows, version 26.0.
RESULTS
Among 1,211 survey respondents, 639 complete responders from 160 unique cancer programs across 44 US states contributed to the overall analysis. Of these 639 respondents, 11.7% (n = 75) reported their profession as “oncology nurses, nurse navigators, or advanced practice nurses” and 5.2% (n = 33) as “financial advocates, navigators, or social workers who provide financial counseling.” Any reference to “nurse navigators” alone in this manuscript also includes oncology nurses and advanced practice nurses because these professionals were included in the survey response category; however, the sample sizes were too small for further analyses. Similarly, any reference to “lay navigators” alone also includes financial advocates and social workers. The term “patient navigators” alone is used to refer to all—oncology nurses, nurse navigators, advanced practice nurses, financial advocates, (lay) navigators, or social workers. More than half of the total respondents (54.9%, n = 351) were affiliated with cancer programs that could be categorized as “community based,” namely, Comprehensive Community Cancer Program, Community Cancer Program, Free Standing Cancer Center Program, Hospital Associate Cancer Program, and Integrated Network Cancer Program. Cancer programs were primarily located in urban (57.4%, n = 367) and suburban (32.7%, n = 209) areas.
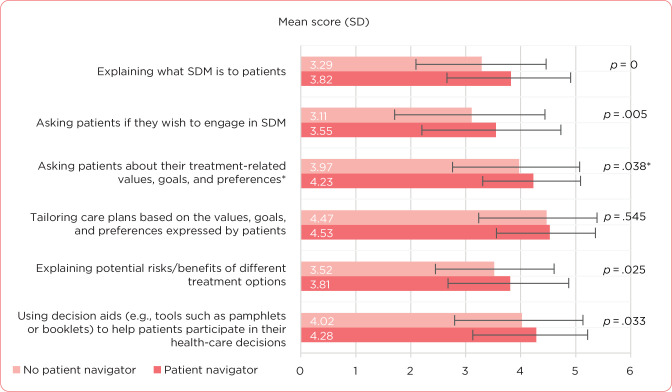
The overall survey results are presented elsewhere (Salgia et al., 2021). Across cancer programs, there was a lack of patient (i.e., nurse or lay person) navigators (22.3% of respondents, n = 101) to assist patients with NSCLC (Figure 1A). Most respondents (82.3%, n = 372) reported no provision of lay navigators in their cancer programs for patients with NSCLC (Figure 1B). Most respondents (90.1%, n = 100) also reported working in cancer programs without formal health literacy assessments for patients with NSCLC (Figure 2).
Figure 1.
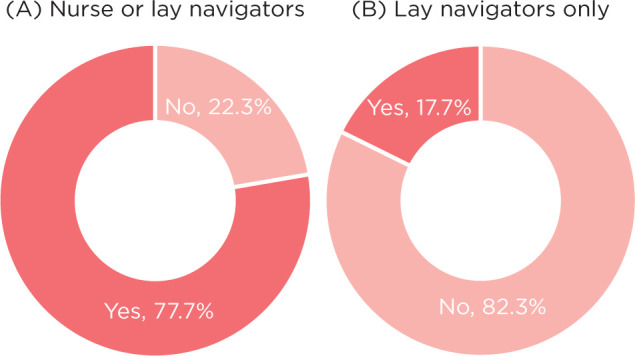
Provision of (A) nurse or lay navigators and (B) lay navigators only in affiliated cancer programs for patients with non–small cell lung cancer (N = 452). The survey question, “Indicate whether your cancer practice has nurse and/or lay navigators for patients with lung cancer,” was recoded, with a valid respondent count of 452.
Figure 2.
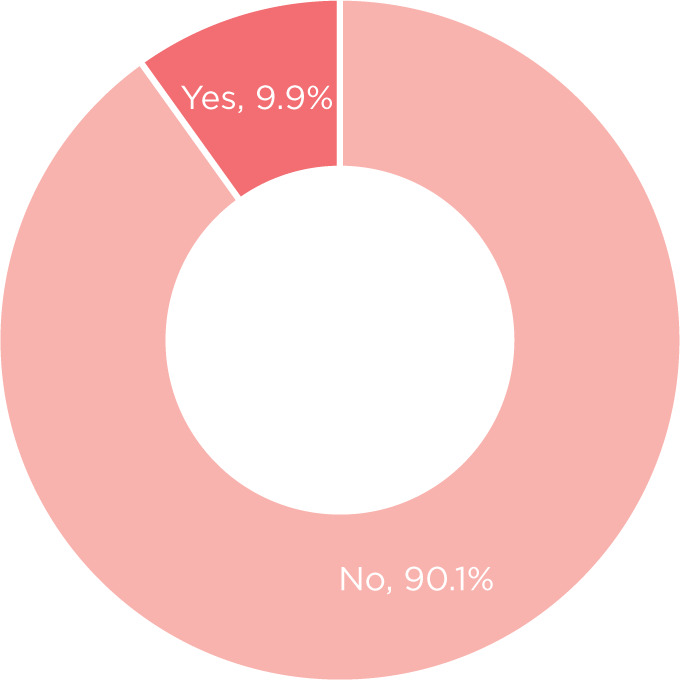
Reported use of formal health literacy assessments in affiliated cancer programs for patients with non–small cell lung cancer (N = 111). The survey question, “At your cancer practice, indicate how health literacy is assessed among patients with stage III or IV NSCLC,” was recoded, with a valid respondent count of 111.
SUBANALYSES FOR PATIENT NAVIGATION
Geographical Area Classification and Cancer Program Type
No significant associations were observed between the presence of patient navigators in a cancer program and the geographical area where the primary cancer program was located (χ2 = .985, p = .611) or the type of cancer program overall (χ2 = 12.472, p = .188; Table 1). Among the different types of cancer programs, only Integrated Network Cancer Programs were significantly more likely to not have navigators for patients with NSCLC than have navigators (7.9% vs. 3.1%, p < .05; Table 1).
Table 1. Associations Between the Presence of a Patient Navigator in a Cancer Program and Characteristics Such As Geographical Area Classification of the Cancer Program, Type of Cancer Program, and Use of Formal Health Literacy Assessments.
| Characteristics | No patient navigatora, n/N (%) | Patient navigatora, n/N (%) | p valueb |
|---|---|---|---|
| Geographical area classification of cancer programc | .611 | ||
| Urban | 62/101 (61.4) | 196/351 (55.8) | |
| Suburban | 29/101 (28.7) | 115/351 (32.8) | |
| Rural | 10/101 (9.9) | 40/351 (11.4) | |
| Type of cancer programd | .188 | ||
| Comprehensive Community Cancer Program | 13/101 (12.9) | 58/351 (16.5) | |
| Community Cancer Program | 15/101 (14.9) | 65/351 (18.5) | |
| Integrated Network Cancer Program | 8/101 (7.9) | 11/351 (3.1) | |
| Academic Comprehensive Cancer Program | 19/101 (18.8) | 50/351 (14.2) | |
| NCI-designated Comprehensive Cancer Center Program | 17/101 (16.8) | 61/351 (17.4) | |
| NCI-designated Network Cancer Program | 1/101 (1.0) | 9/351 (2.6) | |
| Veterans Affairs Cancer Program | 1/101 (1.0) | 2/351 (0.6) | |
| Hospital Associate Cancer Program | 6/101 (5.9) | 36/351 (10.3) | |
| Free Standing Cancer Center Program | 11/101 (10.9) | 20/351 (5.7) | |
| Other | 10/101 (9.9) | 39/351 (11.1) | |
| Formal health literacy assessments for patients | .492 | ||
| No | 17/18 (94.4) | 82/92 (89.1) | |
| Yes | 1/18 (5.6) | 10/92 (10.9) |
Note. NCI = National Cancer Institute.
Includes oncology nurses, nurse navigators, advanced practice nurses, financial advocates, navigators, and social workers who provide financial counseling and support patient access.
The overall p values reported for Pearson's chi-square cross tabulations.
The survey question and response options were as follows: How would you describe the region in which your main cancer practice is located? (select one) Urban (denoting a town or city), Suburban (outlying district of a city), or Rural (all other territory).
The survey question was as follows: Which of the following Commission on Cancer (CoC) cancer program categories best describe your primary cancer program affiliation? (select one).
Formal Health Literacy Assessments
No significant association was observed between the presence of patient navigators in a cancer program and the use of formal health literacy assessments for patients with NSCLC (χ2 = .472, p = .492; Table 1).
Shared Decision-Making
Based on a response scale ranging from 1 (never) to 5 (almost always), the highest overall mean scores were observed for the following: tailoring care plans based on the values, goals, and preferences expressed by patients (4.5 ± 0.8); asking patients about their treatment-related values, goals, and preferences (4.2 ± 0.9); and using decision aids (e.g., tools such as pamphlets or booklets that help patients participate in their health-care decision; 4.2 ± 1.0). Significantly higher mean scores (p < .05) were observed for most elements of SDM in cancer programs with patient navigators for those with NSCLC vs. programs without patient navigators (Figure 3). These included explaining what SDM is to patients, asking patients if they wish to engage in SDM, explaining potential risks/benefits of different treatment options, and using decision aids (Figure 3).
Figure 3.
Association between the presence of a patient navigator in a cancer program and elements of shared decision-making for patients with non–small cell lung cancer. “Patient navigator” includes oncology nurses, nurse navigators, advanced practice nurses, financial advocates, navigators, and social workers who provide financial counseling and support patient access. Higher mean scores are indicative of a greater occurrence of SDM. Error bars represent standard deviation.*t-test results did not meet the assumption of equal variances, and degrees of freedom were adjusted accordingly. p value (.082) for nonparametric testing was not statistically significant at the .05 alpha level.
Time to Receipt of First Treatment Modality and Difficulty in Obtaining Prior Authorization
From the time of the initial abnormal chest imaging study, the mean time to undergo a diagnostic procedure was 2.3 ± 1.7 weeks, the mean time to complete disease staging was 3.1 ± 1.8 weeks, and the mean time to receive the first treatment was 4.0 ± 1.8 weeks. Based on a response scale ranging from 1 (not difficult) to 3 (significantly difficult), the overall mean score for difficulty in obtaining prior authorization from health insurance companies for biomarker testing was 2.1 ± 0.6, and the overall mean score for difficulty in obtaining prior authorization from health insurance companies for scheduling the first chemotherapy or radiation therapy was 1.9 ± 0.7 for patients with stage III and stage IV NSCLC. No significant associations were observed between time to receipt of the first treatment modality and difficulty in obtaining prior authorization for biomarker testing and treatment (data not shown).
DISCUSSION
The survey successfully obtained the perspectives of different specialties serving on lung cancer MDTs in a variety of cancer care settings across the US. The survey findings provided a national baseline understanding and real-world evidence on the key challenges in patient-centered care delivery for advanced NSCLC, including those applicable to patient navigation services.
The lack of patient navigators in the surveyed cancer programs suggests that most patients are unable to benefit from individualized assistance. Patient navigation in cancer programs can positively impact patient satisfaction (Wells et al., 2018) and facilitate improved clinical resource allocation; reduce waiting times between patient referral, consultation, and treatment; and increase timely molecular testing, preferably at the time of referral (Zibrik et al., 2016). Moreover, the inclusion of patient navigation can help streamline process-related workflows across the cancer care continuum, conserve the time of other MDT members through optimal resource allocation, and in turn, alleviate concerns regarding burnout and decreased workforce resilience (National Academies of Sciences, 2018; Smith et al., 2018). One example of streamlining processes relates to biomarker testing for metastatic NSCLC (Chioda et al., 2017)—this may also ensure that pathology and biomarker testing results are available when discussing treatment options. Consequently, there is an urgent need to increase the uptake of patient navigation services. To do so, it is necessary to select appropriate personnel (i.e., professional/licensed vs. trained nonprofessional vs. volunteer) and apply standard metrics for relevant practice areas (Johnston et al., 2017).
Overall, Integrated Network Cancer Programs had a significantly lower likelihood of navigator presence for patients with NSCLC. This may be a function of the program structure (American College of Surgeons, 2020), with the emphasis on integrating different providers or facilities, and not patient-centered services, and account for “regionalized” navigation services, without consistent application of standard requirements across all facilities operating under the integrated program. Regardless, patient navigation services need to be standardized to reduce variations in care while allowing for flexibility to adapt to patients' needs. In case of institutional challenges, support may be provided through local referral or through telehealth services, such as virtual patient navigation programs (Schaffer et al., 2019).
Low usage of formal health literacy assessments was also noted, with most survey respondents reporting that clinicians spoke with patients to informally assess their level of understanding. This is concerning because a lack of formal health literacy assessments impacts the ability of patients with low health literacy levels to engage in their care and treatment decisions (Dewalt et al., 2004; National Academies of Sciences, 2020; Rudd, 2019). Greater utilization of patient navigators can help promote formal assessments, given the alignment between health literacy needs and the broader scope of patient navigation (Martinez-Donate et al., 2013; Natale-Pereira et al., 2011). These professionals can assist patients along the cancer care continuum by educating patients on MDT member roles, prioritizing questions for health-care providers, and assisting with the development of appropriate educational materials according to patients' reading levels and linguistic needs (National Academies of Sciences, 2020). Strategies include the use of plain language (National Institutes of Health, 2018a), and clear and simple health information materials, such as illustrative or audio-visual content for patients with poor reading and communication skills (National Institutes of Health, 2018b).
Cancer programs with patient navigators performed better on promoting and coordinating most elements of SDM compared with programs without these professionals. These results highlight the importance of empowering patients in the decision-making process by identifying their preferences and priorities, assisting with communicating expectations, and ensuring that available treatment options are understood (Lopez et al., 2019). Other benefits of SDM include a higher perceived quality of care vs. provider-controlled decision-making (Kehl et al., 2015), improved patient knowledge of outcomes and risks, and an increased ability of patients to make more informed value-based choices by using decision aids (Stacey et al., 2014). Therefore, increasing SDM should be prioritized, and the patient navigator can play a key role in facilitating this process.
Although respondents reported some difficulty in obtaining prior authorization, this did not have a statistically significant impact on diagnosis, disease staging, or time to first treatment for patients with advanced NSCLC. Nevertheless, patient navigators can help by encouraging timely review and completion of these steps.
Limitations
This survey had a few limitations. Although the questions passed through iterative rounds with inputs from multidisciplinary experts, the survey was not pilot tested before implementation to verify internal and external validity. All survey data were self-reported and therefore could not be verified. Additionally, the small individual sample sizes of oncology nurses, nurse navigators, and lay person navigators meant that the practices and related outcomes specific to each professional designation could not be ascertained through subanalyses.
Implications for APs
The implications for clinical practice include the need to expand and integrate patient navigation services strategically into lung cancer MDTs to ensure high-quality, patient-centered care delivery for advanced NSCLC. Although services should be tailored to the needs and preferences of patients, standardization of provider competencies is necessary to reduce ambiguity in roles and functions, and variations in care delivery. Greater utilization of patient navigation will empower patients with low health literacy levels through the implementation of formal health literacy assessments that can help tailor educational resources so that patients may participate in the decision-making process and the planning of their care.
CONCLUSION
Patient navigation plays a pivotal role in enhancing the patient experience along the lung cancer care continuum. These services should be expanded and strategically integrated within lung cancer MDTs. Moreover, practices such as SDM should be prioritized, potentially through patient navigators, to reduce the burden on other providers by assisting with patient education, assessing patients' comprehension of their diagnosis and potential therapeutic options, ensuring true informed patient consent, and substantially contributing to all aspects of SDM. Overall, these findings, together with input from other lung cancer MDT disciplines, can help in developing process improvement plans in the future to support ideal, patient-centered care delivery for advanced NSCLC.
Acknowledgment
The multiphase initiative—Fostering Excellence in Care and Outcomes in Patients with Stage III and IV NSCLC—involved the following partner organizations: the American College of Chest Physicians (CHEST), the International Association for the Study of Lung Cancer (IASLC), and LUNGevity Foundation. The authors are grateful for the contributions of the steering committee and patient advocacy partners. The steering committee comprised David Spigel as Chair and the following members: Jennifer Aversano, David Feller-Kopman, Percy Lee, Nicholas Robert, Ravi Salgia, Michelle Shiller, Mark Socinski, Alexander Spira, Brendon Stiles, Karen Van De Steeg, and Howard (Jack) West. Patient advocacy partners were Andrea Ferris and Nikki Martin of LUNGevity Foundation. The authors acknowledge Matthew Smeltzer, PhD, MStat (Division of Epidemiology, Biostatistics, and Environmental Health, School of Public Health, The University of Memphis), and Joseph Kim, MD, MPH, MBA, (Xaf Solutions), for their expert contributions to the National Quality Survey methodology. The authors also thank Elite Research, LLC, for their data analysis services. The authors thank all respondents for their participation in the National Quality Survey and their insights into the roles of oncology nurses, advanced practice nurses, and patient navigation in patient-centered care delivery for advanced NSCLC. Medical writing support was provided by Melissa Furtado, MPH, of Cactus Life Sciences (part of Cactus Communications)—this service was contracted and compensated by AstraZeneca. Although the funder was provided with an opportunity to review the content of this manuscript for medical and scientific accuracy, as well as for intellectual property considerations, the authors retained full control over the content and approved the final version of this manuscript for submission.
Footnotes
Funding for the initiative, including the National Quality Survey, was provided by AstraZeneca. The authors do not have any conflict of interest to disclose. The findings of this study specific to oncology nursing and patient navigation were selected for poster presentation at the Oncology Nursing Society's 45th Annual Congress (abstract 7765; virtual format, April 29−May 3, 2020) and the Academy of Oncology Nurse & Patient Navigators® (AONN+) Annual Conference (virtual format, November 4−8, 2020).
References
- Alsamarai, S., Yao, X., Cain, H. C., Chang, B. W., Chao, H. H., Connery, D. M.,…Rose, M. G. (2013). The effect of a lung cancer care coordination program on timeliness of care. Clinical Lung Cancer, 14(5), 527–534. 10.1016/j.cllc.2013.04.004 [DOI] [PubMed] [Google Scholar]
- American College of Surgeons. (2020). Integrated network cancer programs. https://www.facs.org/quality-programs/cancer/coc/accreditation/categories
- Bubendorf, L., Lantuejoul, S., de Langen, A. J., & Thunnissen, E. (2017). Nonsmall cell lung carcinoma: Diagnostic difficulties in small biopsies and cytological specimens. European Respiratory Review, 26(144), 170007. 10.1183/16000617.0007-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chioda, M., Jamil, A., Kaushal, S., & Ryan, J. C. (2017). Biomarker testing in metastatic non-small cell lung cancer: Process gaps and best practices reported by nurse navigators and nurse practitioners. Journal of Oncology Navigation and Survivorship, 8(11). http://www.jons-online.com/issues/2017/november-2017-vol-8-no-11?view=article&artid=1722:category-ix-clinical-researchbiomarker-testing-in-metastatic-non-small-cell-lung-cancer-process-gaps-and-best-practices-reported-by-nurse-navigators-and-nurse-practitioners [Google Scholar]
- Desveaux, L., McBrien, K., Barnieh, L., & Ivers, N. M. (2019). Mapping variation in intervention design: A systematic review to develop a program theory for patient navigator programs. Systematic Reviews, 8(1), Article 8. 10.1186/s13643-018-0920-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewalt, D. A., Berkman, N. D., Sheridan, S., Lohr, K. N., & Pignone, M. P. (2004). Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine, 19(12), 1228–1239. 10.1111/j.1525-1497.2004.40153.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella, K., Ransom, S., Jean-Pierre, P., Cella, D., Stein, K., Bauer, J. E.,…Walsh, K. (2011). Patient-reported outcome measures suitable to assessment of patient navigation [Supplemental material]. Cancer, 117(15, Suppl), 3603–3617. 10.1002/cncr.26260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman, H. P. (2012). The origin, evolution, and principles of patient navigation. Cancer Epidemiology, Biomarkers & Prevention, 21(10), 1614–1617. 10.1158/1055-9965.epi-12-0982 [DOI] [PubMed] [Google Scholar]
- Freeman, H. P., & Rodriguez, R. L. (2011). History and principles of patient navigation [Supplemental material]. Cancer, 117(15, Suppl), 3539–3542. 10.1002/cncr.26262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freund, K. M. (2017). Implementation of evidence-based patient navigation programs. Acta Oncologica, 56(2), 123–127. 10.1080/0284186x.2016.1266078 [DOI] [PubMed] [Google Scholar]
- Gorin, S. S., Haggstrom, D., Han, P. K. J., Fairfield, K. M., Krebs, P., & Clauser, S. B. (2017). Cancer care coordination: A systematic review and meta-analysis of over 30 years of empirical studies. Annals of Behavioral Medicine, 51(4), 532–546. 10.1007/s12160-0179876-2 [DOI] [PubMed] [Google Scholar]
- Howlader, N., Noone, A. M., Krapcho, M., Miller, D., Brest, A., Yu, M.,…Cronin, K. A. (Eds.). (2019). SEER Cancer Statistics Review, 1975-2016 [based on November 2018 SEER data submission, posted to the SEER website]. National Cancer Institute. https://seer.cancer.gov/csr/1975_2016/ [Google Scholar]
- Hunnibell, L. S., Rose, M. G., Connery, D. M., Grens, C. E., Hampel, J. M., Rosa, M., & Vogel, D. C. (2012). Using nurse navigation to improve timeliness of lung cancer care at a Veterans hospital. Clinical Journal of Oncology Nursing, 16(1), 29–36. 10.1188/12.cjon.29-36 [DOI] [PubMed] [Google Scholar]
- Hunnibell, L. S., Slatore, C. G., & Ballard, E. A. (2013). Foundations for lung nodule management for nurse navigators. Clinical Journal of Oncology Nursing, 17(5), 525–531. 10.1188/13.cjon.525-531 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine, Board on Health Care Services, & Committee on Improving the Quality of Cancer Care: Addressing the Challenges of an Aging Population. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis (Levit, L. A., Balogh, E. P., Nass, S. J., & Ganz, P.A., Eds.). The National Academies Press. 10.17226/18359 [DOI] [PubMed] [Google Scholar]
- Johnston, D., Sein, E., & Strusowski, T. (2017). Academy of Oncology Nurse & Patient Navigators announces standardized navigation metrics. Journal of Oncology Navigation & Survivorship, 8(2). https://www.jons-online.com/issues/2017/february-2017-vol-9-no-2/1590-academy-of-oncology-nurse-patient-navigators-announces-standardized-navigation-metrics [Google Scholar]
- Kehl, K. L., Landrum, M. B., Arora, N. K., Ganz, P. A., van Ryn, M., Mack, J. W., & Keating, N. L. (2015). Association of actual and preferred decision roles with patient-reported quality of care: Shared decision making in cancer care. JAMA Oncology, 1(1), 50–58. 10.1001/jamaoncol.2014.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez, D., Pratt-Chapman, M. L., Rohan, E. A., Sheldon, L. K., Basen-Engquist, K., Kline, R.,…Flores, E. J. (2019). Establishing effective patient navigation programs in oncology. Supportive Care in Cancer, 27(6), 1985–1996. 10.1007/s00520-019-04739-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martelli-Reid, L., Baker, S., Smith, C. A., Lacchetti, C., Ung, Y. C., & Evans, W. K. (2008). Nursing care for patients with non-small cell lung cancer receiving adjuvant chemotherapy: Evidence–based implications for practice. Canadian Oncology Nursing Journal, 18(3), 1–5. 10.5737/1181912x18315 [DOI] [Google Scholar]
- Martinez-Donate, A. P., Halverson, J., Simon, N. J., Strickland, J. S., Trentham-Dietz, A., Smith, P. D.,…Wang, X. (2013). Identifying health literacy and health system navigation needs among rural cancer patients: Findings from the Rural Oncology Literacy Enhancement Study (ROLES). Journal of Cancer Education, 28(3), 573–581. 10.1007/s13187-013-0505-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natale-Pereira, A., Enard, K. R., Nevarez, L., & Jones, L. A. (2011). The role of patient navigators in eliminating health disparities [Supplemental material]. Cancer, 117(15, Suppl), 3543–3552. 10.1002/cncr.26264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2018). Establishing effective patient navigation programs in oncology: Proceedings of a workshop. The National Academies Press. 10.17226/25073 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, National Cancer Policy Forum, Roundtable on Health Literacy, Board on Health Care Services, Zevon, E., Balogh, E., Alper, J., & Nass, S. (2020). Health literacy and communication strategies in oncology: Proceedings of a workshop. The National Academies Press. 10.17226/25664 [DOI] [PubMed] [Google Scholar]
- National Institutes of Health, Office of Communications and Public Liaison. (2018a). Clear communication: Plain language. U.S. Department of Health & Human Services. https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/plain-language [Google Scholar]
- National Institutes of Health, Office of Communications and Public Liaison. (2018b). Clear communication: Clear and simple. U.S. Department of Health & Human Services. https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/clear-simple [Google Scholar]
- Oncology Nursing Society. (2016). Oncology nurse generalist competencies. https://www.ons.org/sites/default/files/Oncology%20Nurse%20Generalist%20Competencies%202016.pdf
- Oncology Nursing Society. (2017). 2017 oncology nurse navigator core competencies. https://www.ons.org/sites/default/files/2017-05/2017_Oncology_Nurse_Navigator_Competencies.pdf
- Oncology Nursing Society. (2019). Oncology nurse practitioner competencies 2019. https://www.ons.org/sites/default/files/2019-10/2019%20ONP%20Competencies%20%282%29.pdf
- Oncology Nursing Society, Association of Oncology Social Work, & National Association of Social Workers. (2010). Oncology Nursing Society, the Association of Oncology Social Work, and the National Association of Social Workers joint position on the role of oncology nursing and oncology social work in patient navigation. Oncology Nursing Forum, 37(3), 251–252. https://onf.ons.org/onf/37/3/oncology-nursing-society-association-oncology-social-work-and-national-association-social [PubMed] [Google Scholar]
- Peckham, J., & Mott-Coles, S. (2018). Interprofessional lung cancer tumor board: The role of the oncology nurse navigator in improving adherence to national guidelines and streamlining patient care. Clinical Journal of Oncology Nursing, 22(6), 656–662. 10.1188/18.cjon.656-662 [DOI] [PubMed] [Google Scholar]
- Reuland, D. S., Brenner, A. T., Hoffman, R., McWilliams, A., Rhyne, R. L., Getrich, C.,…Pignone, M. P. (2017). Effect of combined patient decision aid and patient navigation vs usual care for colorectal cancer screening in a vulnerable patient population: A randomized clinical trial. JAMA Internal Medicine, 177(7), 967–974. 10.1001/jamainternmed.2017.1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd, R. E. (2019). Health literacy considerations for a new cancer prevention initiative [Supplemental material]. Gerontologist, 59(1, Suppl), S7–S16. 10.1093/geront/gnz032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salgia, R., Boehmer, L., Celestin, C., Yu, H., & Spigel, D. R. (2021). Improving care for patients with stage III/IV NSCLC: Learnings for multidisciplinary teams from the ACCC National Quality Survey. JCO Oncology Practice, 17(8), e112–e1130. 10.1200/OP.20.00899 [DOI] [PubMed] [Google Scholar]
- Schaffer, J., Häag, S. G., Borazanci, E. H., & Von Hoff, D. D. (2019). Oncology navigation: A virtual model to promote self-advocacy in the cancer continuum. Journal of Oncology Navigation & Survivorship, 10(1), 12–18. http://www.jons-online.com/issues/2019/january-2019-vol-10-no-1/2217-oncology-navigation-a-virtual-model-to-promote-self-advocacy-in-the-cancer-continuum [Google Scholar]
- Siegel, R. L., Miller, K. D., & Jemal, A. (2019). Cancer statistics, 2019. CA: A Cancer Journal for Clinicians, 69(1), 7–34. 10.3322/caac.21551 [DOI] [PubMed] [Google Scholar]
- Smith, C. D., Balatbat, C., Corbridge, S., Dopp, A. L., Fried, J., Harter, R.,…Sinsky, C. (2018). Implementing optimal team-based care to reduce clinician burnout. National Academy of Medicine. 10.31478/201809c [DOI] [Google Scholar]
- Specchia, M. L., Frisicale, E. M., Carini, E., Di Pilla, A., Cappa, D., Barbara, A.,…Damiani, G. (2020). The impact of tumor board on cancer care: evidence from an umbrella review. BMC Health Services Research, 20(1), Article 73. 10.1186/s12913-020-4930-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey, D., Legare, F., Col, N. F., Bennett, C. L., Barry, M. J., Eden, K. B.,…Wu, J. H. C. (2014). Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews, (1), CD001431. [DOI] [PubMed] [Google Scholar]
- Wells, K. J., Campbell, K., Kumar, A., Clark, T., & Jean-Pierre, P. (2018). Effects of patient navigation on satisfaction with cancer care: A systematic review and meta-analysis. Supportive Care in Cancer, 26(5), 1369–1382. 10.1007/s00520-018-4108-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibrik, K., Laskin, J., & Ho, C. (2016). Implementation of a lung cancer nurse navigator enhances patient care and delivery of systemic therapy at the British Columbia Cancer Agency, Vancouver. Journal of Oncology Practice, 12(3), e344–e349. 10.1200/jop.2015.008813 [DOI] [PubMed] [Google Scholar]