Abstract
The presence of preformed donor‐specific antibodies in transplant recipients increases the risk of acute antibody‐mediated rejection (AMR). Results of an open‐label single‐arm trial to evaluate the safety and efficacy of eculizumab in preventing acute AMR in recipients of deceased‐donor kidney transplants with preformed donor‐specific antibodies are reported. Participants received eculizumab as follows: 1200 mg immediately before reperfusion; 900 mg on posttransplant days 1, 7, 14, 21, and 28; and 1200 mg at weeks 5, 7, and 9. All patients received thymoglobulin induction therapy and standard maintenance immunosuppression including steroids. The primary end point was treatment failure rate, a composite of biopsy‐proved grade II/III AMR (Banff 2007 criteria), graft loss, death, or loss to follow‐up, within 9 weeks posttransplant. Eighty patients received transplants (48 women); the median age was 52 years (range 24‐70 years). Observed treatment failure rate (8.8%) was significantly lower than expected for standard care (40%; P < .001). By 9 weeks, 3 of 80 patients had experienced AMR, and 4 of 80 had experienced graft loss. At 36 months, graft and patient survival rates were 83.4% and 91.5%, respectively. Eculizumab was well tolerated and no new safety concerns were identified. Eculizumab has the potential to provide prophylaxis against injury caused by acute AMR in such patients (EudraCT 2010‐019631‐35).
Keywords: clinical research/practice, complement biology, donors and donation: deceased, immunosuppressant‐fusion proteins and monoclonal antibodies, kidney transplantation/nephrology, rejection: antibody‐mediated (ABMR), sensitization
Short abstract
In this study of terminal complement inhibition to prevent antibody‐mediated rejection in deceased‐donor kidney transplant recipients with donor‐specific antibodies, the treatment failure rate for eculizumab is low compared with the expected rate for standard of care, suggesting that terminal complement inhibition has the potential to prevent acute AMR in patients sensitized to their donors. See the companion article by Marks et al on page 2876.
Abbreviations
- AMR
antibody‐mediated rejection
- BFXM
B cell flow crossmatch
- CDC
complement‐dependent cytotoxicity
- CI
confidence interval
- DGF
delayed graft function
- DSA
donor‐specific antibody
- HLA
human leukocyte antigen
- IdeS
IgG‐degrading endopeptidase derived from Streptococcus pyogenes
- IgG
immunoglobulin G
- IVIg
intravenous immunoglobulin
- mcs
mean channel shift
- MFI
mean fluorescence intensity
- MMF
mycophenolate mofetil
- PP
plasmapheresis
- SAE
serious adverse event
- SCr
serum creatinine
- SD
standard deviation
- TAC
tacrolimus
- TEAE
treatment‐emergent adverse event
- TFXM
T cell flow crossmatch
1. INTRODUCTION
Kidney transplant is the optimal treatment for patients with end‐stage renal disease.1 However, pretransplant sensitization to donors, defined by the presence of circulating antibodies against human leukocyte antigens (HLAs), affects up to 43% of kidney transplant candidates on the transplant waitlist, and 23% of candidates are highly sensitized.2 Although antibodies against HLAs may be present in the absence of a recognized sensitizing event, sensitization is most commonly induced after blood transfusions, pregnancy, and previous organ transplant.3
The presence of preformed donor‐specific antibodies (DSAs) is a major risk factor for the development of acute and chronic antibody‐mediated rejection (AMR) after kidney transplant.4, 5, 6 The rate of acute AMR in kidney transplant recipients is reported to range between 20% and 40%, depending on multiple factors,7, 8, 9, 10, 11, 12 and is associated with a >4‐fold increase in the risk of graft loss compared with that in recipients not experiencing acute AMR.13 In patients with preformed DSAs, acute AMR most commonly occurs within 2 to 3 months posttransplant14, 15 but often occurs within the first 2 weeks.16 Importantly, in addition to the risk of acute graft loss, patients who develop acute AMR are at a much greater risk of experiencing subsequent chronic AMR and late graft loss than are those who do not develop acute AMR.4, 8, 11, 16, 17
Acute AMR occurs frequently in highly sensitized patients. As reported in a study by Burns et al, acute AMR occurred in 39% of a cohort of patients with high levels of preformed DSA (defined as having T cell flow crossmatch [TFXM] or B cell flow crossmatch [BFXM] channel shift ≥300 mean channel shift [mcs]).7 Because of the increased risk of developing acute AMR and the lack of a safe and effective treatment, such highly sensitized patients are frequently denied access to transplant.18, 19, 20 These patients face prolonged wait times for transplant and are disproportionately represented on transplant waitlists.20 As described by Jordan et al, the financial and emotional costs of maintaining highly sensitized transplant candidates on dialysis for years are extremely high, and these patients experience low quality of life and high mortality while waiting for transplant.1, 2, 4, 20
Activation of the terminal complement system through the classic pathway is thought to be responsible for many of the manifestations of acute AMR. Terminal complement products damage the capillary vascular endothelium directly through the C5b9 membrane attack complex and indirectly initiate intense, local, acute inflammatory responses through the actions of C5a, the most potent anaphylatoxin in the body.21
Eculizumab is a humanized monoclonal anti‐C5 antibody that blocks the cleavage of complement component C5 and thereby inhibits the formation of terminal complement products. In a rat model of acute AMR after kidney transplant, terminal complement blockade preserved kidney allograft function and resulted in statistically significantly longer survival than in recipients who did not receive C5 blockade.22
Clinical experience of using eculizumab for the treatment and prevention of acute AMR has had mixed results.23, 24, 25 In a single‐center study, eculizumab lowered the incidence of acute AMR in the first 3 months posttransplant in living‐donor kidney recipients who were sensitized to their donor compared with a well‐matched historical control group (7.7% [2 of 26] and 41.2% [21 of 51], respectively; P = .0031).26 In a related study at the same center, there were no significant differences in C4d score, chronic glomerulopathy score, or peritubular capillaritis between the eculizumab and control groups at 12 months.27 Together, these findings suggest that eculizumab may be clinically important in preventing acute AMR in the first days to weeks posttransplant.
The objective of this study was to evaluate the safety and efficacy of eculizumab for the prevention of acute AMR, and its effect on patient and graft survival, in individuals with preformed DSAs after deceased‐donor kidney transplant.
2. MATERIALS AND METHODS
2.1. Study design
This was an open‐label single‐arm multicenter, international, phase 2 study to evaluate the safety and efficacy of eculizumab (Soliris®, Alexion Pharmaceuticals, Inc., Boston, MA) for the prevention of acute AMR occurring within the first 9 weeks posttransplant in sensitized recipients of a deceased‐donor kidney transplant. The incidence of biopsy‐proved acute AMR, graft loss, death, or loss to follow‐up (without other events that contributed to the composite end point) within the first 9 weeks posttransplant was recorded to generate a composite treatment failure rate. The results presented focus on the first 12 months and the 36‐month safety follow‐up period.
The study (EudraCT number 2010‐019631‐35; ClinicalTrials.gov identifier NCT01567085) was conducted in accordance with the Declaration of Helsinki, and the study protocol (C10‐002) was approved by the appropriate ethics committee for each study site (Table S1). Participants provided written informed consent before study entry. The study was sponsored by Alexion Pharmaceuticals. The study design is illustrated in Figure 1.
Figure 1.
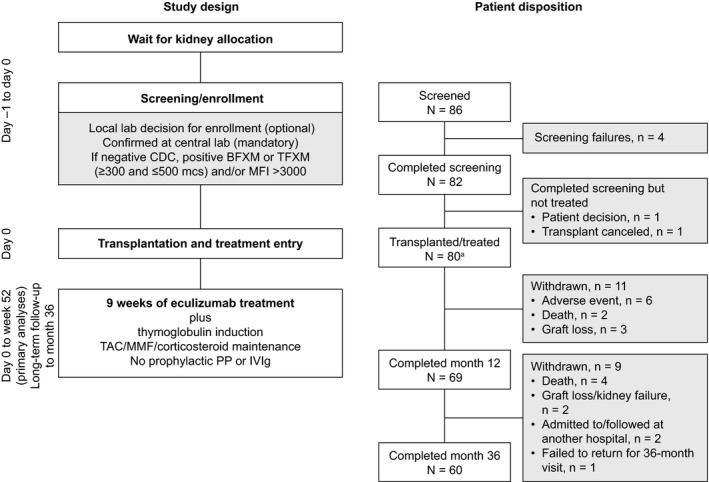
Single‐arm, open‐label study design and patient disposition. aAll patients transplanted/treated were analyzed. BFXM, B cell flow crossmatch; CDC, complement‐dependent cytotoxicity; IVIg, intravenous immunoglobulin; mcs, mean channel shift; MFI, mean fluorescence intensity; MMF, mycophenolate mofetil; PP, plasmapheresis; TAC, tacrolimus; TFXM, T cell flow crossmatch
Because of the association between terminal complement inhibition and Neisseria meningitidis infection, patients were required to be vaccinated against N. meningitidis at least 14 days before receiving the first dose of eculizumab or to be vaccinated at the time of transplant and receive prophylaxis with an appropriate antibiotic for 14 days after the vaccination.
All patients received antithymocyte globulin (Thymoglobulin, Sanofi Genzyme, Cambridge, MA) induction therapy (recommended total dose, 6 mg/kg) and prophylactic anti‐infective medications, according to local standard practice. A maintenance immunosuppression schedule was recommended, but its modification was permitted if it was not tolerated, although no calcineurin inhibitor avoidance or withdrawal, or steroid‐free protocols were allowed. Concomitant medications were administered to recipients according to the local institution's protocols. Eculizumab (1200 mg) was administered intravenously approximately 1 hour before reperfusion of the allograft (day 0) with subsequent doses according to the following regimen: 900 mg on posttransplant days 1, 7, 14 (± 2 days), 21 (± 2 days), and 28 (± 2 days) and 1200 mg during posttransplant weeks 5 (± 2 days), 7 (± 2 days), and 9 (± 2 days).
No plasmapheresis (PP) or intravenous immunoglobulin (IVIg) was administered during the first 9 weeks posttransplant unless biopsy‐proved AMR was diagnosed. Any patient diagnosed by using local pathology with clinically relevant acute AMR of any stage during this period was initially treated with PP and/or IVIg. If patients were diagnosed with acute AMR after the initial 9‐week eculizumab regimen, they were permitted to receive further treatment with eculizumab for up to 9 weeks (minimum of 5 weeks), at the discretion of the primary investigator. To maintain therapeutic eculizumab levels, patients who were treated for acute AMR with PP or fresh‐frozen plasma received supplemental eculizumab (600 mg) within 1 hour after each PP session and at least 1 hour before its infusion, respectively.
Protocol‐specified biopsies were performed during surgery postreperfusion, at day 14, month 3, and month 12 posttransplant. “For‐cause” kidney biopsies were defined as those obtained owing to clinical signs of allograft dysfunction based on at least 1 of the following criteria, with or without elevation of DSAs from baseline (day 0; ie, day of transplant): a decrease from day 0 of <10% in serum creatinine (SCr) for 3 consecutive days in the first week posttransplant; an increase in SCr; oliguria; clinical suspicion of acute AMR or delayed graft function (DGF); or proteinuria. In addition, biopsies performed for other specified reasons were reviewed by the medical monitor to determine if they should also be classified as biopsies performed “for cause.” All protocol‐specified and “for‐cause” kidney biopsy specimens were processed and analyzed by the investigating site's local pathologists. Their analyses are referred to as local pathology and were used to guide clinical management. Digitized images (Biomedical Systems, Maryland Heights, MO) of whole slides from local pathology were presented to a panel of 3 independent pathologists (2 primary readers and 1 adjudicator) with expertise in AMR histopathology. Their analyses are herein referred to as central pathology. DSA analyses were also performed by both local and central laboratories.
2.2. Study population
Patients were recruited from 15 sites in 6 countries across Europe and Australia (Table S2). Patients aged 18 years or older were eligible for inclusion if they had stage V chronic kidney disease and were identified to receive a kidney transplant from a deceased donor to whom they were sensitized. Eligible patients had a history of previous exposure to HLA, and were required to have a negative complement‐dependent cytotoxicity (CDC) assay at the time of transplant plus 1 or more of the following: historical positive CDC crossmatch, BFXM or TFXM of ≥300 and ≤500 mcs,7 or DSAs identified by single antigen bead assay (Luminex Labscreen assay) with a single mean fluorescence intensity >3000 at <3 months pretransplant.5
2.3. Primary efficacy end point
The primary efficacy end point was the treatment failure rate within 9 weeks posttransplant. This was a composite end point defined as the occurrence of any 1 of the following: biopsy‐proved acute AMR (Banff 2007 criteria grades II/III28); graft loss; patient death; or loss to follow‐up (ie, discontinuation for any reason but without other events that contributed to the composite endpoint).
Local pathological diagnoses of AMR, local laboratory analyses for DSAs, and clinical evidence of graft dysfunction were used to guide treatment. For determination of the primary end point, diagnosis of acute AMR was based solely on the review of “for‐cause” kidney biopsy specimens performed by the central pathologists according to Banff 2007 criteria for grades II and III acute AMR. Grade I acute AMR was not included in the primary end point because of differences in clinical practice in diagnosing and treating grade I AMR at the time this study was initiated. AMR was therefore defined as circulating DSAs and morphologic evidence of acute tissue injury, including the presence of C4d‐positive immunoperoxidase staining.28 For grade II AMR, this injury could be capillary and/or glomerular inflammation (peritubular capillaritis/glomurilits >0) and/or thromboses. For grade III AMR, the injury could be arterial (v3 intimal arteritis score). C4d‐negative AMR was not included in the endpoint (it was not a recognized Banff category at the time of trial design).
2.4. Patient and graft survival
Graft and patient survival at 6 and 12 months posttransplant were secondary end points for this study; 36‐month survival was also recorded. Patient survival was defined as time from transplant until date of death. Patients were censored if they discontinued or were lost to follow‐up. Graft survival was defined as time from transplant until date of death or date of graft loss. Kaplan‐Meier methods were used for all survival estimates.29
2.5. Other secondary efficacy end points
Additional secondary end points included treatment failure rate (as defined earlier) at 12 months posttransplant; cumulative number of PP treatments up to 12 months posttransplant; cumulative incidence of patients requiring splenectomy up to 12 months posttransplant; incidence of DGF posttransplant (defined as the requirement for dialysis within the first week posttransplant for reasons other than postoperative hyperkalemia, acute pulmonary edema, or fluid overload due to comorbid conditions); cumulative incidence and duration of dialysis after day 7 through month 12 posttransplant; and number of days that SCr was >30% above nadir (lowest level during the first week posttransplant) after acute AMR diagnosis.
2.6. Safety end points
Safety end points were evaluated throughout the study and at up to 36 months posttransplant. Safety assessments included recording and monitoring all treatment‐emergent adverse events (TEAEs) and serious adverse events. The cumulative incidence of biopsy‐proved acute cellular rejection was recorded.
2.7. Statistical methods
The null hypothesis was that the true treatment failure rate within the first 9 weeks posttransplant with standard of care in this population was expected to be 40%. This failure rate was derived from a pooled analysis of AMR data obtained from the literature:8, 9, 10, 11, 12 using a random‐effects model, the background rate of AMR was calculated to be 34.8% (random‐effects confidence interval [CI] 26.3% to 44.3%). This was conservatively increased to the expected treatment failure rate of 40% to account for the other end point components (graft loss, death, and loss to follow‐up, which may be unrelated to AMR). The null hypothesis was tested by using the exact binomial test. Sample size was determined based on a 2‐sided 5% level of significance, the null hypothesis, and an alternative hypothesis of composite end point treatment failure rate of 20% at 9 weeks posttransplant with eculizumab. The sample size of 80 gave a power of >90%. All statistical analyses were performed by using the SAS statistical software system version 9.4 (SAS Institute, Cary, NC).
2.8. Analyses
Efficacy and safety analyses were conducted by using data from all enrolled patients who received a deceased‐donor kidney transplant and at least 1 dose of eculizumab. Owing to the small number of patients expected to enroll at each center, all summaries and analyses were performed by using data pooled across centers.
3. RESULTS
3.1. Patient disposition and characteristics
Eighty‐six patients were screened for study inclusion; 80 eligible patients were enrolled and received a deceased‐donor kidney plus at least 1 dose of eculizumab. Seventy‐six patients completed all 9 weeks of the eculizumab treatment regimen (Figure 1). Sixty percent of recipients were women, and all patients were dialysis‐dependent at time of transplant (mean duration [range], 162.2 [6‐510] months; recipient and donor characteristics are shown in Table 1). Patients’ DSA information is displayed in Table 2. The median organ cold ischemia time was 968.5 minutes (Table S3).
Table 1.
Baseline characteristics for donors and recipients
| Characteristic | Recipients (N = 80) | Donors (N = 80) |
|---|---|---|
| Age (y), median (range) | 52.0 (24‐70) | 51.5 (18‐75) |
| Women, n (%) | 48 (60.0) | 39 (48.8) |
| Race, n (%) | ||
| Asian | 5 (6.3) | 0 (0.0) |
| Black or African American | 7 (8.8) | 1 (1.3) |
| White | 59 (73.8) | 29 (36.3) |
| Other | 9 (11.3) | 2 (2.5) |
| Unknown | 0 (0.0) | 48 (60.0) |
| Recipient characteristics | ||
| Duration of end‐stage renal disease before transplant (mo), mean (SD) | 197.0 (141.72) | |
| Patients on dialysis at time of transplant, n (%) | 80 (100.0) | |
| Duration of dialysis (mo), mean (SD) | 162.2 (124.90) | |
| Donor characteristics | ||
| Donor type, n (%) | ||
| Standard criteria donor | 58 (72.5) | |
| Expanded criteria donor | 17 (21.3) | |
| Donation after cardiac death | 5 (6.3) | |
Table 2.
Summary of DSA information for treated patients
| Recipient DSAa | Baseline (N = 80) |
|---|---|
| DSA overall (class I/II), n = 71b | |
| Highest single DSA (MFI), median (range) | 5072.0 (590‐23 365) |
| Total DSA (MFI), median (range) | 8159.0 (590‐42 903) |
| Total number of DSA, median (range) | 2.0 (1‐6) |
| Class I, n = 58 | |
| Highest single DSA (MFI), median (range) | 4410.5 (590‐23 365) |
| Total DSA (MFI), median (range) | 5854.0 (590‐37 161) |
| Total number of DSA, median (range) | 1.0 (1‐4) |
| Class II, n = 43 | |
| Highest single DSA (MFI), median (range) | 4290.0 (779‐18 126) |
| Total DSA (MFI), median (range) | 4654.0 (779‐28 753) |
| Total number of DSA, median (range) | 1.0 (1‐4) |
DSA, donor‐specific antibody; MFI, mean fluorescence intensity.
Central laboratory data were confirmatory only and are included for consistency; local laboratory data and historical data were used to evaluate patient eligibility; N = 79 for this variable.
Eight patients had no DSAs at transplant but were included in the study because they had a historical positive crossmatch.
3.2. Treatment outcomes
At 9 weeks posttransplant, treatment failure rate (with AMR determined by central pathology) was 8.8%, which was significantly lower than the expected failure rate of 40% for the standard of care in this population (exact binomial 95% CI 3.6% to 17.2%; P < .001). Treatment failure rate at 9 weeks posttransplant with AMR determined by local pathology was 13.8%, which was slightly higher than the failure rate determined by central pathology but still significantly lower than the expected failure rate of 40% for this population (95% CI 7.1% to 23.3%; P < .001). At 12 months posttransplant, the treatment failure rates determined by central and local pathology increased to 18.8% and 26.3%, respectively (Table 3).
Table 3.
Summary of composite end point at week 9 and month 12
| End point | Week 9 (N = 80) | Month 12 (N = 80) | ||
|---|---|---|---|---|
| Treated patients, n (%) | Exact 95% CI, P valuea | Treated patients, n (%) | Exact 95% CI | |
| Central pathology | ||||
| Treatment failure | ||||
| Yes | 7 (8.8) | 3.6‐17.2, <.001 | 15 (18.8) | 10.9‐29.0 |
| No | 73 (91.3) | 65 (81.3) | ||
| Composite end point componenta | ||||
| Biopsy‐proved acute AMRb | 3 (3.8) | 5 (6.3) | ||
| Graft loss | 4 (5.0) | 10 (12.5) | ||
| Death | 1 (1.3) | 2 (2.5) | ||
| Loss to follow‐upb | 0 (0.0) | 0 (0.0) | ||
| Local pathology | ||||
| Treatment failure | ||||
| Yes | 11 (13.8) | 7.1‐23.3, <.01 | 21 (26.3) | 17.0‐37.3 |
| No | 69 (86.3) | 59 (73.8) | ||
| Composite end point componenta | ||||
| Biopsy‐proved acute AMRb | 7 (8.8) | 12 (15.0) | ||
| Graft loss | 4 (5.0) | 10 (12.5) | ||
| Death | 1 (1.3) | 2 (2.5) | ||
| Loss to follow‐upb | 0 (0.0) | 0 (0.0) | ||
AMR, antibody‐mediated rejection; CI, confidence interval.
A patient experiencing multiple events is counted only once for the composite treatment failure rate but is counted for each end point component.
Loss to follow‐up without other events that contributed to the composite end point.
P value refers to the comparison between the observed treatment failure rate and the 40% treatment failure rate estimated for patients receiving standard of care from a literature search.
Banff 2007 grade II or grade III AMR detected in “for‐cause” biopsies.
The incidence of AMR was a key component of the treatment failure rate. The numbers of patients diagnosed with AMR, based on “for‐cause” biopsy results, within 9 weeks by central and local pathology were 3 (3.8%) and 7 (8.8%), respectively; after 12 months, these numbers increased to 5 (6.3%) and 12 (15.0%), respectively (Table 3). All cases of AMR were grade II.
3.3. Patient and graft survival
The number of graft losses increased from 4 (5.0%) by 9 weeks to 10 (12.5%) by 12 months (Table 3). Eight of these 10 graft losses occurred at 2 sites. The 4 graft losses that occurred by week 9 resulted from nonimmunologic processes: primary nonfunction (with no initial renal output in 2 patients, due to technical problems according to the principal investigators) and renal artery thrombosis (by study day 1 in 2 patients). The 6 graft losses that occurred between 9 weeks and 12 months included 3 cases of chronic rejection, 2 cases of acute AMR (1 with features of thrombotic microangiopathy), and 1 case of acute cellular rejection (Table S4). During the 3‐year study period, there were 14 graft losses. The 4 graft losses that occurred between 12 and 36 months were attributed to chronic rejection (chronic AMR in 3 cases [only preceded by biopsy‐proved acute AMR in 1 case] and chronic T cell–mediated rejection in 1 case). At 12 and 36 months, patient survival was 97.5%, and 91.5%, respectively, and graft survival was 87.4% and 83.4%, respectively (Figures 2 and S1).
Figure 2.
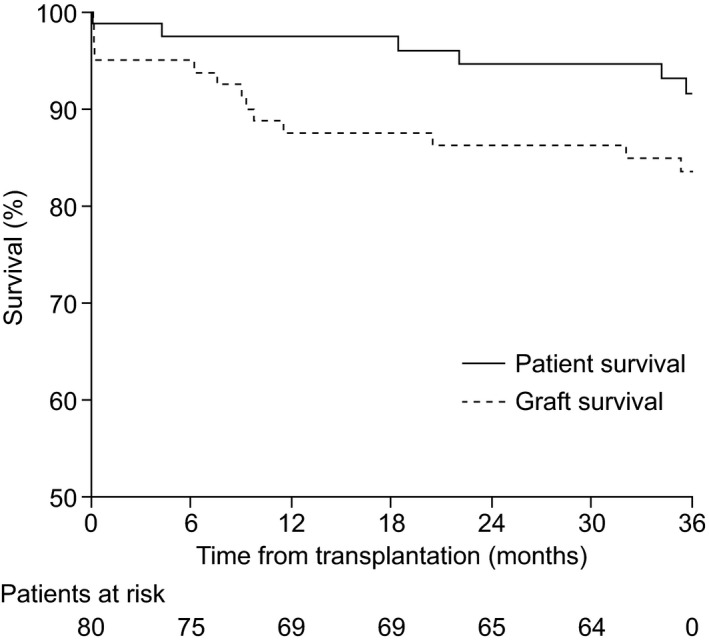
Patient and graft survival after 36 months. Patient survival was defined as time from transplantation until date of death. Patients were censored if they discontinued or were lost to follow‐up. Graft survival was defined as time from transplantation until date of death or date of graft loss. After 12 months, patient survival was 97.5%, and graft survival was 87.4%. After 36 months, patient survival was 91.5%, and graft survival was 83.4%
3.4. Other functional outcomes
The mean cumulative number of PP treatments per patient over 12 months was 2.5 (standard deviation, 7.35). Only 26.3% of patients (21 of 80) required PP by month 12 (Table 4). By the end of 12 months, 1 patient (1.3%) required splenectomy. Excluding the 4 patients who lost their grafts within the first week posttransplant, 13 of the 76 remaining patients (17.1%) experienced DGF. Excluding patients who, within the first 7 days, died, lost their graft, or had dialysis for any reason, 4 patients required dialysis within the first 12 months. Patients’ SCr levels over the course of the study are summarized in Table S5. SCr levels that were >30% above nadir for a median of 325.5 days were observed in 2 patients after a diagnosis of acute AMR. Protocol‐specified biopsy specimens at 12 months revealed chronic AMR in 1 patient and chronic T cell–mediated rejection in 1 patient (Table S6).
Table 4.
Summary of functional outcomes including plasmapheresis, dialysis, and serum creatinine
| Parameter | Summary |
|---|---|
| Cumulative number of plasmapheresis treatments, N = 80 | |
| 21 patients had ≥1 plasmapheresis treatment | |
| Day 0, mean (range) | 0.1 (0‐1) |
| Week 9, mean (range) | 1.0 (0‐18) |
| Month 12, mean (range) | 2.5 (0‐57) |
| Delayed graft functiona, N = 76 | |
| Yes, n (%) | 13 (17.1) |
| No, n (%) | 63 (82.9) |
| Cumulative incidence of the need for dialysis between day 7 and month 12, N = 48 | |
| Day 63, n (%) | 1 (2.1) |
| Day 90, n (%) | 1 (2.1) |
| Day 180, n (%) | 2 (4.2) |
| Day 364, n (%) | 4 (8.3) |
| Duration of dialysis after day 7 through month 12, N = 4 | |
| Median (range) | 9.5 (1‐64) |
| Number of dialysis treatments after day 7 through month 12, N = 4 | |
| Median (range) | 5.0 (1‐10) |
| Days of serum creatinine >30% above nadir1 after acute AMR diagnosis, N = 2 | |
| Median (range) | 325.5 (14‐637) |
AMR, antibody‐mediated rejection.
Nadir is defined as the lowest serum creatinine level within the first week posttransplant.
3.5. Safety assessments
In total, 95.0% of patients (76 of 80) received the planned 9 doses of eculizumab; administration was ceased prematurely in 4 patients (5.0%) due to graft loss or death. Twelve patients received additional doses of eculizumab after 9 weeks to treat AMR. Complete 12‐ and 36‐month data were obtained for 69 and 60 patients, respectively (Figure 1). TEAEs occurring throughout the study are presented in Tables 5 and S7. All patients experienced at least 1 TEAE. The most frequent TEAEs were anemia (63.8%), diarrhea (47.5%), and transplant rejection (including a range of immunological biopsy findings; 43.8%). During the study, 70 patients (87.5%) experienced a serious adverse event: 5 patients (6.3%) experienced a drug‐related serious adverse event, and 65 patients (81.3%) experienced a confirmed, clinically significant infection (Table 5). At 12 and 36 months, 3 and 5 patients, respectively, had experienced biopsy‐proved acute cellular rejection (Table 6).
Table 5.
Overview of TEAEs at 36 mo
| TEAEs | Treated patients (N = 80), n (%) | Number of events |
|---|---|---|
| Patients with TEAEs | ||
| Any | 80 (100.0) | 2446 |
| Drug relateda | 24 (30.0) | 83 |
| Not drug relateda | 56 (70.0) | 2363 |
| Mild | 1 (1.3) | 1441 |
| Moderate | 30 (37.5) | 847 |
| Severe | 49 (61.3) | 158 |
| Patients with SAEs (fatal and nonfatal) | ||
| Any | 70 (87.5) | 338 |
| Drug relateda | 5 (6.3) | 9 |
| Not drug relateda | 65 (81.3) | 329 |
| Patients with a confirmed clinically significant infectionb | 65 (81.3) | 354 |
| Deaths | 6 (7.5) | |
SAE, serious adverse event; TEAE, treatment‐emergent adverse event.
Drug‐related events are defined as those judged by the investigator to be possibly, probably, or definitely related to the study drug. Events that are judged by the investigator to be unlikely to be related or unrelated to study drug were defined as not drug‐related events.
Results include clinically significant for cytomegalovirus, BK virus, and encapsulated bacterial, fungal, and aspergillus infection confirmed by culture, biopsy, genomic, or serologic findings that required hospitalization or anti‐infective treatment, or otherwise deemed significant by the investigator.
Table 6.
Cumulative incidence of biopsy‐proved acute cellular rejection based on local pathology
| Time from baseline to event | Eculizumab‐treated patients (N = 80) | |||
|---|---|---|---|---|
| n (%) | CIF | SE | 95% CI | |
| Week 9 | 1 (1.3) | 0.0125 | 0.0125 | 0.00‐0.06 |
| Month 12 | 3 (3.8) | 0.0375 | 0.0214 | 0.01‐0.10 |
| Month 36 | 5 (6.3) | 0.0647 | 0.0283 | 0.02‐0.14 |
CI, confidence interval; CIF, cumulative incidence function; SE, standard error.
Acute cellular rejection of any grade that meets Banff 2007 criteria, not including borderline changes.
Competing risks include death and graft loss.
4. DISCUSSION
There is currently no definitive therapy to prevent reliably the development of acute AMR in kidney transplant recipients who are sensitized to their deceased donors. In candidates for transplant who are sensitized to their living donors, desensitization therapy is commonly used pretransplant. However, this approach cannot be used for candidates waiting to receive a deceased‐donor kidney as neither organ availability nor DSA status can be known far enough in advance of transplant to allow for desensitization therapy. Consequently, transplant is frequently considered to be contraindicated for patients highly sensitized to potential deceased donors, in order to avoid AMR.17
Reports of the use of eculizumab to treat acute AMR in recipients of solid organ transplants (including kidney) have revealed mixed results,21 but no formal trials of the use of eculizumab for treatment of acute AMR have been undertaken to date. A single‐center study by Stegall et al found that eculizumab was effective in preventing acute AMR in sensitized patients receiving kidney transplants from living donors, compared with a sequential historical control group at the same institution.26 The current study was conducted to assess the effect of eculizumab on graft and patient survival in a population of highly sensitized patients, who may not usually have been eligible for transplant because of their DSA status. They were therefore expected to be at a high risk of developing acute AMR under the current standard of care for posttransplant management and had been on long‐term dialysis. The objective was to determine the efficacy and safety of eculizumab to prevent acute AMR from occurring in this unique patient population.
In this study, the proportion of recipients who experienced treatment failure within 9 weeks of kidney transplant (8.8%) was significantly lower than the expected rate of treatment failure (40%) for patients receiving standard of care according to the null hypothesis derived from published data. As expected, the incidence of AMR decreased after the first 9 weeks. Interestingly, the treatment failure rate reported here in deceased‐donor kidney recipients is similar to that observed in the eculizumab arm of a phase 2, randomized controlled study in living‐donor transplant recipients (9.8%).30
Graft loss was a significant contributor to the outcome of this study. In total, 14 patients lost their transplanted kidneys during the study. It is noteworthy that 9 of these graft losses occurred at 2 institutions, which may have influenced the overall interpretation of the data. Nonimmunological causes of graft loss (primary nonfunction attributed to technical complications by the principal investigator in 2 cases and renal artery thrombosis in 2 cases) at these 2 institutions accounted for all 4 treatment failures that occurred within the first 9 weeks after transplant. Only 2 of the 10 graft losses that occurred after week 9 were due to acute AMR. Patient and graft survival rates after 3 years (91.5% and 83.4%, respectively) were favorable considering the long duration of pretransplant dialysis in these patients, which is known to be a strong risk factor for poor renal transplant outcomes.31 Key secondary outcomes (requirement of dialysis, splenectomy, or PP, or incidence of cellular rejection) were consistent with results expected in nonsensitized patients.
The incidence of adverse events, including infections, was consistent with the expected incidence for a highly sensitized population of patients with stage V chronic kidney disease receiving high doses of immunosuppressant agents.32, 33, 34, 35, 36, 37, 38, 39 No new safety signals for eculizumab were detected. The safety profile was consistent with that reported for eculizumab's use for approved indications, including atypical hemolytic uremic syndrome40, 41 and paroxysmal nocturnal hemoglobinuria.42
There are few published reports of desensitization of the sensitized recipients of deceased‐donor kidney transplants. In a study investigating the effectiveness of 4 weeks of desensitization with IVIg and rituximab, only 6 highly sensitized patients received deceased‐donor kidney transplants and survived for 12 months,43 compared with 70 sensitized patients in this study. Recently Jordan et al reported that administration of IdeS, an IgG‐degrading endopeptidase derived from Streptococcus pyogenes, 4 to 6 hours before transplant facilitated successful deceased‐donor kidney transplant in 25 highly sensitized patients.44 However, antibody rebound occurred, and histological evidence of AMR was identified in 40% of these patients within 5 months posttransplant compared with 6.3% of eculizumab‐treated patients within 12 months in this study. Administration of an agent that can prevent acute AMR could potentially improve outcomes in patients treated with IdeS.
Key limitations of this study include the single‐arm design. Estimates for key outcomes were derived from limited existing literature. Another limitation is the use of central pathology biopsy assessment without clinical information or inclusion of clinically relevant grade I AMR to diagnose AMR for primary end point determination. Local pathology, used to guide patient management and therefore including clinically relevant acute AMR of any stage, reported a higher rate of AMR diagnosis, which was based on both biopsy and clinical information. Discordance in Banff classification between pathologists has been reported previously45 and was investigated in a study of eculizumab in living‐donor kidney transplant recipients.30 In addition, differences in patient populations and deceased‐donor transplant practices between transplant centers may have influenced interpretation of the data. The rate of early nonimmunologic graft loss at 2 transplant centers may have reduced the apparent effectiveness of eculizumab in this study. Further, these highly sensitized patients had a long median time on dialysis before transplant, exceeding 10 years, which put them at higher than average risk for poor transplant outcomes, including those that constituted the primary end point.46, 47 Considering this, the rate of successful transplant among them is notable.
It is unlikely that the investigator community would be willing to conduct a 2‐arm randomized controlled study comparing eculizumab with standard immunosuppression and posttransplant management of acute AMR in sensitized deceased‐donor recipients because of the potential serious risks associated with early acute AMR. Information derived from this study should therefore prove useful in the design of future studies that will be necessary to understand more fully the role of eculizumab in preventing early acute AMR in sensitized recipients of kidneys from deceased donors. In light of advances in medical knowledge since this study was designed, future studies of the effect of complement inhibition in sensitized kidney transplant recipients should evaluate end points according to Banff 2017 criteria and take into account subclinical AMR and C4d‐negative AMR. Such studies may also contribute to understanding the impact of eculizumab on other clinically important entities, such as subclinical AMR and C4d‐negative AMR.
The results of this study suggest that eculizumab administered for 9 weeks posttransplant may have the potential to prevent acute AMR (as defined in the Banff 2007 criteria28) in kidney recipients who are sensitized to their deceased donors. Importantly, no grafts were lost to acute AMR in the early posttransplant period, which adds support to the observations that, despite activation of the classical complement pathway, eculizumab may limit the clinical consequences of acute AMR soon after transplant.26, 30 In addition, this study demonstrated that prophylactic eculizumab introduced no new safety concerns in this vulnerable patient population.
This study has shown that sensitized patients, who constitute an increasing proportion of individuals on transplant waiting lists, and who may never receive a transplant and thus face a lifetime of dialysis, can be successfully transplanted using prophylactic eculizumab.
DISCLOSURES
The research was funded by Alexion Pharmaceuticals, Inc., Boston, MA. The authors of this manuscript have conflicts of interest to disclose as described by the American Journal of Transplantation. Denis Glotz has received speakers’ fees and travel support from Alexion and Sanofi. William H. Marks (retired) was an employee of Alexion Pharmaceuticals at the time that this study was conducted, and has no conflicts of interest. Graeme Russ has received fees from Astellas and Novartis. Lionel Rostaing has received speakers’ fees and travel support from Novartis, Chiesi, BMS, Sanofi and Neovii. Christophe Legendre has received speakers’ fees and travel grants from Alexion Pharmaceuticals, Astellas, CSL Behring, and Novartis. Steve Chadban has received institutional support for trial conduct from Alexion Pharmaceuticals, Astellas, MSD, and Novartis, and speakers’ fees or travel support from Alexion Pharmaceuticals, Astellas, and Novartis. Nizam Mamode has received fees from Alexion Pharmaceuticals for consultancy work and was funded/supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy's and St Thomas’ NHS Foundation Trust and King's College, London, UK. The views expressed are those of the authors and are not necessarily those of the NHS, the NIHR, or the UK Department of Health. Mary Garfield, Tristan Richard, and Bradley Dain are former employees of Alexion Pharmaceuticals. Masayo Ogawa is an employee of Alexion Pharmaceuticals. Gunnar Tufveson, Josep Grinyó, Paolo Rigotti, Lionel Couzi, Matthias Büchler, and Silvio Sandrini have no conflicts of interest.
Supporting information
ACKNOWLEDGMENTS
The authors acknowledge Ram Gudavalli (Alexion Pharmaceuticals) for statistical programming support, Judith Boice (formerly of Alexion Pharmaceuticals) for critical review of the manuscript, and Sorcha Mc Ginty and Ruth Gandolfo (Oxford PharmaGenesis, Oxford, UK) who provided medical writing assistance in the production of the manuscript (funded by Alexion Pharmaceuticals).
Glotz D, Russ G, Rostaing L, et al.; the C10‐002 Study Group . Safety and efficacy of eculizumab for the prevention of antibody‐mediated rejection after deceased-donor kidney transplantation in patients with preformed donor‐specific antibodies. Am J Transplant. 2019;19:2865‐2875. 10.1111/ajt.15397
Footnotes
Delayed graft function is defined as the requirement for dialysis within the first week posttransplant for reasons other than postoperative hyperkalemia, acute pulmonary edema, or fluid overload due to comorbid conditions.
Contributor Information
Denis Glotz, Email: denis.glotz@aphp.fr.
the C10‐002 Study Group:
Pierre Merville, Yvon Lebranchu, Lars Mjörnstedt, Peter Hughes, Nicholas Torpey, and Nassim Kamar
DATA AVAILABILITY STATEMENT
Qualified academic investigators may request participant‐level, deidentified clinical data and supporting documents (statistical analysis plan and protocol) pertaining to this study. Further details regarding data availability, instructions for requesting information and our data disclosure policy will be available on the Alexion.com website (http://alexion.com/research-development).
REFERENCES
- 1. Abecassis M, Bartlett ST, Collins AJ, et al. Kidney transplantation as primary therapy for end‐stage renal disease: a National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQI™) conference. Clin J Am Soc Nephrol. 2008;3(2):471‐480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pruthi R, Hilton R, Pankhurst L, et al. UK Renal Registry 16th annual report: chapter 4 demography of patients waitlisted for renal transplantation in the UK: national and centre‐specific analyses. Nephron Clin Pract. 2013;125(1‐4):81‐98. [DOI] [PubMed] [Google Scholar]
- 3. Butler CL, Valenzuela NM, Thomas KA, Reed EF. Not all antibodies are created equal: factors that influence antibody mediated rejection. J Immunol Res. 2017;2017:7903471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dunn TB, Noreen H, Gillingham K, et al. Revisiting traditional risk factors for rejection and graft loss after kidney transplantation. Am J Transplant. 2011;11(10):2132‐2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lefaucheur C, Loupy A, Hill GS, et al. Preexisting donor‐specific HLA antibodies predict outcome in kidney transplantation. J Am Soc Nephrol. 2010;21(8):1398‐1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mohan S, Palanisamy A, Tsapepas D, et al. Donor‐specific antibodies adversely affect kidney allograft outcomes. J Am Soc Nephrol. 2012;23(12):2061‐2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Burns JM, Cornell LD, Perry DK, et al. Alloantibody levels and acute humoral rejection early after positive crossmatch kidney transplantation. Am J Transplant. 2008;8(12):2684‐2694. [DOI] [PubMed] [Google Scholar]
- 8. Thielke JJ, West‐Thielke PM, Herren HL, et al. Living donor kidney transplantation across positive crossmatch: the University of Illinois at Chicago experience. Transplantation. 2009;87(2):268‐273. [DOI] [PubMed] [Google Scholar]
- 9. Stegall MD, Tayyab D, Cornell DL, Burns J, Dean GP, Gloor MJ. Terminal complement inhibition decreases early acute humoral rejection in sensitized renal transplant recipients [abstract 1]. Am J Transplant. 2010;10(Suppl 4):39. [DOI] [PubMed] [Google Scholar]
- 10. Magee CC, Felgueiras J, Tinckam K, Malek S, Mah H, Tullius S. Renal transplantation in patients with positive lymphocytotoxicity crossmatches: one center's experience. Transplantation. 2008;86(1):96‐103. [DOI] [PubMed] [Google Scholar]
- 11. Stegall MD, Gloor J, Winters JL, Moore SB, Degoey S. A comparison of plasmapheresis versus high‐dose IVIG desensitization in renal allograft recipients with high levels of donor specific alloantibody. Am J Transplant. 2006;6(2):346‐351. [DOI] [PubMed] [Google Scholar]
- 12. Vo AA, Peng A, Toyoda M, et al. Use of intravenous immune globulin and rituximab for desensitization of highly HLA‐sensitized patients awaiting kidney transplantation. Transplantation. 2010;89(9):1095‐1102. [DOI] [PubMed] [Google Scholar]
- 13. Orandi BJ, Chow EH, Hsu A, et al. Quantifying renal allograft loss following early antibody‐mediated rejection. Am J Transplant. 2015;15(2):489‐498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aubert O, Loupy A, Hidalgo L, et al. Antibody‐mediated rejection due to preexisting versus de novo donor‐specific antibodies in kidney allograft recipients. J Am Soc Nephrol. 2017;28(6):1912‐1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Haas M, Mirocha J, Reinsmoen NL, et al. Differences in pathologic features and graft outcomes in antibody‐mediated rejection of renal allografts due to persistent/recurrent versus de novo donor‐specific antibodies. Kidney Int. 2017;91(3):729‐737. [DOI] [PubMed] [Google Scholar]
- 16. Schinstock C, Stegall MD. Acute antibody‐mediated rejection in renal transplantation: current clinical management. Curr Transplant Rep. 2014;1(2):78‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Djamali A, Kaufman DB, Ellis TM, Zhong W, Matas A, Samaniego M. Diagnosis and management of antibody‐mediated rejection: current status and novel approaches. Am J Transplant. 2014;14(2):255‐271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wan SS, Ying TD, Wyburn K, Roberts DM, Wyld M, Chadban SJ. The treatment of antibody‐mediated rejection in kidney transplantation: an updated systematic review and meta‐analysis. Transplantation. 2018;102(4):557‐568. [DOI] [PubMed] [Google Scholar]
- 19. Couzi L, Manook M, Perera R, et al. Difference in outcomes after antibody‐mediated rejection between ABO‐incompatible and positive cross‐match transplantations. Transpl Int. 2015;28(10):1205‐1215. [DOI] [PubMed] [Google Scholar]
- 20. Jordan SC, Vo AA, Peng A, Toyoda M, Tyan D. Intravenous gammaglobulin (IVIg): a novel approach to improve transplant rates and outcomes in highly HLA‐sensitized patients. Am J Transplant. 2006;6(3):459‐466. [DOI] [PubMed] [Google Scholar]
- 21. Cernoch M, Viklicky O. Complement in kidney transplantation. Front Med. 2017;4:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yu ZX, Qi S, Lasaro MA, et al. Targeting complement pathways during cold ischemia and reperfusion prevents delayed graft function. Am J Transplant. 2016;16(9):2589‐2597. [DOI] [PubMed] [Google Scholar]
- 23. Burbach M, Suberbielle C, Brochériou I, et al. Report of the inefficacy of eculizumab in two cases of severe antibody‐mediated rejection of renal grafts. Transplantation. 2014;98(10):1056‐1059. [DOI] [PubMed] [Google Scholar]
- 24. Eskandary F, Wahrmann M, Mühlbacher J, Böhmig GA. Complement inhibition as potential new therapy for antibody‐mediated rejection. Transpl Int. 2016;29(4):392‐402. [DOI] [PubMed] [Google Scholar]
- 25. Tran D, Boucher A, Collette S, et al. Eculizumab for the treatment of severe antibody‐mediated rejection: a case report and review of the literature. Case Rep Transplant. 2016;2016:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stegall MD, Diwan T, Raghavaiah S, et al. Terminal complement inhibition decreases antibody‐mediated rejection in sensitized renal transplant recipients. Am J Transplant. 2011;11(11):2405‐2413. [DOI] [PubMed] [Google Scholar]
- 27. Cornell LD, Schinstock CA, Gandhi MJ, Kremers WK, Stegall MD. Positive crossmatch kidney transplant recipients treated with eculizumab: outcomes beyond 1 year. Am J Transplant. 2015;15(5):1293‐1302. [DOI] [PubMed] [Google Scholar]
- 28. Solez K, Colvin RB, Racusen LC, et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant. 2008;8(4):753‐760. [DOI] [PubMed] [Google Scholar]
- 29. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457‐481. [Google Scholar]
- 30. Marks WH, Mamode N, Montgomery R, et al. Safety and efficacy of eculizumab in the prevention of antibody-mediated rejection in living-donor kidney transplant recipients requiring desensitization therapy: A randomized trial [published online ahead of print March 19, 2019]. Am J Transplant. 10.1111/ajt.15364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Meier‐Kriesche HU, Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation. 2002;74(10):1377‐1381. [DOI] [PubMed] [Google Scholar]
- 32. Abbott KC, Swanson SJ, Richter ER, et al. Late urinary tract infection after renal transplantation in the United States. Am J Kidney Dis. 2004;44(2):353‐362. [DOI] [PubMed] [Google Scholar]
- 33. Azevedo LS, Pierrotti LC, Abdala E, et al. Cytomegalovirus infection in transplant recipients. Clinics. 2015;70(7):515‐523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dörje C, Midtvedt K, Holdaas H, et al. Early versus late acute antibody‐mediated rejection in renal transplant recipients. Transplantation. 2013;96(1):79‐84. [DOI] [PubMed] [Google Scholar]
- 35. Singh N. Antifungal prophylaxis for solid organ transplant recipients: seeking clarity amidst controversy. Clin Infect Dis. 2000;31(2):545‐553. [DOI] [PubMed] [Google Scholar]
- 36. Stoumpos S, Jardine AG, Mark PB. Cardiovascular morbidity and mortality after kidney transplantation. Transpl Int. 2015;28(1):10‐21. [DOI] [PubMed] [Google Scholar]
- 37. Collins AJ, Foley RN, Chavers B, et al. US renal data system 2013 annual data report. Am J Kidney Dis. 2014;63(1 Suppl):A7. [DOI] [PubMed] [Google Scholar]
- 38. Tacrolimus [Prescribing Information]. Princeton, NJ: Sandoz Inc; 2009. [Google Scholar]
- 39. Mycophenolate Mofetil [Prescribing Information]. Columbus, OH: Roxane Laboratories Inc; 2008. [Google Scholar]
- 40. Legendre CM, Licht C, Muus P, et al. Terminal complement inhibitor eculizumab in atypical hemolytic–uremic syndrome. N Engl J Med. 2013;368(23):2169‐2181. [DOI] [PubMed] [Google Scholar]
- 41. Licht C, Greenbaum LA, Muus P, et al. Efficacy and safety of eculizumab in atypical hemolytic uremic syndrome from 2‐year extensions of phase 2 studies. Kidney Int. 2015;87(5):1061‐1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hillmen P, Young NS, Schubert J, et al. The complement inhibitor eculizumab in paroxysmal nocturnal hemoglobinuria. N Engl J Med. 2006;355(12):1233‐1243. [DOI] [PubMed] [Google Scholar]
- 43. Vo AA, Lukovsky M, Toyoda M, et al. Rituximab and intravenous immune globulin for desensitization during renal transplantation. N Engl J Med. 2008;359(3):242‐251. [DOI] [PubMed] [Google Scholar]
- 44. Jordan SC, Lorant T, Choi J, et al. IgG endopeptidase in highly sensitized patients undergoing transplantation. N Engl J Med. 2017;377(5):442‐453. [DOI] [PubMed] [Google Scholar]
- 45. Furness PN, Taub N, Convergence of European Renal Transplant Pathology Assessment Procedures P . International variation in the interpretation of renal transplant biopsies: report of the CERTPAP Project. Kidney Int. 2001;60(5):1998−2012. [DOI] [PubMed] [Google Scholar]
- 46. Rose C, Gill J, Gill JS. Association of kidney transplantation with survival in patients with long dialysis exposure. Clin J Am Soc Nephrol. 2017;12(12):2024‐2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gloor JM, Winters JL, Cornell LD, et al. Baseline donor‐specific antibody levels and outcomes in positive crossmatch kidney transplantation. Am J Transplant. 2010;10(3):582‐589. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Qualified academic investigators may request participant‐level, deidentified clinical data and supporting documents (statistical analysis plan and protocol) pertaining to this study. Further details regarding data availability, instructions for requesting information and our data disclosure policy will be available on the Alexion.com website (http://alexion.com/research-development).


