Abstract
Background:
Modified ride-on cars (MROC) are a low-cost option to provide self-directed mobility to children with mobility limitations, in lieu of or as a precursor to other powered mobility devices.
Objectives:
We appraised evidence to (1) describe and categorize MROC study characteristics, (2) synthesize existing knowledge of children’s use of MROCs and (3) frame outcomes within the International Classification of Functioning, Disability and Health (ICF) framework.
Methods:
Articles were identified through four electronic databases: Medline, CINAHL, PsycNET, and Web of Science. We included all published, peer-reviewed studies involving MROC use. Relevant data were extracted, and articles were appraised using the American Academy of Cerebral Palsy and Developmental Medicine criteria for group and single-subject designs.
Results:
23 studies met inclusion criteria of 204 titles identified from 1980 to 2021. Study designs included case studies, case series, group designs, and qualitative research, but only three studies were rated evidence level III or higher. Children with a range of disabilities used MROCs across multiple settings, including the home, hospital, and community, though use and adherence varied widely. Positive impacts were reported on a range of outcomes related to the ICF framework, with an emphasis on activity and participation.
Conclusions:
MROC studies have primarily addressed activity and participation, with most studies suggesting increased functional mobility and social interactions due to MROC use. More robust research designs with larger samples are needed in order to develop evidence-based strategies for MROC use.
Keywords: disabled children, mobility limitation, wheelchairs, play and playthings, social participation
Introduction
Self-directed mobility is mobility controlled by an individual, including (a) ambulation (e.g., crawling, walking), (b) use of non-powered technology (e.g., prosthetics, walking aids, manual wheelchairs), and (c) use of powered technology (e.g., motorized wheelchairs, battery-powered ride-on toy cars) [1]. But self-directed mobility is more than a means of moving from one place to another—mobility also supports individual function, activity, and community participation across the lifespan [2]. For children with disabilities, the introduction of powered mobility devices is associated with gains in peer interaction, communication, environmental exploration, and some cognitive processes, such as increased understanding of cause-and-effect relationships [3–7]. Growing acknowledgement of the importance of self-directed mobility over the past decade, contrasted with the relative inaccessibility of options like motorized wheelchairs for children, has increased the provision of modified ride-on cars (MROCs) to children with disabilities for engagement in self-directed mobility [2].
Rationale
MROCs are off-the-shelf, battery-operated toy cars that are fitted with a large, easy to press activation switch and additional, customized seating using common materials such as PVC pipe, foam noodles, and foam kickboards. MROCs are an affordable alternative to traditional powered mobility devices, which may not be valued, promoted, or widely utilized due to numerous access barriers. Barriers include high cost, lack of insurance coverage, poor environmental access, difficulty transporting devices, negative social stigma, and pervasive medical beliefs viewing powered mobility devices as a “last resort,” thereby discouraging families and clinicians from use [2,8]. MROCs address many of these barriers, and offer one strategy to provide mobility and play opportunities for children with disabilities [1,9]. Published technical reports, publicly available how-to guides, and online discussion forums are available to assist in the modification process (www.gbgconnect.com) [10,11]. MROCs are small, low-cost ($200–300), lightweight, and portable [12]. MROCs may offer an opportunity to facilitate self-directed mobility experiences, both in rehabilitation and in family and community life.
To date, one scoping review paper has been published on children’s MROC use. The current systematic review builds on this work and contributes new knowledge in four key ways [13]. First, 14 additional studies are included in this review. Second, this review is structured using PRISMA (Preferred Reporting Items for Systematic review and Meta-Analyses) guidelines, and uses a more rigorous set of article inclusion criteria to ensure that all included studies were peer-reviewed [14]. Finally, the current systematic review synthesizes MROC outcomes and knowledge gaps within the clinically relevant International Classification of Disability, Functioning and Health (ICF) framework; the ICF frames disability as a dynamic interaction between body structure and function, activity, and participation, influenced by environmental and personal factors, and is a useful therapeutic tool for conceptualizing the synergistic nature of human functioning.
Objectives
We conducted a systematic review with three primary aims: (1) describe and categorize study characteristics of published MROC research (with no limitations placed on interventions, comparisons, outcomes, and study design); (2) synthesize existing knowledge of children’s use of MROCs (with no limitation on the age of the child or type of disability); and (3) frame outcomes of MROC use within the context of the International Classification of Functioning, Disability and Health (ICF), a conceptual, bio-psychosocial framework for disability [15].
Materials and methods
Study design
This study is a systematic review that followed the PRISMA (Preferred Reporting Items for Systematic review and Meta-Analyses) statement [14].
Eligibility criteria
We used the following inclusion criteria: (1) included primary data collection of MROC use by children with disabilities; (2) published in peer-reviewed journals; (3) available in English to ensure accessibility to authors; and (4) published between January of 1980 and January of 2021. Consistent with our primary aims, no limits were placed on the type of MROC, the age of the child, the type of disability, or design methodology. We used the following exclusion criteria: (1) did not involve primary data collection (e.g., technical reports, reviews, perspectives, government documents, or policy statements); (2) not published in peer-reviewed journals (e.g., theses, dissertations, or conference abstracts); (3) not available in English; (4) full-text not available.
Information sources, search, and study selection
We searched four medical electronic databases: Medline, CINAHL, PsycNET, and Web of Science. We developed an initial search strategy through Medline and adapted the search strategy for the other three databases. The primary keywords were “ride on car” and “toy car” (see Supplemental Table 1 for full search strategy for each database). The search was limited to the dates specified and results were filtered to identify peer-reviewed journal articles. We purposefully kept search terms broad to enable comprehensive coverage; the relative uniqueness of the terms kept returned results to reasonable numbers. Titles and abstracts were independently reviewed by two authors (CH and SL). Full text was obtained if the abstract appeared relevant and consensus was achieved without the need to involve a third reviewer. We also performed a manual “snowball search” of the reference lists of included articles, reviewed the first ten pages of Google Scholar results, consulted a working bibliography created by a leading powered mobility researcher, and each author confirmed inclusion of relevant studies based on their knowledge of the literature.
Data collection process and data items
After assembling the final list of studies included in this review, the first author extracted theoretically and/or methodologically relevant characteristics. A data extraction form was developed iteratively in consultation with all authors. The following items were extracted by the first author, per the objectives of this review: (1) author(s), year of publication, and country of origin, (2) research design and aims/purpose, (3) study population and sample size, (4) intervention type, duration, and frequency, (5) outcomes assessed and measures used, (6) suggested use and reported use, and (7) any outcomes relevant to the ICF framework. Articles were appraised using the McMaster critical review form for quantitative studies and the SRQR for qualitative studies [16,17]. The quality of articles was assessed using the Levels of Evidence (I-V scale, I = highest evidence, V = lowest evidence) provided by the American Academy of Cerebral Palsy and Developmental Medicine (AACPDM) criteria for group and single-subject designs [18]. Studies rated as Level I-III per AACPDM criteria qualified for quality ratings; the quality of studies rated as Level IV or V were summarized using data from the McMaster quantitative review form. Qualitative studies were not eligible for review per the AACPDM criteria and were instead analysed for rigour using the Standards for Reporting Qualitative Research (SRQR) [17]. Extracted items, article appraisals, and quality ratings were reviewed by a second author; in case of disagreement, items were discussed until agreement was reached.
Synthesis of results
The heterogeneity and largely descriptive nature of identified studies precluded a quantitative synthesis and use of summary measures. Data were organized in tables and summarized narratively to synthesize findings to the extent possible.
Results
Study selection
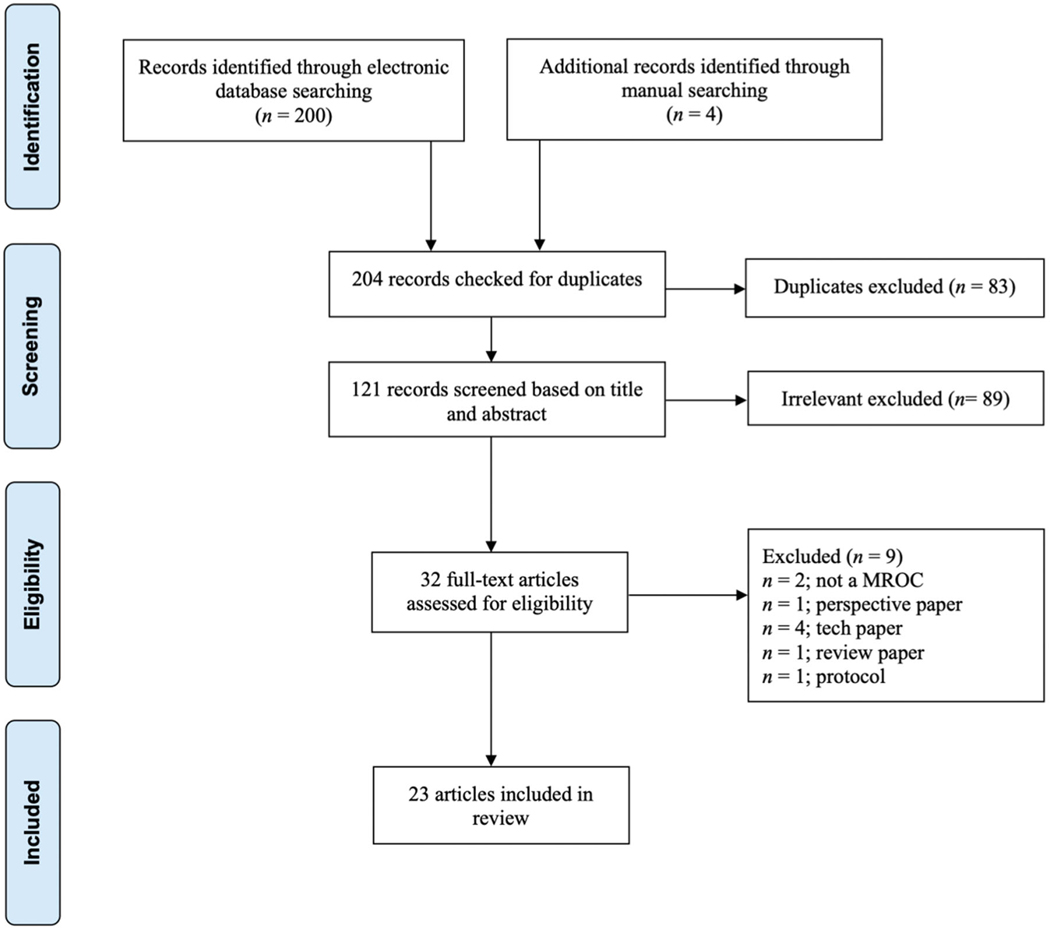
Of the 204 titles initially identified, following the removal of duplicate articles and irrelevant titles, 32 full-text articles were assessed for eligibility (Figure 1). Following full-text review, 23 articles met the inclusion criteria, and 100% agreement for article inclusion was reached by two authors (CH, SL) These 23 articles represented 19 individual research studies, with four instances of a single study producing two articles focusing on distinct outcomes (see superscript letters in Table 1).
Figure 1.
PRISMA flow diagram of study search and selection.
Table 1.
Study characteristics. Articles are numbered chronologically based on the year in which they were published.
| Article | Participants | Setting; MROC Model (Country) | Intervention Design | Purpose | Study Design (Level of Evidence) |
|---|---|---|---|---|---|
| 1. Zazula & Foulds (1983) | 11-month-old with phocomelia | Home; Seated (United States) | Not intervention, used for six months | Determine the feasibility of adapting commercially available ride-on car materials for use as a powered mobility device | Case report (V) |
| 2. Chiulli et al. (1988) | 4-year-old with post-polio syndrome and 3-year-old with spastic quadriplegia | Community; Seated (United States) | Not intervention, used for one day | Assess the feasibility of using a MROC for use as a powered mobility device | Case series (V) |
| 3. Deitz et al. (2002) | Two 5-year-olds with spastic quadriplegia | Community; Seated (United States) | 10-weeks baseline 2- to 3-weeks intervention 2- to 3- weeks post-intervention | Explore the effects of a MROC on the participation of children with disabilities (movement, contact with others, affect) | SSRD ABA for one child; SSRD ABAB for one child (IV) |
| 4. Huang et al. (2014) | 21-month-old with cerebral palsy | Home; Seated (United States) | 1-week baseline 12-weeks intervention 2-weeks post-intervention | Determine the feasibility of using a MROC (sitting tolerance, driving ability, interest in daily use, family compliance) | SSRD ABA* (IV) *identified as case report in article |
| 5. Logan et al. (2014) | 13-month-old with Down syndrome | Home; Seated (United States) | 12-weeks baseline 12-weeks intervention 4-weeks retention | Quantify the feasibility and family perceptions of using a MROC for increasing daily mobility, socialisation, and fun | SSRD ABA* (IV) *identified as single case study in article |
| 6. Logan et al. (2016) | Three children with complex medical needs: (A) 6-month-old; (B) 19-month-old; (C) 6-year-old | Hospital; Seated (United States) | 12-weeks baseline 5–8 weeks intervention (shortened due to health complications) | Determine the feasibility of short-term MROC use for exploration and enjoyment by children with complex medical needs | SSRD AB case series (V) |
| 7. Logan et al. (2017) | 4.5-year-old with tethered spinal cord | Community; Sit-to-stand (United States) | Not intervention, duration of use not specified | Document and compare how different assistive devices (forearm crutches and MROC) impact play behaviours | Case report (V) |
| 8. Huang & Chen (2017)a | 20 1- to 3-year-olds with mild to moderate motor disabilities (10 with MROC): cerebral palsy (4); Down syndrome (2); developmental delay (2); other (2) | Hospital; Seated (Taiwan) | 9-weeks intervention | Examine the effects of MROC training versus conventional therapy on mobility and social function of children, and assess the effects of MROC training on caregivers’ perceived stress levels | Non-equivalent preposttest control group design (III) |
| 9. Huang et al. (2017)a | *Same sample as Huang & Chen (2017) | Characterize behavioural changes in mobility and socialisation in children receiving MROC training in hospital environment | Observational data of non-equivalent preposttest control group design (IV) | ||
| 10. Ross et al. (2018) | Five 16- to 20-month-olds with mild to moderate motor disabilities: cerebral palsy (3), Down syndrome (1), Dandy Walker and cerebral palsy (1) | Community; Seated (United States) | 5-weeks baseline 11-weeks intervention | Determine the feasibility of MROC use during an inclusive playgroup, and determine the effect of MROC use on play behaviours of children with and without disabilities | SSRD AB case series (V) |
| 11. Logan et al. (2018) | Three young children with various disabilities: (A) 29-month-old with cerebral palsy; (B) 12-month-old with microdeletion; (C) 21-month-old with microcephaly | Home; Seated (United States) | 12-weeks baseline 12-weeks intervention | Determine the effect of MROC use in natural environments on mobility | Nonrandomized SSRD AB case series (V) |
| 12. Huang, Chen, et al. (2018)b | 29 1- to 3-year-olds with motor disabilities (15 with MROC): developmental delay (11); cerebral palsy (2); other (2) | Hospital; Seated (Taiwan) | 9-weeks intervention 9-weeks follow-up | Examine the effects of combining MROC training with an adult-directed social interaction program in hospital-based environment on mobility and social functions | Non-equivalent preposttest control group design (III) |
| 13. Huang, Huang, et al. (2018)b | *Same sample as Huang et al. (2018) | Examine the effects of combining MROC training with an adult-directed social interaction program in hospital-based environment on improving mastery motivation and home affordances | Non-equivalent preposttest control group design (III) | ||
| 14. Feldner et al. (2019)c | 4-year-old with cerebral palsy | Home; Seated (United States) | Not intervention, used for one year | Investigate children’s and family’s experiences of powered mobility provision processes and early use of their new technology, using their own words and images | Qualitative case study (N/A) |
| 15. Logan, Catena, et al. (2019) | Four 7-9month-olds with Down syndrome | Home; Seated and sit-to-stand (United States) | 9-months intervention | Determine the feasibility of use of a MROC with seated and standing modes | Case series (IV) |
| 16. Plummer (2019) | 21-month-old with Segawa syndrome | Home; Seated (United States) | 8-weeks intervention | Examine behavioural changes of a child using a MROC and assess the validity of an observational and mobility skills checklist | Case report (V) |
| 17. Restrepo et al. (2019) | Three 3- to 4-year-olds with cerebral palsy | Community; Seated (Colombia) | Not intervention, used for one day | Examine the feasibility of implementing a Go Baby Go program in Colombia | Case series (IV) |
| 18. Pritchard-Wiart et al. (2019) | Five 3–58month-olds with various disabilities: cerebral palsy (4); arthrogryposis and hypotonia (1) | Home; Seated (United States) | 8-weeks intervention | Describe required modifications for children with more severe mobility limitations, report use, describe parents’ roles, and explore therapist and parent perspectives regarding MROC use | Case series (IV) |
| 19. Logan, Hospodar, et al. (2019)d | 14 1- to 3-year-olds with various disabilities: cerebral palsy (3); Down syndrome (2); spina bifida (3); developmental delay (3); Sjogren-Larsson syndrome (1); Wolf Hirschhorn (1); microcephaly (1) | Home; Seated (United States) | Not intervention, used for 3 months | Describe real-world use of MROC and compare parent-reported use with use reported by an electronic tracker | Case series (IV) |
| 20. Feldner (2019)c | *Same sample as Feldner et al. (2019) | Understand the perceptions and experiences of children with disabilities and their families during the introduction process to powered mobility, with a specific focus on the shaping of disability identity | Qualitative case study (N/A) | ||
| 21. Hospodar et al. (2020) | Eight 6.5- to 12.5-month-olds with Down syndrome | Home; Seated, sit-to-stand, and power-push (United States) | 7- to 15-months intervention | Describe total dosage and daily use of three distinct MROC modes, assess ability of young children with Down syndrome to independently activate the MROCs, and describe the age of onset of selected motor milestones of children in the intervention compared to norms | Case series (IV) |
| 22. Logan et al. (2020)d | *Same sample as Logan et al. (2019) | Examine how caregivers’ perceived barriers of use change before and after a three-month period of MROC use | Qualitative case series (N/A) | ||
| 23. Livingstone et al. (2020) | 74 9–68-month-olds with mobility limitations | Community; Seated | Not intervention, used for one day | Describe and compare children’s use of and parents’ preference for MROCs compared to three other powered mobility devices | Case series (IV) |
Superscript letters denote pairs of articles that used the same sample. See Results for a description of the different modified ride-on car (MROC) models. See Wiart et al. [18] for “Levels of Evidence” criteria for single-subject and group designs; the quality of qualitative studies was not rated. SSRD=single subject research design.
Study characteristics
Sample
To date, MROC research has included a total of 164 children ranging in ages from 7-months to 6-years. Most studies involved children 7- to 21-months old (Table 1). Of note, 74 of the 164 children were from one study that examined families’ device preferences at a one-day event [19]. Apart from this study, sample sizes were small, ranging from one to 29 children, with the maximum belonging to a group study where only 15 children were in the treatment group and therefore actually used a MROC (n = 15 used in the calculation for total number of children) [20,21]. Children had a wide range of disabilities and/or medical conditions, but the most represented were cerebral palsy (n = 81), Down syndrome (n = 18), unspecified developmental delay (n = 16), and neurologic or neural tube diagnoses (e.g., spina bifida, n = 15). Other diagnoses accounted for four or less children per diagnosis.
Setting
Research was conducted primarily in the home (n = 12) [1,12,23–31], but was also conducted in hospitals (n = 5) [20,21,32–34], a clinic (n = 3) [19,35,36], a pre-school (n = 2) [37,38], and an inclusive playgroup (n = 1) [9]. Studies classified as home-based often extended into the community, with families using MROCs in schools, parks, and other community locations.
The majority of studies were conducted in the United States, with the exception of four hospital-based studies in Taiwan [20,21,33,34], one community-based study in Colombia [36], and one community-based study in Canada [19].
Research design
Case series were the most common research design, including both single-subject AB case series designs (n = 3) [1,9,32], single-subject ABA case series designs (n = 3) [23,24,37], and group design case series (n = 7) [19,26,28–30,35,36]. Other designs included case reports [22,27,38], pretest-posttest control group designs [20,21,33,34], and qualitative studies [12,25,39].
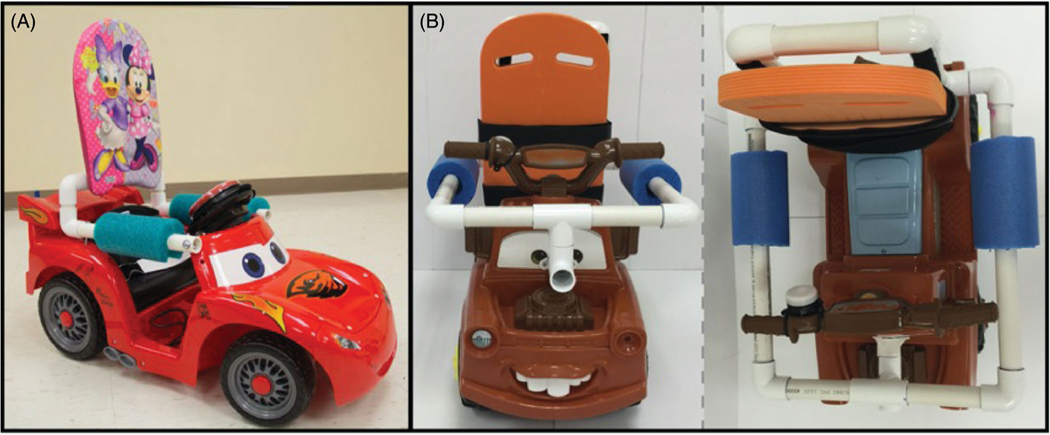
MROC models
All but three studies used a seated MROC with the switch placed in an accessible location for the child to activate in a seated position (Figure 2(A)). The other three studies utilized a more recent model called a sit-to-stand MROC (Figure 2(B)) [26,30,38]. In this model, a reverse-activated pressure switch is embedded in the seat of the MROC, so the child must pull to stand and remain standing to power the MROC. This model was created to incorporate dynamic balance and pull-to-stand experiences while simultaneously providing self-directed mobility. One of the three studies included an additional power-push mode, where the child could hold onto a bar on the back of the MROC and step to keep up with the slowly moving vehicle [30].
Figure 2.
One version of a (A) seated modified ride-on car and (B) sit-to-stand modified ride-on car.
Level of evidence and study quality
Level of evidence and study quality were variable, though the majority of studies (n = 17) were consistent with criteria describing evidence level IV or V (lowest level of evidence) per AACPDM protocol [18]. Only three studies were identified as Level III, and only these studies were assigned quality ratings [20,33,34].
Level IV and V studies clearly stated the purpose of the study and included appropriate literature review with theoretical and clinical rationale. Study designs ranged from case reports to Single Subject Research Design (SSRD) AB case series. Outcome measures were clearly defined, although reliability and validity of measures was not always included. For studies that used video coding of data, reliability information for coders was included. The largest sample size in studies of Level IV and V was 20 children (with only 10 children in the treatment group and therefore using the MROC) [21]. None of the studies explicitly justified the sample size, but methods were clearly defined in all studies. Given the small sample sizes, analyses were limited, and none included effect size information. Most studies did not include statistical significance, given the small sample sizes, but all did provide a conclusion, with the majority including clinical applications. All studies included a statement about ethics and informed consent.
The three Level III studies were rated as weak based on AACPDM conduct ratings [20,33,34]. They provided inclusion and exclusion criteria, clearly described valid and reliable outcome measures, and blinded assessors. However, while the intervention was well described, the adherence to the intervention included less detail, no power calculations were included, dropout was not reported, and the children were not randomized to treatment and control groups due to geographical reasons, which may have introduced uncontrolled confounders.
SRQR assessment of the three qualitative studies indicated high levels of qualitative rigour as measured by the authors’: definition and description of the qualitative approach, research paradigm, and positionality of the researcher; use of thick, rich descriptions of the context and inclusion of quotes or images as primary source data; demonstration of step-by-step data analysis and thematic coding processes; and description of how study participants were engaged and how data was triangulated, to ensure the credibility and trustworthiness of the data [12,25,31].
MROC use
Goal use
Only six studies provided a recommended goal for MROC use (Table 2); all six studies were interventions, with five in the home [1,23,24,26,30] and one in the hospital [32]. Five of these six studies recommended 20–30 min per day for at least five days per week; the sixth gave a recommendation of eight minutes per day for five days per week [26]. Of the remaining 17 studies that did not provide a goal, seven studies described natural use and/or the family’s experience of acquiring a device [12,22,25,28,29,39,40]; five studies used MROCs only in specific clinician- or researcher-administered sessions and were not left for use outside of the prescribed sessions [9,20,21,33,34]; three studies reported only a single session or day of use [19,35,36]; and two studies were described like interventions but did not report in text whether a goal was provided [27,37].
Table 2.
Goal use for MROC provided by researchers/clinicians, reported use, and resulting adherence rates.
| Article | Goal use | Reported use | Adherence |
|---|---|---|---|
| 1. Zazula & Foulds (1983) | Not reported | Not reported | Not applicable |
| 2. Chiulli et al. (1988) | Not reported | Not reported | Not applicable |
| 3. Deitz et al. (2002) | Not reported | Not reported | Not applicable |
| 4. Huang et al. (2014) | 20min per day; 5 days per week | 1150 min over 39 days M = 29.5 min per session* |
65% *Based on days of use |
| 5. Logan et al. (2014) | 20–30 min per day; 7 days per week | 595 min over 25 days M = 23.9 (SD = 8.6) minutes per session |
42% *Based on days of use |
| 6. Logan et al. (2016) | 20–30 min per day; 7 days per week | Not reported | Not reported |
| 7. Logan et al. (2017) | Not reported | Not reported | Not applicable |
| 8. Huang & Chen (2017)a | Not reported | Not reported | Not applicable |
| 9. Huang et al. (2017)a | *Same as Huang & Chen (2017) | Not reported | Not applicable |
| 10. Ross et al. (2018) | Not reported | At least 30 min per session for a majority of intervention sessions | Not applicable |
| 11. Logan et al. (2018) | 20–30 min per day; 5 days per week | Child A: 2210 min over 64 days M = 34.5 (SD = 5.7) minutes per session Child B: 1225 min over 46 days M = 26.6 (SD = 8.9) minutes per session Child C: 120 min over 6 days M = 20 (SD = 0) minutes per session |
Child A: 100% Child B: 67% Child C: 10% *Based on days of use with at least 20 min of use |
| 12. Huang, Chen, et al. (2018)b | Not reported | Not reported | Not applicable |
| 13. Huang, Huang, et al. (2018)b | *Same as Huang, Chen, et al. (2018) | Not reported | Not applicable |
| 14. Feldner et al. (2019)c | Not reported | Not reported | Not applicable |
| 15. Logan et al. (2019) | 8 min per day, 5 days per week | Child A: 1156 min over 78 days M = 14.8 (SD = 4) minutes per session Child B: 31 min over 3 days M = 10.3 (SD = 3.2) minutes per session Child C: 2146 min over 115 days M = 18.7 (SD = 7.8) minutes per session Child D: 551 min over 39 sessions M = 14.1 (SD = 5) minutes per session |
Child A: 43% Child B: 2% Child C: 64% Child D: 22% |
| 16. Plummer (2019) | Not reported | Not reported | Not applicable |
| 17. Restrepo et al. (2019) | Not reported | Not reported | Not applicable |
| 18. Pritchard-Wiart et al. (2019) | Not reported | Child 1: 1.3 days per week M = 45.4 (SD = 25.4) minutes per session Child 2: 2.9 days per week M = 30.6 (18.9) minutes per session Child 3: 2.3 days per week M = 12.1 (SD = 3.9) minutes per session Child 4: 2.4 days per week M = 62.5 (22.7) minutes per session |
Not applicable |
| 19. Logan et al. (2019)d | Not reported | Parent reported: M = 195.1 (SD = 234.8) minutes over three months M = 17.8 (SD = 9.9) minutes per session Objective tracking reported: M = 171.4 (SD = 206.1) minutes over three months M = 16.5 (8.6) minutes per session |
Not applicable |
| 20. Feldner (2019)c | *Same as Feldner et al. (2019) | Not reported | Not applicable |
| 21. Hospodar et al. (2020) | 30 min per day; 7 days per week |
M = 6454 (SD = 3102) minutes over 7–15 months M session times were similar among children (24–30 min) |
40–96% |
| 22. Logan et al. (2020)d | *Same as Logan et al. (2019) | Not reported | Not applicable |
| 23. Livingstone et al. (2020) | Not reported | Not reported | Not applicable |
“Not reported” includes instances where the authors did not include this information in the publication, or the authors explicitly stated in text that they did not provide families with guidelines. “Not applicable” is present for adherence when no goal use was provided. Green highlights hospital-based studies (n=5). Yellow highlights community-based studies (n=6). Home-based studies are not highlighted (n=12). Bold article titles indicate interventions (n=14). Superscript letters denote pairs of articles that used the same sample.
Calculated by authors of this review as total number of minutes used divided by total days of use.
Reported use
A limited number of studies provided actual use data (n = 7) [1,23,24,26,28–30]. Five of the six studies that provided a recommended goal provided use data; only the hospital-based study provided a recommendation but did not report use data [26]. Two studies that did not provide a recommended goal nonetheless provided detailed use data [28,29]; these studies specifically did not provide families with a recommendation in order to capture natural use, but it was an explicit aim to quantify use. Reported use data suggests that children typically engage in MROC sessions of approximately 20–25 min. There were no adverse events reported related to MROC use.
Adherence
Only five studies that provided both a recommended goal and use data included adherence rates [1,23,24,26,30]. Adherence rates varied widely, ranging from 2% to 100%. All five studies included education and training to promote adherence, including researcher visits to families’ homes either weekly [1,23,24] or every other week [26,30]. Education and training topics included safe use of the MROC, a pamphlet with suggested driving activities, researcher facilitated driving sessions, and conversations between the researcher and family to discuss the child’s past driving experiences, and co-creation of new driving activities.
Outcomes across domains of the ICF
The domains of the ICF include: body structures/functions (physiological and psychological functions and anatomical parts of the body), activity (tasks or actions), participation (involvement in life situations), environmental factors (physical, social, and attitudinal environment), and personal factors (particular background of an individual’s life) [15]. Most studies included outcome measures related to activity (n = 19), participation (n = 17), and environmental/personal factors (n = 18; Table 3). Findings indicate that children can learn how to use MROCs, resulting in gains in mobility and increased social interactions. Children demonstrated high enjoyment, through positive facial expressions and communicative sounds or gestures, while using the MROC. Further, MROC use resulted in positive changes in environmental and personal factors. Parents who participated in a MROC intervention had significantly decreased stress scores, and questionnaires suggest that the use of MROCs positively impacts families’ understanding of their child’s abilities and can change perceptions regarding powered mobility device use. Few studies (n = 8) targeted body structure and function outcomes, though some reported varied patterns of visual attention to the activation switch. Only two studies specifically targeted physical skills through use of the sit-to-stand model of the MROC, reporting preliminary positive changes. Some studies described anecdotal changes (e.g., increased crawling outside of the MROC, improved head and trunk position, etc.) in children’s physical ability, but these were not formally measured. There were no reported negative effects of children’s MROC use on ICF domains.
Table 3.
(A) Outcome measures used in each article. See 3B for article citations. (B) Outcomes separated by the domains of the ICF framework.
| (A) | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8a | 9a | 10 | 11 | 12b | 13b | 14c | 15 | 16 | 17 | 18 | 19d | 20c | 21 | 22d | 23 | |
| Behavioural video coding | |||||||||||||||||||||||
| Driving mobility | X | X | X | X | X | X | X | X | X | ||||||||||||||
| Visual attention to switch | X | X | X | X | X | ||||||||||||||||||
| Switch contacts | X | ||||||||||||||||||||||
| Stop at target | X | X | |||||||||||||||||||||
| Reaches | X | X | X | ||||||||||||||||||||
| Facial expressions | X | X | X | X | X | X | |||||||||||||||||
| Vocalizations | X | ||||||||||||||||||||||
| Natural play | X | X | X | ||||||||||||||||||||
| Play/social behaviours | X | X | X | X | |||||||||||||||||||
| Standardized assessments | |||||||||||||||||||||||
| PEDI | X | X | X | X | X | ||||||||||||||||||
| Bayley | X | ||||||||||||||||||||||
| Use tracking | |||||||||||||||||||||||
| Activity log | X | X | X | X | X | X | X | X | X | ||||||||||||||
| Electronic tracking | X | ||||||||||||||||||||||
| Interview methods | |||||||||||||||||||||||
| Family interview | X | X | X | X | X | X | X | ||||||||||||||||
| Clinician interview | X | ||||||||||||||||||||||
| Anecdotal | X | X | |||||||||||||||||||||
| Photo narration | X | ||||||||||||||||||||||
| Personal factors | |||||||||||||||||||||||
| Goal Attainment Scaling | X | ||||||||||||||||||||||
| Mastery questionnaire | X | ||||||||||||||||||||||
| Power mobility skills checklist | X | X | |||||||||||||||||||||
| Family factors | |||||||||||||||||||||||
| Parental Stress Index | X | X | |||||||||||||||||||||
| Affordance in the Home Environment for Motor Development (AHEMD) | X | ||||||||||||||||||||||
| (B) | ||||
|---|---|---|---|---|
|
| ||||
| Article | Body structure and function | Activity | Participation | Environmental and personal factors |
| 1. Zazula & Foulds (1983) | None | Child was able to fully control MROC | None | None |
| 2. Chiulli et al. (1988) | Improved symmetry of trunk alignment and upright postural stance | None | None | None |
| 3. Deitz et al. (2002) | None | Increased movement for both children | Mixed results for contact behaviours with peers and adults | No substantial changes in affect |
| 4. Huang et al. (2014) | Visual attention to switch decreased Increased upright head and trunk position, and more head and arm movements | Learned to independently press the activation switch Learned to stop independently at a target Improvement in functional mobility (PEDI) Increased reaching during MROC play but not natural play | Increased physical and social interaction with family Improvement in functional social skills (PEDI) Demonstrated new play behaviours Dad started playing ball with child - family noted that these were some of the first father-son play sessions | Increased positive facial expressions for MROC and natural play High enjoyment Family’s understanding of child’s abilities increased Vocalized more during intervention to express positive emotions |
| 5. Logan et al. (2014) | Visual attention to switch increased from baseline to intervention, then declined during follow-up | Learned to independently press the activation switch Little reaching during MROC sessions Decreased reaching during natural play over the course of the intervention. Improvement in functional and caregiver assisted mobility (PEDI) |
Improved functional and caregiver assisted self-care and social skills (PEDI) Increased socialisation with sister | Positive facial expressions increased. High variability with negative facial expressions High enjoyment Changed parents’ perception of powered mobility device use Family noticed frustration during follow-up period due to lack of MROC |
| 6. Logan et al. (2016) | None | All children learned to independently press the activation switch Two of three children used the MROC for open exploration of the environment | Child C used MROC to play hide-and-seek and interact with peers | Two of the three children displayed a majority of positive facial expressions One child displayed a majority of negative facial expressions Changed caregiver’s expectations of child’s abilities |
| 7. Logan et al. (2017) | None | Child was less fatigued and faster when using a MROC compared to forearm crutches | Engaged in less solitary play and more parallel play in the gymnasium while using a MROC compared to forearm crutches Engaged in more peer interaction, including complex social games like tag and role playing, and less teacher interaction on the playground when using a MROC compared to forearm crutches | None |
| 8. Huang & Chen (2017)a | None | Treatment group: Significant improvement in mobility function. 4 of 10 children demonstrated clinically significant gains in mobility function (PEDI). Control group: No improvement in mobility function. 2 of 10 children demonstrated clinically significant gains in functional mobility (PEDI). |
Treatment group: Significant improvement in social function. 3 of 10 children demonstrated clinically significant gains in social function (PEDI). Control group: Significant improvement in social function. 1 of 10 children demonstrated clinically significant gains in social function (PEDI). |
Treatment group: Significantly decreased scores of parenting stress. Control group: No changes in parenting stress. |
| 9. Huang et al. (2017)a | Visual attention to switch decreased | All children learned to independently press the activation switch All children learned to stop independently at target. | Few child-initiated social interactions. Social interactions with children from adults increased slightly. | Positive facial expressions did not increase during MROC play but did increase during natural play |
| 10. Ross et al. (2018) | None | None | Child B increased direct peer interactions. Child C decreased solitary play and increased adult interactions. Child E increased parallel peer play. More interactions between children with and without disabilities Friendships established during the inclusive playgroup continued after the study |
None |
| 11.. Logan et al. (2018) | Two of three children demonstrated a co-occurrence trend between visual attention and switch contacts | All children learned to independently press the activation switch Two children demonstrated clinically significant changes in functional and caregiver assisted mobility (PEDI) | Child B noticed a cat 20 feet away, pointed to it, and used the MROC to go play with it | High enjoyment |
| 12. Huang, Chen, et al. (2018)b | None | Treatment group: Significant improvement in mobility function. Caregivers reported that children were more active and mobile outside of the ROC than before the intervention. Control group: Significant improvement in mobility function |
Treatment group: Significant improvement in social function. Significant improvement in goal achievement at posttest compared to the control group | Treatment group: Significantly decreased parental stress Control group: No changes in parenting stress |
| 13. Huang, Huang, et al. (2018)b | None | None | Treatment group: Significantly greater improvements of object persistence compared to control group | Treatment and control groups: Significant improvements in mastery pleasure and home affordances scores |
| 14. Feldner et al. (2019)c | None | MROC and powered mobility device facilitated mobility | Mom and child both independently identified an increase in participation Played tag and chase |
Mom still did not want a powered wheelchair following end of study but was very supportive of MROC use Mom reported she would not have pursued MROC without support of a physical therapist |
| 15. Logan, Catena et al. (2019) | Families reported that the children practiced pulling to stand and supported standing more often in the MROC compared to outside of the MROC | Three of four children learned to independently press the activation switch in both seated and standing modes Three of the four children learned to engage in goal directed mobility | Children used MROC to openly explore environment Increased sibling play | Displayed a majority of positive facial expressions High enjoyment |
| 16. Plummer (2019) | None | Increased scores on power mobility skills checklist | Increased social interaction | Increased environmental interaction Increased positive facial expressions and vocalizations |
| 17. Restrepo et al. (2019) | None | All children learned how to press the activation switch | None | All parents rated the experience as “extremely fun” |
| 18. Pritchard-Wiart et al. (2019) | One family reported increased crawling outside of the MROC after the study began | Four of five children were able to be fitted into a MROC Three of four children learned to press the activation switch with low assistance | Increased opportunities to play and socialize with siblings and children in the community Greater engagement in activities as a family Primarily used MROC outdoors | Parents reported being more open to the idea of other powered mobility options and therapists agreed it encouraged conversation High enjoyment Parents rated children as highly motivated |
| 19. Logan, Hospodar, et al. (2019)d | None | Greater use of MROCs in the first 45 days compared to the last 45 days Child with the most severe mobility limitations used the MROC the most | MROC used in home, outdoors, and community spaces | Moderate enjoyment |
| 20. Feldner (2019)c | None | Able to activate and manoeuvre the MROC | Increased participation in the classroom and on the playground | Changed parental perceptions regarding child’s ability and disability identity |
| 21. Hospodar et al. (2020) | Most motor milestones achieved earlier than expected for DS norms | All children learned to independently press the activation switch in both seated and standing modes | None | None |
| 22. Logan et al. (2020)d | None | None | None | Environmental and device barriers were the most frequently reported at pre- and post-intervention |
| 23. Livingstone et al. (2020) | None | Children able to activate car | None | Environmental factors were not related to parent device preference. Children’s ability to use difference devices and parent device preferences were varied depending upon several factors. |
Superscript letters denote pairs of articles that used the same sample (e.g., 8a and 9a are different papers published from the same study).
Discussion
The purpose of this systematic review of MROC research was to (1) describe and categorize past study characteristics; (2) synthesize existing knowledge of children’s use of MROCs; and (3) frame outcomes within the context of the International Classification of Functioning, Disability and Health (ICF). Evidence from the 23 included studies indicates that the majority of study designs did not contribute strong quality of evidence. As a result, it is important to interpret the findings of the current systematic review with caution. A lack of strong quality of evidence makes it difficult to make confident conclusions about the true effect of MROC interventions for children with disabilities. However, based on the peer-reviewed research articles that met our inclusion criteria, evidence suggests that MROCs are feasible for use with different populations and across settings, though reported use and adherence to researcher suggestions varies widely. Further, MROC use has primarily addressed activity and participation domains for children with disabilities, with outcomes largely reflecting a focus on functional mobility and social interactions.
Summary of evidence
Study characteristics
Sample.
Studies typically included a small sample of young children (<24 months), with a range of function across studies. Children’s disabilities most often included cerebral palsy, Down syndrome, and general developmental delay, although a range of unique disabilities and diagnoses were represented across studies. It is unclear whether level of functional ability (i.e., severity of disability) relates to the efficacy of MROC use, but findings suggest MROC use is feasible for young children with a variety of disabilities. When determining if children with disabilities are strong candidates for powered mobility, factors considered include a child’s age, physical skills (e.g., child’s ability to sit with support and reach in midline), cognitive abilities (e.g., child’s understanding of cause and effect), future potential for motor skill development (e.g., expectation of walking, delayed walking, or future mobility device use), and perceptions of powered mobility (e.g., opportunity versus ‘last resort’) [8]. This systematic review indicates that MROC interventions are feasible for children with disabilities who may not be considered typical candidates for powered mobility, such as young children under 12 months of age [1,26,28,30,32], and children with a wide range of physical skills and cognitive abilities [24,32].
Setting.
MROC studies were conducted mainly within the home (n = 12), but were also conducted in the hospital (n = 5) and community setting (n = 6). Home-based interventions align with the birth-to-three early intervention service model’s emphasis on providing services in the child’s primary natural environment [41,42]. However, environmental barriers may also prevent MROC use in the home setting. For example, in Taiwan, most homes lack the necessary space to use MROCs. Because of this, four of the five hospital-based studies occurred in a paediatric care facility in Taiwan for the main purpose of minimizing environmental barriers to home MROC use. Although many of the home-based and hospital-based studies include community elements, only three studies occurred exclusively in community environments for extended periods of time; all three examined changes in social play behaviours: Deitz et al. assessed children’s interactions with peers and adults when using MROCs in school settings (gym and recess) [37]; Logan et al. compared the interactions of one child in an inclusive pre-school classroom, gym, and playground while using forearm crutches or a MROC [38]; and Ross et al. examined play behaviours of children with and without disabilities during an inclusive playgroup where MROCs were available for use [9]. The three additional community-based studies were one-day clinic visits designed to determine the feasibility of MROC use. Two of the qualitative studies that examined caregiver perceptions of powered mobility technology and identity development in children were identified as home-based studies for the purpose of this review, but also largely took place in school environments [12,25]. Community settings, particularly school-based settings, may be especially important for promoting outcomes related to participation and for exploring the relative physical accessibility and capacity for universal design in schools.
Level of evidence and study quality.
Our findings indicate that the level of evidence is generally weak in support of MROC interventions. While three studies were rated as Level III, the majority of studies were rated as level IV and V. This is not surprising given the indicated purpose of studies as exploratory or descriptive rather than experimental. Case reports and single-subject research designs also introduce sample bias that may affect study quality—parents who self-select to participate in MROC studies are likely very proactive with therapy in general, so it is impossible to conclude that observed changes were not due to other factors. Further, the amount of time spent using a MROC and its effect on the observed changes in children’s behaviours and development remains unclear. Most studies did not use the same outcomes, or did not measure them identically, which makes outcomes difficult to compare. However, two studies from the same data source directly compared the provision and use of a MROC to a more traditional paediatric powered mobility device, and one study examined children’s learning of and parents’ preference for different mobility devices [12,19,25]. These results suggest a complex interplay amongst device characteristics, such as size and usability features, child ability levels, family dynamics, and the physical and social environments where the devices were used on a regular basis.
MROC use
Goal use and reported use.
Our findings indicate that families were infrequently provided with a use goal and actual use was either not reported or was highly variable. Even though setting realistic and achievable goals is related to behaviour change and success, the majority of studies did not provide families with a use goal [9,12,19–22,25,28,29,31,33–38]. The most commonly reported use goal was 20–30 min for at least five days per week—but this goal was only based on pilot feasibility. It remains unknown whether this goal is the optimal amount of dosage for positive developmental or participation outcomes. Further, MROC use was substantially higher in research studies where families were provided weekly or bi-weekly, in-person support compared to when no ongoing support was provided. This suggests that providing ongoing support may be crucial to encourage use, and further highlights the need to define optimal dosage with powered mobility technology in young children with disabilities [29].
Adherence.
Adherence rates were either not provided or were calculated differently across studies based on varied recommendations provided to families. Reported adherence ranged from 2% to 100%. Recent studies suggest that perceived barriers related to the environment and device inhibit MROC use and adherence [31,39], similar to other forms of assistive technology [43–45]. Qualitative studies highlighted freedom and independence provided by the MROC, even when reporting relatively infrequent use [12,25]. Low adherence may also be due to child-related perceived barriers regarding health, tolerance, and abilities, and caregiver-related perceived barriers regarding physical requirements, lack of time, and motivation [39]. Given the range in adherence and differences in recommendations, more research is needed to identify optimal dosage, both in terms of achieving independent switch activation and providing a realistic recommendation of MROC use for families. In combination with dosage, it is also important to consider the quality of driving experiences that may facilitate positive outcomes. The quality of driving experiences may be related to the type of driving activities that are encouraged, such as open exploration, goal-directed driving, and play in enriched environments with family and peers. It is critical that paediatric physical and occupational therapists collaborate with families to develop strategies for using a MROC, overcoming perceived barriers to use, and to create feasible use goals to optimize adherence.
Outcomes across domains of the ICF
Outcomes of MROC studies were primarily related to activity and participation. Some studies included environmental and personal factors, and limited studies focussed on body structure and function. MROCs directly impact activity by providing mobility, which was primarily assessed through behavioural coding of video recordings to assess children’s mobility behaviours. Positive impacts on participation, such as social interactions and play behaviours, were measured by assessing family-directed goals and benchmarks, conducting semi-structured interviews, and collecting activity logs, surveys, and photo narratives. However, researchers noted challenges in capturing some of the anecdotal or unanticipated participation outcomes that emerged from MROC use, such as the development of more complex play interactions noted by pre-school staff [38], a perceived ‘first’ father-son play interaction [23], or the continued friendships that developed outside researcher-initiated playgroups [9]. Improvements in environmental and personal factors suggest that MROCs may provide a good fit between device, family and environment [12,28].
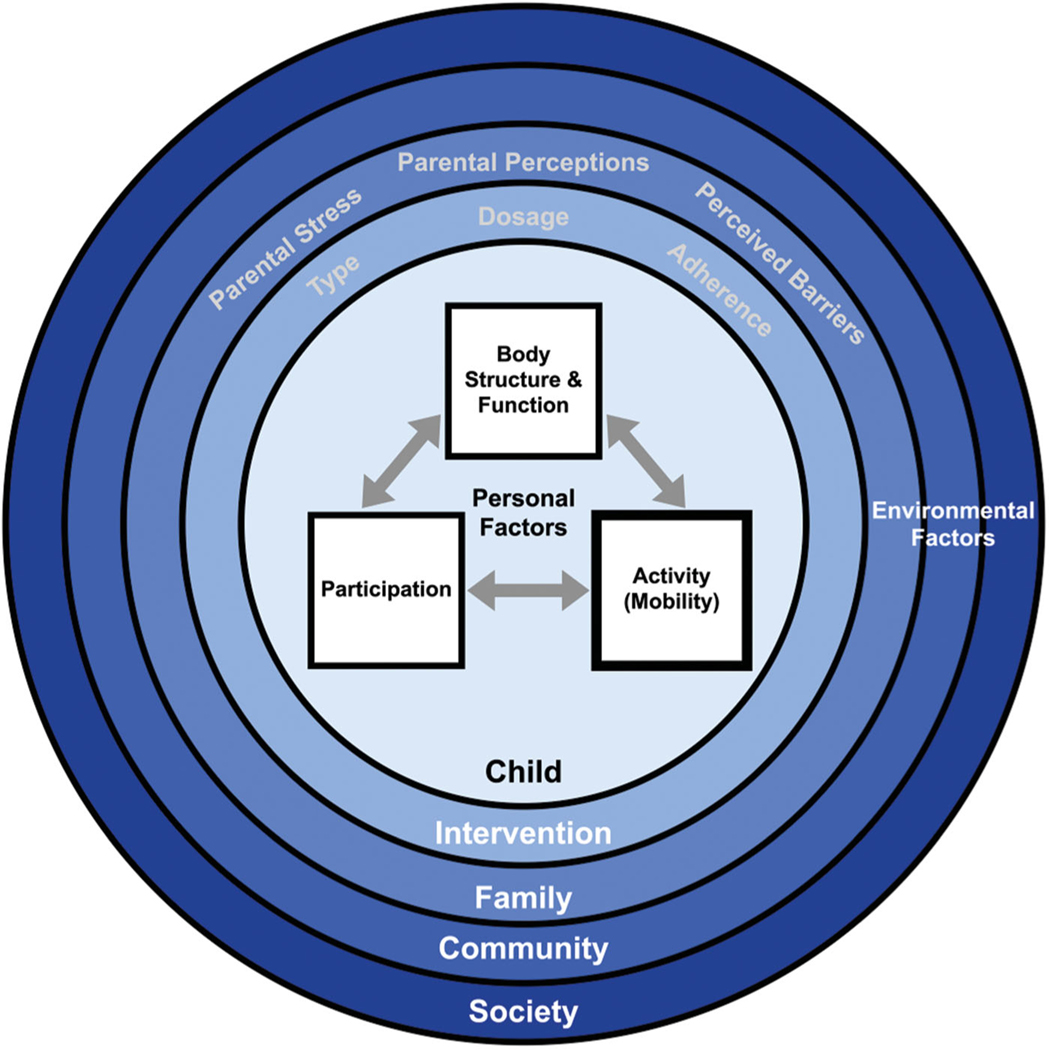
Although MROC interventions most explicitly impact activity, increased activity can propel advancement of all domains of the ICF, and can also exert ecological, bidirectional ripples on the family, community, and society (Figure 3). However, future research is necessary to investigate these potential connections.
Figure 3.
Intervention model for MROCs, displaying nested levels of influence (inspired by Bronfenbrenner [53]). Activity (bolded) is the main focus of MROC interventions because they provide an immediate source of mobility. Increased mobility may more immediately increase participation compared to traditional interventions, where participation is often a downstream effect. The sit-to-stand MROC concurrently targets body structure and function, along with activity. Personal factors (e.g., disability severity, enjoyment of MROC) can influence the relation among child factors. MROC interventions principally aim to impact the child, and ripple outwards, which may result in additional benefits (e.g., child’s increasing mobility improves parents’ perceptions of child’s abilities, so parents provide more opportunities to use the MROC in the community, thereby increasing community engagement and participation).
Future directions
Based on our synthesis of peer-reviewed research articles that met our inclusion criteria, we offer four specific directions for future research:
Larger sample sizes of children, diagnosed with one type of disability and within a narrow age band, are needed. Limiting the heterogeneity of future samples can increase the external validity of results and lead to greater confidence in findings.
Research must use more robust research designs that increase the level of evidence of findings. To date, no randomized controlled trials (RCTs) of MROC interventions were conducted, and only one RCT exists of a powered mobility intervention for young children with disabilities [3]. Other experimental designs, such as randomized crossover trials, or longitudinal studies that include longer intervention periods and follow-up assessments to track changes in developmental outcomes over time, may also be beneficial.
Evidence-based strategies are needed to support families and children in using MROCs on a regular basis. MROC use varies extensively from study to study, and is often very low [29], which parallels findings of low adherence to home exercise programs [46–49], and low use of assistive technology [43–45], despite positive perceptions of the benefits. Research highlights families’ perceived barriers to providing their child with opportunities to use a MROC [31,39]. Effective strategies to support families and children are needed to successfully implement RCTs; reciprocally, RCTs are needed to characterize
the dose-response relation between MROC use and outcomes, which would inform evidence-based recommendations for use.
Research is needed to determine the effect of MROC use on outcomes across the ICF framework. MROC primarily targets activity and participation through mobility, but better outcome measures should be used to capture these changes. The PEDI is the only standardized assessment used in included studies that targeted the activity and participation domain of the ICF [1,20,23,24,33]. Future studies could include other outcome measures, such as the Childhood Assessment of Participation and Enjoyment (CAPE) [50], Canadian Occupational Performance Measure (COPM) [51], or Child Engagement in Daily Life- Participation and Recreation subscale [52]. Although initial work with the sit-to-stand MROC examined effects related to body structure and function outcomes, this research is limited, and additional research using clinically-relevant and appropriate outcome measures is needed [13].
Limitations
Several limitations are present in this systematic review. One limitation is our narrowly defined inclusion criteria. For example, studies had to be published in peer-reviewed journals for inclusion. Our intent with this inclusion criterion was to ensure a minimal level of study quality and prevent double counting of data from scholarly outcomes such as conference presentations that were later published as articles. It is possible that research included in this systematic review is due to publication bias where only articles with significant or meaningful results were published. Further, eight of the articles included in this review use data from the same initial study design (i.e., four instances of two papers being published from the same dataset). We included all articles to more precisely assess the number of papers that report specific outcomes, but this slightly overestimates the total number of unique MROC research studies. Another limitation is that authors of this systematic review are contributors to MROC research, which may introduce bias in interpreting the studies. However, 12 studies (52%) included in this systematic review were from other research groups, which suggests some degree of independent verification of results. We included two raters throughout the study selection and data collection and involved a third rater as necessary to ensure agreement and mitigate potential bias. We were not able to include studies published in a language other than English due to lack of resources. However, only three studies were excluded for this reason. We mitigated bias by critically evaluating our own position within this topic area as we evaluated the evidence. It is important for other researchers to continue to explore the effect of MROCs and independently validate or repudiate previous research findings.
Conclusions
This systematic review suggests three conclusions: (1) MROCs have been used by young children with a variety of disabilities across settings, including the home, hospital, and schools, with no adverse events reported; (2) Children with disabilities were able to activate MROCs as young as 7-months old, and a majority of children enjoyed using MROCs; (3) MROCs increase children’s activity and participation, and positively impact family life and parent outcomes; (4) The overall low quality of evidence across studies precludes strong inferences regarding direct outcomes of MROC use. Future research is needed to further investigate the outcomes of MROC use for children with disabilities and their families.
Supplementary Material
IMPLICATIONS FOR REHABILITATION.
Physical and occupational therapists may consider using MROCs as a therapeutic tool or accessible play opportunity as part of a multi-modal approach to increase children’s mobility, family engagement, and participation in community life.
Personal (e.g., child’s enjoyment) and environmental factors (e.g., caregiver attitudes and stress) must be considered when developing plans of MROC use.
Funding
Support for Dr. Feldner’s time was funded by the NIH National Centre for Advancing Translational Science under Award Number KL2 TR002317.
Footnotes
Disclosure statement
The authors report no conflict of interest, financial or otherwise.
Data availability statement
There is no data set associated with this study.
References
- [1].Logan SW, Hospodar CM, Feldner HA, et al. Modified ride-on car use by young children with disabilities. Pediatr Phys Ther. 2018;30(1):50–56. [DOI] [PubMed] [Google Scholar]
- [2].Feldner HA, Logan SW, Galloway JC. Why the time is right for a radical paradigm shift in early powered mobility: the role of powered mobility technology devices, policy and stakeholders. Disabil Rehabil Assist Technol. 2016;11(2):89–102. [DOI] [PubMed] [Google Scholar]
- [3].Jones MA, McEwen IR, Neas BR. Effects of power wheelchairs on the development and function of young children with severe motor impairments. Pediatr Phys Ther. 2012;24(2):131–140. [DOI] [PubMed] [Google Scholar]
- [4].Butler C. Effects of powered mobility on self-initiated behaviors of very young children with locomotor disability. Dev Med Child Neurol. 1986;28(3):325–332. [DOI] [PubMed] [Google Scholar]
- [5].Guerette P, Furumasu J, Tefft D. The positive effects of early powered mobility on children’s psychosocial and play skills. Assist Technol. 2013;25(1):39–48. [DOI] [PubMed] [Google Scholar]
- [6].Livingstone R, Field D. Systematic review of power mobility outcomes for infants, children and adolescents with mobility limitations. Clin Rehabil. 2014;28(10):954–964. [DOI] [PubMed] [Google Scholar]
- [7].Henderson S, Skelton H, Rosenbaum P. Assistive devices for children with functional impairments: impact on child and caregiver function. Dev Med Child Neurol. 2008;50(2):89–98. [DOI] [PubMed] [Google Scholar]
- [8].Livingstone R, Paleg G. Practice considerations for the introduction and use of power mobility for children. Dev Med Child Neurol. 2014;56(3):210–221. [DOI] [PubMed] [Google Scholar]
- [9].Ross SM, Catena MA, Twardzik E, et al. Feasibility of a modified ride-on car intervention on play behaviors during an inclusive playgroup. Phys Occup Ther Pediatr. 2018;38(5):493–509. [DOI] [PubMed] [Google Scholar]
- [10].Huang HH, Galloway JC. Modified ride-on toy cars for early power mobility: a technical report. Pediatr Phys Ther. 2012;24(2):149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Logan SW, Feldner HA, Bogart KR, et al. Toy-based technologies for children with disabilities simultaneously supporting self-directed mobility, participation, and function: a tech report. Front Robot Ai. 2017;4:7. [Google Scholar]
- [12].Feldner HA, Logan SW, Galloway JC. Mobility in pictures: a participatory photovoice narrative study exploring powered mobility provision for children and families. Disabil Rehabil Assist Technol. 2019;14(3):301–311. [DOI] [PubMed] [Google Scholar]
- [13].James D, Pfaff J, Jeffries LM. Modified ride-on cars as early mobility for children with mobility limitations: a scoping review. Phys Occup Ther Pediatr. 2019;39(5):525–542. [DOI] [PubMed] [Google Scholar]
- [14].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- [15].WHO. International classification of functioning, disability and health: children and youth version: ICF-CY. Geneva: World Health Organization; 2007. [Google Scholar]
- [16].Law M, Stewart D, Letts L, et al. Guideline for critical review of qualitative studies. Hamilton: McMaster University Occupational Therapy Evidence-Bassed Practice Research Group; 1998. [Google Scholar]
- [17].O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. [DOI] [PubMed] [Google Scholar]
- [18].Wiart L, Kolaski K, Butler C, et al. Interrater reliability and convergent validity of the american academy for cerebral palsy and developmental medicine methodology for conducting systematic reviews. Dev Med Child Neurol. 2012; 54(7):606–611. [DOI] [PubMed] [Google Scholar]
- [19].Livingstone RW, Bone J, Field DA. Beginning power mobility: an exploration of factors associated with child use of early power mobility devices and parent device preference. J Rehabil Assist Technol Eng. 2020;7:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Huang HH, Chen CL. The use of modified ride-on cars to maximize mobility and improve socialization-a group design. Res Dev Disabil. 2017;61:172–180. [DOI] [PubMed] [Google Scholar]
- [21].Huang HH, Chen YM, Huang HW. Ride-on car training for behavioral changes in mobility and socialization among young children with disabilities. Pediatr Phys Ther. 2017;29(3):207–213. [DOI] [PubMed] [Google Scholar]
- [22].Zazula JL, Foulds RA. Mobility device for a child with phocomelia. Arch Phys Med Rehabil. 1983;64(3):137–139. [PubMed] [Google Scholar]
- [23].Huang HH, Ragonesi CB, Stoner T, et al. Modified toy cars for mobility and socialization: case report of a child with cerebral palsy. Pediatr Phys Ther. 2014;26(1):76–84. [DOI] [PubMed] [Google Scholar]
- [24].Logan SW, Huang HH, Stahlin K, et al. Modified ride-on car for mobility and socialization: single-case study of an infant with Down syndrome. Pediatr Phys Ther. 2014;26(4):418–426. [DOI] [PubMed] [Google Scholar]
- [25].Feldner HA. Impacts of early powered mobility provision on disability identity: a case study. Rehabil Psychol. 2019;64(2):130–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Logan SW, Catena MA, Sabet A, et al. Standing tall: feasibility of a modified ride-on car that encourages standing. Pediatr Phys Ther. 2019;31(1):E6–E13. [DOI] [PubMed] [Google Scholar]
- [27].Plummer T. Observed behaviors of a child while using an adapted ride-on car: a case study. APhOT. 2018;2(1):119. [Google Scholar]
- [28].Pritchard-Wiart L, Bragg E, Thompson-Hodgetts S. The young movers project: a case series describing modified toy car use as an early movement option for young children with mobility limitations. Phys Occup Ther Pediatr. 2019;39(6):598–613. [DOI] [PubMed] [Google Scholar]
- [29].Logan SW, Hospodar CM, Bogart KR, et al. Real world tracking of modified ride-on car usage in young children with disabilities. J Mot Learn Dev. 2019;7(3):336–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hospodar CM, Sabet A, Logan SW, et al. Exploratory analysis of a developmentally progressive modified ride-on car intervention for young children with Down syndrome. Disabil Rehabil: Assist Technol. 2020;2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Logan SW, Feldner HA, Bogart KR, et al. Perceived barriers of modified ride-on car use of young children with disabilities: a content analysis. Pediatr Phys Ther. 2020;32(2):129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Logan SW, Feldner HA, Galloway JC, et al. Modified ride-on car use by children with complex medical needs. Pediatr Phys Ther. 2016;28(1):100–107. [DOI] [PubMed] [Google Scholar]
- [33].Huang HH, Chen YM, Huang HW, et al. Modified ride-on cars and young children with disabilities: effects of combining mobility and social training. Front Pediatr. 2018;5:299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Huang HH, Huang HW, Chen YM, et al. Modified ride-on cars and mastery motivation in young children with disabilities: effects of environmental modifications. Res Dev Disabil. 2018;83:37–46. [DOI] [PubMed] [Google Scholar]
- [35].Chiulli C, Corradi-Scalise D, Donatelli-Schultheiss L. Powered mobility vehicles as aids in independent locomotion for young children. Suggestion from the field. Phys Ther. 1988;68(6):997–999. [DOI] [PubMed] [Google Scholar]
- [36].Restrepo P, Velasquez J, Munera S, et al. Adapting ride-on toy cars as a tool to promote leisure: a feasibility study in Colombia. Assist Technol. 2019;2019:1–6. [DOI] [PubMed] [Google Scholar]
- [37].Deitz J, Swinth Y, White O. Powered mobility and pre-schoolers with complex developmental delays. Am J Occup Ther. 2002;56(1):86–96. [DOI] [PubMed] [Google Scholar]
- [38].Logan SW, Lobo MA, Feldner HA, et al. Power-up: exploration and play in a novel modified ride-on car for standing. Pediatr Phys Ther. 2017;29(1):30–37. [DOI] [PubMed] [Google Scholar]
- [39].Logan SW, Feldner HA, Bogart KR, et al. Perceived barriers before and after a three month period of modified ride-on car use. Pediatr Phys Ther. 2020;32(3):243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Logan S, Ross SM, Schreiber MA, et al. Why we move: social mobility behaviors of non-disabled and disabled children across childcare contexts. Front Public Health. 2016;4:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].McWilliam RA. Birth to three: early intervention. In: Reichow B, Boyd B, Barton E, et al. , editors. Handbook of early childhood special education. Switzerland: Springer International Publishiing; 2016. [Google Scholar]
- [42].Dunst CJ, Bruder MB, Trivette CM, et al. Everyday activity settings, natural learning environments, and early intervention practices. J Policy Pract Intell Disabil. 2006;3(1):3–10. [Google Scholar]
- [43].Copley J, Ziviani J. Barriers to the use of assistive technology for children with multiple disabilities. Occup Ther Int. 2004;11(4):229–243. [DOI] [PubMed] [Google Scholar]
- [44].Huang IC, Sugden D, Beveridge S. Assistive devices and cerebral palsy: factors influencing the use of assistive devices at home by children with cerebral palsy. Child Care Health Dev. 2009;35(1):130–139. [DOI] [PubMed] [Google Scholar]
- [45].Østensjø S, Carlberg EB, Vøllestad NK. The use and impact of assistive devices and other environmental modifications on everyday activities and care in young children with cerebral palsy. Disabil Rehabil. 2005;27(14):849–861. [DOI] [PubMed] [Google Scholar]
- [46].Law M, King G. Parent compliance with therapeutic interventions for children with cerebral palsy. Dev Med Child Neurol. 1993;35(11):983–990. [DOI] [PubMed] [Google Scholar]
- [47].Basaran A, Karadayut KI, Uneri SO. Adherence to home exercise program among caregivers of children with cerebral palsy. Turk J Phys Med Rehabil. 2014;60:85–90. [Google Scholar]
- [48].Peplow UC, Carpenter C. Perceptions of parents of children with cerebral palsy about the relevance of, and adherence to, exercise programs: a qualitative study. Phys Occup Ther Pediatr. 2013;33(3):285–299. [DOI] [PubMed] [Google Scholar]
- [49].Taylor NF, Dodd KJ, McBurney H, et al. Factors influencing adherence to a home-based strength-training programme for young children with cerebral palsy. Physiotherapy. 2004;90(2):57–63. [Google Scholar]
- [50].King G, Law M, King S, et al. Children’s assessment of participation and enjoyment (CAPE) and preferences for activities of children (PAC). San Antonio: Harcourt Assessment; 2004. [Google Scholar]
- [51].Law M, Baptiste S, McColl M, et al. The canadian occupational performance measure: an outcome measure for occupational therapy. Can J Occup Ther. 1990;57(2):82–87. [DOI] [PubMed] [Google Scholar]
- [52].Chiarello LA, Palisano RJ, McCoy SW, et al. Child engagement in daily life: a measure of participation for young children with cerebral palsy. Disabil Rehabil. 2014;36(21):1804–1816. [DOI] [PubMed] [Google Scholar]
- [53].Bronfenbrenner U. The ecology of human development: experiments by nature and design. Cambridge (MA): Harvard University Press; 1979. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
There is no data set associated with this study.