Abstract
Purpose
Shift work has detrimental effects on healthcare workers, which may be further compounded by frontline work during the COVID-19 pandemic. We postulated that sleep would worsen and distress would increase during COVID-ward service.
Methods
Doctors (n = 18) were recruited from a tertiary centre during the second wave of the COVID-19 pandemic in Melbourne, Australia. Participants had been rostered ON to consecutive 7 day or night shifts and a week OFF over a fortnight. 9 worked on COVID wards managing positive/suspected COVID patients, and 9 were allocated to general MEDICAL wards. Participants wore wrist actigraphy, and completed the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and Kessler Psychological Distress Scale (K10) at baseline and the end of each week.
Results
Both the COVID and MEDICAL groups spent less time in bed and had reduced total sleep time during their week ON shift compared to week OFF shift. The COVID group had worse sleep quality (PSQI Δ + 1.0, 6.8 vs 5.8, p = 0.036), daytime sleepiness (ESS Δ + 2.6, 8 vs 5.4, p = 0.014) and greater distress (K10 Δ + 1.7, 17 vs 15.3, p = 0.002) during their week ON compared to BASELINE.
Conclusion
During the COVID-19 pandemic shift workers had poorer sleep during their week ON. Those working on COVID wards had greater distress during their week ON than those working on general MEDICAL wards. It is important to recognise the potential for sleep deficits and greater distress in medical workers during the pandemic.
Keywords: Shift work, COVID-19, Junior doctors, Mood, Sleep disturbance, Psychological distress
Introduction
Shift workers are susceptible to detrimental health effects associated with sleep loss due to circadian misalignment. These effects include increased sleepiness during waking hours [1], decreased mood, impaired neurocognitive function and poorer work performance [2–5]. Additionally, the current COVID-19 pandemic has placed extra burden on medical staff which has resulted in increased levels of reported sleep disturbance across frontline workers on a global scale [6–8]. In this study, we aimed to assess the effects of shift work on doctors’ sleep and mood whilst working on a COVID ward compared to doctors performing shift work on a standard medical ward.
Methods
During the COVID-19 pandemic’s second wave in Melbourne Australia, where there was a resurgence of case transmissions from June 2020 until its elimination in community viral transmission in November 2020 [9], 21 doctors were recruited from a tertiary hospital between August and December 2020. Over a 2-week period participants were rostered to their regular week of shift work with seven consecutive shifts (day or night) and a week off, in either order. 11 participants worked exclusively on the COVID ward treating only patients with confirmed or suspected COVID-19 infection (COVID), and 10 participants worked on the general medical wards with the same working conditions as prior to the COVID pandemic (MEDICAL).
In the COVID group, three of the 11 participants were rostered to seven consecutive night shifts during their week on, and the remainder worked seven consecutive day shifts. Two of the ten participants in the MEDICAL group worked nightshifts and eight worked day shifts. The duration of each shift varied between 10 and 12 h.
This study was approved by Eastern Health Ethics committee (approval number LR20/057) where during the fortnight, participants wore continuous wrist actigraphy (Actiwatch Spectrum Pro-MiniMitter Philips) and completed a sleep diary. Sleep diary was used as an aid to facilitate actigraphy analysis. Questionnaire data were collected at baseline (BASELINE), end of week on (ON) and end of week off (OFF). This comprised the Pittsburgh Sleep Quality Index (PSQI), the Epworth Sleepiness Scale (ESS), and the Kessler Psychological Distress Scale (K10), which provide subjective measures of sleep quality, daytime sleepiness, and psychological distress [10–12] and delta change measures were calculated between weeks ON and OFF. The change in questionnaire measures between groups were tested using t-tests, while the change within groups were tested using paired t-tests.
Results
Of the 21 participants, two withdrew from the study and one participant had incomplete data leaving 18 participants in total, nine in each group. There were no significant differences in age or gender between the groups with median age 28 years across the whole sample (range 23–49 years, p = 0.687), with five females in each. Comparing the COVID to MEDICAL group, there were no significant differences in baseline PSQI (CI − 0.098 to 4.53, p value = 0.191), ESS (CI − 1.651 to 3.873, p value = 0.406), or K-10 (CI − 4.72 to 2.95, p value = 0.630) scores (Fig. 1).
Fig. 1.
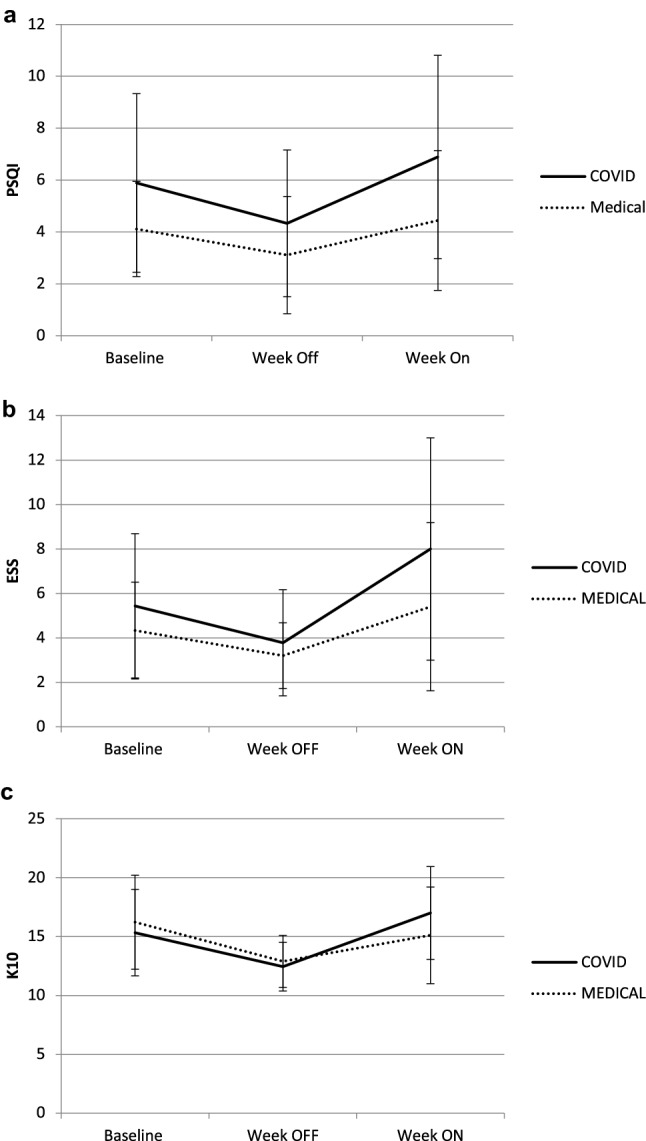
a Pittsburgh sleep quality index, b Epworth sleep scale. c Kessler psychological index. Mean scores and standard deviation at BASELINE, week OFF and week ON for doctors working in COVID-ward service and MEDCIAL service
PSQI
For the COVID group there was a significant improvement in PSQI during the week OFF (Δ − 1.6, 4.3 vs 5.9) and deterioration during week ON (Δ + 1.0, 6.9 vs 5.9) compared to baseline (p = 0.036). For the MEDICAL group there was no significant change in PSQI during week OFF (Δ − 1.0, 3.1 vs 4.1) or week ON (Δ + 0.3, 4.4 vs 4.1). Comparing COVID to MEDICAL there was no significant difference in the change in PSQI from baseline to week ON or OFF between groups (Fig. 1a). Overall the PSQI tended to be higher in the COVID group than the MEDICAL group at all 3 time points but did not reach statistical significance.
ESS
For the COVID group there was a significant improvement in ESS during the week OFF (Δ − 1.7, 3.7 vs 5.4) and deterioration during week ON (Δ + 2.6, 8 vs 5.4) compared to baseline (p = 0.014). For the MEDICAL group there was no significant change in ESS during week OFF (Δ − 1.1, 3.2 vs 4.3) or week ON (Δ + 1.1, 5.4 vs 4.3). Comparing COVID to MEDICAL there was no significant difference in the change in ESS from baseline to week ON or OFF between groups (Fig. 1b).
K10
For the COVID group there was a significant improvement in K10 during the week OFF (Δ − 2.9, 12.4 vs 15.3) and deterioration during week ON (Δ + 1.7, 17 vs 15.3) compared to baseline (p = 0.002). For the MEDICAL group there was a significant improvement in K10 during the week OFF (Δ − 3.3, 12.9 vs 16.2) and the week ON (Δ − 1.1, 15.1 vs 16.2) compared to baseline (p = 0.033). Comparing the COVID and MEDICAL groups, there was no significant difference in the change in K10 from baseline to the week OFF, but from baseline to week ON the COVID group was significantly worse (p = 0.04) than the MEDICAL group (Fig. 1c).
Actigraphy
According to actigraphy data, both COVID and MEDICAL groups had a significant decrease in total time in bed and total sleep time during their week ON compared to their week OFF (Table 1).
Table 1.
Actigraphy data for COVID and MEDICAL groups across week OFF and week ON
| COVID group week OFF | COVID group week ON | MEDICAL group week OFF | MEDICAL group week ON | |
|---|---|---|---|---|
| TIB (min) | 537 (± 81) | 432# (± 68) | 514 (± 36) | 448† (± 60) |
| TST (min) | 447 (± 46) | 374# (± 51) | 435 (± 37) | 380† (± 52) |
| SE (%) | 86 (± 5) | 87 (± 4) | 85 (± 5) | 86 (± 3) |
| BT (24 h notation hh:mm) | 23:40 (± 01:20) |
DS 23:45 (± 00:45) NS 08:59 (± 01:37) |
23:40 (± 01:15) |
DS 23:14 (± 00:21) NS 10:45 (± 02:39) |
| SOL (min) | 19 (± 19) | 14 (± 12) | 15 (± 6) | 15 (± 11) |
| WASO (min) | 44 (± 16) | 26 (± 8) | 42 (± 8) | 34 (± 11) |
| No. of awakenings | 29 (± 12) | 29 (± 9) | 33 (± 8) | 22 (± 10) |
TIB time in bed, TST total sleep time, SE sleep efficiency, BT bed time, DS day shift workers, NS night shift workers, SOL sleep onset latency, WASO wake after sleep onset
Data presented are mean (SD)
#p < 0.05 †p < 0.05
Discussion
During the COVID pandemic in Melbourne, doctors spent less time in bed and slept less overall during their week ON shift compared to week OFF measured objectively with actigraphy. This occurred irrespective of whether they were working frontline on the COVID ward or general MEDICAL ward. In examining different components of sleep episodes, we found that sleep efficiency was preserved and WASO and nocturnal awakenings did not change during week ON indicating that insufficient sleep time rather than sleep disruption was the major concern for this group. Changes in Bed Time recorded on actigraphy reflect the circadian rhythm changes affecting those on night shifts compared to day shifts. Subjectively, participants on COVID-ward service reported poorer sleep quality (on PSQI) and more daytime sleepiness (on ESS) during their week ON compared to BASELINE, whilst the opposite was true during their week OFF. Although those on general MEDICAL ward service did not change subjectively during their week ON, overall there was no significant difference in PSQI and ESS between the COVID and MEDICAL groups from BASELINE to week ON. Mood worsened in the COVID group (on the K10) during week ON compared to BASELINE and this was significantly worse than in the MEDICAL group. Part of this difference was explained by an unexpected improvement in mood in the MEDICAL group during week ON.
Our findings are consistent with literature which has assessed sleep and affective disorders in healthcare workers during the COVID-19 pandemic. For example, a systematic review and meta-analysis reported high rates of depression (31%) and sleep disorders (44%) in healthcare workers during the COVID-19 pandemic [7]. Shift work disorder and psychological distress has been identified in nursing cohorts during the COVID-19 pandemic [13–15] However, as far as we are aware our study is the first to demonstrate a significant worsening in sleep and mood during the week ON shift in doctors during the pandemic. Furthermore, we found that psychological distress was significantly worse in those working on the COVID ward compared to the general MEDICAL ward. Whilst we can only speculate as to the origin of the increased psychological stress (e.g. working in a high-pressure environment with increased personal protective equipment requirements), it has significant implications given that previous research has linked prolonged distress and clinician burnout in hospital settings [16]. Given the continued nature of the pandemic, our findings have implications for the continued health and safety of staff, and suggest that opportunities to obtain adequate sleep and maintain mental health are vital.
There are several limitations to the current study. This is a single centre study which limits the generalisability of the findings. The small sample size means negative results may be due to type 2 errors. In addition, although there were shifts in circadian rhythm sleep–wake times in night shifts compared to week off and day shift workers, the sample size prevented analysis of day versus night shifts in the study population. Future studies should examine differences based on shift type given that previous research has identified decreased health and productivity outcomes associated with night shift work [3], as well as higher impacts on social life outside of work [17]. However, this opportunistic real world study during the second wave of the COVID pandemic in Melbourne allowed collection of objective sleep data and detailed subjective data at three timepoints.
Conclusion
During the COVID-19 pandemic, medical staff performing shift work had less sleep opportunity and slept less during their week ON shift. Those working on the COVID ward had lower mood during their week ON shift, than those working on the general MEDICAL ward. The COVID-ward participants also had greater subjective sleep disturbance and daytime sleepiness during their week ON shift compared to baseline. It is important to recognise this sleep deficit for medical staff performing shift work during the COVID pandemic and in particular the potential detrimental effects on mood for those working exclusively on the COVID ward.
Funding
No funding was received for this research.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (name of institute/committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Folkard S. Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythms. Chronobiol Int. 2008;25:215–224. doi: 10.1080/07420520802106835. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher KE, et al. Effects of work hour reduction on residents’ lives. JAMA. 2005;294:1088–1100. doi: 10.1001/jama.294.9.1088. [DOI] [PubMed] [Google Scholar]
- 3.Ganesan S, et al. The impact of shift work on sleep, alertness and performance in health care workers. Sci Rep. 2019;9:4635. doi: 10.1038/s41598-019-40914-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gohar A, et al. Working memory capacity is decreased in sleep-deprived internal medicine residents. J Clin Sleep Med. 2009;5(3):191–197. doi: 10.5664/jcsm.27484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnedt JT, et al. Neurobehavioural performance of residents after heavy night call vs after alcohol ingestion. JAMA. 2005;294(9):1025–1033. doi: 10.1001/jama.294.9.1025. [DOI] [PubMed] [Google Scholar]
- 6.San Martin AH, et al. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep Med. 2020;75:388–394. doi: 10.1016/j.sleep.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marvaldi M, et al. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;216:252–264. doi: 10.1016/j.neubiorev.2021.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin YN, et al. Burden of sleep disturbance during COVID-19 pandemic: a systematic review. Nat Sci Sleep. 2021;13:933–966. doi: 10.2147/NSS.S312037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Milne GJ, et al. A modelling analysis of the effectiveness of second wave COVID-19 response strategies in Australia. Sci Rep. 2021;11:11958. doi: 10.1038/s41598-021-91418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kilgore WDS, et al. Daytime sleepiness is associated with altered resting thalamocortical connectivity. NeuroReport. 2015;26:779–784. doi: 10.1097/WNR.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 12.Mollayeva T, et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Bilgiç S, et al. Stress level and sleep quality of nurses during the COVID-19 pandemic. Work. 2021;70(4):1021–1029. doi: 10.3233/WOR-210538. [DOI] [PubMed] [Google Scholar]
- 14.Li Y, et al. Predictors of shift work sleep disorder among nurses during the COVID-19 pandemic: a multicenter cross-sectional study. Front Public Health. 2021;9:785518. doi: 10.3389/fpubh.2021.785518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Subhas N, et al. The cross-sectional relations of COVID-19 fear and stress to psychological distress among frontline healthcare workers in Selangor, Malaysia. Int J Environ Res Public Health. 2021;18(19):10182. doi: 10.3390/ijerph181910182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higuchi Y, et al. A cross-sectional study of psychological distress, burnout and the associated risk factors in hospital pharmacists in Japan. BMC Public Health. 2016;16:534. doi: 10.1186/s12889-016-3208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martyn J, et al. Do polish nurses have a problem with sleepiness during the epidemiological threat of the SARS-CoV-2 virus? Inquiry. 2021;58:469580211022909. doi: 10.1177/00469580211022909. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.


