Abstract
Background
COVID-19 vaccinations applied in pharmacies can facilitate accessibility and potentially increase the vaccination rate but remain controversial in many countries. This study aimed to explore the patients’ motivation to receive their COVID-19 vaccination in a pharmacy and examine patient and provider satisfaction with this novel service.
Methods
The study was designed as an explorative cross-sectional multicenter in-house quantitative survey and was conducted during the first weeks of COVID-19 vaccinations in German pharmacies from February to April 2022. The survey consisted of a paper-based questionnaire with scaling questions, multiple choice questions and open questions. Patients were recruited consecutively before their vaccination and completed the survey directly after the service. Vaccinating pharmacists were also invited to answer a questionnaire on their experiences, motivation and expectations.
Results
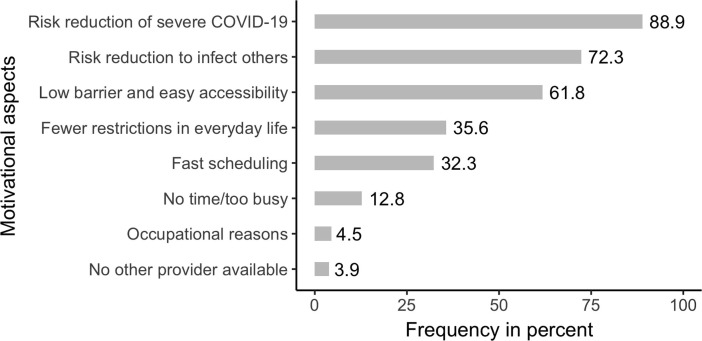
A total of 427 questionnaires out of 11 pharmacies were be included. The overall patient satisfaction with vaccinations in pharmacies was rated with the highest remarks by 91.5% of the participants, another 7.8% were fairly satisfied. Patient satisfaction with scheduling, waiting time, information, hygiene, vaccination technique and a feeling of safety was very high (96.5–97.9%). Patients’ motivation on COVID-19 vaccination was to prevent severe COVID-19 symptoms (88.9%) and to protect others (72.3%). Easy accessibility, low barriers and proximity were other reasons for utilizing this service, mentioned by 61.8% of the patients. Pharmacists were highly motivated and found the task meaningful but experienced considerable personnel shortage. General practitioners rather expressed relief on their workload.
Conclusions
Data of this study strongly supports to include pharmacies as additional providers of COVID-19 vaccinations. Patients stated marked satisfaction with this setting and expressed a feeling of safety and trust. Whereas most patients may have utilized the service for convenience, easy accessibility and low barriers were appreciated and can potentially contribute to higher vaccination rates.
Keywords: Vaccination, COVID-19, Pharmacist, Clinical pharmacy service, Patient satisfaction, Questionnaire
1. Introduction
Pharmacies across the world play a crucial role in fighting the SARS-CoV-2 pandemic [1]. Educating the population, testing patients and distributing masks, disinfectants and vaccines, provided a quick response and remained a strong column in disease control throughout the pandemic [1], [2]. Reaching out for high vaccination rates however remains a challenge for most societies, despite its undoubtful effects on morbidity and mortality [3]. Easy accessibility is an obvious way to enhance acceptance. Whereas some healthcare systems offer vaccinations through their existing facilities, others try to reach people where they live, where there work or where they play [4]. One approach to facilitate COVID-19 vaccinations is to include community pharmacies to the range of providers [5]. There is a long history of vaccinations by pharmacists in the United States, dating back to as early as 1996 [6], [7]. A recent survey found that pharmacies are regarded as ideal vaccination settings by the population [8]. However, by spring 2021 only few jurisdictions in Europe permitted pharmacists to conduct COVID-19 vaccinations [1], [9], [10], [11], [12]. Moreover, there is a sometimes shameful controversy among healthcare providers on who is eligible to provide vaccinations and who is not, instead of reaching out for higher vaccination rates [13], [14]. In Germany, pharmacies were offered a medical education course in January 2022 and the first COVID-19 vaccinations were administered on February 8, 2022 as a novel clinical pharmacy service for all patients ≥ 12 years of age.
1.1. Aims
This study aimed to explore patient and provider satisfaction with COVID-19 vaccinations in pharmacies and their motivation. Insight in potential barriers and facilitators of vaccinations by pharmacists were expected to help adopting the service according to population needs and hence contribute to increase the vaccination rates.
2. Methods
The study was designed as a cross-sectional multicenter in-house survey. Community pharmacies in Germany were invited to participate by an editorial appeal, published in the Deutsche Apotheker Zeitung (DAZ) in February 2022. The DAZ is a widespread weekly journal for pharmacists, which is subscribed by most of the 18,500 pharmacies in the country. Patients of participating pharmacies willing to be vaccinated were recruited consecutively within the initial ten weeks of performing this novel service, from February 8 until April 15, 2022. Patients were offered mRNA-based (Comirnaty®, Spikevax®) and later also protein-based (Nuvaxovid®) vaccines during the study time. Both vaccines needed to be prepared and reconstituted in the pharmacy before administration. Pharmacists were free to vaccinate by appointment or spontaneously.
Before each vaccination, the questionnaire and the study information were provided to all patients upon verbal consent to participate. Participants completed the paper-based questionnaire after vaccination and while they were being observed for tolerability and waited for their vaccination certificates. The questionnaires were inserted into a ballot box after filling. The survey could also be answered with the help of a family member (especially in patients younger than 18 years old) or caregiver. Participation was voluntary and data were collected anonymously. Patients who could not read German language or denied participation were excluded. By the end of the study period, vaccinating pharmacists were also invited to answer a questionnaire on their experiences, motivation, collaboration and expectations.
The ethics committee of the University of Wuppertal has approved the study (Az: MS/AE 220223).
2.1. Instruments
The patient survey included self-developed items which were structured by six different domains:
-
•
demographics characteristics of the patient, including the number of previously received COVID-19 vaccinations, age group and gender
-
•
perceived quality of the vaccination service: making the appointment, waiting time, quality of provided information, education, hygiene, vaccination technique and perceived safety (on 4-point Likert scales)
-
•
overall satisfaction with the vaccination service applied (on a 5-point Likert scale)
-
•
motivation in terms of general accessibility of a COVID-19 vaccination and anticipated benefits (by multiple options questions)
-
•
an open-ended question was provided to permit patients to express further comments
Survey development was informed by Boynton et al. [15]. To receive a high response rate the questionnaire was designed to be completed anonymously in at least 7 min. To further collect information on participating pharmacies, key persons of each pharmacy were asked by a separate short-questionnaire. All questions for pharmacists were multiple choice questions, some of them with free text fields for additional comments.
2.2. Statistical analyses
Data were analyzed descriptively and stratified by pharmacy, where applicable, to depict the heterogeneity between organizations. Due to the explorative nature of this investigation and the low case numbers in some participating pharmacies, we did not apply statistical testing. Missing data were listwise deleted. Closed-ended survey questions were analyzed using SPSS Statistics version 27 (IBM, Chicago, Illinois, USA). Qualitative data analysis was driven by the following question: “what prompted you to have the vaccination done today?” To systematically explore the content of this open-ended survey question, analysis was conducted by three researchers. Therefore, we imported the answers to Microsoft® Excel® 2016 (Microsoft, Redmond, Washington, USA). Themes were created by developing a set of codes during the first step. Codes were inductively interpreted by the first researcher (OR) and a final set of key codes was developed. The second (SE) and third researcher (JKN) coded the data and reviewed each other’s coding to ensure completeness and accuracy. Three main themes emerged: ease of scheduling, perceived fit within daily routine and proximity of the pharmacy.
3. Results
3.1. Sample description
A total of eleven pharmacies participated in the study and 427 patients were recruited between February 8 and April 15, 2022. There were no refusals to participate and all 427 questionnaires were included into analyses. Pharmacies were located in the states of North Rhine-Westphalia, Lower Saxony and Hamburg, and in small towns (<50,000 inhabitants, n = 9; 81.8 %) as well as in urban (50,000 to ≤ 500,000 inhabitants, n = 1; 9.1 %) or metropolitan areas (>500,000 inhabitants, n = 1; 9.1 %). Key persons of the participating pharmacies were between 30 and 39 years of age (n = 5; 45.5 %) or between 50 and 59 years old (n = 5; 45.5 %). There was only one younger pharmacist in the age group of 20–29 years engaged and nobody at the age group of 40–49 years. Participants came from ten out of eleven pharmacies. With one exception, all pharmacies stated that they expected to have more regular than casual patients than the average German pharmacy. COVID-19 vaccinations were administered only by appointment. Appointments were scheduled either online or in person during a visit to the pharmacy. Almost all vaccinations offered and chosen by the patients were mRNA-based. In nine cases Nuvaxovid® was administered in only one out of the eleven pharmacies. All pharmacies were provided with an emergency algorithm and an epinephrine pen but reported no accidents or acute reactions during the study period. In one case the needle was not properly fixed and fell off the syringe. Pharmacists reported no adverse drug reactions during vaccination and observation and no incidence of needle or blood-related fainting. There were no dropouts among the included patient and provider questionnaires and only few data were omitted, mainly on demographics and the number of previously received vaccinations.
The majority of surveyed patients were 50 years and older (n = 259; 60.9 %), with 132 patients between 18 and 49 years of age (31.1 %). Teenagers ≥ 12 years and younger than 18 years were also included (n = 34; 8 %). Two participants did not indicate their age group. More than half of the participating patients were female (57.1 %) and used the new vaccination service of the pharmacy mainly for their third or fourth COVID-19 vaccination (34.6 % vs 59.6 %). Only 1.2 % percent of the item responders indicated the service as their first vaccination. Table 1 summarizes the complete sample characteristics.
Table 1.
Patient baselines and characteristics.
| Characteristics | Survey responder n (%) |
|---|---|
| Age group | |
| 12–17 | 34 (8) |
| 18–29 | 53 (12.5) |
| 30–39 | 41 (9.6) |
| 40–49 | 38 (8.9) |
| 50–59 | 60 (14.1) |
| 60–69 | 75 (17.6) |
| 70–79 | 88 (20.7) |
| 80 and older | 36 (8.5) |
| total item responses | 425 (99.5) |
| Gender | |
| male | 139 (42.6) |
| female | 186 (57.1) |
| diverse | 2 (0.3) |
| total item responses | 326 (76.3) |
| COVID-19 Vaccination | |
| First | 5 (1.5) |
| Second | 15 (4.4) |
| Third | 119 (34.6) |
| Fourth | 205 (59.6) |
| total item responses | 344 (80.6) |
3.2. Perceived quality of the vaccination service and overall satisfaction
Responses to survey items on perceived quality of the vaccination service showed very high satisfaction. Upon arranging an appointment, 96.5 % of the participants strongly agreed that it was very easy to fix the planning (412 out of 427). Another 97.2 % (414 out of 426 responses without missing values) strongly rated their waiting time as appropriate. The quality of provided information, hygiene, observed and experienced vaccination techniques was also perceived to be on a very high professional level (see Table 2 ). Furthermore, 97.9 % of the patients (418 out of 427) strongly stated that they felt safe during vaccination in the pharmacy. The overall satisfaction with the vaccination service applied was rated by 425 patients (99.5 % of the total sample) and 91.5 % (n = 398) were completely satisfied with the vaccination service, 7.8 % (n = 33) rated the service as good and 0.7 % (n = 3) as fairly satisfied. No participant rated the received services as “rather not satisfied” or “not satisfied at all”. All ratings were homogeneous over the participating pharmacies, gender and age groups.
Table 2.
Perceived quality of the vaccination service and satisfaction with it.
| Items of satisfaction | n (%) |
|---|---|
| It was easy for me to make an appointment for COVID-19 vaccination in the pharmacy | |
| strongly agree | 412 (96.5) |
| agree | 15 (3.5) |
| disagree | 0 (0) |
| strongly disagree | 0 (0) |
| total item responses | 427 (1 0 0) |
|
The waiting time in the pharmacy to get the vaccination was appropriate strongly agree agree disagree strongly disagree |
414 (97.2) 12 (2.8) 0 (0) 0 (0) |
| total item responses | 426 (99.8) |
| Information on the vaccine, risk and adverse effects was provided in a professional and understandable manner | |
| strongly agree | 409 (97.6) |
| agree | 9 (2.1) |
| disagree | 1 (0.3) |
| strongly disagree | 0 (0) |
| total item responses | 419 (98.1) |
| Hygiene and vaccination techniques seemed to follow high quality standards | |
| strongly agree | 409 (97.8) |
| agree | 8 (1.9) |
| disagree | 1 (0.2) |
| strongly disagree | 0 (0) |
| total item responses | 418 (97.9) |
| During my vaccination I felt comfortable and safe | |
| strongly agree | 418 (97.9) |
| agree | 8 (1.9) |
| disagree | 0 (0) |
| strongly disagree | 1 (0.2) |
| total item responses | 427 (1 0 0) |
| Overall, I am satisfied with the COVID-19 vaccination service received | |
| completely | 389 (91.5) |
| good | 33 (7.8) |
| fairly | 3 (0.7) |
| rather not | 0 (0) |
| not at all | 0 (0) |
| total item responses | 425 (99.5) |
3.3. Patient motivation
Survey items on motivation were rated by 424 respondents and were homogeneous over the participating pharmacies. The great majority of participating patients (93.4 %; n = 399) stated that they were motivated to get the vaccination to reduce their own risk of severe symptoms (88.9 %; n = 377) or to protect others from infection (72.3 %; n = 306). Another 35.6 % (n = 151) of patients stated fewer restrictions in everyday life as a motivational factor, only 4.5 % (n = 19) of surveyed patients named occupational reasons, like being prompted by law or by the employer. Additionally, participants indicated that utilization of the COVID-19 vaccination service in pharmacies was mainly driven by the low barrier, the easy accessibility and the fast scheduling. Availability as a facilitator was underlined by 12.8 % of patients who stated that they had no time to visit a physician during business hours. On the other hand, low accessibility of a general practitioner or other physician or vaccination center was rarely mentioned to play a role when deciding for the pharmacies’ vaccination services (see Fig. 1 ).
Fig. 1.
Motivational aspects for patients to get the COVID-19 vaccination in a pharmacy.
3.4. Qualitative outcomes
Even though patients were vaccinated in all pharmacies only by appointment, patients frequently praised easy and short-term scheduling by using the open-ended question and the free-text field: “fast and straightforward scheduling”, “making an appointment was fast and easy”,”short-term vaccination close by”, “appointment without any difficulty”, “my general practitioner prefers other patient groups”, “online scheduling was superb”, “registration was without any problems”.
Some patients explicitly mentioned the convenient time slots after work as a motivation or chance for them to get the vaccination: “as I usually have time in the evening, that is why I came for vaccination”, “occasion to get the vaccination on a Sunday”, “due to work I only have time at the weekend”.
The proximity of the pharmacy was mentioned several times. Some patients stated that they preferred this close-by service over the vaccination centers, which offered COVID-19 vaccinations on a county level and were perceived as being quite remote for the patients: “jab in the neighborhood, vaccination center too far away, petrol is expensive”, “close-by”, “nicely close to where I am living”, “was the fastest way to get the vaccination in this area”. One patient (≥80 years old) stated that this was his first vaccination since early childhood as he was afraid of the needle stick. Easy accessibility prompted him to overcome his fears. There were many thanks and smiles in the free-text field.
3.5. Pharmacists’ perspective
Feedback on motivation, experiences and attitudes was recorded from ten out of eleven participating pharmacies. All responding pharmacists (n = 11) reported that they felt that their COVID-19 vaccinations were meaningful, that patients were grateful and that they enjoyed this new professional service. To recruit a team for vaccinations was difficult in all pharmacies due to existing work overload and personnel shortage. Almost all pharmacies provided vaccinations either during quiet time slots (n = 4) or outside of regular opening times (n = 9). Pharmacy technicians were part of the vaccination team in most pharmacies and supported with ordering vaccines, scheduling patients, reconstitution of the vaccines and documentation (vaccination certificates and pharmacy documentation system). Information on potential risks, adverse reactions and education on the vaccination was provided solely by pharmacists in all cases. When asked on feedback of physicians, four pharmacists reported that they received thanks for relief, four pharmacists didn‘t get any feedback from physicians and two pharmacists experienced complaints on the competition. All pharmacists expressed their trust that they will continue to provide COVID-19 vaccinations “because it is important and meaningful” or because “we are a highly motivated team”, three of them said that they would appreciate single-dose units very much to reduce waste in the future. Further barriers for permanent implementation which were mentioned were “not enough space in the pharmacy” and “limited personnel staffing”. Reimbursement was criticized as not sufficient by some pharmacists.
4. Discussion
This survey explored the novel clinical pharmacy service of COVID-19 vaccinations in Germany for the first time. To the best of our knowledge, there were no comparable field research studies on vaccinations by German pharmacists to date published in peer-reviewed journals in other indications as well. Previous experiences with vaccinations in German pharmacies were very limited. Apart from a model project with certain pharmacies and a particular health insurance, most pharmacies in the country had no experience with administering vaccinations. The study was planned along with pharmacists training to qualify for vaccination and started on the very first day of the new regulation. It was conducted as an evaluation of the very early phase of COVID-19 vaccinations in pharmacies and was intended to provide insight into facilitators and barriers, which could be modified to optimize outcomes later on. Studies by Stämpfli et al., Burt et al. and Sepp et al. on influenza vaccinations and by Stämpfli et al. on COVID-19 vaccinations in Switzerland followed a similar approach and inspired this survey [10], [16], [17], [18]. Whereas Stämpfli et al. focused on healthcare outcomes, Burt et al. investigated marketing aspects. Sepp et al. explored the pharmacists’ attitude on vaccinations. Our survey tried to gain insight into perceived professionalism, standards and a feeling of safety at the novel setting as well as in the motivation to embrace this service. Another aspect was to receive information on existing barriers and facilitators from the providers’ view. Sampling sizes of Stämpfli et al. (n = 421) and Burt et al. (n = 436) were comparable to this study (n = 427) [10], [17]. The demographic distribution showed that all age groups accepted pharmacies as vaccination settings with no differences in perception. Satisfaction with timing, waiting time, hygiene, injection technique and a feeling of safety was extremely high for all patients, which corresponded to the previous mentioned international studies and was even higher than in the Swiss study, which used a 6-point Likert scale though [10]. A qualitative result regarding the provider perspective was that physicians rather seemed to appreciate the relief by vaccinating pharmacists. After one year of COVID-19 vaccinations, it seemed that general practitioners were exhausted by the SARS-CoV-2 pandemic, by scheduling patients for vaccinations and by struggling with conflicting medical routine care. This impression to some of the pharmacists differed to the pronounced statements of the German National Association of Statutory Health Insurance Physicians, which regards the pharmacies as irritating competitors and doubts positive evaluations [19]. However, pharmacies had marked difficulties to offer vaccinations during standard operating hours. This might be partly caused by personnel shortage and partly by the immediate action, which didn‘t permit much preparation time for the pharmacies. In some cases, the time slots at evening or on the weekend were intended to reach busy workers and to provide an additional opportunity. Pharmacists reported no complications or acute adverse or allergic reactions, which is in line with results by Papastergiou et al. regarding influenza immunizations [20] and with the low rate of complications from large population studies and data from pharmacovigilance systems [21]. Epinephrine, which was on standby in all pharmacies, was not applied. Governmental reimbursement of 28 Euros per shot (36 Euros on weekends) was criticized as not sufficient by some pharmacists, as reconstitution, patient education and documentation were time-consuming.
4.1. Limitations
Even though the number of respondents was high, the number of participating pharmacies was limited. An explanation might be that recruitment of pharmacies was done even before the initial phase of introducing vaccinations to pharmacies, when only few pharmacists were prepared. The early stage was chosen to utilize the gained insight in optimizing and amending the campaign with the aim to increase the applied vaccinations over time. Pharmacies did not extensively depict different city sizes and states of Germany but the homogenous results indicate that potential differences might be small. The number of questions in the questionnaire were limited with respect to feasibility. More comprehensive interviews could have led to different results. Typical advantages of a questionnaire, like quickly gaining data, easy standardization, first-hand information and respondent comfort, were opposed by disadvantages like answer dishonesty and potentially inaccurate responses. This survey covered patients in the pharmacy only, which imposes a selection bias.
5. Conclusions
As authorities and healthcare providers in Europe and other countries grapple with COVID-19 vaccinations in pharmacies, this survey provides insight into patients’ and providers’ motivation and satisfaction with this novel service. Patients of all age groups stated high trust and confidence in the pharmacists’ ability to inform and educate. They have been extremely satisfied with the skills, the setting and praised easy scheduling. Patients chose the pharmacy due to convenience, accessibility and availability, which might enhance vaccination rates in an underserved population and relief some pressure during pandemic waves in the future. Pharmacists experienced vaccinations as a meaningful activity but could cover the additional burden only with difficulties, overtime hours and mostly when the pharmacies were closed. Pharmacy technicians assisted only at times and in selective activities, which might be due to the early stage of introducing the service and intensive control by the pharmacists, who did most parts of the vaccinations themselves. Physicians rather appreciated the relief by pharmacists. Data of this survey clearly supports utilization of vaccinating pharmacies in fighting infectious diseases and pandemics.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
The authors would like to thank Andreas Bröck, Dr. Dorothee Dartsch, Melanie Elfers, Nawal El Shamsy, Johanne Elias, Anton Justus, Anna Martens, Dorothee Michel, Dr. Hannes Müller, Edward Mosch, Steffen Johannes Schmidt, Julia Trost and Johanna Weitzel on behalf of all participating pharmacists. We acknowledge their valuable contributions.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
Data will be made available on request.
References
- 1.Costa S., Romão M., Mendes M., Horta M.R., Rodrigues A.T., Carneiro A.V., et al. Pharmacy interventions on COVID-19 in Europe: Mapping current practices and a scoping review. Res Social Adm Pharm. 2022;18(8):3338–3349. doi: 10.1016/j.sapharm.2021.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maidment I., Young E., MacPhee M., et al. Rapid realist review of the role of community pharmacy in the public health response to COVID-19. BMJ Open. 2021;11(6) doi: 10.1136/bmjopen-2021-050043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conlon A., Ashur C., Washer L., Eagle K.A., Hofmann Bowman M.A. Impact of the influenza vaccine on COVID-19 infection rates and severity. Am J Infect Control. 2021;49(6):694–700. doi: 10.1016/j.ajic.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ezeude G.I., Glover K.R., Nieves Santiago A.A., et al. Roadblocks and successes in preparing COVID-19 vaccination clinics: Perspectives from pharmacy residents. Am J Health Syst Pharm. 2022;79(2):102–109. doi: 10.1093/ajhp/zxab347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Czech M., Balcerzak M., Antczak A., Byliniak M., Piotrowska-Rutkowska E., Drozd M., et al. Flu Vaccinations in Pharmacies-A Review of Pharmacists Fighting Pandemics and Infectious Diseases. Int J Environ Res Public Health 2020;17(21) 2020;17(21):7945. doi: 10.3390/ijerph17217945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hogue M.D., Grabenstein J.D., Foster S.L., Rothholz M.C. Pharmacist involvement with immunizations: a decade of professional advancement. Journal of the American Pharmacists Association. 2006;46(2):168–182. doi: 10.1331/154434506776180621. [DOI] [PubMed] [Google Scholar]
- 7.Richardson W.M., Wertheimer A.I. A Review of the Pharmacist as Vaccinator. Innov Pharm 2019;10(3) 2019;10(3):4. doi: 10.24926/iip.v10i3.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kowalczuk A., Wong A., Chung K., et al. Patient Perceptions on Receiving Vaccination Services through Community Pharmacies. Int J Environ Res Public Health. 2022;19(5) doi: 10.3390/ijerph19052538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paudyal V., Fialová D., Henman M.C., Hazen A., Okuyan B., Lutters M., et al. Pharmacists’ involvement in COVID-19 vaccination across Europe: a situational analysis of current practice and policy. Int J Clin Pharm. 2021;43(4):1139–1148. doi: 10.1007/s11096-021-01301-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stämpfli D., Martinez-De la Torre A., Simi E., Du Pasquier S., Berger J., Burden A.M. Community Pharmacist-Administered COVID-19 Vaccinations: A Pilot Customer Survey on Satisfaction and Motivation to Get Vaccinated. Vaccines (Basel) 2021;9(11):1320. doi: 10.3390/vaccines9111320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turcu-Stiolica A., Kamusheva M., Bogdan M., Tadic I., Harasani K., Subtirelu M.-S., et al. Pharmacist's Perspectives on Administering a COVID-19 Vaccine in Community Pharmacies in Four Balkan Countries. Front Public Health 2021;9:766146. 2021;9 doi: 10.3389/fpubh.2021.766146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirkdale C.L., Nebout G., Taitel M., Rubin J., Jacinto I., Horta R., et al. Implementation of flu vaccination in community pharmacies: Understanding the barriers and enablers. Annales Pharmaceutiques Françaises. 2017;75(1):9–16. doi: 10.1016/j.pharma.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 13.MacDougall D., Halperin B.A., Isenor J., MacKinnon-Cameron D., Li L., McNeil S.A., et al. Routine immunization of adults by pharmacists: Attitudes and beliefs of the Canadian public and health care providers. Hum Vaccin Immunother. 2016;12(3):623–631. doi: 10.1080/21645515.2015.1093714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Can Pharm J (Ott) 2021;154(2):76. 2021, doi: 10.1177/1715163521997319. doi:10.1177/1715163521997319 [published Online First: 22 February. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boynton P.M., Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ. 2004;328(7451):1312–1315. doi: 10.1136/bmj.328.7451.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stämpfli D., la Torre A.-D., Du Pasquier S., Stegmann D., Brügger A., Burden A.M. Community pharmacist-administered seasonal influenza vaccination: a national customer survey. J Pharm Policy Pract 2020;13:57. 2020;13(1) doi: 10.1186/s40545-020-00259-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burt S., Hattingh L., Czarniak P. Evaluation of patient satisfaction and experience towards pharmacist-administered vaccination services in Western Australia. Int J Clin Pharm. 2018;40(6):1519–1527. doi: 10.1007/s11096-018-0738-1. [DOI] [PubMed] [Google Scholar]
- 18.Sepp K., Kukk C., Cavaco A., Volmer D. How involvement of community pharmacies improves accessibility to and awareness about flu vaccination? – An example from Estonia. Expert Review of Vaccines. 2020;19(10):983–990. doi: 10.1080/14760584.2020.1825949. [DOI] [PubMed] [Google Scholar]
- 19.Kassenärztliche Bundesvereinigung. „Impfen ist und bleibt originär ärztliche Aufgabe“ 2022. Available at: https://www.kbv.de/html/2022_57983.php Accessed February 11, 2022.
- 20.Papastergiou J., Folkins C., Li W., Zervas J. Community pharmacist-administered influenza immunization improves patient access to vaccination. Can Pharm J (Ott) 2014;147(6):359–365. doi: 10.1177/1715163514552557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shimabukuro T.T., Cole M., Su J.R. Reports of Anaphylaxis After Receipt of mRNA COVID-19 Vaccines in the US-December 14, 2020-January 18, 2021. JAMA. 2021;325(11):1101–1102. doi: 10.1001/jama.2021.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.