Abstract
The prevention of a complex phenomenon, such as suicide, requires an interdisciplinary approach that provides a comprehensive response to the care needs of people with suicidal behavior (SB). The aim of this study is to investigate the clinical and healthcare features of people presenting thoughts and/or attempts of suicide to define risk factors for recurrence.
ABSTRACT
Introduction
The prevention of a complex phenomenon, such as suicide, requires an interdisciplinary approach that provides a comprehensive response to the care needs of people with suicidal behavior (SB). The aim of this study is to investigate the clinical and healthcare features of people presenting thoughts and/or attempts of suicide to define risk factors for recurrence.
Methods
A cohort study was carried out with a 6-month follow-up. The cohort consisted of persons admitted to the emergency department of the Hospital Universitario Marqués de Valdecilla (Santander) presenting thoughts and/or attempts of suicide, throughout a 4-month recruitment period: 1-March to 30-June 2015. Sociodemographic and clinical variables were collected in the index episode and visits to the emergency department during the following 6 months.
Results
143 patients were assessed by SB, and it was possible to collect information on recurrence in 110 (average age of 43.31; range 16-84; 65% women). Twenty-one percent presented recurrence of SB: 10% attempted, 6% thoughts, and 5% both; 1 (0.7%) committed suicide; most frequently with age 30-65 years and with a history of mental illness. During follow-up, 60% consulted repeatedly in the emergency department not only for SB but also for other psychiatric or medical reasons, independently of follow-up in the mental health service.
Conclusions
Recurrence of SB is common despite being followed up in the mental health service. In addition, people with SB frequently and repeatedly consult the emergency department for other psychiatric and medical reasons, suggesting that the conventional approach to comorbidity with SB is insufficient. Further studies are needed to define risk profiles and design specific interdisciplinary strategies for SB management and suicide prevention, avoiding fragmentation. This will contribute more efficiently to early identification, appropriate management and prevention of suicide recurrences and deaths.
INTRODUCTION
The World Health Organisation (WHO) reports that nearly one million people worldwide die by suicide each year and encourages national suicide prevention programmes(1). Suicide is one of the three leading causes of death among people in the most productive age groups (15-44 years) and the second leading cause of death in the 15-19 age group worldwide(2). Since 2010, suicide is the leading cause of death due to external factors in Spain, even ahead of traffic accidents, which it doubles in number, with an increasing trend in both absolute terms and rates(3). While Cantabria remains having one of the lowest rates in the country, the truth is that this increasing trend has also been maintained up to 2016(3).
Suicide is a multifaceted phenomenon. While its causes are not fully understood, we have evidence suggesting that it is probably the result of a complex combination of neurobiological and environmental factors, in which personality, cognitive aspects and early negative events are key determinants of suicidal behaviour across the lifespan(4)-(5). Extensive evidence suggests that the best predictor of risk for future attempt and completed suicide is previous suicide attempts(5)-(9), becoming 30 to 100 times more frequent in comparison to the general population without previous attempts(6)-(8)-(10). Suicidal thoughts also play an important role in suicide prevention(11)–(13) and onethird of suicide attempts were found preceded by suicidal ideation over the previous 6 months(14), which is similar to figures reported in recurrence of suicide attempts after a previous attempt(10).
Most population-based and cohort studies about suicide attempts find a higher frequency in women, aged between the 2nd-4th decades of life, unemployed and without a partner, who use drug poisoning(6)-(10)-(11)-(15)-(16). Concerning clinical variables, the existence of psychiatric pathology is the greatest individual risk factor found in the literature(10)-(11)-(14)-(17)-(18) but certain features such as impulsivity and hopelessness also increase the risk of suicide attempts(5)-(9)-(19)-(21). Moreover, there is substantial evidence showing that chronic medical illness resulting in functional disability or chronic pain is associated with an increased risk of suicidal thoughts, attempts and completed suicide(22)-(25), even in the absence of mental illness(23)-(24) and most particularly in elderly groups(25)-(26). In addition, certain health conditions such as essential hypotension(27) or asthma(26) have been associated with increased risk of suicidal behaviour.
The aim of this study is to identify the socio-demographic and clinical profile of people showing suicidal behaviour (attempts and/or thoughts) on admission to the emergency department and follow-up both the recurrence of suicidal behaviour and emergency consultations for other medical or psychiatric reasons in the 6 months following this index episode, with the purpose of determining a more comprehensive approach to their healthcare needs.
METHODS
A Pilot Study was carried out in 2015 to estimate the prevalence of suicidal behavior in Cantabria, in preparation for the design of a Suicide Prevention Program. For this purpose, the systematic collection of sociodemographic, clinical and assistance data related to people who attended the Emergency Department of University Hospital Marqués de Valdecilla in Santander (Cantabria, Spain) (HUMV) with Suicidal Thoughts and/or Attempts during a 4-month period (March 1-June 30) was implemented. They were also monitored during the following 6 months. The results of this study reveals fairly accurate information about the number of people consulting for suicidal behavior in Cantabria (population: 585,179), considering that this hospital is the only one with on-site emergency psychiatric care 24 hours a day, all 365 days a year. There may be a downward discrepancy if some people with suicidal thoughts or attempts were treated in other healthcare services available in the network, without being referred to the Emergency Department of the HUMV.
Design: a cohort study with 6-month follow-up.
Setting: emergency department of the University Hospital Marqués de Valdecilla (Santander, Cantabria, Spain).
Study period: from March 1 to June 30, 2015.
Subjects: during these 4 months, 143 patients were assessed by the on-call psychiatrist for suicide attempts and/or suicidal thoughts (index episode). During the 6-month follow-up after the index episode, information in the electronic health record (EHR) of the Cantabrian Health Service (SCS) was available for only 110 of them, who constitute the monitoring group. In observance of international standards in research ethics, this study was conducted with the approval of the Ethics Committee for Research, Medicines and Medical Devices (CEIm) of Cantabria.
Variables were collected at two moments: At the index episode: antecedents, typology of suicidal behaviour, socio-demographic data, clinical parameters, DSM-IV-R diagnostic category and assistance data. We obtained this information from the anamnesis and mental state examination carried out by the on-call psychiatrist, following a standardised assessment in accordance with the recommendations of the Clinical Practice Guide for the Prevention and Treatment of Suicidal Behaviour of the Ministry of Health(29). The SAD PERSONS suicide risk scale(30) was also completed as a summary of this assessment.
At 6 months, using the information in the EHR: recurrence of suicidal behaviour, emergency consultations for other psychiatric or medical reasons, hospital admissions, contacts with outpatient mental health services and the eventuality of death by suicide or other causes, during the 6 months following the index episode.
Data analysis: a descriptive analysis of the socio-demographic and clinical variables of the sample was performed at the time of the index episode (frequencies and means) and a further comparative analysis between the two groups with and without suicidal recurrence during follow-up (contingency tables, chi-square).
RESULTS
During the 4 months of the pilot study a total of 143 people were seen for suicidal behaviour. This figure represents a daily average of 1-2 emergency consultations for this reason (41% for suicidal thoughts and 59% for suicide attempts). In (Table 1) we present the socio-demographic description of the sample at time of care in the index episode of suicidal behaviour, and its comparison with those of the follow-up cohort extracted from it, after eliminating 33 cases in whom no documentary information could be obtained in EHR. Sociodemographic characteristics are similar in both cohorts, although it is worth mentioning the 4% decrease of males in the follow-up cohort. They are more frequently women (61%), unemployed (68%) and stressful life events are found in 64% of cases. Other risk factors were found less frequently: not living with a partner (46%), poor socio-familial support (19%) and history of mistreatment/abuse (12%). Fifty-five percent of the people in our study had not been in contact with mental health services when the index episode of suicidal behaviour occurred.
1. Table 1.
Description of socio-environmental variables in the index episode of suicidal behaviour: total sample and comparison with the follow-up cohort
| INDEX EPISODE OF SUICIDAL BEHAVIOUR Socio-environmental variables | TOTAL SAMPLE | FOLLOW-UP COHORT | |
| N = 143 | N = 110 | ||
| Gender | Male Female | 56 (39%) 87 (61%) | 38 (35%) 72 (65%) |
| Age groups | Under 30 years old 30-65 years old Over 65 years old | 22 (15%) 112 (78%) 9 (7%) | 21 (19%) 82 (75%) 7 (6%) |
| Cohabitation | Without Partner With Partner | 66 (46%) 77 (54%) | 50 (45%) 60 (55%) |
| Employment | NO YES | 98 (68%) 45 (32%) | 75 (68%) 35 (32%) |
| Available socio[1]familial support | NO YES | 27 (19%) 116 (81%) | 19 (17%) 91 (83%) |
| Stressful life events | NO YES | 52 (36%) 91 (64%) | 40 (36%) 70 (64%) |
| History of abuse | NO YES | 126 (88%) 17 (12%) | 97 (88%) 13 (12%) |
| Mean age (range) | 43,57 (16-84) | 43,41 (16-84) | |
The variables relating to illness (medical, psychiatric, and suicidal) in both samples are shown in (Table 2), with no appreciable differences between the two samples, with the exception for two variables: history of previous suicide attempts and concurrent medical illness, which differ by 5%.
2. Table 2.
Description of clinical variables in the index episode of suicidal behaviour: total sample and comparison with the follow-up cohort
| INDEX EPISODE OF SUICIDAL BEHAVIOUR | TOTAL SAMPLE | FOLLOW-UP COHORT | |
| Clinical Variables | N = 143 | N = 110 | |
| Previous Suicide Attempts | NO YES | 79 (55%) 64 (45%) | 55 (50%) 55 (50%) |
| Actual Mental Illness | NO YES | 60 (42%) 83 (58%) | 45 (40%) 65 (60%) |
| Actual Mental Illnes | NO Depression Others | 60 (42%) 18 (13%) 65 (45%) | 45 (40%) 16 (15%) 49 (45%) |
| Personality Disorder | NO YES | 106 (74%) 37 (26%) | 79 (72%) 31 (28%) |
| Substance Abuse | NO YES | 112 (90%) 31 (10%) | 98 (89%) 12 (11%) |
| Associated Medical Conditions | NO YES | 110 (77%) 33 (23%) | 80 (72%) 30 (28%) |
| Contact with Men[1]tal Health Services | NO YES | 60 (42%) 83 (58%) | 45 (45%) 65 (55%) |
| Average number of attempted suicides (range) | 1,75 (1-6) | 1,76 (1-6) | |
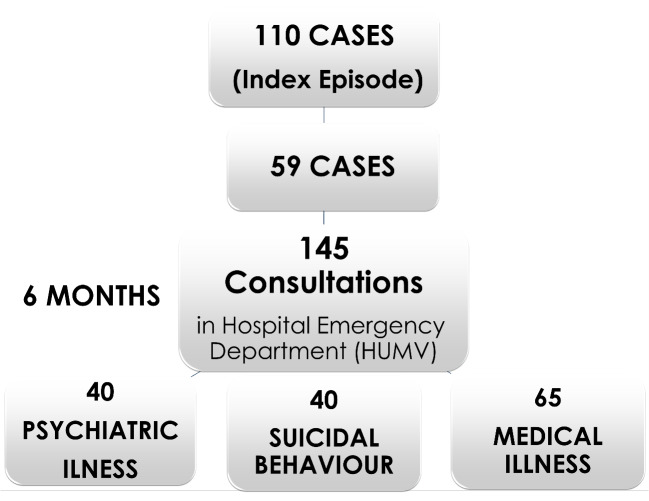
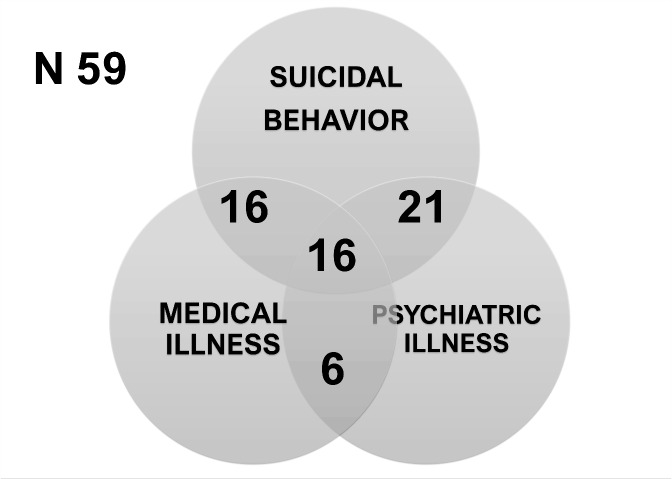
Within 6 months post-index episode follow-up, 60% of those presenting suicidal behaviour (59) made further visits to the emergency department (mean 2.45 visits per person), not only for recurrence of suicidal behaviour but also for other psychiatric and medical reasons (Figure 1). There is a group of high frequenters (27%) who repeatedly consult for all three reasons: suicidal behaviour, other psychiatric problems and medical problems (Figure 2 and Figure 3). Most of this group have history of mental disorders (92%), and far less a history of chronic medical diseases or chronical pain (23%). While not statistically significant, patients with a history of mental illness who consult repeatedly, both for suicidal behaviour and for medical reasons, consulted three times more often than those without prior mental illness (15% vs. 4%).
Figure 1.
Rate of visits to hospital emergency department during the six months of follow-up after index episode
Figure 2.
Rate of visit to hospital emergency department during the six months of follow-up after index episode
Figure 3.
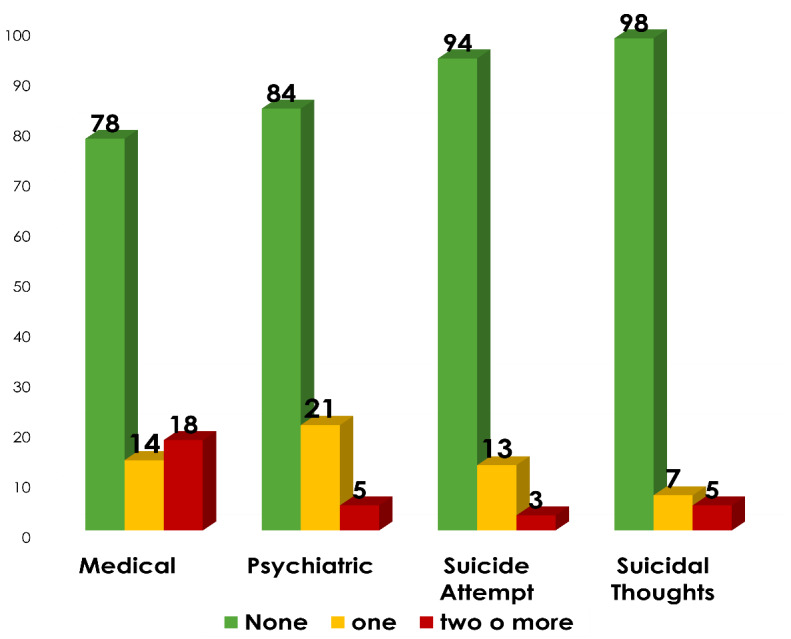
Number and reason for visits to the emergency department during the first six months follow-up after the index event
Twenty-three of the 110 patients monitored (21%) presented a recurrence of suicidal behaviour (10% attempt, 6% ideation and 5% both) and one-quarter of them required a hospital admission (equal percentage to the index episode). A suicide attempt was made in 14% of the cases with suicidal thoughts in the index episode, of which one case (0.7%) was a consummated suicide. There were differences regarding age when we compared the group with recurrent suicidal behaviour (23 cases) with those who did not (87 cases). The middle-age group is the most recurrent group compared to the youngest (under 30 years) and the oldest (over 65 years), resulting into a statistically significant difference (Table 3).
3. Table 3.
Comparison between the sample with and without recurrence of suicidal behaviour during the 6 months following the index episode. Socio-environmental variables
| INDEX EPISODE OF SUICIDAL BEHAVIOUR | SUICIDAL BEHAVIOUR in the next 6 months | TOTAL (N = 110) | ||
| Socio-environmental variables | NO (N=87) | YESY (N=23) | ||
| Gender | Male Female | 31 (81,6%) 56 (77,8%) | 7 (18,4%) 16 (22,2%) | 38 (100%) 72 (100%) |
| Age groups | Under 30 years old 30-65 years old Over 65 years old | 21 (100%) 60 (73,2%) 6 (85,7%) | 0 (0,0%) 22 (26,8%) * 1 (14,3%) | 21 (100%) 82 (100%) 7 (100%) |
| Cohabitation | Without Partner With Partner | 62 (78,5%) 25 (80,6%) | 17 (21,5%) 6 (19,4%) | 79 (100%) 31 (100%) |
| Employment | NO YES | 58 (77,3%) 29 (82,9%) | 17 (22,7%) 6 (17,1%) | 75 (100%) 35 (100%) |
| Available socio[1]familial support | NO YES | 13 (68,4%) 74 (81,3%) | 6 (31,6%) 17 (18,7%) | 19 (100%) 91 (100%) |
| Stressful life events | NO YES | 29 (72,5%) 58 (82,9% | 11 (27,5%) 12 (17,1%) | 40 (100%) 70 (100%) |
| History of abuse | NO YES | 76 (78,4%) 11 (84,6%) | 21 (21,6%) 2 (15,4%) | 97 (100%) 13 (100%) |
(* p=0,024)
While the unemployed and socially unsupported individuals reported a recurrence of suicidal behaviour, the differences were not statistically significant. No differences were found regard to gender, living with a partner, or the existence of a history either of abuse or of stressful life events.
Only the existence of mental illness was found with a statistically significant relationship with the recurrence of suicidal behaviour during the 6-month follow-up period, as summarised in (Table 4), among the factors related to health status.
4. Table 4.
Comparison between the sample with and without recurrence of suicidal behaviour during the 6 months following the index episode. Variables related to health status
| INDEX EPISODE OF SUICIDAL BEHAVIOUR | SUICIDAL BEHAVIOUR in the next 6 months | TOTAL (N = 110) | ||
| Clinical Variables | NO (N=87) | YESY (N=23) | ||
| Previous Suicide Attempts | NO YES | 43 (78,2%) 44 (80,0%) | 12 (21,8%) 11 (20,0%) | 55 (100%) 55 (100%) |
| Actual Mental Illness | NO YES | 43 (78,2%) 44 (80,0%) | 4 (10,5%) 19 (26,4%)* | 38 (100%) 72 (100%) |
| Actual Mental Illnes | NO Depression Others | 34 (89,5%) 12 (75,0%) 36 (73,5%) | 4 (10,5%) 4 (25,0%) 13 (26,5%) | 38 (100%) 16 (100%) 49 (100%) |
| Personality Disorder | NO YES | 63 (79,7%) 24 (77,4%) | 16 (20,3%) 7 (22,6%) | 79 (100%) 31 (100%) |
| Substance Abuse | NO YES | 77 (78,6%) 10 (83,3%) | 21 (21,4%) 2 (16,7%) | 79 (100%) 31 (100%) |
| Associated Medical Conditions | NO YES | 64 (80,0%) 23 (76,7%) | 16 (20,0%) 7 (23,3%) | 80 (100%) 30 (100%) |
| Follow-up in Mental Health Services | NO YES | 36 (80,0%) 51 (78,5% | 9 (20,0%) 14 (21,5%) | 45 (100%) 65 (100%) |
(*<0,05)
DISCUSSION
The higher frequency of women, unemployed people and presence of stressful life events found in this present survey is consistent with the usual findings in most literature(6)-(10)-(11)-(15)-(16). However, other risk factors found in other studies do not appear in ours, such as: not living with a partner, lack of family and social support or history of maltreatment/abuse. These disparities may reflect real differences in our setting, as evidenced in large population-based studies comparing regions and countries(14)-(31) or temporal changes in risk factors over long periods of time within the same populations(32). However, our small sample size requires caution in interpreting these findings. Other possible explanations should be considered, such as differences in methodological design, considering that we included suicidal thoughts within suicidal behaviour, in contrast to most studies that focus only on attempts. Although risk factors for suicidal ideation and suicide have been found to be similar, albeit with different age and gender patterns(16), it is possible that different subgroups of people with suicidal behaviour have different risk factor constellations. Larger studies with comparable methodologies are needed, considering that there are many difficulties in making reliable comparisons between studies, as found in meta-analyses and systematic reviews(11)-(18)-(33)-(35).
We found that 60% of the cases visited the emergency department again during the 6 months following the index episode (2.45 consultations per person on average), not only for recurrence of suicidal behaviour but also for other psychiatric and medical reasons. Twenty-seven percent of the cases are high frequenters who repeatedly consult for all three reasons: suicidal behaviour, other psychiatric problems, and medical problems. We found that 92% of this group had a history of mental illness, and among hyper-frequenters, three times more than those without a history of mental illness consulted. These results are consistent with those found in a wide range of studies showing the importance of psychiatric illness(),(11),(14),(17),(18) and medical pathology(22)–(26),(28),(36), in correlation with the risk of suicidal behaviour. This highlights probably an individual’s perception of discomfort as a whole experience, by combining physical and emotional components, resulting in a variety of unspecific urgent consultations, which, depending on the moment and the circumstances, manifest themselves in one direction or another. The relevance lies in the fact of the health system is not providing an adequate assistance response capable to change the natural course of this behaviour. Cross-cutting and disconnected interventions are provided instead of a sustained longitudinal therapeutic approach that ensures continuity of care. This results in a tendency towards chronicity of the condition and, in the congestion of emergency departments. Although no deaths other than suicide have occurred in this group, probably due to the short duration of follow-up, some studies have found a clear increase in the probability of death in people who make a suicide attempt compared to those who have not engaged in suicidal behaviour (6),(8), reaching three times higher in the following 4 years(10), underlining the need for longer followups with attention to medical comorbidity.
Prolonged follow-up after a suicide attempt revealed the interval between 3-6 is the highest risk period, after which recurrences decrease notably(9). The recurrence found in our study (21% in 6 months) is higher than the 14%-15% found by other researchers in both 12-month (8) and longer follow-ups (3-4 years)(6),(9). This could be explained in our study because we have also considered not only suicidal attempts but also suicidal thoughts as recurrence, although high recurrence rates of suicidal attempts (16-34% in 1-2 years) have also been found in systematic reviews(11).
Since both the rate of death by suicide found in follow- ups of people with previous suicidal behaviour and the length of follow-up vary across studies(9),(10), comparisons are difficult to establish. Nevertheless, we know that on average 45% of people who died by suicide had consulted during the previous month for suicidal thoughts with their general health practitioner and 20% with mental health services(12). Many studies have also found that about 60% of transitions from suicidal thoughts to attempts occurring within the year after onset of suicidal ideation(14), hence the importance of considering suicidal thoughts as a risk factor for suicide in the implementation of preventive programmes. There were considerably more people in our study who were not in contact with mental health services (55%) than the average found by Luoma et al. in their review of 40 studies in the US (33%)(12). This is particularly important to ensure continuity of healthcare after suicidal behaviour, considering that the entry into the system has been the emergency department consultation in more than the half of the cases. On the other hand, in our study we have found no differences in the recurrence of suicidal behaviour depending on the follow- up in mental health services. This finding highlights the need to design specific intervention programmes for people with suicidal behaviour, other than usual treatment, which does not seem to prevent recurrence or the need for hospital admission, which is maintained in a quarter of patients. The presence of mental illness was statistically significantly related to the recurrence of suicidal behaviour during the 6-month follow-up period, in agreement with the usual findings in the literature(10),(11),(14),(17),(18). However, we found no differences regarding type of diagnosis, substance abuse, existence of prior suicide attempts at index episode of suicidal behaviour, or comorbidity with medical illness.
We share the current view of suicide as a complex phenomenon, resulting from the convergence of genetic, psychological, social, and cultural factors in combination with experiences of trauma or loss. Individual and environmental risk factors and their relationships to each other can be explained through different theoretical models, such as stress diathesis(9),(37), in both clinical and neurobiological terms, framed by gene-environment interactions adjusted according to the timing of external events, from early adverse experiences to stressful events at different stages of life(38). These approaches not only facilitate the understanding and prediction of suicidal behaviour, but also allow the design of relevant targets for therapeutic intervention, especially on modifiable individual predisposing factors. Furthermore, these models also guide us in the design of specific programmes for the multidisciplinary management of suicidal behaviour involving the approach to non-modifiable individual factors (age groups, gender, experiences linked to trauma or loss) in an integrated way, to provide a integrated response to the assistance requirements of the person.
CONCLUSIONS
During the 6 months following the index episode of suicidal behaviour, people frequently consulted the emergency department again (60%) for various psychiatric and medical reasons, an average of 2.5 consultations per person, with recurrence of suicidal behaviour being the reason for urgent consultation in more than 20% of cases and with one death by suicide occurring during this period after the index episode. There is a group of high frequenters, which constitutes 27% of those who consult the emergency department again during the follow-up period, who make repeated emergency consultations for all causes, both suicidal behaviour and other psychiatric and medical reasons. These findings alert us about the need to provide a comprehensive approach in strategies for the management of suicidal behaviour.
The usual findings are confirmed regarding gender (higher frequency in women 61%), age (higher frequency in the middle-age of life, 78% between 30-65 years, with an average of 43 years), unemployment (68%) and the existence of stressful life events (64%). However, the absence of a partner (46%) and mental illness (58%) appeared in only half of the cases. In contrast, other risk factors commonly described in the literature were infrequent in our study, such as substance abuse (10%), history of abuse (12%), no support available (19%) or medical illness (23%).
Only age (30-65 years) and presence of psychiatric disorders have shown a statistically significant relationship with the recurrence of suicidal behaviour after the index episode.
The high complexity of the suicide phenomenon requires a systematic review of approach models, both in terms of assessment and therapeutic intervention. Standardised comprehensive assessment (medical, psychiatric, and social) of people consulting hospital emergency departments for suicidal behaviour should be introduced into routine assistance protocols; multidisciplinary interventions must be implemented rapidly to avoid immediate morbidity and mortality; and then close follow-up during the months following the index episode to prevent recurrence of suicidal behaviour and death by suicide.
The main limitations of our study concern the small sample size, as well as the short sample collection period, which may lead to bias, limit the statistical power of the results, and hinder comparative analyses that could provide more clarity on the nature of features in the most-at-risk group. This research was an exploratory descriptive study which has provided the basis for the design of a comprehensive and interdisciplinary intervention programme for preventing suicide risk, the High-Resolution Programme for the Management of Suicidal Behaviour and Suicide Prevention (CARS), which started on the 1st of March 2016 at the Psychiatry Department of the University Hospital Marqués de Valdecilla (Santander, Spain). The CARS Programme was a finalist in the 2017 BIC Awards in the category of Best Care Coordination Programme(39) and the winner of the First Prize in the VI Edition of the Affective-Effective Awards in 2020(40).
Whenever we can increase the sample size and improve the analysis of results with the data collected in this programme, we will be able to advance in the knowledge of the complexity of the suicide phenomenon, its better treatment and the prevention of its related morbidity and mortality.
CONFLICT OF INTEREST
The Authors declare having no conflicts of interest.
References
- 1.World Health Organization WHO. Public health action for the prevention of suicide. Public health action for the prevention of suicide. 2013 [Google Scholar]
- 2.World Health Organization WHO. A global imperative. Preventing suicide. . 2014 [Google Scholar]
- 3.Instituto Nacional de Estadística INE. según la causa de muerte Estadística de defunciones. 2016 [Google Scholar]
- 4.O’Connor O, Et Nock R. C., M. K. M. K.. The Lancet Psychiatry. The psychology of suicidal behaviour. 2014 doi: 10.1016/S2215-0366(14)70222-6. [DOI] [PubMed] [Google Scholar]
- 5.Turecki T, Gustavo G, Brent B. Lancet. Suicide and suicidal behaviour. 2016 doi: 10.1016/S0140-6736(15)00234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooper J. Am. J. Psychiatry. et al. Suicide after deliberate self-harm: A 4-year cohort study. 2005 doi: 10.1176/appi.ajp.162.2.297. [DOI] [PubMed] [Google Scholar]
- 7.Zanl Z, Hawton K. Br. J. Psychiatry. Repetition of deliberate selfharm and subsequent suicide risk:Long-term follow-up study of 11 583 patients. 2004 doi: 10.1192/bjp.185.1.70. [DOI] [PubMed] [Google Scholar]
- 8.Owens D, Horrocks J, House A. Systematic review. A. Fatal and non-fatal repetition of self-harm. 2002 doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 9.Oquendo M. A. Am. J. Psychiatry. et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. 2004 doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- 10.Christiansen E, Jensen B. F.. Aust. New Zeal. J. Psychiatry. a Register-Based Survival Analysis. 2007 doi: 10.1080/00048670601172749. [DOI] [PubMed] [Google Scholar]
- 11.Mendez-Bustos P, De Leon-Martinez V, Miret M, Baca- Garcia E, Lopez-Castroman J. Harv. Rev. Psychiatry. Suicide reattempters: A systematic review. 2013 doi: 10.1097/HRP.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 12.Luoma J. B., Martin M, Pearson J. L. . Am. J. Psychiatry. Suicide : A Review of the Evidence. 2012 doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayuso-Mateos J. L. . Rev. Psiquiatr. Salud Ment. et al. Recommendations for the prevention and management of suicidal behaviour. 2012 doi: 10.1016/j.rpsm.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Nock MK. Br. J. Psychiatry. et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. 2004 doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El Majzoub, I. Ann. Gen. Psychiatry. et al. Characteristics of patients presenting post-suicide attempt to an Academic Medical Center Emergency Department in Lebanon. 2018 doi: 10.1186/s12991-018-0191-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunnell D, Harbord R, Singleton N, Jenkins R, Lewis G. Br. J. Psychiatry. Factors influencing the development and amelioration of suicidal thoughts in the general population: Cohort study. 2004 doi: 10.1192/bjp.185.5.385. [DOI] [PubMed] [Google Scholar]
- 17.Fazel S, Wolf A, Palm C, Lichtenstein P. The Lancet Psychiatry. Violent crime, suicide, and premature mortality in patients with schizophrenia and related disorders: A 38-year total population study in Sweden. 2014 doi: 10.1016/S2215-0366(14)70223-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chesney E, Goodwin G. M., Fazel S. World Psychiatry. Risks of all-cause and suicide mortality in mental disorders: A meta-review. 2014 doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Touriño R. Actas Esp. Psiquiatr. Riesgo suicida, desesperanza y depresión en pacientes con esquizofrenia y autoestigma. 2018 [Google Scholar]
- 20.McMillan D, Gilbody S, Beresford E, N. L.. Psychol Med. Can we predict suicide and non-fatal self- harm with the Beck Hopelessness Scale? A meta-analysis. 2007 doi: 10.1017/S0033291706009664. [DOI] [PubMed] [Google Scholar]
- 21.Toro-Tobar R. A., Grajales-Giraldo F. L., Sarmiento- López J. C.. Aquichan Riesgo suicida según la tríada cognitiva negativa, ideación, desesperanza y depresión. 2016 [Google Scholar]
- 22.Bolton J. M, Walld R, Chateau D, Finlayson G, Sareen J. Psychol. Med. Risk of suicide and suicide attempts associated with physical disorders: a population-based, balancing score-matched analysis. 2015 doi: 10.1017/S0033291714001639. [DOI] [PubMed] [Google Scholar]
- 23.Khazem, L. R., Anestis M. D. . J. Clin. Psychol. Do physical disabilities differentiate between suicidal ideation and attempts? An examination within the lens of the ideation to action framework of suicide. 2019 doi: 10.1002/jclp.22735. [DOI] [PubMed] [Google Scholar]
- 24.Scott K. M.. Psychosom. et al. Chronic physical conditions and their association with first onset of suicidal behavior in the world mental health surveys. 2010 doi: 10.1097/PSY.0b013e3181e3333d. [DOI] [PubMed] [Google Scholar]
- 25.Fässberg M. M.. Psychosom. systematic review of physical illness, functional disability, and suicidal behaviour among older adults. 2016 doi: 10.1080/13607863.2015.1083945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah A, Bhat R, Zarate-Escudero S, Deleo D, Erlangsen A. Aging Ment. Heal. Suicide rates in five-year age-bands after the age of 60 years: The international landscape. 2016 doi: 10.1080/13607863.2015.1055552. [DOI] [PubMed] [Google Scholar]
- 27.Joung K. I., Cho S. BMC Public Health. Association of low blood pressure with suicidal ideation: A cross-sectional study of 10,708 adults with normal or low blood pressure in Korea. 2018 doi: 10.1186/s12889-018-5106-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goodwin R. D.. Am. J. Public Health. Asthma, suicidal ideation, and suicide attempts: Findings from the Baltimore epidemiologic catchment area follow‐up. 2005 doi: 10.2105/AJPH.2003.019109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ministerio de Sanidad MDS. Guía de práctica clínica de prevención y tratamiento de la conducta suicida guía de práctica clínica Ministerio de Sanidad. 2012 [Google Scholar]
- 30.Patterson WM, Dohn HH, Patterson J, P. G.. The SAD PERSONS scale. Evaluation of suicidal patients: 1983 doi: 10.1016/S0033-3182(83)73213-5. [DOI] [PubMed] [Google Scholar]
- 31.Reilly D, Rosato M, Connolly S, Cardwell C. Br. J. Psychiatry. Area factors and suicide: 5-year follow-up of the Northern Ireland population. 2008 doi: 10.1192/bjp.bp.107.040360. [DOI] [PubMed] [Google Scholar]
- 32.Lövestad S. BMC Public Health. et al. Suicidal ideation and attempts in population-based samples of women: Temporal changes between 1989 and 2015. 2019 doi: 10.1186/s12889-019-6685-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tøllefsen I. M ., Hem E, Ekeberg O. BMC Psychiatry. The reliability of suicide statistics: A systematic review. 2012 doi: 10.1186/1471-244X-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zalsman G. The Lancet Psychiatry. et al. Suicide prevention strategies revisited: 10-year systematic review. 2016 doi: 10.1016/S2215-0366(16)30030-X. [DOI] [PubMed] [Google Scholar]
- 35.Cleare S, Gumley A, Connor R. C.. Clin. Psychol. Psychother. Self-compassion, self-forgiveness, suicidal ideation, and self-harm: A systematic review. 2019 doi: 10.1002/cpp.2372. [DOI] [PubMed] [Google Scholar]
- 36.Petrosky E. Ann. Intern. Med. et al. Chronic pain among suicide decedents, 2003 to 2014: Findings from the national violent death reporting system. 2018 doi: 10.7326/M18-0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mann, J. J. . Ann Intern Med. A current perspective of suicide and attempted suicide. 2002 doi: 10.7326/0003-4819-136-4-200202190-00010. [DOI] [PubMed] [Google Scholar]
- 38.Mann J. J.. Nat. Rev. Neurosci. Neurobiology of suicidal behaviour. 2003 doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 39.Premios Best in Class BIC. Premios Best in Class Premios Best in Class. 2017 [Google Scholar]
- 40.FORO PREMIOS AFECTIVO-EFECTIVO FPAE. VI Edicion https://foropremiosafectivoefectivo.com/ediciones/2020/ premiados#menu-editions. 2020 [Google Scholar]