SUMMARY
Introduction
Nasal endoscopy is likely to be the method of choice to evaluate nasal obstruction and adenoid hypertrophy (AH) in children given its excellent diagnostic accuracy and low risk for the patient. The aim of this study was to update the previous classification of AH to guide physicians in choosing the best therapeutic option.
Materials and methods
This is a retrospective observational study including 7621 children (3565 females; mean age 5.92; range: 3-14 years) who were managed for adenoid hypertrophy at our institution between 2003 and 2018. All patients were initially treated with medical therapy and then with surgery if not adequately controlled. We performed a specific analysis based on the presence or absence of comorbidities.
Results
In 1845 (24.21%) patients, adenoid obstruction was classified as Grade I when the fiberoptic endoscopy showed adenoid tissue occupying < 25% of choanal space. In 2829 of 7621 (37.12%) patients, the adenoid tissue was scored as Grade II since it was confined to the upper half of nasopharynx, with sufficiently pervious choana and visualisation of tube ostium. In 1611 of 7621 (21.14%) cases, adenoid vegetation occupied about 75% of the nasopharynx with partial involvement of tube ostium and considerable obstruction of choanal openings, and was classified as Grade III. Finally, 1336 of 7621 (17.53%) patients were scored as Grade IV due to complete obstruction with adenoid tissue reaching the lower choanal border without allowing the visualisation of the tube ostium. Based on resolution of symptoms in Grade III obstruction after medical therapy (that was mostly seen in patients without comorbidities), we divided patients in two subclasses: Grade IIIA was not associated with comorbidities, while Grade IIIB was correlated with important comorbidities.
Conclusions
These results can be useful to guide medical or surgical therapeutic intervention. In patients with class IIIB AH, surgical treatment offered adequate control not only of nasal symptoms but also of associated comorbidities.
KEY WORDS: adenoid hypertrophy, classification, nasal endoscopy
RIASSUNTO
Introduzione
L’endoscopia nasale è probabilmente il metodo di scelta per valutare l’ostruzione nasale e l’ipertrofia adenoidea (IA) nei bambini, poiché ha un’eccellente accuratezza diagnostica e un basso rischio per il paziente. Lo scopo di questo studio è di aggiornare la precedente classificazione di IA per guidare i medici a scegliere la migliore opzione terapeutica.
Materiali e metodi
Questo è uno studio osservazionale retrospettivo che include 7621 bambini (3565 femmine; età media 5,92; range: 3-14 anni) che sono stati seguiti per l’ipertrofia adenoidea presso il nostro istituto tra il 2003 e il 2018. Tutti i pazienti sono stati inizialmente trattati con terapia medica e successivamente con terapia chirurgica, se non adeguatamente controllati. Un’analisi specifica è stata condotta sulla base delle comorbidità.
Risultati
In 1845 pazienti (24,21%) l’immagine dell’endoscopia a fibre ottiche evidenziava uno scarso tessuto adenoideo occupante < 25% delle aperture coanale: ostruzione adenoidea di Grado I. In 2829/7621 (37,12%) il tessuto adenoideo era confinato alla metà superiore del rinofaringe, con coana sufficientemente pervia e visualizzazione dell’ostio tubarico: Grado II. In 1611/7621 (21,14%), la vegetazione adenoidea occupava circa il 75% del rinofaringe, con parziale coinvolgimento dell’ostio tubarico e notevole ostruzione delle aperture coanali: Grado III. In 1336/7621 (17,53%) l’ostruzione era quasi completa e il tessuto adenoideo raggiungeva il bordo inferiore della coana senza consentire la visualizzazione dell’ostio tubarico: Grado IV. Sulla base della risoluzione dei sintomi nell’ostruzione di Grado III dopo terapia medica (che è stata evidenziata principalmente nei pazienti senza comorbidità), abbiamo diviso i pazienti in due sottoclassi: il Grado IIIA non era associato a comorbidità, mentre il Grado IIIB era correlato a comorbidità importanti.
Conclusioni
I nostri risultati possono essere utili per indicare un intervento terapeutico medico o chirurgico. Essi dimostrano che nei pazienti di Grado IIIB, il trattamento chirurgico offre un buon controllo non solo dei sintomi nasali, ma anche delle principali comorbidità.
PAROLE CHIAVE: ipertrofia adenoidea, classificazione, endoscopia nasale
Introduction
Early detection of nasal obstruction and adenoid hypertrophy (AH) is fundamental to avoid important complications (recurrent otitis, sleep apnoea syndrome and lower airway diseases) and to prevent alterations of craniofacial development in growing children. A wide range of alternative diagnostic methods have been proposed for diagnosis with variable sensitivity and specificity over the last few years 1. These are both clinical exams, such as structured examinations with nasal obstruction index (NOI) 2,3, and imaging techniques (i.e. videofluoroscopy, multirow detector computed tomography-CT 1,4, and lateral cephalogram 5). Nasal endoscopy is likely to be the method of choice to evaluate the nasopharynx in children given its excellent diagnostic accuracy and low risk for the patient 6,7. Flexible fiberoptic endoscopy examination is a safe, accurate and well tolerated procedure that does not require anaesthesia and allows direct visualisation of the nasal cavities and nasopharynx with high sensitivity and specificity 8, as confirmed by authors who demonstrated a high correlation between fiberoptic endoscopy examination and intraoperative nasopharyngoscopy performed during adenoidectomy 9. Only a few authors underlined some disadvantages such as the lack of objective measurements that often cause low inter-observer agreement 10.
Currently there are several methods to grade AH in the literature 11,12. The method that we previously proposed 6 is used by most clinicians worldwide because it is easily accessible and applicable by any observer 13,14 and can be very useful to guide physicians in choosing the best therapeutic option.
The aim of this study was to analyse the impact on clinical management of the endoscopic grading system for adenoid hypertrophy that we proposed in 2003. For this reason, we retrospectively reviewed all cases of children affected by AH and classified by our endoscopic grading system at our institution, analysing outcomes of medical and surgical treatment. Furthermore, we performed specific analyses based on the presence or absence of comorbidities.
Materials and methods
Study population and study design
This is a retrospective observational study including 7621 children (3565 females; mean age 5.92; range: 3-14 years) who were managed for AH at the Department of Otolaryngology at the University Hospital of Foggia between 2003 and 2018. We enrolled patients younger than 14 years with a confirmed diagnosis of adenoid hypertrophy with or without comorbidities, and out of therapy since at least 6 months. Exclusion criteria were previous surgery, nasal obstruction due to anatomic malformations (i.e. choanal atresia or diaphragm, septal deviations etc.) and chronic rhinosinusitis with nasal polyps. Finally, we excluded patients who did not complete at least 18 months of follow-up.
Diagnostic protocol at our institution in clinical practice for patients with AH
In our clinical practice, fiberoptic endoscopy exam is generally performed if AH is suspected. Endoscopy is routinely performed in children with a paediatric 2.7 mm fibre-endoscope (11101 – SK1 - Karl Storz® – Germany). The aim of this examination is to confirm the chronic presence of purulent secretion and to establish the grade of AH. We classified obstruction into four degrees according to the endoscopic classification system that we proposed in 2003. During the investigation, fiberoptic endoscopy images of the choanal openings are divided into four segments from the upper choanal border to the nasal floor. GRADE I is scored when fiberoptic endoscopy imaging revealed adenoid tissue occupying only the upper segment of the nasopharyngeal cavity (≤ 25%) with almost completely free choanal openings. GRADE II is scored if the adenoid tissue is confined to the upper half (≤ 50%) of the nasopharyngeal cavity with sufficiently pervious choana and perfect visualisation of the tube ostium. GRADE III obstruction is given if adenoid tissue occupies about 75% of the nasopharynx with partial involvement of the tube ostium and considerable obstruction of choanal openings. In GRADE IV cases, the adenoid tissue reaches the lower choanal border without allowing visualisation of the tube ostium (> 75%).
Moreover, children with AH usually undergo otoscopic and audiological evaluation. Patients with allergic symptoms undergo a Prick test and/or radioallergosorbent test (RAST). Since 2006, in our institution, patients reporting sleep disorders (i.e. snoring, sleep apnoea etc.) are generally examined with full-night polysomnography in order to exclude OSAS. We classify patients according to their Apnoea-Hypopnoea Index (AHI) as mild (AHI: 1-4), moderate (AHI: 5-10) and severe (AHI: > 10).
Management of AH in our routine practice
If AH is confirmed, we routinely propose a first approach with medical treatment and a re-evaluation after 3 months. Outcomes of medical treatment are considered as resolved (complete resolution of symptoms), improved (incomplete resolution of symptoms), unchanged (any modification on symptoms), or worsened (worsening of symptoms). Surgery is taken into consideration in case of failure after 3 months of medical treatment, and especially in the presence of comorbidities.
Clinical data collection and outcomes
The data were directly extracted from our clinical system and from medical records of outpatients. We specifically assessed clinical data, and in particular we analysed outcomes of medical treatment and surgery. We finally analysed data according to the presence/absence of associated pathologies that may have a physiopathological link with AH such as recurrent acute otitis media (AOM), otitis media with effusion (OME), recurrent upper respiratory tract infections (URTI - i.e. tonsillitis, sinusitis), lower airway diseases (i.e. tracheitis, bronchitis, pneumonitis) and sleep disorders.
Results
Results of diagnostic work up and analysis of comorbidities
Fiberoptic endoscopy showed in 1845 patients (24.21%) aged 3-14 years a Grade I score of rhino-pharynx obstruction. In 2829 patients (37.12%) aged 2-14 years, the adenoid tissue appeared to be confined to the upper half of the nasopharyngeal cavity and was scored as Grade II. In 1611 patients (21.14%) aged 2-13 years, a Grade III obstruction was diagnosed. Finally, in 1336 patients (17.53%) aged 1-7 years, the obstruction was almost complete and was classified as Grade IV.
Parents referred a frequent presence of mucous and/or purulent nasal secretion in 2675 (35.1%) cases. Allergic rhinitis (AR) was diagnosed by Prick-test and/or RAST in 692 (9.1%) children (range: 5-14 years). A turbinate hypertrophy was seen together with the AH in all patients affected by allergies. A history of AOM was observed in 296 (3.9%) patients, while OME was diagnosed in 671 (8.8%). An history of recurrent tonsillitis was reported in 302 (3.9%) patients. Recurrent episodes of lower airway disease (i.e. tracheitis, bronchitis, pneumonitis) were observed in 216 subjects (2.8%). A history of sleep disorders was observed in 2762 (36.2%) cases. Full-night polysomnography was performed in 1721 (22.6%) patients and revealed obstructive sleep apnoea (OSA) in 562 (7.4%) cases which was distributed as follows: mild in 72 (0.9%) children, moderate in 247 (3.2%) and severe in 243 (3.2%).
We summarised the associated pathologies according to the four different classes of AH in Table I.
Table I.
Comorbidities according to the 4 different grades of AH.
| Grade | Recurrent nasal secretions | Recurrent tonsilitis | OME | Recurrent AOM | Referred sleep disturbance | Recurrent lower airway diseases | Allergic rhinitis | OSAS |
|---|---|---|---|---|---|---|---|---|
| Grade I (1845 pts – 24.21%) | 72 (3.9%) | 41 (2.2%) | 43 (2.3%) | 21 (1.1%) | 85 (4.6%) | 11 (0.6%) | 30 (1.6%) | 13 (0.7%) |
| Grade II (2829 pts – 37.12%) | 218 (7.7%) | 54 (1.9%) | 75 (2.6%) | 51 (1.8%) | 275 (9.7%) | 20 (0.7%) | 94 (3.3%) | 32 (1.1%) |
| Grade III (1611 pts – 21.14%) | 962 (59.7%) | 89 (5.5%) | 208 (12.9%) | 84 (5.2%) | 983 (61%) | 75 (4.6%) | 207 (12.8%) | 199 (12.3%) |
| Grade IV (1336 pts – 17.53%) | 1336 (100%) | 107 (8%) | 324 (24.2%) | 127 (9.5%) | 1332 (99.7%) | 101 (7.5%) | 340 (25.4%) | 300 (22.4%) |
| Total (7621) | 2588 (33.9%) | 291 (3.8%) | 650 (8.5%) | 283 (3.7%) | 2675 (35.1%) | 207 (2.7%) | 671 (8.8%) | 544 (7.1%) |
OME: otitis media with effusion; AOM: acute otitis media; OSAS: Obstructive Sleep Apnea.
Medical treatment outcomes
All patients were initially treated with medical therapy. The treatment consisted of nasal irrigations with isotonic saline solution twice a day for three months and corticosteroid nasal spray (mometasone furoate: 2 sprays in each nostril once daily for 30 days). Moreover, an antihistamine medication (levocetirizine: 0.5 drop/kg body weight) was used for a minimum of one month. After 3 months of follow-up, an adequate control of the pathology (reduction of nasal secretions and reduction or maintaining of the same AH degree, resolution of ear and/or lower airways disease) was reached in 5690 (74.6%) patients. Analysing the results for each group based on grade of AH we observed the following: 100% of Grade I patients reached adequate control (1845/1845); 99.8% of Grade II patients (2823/2829), 54.7% of Grade III patients (881/1611) and 0.9% of Grade IV patients (12/1336). None of the patients affected by Grade I of AH requested surgery after medical treatment. In 5 children suffering from Grade II AH, an increase to Grade III occurred, and in these cases surgery (adenotonsillectomy) was necessary due to the presence of severe OSA. In 881 patients (54.7%) belonging to the Grade III group, medical treatment was effective in controlling nasal obstruction and related pathologies and complications. Table II shows the results of medical therapy on symptoms and associated pathologies that may have physiopathological link with AH. Resolution of symptoms in Grade III obstruction was mostly seen in patients without associated pathologies (Fig. 1).
Table II.
Results of medical therapy in Grade III obstruction.
| Nasal obstruction | Nasal secretions | Lower airway disease | Otitis | Referred sleep disturbance | |
|---|---|---|---|---|---|
| Patients (1611) | 1611 | 962 | 2 | 114 | 982 |
| Unchanged | 654 (40.6%) | 693 (72%) | 2 (100%) | 59 (51.8%) | 599 (61%) |
| Resolved | 161 (10%) | 217 (22,6%) | / | 12 (10.5%) | 101 (10.3%) |
| Improved | 720 (44.7%) | 52 (5,4%) | / | 29 (25.4%) | 174 (17.7%) |
| Worsened | 76 (4.7%) | / | / | 14 (12.7%) | 108 (11%) |
Figure 1.
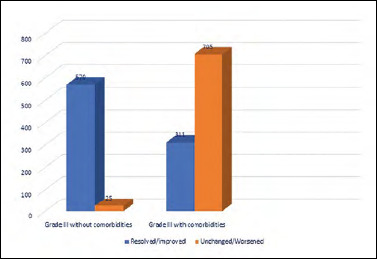
Results of medical therapy on symptoms and comorbidities in Grade III patients.
Outcomes of surgical treatment
In 730/1611 patients (45.3%) with Grade III obstruction, surgical intervention was considered necessary. Thirty-nine patients refused the operation and, therefore, surgery was performed in 691 children. Out of this group, 374 underwent adenoidectomy alone, 259 adenoidectomy and tonsillectomy, 30 adenoidectomy and tympanocentesis, 22 adenoidectomy and ear tube insertion, and 6 adenotonsillectomy and ear tube insertion.
According to this indication and to the large number of associated pathologies that were not resolved with medical therapy, we divided Grade III obstruction in two subclasses, A and B. In Grade IIIA, the volume of adenoid was not correlated with other ENT pathologies and surgical treatment was not necessary, while in Grade IIIB the volume of the adenoid was correlated with associated pathologies that have a very likely physiopathological link with IA and the otolaryngologist deemed surgical treatment necessary (Fig. 2).
Figure 2.
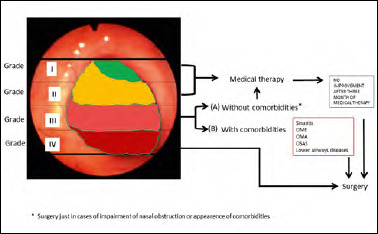
Flow-chart of diagnostic and therapeutic management of AH.
Results after 12 months of postoperative follow-up are reported in Table III along with data concerning nasal obstruction, nasal secretions and associated complications, such as lower airway diseases, otitis and referred sleep disorders.
Table III.
Results of surgical therapy in Grade III of adenoid hypertrophy (AH).
| Nasal obstruction | Nasal secretions | Lower airway disease | Otitis | Referred sleep disturbance | |
|---|---|---|---|---|---|
| Patients (691) | 691 | 668 | 2 | 73 | 610 |
| Unchanged | / | 2 (0.3%) | / | / | 7 (1.1%) |
| Improved | 178 (25.8%) | 92 (13.8%) | / | 22 (30.6%) | 180 (29.6%) |
| Resolved | 513 (74.2%) | 574 (85.9%) | 2 (100%) | 51 (69.4%) | 423 (69.3%) |
| Worsened | / | / | / | / | / |
Surgery was indicated in 1324/1336 (99.1%) patients of the Grade IV group who did not improve after medical therapy; of these, 10 patients refused the operation. Surgery was, therefore, performed in 1314 children (738 adenoidectomy alone, 520 adenotonsillectomy, 13 adenotonsillectomy and ear tube insertion, 27 adenoidectomy and ear tube insertion, 3 adenotonsillectomy and tympanocentesis, 13 adenotonsillectomy and ear tube insertion).
Results after 12 months of postoperative follow-up are reported in Figure 3.
Figure 3.
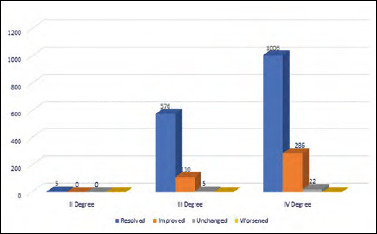
Results of surgery on comorbidities.
Discussion
Diagnosis of nasal obstruction in children is often challenging because of the limited cooperation of paediatric patients and the frequent overestimation of symptoms by their parents. In clinical practice there are numerous ways to determine adenoid size including mirror posterior rhinoscopy, endoscopic examination, lateral X-ray, magnetic resonance imaging (MRI), rhinomanometry and acoustic rhinometry.
Childrens’ cooperation limits the use of mirror examination and can create some difficulties in the execution of rhinomanometry and acoustic rhinometry 15. Lateral radiologic evaluation of the nasopharynx has been used for many years to evaluate adenoid size 16. Lateral cephalograms have good sensitivity (61-75%), but also more variable specificity (41-95%) due to the wide range of inter-observer variability. This exam has the advantage of being non-invasive and quickly accessible in a clinical setting. The limits of this technique are the risk of paediatric exposure to radiation 17 and the indirect correlation between the level of obstruction seen by X-ray and nasal symptoms 6. Additionally, the films are static and give a two-dimensional representation of a three-dimensional space and do not take into account that respiration, swallowing and mouth breathing which may cause soft palate elevation during the examination and, therefore, a reduction of nasopharyngeal cavity size 15,18.
Nasal endoscopy is definitely a more dynamic, safe, quick and well tolerated examination that also demonstrated good correlation between nasal obstructive symptoms and tympanogram type 19. Therefore, in children presenting with nasal obstruction, nasal endoscopy is the best initial choice not only to evaluate adenoid size but also to exclude other rarer causes of chronic nasal obstruction (i.e., turbinate hypertrophy due to AR, rhinosinusitis, nasal polyposis, septal deviations, nasal tumours, choanal atresia etc.) 20. Several methods for assessment of adenoid size by nasal endoscopy have been introduced and are widely used.
Thanks to the development of software and hardware in image processing, objective methods have been proposed such as the “adenoid/choanal (A/C) area ratio” for a two-dimensional objective measure of AH 21. In many cases both subjective and objective methods failed to perform intra- or inter-examiners reproducibility tests and reliability analysis. However, a comparison between various methods revealed that subjective methods have higher rates of inter-examiner agreement compared to objective criteria. For all these reasons, subjective measurement is strongly recommended above all in a clinical setting, where ease of communication among professionals and prompt diagnosis are demanded 22. One of the most valid subjective classification systems of AH is the Parikh method, which evaluates the relationship between the adenoids and surrounding structures. According to this classification, patients meet the criteria for Grade I when the adenoids are not in contact with adjacent structures; Grade II when adenoids are in contact with torus tubarius; Grade III if adenoids are in contact with the vomer and Grade IV when adenoids reach the soft palate 11. Wang also graded adenoids from 1 to 3 based on the distance between the vomer and adenoid tissue during nasal endoscopy, observing a good correlation between adenoid size and upper respiratory symptoms, such as nasal obstruction, snoring and tympanometric alterations 23.
In our previous study 6, we classified obstructions due to AH into four groups in relation to the entity of hypertrophy and to structure involvement. This classification, widely used in clinical practice 13,14,24, can be very useful for therapeutic guidance. Our grading demonstrated a better correlation with symptoms compared to the Parikh classification, especially with regards to AOM and the results of tympanometry 19. This discrepancy can be explained by the involvement of the Eustachian tube; in Grade II of the Parikh classification, involvement is given by the contact with torus tubarius, while in our classification there is direct involvement of the Eustachian tube ostium only in Grade III.
Our case histories indicated that the increase of disorders due to the obstruction of the nasopharyngeal cavity (i.e. mucous-purulent rhinitis, sinusitis, otitis) was directly proportional to the grade of obstruction and affected all children with the most severe forms of obstruction. In fact, patients who presented with ear diseases (i.e. AOM and OME) were predominantly classified as Grade III and IV, demonstrating the involvement of Eustachian tube. Moreover, our results showed that OSA mostly occurred in cases with total or subtotal obstruction; however, the presence of this condition even in lower grades of our classification confirmed the important role of tonsil hypertrophy as a pathogenetic factor.
Allergy also seems to be related to the degree of the obstruction. In fact, allergy occurred in subjects with a higher degree obstruction (Tab. I). These findings seem to agree with Huang’s report, which suggested that allergy was a risk factor for the development of AH 25.
Due to the large percentage of associated pathologies likely linked to AH in Grade III obstructions that are not resolved by medical therapy (Fig. 1), we decided to modify our previous classification and to divide class III in two subclasses, both associated with an occupation of 51-75% of the nasopharyngeal space. Patients in subclass IIIA did not have associated ENT pathologies, while patients in subclass IIIB presented with the same degree of obstruction but with associated pathologies very likely linked to AH (Fig. 2).
The aforementioned findings can be useful to indicate medical or surgical therapeutic intervention. As stated in our previous study 6, in Grade I and II obstructions there is no reason to indicate surgery, since the choanal openings are pervious and, therefore, the airflow is normal. When nasal obstruction also occurs in subjects belonging to the first and second categories, other nasal and nasopharyngeal pathologies (i.e. malformations, allergy, inflammation, or neoplasm) should be suspected and ascertained.
According to our experience, in Grade IIIA three months of therapy with intranasal corticosteroids should be recommended before considering surgery; in fact, according to literature data, with intranasal corticosteroids we obtained good results in improving clinical symptoms and reducing the necessity of surgical treatment 26,27. On the other hand, we observed that patients with Grade III and concomitant comorbidities were not adequately controlled by a medical approach and in this case surgery was very often recommended to achieve control of the disease and comorbidities. For this reason, we propose to update our previous classification by adding the new subclass requesting a surgical indication (IIIB) to guide the therapeutic decision. In fact, in patients with Grade IIIB, surgery resolved not only nasal obstruction but also the associated pathologies pathophysiologically linked to AH in most cases as seen in Table III. This sub-classification may be useful to identify a more aggressive phenotype of patients belonging to Grade III in which surgery may be more likely indicated to resolve associated pathologies that may have a physiopathological link to AH.
According to the results of our study, a clinical approach should be adopted in cases of Grade III obstruction without comorbidities. Therefore, a patient should be sent to surgical therapy only after there is no resolution of associated comorbidities or no improvement of obstructive symptoms after 3 months of medical therapy. Conversely, adenoidectomy should be performed without delay in patients affected by Grade III associated with comorbidities and in Grade IV (Fig. 2). In fact, in such cases nasopharyngeal obstruction can lead to complications when associated with comorbidities and poor results are reached with medical therapy (Fig. 1). Finally, subjects with persistent symptoms after adenoidectomy should be further studied through allergic assessment in case of residual nasal obstruction and/or Eustachian tube function tests if episodes of recurrent otitis persist with the aim of indicating other treatments.
Another topic to be considered is the possible coexistence of AR in children with AH. Therefore, it is mandatory to inspect the nasopharynx of an allergic patient with obstruction, but on the other side it is important to diagnose the presence of AR in children with nasal symptoms and AH to define adequate targeted therapy and avoid unnecessary adenoidectomies 28. For these reasons, we propose to insert patients with Grade III AH and AR in subclass IIIA because in many cases targeted medical therapy may improve the patient’s symptoms; in such cases, surgical therapy is unnecessary. This issue could explain the percentage of patients (25.8%) who obtained only partial improvement of nasal obstruction after adenoidectomy (Tab. III). In fact, Prick-test and/or RAST were performed only in 20.9% patients with symptoms and signs of AR. A larger percentage of allergic patients were probably present in our sample, and undiagnosed cases of AR could have not benefit from surgery.
Interestingly, our results showed that patients with almost similar degrees of AH can have different outcomes after adenoidectomy, even in cases of otologic diseases. In fact, ear pathologies showed the highest percentage of incomplete resolution (30.6%). These findings can be explained by considering the Eustachian tube function that in many children may be ineffective because of the immaturity of its physiologic opening or, especially in allergic patients, because of chronic oedema involving tubal walls 29. Therefore, in these patients the pathogenesis of otologic diseases is related not only to AH. Nontheless, the large percentages of cases that resolved (69.4%) justified our therapeutic choice in these patients.
Good results were obtained in OSA patients mainly because tonsillectomy was associated to adenoidectomy in these cases. Our data agreed with studies in the literature considering nasal obstruction as a secondary causal factor of OSA, in comparison with pharyngeal obstruction due to tonsil hypertrophy 25-30.
Conclusions
The present study, based on a large sample, showed the opportunity to update our previous grading. This new endoscopic classification of nasopharyngeal obstruction obtained by fibre endoscopy allowed for more accurate selection of surgical candidates; Grade III AH represented 21.14% of our study group and this category has to be carefully studied to avoid inappropriate surgical decisions. The updated subdivision in Grade IIIA and IIIB allowed to identify cases that could definitely improve nasal obstruction and associated pathologies with proper medical therapy (IIIA) and cases that probably would not benefit from medical therapy and likely require adenoidectomy to resolve symptoms (IIIB). Surgical treatment in patients belonging to IIIB and IV classes was effective not only in resolving nasal obstruction, but also in most cases of associated comorbidities such as otitis and OSAS.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions
MC and PC conceived of the presented idea; RG and VF developed the theory and performed the computations; DM and EDC verified the analytical methods; MC and MG encouraged to investigate and supervised the findings of this work; all authors discussed the results and contributed to the final manuscript.
Ethical consideration
This study was approved by the Institutional Review Board (IRB) (5/2019) of Unit Of Otolaryngology, University of Foggia.
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Informed consent for consultation of clinical data was obtained from parents at the time of original data collection. The data were anonymously collected and analysed.
Figures and tables
References
- 1.Major MP, Saltaji H, El-Hakim H, et al. The accuracy of diagnostic tests for adenoid hypertrophy: a systematic review. J Am Dent Assoc 2014;145:247-254. https://doi.org/10.14219/jada.2013.31 10.14219/jada.2013.31 [DOI] [PubMed] [Google Scholar]
- 2.Chandra RK, Patadia MO, Raviv J. Diagnosis of nasal airway obstruction. Otolaryngol Clin North Am 2009;42:207-225. https://doi.org/10.1016/j.otc.2009.01.004 10.1016/j.otc.2009.01.004 [DOI] [PubMed] [Google Scholar]
- 3.Marchisio P, Torretta S, Capaccio P, et al. Clinical assessment of adenoidal obstruction based on the nasal obstruction index is no longer useful in children. Otolaryngol Head Neck Surg 2010;142:237-241. https://doi.org/10.1016/j.otohns.2009.10.027 10.1016/j.otohns.2009.10.027 [DOI] [PubMed] [Google Scholar]
- 4.Ysunza A, Pamplona MC, Quiroz J, et al. Maxillary growth in patients with complete cleft lip and palate, operated on around 4-6 months of age. Int J Pediatr Otorhinolaryngol 2010;74:482-485. https://doi.org/10.1016/j.ijporl.2010.01.024 10.1016/j.ijporl.2010.01.024 [DOI] [PubMed] [Google Scholar]
- 5.Ysunza A, Pamplona MC, Ortega JM, et al. Video fluoroscopy for evaluating adenoid hypertrophy in children. Int J Pediatr Otorhinolaryngol 2008;72:1159-1165. https://doi.org/10.1016/j.ijporl.2008.03.022 10.1016/j.ijporl.2008.03.022 [DOI] [PubMed] [Google Scholar]
- 6.Cassano P, Gelardi M, Cassano M, et al. Adenoid tissue rhinopharyngeal obstruction grading based on fiberendoscopic findings: a novel approach to therapeutic management. Int J Pediatr Otorhinolaryngol 2003;67:1303-1309. https://doi.org/10.1016/j.ijporl.2003.07.018 10.1016/j.ijporl.2003.07.018 [DOI] [PubMed] [Google Scholar]
- 7.Eweiss A, Al Yaghchi C, Sharma S, et al. Assessment of posterior choanal obstruction caused by adenoidal hypertrophy: intra-operative mirror versus rigid nasendoscopic examination. Int J Pediatr Otorhinolaryngol 2018;110:144-146. https://doi.org/10.1016/j.ijporl.2018.04.022 10.1016/j.ijporl.2018.04.022 [DOI] [PubMed] [Google Scholar]
- 8.Pagella F, Pusateri A, Chu F, et al. Adenoid assessment in paediatric patients: the role of flexible nasal endoscopy. Int J Immunopathol Pharmacol 2011;24(4 Suppl):49-54. https://doi.org/10.1177/03946320110240S410 10.1177/03946320110240S410 [DOI] [PubMed] [Google Scholar]
- 9.Lertsburapa K, Schroeder JW, Sullivan C. Assessment of adenoid size: a comparison of lateral radiographic measurements, radiologist assessment, and nasal endoscopy. Int J Pediatr Otorhinolaryngol 2010;74:1281-1285. https://doi.org/10.1016/j.ijporl.2010.08.005 10.1016/j.ijporl.2010.08.005 [DOI] [PubMed] [Google Scholar]
- 10.Major MP, Flores-Mir C, Major PW. Assessment of lateral cephalometric diagnosis of adenoid hypertrophy and posterior upper airway obstruction: a systematic review. Am J Orthod Dentofacial Orthop 2006;130:700-708. https://doi.org/10.1016/j.ajodo.2005.05.050 10.1016/j.ajodo.2005.05.050 [DOI] [PubMed] [Google Scholar]
- 11.Parikh SR, Coronel M, Lee JJ, et al. Validation of a new grading system for endoscopic examination of adenoid hypertrophy. Otolaryngol Head Neck Surg 2006;135:684-687. https://doi.org/10.1016/j.otohns.2006.05.003 10.1016/j.otohns.2006.05.003 [DOI] [PubMed] [Google Scholar]
- 12.Josephson GD, Duckworth L, Hossain J. Proposed definitive grading system tool for the assessment of adenoid hyperplasia. Laryngoscope 2011;121:187-193. https://doi.org/10.1002/lary.21215 10.1002/lary.21215 [DOI] [PubMed] [Google Scholar]
- 13.Torretta S, Marchisio P, Esposito S, et al. Diagnostic accuracy of the nasal obstruction index in detecting adenoid hypertrophy in children without allergy. Int J Pediatr Otorhinolaryngol 2011;75:57-61. https://doi.org/10.1016/j.ijporl.2010.10.007 10.1016/j.ijporl.2010.10.007 [DOI] [PubMed] [Google Scholar]
- 14.Ramos VM, Nader CM, Meira ZM, et al. Impact of adenotonsilectomy on nasal airflow and pulmonary blood pressure in mouth breathing children. Int J Pediatr Otorhinolaryngol 2019;125:82-86. https://doi.org/10.1016/j.ijporl.2019.06.025 10.1016/j.ijporl.2019.06.025 [DOI] [PubMed] [Google Scholar]
- 15.Baldassari CM, Choi S. Assessing adenoid hypertrophy in children: X-ray or nasal endoscopy? Laryngoscope 2014;124:1509-1510. https://doi.org/10.1002/lary.24366 10.1002/lary.24366 [DOI] [PubMed] [Google Scholar]
- 16.Paradise JL. Otitis media and child development: should we worry? Pediatr Infect Dis J 1998;17:1076-1083; discussion 1099-100. https://doi.org/10.1097/00006454-199811000-00038 10.1097/00006454-199811000-00038 [DOI] [PubMed] [Google Scholar]
- 17.Cho JH, Lee DH, Lee NS, et al. Size assessment of adenoid and nasopharyngeal airway by acoustic rhinometry in children. J Laryngol Otol 1999;113:899-905. https://doi.org/10.1017/s0022215100145530 10.1017/s0022215100145530 [DOI] [PubMed] [Google Scholar]
- 18.Caylakli F, Hizal E, Yilmaz I, et al. Correlation between adenoid-nasopharynx ratio and endoscopic examination of adenoid hypertrophy: a blind, prospective clinical study. Int J Pediatr Otorhinolaryngol 2009;73:1532-1535. https://doi.org/10.1016/j.ijporl.2009.07.018 10.1016/j.ijporl.2009.07.018 [DOI] [PubMed] [Google Scholar]
- 19.Saedi B, Sadeghi M, Mojtahed M, et al. Diagnostic efficacy of different methods in the assessment of adenoid hypertrophy. Am J Otolaryngol 2011;32:147-151. https://doi.org/10.1016/j.amjoto.2009.11.003 10.1016/j.amjoto.2009.11.003 [DOI] [PubMed] [Google Scholar]
- 20.Pagella F, Pusateri A, Canzi P, et al. The evolution of the adenoidectomy: analysis of different power-assisted techniques. Int J Immunopathol Pharmacol 2011;24:55-59. https://doi.org/10.1177/03946320110240S411 10.1177/03946320110240S411 [DOI] [PubMed] [Google Scholar]
- 21.Chien C-Y, Chen A-M, Hwang C-F, et al. The clinical significance of adenoid-choanae area ratio in children with adenoid hypertrophy. Int J Pediatr Otorhinolaryngol 2005;69:235-239. https://doi.org/10.1016/j.ijporl.2004.09.007 10.1016/j.ijporl.2004.09.007 [DOI] [PubMed] [Google Scholar]
- 22.Feres MFN, Hermann JS, Sallum AC, et al. Radiographic adenoid evaluation: proposal of an objective parameter. Radiol Bras 2014;47:79-83. https://doi.org/10.1590/S0100-39842014000200008 10.1590/S0100-39842014000200008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang DY, Bernheim N, Kaufman L, et al. Assessment of adenoid size in children by fibreoptic examination. Clin Otolaryngol Allied Sci 1997;22:172-177. https://doi.org/10.1046/j.1365-2273.1997.00002.x 10.1046/j.1365-2273.1997.00002.x [DOI] [PubMed] [Google Scholar]
- 24.Moffa A, Carbone S, Costantino A, et al. Potential role of topical ectoine for prevention of pediatric upper respiratory tract infection: a preliminary observational study. J Biol Regul Homeost Agents 2019;33:1935-1940. https://doi.org/10.23812/19-387-L 10.23812/19-387-L [DOI] [PubMed] [Google Scholar]
- 25.De Corso E, Galli J, Di Cesare T, et al. A systematic review of the clinical evidence and biomarkers linking allergy to adeno-tonsillar disease. Int J Pediatr Otorhinolaryngol 2021;147:110799. https://doi:10.1016/j.ijporl.2021.110799. 10.1016/j.ijporl.2021.110799 [DOI] [PubMed] [Google Scholar]
- 26.Hong H, Chen F, Zheng X, et al. Decreased frequency of adenoidectomy by a 12-week nasal budesonide treatment. Ther Clin Risk Manag 2017;13:1309-1316. https://doi.org/10.2147/TCRM.S144659 10.2147/TCRM.S144659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sakarya EU, Muluk NB, Sakalar EG, et al. Use of intranasal corticosteroids in adenotonsillar hypertrophy. J Laryngol Otol 2017;131:384-390. https://doi.org/10.1017/S0022215117000408 10.1017/S0022215117000408 [DOI] [PubMed] [Google Scholar]
- 28.Colavita L, Miraglia Del Giudice M, Stroscio G, et al. Allergic rhinitis and adenoid hypertrophy in children: is adenoidectomy always really useful? J Biol Regul Homeost Agents 2015;29 (Suppl 1):58-63 (http://www.ncbi.nlm.nih.gov/pubmed/26634589). [PubMed] [Google Scholar]
- 29.De Corso E, Cantone E, Galli J, et al. Otitis media in children: Which phenotypes are most linked to allergy? A systematic review. Pediatr Allergy Immunol 2021;32:524-534. http://doi.org/10.1111/pai.13431 10.1111/pai.13431 [DOI] [PubMed] [Google Scholar]
- 30.Passàli D, De Benedetto M, Lauriello M, et al. Influence of Waldeyer’s ring hypertrophy on snoring and sleep apnea. Adv Otorhinolaryngol 2011;72:132-135. https://doi.org/10.1159/000324660 10.1159/000324660 [DOI] [PubMed] [Google Scholar]


