Abstract
Background
The COVID-19 pandemic has exacerbated the risk factors associated with suicidal behavior and thus, prioritizing its prevention is recommended.
Methods
This study systematically reviewed the global evidence on the incidence of suicide/suicidal attempts and the trend in suicidal rates during the COVID-19 pandemic. Cross-sectional and cohort studies investigating the outcomes of suicidal death and suicidal attempts at any setting during the COVID-19 pandemic were searched in Medline, Embase, and PsycINFO databases for papers published from December 2019 to May 2021.
Results
Out of 1052 studies18 studies with 12,746 suicidal attempts and 33,345 suicidal deaths were included in the final analysis. The mental health impact of social distancing, COVID-19 quarantine, and financial crises due to loss of employment were associated risk factors with suicide and/or suicidal attempts during the COVID-19 pandemic. Six common thematic recommendations for preventing suicidal deaths and suicidal attempts were identified.
Conclusions
Unexpected behavior changes during the COVID-19 pandemic may have contributed to the increasing trend of suicidal attempts reported. Domestic conflicts and violence, financial loss, anxiety and depression, and pre-existing mental health condition/s should be considered in preventing suicidal attempts and deaths secondary to the COVID 19 pandemic. Early detection and timely intervention for individuals with suicidal behavior is crucial and collated recommendations in the current study can be utilized for those preventive interventions. More systematic suicide risk screening process should be introduced who are at risk, along with an evidence base prevention approach.
Keywords: COVID-19 pandemic, Lockdown, Mental health, Suicide, Suicidal ideation, Suicide attempted, SARS-CoV-2 infection
Introduction
COVID-19 is an infectious disease caused by SARS-CoV-2 [1]. The first case of COVID-19 was reported in Wuhan, China, on December 31st, 2019, and afterward continued to spread across nearly 200 countries, causing an infection fatality rate of ~ 0.15% [2]. Considering the alarming levels of spread and severity, World Health Organization (WHO) declared it a pandemic on March 11th, 2020 [3]. Almost all the countries in the world provoked public health measures such as home confinement, closure of schools and universities, travel restrictions, and limit/ withhold social and physical distancing, while some countries declared it a public health emergency [4]. Many countries had to impose periods of lockdowns as an attempt to limit the spread of SARS-CoV-2. By early April 2020, more than one-third of the global population was under some form of movement restriction [5]. These strategies implemented in different countries intensively have caused substantial social and economic disruptions to individuals and the whole community [6]. While this disease has already directly impacted the physical health of millions of people, it is also causing mental health problems globally [7–9]. The evidence on the mental health harms caused by the response to COVID-19 found to be overwhelming, and studies on the general public revealed lower psychological well-being and higher scores of anxiety and depression compared to before COVID-19 [10]. The WHO also expressed its concern on the effect of COVID-19 on mental health and psycho-social consequences of an individual and it is estimated that COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide [11]. As new measures imposed in many countries such as self-isolation and quarantine, which affects day-to-day activities, routines, and livelihoods of people, they may lead to an increase in loneliness, anxiety, depression, insomnia, harmful alcohol and drug use, and self-harm or suicidal behaviour [12]. There is substantial evidence to demonstrate the deterioration of mental health among people during and after the COVID-19 pandemic compared to the pre-COVID-19 period [13–16]. Stack and Rockett (2021) discovered an increased suicide rate during the Spanish flu epidemic in 43 large cities, which was connected to the degree of social distancing, independent of the influenza fatality rate [17]. According to WHO, Every year more than 700,000 people die due to suicide [18]. However, there was no consistent evidence of a rise in suicide during and post-COVID era [19]. In this context, the research evidence on the effect of COVID-19 on suicides and suicidal attempts began to expand very rapidly. It is, therefore, timely and important to collate the global evidence on the incidence of suicide/suicidal attempts and the trend in suicidal rates during the COVID-19 pandemic. Thus, this study aimed to systematically review the available literature on (i) the incidence of suicidal attempts, suicidal deaths, and the trends in suicidal rates during the COVID-19 pandemic (ii) the risk factors for suicidal attempts and suicidal deaths during the COVID-19 pandemic, and (iii) the recommendations in preventing suicidal attempts or suicidal deaths during the COVID-19 pandemic.
Methods
Information sources and search strategy
The protocol for this systematic review was registered with the International Prospective Register of Systematic Reviews on May 5th 2021 (CRD42021253347). The Medline, Embase, and PsycINFO databases were searched for relevant studies from December 2019 to May 2021. The search strategy included a combination of keywords for COVID-19 and suicide/suicidal attempts. The language was restricted to English.
Study selection
Eligibility criteria for study inclusion were as follows: (1) studies that investigated suicidal deaths/ attempts of humans during COVID-19 pandemic (2) published after December 2019 and (3) adequately described the data on outcomes of suicidal death and suicidal attempts at any setting. Studies were excluded if any of the following criteria were noticed: (1) studies in languages other than English (2) study designs such as case studies, case reports, commentaries, editorials, letters to editor, reports, reviews, and systematic reviews, and (3) non-peer-reviewed articles and conference abstracts. The updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. Also the review has conducted in accordance with Cochrane handbook for systematic reviews [20]. The studies yielded during the search were exported to the Endnote (EndNote X9. 3. 3 version) reference manager software. Following the removal of duplicates, screening against the inclusion and exclusion criteria was undertaken by two independent individuals in two stages; 1) title and abstract screening, and 2) full-text screening in Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). Any discrepancies were resolved by consensus or by consultation with a third reviewer.
Data extraction
Two individuals extracted the data independently from the included full texts into an Excel spread sheet and cross-checked for further accuracy. Any discrepancies were resolved by consensus. Extracted information included the publication details (year, authors, country), characteristics of the studied sample (age, sex, and studied population), outcome variables (suicide deaths and suicidal attempts, method of suicide, previous history of suicide, and other risk factors reported), and recommendations to prevent future suicidal deaths or attempts.
Assessment of the quality of the studies
We assessed the quality of the included articles using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [21]. The checklist contained fourteen items, including 1) Was this paper’s research question or objective clearly stated? 2) Was the study population clearly specified and defined? 3) Was the participation rate of eligible persons at least 50%? 4) Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? 5) Was a sample size justification, power description, or variance and effect estimates provided? 6) For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? 7) Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? 8) For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure or exposure measured as continuous variable)? 9) Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? 10) Was the exposure(s) assessed more than once over time? 11) Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? 12) Were the outcome assessors blinded to the exposure status of participants? 13) Was loss to follow-up after baseline 20% or less? 14) Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? Two reviewers assessed the articles against each of the 14 items independently and then cross-checked them. Any discrepancies were resolved by consensus.
Data analysis
Descriptive statistics were used to report the findings of included studies according to the research objectives. Tables and graphs were used accordingly to present the details of the publication, characteristics of the sample and outcome variables. Common themes were identified and reported in presenting future recommendations for preventing COVID-19 related suicidal deaths and attempts.
Results
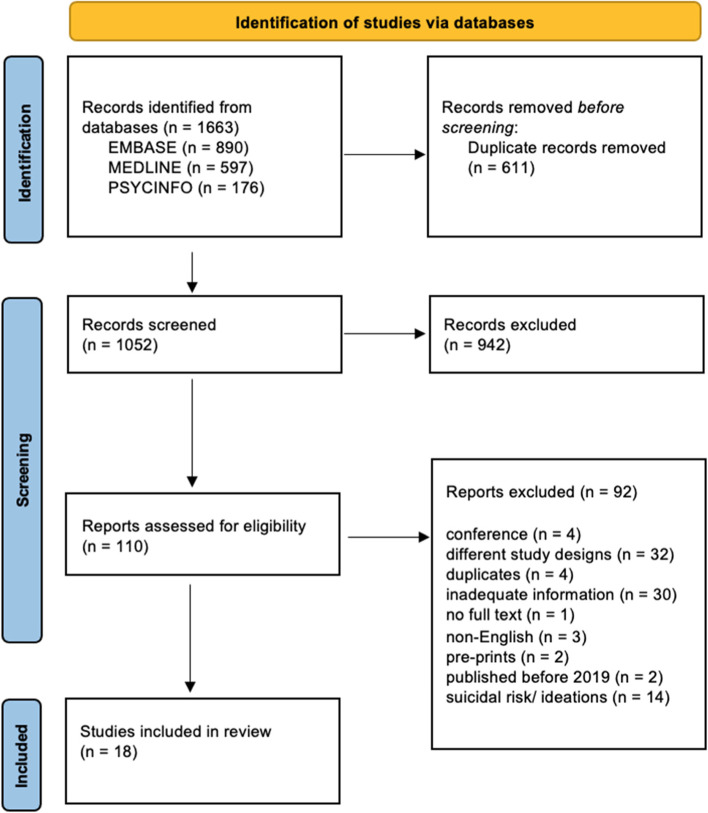
Based on the database search, 1663 articles published between December 2019 and May 2021 were retrieved, and 611 duplicates were removed. Out of 1052 studies, 942 were excluded during the title and abstract screening. Subsequently, 110 full articles were screened at the full-text screening stage, and 18 were included. The main reasons for exclusions were different study designs, suicidal risk/ ideations, and inadequate information. The study flow chart outlines the detailed review process (Fig. 1).
Fig. 1.
PRISMA flow chart of included studies
Characteristics of included studies
The main characteristics of the included studies are listed in Table 1. Some of the studies’ studied samples were composed only of suicidal attempts or suicidal deaths [22–29], while some of the studies included a wider sample to see the incidence of suicidal deaths and suicidal attempts [30–38]. The sample sizes of the studies that included only the suicidal deaths or suicidal attempts were ranged from 53 to 17,794. Sixteen (16) studies (88.9%) had a cross-sectional design and two studies [24, 26] have followed cohort design. Out of 18 studies included, 8 (44.4%) were from the United State of America [22, 24, 26, 30, 32, 34, 36, 38], 4 (22.2%) from Japan [25, 27, 29, 35], 2 (11.1%) from India [23, 37] and 1 (5.6%) each from Austria [31], Canada [33], German [28] and Nepal [39].
Table 1.
Characteristics of included studies
| Study (author and year) | Geography | Data collection period | Source of information | Design of the study | Studied population/occupation | Characteristics of the study sample | |||
|---|---|---|---|---|---|---|---|---|---|
| Sample size† | Age | Female/ male n (%) | Occupation | ||||||
| Ammerman et al., 2021 [30] | USA | April 03 – 04, 2020 | Online survey | Cross-sectional study | Amazon Mechanical Turk (mTurk) population | 907 | Mean (SD) 36.43 (11.02) |
Male 511 (56.3); Female 387 (42.6); Trans-gender 4 (0.4); Preferred not to answer 5 (0.6) |
Amazon Mechanical Turk (mTurk) |
| Bergmans and Larson 2021 [22] | USA | March 10th—October 31st, 2020 | Electronic medical records | Retrospective cross-sectional study | Daily ED encounters for suicide attempts and intentional self-harm to the University of Michigan Health System | 1348 |
Mean (SD) 27.9 (14.3) |
Male 533 (39.5); Female 815 (60.5); |
NR |
| Carlin et al., 2021 [31] | Austria | March 16th—May 15th, 2020 | Admission data at Trauma Resuscitation room of the Level 1 Trauma Center of the Medical University of Vienna-Austria | Retrospective cross-sectional study | Admissions to the level 1 Trauma Centre of the Medical University of Vienna | 65 |
Mean (SD) 38.7 (12.2) |
Male 17 (73.9); Female 06 (26.1) |
NR |
| Chiba et al., 2020 [32] | State of California, USA | March 20th—June 30th, 2020 | Trauma registry of Los Angeles County and University of Southern California Medical Center | Retrospective cross-sectional study | Trauma admissions to the Los Angeles County and University of Southern California Medical Center | 1,202 | Median (IQR) 40 (27–57) |
Male 927 (77.2) Female 275 (22.8) |
NR |
| Choudhury, 2020 [23] | India | March 24th—May 31st, 2020 | Police records- Lucknow, India | Retrospective cross-sectional study | Suicidal deaths in Lucknow, India | 59 | NR |
Male 33(55.9); Female 26(44.4) |
Business /self-employed 10(16.9%); Daily wages worker 15(25.4%); Govt. employee 3(5.0%); Domestic help 9(15.2%); Housewife 10(16.9%); Farmer 4(6.7%); Student 5(8.4%); Health care worker 3(5.0%) |
| Daly et al., 2021[33] | Canada | May 14 – 29, 2020 | Online survey | Cross-sectional study | Canadian adults | 3000 | Range 18 to 55 + |
Male 1460 (48.7); Female 1519 (50.6); Other 21 (0.7) |
NR |
| Faust et al., 2021 [24] | USA | January—July 2020 | Health Registry of Vital Records and Statistics | Cohort study | Suicide death data from the Massachusetts Department of Health Registry of Vital Records and Statistics | 139 | Mean 48.6 |
Male 105 (75.5); Female 34 (24.5) |
NR |
| Hill et al., 2021 [34] | Texas, USA | January to July 2020 | Electronic health records data for suicide-risk screens of an emergency department in a major metropolitan area in Texas | Cross-sectional study | Youth aged 11 and older who presented to the ED within any of three connected pediatric hospitals for any presenting complaint | 12,827 | NR |
Male 5257 (41%) Female 7570 (59%) |
NR |
| Holland et al., 2021 [35] | Japan | December 29th, 2019—October 10th, 2020 | Centres for Disease Control and Prevention’s National Syndromic Surveillance Program | Cross-sectional study | Patients who visited USA Emergency Departments for mental health conditions, suicide attempts, all drug overdose, opioid overdose, intimate partner violence, and child abuse and neglect | 1,872,945 | NR | Female 1,013,585 (0.54); Male 859,360 (0.46) | NR |
| Isumi et al., 2021 [25] | Japan | March–May 2020 | Public data on suicide statistics compiled by the Ministry of Health, Labor and Welfare | Cross-sectional study | Suicidal death among children and adolescents under 20 years of age | NR | NR | NR | NR |
| Mitchell & Li 2021 [26] | USA | March 10th—May 20th, 2020 | Connecticut Office of the Chief Medical Examiner | Retrospective cohort study | Residents in Connecticut State | 74 | Mean (SD) 50.8 (18.5) | Male 55 (74.3); Female 19 (25.7) | NR |
| Nomura et al., 2021 [27] | Japan | January—September 2020 | Monthly mortality data from the National Police Agency | Cross-sectional study | Suicidal deaths in Japan | 15,066 | NR |
Male 10,239 (68); Female 4827 (32) |
NR |
| Ontiveros et al., 2021 [36] | USA | March–May, 2020 | California Poison Control System database | Cross-sectional study | Calls received to the California Poison Control System regarding suicide attempts (suicidal ingestion) | 5807 | Range 12 to 70 + |
Male 2149 (37); Female 3658 (63) |
NR |
| Radeloff et al., 2021 [28] | German | January 1st—September 30th, 2020 | City of Leipzig’s cause of death statistics | Cross-sectional study | Data on suicide events in a major city in Germany- Saxony | 53 | NR | NR | NR |
| Sakamoto et al., 2021 [29] | Japan | January—December 2020 | National data on suicide deaths compiled by the National Police Agency | Cross-sectional study | National data of the number of individuals who died of suicide – Japan Self-employed-1019 (6%); Emplyed-5231 (31%); Student-1576 (9.4%); Unemployed-8095 (48%); Home maker-938 (5.6%) Occupational Data missing ( 935) | 17,794 | Range < 30 to ≥ 70 |
Male 11,779 (66.2); Female 6015 (33.8) |
NR |
| Sengupta et al., 2020 [37] | India | January 25- April 24, 2020 | Inquest reports, bed head tickets, injury reports and other relevant documents. Information was gathered from the deceased’s close relatives, friends, police and other available persons | Cross-sectional study | Autopsies conducted in the Department of Forensic Medicine and Toxicology, Cooch Behar Government Medical College and Hospital | 334 | Range 11 to 70 + |
Male- 60 (54.5); Female-50 (45.5) |
Farmers- 12 (10.9%) Labourer-16 (14.6%) Service men-5 (4.5%) Businessmen-12 (10.9%) Stduents-10 (9.1%) Housewives- 34 (30.9%) Unemployed-16 (14.6%) Unknown-5 (4.5%) |
| Shrestha et al., 2021 [39] | Nepal | March 24—June 23, 2020 | The electronic medical records of a Hospital | Cross sectional study | Patients presented to the ED of Dhulikhel hospital-Kathmandu University Hospital (DH-KUH) -Nepal | 55 | Median (95% CI) 29.7 (26.2–33.3) |
Male 21 (38.2); Female 34 (61.8) |
NR |
| Yeates et al., 2021 [38] | USA | January 1st—June 30th, 2020 | Trauma Center Records | Cross-sectional study | Southern California trauma population | 12,741 | NR | NR | NR |
†Sample size presented relevant to the data collection period mentioned in the same table, SD Standard deviation, NR Not reported
Incidence and the trends of suicide/suicidal attempts during the COVID-19 pandemic
12,746 suicidal attempts and 33,345 suicidal deaths were reported during the COVID-19 pandemic in the included studies. One other study has not reported separate data for suicidal attempts and deaths (n = 55), while one has presented rates. Because of the different durations used for data collection during the COVID-19 pandemic and the previous year (for non-COVID time comparison), it was unable to estimate or compare the suicidal incidence rate or to pool the data together for a meta-analysis. 16.7% (n = 3) of studies have no reported data on suicidal attempts or suicidal deaths trends. Regarding trends in suicidal attempts during the COVID-19 pandemic, an increasing trend was reported in 22.2% (n = 4) studies, while a decreased trend was reported in 11.1% (n = 2) studies. 5.6% (n = 1) of studies reported no increased or decreased trend in suicidal attempts. An increasing trend of suicidal deaths during the COVID-19 pandemic was found in 16.7% (n = 3), while decreased in 5.6% (n = 1) studies. 16.7% (n = 3) of studies reported no increased or decreased trends in suicidal deaths. Finally, 5.6% (n = 1) of studies reported decreased trends during the crisis but increased after the immediate crisis had passed (Table 2).
Table 2.
The impact of the COVID-19 pandemic on suicidal attempts, death rates and trends
| Study (author and year) | Suicidal deaths (SD)/ suicidal attempts (SA) during COVID-19 | Number of events during the corresponding period of the previous year (2019) | Method of suicide/ suicidal attempts | Previous history of attempts | The trend of suicides/ suicidal attempts during COVID pandemic |
|---|---|---|---|---|---|
| Ammerman et al., 2021 [30] | SA: 44 (4.9%) | NR | NR | NR | NR |
| Bergmans and Larson 2021 [22] | SA and Intentional self-harm: 1348 | October 1st, 2015 to March 9th, 2020: 9405 | NR | NR | SA and Intentional self-harm: Decreased |
| Carlin et al., 2021 [31] | SA: 23 (35.4%) | 2019: 8 |
Jump from a height 10 (43.5%); Jump in front of a moving object 2 (8.7%); Cutting 6 (26.1%); Driving off the street 1 (4.3%); Self-immolation 1 (4.3%); Hanging 2 (8.7%); Ingestion of poison, harmful substance etc. 1 (4.3%) |
NR | SA: Increased |
| Chiba et al., 2020 [32] | SA: 36 (3%) | 2019: 26 | NR | NR | SA: Increased |
| Choudhury, 2020 [23] | SD: 59 | NR |
Hanging 55(93.2%); Poisoning 2 (3.3%); Drowning 2 (3.3%) |
NR | NR |
| Daly et al., 2021 [33] | Deliberate self-harm: 48 (1.6%) | NR | NR | NR | NR |
| Faust et al., 2021 [24] | SD: 139 | 2019: 166 | NR | NR | SD: No change |
| Hill et al., 2021 [34] | SA: 286 (2.2%) | 2019: 268 | NR | NR | SA: Increased during some months (corresponds to COVID-19–related stressors and community responses were heightened) |
| Holland et al., 2021 [35] | SA: 5029 | 2019; 4614 | NR | NR | SA: Increased |
| Isumi et al., 2021 [25] | SD: Only the rates presented- March 0.229, April 0.201, May 0.216 per 100,000) | NR | NR | NR | SD: No change |
| Mitchell & Li 2021 [26] | SD: 74 (Age adjusted suicidal rate in 2020- 9.4 per 100,000 persons) | 2014 to 2019; 495 (Total) |
Suffocation- 35 (47.3%) Firearm- 21 (28.4%) Poisoning- 13 (17.6%) Other—5 (6.8%) |
NR | SD: Decreased |
| Nomura et al., 2021 [27] | SD: 15,066 | 2019; 15,520 | NR | NR | SD: Decreased during the time of crisis but increased after the immediate crisis has passed |
| Ontiveros et al., 2021 [36] | SA: 5807 | 2018 and 2019; 13,800 (Total) | Ingestion of poison | NR | SA: Decreased |
| Radeloff et al., 2021 [28] | SD: 53 | 2010 to 2019; 590 (Total) | NR | NR | SD: Not changed |
| Sakamoto et al., 2021 [29] | SD: 17,794 | 2016 to 2019; 12,398 (total of monthly mean number from) | NR | NR | SD: Increased |
| Sengupta et al., 2020 [37] | SD: 110 (February to April 2020); April 2020: 50 | SD: 33 (April 2019) |
Burns-10 (9.1%) Hanging- 80 (72.7%) Poisoning-15 (13.7%) Others- 5 (4.5%) |
NR |
SD: Increased *The number of suicide cases during the first month of the lockdown following the pandemic has drastically increased compared to a couple of months prior |
| Shrestha et al., 2021 [39] | SD & Self-harm: 55 | 2019; 38 | Poisoning 47 (85.5%), Drug overdose 4 (7.3%), Hanging 4 (7.3%) | NR | SD and Self-harm: Increased |
| Yeates et al., 2021 [38] | SA: 125 (1.9%) | 2019; 120 (1.6%) | NR | NR | SA: No change |
SD Suicidal deaths, SA Suicidal attempts, NR Not reported
Risk factors associated with suicide/suicidal attempts during COVID-19 pandemic
Out of 18 studies included in this systematic review, only six studies [22, 23, 27, 30, 33, 39] provided data on associated factors for suicide and/or suicidal attempts during the COVID-19 pandemic. The mental health impact of social distancing was reported as an associated factor by Ammerman et al., 2021, while COVID-19 quarantine was mentioned as an associated factor identified by Daly et al., 2021. Three studies [23, 27, 39] reported that financial crises due to loss of employment are associated with suicide and/or suicidal attempts during COVID-19. Table 3 shows the reported associated factors of suicide/suicide attempts during the COVID-19 pandemic.
Table 3.
Risk factors associated with suicidal deaths and suicidal attempts
| Study | Reported risk factors |
|---|---|
| Ammerman et al., 2021 [30] |
General distress Physical safety concerns Mental health impact of social distancing |
| Bergmans and Larson 2021 [22] |
Male sex Aged group of 18–65 years Having a history of three or more encounters of suicide attempt or intentional self-harm Unmarried |
| Choudhury, 2020 [23] |
Financial losses/job loss Domestic conflicts & violence Poverty and hunger Anxiety and depression |
| Daly et al., 2021 [33] |
COVID-19 quarantine Pre-existing mental health condition/s |
| Nomura et al., 2021 [27] |
Gender-based violence Loss of employment |
| Shrestha et al., 2021 [39] |
Disputes with family members Economic crisis |
Recommendations for prevention of suicide/suicidal attempts during the COVID-19 pandemic
Recommendations for preventing suicide/suicide attempts were provided in nine studies [23, 25, 27, 28, 30, 31, 33, 35, 37]. Of them, we have identified common thematic recommendations for preventing suicidal deaths and suicidal attempts, and those were; 1) Develop a systematic suicide screening process and increase the suicide risk screening [23, 25, 28, 30, 37]. 2) Facilitate communication and increase access to the interventions for the people at risk [30, 35], 3) Design, develop, and provide interventions for mental health and psychological well-being for the people at risk (including mental health awareness programs, promoting social connectedness) [23, 30, 31, 33, 35, 37] 4) Implement measures to mitigate the impact on the economy (e.g., Provision of economic supports and changes in payment policies) [35, 37], and 5) Regulation of media reporting [27, 37]. The study done by Nomura et al., 2021 in Japan revealed an increased rate of suicide among women. Therefore, they recommended feasible ways of strengthening the financial condition of women by providing direct income support, cut down of tax, postponement or exemption of social security payments for temporary workers, support for women's income security to end the gender pay gaps and regulations to correct the under-valuation of women’s work, and provision of paid leave and flexible working arrangements [27]. Ammerman et al., 2021 stress the need of empowering suicidal risk screening to identify those who are at risk [30]. One potential option to facilitate large-scale risk detection is to incorporate suicide risk screenings into the protocol at COVID-19 testing sites, as the routine screenings are not possible due to the social distancing and stay-at-home regulations. This may be accomplished by including one- or two-question screener that would result in a follow-up phone call to facilitate care linkage if a suicide risk is recognized [30]. Recommendations for preventing suicide/suicidal attempts during the COVID-19 pandemic suggested by individual studies are shown in Table 4.
Table 4.
Recommendations for preventing suicidal deaths and suicidal attempts
| Study | Recommendations |
|---|---|
| Ammerman et al., 2021 [30] |
− Increase suicide risk screening to identify those who are at risk − Introduce a more systematic screening process (e.g. integrate suicide risk screenings into the protocol at COVID-19 testing sites) − Implementation of follow-up phone calls to facilitate care connection, if suicide risk is indicated − Increase access to intervention for those who are experiencing psychological distress related to COVID-19 |
| Carlin et al., 2021 [31] | − Consideration of mental health and psychological well-being when establishing lockdown policies |
| Choudhury, 2020 [23] |
− Develop strategies and implement appropriate and timely interventions to eliminate the contributing predisposing factors to suicide − Implementation of community-based gatekeeper training programmes for early identification of suicidal ideations − Improvement of mental health awareness of individuals by the government along with the help of various NGOs − Strengthening of suicide screening services in the health care sector |
| Daly et al., 2021 [33] | − Implementation of evidenced based strategies to minimize the risk of mental health deterioration associated with COVID-19 quarantine |
| Holland et al., 2021 [35] |
− Provision of counselling for those who are presented to emergency departments with risk of suicide/suicide attempts − Make linkage with existing behavioural health and social support services to provide immediate support for those who are in crisis − Conversion of existing in-person services health and social service to virtual means − Implementation of mass media campaigns that emphasize resilience, help-seeking, and available resources − Provision of economic supports to minimize financial stress, changes in payment policies − Regulatory changes to support telehealth − Promoting social connectedness |
| Nomura et al., 2021 [27] |
− Implementation of immediate measures to mitigate the negative economic impact of COVID-19 on women − Strengthening virtual linkages for social support and mental health care delivery utilizing virtual platforms like video calls, telephones and social media − Regulation for media reporting to ensure the avoidance of fear and hopelessness among people |
| Radeloff et al., 2021 [28] | − Careful monitoring of the suicidal rate as the COVID-19 crisis progresses in order to establish an evidence base prevention approaches |
| Sengupta et al., 2020 [37] |
− Increase public awareness on how to deal with pressure and anxiety during the COVID-19 crisis − Implementation of targeted mental health surveillance of population at risk (e.g. patients with prior mental health diagnosis and older adults) − Provision of financial grants for food and unemployment support by the government − Refrain from irresponsible media reporting of suicide and highlight the precise facts about the causes and circumstances of suicide with due consideration to mental health problems − Establishment of policies/regulations for media reporting regarding reporting of such suicidal deaths |
| Isumi et al., 2021 [25] | − Close monitoring of suicide rates in children as the COVID-19 crisis in order to implement preventive measures, particularly after the reopening of schools |
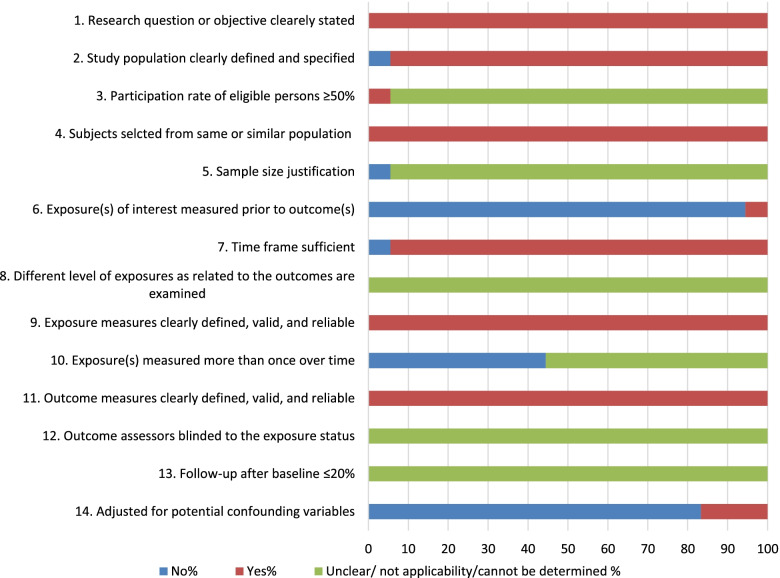
The quality of the included studies
In terms of the quality of included studies, six criteria out of 14 (43%) were satisfied by almost all of the included studies. Those criteria were; clearly defined research objective/s, clearly defined study populations, selection of subjects from a similar population, sufficient time frame, clearly defined exposure measures and clearly defined outcome measures. More than 80% of the studies have not measured the exposure before outcomes and adjusted for confounding variables. More than 40% of studies measured the exposure more than once over a time. Lastly, there were five criteria (36%) that we could not determine the quality or not applicable to assess the particular criteria in almost all the studies. Those criteria were; over ≥ 50% participation rate of the eligible person, having a justified sample size, having a different level of exposures as related to the outcomes examined, having blinded assessors of outcome/ s to the exposure status, and having a ≤ 20 follow-up from baseline (Fig. 2).
Fig. 2.
Quality assessment of included studies
Discussion
This systematic review presents several vital factors based on more than 12,746 suicidal attempts and 33,345 suicidal deaths reported during the COVID-19 pandemic. Suicidal death is a preventable loss that disturbs families, communities, and countries. Globally, it is a significant public health problem, and more than 700 000 people die due to suicide every year [40]. The present review found that the majority of the studies reported an increasing trend of suicidal attempts during the COVID 19 pandemic compared to the rates reported before the pandemic. Nevertheless, a review done in 2020 to find the suicidal behaviors and ideation during emerging viral disease outbreaks before the COVID-19 pandemic found weak evidence to suggest a significant increase in suicidal attempts and deaths by suicide during emerging viral disease outbreaks [41]. Compared to the global past pandemics, COVID 19 has tricky and complex mechanisms that have facilitated its rapid and catastrophic spread worldwide [42]. It is considered the most severe pandemic of the twenty-first century [43]. The rise in community distress due to the unexpected spread and rise of covid-19 virus has led to a pandemic status, eventually may have caused for the increasing trend of suicidal attempts reported during the COVID 19 pandemic compared to similar pandemics the world experienced before.
According to the WHO, a prior suicide attempt in normal circumstances is considered the most critical risk factor for suicide in the general population. However, the present systematic review reported domestic conflicts and violence, financial loss/job loss, anxiety and depression, and pre-existing mental health condition/s were there among the identified risk factors for suicidal attempts and suicidal deaths during the COVID-19 pandemic.
The social restriction practices and policies imposed by different countries secondary to the COVID 19 pandemic might have negatively influenced the fore-said risk factors that has been indirectly led increased rates of suicidal attempts and deaths. Moreover, in the wake of COVID 19, millions of people lost their access to employment and experienced financial hardships in day-to-day life [44]. It was evident that financial/employment-related issues substantially contribute to 13% of suicide deaths [45]. On the other hand, job loss or financial hardships independently lead to significant and persistent increases in domestic violence [46]. Similarly, social isolation and stay-at-home rules imposed by many counties badly resulted in domestic violence, making survivors of domestic violence at risk for further violence and isolating them from networks of support [47]. Furthermore, it is evident that during pandemics, a considerable number of people present with anxiety and depressive symptoms though they do not have any pre-existing mental health conditions [8]. As a result of this, some experience post-traumatic stress disorders in due course of their lives, which can end up with suicidal attempts or deaths. Nonetheless, a delayed increase in suicide rates is possible following major disasters [48–50]. Therefore, preventing suicidal attempts and deaths in the context of COVID 19 is a critical public health priority.
Considering the importance of preventing suicidal attempts and deaths secondary to the COVID 19 pandemic, early detection and timely intervention for individuals with suicidal behaviors is crucial [51]. Unlike previous pandemics, COVID-19 is occurring in the modern digital world, where video conferencing and virtual healthcare provision are widely available [52]. Although some people experience suicidal ideas during this pandemic, they might not attempt to seek help because of fear that meeting a health care professional face-to-face might put them at risk of contacting COVID-19. In this regard, as several studies have already identified the positive effects of new technologies in combating and preventing suicidal behavior, virtual platforms can be used as an effective way of screening to identify the people those at risk at the early stages [51, 53]. To strengthen this approach, community-based training programs can be used periodically to approach the neediest people early. Moreover, media should also be responsible when reporting facts, avoiding stoking fear and hopelessness among people in the community [18]. Therefore, it is recommended to use the recommendations given by this review to prevent suicidal attempts or suicidal deaths during the COVID-19 pandemic.
There are a few limitations in this review. The findings of this review can be limited because of not including the potential articles beyond the search strategies. Besides, the studies included in this review used different durations for data collection during the COVID 19 pandemic making it difficult to estimate the incidence rate of suicidal attempts and deaths only for the COVID 19 pandemic. Moreover, the inter-rater agreement was not calculated for this review as the screening process was undertaken in Covidence systematic review manager software. Despite these limitations, this review provides; (i) the first observation of suicidal attempts and suicidal deaths during the COVID-19 pandemic, (ii) the risk factors for suicidal attempts and suicidal deaths during the COVID-19 pandemic, and (iii) the recommendations in preventing suicidal attempts or suicidal deaths during the COVID-19 pandemic. Suicide prevention in the COVID-19 era and similar pandemics are crucial and challenging. Therefore, it is essential to select appropriate suicide prevention strategies based on strong evidence. The findings of this study can be used when selecting appropriate suicide prevention strategies considering the identified risk factors and recommendations given. It is recommended to discuss the longitudinal trends in future studies.
Acknowledgements
Not applicable.
Authors’ contributions
I.W, M.L.P., H.M.R.K.G.N. and A.M.M.P.A. conceptualized the study. M.L.P., H.M.R.K.G.N., and A.M.M.P.A selected studies. M.L.P., H.M.R.K.G.N. and I.W extracted and analysed data and drafted the manuscript. All the authors were critically reviewed and approved the final version of the manuscript.
Funding
There was no funding provided for this study.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author.
Declarations
Ethics approval and consent to participate
This study did not require ethical approval, because this review was based on publicly available scientific literature.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Coronavirus disease (COVID-19) pandemic [https://www.who.int/emergencies/diseases/novel-coronavirus-2019]
- 2.Ioannidis JPA. Reconciling estimates of global spread and infection fatality rates of COVID-19: An overview of systematic evaluations. Eur J Clin Invest. 2021 doi: 10.1111/eci.13554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta bio-med. 2020 doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jernigan DB, CDC COVID-19 Response Team Update: public health response to the coronavirus disease 2019 outbreak—United States, February 24, 2020. Morb Mortal Wkly Rep. 2020;69(8):216–216. doi: 10.15585/mmwr.mm6908e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koh D. COVID-19 lockdowns throughout the world. Occup Med. 2020;70(5):322. doi: 10.1093/occmed/kqaa073. [DOI] [Google Scholar]
- 6.Asahi K, Undurraga EA, Valdés R, Wagner R. The effect of COVID-19 on the economy: evidence from an early adopter of localized lockdowns. J Glob Health. 2021;11:05002. doi: 10.7189/jogh.10.05002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cullen W, Gulati G, Kelly BD. Mental health in the Covid-19 pandemic. QJM: Int J Med. 2020;113(5):311–2. doi: 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 9.Talevi D, Socci V, Carai M, Carnaghi G, Faleri S, Trebbi E, di Bernardo A, Capelli F, Pacitti F. Mental health outcomes of the CoViD-19 pandemic. Riv Psichiatr. 2020;55(3):137–144. doi: 10.1708/3382.33569. [DOI] [PubMed] [Google Scholar]
- 10.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behavior Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization: Mental health and psychosocial considerations during COVID-19 outbreak. World Health Organization. 2020 (January). p. 1–6.
- 12.Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health. 2020;30(1):1–2. doi: 10.1080/09638237.2020.1757052. [DOI] [PubMed] [Google Scholar]
- 13.Breslau J, Finucane ML, Locker AR, Baird MD, Roth EA, Collins RL. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev Med. 2021;143:106362. doi: 10.1016/j.ypmed.2020.106362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benke C, Autenrieth LK, Asselmann E, Pané-Farré CA. Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020;293:113462. doi: 10.1016/j.psychres.2020.113462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36(4):e00054020. doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- 16.Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, Kontopantelis E, Webb R, Wessely S, McManus S, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stack S, Rockett IRH. Social distancing predicts suicide rates: Analysis of the 1918 flu pandemic in 43 large cities, research note. Suicide Life-Threat Behav. 2021;51(5):833–835. doi: 10.1111/sltb.12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organiztion . Preventing suicide: A global imperative: World Health Organization. 2014. [Google Scholar]
- 19.John A, Eyles E, Webb RT, Okolie C, Schmidt L, Arensman E, Hawton K, O’Connor RC, Kapur N, Moran P, et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review. F1000Res. 2020;9:1097. doi: 10.12688/f1000research.25522.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA , 2022. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 In.: Cochrane; (updated February 2022).
- 21.Study Quality Assessment Tools [https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools]
- 22.Bergmans RS, Larson PS. Suicide attempt and intentional self-harm during the earlier phase of the COVID-19 pandemic in Washtenaw County, Michigan. J Epidemiol Community Health. 2021;75(10):963–969. doi: 10.1136/jech-2020-215333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choudhury R. An observational analysis of suicidal deaths during COVID 19 pandemic lockdown at Lucknow, India. Indian J Forensic Med Toxicol. 2020. 10.37506/ijfmt.v14i4.11517.
- 24.Faust JS, Shah SB, Du C, Li SX, Lin Z, Krumholz HM. Suicide Deaths During the COVID-19 Stay-at-Home Advisory in Massachusetts, March to May 2020. JAMA Netw Open. 2021;4(1):e2034273. doi: 10.1001/jamanetworkopen.2020.34273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Isumi A, Doi S, Yamaoka Y, Takahashi K, Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020;110(Pt 2):104680. doi: 10.1016/j.chiabu.2020.104680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell TO, Li L. State-Level Data on Suicide Mortality During COVID-19 Quarantine: Early Evidence of a Disproportionate Impact on Racial Minorities. Psychiatry Res. 2021;295:113629. doi: 10.1016/j.psychres.2020.113629. [DOI] [PubMed] [Google Scholar]
- 27.Nomura S, Kawashima T, Yoneoka D, Tanoue Y, Eguchi A, Gilmour S, Kawamura Y, Harada N, Hashizume M. Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Res. 2021;295:113629. doi: 10.1016/j.psychres.2020.113622. [DOI] [PubMed] [Google Scholar]
- 28.Radeloff D, Papsdorf R, Uhlig K, Vasilache A, Putnam K, von Klitzing K. Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol Psychiatr Sci. 2021;30:e16. doi: 10.1017/S2045796021000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakamoto H, Ishikane M, Ghaznavi C, Ueda P. Assessment of Suicide in Japan During the COVID-19 Pandemic vs Previous Years. JAMA Netw Open. 2021;4(2):e2037378. doi: 10.1001/jamanetworkopen.2020.37378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ammerman BA, Burke TA, Jacobucci R, McClure K. Preliminary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the U.S. J Psychiatr Res. 2021;134:32–38. doi: 10.1016/j.jpsychires.2020.12.037. [DOI] [PubMed] [Google Scholar]
- 31.Carlin GL, Baumgartner JS, Moftakhar T, Konig D, Negrin LL. Impact of COVID-19 lockdown on suicide attempts : A retrospective analysis of the springtime admissions to the trauma resuscitation room at the Medical University of Vienna from 2015–2020. Wien Klin Wochenschr. 2021;133(17-18):915–922. doi: 10.1007/s00508-021-01839-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chiba H, Lewis M, Benjamin ER, Jakob DA, Liasidis P, Wong MD, Navarrete S, Carreon R, Demetriades D. "Safer at home": The effect of the COVID-19 lockdown on epidemiology, resource utilization, and outcomes at a large urban trauma center. J Trauma Acute Care Surg. 2021;90(4):708–713. doi: 10.1097/ta.0000000000003061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daly Z, Slemon A, Richardson CG, Salway T, McAuliffe C, Gadermann AM, Thomson KC, Hirani S, Jenkins EK. Associations between periods of COVID-19 quarantine and mental health in Canada. Psychiatry Res. 2021;295:113631. doi: 10.1016/j.psychres.2020.113631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide Ideation and Attempts in a Pediatric Emergency Department Before and During COVID-19. Pediatrics. 2021;147(3):e2020029280. doi: 10.1542/peds.2020-029280. [DOI] [PubMed] [Google Scholar]
- 35.Holland KM, Jones C, Vivolo-Kantor AM, Idaikkadar N, Zwald M, Hoots B, Yard E, D'Inverno A, Swedo E, Chen MS, et al. Trends in US Emergency Department Visits for Mental Health, Overdose, and Violence Outcomes Before and During the COVID-19 Pandemic. JAMA Psychiat. 2021;78(4):372–379. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ontiveros ST, Levine MD, Cantrell FL, Thomas C, Minns AB. Despair in the time of COVID: A look at suicidal ingestions reported to the California Poison Control System during the pandemic. Acad Emerg Med. 2021;78(4):372–379. doi: 10.1111/acem.14209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sengupta D, Saha S, Bharatee P, Prasad R. Pattern of Suicidal Deaths in the First Month of Lockdown at A Tertiary Care Hospital: a Time Trend Analysis. Indian J Forensic Med Toxicol. 2020;14(4):167. [Google Scholar]
- 38.Yeates EO, Grigorian A, Barrios C, Schellenberg M, Owattanapanich N, Barmparas G, Margulies D, Juillard C, Garber K, Cryer H, et al. Changes in traumatic mechanisms of injury in Southern California related to COVID-19: Penetrating trauma as a second pandemic. J Trauma Acute Care Surg. 2021;90(4):714–721. doi: 10.1097/TA.0000000000003068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shrestha R, Siwakoti S, Singh S, Shrestha AP. Impact of the COVID-19 pandemic on suicide and self-harm among patients presenting to the emergency department of a teaching hospital in Nepal. PLoS ONE. 2021;16(4):e0250706. doi: 10.1371/journal.pone.0250706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suicide [https://www.who.int/news-room/fact-sheets/detail/suicide]
- 41.Leaune E, Samuel M, Oh H, Poulet E, Brunelin J. Suicidal behaviors and ideation during emerging viral disease outbreaks before the COVID-19 pandemic: a systematic rapid review. Prev Med. 2020;141:106264. doi: 10.1016/j.ypmed.2020.106264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pitlik SD. COVID-19 compared to other pandemic diseases. Rambam Maimonides Med J. 2020;11(3):e0027. doi: 10.5041/RMMJ.10418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yamamoto V, Bolanos JF, Fiallos J, Strand SE, Morris K, Shahrokhinia S, Cushing TR, Hopp L, Tiwari A, Hariri R. COVID-19: review of a 21st century pandemic from etiology to neuro-psychiatric implications. J Alzheimers Dis. 2020;77(2):459–504. doi: 10.3233/JAD-200831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crayne MP. The traumatic impact of job loss and job search in the aftermath of COVID-19. Psychol Trauma. 2020;12(S1):S180–S182. doi: 10.1037/tra0000852. [DOI] [PubMed] [Google Scholar]
- 45.Coope C, Donovan J, Wilson C, Barnes M, Metcalfe C, Hollingworth W, Kapur N, Hawton K, Gunnell D. Characteristics of people dying by suicide after job loss, financial difficulties and other economic stressors during a period of recession (2010–2011): A review of coroners׳ records. J Affect Disord. 2015;183:98–105. doi: 10.1016/j.jad.2015.04.045. [DOI] [PubMed] [Google Scholar]
- 46.Bhalotra S, Britto GCD, Pinotti P, Sampaio B. ob displacement, unemployment benefits and domestic violence. 2021. [Google Scholar]
- 47.Anurudran A, Yared L, Comrie C, Harrison K, Burke T. Domestic violence amid COVID-19. Int J Gynaecol Obstet. 2020;150(2):255–256. doi: 10.1002/ijgo.13247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Orui M, Suzuki Y, Maeda M, Yasumura S. Suicide Rates in Evacuation Areas After the Fukushima Daiichi Nuclear Disaster. Crisis. 2018;39(5):353–363. doi: 10.1027/0227-5910/a000509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kõlves K, Kõlves KE, De Leo D. Natural disasters and suicidal behaviours: A systematic literature review. J Affect Disord. 2013;146(1):1–14. doi: 10.1016/j.jad.2012.07.037. [DOI] [PubMed] [Google Scholar]
- 50.Matsubayashi T, Sawada Y, Ueda M. Natural disasters and suicide: Evidence from Japan. Soc Sci Med. 2013;82:126–33. doi: 10.1016/j.socscimed.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 51.McIntyre RS, Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020;19(2):250–251. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sinyor M, Knipe D, Borges G, Ueda M, Pirkis J, Phillips MR, Gunnell D. Suicide risk and prevention during the COVID-19 pandemic: one year on. Arch Suicide Res. 2021;23:1–6. 10.1080/13811118.2021.1955784. [DOI] [PubMed]
- 53.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. 2020;26(5):571–3. 10.1089/tmj.2020.29040.rb. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.