Abstract
(1→3)-β-d-Glucans have been recognized as a potential causative agent responsible for bioaerosol-induced respiratory symptoms observed in both indoor and occupational environments. A specific enzyme immunoassay was developed to quantify (1→6) branched, (1→3)-β-d-glucans in environmental samples. The assay was based on the use of a high-affinity receptor (galactosyl ceramide) specific for (1→3)-β-d-glucans as a capture reagent and a monoclonal antibody specific for fungal cell wall β-d-glucans as a detector reagent. The assay was highly specific for (1→6) branched, (1→3)-β-d-glucans (such as that from Saccharomyces cerevisiae) and did not show any response at 200 ng/ml to curdlan, laminarin, pustulan, dextran, mannan, carboxymethyl cellulose, and endotoxins. The detection level was 0.8 ng/ml for baker's yeast glucan and Betafectin. A coefficient of variation of 7.8% was obtained for (1→3)-β-d-glucans in house dust samples. Metal working fluids spiked with (1→3)-β-d-glucans inhibited the glucan assay. Because the assay is specific for (1→6) branched, (1→3)-β-d-glucans and is sensitive and reproducible, it will be useful for the investigation of health effects from exposure to this class of biologically active molecules.
(1→3)-β-d-Glucans are carbohydrate polymers found in the cell walls of most fungi, some bacteria, yeasts, and higher and lower plants. The molecular weight, degree of (1→6)-linked side branching, helical conformation, and solubility are the most important factors which determine the biological activities of (1→3)-β-d-glucans. The biological activities of (1→3)-β-d-glucans include host-mediated antitumor activity (11), adjuvant effects (21), and activation of neutrophils (34), eosinophils (23), macrophages (15, 27), and complement (26).
There is increasing evidence that (1→3)-β-d-glucans cause nonspecific inflammatory reactions (9, 10) and are responsible for bioaerosol-induced respiratory symptoms observed in both indoor (24, 25, 32) and occupational (4, 5) environments. Dose-response relationships have been found between levels of (1→3)-β-d-glucans and eye and throat irritation, dry cough, and itching skin (25). Relationships have also been found among exposure to (1→3)-β-d-glucans and an increased prevalence of atopy, a decrease in forced expiratory volume in 1 s in adults (30), and peak flow variability in children (6). Recent studies have reported significantly high levels of (1→3)-β-d-glucans in residential (31, 33) and occupational (3) environments.
At present, the inhibition enzyme immunoassay and the Limulus assay are widely used to quantify (1→3)-β-d-glucans. The inhibition enzyme immunoassay described by Douwes et al. (3) reacts with both linear and branched (1→3)-β-d-glucans. The reactions of antibodies with plant glucans [e.g., barley glucan, a (1→3)(1→4)-β-d-glucan] suggest that this assay is not highly specific for the (1→6) branched, β(1→3)-glucans characteristic of fungi. The detection limit of 40 ng/ml limits this assay to only high-exposure environments and settled dust from homes.
Like the inhibition enzyme immunoassay, the glucan-reactive Limulus assay recognizes both linear and branched β-glucans (29). The assay is extremely sensitive (1 to 10 pg/ml). However, its reactions with gyrophoran [(1→6)-β-d-glucan], negaran [(1→3)(1→4)-α-d-glucan], and yeast α-d-mannan [(1→2)(1→3)(1→6)-α-d-glucan] demonstrate the low specificity of this assay for (1→3)-β-d-glucans. Moreover, the reactivity of factor G, the Limulus protein that binds (1→3)-β-d-glucans, is dependent on the molecular weight, conformation, and degree of branching of the glucans (18). (1→3)-β-d-Glucans with higher molecular weights show greater reactivity with glucan-reactive Limulus, and single-helix and randomly coiled conformers are favored over triple-helix structures. However, all three conformers of (1→3)-β-d-glucans are recognized as important factors contributing to the biological activities of glucans (18, 20).
In the present study, we describe the use of an enzyme-linked immunosorbent assay (ELISA), which was originally developed as a diagnostic assay for systemic fungemia (8), to assay (1→3)-β-d-glucans in house dust samples, some mould cultures, and metal working fluid samples. The assay is based on the use of a high-affinity receptor (galactosyl ceramide, a sphingolipid) specific for (1→3)-β-d-glucans as a capture reagent and a monoclonal antibody specific for complex fungal cell wall (1→3)-β-d-glucans as a detector reagent. The assay is reported to be rapid, specific for fungal β-glucans, and insensitive to interference caused by agents which affect the Limulus assay.
MATERIALS AND METHODS
Galactosyl ceramide (Galactercerebroside type II; Sigma, St. Louis, Mo.) and 1% bovine serum albumin (BSA) (Sigma) in Tris-buffered saline (pH 8.0) (TBS) were used, respectively, for coating and blocking. Immulon 96-well polystyrene microtiter plates (Thermo Labsystems, Franklin, Mass.) were used for the immunoassay.
We obtained baker's yeast glucan (Saccharomyces cerevisiae), barley glucan, mushroom glucan (Pleurotus ostreatus), laminarin (Laminaria digitata), curdlan (Alcaligenes faecalis), mannan (S. cerevisiae), dextran (Leuconostoc mesenteroides), and carboxymethyl cellulose from Sigma and pustulan (Umbilicaria papullosa) from Calbiochem (La Jolla, Calif.). The pharmaceutical-grade glucan Betafectin (S. cerevisiae) and the mouse anti-(1→3)-β-d-glucan immunoglobulin M (IgM) monoclonal antibody were obtained from The Collaborative Group (Hauppauge, N.Y.), and goat anti-mouse IgM-horseradish peroxidase conjugate and tetramethylbenzidine were obtained from Calbiochem.
House dust, some selected fungi, and metal working fluids (synthetic, semisynthetic, and soluble) were assayed for (1→3)-β-d-glucans.
For microbiological culturing of fungi, we obtained dichloran-glycerol agar (DG18) from Remel Inc. (Lenexa, Kans.). Malt extract agar was prepared in the laboratory by dissolving 20 g of malt extract, 20 g of dextrose, 15 g of agar, and 1 g of peptone in 1 liter of distilled water.
We were provided with house dust samples collected as part of an ongoing study of childhood asthma in Connecticut. Samples were collected from 20 homes; 10 samples were from houses having dogs, and the rest were from houses without dogs. House dust samples were collected in the main living area by vacuuming (Eureka Mighty-Mite vacuum cleaner) the furniture (including seat cushions, seat back, and arms of the chair) used most often by the family for 3 min and a 1-m2 area in the center of the room for 2 min. The dust samples were collected in cellulose extraction thimbles (Whatman International Ltd., Maidstone, United Kingdom). The thimbles containing dust samples were placed carefully inside Ziplock bags and kept at 4°C immediately after sampling and during transportation to the laboratory. The thimbles were stored at −70°C in the laboratory until the samples were processed for endotoxin and glucan assays.
Samples (approximately 25 mg of house dust) were sonicated (model 3200R-1 sonicator; Branson Cleaning Equipment Co., Shelton, Conn.) in 5 ml of triethylamine phosphate buffer, containing 0.01% triethylamine and 0.05 M potassium phosphate (pH 7.5). After the first 15 min of sonication, each sample was vortexed (VWR vortexer 2; Scientific Industries Inc., Bohemia, N.Y.) for 1 min and separated into two equal portions. One portion was further sonicated for another 45 min and assayed for endotoxins according to the method described by Milton et al. (16, 17). The other portion was further vortexed for 1 min and autoclaved at 120°C (105 Pa) (Sterilmatic incubator; Market Forge Industries, Everett, Mass.) for 1 h. After being vortexed for 5 min, the portions were centrifuged for 15 min at 1,000 × g (Heraeus Megafuge 20R; Kendro Lab Products GmbH, Hanau, Germany), the supernatants were assayed immediately, and the remaining solutions were stored at −20°C for further assays. Samples were analyzed in triplicate on three different days. Prior to each replicate glucan assay, both the stored sample extracts and the standards were reautoclaved.
Fungi from air were originally recovered on DG18 plates using a Burkard portable culture plate sampler (Burkard Manufacturing Co. Ltd., Rickmansworth, United Kingdom). The sampling was carried out at a flow rate of 30 liter/min for 1 min. Other isolates were recovered directly on 2% malt extract agar plates. Then, the plates were incubated, and the pure cultures of selected fungi were prepared by transferring isolates from the original plates to 2% malt extract agar plates using a sterile wire loop. After inoculation, the plates were incubated at room temperature for 1 week. One-week-old pure cultures (mycelium and spores together) were used for the assay. First, the surface of the agar medium was carefully scraped using a sterile spatula; then, the fungal biomass was transferred to a preweighed sterile tube. After the sample weights were taken, the fungal samples were extracted by the procedure used above and assayed for (1→3)-β-d-glucans.
Neat synthetic, semisynthetic, and soluble metal working fluids were obtained from General Motors Corporation. Neat fluids were diluted (1:20) to obtain the working-strength solutions used in the industry. Then, the diluted solutions were spiked with baker's yeast to a final (1→3)-β-d-glucan concentration of 10 μg/ml, extracted, and assayed for (1→3)-β-d-glucans.
Most of the purified glucans used as positive and negative controls (mentioned above) were insoluble in water. Therefore, the stock solutions of these glucans in TBS were prepared by autoclaving solutions for 15 min at 120°C (105 Pa).
The ELISA was performed as follows. Galactosyl ceramide (0.1 mg/ml) dissolved in absolute alcohol by gentle heating was used to coat (100 μl) each well of an Immulon plate. The contents of the plate were allowed to evaporate at room temperature. Then, the free sites of the wells were blocked with 1% BSA in TBS (200 μl per well) for 1 h. The plate contents were decanted immediately prior to the addition of the standard and samples. Five dilutions of the standard and samples were prepared in TBS. Baker's yeast glucan (derived from S. cerevisiae) was used as the standard with serial 1:3 or 1:4 dilutions starting from 200 ng/ml. The dilutions were then added to the plate (100 μl per well) and incubated for 4 h or overnight at 37°C. The mouse anti-(1→3)-β-d-glucan IgM monoclonal antibody (approximately 8.8 mg/ml) was diluted 1:10,000 in 1% BSA in TBS and added (100 μl per well) to the plate after the plate was washed with TBS. The plate was incubated for 2 h at 37°C. Then, the plate was washed again before the goat anti-mouse IgM-horseradish peroxidase conjugate (1:10,000 dilution prepared in 1% BSA in TBS from the original 1-mg/ml conjugate solution) was added (100 μl per well). The plate was incubated at 37°C for 1 h and was washed several times with TBS. Tetramethylbenzidine (100 μl per well) was used to develop color. The plate was read at 620 nm during 30 min of incubation at 37°C in a microtiter plate reader (Kinetic-QCL; Whittaker Bioproducts, Walkersville, Md.).
For each microtiter plate, five dilutions in duplicate of the standard and each sample were included together with six control wells. The maximum absorbance at 28 min minus the baseline absorbance for each well was used as the response. A four-parameter logistic-fit with inverse prediction (1) was used to calculate the (1→3)-β-d-glucan concentrations and the assay-based standard error for each pair of dilutions of the unknown samples. We reported for each unknown the mean from the dilutions of the unknown that gave a response closest to the middle of the standard curve and that gave the lowest standard error.
The coefficient of variation for (1→3)-β-d-glucans in the house dust samples was computed with PROC MIXED (version 8.1; SAS Institute, Cary, N.C.) using a random effect of sample. The limit of detection was defined as the concentration that produced an absorbance reading twice that of the blanks.
RESULTS
The limit of detection for baker's yeast and Betafectin was 0.8 ng/ml (Table 1). Mushroom glucan derived from the fungus P. ostreatus showed a limit of detection of 60 ng/ml. For laminarin, the limit of detection was 5,000 ng/ml, and for pustulan, the level was 1,000 ng/ml. The monoclonal antibody did not show any response to curdlan, carboxymethyl cellulose, dextran, mannan, and endotoxins. Betafectin and baker's yeast glucan had similar responses; 1 ng of Betafectin was equivalent to 1.06 ng (standard deviation, ±0.26) of baker's yeast glucan. Mushroom glucan from P. ostreatus had a low affinity for the antibody; 1 ng of mushroom glucan was equivalent to 0.013 ng (standard deviation, ±0.002) of baker's yeast glucan.
TABLE 1.
Specificity of the immunoassay
| (1→3)-β-d-Glucans and related polysaccharides | Source | Main linkagea | Mol wt | Limit of detection (ng/ml)b |
|---|---|---|---|---|
| Endotoxin | Escherichia coli | (1→2)-β-d-Oligoglucosides | 8,000 | NDc |
| Curdlan | Alcaligenes faecalis | (1→3)-β-d-glucan (L, homogeneous) | 136,000 | NDd |
| Barley glucan | Barley plant | (1→3)(1→4)-β-d-glucan (L) | 23,100 | NDd |
| Mushroom glucan | Pleurotus ostreatus | (1→4)(1→6)(1→3)-β-d-glucan | 720,000 | 60 |
| Yeast glucan | Saccharomyces cerevisiae | (1→6)(1→3)-β-d-glucan (B-on-B) | 17,200 | 0.8 |
| Betafectin | Saccharomyces cerevisiae | (1→6)(1→3)-β-d-glucan (B-on-B) | 150,000 | 0.8 |
| Laminarin | Laminaria digitata | (1→6)(1→3)-β-d-glucan (LSB) | 5,850 | 5,000 |
| Carboxymethyl cellulose | Synthetic | (1→4)-β-d-glucan (L) | NDc | |
| Pustulan | Umbilicaria papullosa | (1→6)-β-d-glucan (L) | 20,000 | 1,000 |
| Dextran | Leuconostoc mesenteroides | (1→6)-α-d-glucan (L) | 513,000 | NDc |
| Mannan | Saccharomyces cerevisiae | (1→2)(1→3)(1→6)-α-d-glucan (B) | 34,500 | NDc |
See reference 25. L, Linear; B-on-B, branch-on-branch; LSB, linear with side branches; B, branched.
ND, not detected.
Maximum concentration tested, 200 ng/ml.
Maximum concentration tested, 5 μg/ml.
We tested cultures of nine fungi commonly isolated from house dust for (1→3)-β-d-glucans. The culture of a Eurotium species showed a high level of (1→3)-β-d-glucans, compared with the culture of its anamorph Aspergillus and individual cultures of other fungal species (Table 2). The culture of an environmental Stachybotris isolate had very low levels of detectable (1→3)-β-d-glucans. Repeated assays at high concentrations were required to detect any glucans in the Stachybotris culture.
TABLE 2.
(1→3)-β-d-Glucan levels in cultured fungal isolates as measured by a monoclonal IgM ELISAa
| Fungus | Source of isolate | (1→3)-β-d-glucan concn (ng/mg) |
|---|---|---|
| Eurotium sp. | Air sample, bedroom | 2,200 |
| Aspergillus niger | Stored urine | 190 |
| Aspergillus flavus | Stored urine | 160 |
| Aspergillus ochraceus | Air sample, outdoors | 57 |
| Penicillum corylophilum | Air sample, indoor basement | 170 |
| Alternaria sp. | Air sample, bedroom | 120 |
| Cladosporium sp. | Air sample, bedroom | 78 |
| Stachybotris chatarum sp. | Wallboard | 2.3 |
| Wallemia sp. | Air sample, outdoors | 13 |
Results are representative data from repeated assays of extracts made from single fungal cultures.
(1→3)-β-d-Glucans were not detected in unspiked freshly diluted working-strength metal working fluid samples. The spiked solutions of neat synthetic and neat semisynthetic metal working fluids showed 68 and 44% recoveries of (1→3)-β-d-glucans, respectively (Table 3). The soluble metal working fluid showed a very low recovery of 0.19% (1→3)-β-d-glucan.
TABLE 3.
Percent recovery of (1→3)-β-d-glucans from metal working fluid samples
| Neat samplea | % Recovery of (1→3)-β-d-glucans |
|---|---|
| Synthetic | |
| 1 | 65.93 |
| 2 | 69.84 |
| Semi synthetic | |
| 1 | 43.68 |
| 2 | 43.61 |
| Soluble | |
| 1 | 0.19 |
| 2 | 0.19 |
Duplicate samples were tested.
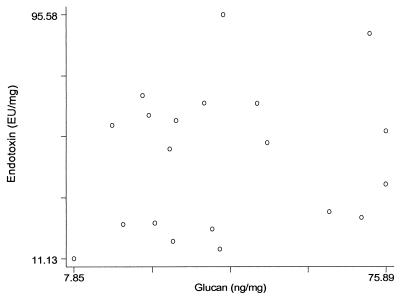
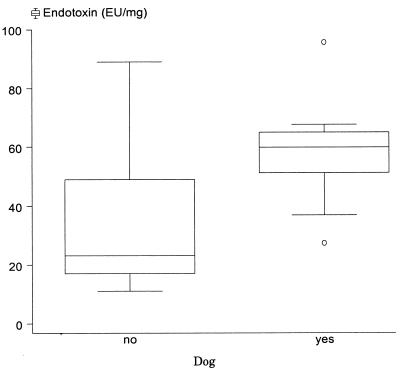
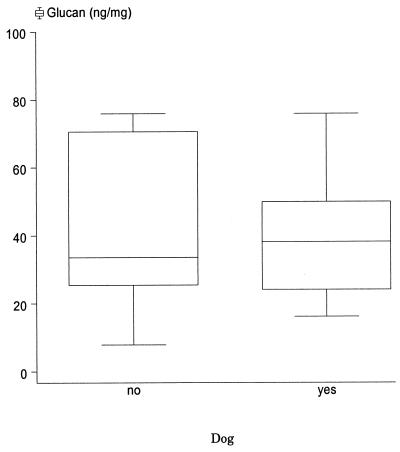
We assessed 20 house dust samples, 10 from houses with dogs plus another 10 from houses without dogs, for endotoxin and (1→3)-β-d-glucans. There was no significant correlation between endotoxin (geometric mean [GM], 38.65 endotoxin units [EU/mg] with reference to the United States Pharmacopeial Convention standard ECG); geometric standard deviation (GSD), 1.88; n = 20) and glucan (GM, 35.1 ng/mg; GSD, 1.80; n = 20) levels in house dust samples (Fig. 1). The samples collected from the houses having dogs showed significantly higher endotoxin levels (GM, 55.66 EU/mg; GSD, 1.41) than those collected from the houses without dogs (GM, 26.84 EU/mg; GSD, 1.91) (t = 3.14; two-tailed P = 0.007) (Fig. 2). There was no significant difference between geometric mean glucan levels for the samples collected from the houses having dogs (GM, 36.76 ng/mg; GSD, 1.62) and those collected from the houses without dogs (GM, 33.58 ng/mg; GSD, 2.02) (t = 0.33; two-tailed P = 0.74) (Fig. 3).
FIG. 1.
House dust endotoxins and house dust (1→3)-β-d-glucans. Samples from the main living area of 20 Connecticut homes participating in a study of childhood asthma were assayed for both endotoxins and (1→3)-β-d-glucans.
FIG. 2.
House dust endotoxins and the presence of a dog. The samples shown in Fig. 1 were divided into two groups, 10 samples from homes with dogs and 10 samples from homes without dogs. The upper and lower box edges show the inner quartile range, the line across the box is the median, the error bars show the limits of the data within two times the inner quartile range from the median, and circles denote the locations of outliers.
FIG. 3.
(1→3)-β-d-Glucans in house dust and the presence of a dog. See the legend to Fig. 2 for details.
The coefficient of variation for (1→3)-β-d-glucan in the house dust samples (based on triplicate analyses) was 7.80%.
DISCUSSION
The results presented in Table 1 indicate that the monoclonal antibody is highly specific for (1→6) branched,(1→3)-β-d-glucans, such as baker's yeast glucan and Betafectin. Based on the linkages, baker's yeast glucan can be classified as a branch-on-branch (1→6)(1→3)-β-d-glucan (28). The baker's yeast glucan that we obtained from Sigma was reported by the manufacturer to consist of 85% β-1,3 linkages and 3% β-1,6 linkages. Similarly, Betafectin is a branch-on-branch (1→6)(1→3)-β-d-glucan—a highly purified, water-soluble, pharmaceutical-grade (1→3)-β-d-glucan manufactured from S. cerevisiae (35).
Mushroom glucan showed a response at a concentration range of 60 to 5,000 ng/ml. According to the manufacturer, mushroom glucan is a (1→6) branched, (1→3)-β-d-glucan, composed of a β-1,3-glucan base with branching at every third glucose unit of alternating β-1,6 and β-1,4 chains. The interspersed nature of the β(1→4)(1→3) and β(1→6)(1→3) branches may be the reason why mushroom glucan reacted only at very high concentrations (on a weight basis) compared to those of baker's yeast and Betafectin.
The nonreactivity of the antibody with other (1→3)-β-d-glucans, such as curdlan [linear, essentially homogeneous (1→3)-β-d-glucan] and barley glucan [linear, (1→3)(1→4)-β-d-glucan, with 70% β-1,4 linkages and 30% β-1,3 linkages, according to the manufacturer], was due to their linear structures and different linkages. The assay described here detects specifically branch-on-branch (1→6)(1→3)-β-d-glucans with a sensitivity more than 5,000 times greater than that for laminarin [linear, (1→3)-β-d-glucan, with (1→6)-β-glucosyl side branches]. Similar to the results of Douwes et al. (3), we also found evidence of (1→6) branched, (1→3)-β-d-glucans in pustulan obtained from Calbiochem.
Previous studies have shown that there is a trend for high-molecular-weight glucans or (1→6) branched, (1→3)-β-d-glucans to be more stimulatory (2, 19). According to Ohno et al. (19), a high molecular weight, a high degree of branching, and a helical structure are important for in vivo priming of macrophages for lipopolysaccharide-triggered tumor necrosis factor alpha release. An in vitro study has also concluded that the cytokine-stimulating activity of (1→3)-β-d-glucans is dependent on branching pattern, molecular weight, and triple-helix conformation (7). Therefore, the assay described here, specific for (1→6) branched, (1→3)-β-d-glucans, may be a good method for determining exposure to glucans likely to have important health effects. However, this assay is not a good measure of fungal biomass, because fungi vary greatly in their glucan contents, as shown in Table 2. Thus, other markers, such as ergosterol, may be more appropriate if measurement of fungal biomass is the goal.
Exposure to metal working fluids can cause respiratory illnesses (12, 13). Endotoxins and fungi are often present in the air of workplaces using water-based metal working fluids and implicated as causal factors in work-related respiratory illnesses (13, 14). Therefore, in this study, we investigated the utility of the new ELISA method for quantifying (1→3)-β-d-glucans in metal working fluids. Unfortunately, metal working fluid samples showed some inhibition in the glucan assay. The low recovery may have been due to washing off of the coating agent (galactosyl ceramide) by the surfactants in metal working fluids.
The assay described here was more sensitive (detection level, 0.8 ng/ml) than the inhibition enzyme immunoassay (detection level, 40 ng/ml) described by Douwes et al. (3). The reproducibility of our assay was also high.
The settled house dust samples collected from the houses having dogs showed high endotoxin levels. A recent cohort study on the relative risk of wheezing in relation to house dust endotoxins concluded that the presence of a dog was an important contributor to increased endotoxin levels in house dust (22). This association was evident, even in the small number of samples studied here. However, we did not find a similar association of glucans with the presence of a dog in the home. The variability of (1→3)-β-d-glucans across all the samples (GSD, 1.80) was almost the same as that of endotoxins (GSD, 1.88).
Our assay is extremely specific, highly sensitive, and reproducible. Therefore, this assay can be very useful for exposure assessment in epidemiological studies.
ACKNOWLEDGMENTS
This work was supported by National Institute for Occupational Safety and Health grant R01 OH03489, by National Institute of Environmental Health Sciences grant R01 ES007036, and by National Institute of Environmental Health Sciences Center grant 2P30ES00002.
We are grateful to Brian Leaderer, Yale School of Medicine, for providing house dust samples and the participants in Childhood Asthma Study—Phase II for their cooperation with sample collections. We thank The Collaborative Group for providing Betafectin and the monoclonal antibody for the study. We also thank Denise Schwerzler, Department of Environmental Science and Engineering, Harvard School of Public Health, for sharing expertise with us.
REFERENCES
- 1.Chew G L, Higgins K M, Milton D K, Burge H A. The effects of carpet fresheners and other additives on the behaviour of indoor allergen assays. Clin Exp Allergy. 1999;29:470–477. doi: 10.1046/j.1365-2222.1999.00490.x. [DOI] [PubMed] [Google Scholar]
- 2.Cleary J A, Kelly G E, Husband A J. The effect of molecular weight and β-1,6-linkages on priming of macrophage function in mice by (1,3)-β-d-glucan. Immunol Cell Biol. 1999;77:395–403. doi: 10.1046/j.1440-1711.1999.00848.x. [DOI] [PubMed] [Google Scholar]
- 3.Douwes J, Doekes G, Montijn R, Heederik D, Brunekreef B. Measurement of β(1→3)-glucans in the occupational and home environment with an inhibition enzyme immunoassay. Appl Environ Microbiol. 1996;62:3176–3182. doi: 10.1128/aem.62.9.3176-3182.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Douwes J, McLean D, van der Maarl E, Heederik D, Pearce N. Worker exposures to airborne dust, endotoxin and β(1,3)-glucan in two New Zealand sawmills. Am J Ind Med. 2000;38:426–430. doi: 10.1002/1097-0274(200010)38:4<426::aid-ajim8>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 5.Douwes J, Wouters I, Dubbeld H, van Zwieten L, Steerenberg P, Doekes G, Heederik D. Upper airway inflammation assessed by nasal lavage in compost workers: a relation with bio-aerosol exposure. Am J Ind Med. 2000;37:459–468. doi: 10.1002/(sici)1097-0274(200005)37:5<459::aid-ajim2>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 6.Douwes J, Zuidhof A, Doekes G, van der Zee S, Wouters I, Boezen H M, Brunekreef B. (1→3)-β-d-Glucan and endotoxin in house dust and peak flow variability in children. Am J Respir Crit Care Med. 2000;162:1348–1354. doi: 10.1164/ajrccm.162.4.9909118. [DOI] [PubMed] [Google Scholar]
- 7.Falch B H, Espevik T, Ryan L, Stokke B T. The cytokine stimulating activity of (1→3)-β-d-glucans is dependent on the triple helix conformation. Carbohydr Res. 2000;329:587–596. doi: 10.1016/s0008-6215(00)00222-6. [DOI] [PubMed] [Google Scholar]
- 8.Fisette L, Crotty C, Mackin W. Proceedings of Focus on Fungal Infections, 4 to 6 March 1998, Orlando, Fla. 1998. Development of a novel β-glucan-detection ELISA as a diagnostic assay for systemic fungemia. [Google Scholar]
- 9.Fogelmark B, Goto H, Yuasa K, Marchat B, Rylander R. Acute pulmonary toxicity of inhaled β-1,3-d-glucan and endotoxin. Agents Action. 1992;35:50–56. doi: 10.1007/BF01990951. [DOI] [PubMed] [Google Scholar]
- 10.Fogelmark B, Sjöstrand M, Ryalnder R. Pulmonary inflammation induced by repeated inhalations of β(1,3)-d-glucan and endotoxin. Int J Exp Pathol. 1994;75:85–90. [PMC free article] [PubMed] [Google Scholar]
- 11.Gomaa K, Kraus J, Roβkopf F, Röper H, Franz G. Antitumor and immunological activity of a β1→3/1→6 glucan from Glomerella cingulata. J Cancer Res Clin Oncol. 1992;118:136–140. doi: 10.1007/BF01187502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greaves I A, Eisen E A, Smith T J, Pothier L J, Kriebel D, Woskie S R, Kennedy S M, Shalat S, Monson R R. Respiratory health of automobile workers exposed to metal-working fluid aerosols: respiratory symptoms. Am J Ind Med. 1997;32:450–459. doi: 10.1002/(sici)1097-0274(199711)32:5<450::aid-ajim4>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 13.Kriebel D, Sama S R, Woskie S, Christiani D C, Eisen E A, Hammond S K, Milton D K, Smith M, Virji M A. A field investigation of the respiratory effects of metal working fluids. 1. Effects of aerosol exposures. Am J Ind Med. 1997;31:756–766. doi: 10.1002/(sici)1097-0274(199706)31:6<756::aid-ajim13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 14.Laitinen S, Linnainmaa M, Laitinen J, Kiviranta H, Reiman M, Liesivuori J. Endotoxins and IgG antibodies as indicators of occupational exposure to the microbial contaminants of metal-working fluids. Int Arch Occup Environ Health. 1999;72:443–450. doi: 10.1007/s004200050397. [DOI] [PubMed] [Google Scholar]
- 15.Ljungman A G, Leanderson P, Tagesson C. (1→3)-β-d-Glucan stimulates nitric oxide generation and cytokine mRNA expression in macrophages. Environ Toxicol Pharmacol. 1998;5:273–281. doi: 10.1016/s1382-6689(98)00011-8. [DOI] [PubMed] [Google Scholar]
- 16.Milton D K, Feldman H A, Neuberg D S, Bruckner R J, Greaves I A. Environmental endotoxin measurement: the kinetic Limulus assay with resistant-parallel-line estimation. Environ Res. 1992;57:212–230. doi: 10.1016/s0013-9351(05)80081-7. [DOI] [PubMed] [Google Scholar]
- 17.Milton D K, Johnson D K, Park J H. Environmental endotoxin measurement: interference and sources of variation in the Limulus assay of house dust. Am Ind Hyg Assoc J. 1997;58:861–867. doi: 10.1080/15428119791012199. [DOI] [PubMed] [Google Scholar]
- 18.Nagi N, Ohno N, Adachi Y, Aketagawa J, Tamura H, Shibata Y, Tanaka S, Yadomae T. Application of Limulus test (G pathway) for the detection of different conformers of (1→3)-β-d-glucans. Biol Pharm Bull. 1993;16:822–828. doi: 10.1248/bpb.16.822. [DOI] [PubMed] [Google Scholar]
- 19.Ohno N, Asada N, Adachi Y, Yadomae T. Enhancement of LPS triggered TNF-α (tumor necrosis factor-α) production by (1→3)-β-d-glucans in mice. Biol Pharm Bull. 1995;18:126–133. doi: 10.1248/bpb.18.126. [DOI] [PubMed] [Google Scholar]
- 20.Ohno N, Miura N N, Chiba N, Adachi Y, Yadomae T. Comparison of the immunopharmacological activities of triple and single-helical Schizophyllan in mice. Biol Pharm Bull. 1995;18:1242–1247. doi: 10.1248/bpb.18.1242. [DOI] [PubMed] [Google Scholar]
- 21.Ormstad H, Groeng E C, Løvik M, Hetland G. The fungal cell wall component β-1,3-glucan has an adjuvant effect on the allergic response to ovalbumin in mice. J Toxicol Environ Health. 2000;61:55–67. doi: 10.1080/00984100050116780. [DOI] [PubMed] [Google Scholar]
- 22.Park J H, Gold D R, Spiegelman D L, Burge H A, Milton D K. House dust endotoxin and wheeze in the first year of life. Am J Respir Crit Care Med. 2001;163:322–328. doi: 10.1164/ajrccm.163.2.2002088. [DOI] [PubMed] [Google Scholar]
- 23.Ramani M, Howell C J, Spur B W, Youlten L J F, Clark T J M, Lessof M H, Lee T H. The generation and cellular distribution of leukotriene C4 in human eosinophils stimulated by unopsonized zymosan and glucan particles. Clin Immunol. 1988;81:696–705. doi: 10.1016/0091-6749(88)91041-x. [DOI] [PubMed] [Google Scholar]
- 24.Rylander R. Airway responsiveness and chest symptoms after inhalation of endotoxin or (1→3)-β-d-glucan. Indoor Built Environ. 1996;5:106–111. [Google Scholar]
- 25.Rylander R, Persson K, Goto H, Yuasa K, Tanaka S. Airborne beta-1,3-glucan may be related to symptoms in sick buildings. Indoor Environ. 1992;1:263–267. [Google Scholar]
- 26.Saito K, Nishijima M, Ohno N, Nagi N, Yadomae T, Miyazaki T. Activation of complement and limulus coagulation systems by an alkali-soluble glucan isolated from Omphalia lapidescens and its less branched derivates. Chem Pharm Bull. 1992;40:1227–1230. doi: 10.1248/cpb.40.261. [DOI] [PubMed] [Google Scholar]
- 27.Sakurai T, Ohno N, Yadomae T. Changes in immune mediators in mouse lung produced by administration of soluble (1→3)-β-d-glucan. Biol Pharm Bull. 1994;17:617–622. doi: 10.1248/bpb.17.617. [DOI] [PubMed] [Google Scholar]
- 28.Stone B A, Clarke A E. Chemistry and biology of (1→3)-β-d-glucans. Victoria, Australia: La Trobe University Press; 1992. [Google Scholar]
- 29.Tanaka S, Aketagawa J, Takahashi S, Shibata Y, Tsumuraya Y, Hashimato Y. Activation of Limulus factor G by (1→3)-β-d-glucans. Carbohydr Res. 1991;218:167–174. doi: 10.1016/0008-6215(93)80008-3. [DOI] [PubMed] [Google Scholar]
- 30.Thorn J, Rylander R. Airway inflammation and glucan in a rowhouse area. Am J Respir Crit Care Med. 1998;157:1798–1803. doi: 10.1164/ajrccm.157.6.9706081. [DOI] [PubMed] [Google Scholar]
- 31.van Strien R T, Doekes G, Douwes J, Koopman L P, Kerkhof M, Aalberse R C, Brunekreef B. Home characteristics and levels of endotoxin, β(1,3), glucan, and fungal polysaccharide antigen in house dust in the PIAMA study. J Allergy Clin Immunol. 2000;104:S374–S375. [Google Scholar]
- 32.Wan G H, Li C S. Indoor endotoxin and glucan in association with airway inflammation and systemic symptoms. Arch Environ Health. 1999;54:172–179. doi: 10.1080/00039899909602256. [DOI] [PubMed] [Google Scholar]
- 33.Wouters I M, Douwes J, Doekes G, Thorne P S, Brunekreef B, Heederik D J J. Increased levels of markers of microbial exposure in homes with indoor storage of organic household waste. Appl Environ Microbiol. 2000;66:627–631. doi: 10.1128/aem.66.2.627-631.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang K, Petty H R. Influence of polysaccharides on neutrophil function: specific antagonists suggest a model for cooperative saccharide-associated inhibition of immune complex-triggered superoxide production. J Cell Biochem. 1994;56:225–235. doi: 10.1002/jcb.240560217. [DOI] [PubMed] [Google Scholar]
- 35.Zimmerman J W, Lindermuth J, Fish P A, Palace G P, Stevenson T T, DeMong D E. 1998. A novel carbohydrate-glycosphingolipid interaction between a β-(1–3)-glucan immunomodulator, PGG-glucan, and lactosylceramide of human leukocytes. J Biol Chem. 2020;273:22014–22020. doi: 10.1074/jbc.273.34.22014. [DOI] [PubMed] [Google Scholar]